Abstract
Studies analyzing Ebola virus replication have been severely hampered by the extreme pathogenicity of this virus. To permit analysis of the host range and function of the Ebola virus glycoprotein (Ebo-GP), we have developed a system for pseudotyping these glycoproteins into murine leukemia virus (MLV). This pseudotyped virus, MLV(Ebola), can be readily concentrated to titers which exceed 5 × 106 infectious units/ml and is effectively neutralized by antibodies specific for Ebo-GP. Analysis of MLV(Ebola) infection revealed that the host range conferred by Ebo-GP is very broad, extending to cells of a variety of species. Notably, all lymphoid cell lines tested were completely resistant to infection; we speculate that this is due to the absence of a cellular receptor for Ebo-GP on B and T cells. The generation of high-titer MLV(Ebola) pseudotypes will be useful for the analysis of immune responses to Ebola virus infection, development of neutralizing antibodies, analysis of glycoprotein function, and isolation of the cellular receptor(s) for the Ebola virus.
Ebola viruses are the causative agent of a severe hemorrhagic fever disease associated with mortality rates of up to 88% in humans (1, 15); because of this, they have been classified as biosafety level 4 agents. The Ebola and closely related Marburg viruses are nonsegmented, negative-sense RNA viruses that constitute the filovirus family (16). They have a unique filamentous morphology with a uniform diameter of 80 nm and variable length of up to 14 μm. Filoviruses are enveloped and express a single membrane-anchored glycoprotein that has been shown to exist as a homotrimer for the Marburg virus (8). The Ebola virus envelope glycoprotein (Ebo-GP) has a molecular mass of approximately 140 kDa and, as the sole viral spike protein, is presumed to be responsible for mediating viral entry into target cells (7, 31).
By a process known as pseudotyping, enveloped viruses can incorporate heterologous viral glycoproteins into their lipid membranes during budding (6, 18, 27). These pseudotyped viruses acquire the host range of the virus from which the heterologous glycoprotein was derived (3, 28). The use of such pseudotyped viruses enables the rapid analysis of the function of a viral glycoprotein. For instance, we have previously shown that the effects of a variety of mutations within the subgroup A avian sarcoma and leukosis virus (ASLV-A) glycoprotein on viral entry can be evaluated through the production of murine leukemia virus (MLV) virions pseudotyped with these mutant glycoproteins (24).
Productive Ebola virus infections have been found to occur in a variety of animal systems, including human, simian, and bat (1, 2, 29). However, few reports describe the cell tropism of Ebola virus (22, 30), and restrictions to viral entry at the cellular level are unclear. To investigate the cellular tropism of Ebola virus, we examined the host range of MLV particles pseudotyped with the Zaire subtype of Ebo-GP [MLV(Ebola)]. Infectious MLV(Ebola) pseudotypes were efficiently produced and could be concentrated to high titers. MLV(Ebola) exhibited a very broad host range, infecting a variety of different cell lines from multiple species and tissue types. We found that MLV(Ebola) did not infect cells of the lymphoid system, while control vesicular stomatitis virus (VSV) G protein-pseudotyped MLV virions did. Therefore, our results suggest that one in vivo block to Ebola virus replication in lymphoid cells is the lack of a functional viral receptor on these cells.
The production of MLV(Ebola) pseudotypes allowed us to evaluate the ability of a polyclonal antiserum raised against Ebo-GP to inhibit MLV(Ebola) infection. Antibodies capable of abrogating Ebo-GP-mediated entry might have important utility as a therapeutic agent for Ebola virus infection. The results of our experiments indicate that neutralizing epitopes do exist within Ebo-GP and suggest that MLV(Ebola) pseudotypes will provide a rapid and efficient means to screen panels of antibodies for a neutralizing effect against Ebola virus.
In addition, these pseudotyped viruses provided us with a means to better characterize the Ebo-GP-mediated entry event. We examined the effects of weak bases, such as chloroquine and ammonium chloride, on MLV(Ebola) infection. Our results indicate that Ebo-GP-mediated entry is a pH-dependent process and thus show that these pseudotyped viruses are a useful reagent with which to examine the function of Ebo-GP.
MATERIALS AND METHODS
Cell lines and antibodies.
Human embryonic kidney 293T cells, baby hamster kidney (BHK) cells, and murine NIH 3T3 cells were maintained in Dulbecco’s modified Eagle medium supplemented with 10% bovine calf serum. Human cervical carcinoma (HeLa) cells, human microglial (U87) cells, African green monkey kidney cells (Vero, BSC-1, and Cos-7), Madin-Darby canine kidney (MDCK) cells, Madin-Darby bovine kidney (MDBK) cells, bovine aorta endothelial cells (BAEC), and porcine kidney (PK-15) cells were maintained in Dulbecco’s modified Eagle medium supplemented with 10% fetal calf serum. Chinese hamster ovary (CHO) cells were maintained in Ham’s F12 medium supplemented with 10% fetal calf serum. The Nalm-6 and Daudi human B-cell lines were maintained in RPMI 1640 medium supplemented with 20% fetal calf serum. The HUT-78 and CEM(E) human T-cell lines were maintained in RPMI 1640 supplemented with 10% fetal calf serum. IF-1 murine γδ T cells were maintained similarly to the HUT-78 cells with the addition of nonessential amino acids (0.1 mM), l-glutamine (2 mM), vitamins, β-mercaptoethanol (10−5 M), and sodium pyruvate (1 mM). WEHI murine B cells were maintained similarly to the Nalm-6 cells with the addition of nonessential amino acids (0.1 mM) and sodium pyruvate (1 mM). Tb 1 Lu bat lung cells were maintained in modified Eagle medium supplemented with 10% fetal calf serum. Pt K1 marsupial cells were maintained like the Tb 1 Lu cells with the addition of sodium pyruvate (1 mM). QT6 quail sarcoma cells, turkey embryonic fibroblasts (TEF), and chicken embryonic fibroblasts (CEF) were maintained in M199 medium supplemented with 5% fetal calf serum, 1% chicken serum, and 10% tryptose phosphate broth. All cell lines were in addition supplemented with penicillin (100 U/ml), and streptomycin (100 μg/ml).
