Abstract
Background:
Exercise is an important factor for the treatment and rehabilitation of depression. Traditional Chinese exercise is considered as an effective treatment for depression. In recent years, many studies have shown that Chinese exercise therapy may be safe in the treatment of depression. To evaluate the therapeutic effect of traditional Chinese exercise on depression using network meta-analysis.
Methods:
PubMed, Cochrane Library, Web of Science, China National Knowledge Infrastructure, VIP shop Database, China Biomedical Literature Database, and Wan Fang Data Knowledge Service Platform were included in randomized controlled studies on traditional Chinese exercises for the treatment of depression from the establishment of the library to July 2023. The literature was extracted and assessed for risk of bias using the Cochrane Risk of Bias Assessment and statistically analyzed using Review Manager 5.4 and Stata 14.2.
Results:
A total of 25 studies involving 3 exercises with a total of 1605 cases were included. The results of the network meta-analysis showed that each exercise significantly reduced the 24-item Hamilton Depression Scale (HAMD-24), Hamilton Anxiety Scale, Beck Depression Inventory, and Self-rating Depression Scale scores. However, conventional treatments have the advantage of improving the sleep quality of patients with depression.
Conclusions:
The 3 exercises included in this study were effective for depression. Baduanjin and Tai Chi were better at improving the outcomes related to depression and anxiety. The effect of sleep quality intervention was slightly worse. Larger, high-quality randomized controlled trials are needed to compare interventions across exercises in a more granular manner.
Keywords: Baduanjin, depression, network meta-analysis, Tai Chi, traditional Chinese exercises, Wuqinxi
1. Introduction
Depression is a psychosomatic disease characterized by a low mood, depression, and decreased interest. According to statistics from the World Health Organization, the global incidence rate of depression is approximately 11%, and the lifetime prevalence of depression in China is approximately 6.8%.[1] It is estimated that by 2030,[2]depression will become the world’s largest disease burden. Depression can significantly reduce the quality of life and social functioning of patients,[3] while the disease itself increases the burden on society and families.[4]
Exercise can help people relax and strengthen their bodies; Traditional Chinese medicine (TCM) exercise therapy is a disease prevention and treatment method that has evolved based on traditional Chinese sports, including Tai Chi, Baduanjin, Wuqinxi, and Yijinjing. Research has shown that traditional exercise therapy has a very positive effect on the entire cycle and health status of various diseases.[5,6] At present, relevant studies have shown that the above 4 traditional sports have significant recovery effects on patients with depression,[7–9] but there is still a lack of comprehensive and direct comparison of each project for primary depression. A mesh meta-analysis can represent the direct and indirect connections between multiple intervention methods under the same conditions. Therefore, this study conducted a network meta-analysis of a randomized controlled trial of TCM exercise therapy intervention in the treatment of depression, providing a certain data basis for the evaluation of the efficacy of TCM exercise therapy intervention in depression.
2. Methods
2.1. Protocol and registration
This systematic review followed the Preferred Reporting Item statement for systematic review and meta-analysis.[10] This study was registered with PROSPERO in July 2023 (CRD42023446637).
2.2. Ethic approval
Ethical approval is not necessary because this network meta-analysis only uses published papers that do not reveal personal privacy or violate human rights.
2.3. Inclusion criteria for study selection
2.3.1. Type of studies.
Only randomized controlled trials were included in our study, and case reports, animal experiments, and reviews were excluded. The language was restricted to both Chinese and English.
2.3.2. Types of patients.
The patients were aged 18 years or older and had no other psychological or physical disease. Regardless of nationality, sex, and race, patients who met the diagnostic criteria for depression were included as participants.
2.3.3. Types of interventions.
The treatment methods of the experimental group will be Baduanjin, Tai Chi, Wuqinxi, and Yijinjing training, or combined with medication treatment. The control group will be treated with medication or blank, and trials involving other exercise therapies will be excluded.
