Abstract
Introduction:
Extraforaminal stenosis in L5–S1, or far-out syndrome (FOS), is defined as L5 nerve compression by the transverse process (TP) of the L5 and the ala of the sacrum and disc bulging with/without osteophytes and/or the thickened lumbosacral and extraforaminal ligament. This study aims to describe the unilateral biportal endoscopic decompression technique of the extraforaminal stenosis at L5–S1 or far out syndrome and evaluate its clinical results with a literature review.
Case Report:
A 44-year-old male presented with severe right sharp shooting pain in the buttock, thigh, leg, foot, and/or toes with numbness in the foot and toes (Visual Analog Scale [VAS] 8/10) for six months with an Oswestry disability index (ODI) score of 70%. Her pain aggravated when bending forward and performing daily routine activities. He also complained of exaggeration of pain in daily regular activities. On physical examination, power in the right lower limbs was 5/5 as per the Medical Research Council (MRC) grading, and deep tendon reflexes were normal. Pre-operative X-ray and CT scan showed no instability or calcified disc osteophyte, and magnetic resonance imaging showed extraforaminal stenosis due to disc herniation at L5–S1 in Figure 1. We performed UBE-L5-S1extraforaminal discectomy surgery to resolve his symptoms. The operative time was 68 min; blood loss was 30 mL. After surgery, the patient was followed up at one week, six weeks, three months, six months, 12 months, and two years. The pain and tingling sensation in the legs improved at the 1-week follow-up, with a VAS score of 0/10 and an ODI score of 10% at the 2-year follow-up. Patient satisfaction was surveyed using Macnab’s criteria at the final follow-up visit of 2 years and was found to be excellent. Post-operative imaging showed a good extraforaminal decompression at L5-S.
Conclusion:
Unilateral biportal endoscopy technique has brought a paradigm shift in the treatment of spinal pathologies and has served as another treatment option for the past two decades. The UBE decompression technique for extraforaminal stenosis at L5–S1 has the advantages of minimally invasive spine surgery; it is a safe and effective treatment option for treating extraforaminal stenosis at L5–S1.
Keywords: Unilateral biportal endoscopy, L5–S1 Extraforaminal stenosis, far-out syndrome, minimally invasive spine surgery, lumbar spine
Learning Point of the Article:
The UBE decompression technique for extraforaminal stenosis at L5–S1 has the advantages of minimally invasive spine surgery; it is a safe and effective treatment option for treating extraforaminal stenosis at L5–S1.
Introduction
Extraforaminal stenosis in L5–S1, or far-out syndrome (FOS), is defined as L5 nerve compression by the transverse process (TP) of the L5 and the ala of the sacrum and/or disc bulging with/without osteophytes and/or the thickened lumbosacral and extraforaminal ligament. Wiltse et al., in 1984, initially described the condition [1]. Conservative treatment, which includes analgesics, rest, and pain block procedures, is the first line of treatment for the L5–S1 extraforaminal disc/stenosis/farout syndrome or Bertolotti syndrome. Surgery is indicated if conservative treatment is not successful in improving the symptoms. The diagnosis of extraforaminal stenosis at L5–S1 is critical with clinical presentation and symptoms of L5 nerve root compression- such as a sharp shooting pain in the buttock, thigh, leg, foot, and/or toes. With numbness in the foot and/or toes with the radiological presentation of extraforaminal stenosis at L5–S1[2]. Various surgical techniques have been described, like conventional lumbosacral decompression and fusion surgery, paraspinal/Wiltse approach for decompression, minimallyinvasive decompressive surgery, or recently full endoscopic spine surgery decompression for the treatment of the extraforaminal stenosis at L5–S1[3]. This study aims to describe the unilateral biportal endoscopic decompression technique of the extraforaminal stenosis at L5–S1 or far out syndrome and evaluate its clinical results with a literature review.