Pt K1, Tb 1 Lu, PK-15, MDCK, and MDBK cell lines were generously provided by Richard Sutton (University of California, San Francisco). WEHI cells were kindly provided by Edward Scott (University of Pennsylvania). Nalm-6, Daudi, HUT-78, and CEM(E) cells were kindly provided by James Hoxie (University of Pennsylvania). IF-1 cells were kindly provided by Simon Carding (University of Pennsylvania). U87 and CHO cells were kindly provided by Robert Doms (University of Pennsylvania).
A rabbit polyclonal antibody recognizing the Zaire subtype of Ebo-GP was generously provided by Anthony Sanchez (Centers for Disease Control and Prevention). Goat anti-MLV AKR capsid p30 antibody was purchased from Quality Biotech Inc. (Camden, N.J.).
Plasmids and expression.
The cDNA encoding the Zaire subtype of Ebo-GP was kindly provided by Anthony Sanchez (Centers for Disease Control and Prevention) in the vector pGEM3Zf(−) as a BamHI-KpnI fragment. This gene was excised from pGEM3Zf(−), using the BamHI and EcoRI restriction enzymes, and cloned into the mammalian expression plasmid pCB6 to create the plasmid pCB6-Ebo-GP. Ebo-GP was transiently expressed in 293T cells by a standard CaPO4 transfection procedure. Briefly, 293T cells were seeded at between 50 and 70% confluence the day prior to transfection. The 293T cells were refed 1 h prior to transfection. Then, a DNA cocktail containing between 20 and 60 μg of the DNA to be transfected, 50 μl of 10 × NTE (8.77 g of NaCl, 10 ml of 1 M Tris [pH 7.4], and 4 ml of 0.25 M EDTA [pH 8.0] in a final volume of 100 ml in H2O), and 62.5 μl of 2 M CaCl2, brought to a final volume of 500 μl with H2O, was prepared. This DNA cocktail was added dropwise to 500 μl of 2× transfection buffer (1 ml of 0.5 M HEPES [pH 7.1], 8.1 ml of H2O, 0.9 ml of 2 M NaCl, and 20 μl of 1 M Na2HPO4) and left at room temperature for 30 min. This solution was then added dropwise to the 293T cells and left on overnight. The next day, the cells were refed with fresh medium. Forty-eight hours posttransfection, cell monolayers were lysed in Triton lysis buffer (50 mM Tris [pH 8], 5 mM EDTA, 150 mM NaCl, and 1% Triton X-100). The proteins of the cell lysates were resolved by sodium dodecyl sulfate-polyacrylamide electrophoresis (SDS-PAGE) and then transferred to nitrocellulose membranes. Ebo-GP expression was detected by Western blot analysis as previously described (23), using the anti-Ebo-GP antibody described above at a 1:1,000 dilution and a horseradish peroxidase-conjugated goat anti-rabbit secondary antibody (Pierce, Rockford, Ill.) at a 1:20,000 dilution. The pHIT/G plasmid (10) encoding the VSV G protein was kindly provided by M. Malim (University of Pennsylvania). The pCB6-EnvA plasmid encoding the ASLV-A envelope glycoprotein has been previously described (13). The pHIT60 and pHIT111 plasmids have been previously described (26).
Production of MLV pseudotypes.
A modification of a transient MLV packaging system (26) was used to assay the ability of Ebo-GP to mediate infection. pCB6-Ebo-GP, pHIT/G, or pCB6-EnvA plasmids were mixed with plasmids encoding MLV Gag-Pol (pHIT60) and a packageable genome encoding the β-galactosidase reporter gene (pHIT111). These DNA mixtures were transfected into 293T cells as described above to produce MLV(Ebola), MLV(VSV), and MLV(ASLV-A), respectively. Approximately 20 μg of plasmid was used in each experiment. Forty-eight hours posttransfection, medium containing virus was collected and clarified by both centrifugation for 10 min at 1,500 × g and filtration through a 0.45 μm-pore-size syringe filter. These supernatants were stored at either 4 or −80°C as viral stocks. Transfected-cell monolayers were lysed and analyzed for Ebo-GP expression as described above.
All experiments involving the production and functional analysis of replication-incompetent MLV(Ebola) pseudotypes were performed under biosafety level 2 containment as approved by the University of Pennsylvania Institutional Biosafety Committee.
To analyze the incorporation of Ebo-GP into MLV virions, 3.5 ml of clarified viral stock solution was layered onto 2 ml of 20% sucrose in phosphate-buffered saline (PBS) and centrifuged at 55,000 rpm in an SW55 rotor for 15 min. Pelleted virions were lysed in RIPA buffer (140 mM NaCl, 10 mM Tris [pH 8.0], 5 mM EDTA, 1% sodium deoxycholate, 1% Triton X-100, and 0.1% SDS) and resolved by SDS-PAGE. Western blot analysis was used to detect expression of Ebo-GP as described above, and MLV p30 capsid was detected with the goat anti-MLV AKR capsid p30 serum (described above) at a 1:2,500 dilution and a horseradish peroxidase-conjugated rabbit anti-goat secondary antibody at a 1:20,000 dilution.