2.3.4. Types of outcome measures.
The subjects included in the literature all met the diagnostic criteria for depression in the International Classification of Diseases (11th edition; ICD-11) published by World Health Organization.[11] The primary efficacy measure was the 24-item Hamilton Depression Scale (HAMD-24). The second measures were the Beck Depression Inventory (BDI), Self-rating Depression Scale (SDS), Pittsburgh Sleep Quality Index (PSQI), and Hamilton Anxiety Scale (HAMA). HAMD-24 is the most widely used scale for diagnosis and assessment of depression and it comprises 24 items of depressive symptoms, which are scored in 5 grades.[12] The BDI consists of 21 questions designed for patients aged ≥13 years to score the severity of physical and cognitive symptoms related to depression.[13] The SDS is a 20-item scale designed to measure depression with scores ranging from 20 to 80. Higher scores indicate a higher level of depression.[14] Seven tests were used to assess subjective sleep quality, sleeping time, subjective sleep duration, sleep efficiency, sleep disorders, hypnotic drugs, and daytime dysfunction.[15] The HAMA is a clinician-report tool originally composed of 14 items, each of which represents a cluster in which different symptoms are grouped. It generally represents 2 aspects of somatic anxiety and psychic anxiety.[16]
2.4. Data sources
The Cochrane Library, Web of Science, PubMed, China National Knowledge Infrastructure, Wan Fang Data Knowledge Service Platform (Wan Fang Data), VIP shop Database, and China Biomedical Literature Database were searched using a computer. The language is limited to both Chinese and English. Randomized controlled trials on the intervention of TCM exercise therapy in the treatment of depression from the establishment of the database to June 31, 2023 were included. The search terms were subject and free words. According to the requirements of each database, Boolean logic-word connections in different formats were used for the retrieval. The search terms included “Traditional sports,” “Qigong,” “Tai Chi,” “Taiji,” “Baduanjin,” “Five-animal frolics,” “Wuqinxi,” “Five-animal exercises,” “Yijinjing,” “depression,” “depressive disorder.”
2.5. Search strategy
Using the Cochrane Library database as an example, the specific search strategy is described as follows:
-
#1
Mesh descriptor: [Depression] explode all trees
-
#2
Mesh descriptor: [Depressive Disorder] explode all trees
-
#3
Mesh descriptor: [Qigong] explode all trees
-
#4
Mesh descriptor: [Tai Ji] explode all trees
-
#5
(traditional sports): ti, ab, kw
-
#6
(Baduanjin): ti, ab, kw
-
#7
(five-animal frolics): ti, ab, kw
-
#8
(five-animal exercises): ti, ab, kw
-
#9
(Wuqinxi): ti, ab, kw
-
#10
(Yijinjing): ti, ab, kw
-
#11
#1 OR #2
-
#12
#3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10
-
#13
#11 AND #12
2.6. Literature screening and data extraction
Two researchers used Endnote 20 software to eliminate duplicate literature, followed by preliminary screening of the article abstracts according to the established criteria for inclusion and exclusion of literature. The remaining literature was screened for full-text reading and crosschecked after completion. If there is a disagreement, a third researcher will evaluate it to reach a consensus. Microsoft Excel was used to construct the data extraction tables independently. Information table extraction included baseline data, such as the first author of the literature, study sample size, age, intervention measures, intervention period, and outcome indicators.
2.7. Quality assessment
Literature quality assessment was conducted by 2 researchers using Cochrane’s bias risk assessment method[17] and Review Manager 5.4 software to systematically evaluate and analyze the included literature. We evaluated the 3 levels of low risk, high risk, and unclear risk in the 7 aspects of random allocation method, allocation scheme hiding, blind method of subjects and implementers, blind method of result measurers, data integrity, selective reporting, and other bias risks.[18] If there were differences, a third researcher was consulted to reach a consensus evaluation. Detailed information was obtained when raw data could not be obtained.
2.8. Statistical analysis
The final extracted data were analyzed using Stata 14.2 software for frequency network meta-analysis. Weighted mean difference (MD) and standardized mean difference (SMD) with 95% confidence intervals (CI) were used to represent econometric data. Heterogeneity between studies was assessed using the I2 test. When I2 was less than 50%, it proved that the homogeneity between studies was good, and a fixed effects model was used; When I2 was more than 50%, it indicated significant heterogeneity between studies, using a random effects model.[19] Ninety-five percent CI was used to represent the effect magnitude of the data, and P was less than .05, indicating a statistical difference. The ranking results of the area under the cumulative ranking curve surface under the cumulative ranking curve (SUCRA) for each intervention presented relatively optimal intervention measures in a table format.