Technical note
Careful pre-operative planning is essential with imaging modalities such as X-ray images, three-dimensional computed tomography, and magnetic resonance imaging scans to look for disc bulging with/without osteophytes and/or the thickened lumbosacral and extraforaminal ligament L5 nerve compression by the transverse process (TP) of the L5 and the ala of the sacrum, and the neuroforamen area with dynamic instability of the lumbosacral junction. Also, diagnosis of the lumbosacral transitional vertebrae with its four subtypes is essential in some cases. Type I is associated with hypertrophied L5 transverse process and fusion with the sacral ala (Bertolotti syndrome), and types II and IV are associated with a pseudo-articulation between the L5 transverse process and the sacral ala, accelerating degeneration and leading to facet arthritis and extraforaminal compression of the L5 nerve root [4].
Case Report
A 44-year-old male presented with severe right sharp shooting pain in the buttock, thigh, leg, foot, and/or toes with numbness in the foot and toes (Visual Analog Scale [VAS] 8/10) for six months with an Oswestry disability index (ODI) score of 70%. Her pain aggravated when bending forward and performing daily routine activities. He also complained of exaggeration of pain in daily regular activities. On physical examination, power in the right lower limbs was 5/5 as per the Medical Research Council grading, and deep tendon reflexes were normal. Pre-operative Xray and CT scan showed no instability or calcified disc osteophyte, and magnetic resonance imaging showed extraforaminal stenosis due to disc herniation at L5–S1 (Fig. 1A,1B). We performed UBE-L5-S1extraforaminal discectomy surgery to resolve his symptoms. The operative time was 68 min; blood loss was 30 mL. After surgery, the patient was followed up at one week, six weeks, three months, six months, 12 months, and two years. The pain and tingling sensation in the legs improved at the 1-week follow-up, with a VAS score of 0/10 and an ODI score of 10% at the 2-year follow-up. Patient satisfaction was surveyed using Macnab’s criteria at the final follow-up visit of 2 years and was found to be excellent. Post-operative imaging showed a good extraforaminal decompression at L5-S1 (Fig. 2A,2B).
Figure 1.

A 44-year-old male patient presented with right-sided leg pain. (1A, 1B) The axial and oblique T2-weighted magnetic resonance(MR) images show extraforaminal entrapment of the L5 nerve root with disc protrusion (white arrows).
Figure 2.
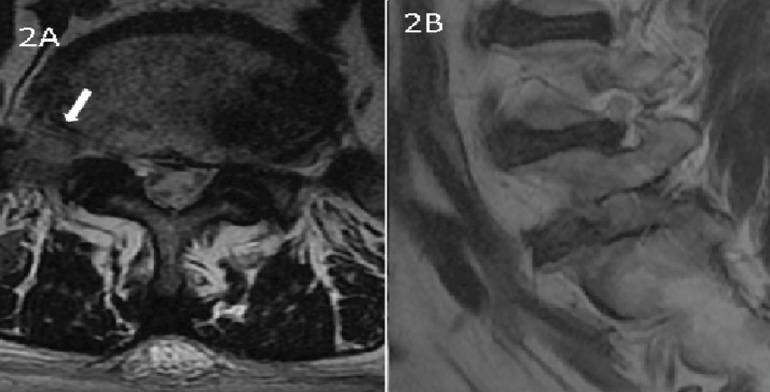
This patient was treated by a unilateral biportal endoscopic approach. (2A,2B) The postoperative MR images reveal complete decompression of the L5 nerve root after unilateral biportal endoscopic surgery (white arrows).
Technical Note
Stepw ise A pproach for UBE- L5- S1 ex traforaminal discectomy/decompression
1.Patient position and Anesthesia
The patient is positioned prone under general endotracheal anesthesia. However, surgeons can choose limited epidural anesthesia with sedation or their preferred choice of anesthesia.
2. Skin Marking
It is essential for the surgeon to get the orientation of the anatomy before skin incision. Under C-arm fluoroscopic guidance, we marked the pedicle of L5 and S1, the L5-S1 disc space, the transverse process of L5, and the iliac crest. The target area of surgery is confirmed and marked as the superior sacral notch (the junction between the lateral aspect of the superior articular process [SAP] and sacral ala) on an anteroposterior view of the C-arm fluoroscopy. The authors suggest using the dominant hand for the working portal and the nondominant hand for the endoscopic portal. In the case of a left-sided disc approached by a right-handed surgeon, the cranial left portal should be planned as the endoscopic portal and the caudal right portal as a working portal. In the case of a right-side approach, the cranial right portal was usually planned as the working portal, and the caudal left portal was the endoscopic portal.