Analysis of Ebo-GP-mediated host range.
The cell lines described above were seeded at 3 × 105 to 5 × 105 cells/well in a six-well dish the day prior to infection. Various dilutions of viral stocks were made in 1 ml (final volume) of maintenance medium. These solutions were then used to challenge target cells. Twelve hours postchallenge, 1 ml of fresh medium was added to the cells. Thirty-six hours later, the cells were washed with PBS and then fixed in 2% paraformaldehyde. The cells were washed in PBS two additional times and then stained for β-galactosidase activity with X-Gal solution (3.5 × 10−2 M potassium ferricyanide [K3Fe(CN)6], 3.5 × 10−2 M potassium ferrocyanide [K4Fe(CN)6 · 3H2O], 10−4 M magnesium chloride (MgCl), and 0.1% 5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside [X-Gal] in PBS) (26). Viral titers were determined by microscopic examination of stained cells and enumeration of β-galactosidase-positive cells. These titers were expressed as the number of β-galactosidase-positive cells per milliliter of viral stock used in the infection (infectious units [IU] per milliliter).
Concentration of virus was performed as described elsewhere (3). Briefly, clarified viral stocks were centrifuged at 25,000 rpm in an SW28 rotor for 90 min. The supernatant was decanted, and various volumes of TNE buffer (50 mM Tris [pH 8], 130 mM NaCl, 1 mM EDTA) were used to resuspend the pelleted virions overnight at 4°C. These suspensions were then used to infect cells as described above.
Neutralization.
MLV(Ebola) viral stocks were incubated with various dilutions of either the polyclonal anti-Ebo-GP antibody described above or a control rabbit nonimmune serum for 30 min at room temperature. The antibody-treated virions were then used to infect 293T cells in the presence of the same concentrations of antibody. Forty-eight hours postinfection, viral titers were enumerated as described above.
pH dependence of MLV(Ebola) infection.
QT6 cells were incubated with various concentrations of either chloroquine or ammonium chloride (Sigma, St. Louis, Mo.) for 1 h at 37°C. These cells were then infected with either MLV(ASLV-A), MLV(VSV), or MLV(Ebola) as described above, in the continued presence of drug. Sixteen hours postinfection, the cells were fed with fresh medium. Enumeration of infected cells was performed 48 h postinfection as described above.
RESULTS
Expression of Ebo-GP.
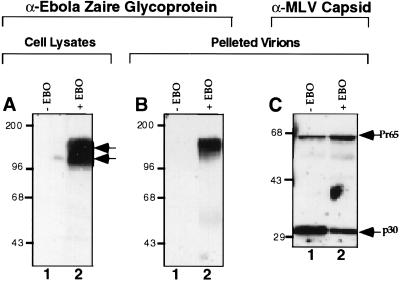
The cDNA encoding the Zaire subtype of Ebo-GP was engineered into the mammalian expression plasmid pCB6 under the control of the cytomegalovirus immediate-early promoter. Ebo-GP expression mediated by this construct was examined by transient transfection of 293T cells. Forty-eight hours posttransfection, cellular lysates were prepared and then analyzed by SDS-PAGE and Western blotting with a polyclonal antiserum raised against Ebo-GP. Analysis of lysates from cells transfected with the pCB6-Ebo-GP construct demonstrated two bands that reacted specifically with the Ebo-GP-specific antiserum (Fig. 1A, lane 2) and whose apparent molecular masses of approximately 110 to 140 kDa corresponded to the previously described sizes for Ebo-GP (7, 31).
FIG. 1.
Protein expression in virion and cell lysates. 293T cells were transiently transfected with MLV Gag-Pol and genome constructs with (+ EBO) or without (− EBO) pCB6-Ebo-GP, a Zaire subtype Ebo-GP expression construct. Viral supernatants were harvested from transfected cells and partially purified by pelleting through 20% sucrose. Cell lysates and lysed pellets were analyzed by Western blotting with anti-Ebo-GP serum and anti-MLV capsid serum. (A) Expression of Ebo-GP in cell lysates. Arrows indicate the two forms of Ebo-GP. (B) Incorporation of Ebo-GP into MLV particles. (C) Analysis of MLV capsid in viral pellets. Arrows indicate MLV Gag precursor (Pr65) and capsid (p30) proteins. The positions of molecular mass markers (in kilodaltons) are shown on the left of each gel.
Production of MLV(Ebola) pseudotypes.
To determine the function of Ebo-GP, we attempted to incorporate this glycoprotein into MLVs as the sole viral spike protein (26). These pseudotyped particles are denoted MLV(Ebola). To determine if Ebo-GP was incorporated into MLV, 293T cells were transiently transfected with plasmids encoding MLV Gag-Pol (pHIT60) and an MLV genome containing a β-galactosidase reporter gene (pHIT111) with or without pCB6-Ebo-GP. Forty-eight hours posttransfection, cellular supernatants were harvested and clarified by centrifugation and filtration. Virions were partially purified by ultracentrifugation through 20% sucrose, and the resulting viral pellets were lysed. Viral particle composition was examined by Western blot analysis of the lysates, using anti-Ebo-GP and anti-MLV capsid sera. Similar amounts of MLV Gag protein (Pr65 and p30) were detected in both viral pellets with an anti-MLV capsid serum (Fig. 1C), indicating that MLV particle production was roughly equivalent in both transfections. In viral pellets from cells cotransfected with Ebo-GP, a 140-kDa band was detected after blotting with an anti-Ebo-GP antiserum (Fig. 1B, lane 2). This suggests that of the two proteins detected in cellular lysates with anti-Ebo-GP antiserum (Fig. 1A, lane 2), only the 140-kDa protein was efficiently incorporated into the MLV virions. The 140-kDa protein appears to correspond to the previously described mature, endo-β-N-acetylglucosaminidase H-resistant form of Ebo-GP presumably found on virions (31), suggesting that MLV(Ebola) pseudotypes are a relevant model for studying Ebo-GP function.
Analysis of Ebo-GP-mediated host range.
The ability of Ebo-GP to mediate infection was initially investigated using human 293T cells as targets for infection. Forty-eight hours after infection with MLV(Ebola), the cells were stained for the β-galactosidase activity encoded by the MLV genome. The titer of MLV(Ebola) on 293T cells was found to range from 104 to 105 IU/ml (see Table 1). Parallel infections were carried out with MLV particles produced in the absence of a viral envelope protein; these virions were unable to mediate detectable levels of infection. We also incorporated the VSV G protein into MLV particles as a control to distinguish a block in entry from postentry effects on the MLV core, since the VSV G protein has been shown to confer a wide host range to MLV (3). The titers of these MLV(VSV) pseudotypes were consistently higher than that of the MLV(Ebola) and ranged between 5 × 105 and 2 × 106 IU/ml on 293T cells (see Table 1).
TABLE 1.
Infection of various cell lines with MLV(Ebola)
| Cell line | Species of origin | Titer (IU/ml) fora:
|
|
|---|---|---|---|
| MLV(Ebola) | MLV(VSV) | ||
| 293T | Human | 4.7 × 104 | 1.5 × 106 |
| HeLa | Human | 7.5 × 102 | 1.4 × 105 |
| Vero | Simian | 2.6 × 102 | 5.3 × 103 |
| BSC-1 | Simian | 1.2 × 103 | 7.9 × 103 |
| Cos-7 | Simian | 5.6 × 103 | 1.6 × 105 |
| NIH 3T3 | Murine | 5.2 × 103 | 4.3 × 105 |
| MDBK | Bovine | 1.2 × 102 | 1.6 × 105 |
| BAEC | Bovine | 9.2 × 102 | 7.9 × 104 |
| PK-15 | Porcine | 6.0 × 101 | 5.5 × 103 |
| BHK | Hamster | 1.9 × 102 | 1.2 × 105 |
| CHO | Hamster | 1.0 × 103 | 1.5 × 105 |
| QT6 | Quail | 2.0 × 103 | 1.3 × 105 |
| CEF | Chicken | 1.6 × 102 | 1.4 × 104 |
| TEF | Turkey | 3.2 × 102 | 9.3 × 104 |
| 293Tb | Human | 2.9 × 106 | 7.8 × 105 |
| U87b | Human | 5.2 × 105 | 2.3 × 105 |
| MDCKb | Canine | 6.0 × 103 | 1.4 × 103 |
| Tb 1 Lub | Bat | 2.3 × 103 | 8.3 × 103 |
| Pt K1b | Marsupial | 1.6 × 102 | 2.4 × 102 |
Data from representative experiments are shown. Similar results have been obtained in replicate experiments.
Concentrated MLV(Ebola) stocks were used for infection of this cell line.
The production of MLV(Ebola) pseudotypes enabled us to examine the potential cellular tropism conveyed by Ebo-GP by assaying infection of a variety of cell lines derived from different species and tissues. All cell lines listed in Table 1 were permissive for both MLV(Ebola) and MLV(VSV), demonstrating the wide cellular tropism conferred by Ebo-GP. The viral titers obtained on the individual cell lines varied quite dramatically, but in general this variation was consistent between MLV(Ebola) and MLV(VSV). For example, compare the titers obtained on 293T, QT6, and BAEC, which all displayed titers for MLV(Ebola) that were generally 100-fold lower than those of MLV(VSV). Thus, this variation might reflect a general defect in viral entry in these cells or, more likely, a problem in integration or expression of the MLV genome. Certain cells, such as the marsupial Pt K1 and bat lung Tb 1 Lu lines, yielded extremely low titers in MLV(Ebola) infection (data not shown). This was not unexpected, since these cells were relatively nonpermissive for MLV(VSV) infection (Table 1). Given that the MLV(Ebola) titers were so low, we attempted to concentrate MLV(Ebola) by centrifugation to facilitate the analysis of MLV(Ebola) infection in these cell lines (3). MLV(Ebola) was produced as described above, and the virion-containing supernatants were gently centrifuged. The resulting viral pellet was resuspended and used to infect target cells. We achieved over 80% virion recovery and increased titers of MLV(Ebola) to 6 × 106 IU/ml as measured on 293T cells (Table 2). Concentrated MLV(Ebola) was used to infect those cell lines for which the MLV(VSV) titer was low (Table 1), clearly demonstrating the ability of MLV(Ebola) to infect them.
TABLE 2.
Concentration of MLV(Ebola) by centrifugation
| Expt | Virus titer (IU/ml)a
|
Fold concn | Total virus (IU)
|
% Recovery | ||
|---|---|---|---|---|---|---|
| Preconcn | Postconcn | Preconcn | Postconcn | |||
| 1 | 5.9 × 104 | 5.4 × 106 | 78 | 4.6 × 106 | 3.8 × 106 | 82.6 |
| 2 | 1.1 × 105 | 6.2 × 106 | 70 | 7.7 × 106 | 6.2 × 106 | 80.5 |
Titers of the concentrated MLV(Ebola) were determined on 293T cells. Preconcentration titer refers to viral supernatant left overnight at 4°C before being used for infection. Postconcentration titer refers to viral supernatant centrifuged at 25,000 rpm in an SW28 rotor for 90 min and resuspended in TNE overnight at 4°C before being used for infection.