3. Skin Incision and Portal Placement
The incisions are approximately 2.5-3.5 cm apart, 1 cm above and 1 cm below the midpoint of the foramen in the C-arm fluoroscopic view and 1 cm lateral to the target L5-S1 foramen. When the caudal incision interferes from the iliac crest due to high riding iliac crest, a caudal incision can be made medially to avoid the iliac crest. The authors’ preferred incisions for the upper portal were about 1cm lateral to the border of the L5 pedicle, and the lower portal was made around the upper endplate of S1 to make sure the landing point and joining of the two portals was over the ipsilateral transverse process of L5(Fig. 3).
Figure 3.

Fluoroscopy image demonstrating working portal and endoscopic portal used for UBE decompression of extraforaminal stenosis at L5–S1.
.4. Gentle Periosteal Dissection
After passing through the skin and fascia, tactile bony feedback is confirmed on the dorsal surface of the L5 lamina, SAP, and transverse process. The endoscopic irrigation system helps form a water chamber above the lamina, which helps to control bleeding with its hydrostatic pressure and provides clear vision over the surgical field. The periosteal dissection is continued to expose the transverse process, mamillary process, isthmus, lateral border of superior articular process, and sacral ala with the help of radiofrequency (RF) probes. The surgical target area of the caudal portion of the L5 transverse process, the lateral portion of the facet, and the sacral ala were identified and exposed with more precision.
5. The Bone Resection
The inferior aspect of TP of L5, the superomedial part of the sacral ala, and the lateral aspect of the SAP of S1 are removed with a high-speed diamond burr first, followed by Kerrison rongeur if necessary. The use of Kerrison rongeur should be very careful and delicate as dorsal root ganglion(DRG) is a highly sensitive and injury-prone structure due to its location and anatomy. The bony resection is considered adequate when the ligament is released from the bony structures. Any bony bleeding, if it occurred, can be encountered with RF or fibrin glue or, bone wax or fibrillar patch. Authors prefer to use RF and fibrin glue over bone wax or fibrillar patch as if these structures retained in the neuroforamen can possibly cause compression of the nerve in the limited space.
6. The Ligament Resection
Once the bony resection is completed, the cranial portion of the ligament is detached and reflected from SAP and TP using a nerve hook/probe/freer/angled curette, followed by resection with Kerrison rongeur. Once the ligament is resected, the exiting nerve root is easily identified. The possible source of bleeding at this step comes from the complex plexus of veins and adhesion around neurovascular structures. The use of radiofrequency (RF) probes of various types, like 30°, 90°, and ball type, is highly suggested to prevent blood loss before cutting epidural veins.
7. Discectomy
The nerve root/DRG is handled gently with a nerve hook, and disc particles are freed with a nerve hook, followed by disc removal with pituitary forceps. The L5 exiting root was assessed from the foraminal to the extraforaminal with nerve hooks to test for residual compression(Fig. 4).
Figure 4.

Endoscopy view demonstrating L5–S1 protruded extraforaminal disc fragment with compressed right L5 nerve root.
8. Wound closure
The authors preferred to close the subcutaneous layer with absorbable suture after inserting a drain, followed by skin closure with glue materials.