In the course of our survey of the cellular tropism of MLV(Ebola), we noted that cells of the lymphoid lineage appeared to be resistant to infection by this virus. Human and murine lymphoid cell lines (Nalm-6 and Daudi [human B cells], HUT-78 and CEM(E) [human T cells], WEHI [murine B cell], and IF-1 [murine γδ T cell]) were challenged with up to 105 IU of MLV(Ebola) or 106 IU of MLV(VSV) as measured on 293T cells (Table 3). MLV(VSV) infected these cell lines efficiently, with titers ranging from 104 IU/ml on HUT-78 human T cells to 106 IU/ml on the Nalm-6 B-cell line. MLV(Ebola), however, was unable to infect any of these six murine or human lymphoid cells.
TABLE 3.
Human and murine lymphoid cell lines are resistant to MLV(Ebola)
| Cell line | Species of origin | Cell type | Titer (IU/ml) for:
|
|
|---|---|---|---|---|
| MLV(Ebola)a | MLV(VSV) | |||
| Nalm-6 | Human | B | 0 | 1.2 × 106 |
| Daudi | Human | B | 0 | 1.0 × 104 |
| HUT-78 | Human | T | 0 | 3.3 × 104 |
| CEM(E) | Human | T | 0 | 3.0 × 104 |
| WEHI | Murine | B | 0 | 5.2 × 105 |
| IF-1 | Murine | T | 0 | 6.0 × 104 |
Concentrated MLV(Ebola) was used for these infections. In the experiments shown, all lymphoid cells were infected with 5 × 105 IU of MLV(Ebola) as measured on 293T cells. A titer of 0 in this column indicates that no cells stained for β-galactosidase activity after 2 days of incubation with that amount of MLV(Ebola).
The fact that the lymphoid cells were permissive for MLV(VSV) infection but refractory to MLV(Ebola) suggested that the receptor for Ebo-GP might not be present on these lymphoid cells. Alternatively, lymphoid cells might secrete a factor that interferes with the interaction between Ebo-GP and the cellular receptor, in a manner similar to that by which chemokines secreted by CD8+ T cells block infection by human immunodeficiency virus type 1 (5). To address whether this was the case, we cocultivated 293T cells with the human Nalm-6 B-cell line for 12 h and then challenged the cocultivated cells with MLV(Ebola). The MLV(Ebola) titer on these 293T cells cocultivated with Nalm-6 cells was evaluated 36 h postinfection and was equivalent to that on 293T cells that had not been cocultivated (data not shown). Similar cocultivation studies with the CEM(E) and Daudi lymphoid cell lines also showed no effect on 293T infection (data not shown). These data suggest that a soluble factor is unlikely to be responsible for the blockade of Ebo-GP-mediated entry into lymphoid cells.
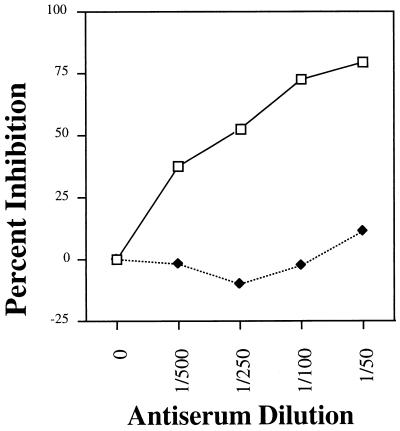
Neutralization of MLV(Ebola).
One potential use of MLV(Ebola) pseudotypes is in the evaluation of antibodies for their ability to neutralize Ebola virus. To address this question, we investigated the ability of an anti-Ebo-GP polyclonal serum to neutralize MLV(Ebola). MLV(Ebola) was incubated with either anti-Ebo-GP or a control serum at various dilutions for 30 min at room temperature and then used to infect 293T cells in the presence of these same concentrations of antiserum (Fig. 2). The anti-Ebo-GP polyclonal serum was able to block MLV(Ebola) infection of 293T cells in a dose-dependent manner, displaying a maximum inhibition of approximately 80% at a dilution of 1:50, whereas a control serum had little effect even at the lowest dilution tested. In experiments with wild-type Ebola virus, similar neutralization results have been observed with this anti-Ebo-GP serum (24a), suggesting the relevance and utility of MLV(Ebola)-pseudotyped viruses as a safe alternative for analyzing host immune responses to Ebola virus and for evaluating potential therapeutic neutralizing antibodies.
FIG. 2.
MLV(Ebola) neutralization by incubation with a polyclonal anti-Ebo-GP serum. Prior to infection of cells, MLV(Ebola) was incubated with either a control serum (⧫) or anti-Ebo-GP serum (□) for 30 min at room temperature.
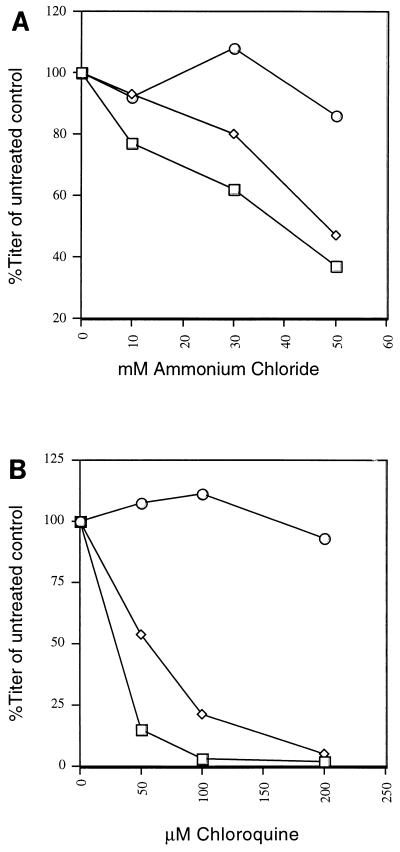
Inhibition of MLV(Ebola) infection by lysosomotropic agents.
To analyze further the Ebo-GP-mediated entry event, we investigated whether MLV(Ebola) infection could be modulated by pretreatment of target cells with lysosomotropic agents. These agents raise the pH of the endosomal compartment and efficiently block viruses that require a low-pH step for entry (19–21). QT6 cells were chosen as targets for infection because they are susceptible to infection by MLV(ASLV-A), which exhibits pH-independent entry (14), and MLV(VSV), whose entry is pH dependent (20, 32). QT6 cells were incubated with various concentrations of chloroquine or ammonium chloride for 1 h and then infected with MLV(Ebola), MLV(VSV), or MLV(ASLV-A). Incubation of target cells with either of these weak bases clearly inhibited MLV(Ebola) infection (Fig. 3). Chloroquine at a concentration of 200 μM had little effect on the MLV(ASLV-A) titer but reduced that of MLV(Ebola) to 0.01% of the untreated control. Similarly, ammonium chloride treatment of target cells did not adversely affect the titer of MLV(ASLV-A) but reduced the MLV(Ebola) titer by 63% at a concentration of 50 mM. Pretreatment of QT6 cells with these agents inhibited infection by the pH-dependent MLV(VSV) with a dose response similar to that seen with MLV(Ebola) (Fig. 3). Together, these data strongly suggest that Ebo-GP-mediated entry is pH dependent.
FIG. 3.
Inhibition of MLV(Ebola) infection by lysosomotropic agents. QT6 cells were treated with the indicated concentrations of either ammonium chloride (A) or chloroquine (B) for 1 h prior to infection with either MLV(Ebola) or MLV(ASLV-A). Cells were fed with fresh medium 16 h postinfection and stained 32 h later. ○, MLV(ASLV-A); □, MLV(Ebola); ◊, MLV(VSV).
DISCUSSION
The high mortality rate associated with filovirus infection and the lack of any effective therapeutic strategy have led to their classification as biosafety level 4 pathogens. This extreme pathogenesis has greatly hindered the study of their replication, and thus they remain a very poorly characterized group of viruses. To study the process of Ebola virus entry, we produced retroviral particles pseudotyped with Ebo-GP. Production of high-titer MLV(Ebola) pseudotypes (up to 6 × 106 IU/ml) allowed analysis of the host range conferred by Ebo-GP. The host range conferred by Ebo-GP is very broad, enabling the infection by MLV(Ebola) of a variety of cell lines from diverse species and tissues. The infection of many of the cell lines described in Table 1 is not unexpected, since humans, monkeys, and bats have all been reported to be infectible by the Ebola virus in vivo (1, 2, 29). A recent report suggests that pigeons and mice may be refractory to Ebola virus infection (29). However, our results suggest that the described block to infection of these animals is not due to an inability of Ebo-GP to mediate viral entry into cells from these species, since NIH 3T3 murine fibroblasts, primary CEF and TEF, and quail muscle sarcoma cells (QT6) were effectively infected by MLV(Ebola).
Interestingly, we found that both human and murine cells of the lymphoid lineage were completely resistant to infection by MLV(Ebola). This block to infection mediated by Ebo-GP correlates with observations made during the course of infections with the Ebola virus in laboratory animals, in which lymphoid cells are generally uninfected by the virus (24a). In addition, both the HUT-78 and CEM(E) human T-cell lines have been shown to be resistant to infection by all subtypes of Ebola virus analyzed, as well as Marburg virus (22). Together, these data suggest that cells of the lymphoid lineage either lack a functional Ebola virus receptor or somehow inhibit the Ebo-GP-mediated entry event. Cocultivation of 293T cells with a number of lymphoid cell lines did not reduce the susceptibility of these cells to infection by MLV(Ebola), indicating that a soluble inhibitory factor was not likely to be the cause of the block to Ebola virus infection of B and T cells. The demonstration that B and T lymphocytes are unable to support Ebola virus entry should enable the cloning of the cellular receptor for Ebola viruses through complementation with genomic DNA or a cDNA library from a cell line susceptible to MLV(Ebola) infection.
The production of high-titer MLV(Ebola) pseudotypes will also allow studies of the function of Ebo-GP to be done. It has been noted that the carboxyl-terminal regions of Ebo-GP and the ASLV envelope glycoprotein are very similar, containing a conserved CX6CC motif, a potential internal fusion peptide domain, and a coiled-coil region (12). These similarities between Ebo-GP and the well-characterized ASLV envelope provide a framework within which to analyze the function of specific regions of Ebo-GP through a targeted mutation strategy. The production of high-titer MLV(Ebola) pseudotypes will also allow studies of the overall function of the glycoprotein to be performed. Since Ebola virus must be handled as a biosafety level 4 pathogen, even relatively simple functional analyses, such as determining the pH dependence of entry, are laborious and expensive. In contrast, using MLV(Ebola) pseudotypes to address such questions is simple and straightforward.