Discussion
The diagnosis of extraforaminal stenosis at L5–S1 is critical. Surgeons should give utmost importance to clinical evaluation and presentation of L5 nerve root compression symptoms. The radiological presentation of extraforaminal stenosis at L5–S1. Conventional methods of diagnosing extraforaminal stenosis at L5–S1 with routine axial and sagittal MR images might be inadequate. Oblique coronal images are handy for the radiological diagnosis of extraforaminal entrapment of the L5 nerve root [5,6]. Few physicians use diffuse tensor images, too, for the same [7]. Authors prefer to use oblique foraminal MRI to diagnose extraforaminal stenosis at L5–S1, and it is part of their standard practice to include oblique foraminal MRI images in diagnosis and to provide additional diagnostic information. CT, dynamic X-rays, and bone scans are also crucial for the diagnosis of L5–S1 extraforaminal stenosis/ far out syndrome/ Bertolotti syndrome. Bertolotti syndrome needs a special mention here. Bertolotti syndrome is a congenital disorder leading to an almost similar clinical presentation like L5–S1 extraforaminal stenosis/ far out syndrome with back pain. It is associated with a lumbosacral transitional vertebra (LSTV), which occurs due to the articulation of the L5 vertebra transverse process(es) with the sacrum, leading to irregular spinal mobility and pain. Very few patients need surgical treatment with resection of the enlarged transverse process and decompression of extraforaminal stenosis at L5–S1[4]. Treatment options have evolved across the last four decades for the surgical management of L5–S1 extraforaminal stenosis, from initial descriptions of the Wiltse approach in 1984 to microscopic decompressive surgeries to full endoscopic approaches[1,8]. Recently, few reports of the UBE approach have also been explained in the literature.
The UBE approach necessitates appropriate coordination between both hands and steady instrument operation with a single hand through the working portal. Both hands are required to operate simultaneously, and the authors preferred to handle the lens in the non-dominant left hand and surgical tools in the right dominant hand. Spinal surgeons need to familiarize themselves with the arthroscopic tools, synchronize their perception of the depth and direction of the lens, move the instruments swiftly and smoothly in and out of the instrument channel, and quickly acquire the field of view in the early phase of the procedure during their learning curve. UBE has several advantages, including minimizing extensive muscle dissection, less blood loss, less post-operative pain, and faster recovery from the surgery. The UBE-TLIF is a versatile approach with good vision, which provides a feasible advantage of reducing muscle damage, blood loss, complications, length of stay, early postoperative recovery, and return to work. The endoscopic fusion technique is performed using 1.5-mm portals; as mentioned earlier, the working portal for the instruments and viewing portal for the endoscope are separate, which helps in the surgical instrument’s handling, making it more convenient than uniportal surgery [9,10].
Moreover, it is worth recalling that there is no surgical range limitation because of the unfettered accessibility of the endoscope. In addition, endoscopic surgery does not simply mean surgery with small skin incisions and wounds. There is no massive bleeding because there is minimal muscle damage and continuous irrigation with hydrostatic pressure. Furthermore, it is widely known that endoscopic surgery is a water-medium technique with an endoscopic lens view of the operative field more specified, showing vital structures at 40–50 times magnification. Continuous real-time irrigation washout naturally forms a water chamber, which helps control bleeding due to hydrostatic pressure and provides clear surgical field visibility. Consequently, clear and high-ratio viewing causes more precise operations, enabling safer surgery. Furthermore, dural tears and cerebral spinal fluid leakage from the previous laminectomy and the risks of infection are very low as the muscle dissection with UBE is minimal.
Fundamentally, most conventional surgery instruments can be inserted with the working portal, and the degree of freedom in selecting surgical instruments is high. Furthermore, the posterior approach in the case of a traditional extension of fusion surgery has the apparent burden of revision on the previous operative area. The cost-effectiveness of this technique can be demonstrated by enabling faster post-operative recovery and an early return to work or social life. In addition, implementing UBE technology does not require the purchase of special lenses and instruments, as seen in the percutaneous transforaminal endoscopic technique. UBE can use general arthroscopic lenses and open spinal surgical instruments, which is more conducive to wide acceptance in most hospitals. There were supplemental benefits, no need for transfusion due to low bleeding during surgery, and a lesser chance of infection. In addition, the other benefits of this approach include enhanced recovery after surgery, even in severely comorbid patients, as it is one of the most minimally invasive endoscopic approaches with minimal post-operative morbidity compared to conventional open surgery[11].