The administration of neutralizing antibodies has been highly successful in mediating clearance of both rabies virus and hepatitis B virus from infected individuals (11, 17), and it has been suggested that the administration of neutralizing antibodies early in the course of an Ebola virus infection might increase survival rates (25). Moreover, in animals recovering from filovirus infection, the development of high-titer antibodies specific for Ebola antigens coincides with viral clearance (9), suggesting that neutralizing antibodies may play a role in the clearance of Ebola virus from infected individuals. Our preliminary results from an analysis of an antiserum made against the viral glycoprotein indicate that neutralizing epitopes may exist within Ebo-GP. Experiments performed with this antiserum and wild-type Ebola virus have yielded very similar neutralization activity (24a). Therefore, MLV(Ebola) should be useful for rapid and effective screening of panels of antibodies for Ebola virus neutralization ability and for characterization of the humoral response to Ebo-GP in infected animals and individuals.
The results of experiments utilizing ammonium chloride and chloroquine show that MLV(Ebola) is very sensitive to pretreatment of target cells with weak bases, as are MLV(VSV) pseudotypes, while infection by MLV(ASLV-A), a pH-independent virus, is unaffected. These data suggest that entry of Ebola virus is pH dependent. The Ebola virus and ASLV glycoproteins exhibit extensive homology in a region postulated to be intimately involved with the fusion process (4, 12). However, despite these similarities, the mechanisms of activation of the fusogenic machinery of Ebola virus and ASLV appear to differ. Further studies to confirm the pH dependence of Ebola virus entry, such as determination of whether cells expressing Ebo-GP can be induced to form syncytia upon treatment with an acidic medium or whether MLV(Ebola) virions can be inactivated by treatment with acid prior to infection of target cells, are currently under way.
We have described a system in which Ebo-GP can be efficiently pseudotyped into murine leukemia virus particles to produce high-titer, infectious MLV(Ebola) pseudotypes. Our results suggest that MLV(Ebola) virions accurately mimic the entry process of the Ebola virus, both in cellular host range and ability to be neutralized by treatment with a polyclonal antiserum raised against Ebo-GP, and indicate that Ebola may be a pH-dependent virus. These pseudotypes thus provide an ideal system in which to analyze immune responses to Ebola virus infection as well as to examine the function of Ebo-GP, and they will be useful in the identification of the cellular receptor for this deadly virus.
ACKNOWLEDGMENTS
We thank Anthony Sanchez for communication of unpublished results, the pGEM3Zf(−)-Ebo-GP clone, and the polyclonal anti-Ebo-GP serum. We acknowledge the generosity of Richard Sutton, Simon Carding, Robert Doms, Edward Scott, and James Hoxie for supplying cell lines and Michael Malim for providing the pHIT/G expression plasmid. We also thank Michael Malim and James Simon for critical readings of the manuscript, Kristen Wool-Lewis for support and encouragement, and the members of the Bates laboratory for useful discussions.
This work was supported by a grant to P.B. from the National Institutes of Health (CA63531).
REFERENCES
- 1.Anonymous. Ebola haemorrhagic fever in Zaire, 1976. Bull W H O. 1978;56:271–293. [PMC free article] [PubMed] [Google Scholar]
- 2.Bowen E T, Platt G S, Simpson D I, McArdell L B, Raymond R T. Ebola haemorrhagic fever: experimental infection of monkeys. Trans R Soc Trop Med Hyg. 1978;72:188–191. doi: 10.1016/0035-9203(78)90058-5. [DOI] [PubMed] [Google Scholar]
- 3.Burns J C, Friedmann T, Driever W, Burrascano M, Yee J K. Vesicular stomatitis virus G glycoprotein pseudotyped retroviral vectors: concentration to very high titer and efficient gene transfer into mammalian and nonmammalian cells. Proc Natl Acad Sci USA. 1993;90:8033–8037. doi: 10.1073/pnas.90.17.8033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carr C M, Kim P S. A spring-loaded mechanism for the conformational change of influenza hemagglutinin. Cell. 1993;73:823–832. doi: 10.1016/0092-8674(93)90260-w. [DOI] [PubMed] [Google Scholar]
- 5.Cocchi F, DeVico A L, Garzino-Demo A, Arya S K, Gallo R C, Lusso P. Identification of RANTES, MIP-1 alpha, and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cells. Science. 1995;270:1811–1815. doi: 10.1126/science.270.5243.1811. [DOI] [PubMed] [Google Scholar]
- 6.Dong J, Roth M G, Hunter E. A chimeric avian retrovirus containing the influenza virus hemagglutinin gene has an expanded host range. J Virol. 1992;66:7374–7382. doi: 10.1128/jvi.66.12.7374-7382.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elliott L H, Kiley M P, McCormick J B. Descriptive analysis of Ebola virus proteins. Virology. 1985;147:169–176. doi: 10.1016/0042-6822(85)90236-3. [DOI] [PubMed] [Google Scholar]
- 8.Feldmann H, Will C, Schikore M, Slenczka W, Klenk H D. Glycosylation and oligomerization of the spike protein of Marburg virus. Virology. 1991;182:353–356. doi: 10.1016/0042-6822(91)90680-A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher-Hoch S P, Perez-Oronoz G I, Jackson E L, Hermann L M, Brown B G. Filovirus clearance in non-human primates. Lancet. 1992;340:451–453. doi: 10.1016/0140-6736(92)91770-9. [DOI] [PubMed] [Google Scholar]
- 10.Fouchier R A M, Meyer B E, Simon J H M, Fischer U, Malim M H. HIV-1 infection of non-dividing cells: evidence that the amino-terminal basic region of the viral matrix protein is important for Gag processing but not for post-entry nuclear import. EMBO J. 1997;16:4531–4539. doi: 10.1093/emboj/16.15.4531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frenia M L, Lafin S M, Barone J A. Features and treatment of rabies. Clin Pharm. 1992;11:37–47. [PubMed] [Google Scholar]
- 12.Gallaher W R. Similar structural models of the transmembrane proteins of Ebola and avian sarcoma viruses. Cell. 1996;85:477–478. doi: 10.1016/s0092-8674(00)81248-9. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert J M, Bates P, Varmus H E, White J M. The receptor for the subgroup A avian leukosis-sarcoma viruses binds to subgroup A but not to subgroup C envelope glycoprotein. J Virol. 1994;68:5623–5628. doi: 10.1128/jvi.68.9.5623-5628.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilbert J M, Mason D, White J M. Fusion of Rous sarcoma virus with host cells does not require exposure to low pH. J Virol. 1990;64:5106–5113. doi: 10.1128/jvi.64.10.5106-5113.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson K M, Lange J V, Webb P A, Murphy F A. Isolation and partial characterisation of a new virus causing acute haemorrhagic fever in Zaire. Lancet. 1977;i:569–571. doi: 10.1016/s0140-6736(77)92000-1. [DOI] [PubMed] [Google Scholar]
- 16.Kiley M P, Bowen E T, Eddy G A, Isaacson M, Johnson K M, McCormick J B, Murphy F A, Pattyn S R, Peters D, Prozesky O W, Regnery R L, Simpson D I, Slenczka W, Sureau P, van der Groen G, Webb P A, Wulff H. Filoviridae: a taxonomic home for Marburg and Ebola viruses? Intervirology. 1982;18:24–32. doi: 10.1159/000149300. [DOI] [PubMed] [Google Scholar]
- 17.Krugman S, Giles J P, Hammond J. Viral hepatitis, type B (MS-2 strain) prevention with specific hepatitis B immune serum globulin. JAMA. 1971;218:1665–1670. [PubMed] [Google Scholar]
- 18.Landau N R, Page K A, Littman D R. Pseudotyping with human T-cell leukemia virus type I broadens the human immunodeficiency virus host range. J Virol. 1991;65:162–169. doi: 10.1128/jvi.65.1.162-169.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marsh M, Helenius A. Virus entry into animal cells. Adv Virus Res. 1989;36:107–151. doi: 10.1016/S0065-3527(08)60583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller D K, Lenard J. Inhibition of vesicular stomatitis virus infection by spike glycoprotein. Evidence for an intracellular, G protein-requiring step. J Cell Biol. 1980;84:430–437. doi: 10.1083/jcb.84.2.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ohkuma S, Poole B. Fluorescence probe measurement of the intralysosomal pH in living cells and the perturbation of pH by various agents. Proc Natl Acad Sci USA. 1978;75:3327–3331. doi: 10.1073/pnas.75.7.3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peters C J, Jahrling P B, Ksiazek T G, Johnson E D, Lupton H W. Filovirus contamination of cell cultures. Dev Biol Stand. 1992;76:267–274. [PubMed] [Google Scholar]
- 23.Rong L, Bates P. Analysis of the subgroup A avian sarcoma and leukosis virus receptor: the 40-residue, cysteine-rich, low-density lipoprotein receptor repeat motif of Tva is sufficient to mediate viral entry. J Virol. 1995;69:4847–4853. doi: 10.1128/jvi.69.8.4847-4853.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rong L, Edinger A, Bates P. Role of basic residues in the subgroup-determining region of the subgroup A avian sarcoma and leukosis virus envelope in receptor binding and infection. J Virol. 1997;71:3458–3465. doi: 10.1128/jvi.71.5.3458-3465.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24a.Sanchez, A. Personal communication.
- 25.Sanchez A, Trappier S G, Mahy B W, Peters C J, Nichol S T. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc Natl Acad Sci USA. 1996;93:3602–3607. doi: 10.1073/pnas.93.8.3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soneoka Y, Cannon P M, Ramsdale E E, Griffiths J C, Romano G, Kingsman S M, Kingsman A J. A transient three-plasmid expression system for the production of high titer retroviral vectors. Nucleic Acids Res. 1995;23:628–633. doi: 10.1093/nar/23.4.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suomalainen M, Garoff H. Incorporation of homologous and heterologous proteins into the envelope of Moloney murine leukemia virus. J Virol. 1994;68:4879–4889. doi: 10.1128/jvi.68.8.4879-4889.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sutton R E, Littman D R. Broad host range of human T-cell leukemia virus type 1 demonstrated with an improved pseudotyping system. J Virol. 1996;70:7322–7326. doi: 10.1128/jvi.70.10.7322-7326.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Swanepoel R, Leman P A, Burt F J, Zachariades N A, Braack L E, Ksiazek T G, Rollin P E, Zaki S R, Peters C J. Experimental inoculation of plants and animals with Ebola virus. Emerg Infect Dis. 1996;2:321–325. doi: 10.3201/eid0204.960407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van der Groen G, Webb P, Johnson K, Lange J, Linsday L, Elliott L. Growth of Lassa and Ebola viruses in different cell lines. In: Pattyn S R, editor. Ebola virus haemorrhagic fever. Amsterdam, The Netherlands: Elsevier/North-Holland Biomedical Press; 1978. pp. 255–260. [Google Scholar]
- 31.Volchkov V E, Becker S, Volchkova V A, Ternovoj V A, Kotov A N, Netesov S V, Klenk H D. GP mRNA of Ebola virus is edited by the Ebola virus polymerase and by T7 and vaccinia virus polymerases. Virology. 1995;214:421–430. doi: 10.1006/viro.1995.0052. [DOI] [PubMed] [Google Scholar]
- 32.White J, Matlin K, Helenius A. Cell fusion by Semliki Forest, influenza, and vesicular stomatitis viruses. J Cell Biol. 1981;89:674–679. doi: 10.1083/jcb.89.3.674. [DOI] [PMC free article] [PubMed] [Google Scholar]