UBE surgery has various advantages over microtubular retractor surgery as UBE is a water-based surgery: The hydrostatic pressure helps to reduce bleeding, constant irrigation helps to separate soft tissue layers such as a thecal sac and ligamentum flavum, the irrigation effect also reduces the risk of infection, and the endoscope can go into the canal; thus, a clear or magnified view can help to see and differentiate anatomical structures in more detail. With tubular retractors, the vision is limited, and the range of motion of surgical instruments is restricted and limited to the tube [12–16].
Limitations
The limitations of the UBE include the learning curve associated with the new technique and the risk of retroperitoneal fluid collection by continuous saline irrigation in the paraspinal Wiltse approach, leading to abdominal pain and discomfort, intracranial pressure elevation, dural irritation and seizure induction. Hence, the authors recommend that surgical time should be quick and completed within 30-45 minutes to avoid risks of these complications. Also, at the L5-S1 disc target area, critical anatomical structures like the common iliac vasculature and its branches are in close vicinity to the anterior surface of the disc. Hence, great precautions are necessary in this area to avoid
Conclusion
Unilateral biportal endoscopy has brought a paradigm shift in the treatment of spinal pathologies and has served as another treatment option for the past two decades. The UBE decompression technique for extraforaminal stenosis at L5–S1 has the advantages of minimally invasive spine surgery; it is a safe and effective treatment option for treating extraforaminal
Clinical Message.
The UBE decompression technique for extraforaminal stenosis at L5–S1 has the advantages of minimally invasive spine surgery; it is a safe and effective treatment option for treating extraforaminal stenosis at L5–S1.
Biography






Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Wiltse LL, Guyer RD, Spencer CW, Glenn W V, Porter IS. Alar transverse process impingement of the L5 spinal nerve:the far-out syndrome. Spine (Phila Pa |y1976) 1984;9:31–41. doi: 10.1097/00007632-198401000-00008. https://doi.org/10.1097/00007632-198401000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Lee S, Kang JH, Srikantha U, Jang IT, Oh SH. Extraforaminal compression of the L-5 nerve root at the lumbosacral junction:clinical analysis, decompression technique, and outcome. J Neuro surg Spine. 2014;20:371–9. doi: 10.3171/2013.12.SPINE12629. https://doi.org/10.3171/2013.12. SPINE12629. [DOI] [PubMed] [Google Scholar]
- 3.Sasaki M, Aoki M, Matsumoto K, Tsuruzono K, Akiyama C, Yoshimine T. Middle-term surgical outcomes of microscopic posterior decompression for far-out syndrome. J Neurol Surg A Cent Eur Neurosurg. 2014;75:79–83. doi: 10.1055/s-0032-1327443. https://doi.org/10.1055/S-0032-1327443. [DOI] [PubMed] [Google Scholar]
- 4.Jancuska JM, Spivak JM, Bendo JA. A Review of Symptomatic Lumbosacral Transitional Vertebrae:Bertolotti's Syndrome. Int J Spine Surg. 2015;9 doi: 10.14444/2042. https://doi.org/10.14444/2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heo DH, Kim SW, Chang HH, Park CK. Usefulness of Oblique Lumbar Magnetic Resonance Imaging for Nerve Root Anomalies and Extraforaminal Entrapment Lesions. Asian Spine J. 2018;12:423–7. doi: 10.4184/asj.2018.12.3.423. https://doi.org/10.4184/ASJ.2018.12.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takeuchi M, Wakao N, Kamiya M, Hirasawa A, Osuka K, Joko M, et al. Lumbar extraforaminal entrapment:performance characteristics of detecting the foraminal spinal angle using oblique coronal MRI. A multicenter study. Spine J. 2015;15:895–900. doi: 10.1016/j.spinee.2015.02.011. https://doi.org/10.1016/J. SPINEE.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 7.Kitamura M, Eguchi Y, Inoue G, Orita S, Takaso M, Ochiai N, et al. A case of symptomatic extra-foraminal lumbosacral stenosis (“far-out syndrome”) diagnosed by diffusion tensor imaging. Spine (Phila Pa1976) 2012;3:7. doi: 10.1097/BRS.0b013e318249537f. https://doi.org/10.1097/BRS.0B013E318249537F. [DOI] [PubMed] [Google Scholar]
- 8.Wiltse LL, Spencer CW. New uses and refinements of the paraspinal approach to the lumbar spine. Spine (Phila Pa 1976) 1988;13:696–706. [PubMed] [Google Scholar]
- 9.Sakhrekar R, Ha JS, Han H-D, Kim D-H, Kim CW, Kulkarni S. The Past, Present, and Future of Unilateral Biportal Endoscopy with a Technical Note on Novel Endoscopic Visualization Pedicle Screw Insertion Technique and UBE-transforaminal Lumbar Interbody Fusion Technique with Literature Review. JOrthop Case Rep. 2023;13:165. doi: 10.13107/jocr.2023.v13.i12.4120. https://doi.org/10.13107/JOCR.2023.V13. I12.4120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sakhrekar R, Ha JS, Don H-, Kim D-H, Kim CW, Kulkarni S. Unilateral Biportal Endoscopic Approach for Symptomatic Adjacent Segment Disease:Case Report and Technical Note. JOrthop Case Rep. 2023;13:172–7. doi: 10.13107/jocr.2023.v13.i12.4122. https://doi.org/10.13107/JOCR.2023. V13. I12.4122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chu P, Wang T, Zheng J, Xu C, Yan Y, Ma Q, et al. Global and Current Research Trends of Unilateral Biportal Endoscopy/Biportal Endoscopic Spinal Surgery in the Treatment of Lumbar Degenerative Diseases:A Bibliometric and Visualization Study. Orthop Surg. 2022;14:635–43. doi: 10.1111/os.13216. https://doi.org/10.1111/os.13216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahn JS, Lee HJ, Choi DJ, Lee KY, Hwang SJ. Extraforaminal approach of biportal endoscopic spinal surgery:a new endoscopic technique for transforaminal decompression and d i s c e c to my. J Neuro surg Spine. 2018;28:492–8. doi: 10.3171/2017.8.SPINE17771. https://doi.org/10.3171/2017.8. SPINE17771. [DOI] [PubMed] [Google Scholar]
- 13.Heo DH, Sharma S, Park CK. Endoscopic Treatment of Extraforaminal Entrapment of L5 Nerve Root (Far Out Syndrome) by Unilateral Biportal Endoscopic Approach:Technical Report and Preliminary Clinical Results. Neurospine. 2019;16:130. doi: 10.14245/ns.1938026.013. https://doi.org/10.14245/NS.1938026.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kotil K, Akcetin M, Bilge T. A minimally invasive transmuscular approach to far-lateral L5-S1 level disc herniations:a prospective study. J Spinal Disord Tech. 2007;20:132–8. doi: 10.1097/01.bsd.0000211268.43744.2a. https://doi.org/10.1097/01. BSD.0000211268.43744.2A. [DOI] [PubMed] [Google Scholar]
- 15.O'Toole JE, Eichholz KM, Fessler RG. Minimally invasive far lateral microendoscopic discectomy for extraforaminal disc herniation at the lumbosacral junction:cadaveric dissection and technical case report. Spine J. 2007;7:414–21. doi: 10.1016/j.spinee.2006.07.008. https://doi.org/10.1016/J. SPINEE.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Tubbs RS, Iwanaga J, Aly I, Moisi MD, Hanscom DR, Chapman JR, et al. Extraforaminal compression of the L5 nerve:An anatomical study with application to failed posterior decompressive procedures. J Clin Neurosci. 2017;41:139–43. doi: 10.1016/j.jocn.2017.03.051. https://doi.org/1016/J. JOCN.2017.03.051. [DOI] [PubMed] [Google Scholar]
- 17.Heo DH, Sharma S, Park CK. Endoscopic Treatment of Extraforaminal Entrapment of L5 Nerve Root (Far Out Syndrome) by Unilateral Biportal Endoscopic Approach: Technical Report and Preliminary Clinical Results. Neurospine. 2019;16:130–7. doi: 10.14245/ns.1938026.013. https://doi.org/10.14245/NS.1938026.013. [DOI] [PMC free article] [PubMed] [Google Scholar]