3. Results
3.1. Literature screening process and basic characteristics
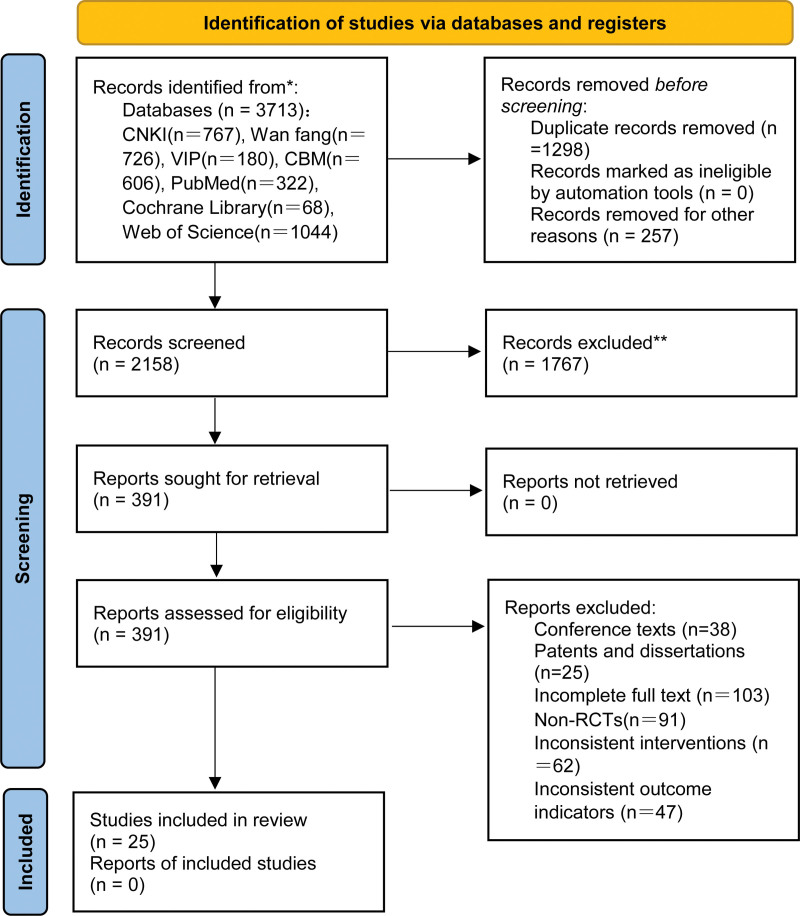
According to the search strategy, 3713 articles were initially obtained, and 25 studies[20-44] were finally included after excluding repetitive articles, abstracts, and full texts. There were 8 English articles, whereas the others were Chinese articles with a total of 1605 subjects. As the included literature does not include the intervention measure of Yijinjing, the intervention effect of Yijinjing will no longer be elaborated. The following section involves only a comparison of the effects of Baduanjin, Tai Chi, and Wuqinxi. The screening process is shown in Figure 1 and the basic characteristics of the included studies are listed in Table 1.
Figure 1.
Flowchart of study selection.
Table 1.
Characteristics of included studies.
| Author | Sample EG/CG | Age (yr) EG/CG | Intervention EG/CG | Time | Outcomes | |||
|---|---|---|---|---|---|---|---|---|
| Zhang et al[20] | 62 | 62 | NA | NA | Baduanjin + CG | Routine | 6 wk | ① |
| Tan[21] | 35 | 35 | NA | NA | Baduanjin | Blank | 10 mo | ② |
| Wang[22] | 30 | 30 | 21.8 ± 1.8 | 22.2 ± 1.6 | Wuqinxi | Blank | 12 wk | ①③ |
| Cheng et al[23] | 15 | 15 | 21.1 ± 1.4 | 21.0 ± 1.6 | Wuqinxi | Blank | 12 wk | ①③ |
| Yang et al[24] | 29 | 29 | 48.2 ± 7.66 | 45.24 ± 8.66 | Baduanjin + CG | Routine | 8 wk | ①④ |
| Cai[25] | 50 | 50 | NA | NA | Tai Chi + CG | Routine | 8 wk | ②⑤ |
| Zhao et al[26] | 26 | 26 | 59.92 | 60.23 | Tai Chi | Blank | 1 yr | ⑥ |
| Lin[27] | 33 | 33 | 61 | 62 | Tai Chi + CG | Routine | 8 wk | ②⑤ |
| Mi[28] | 39 | 38 | 39.4 ± 8.7 | 39.3 ± 9.1 | Tai Chi + CG | Routine | 6 wk | ①② |
| Suo[29] | 30 | 30 | 46 | 45.5 | Baduanjin + CG | Routine | 3 mo | ① |
| Lev et al[30] | 23 | 21 | 31.39 ± 8.03 | 32.1 ± 10.56 | Baduanjin + CG | Routine | 6 wk | ①③⑦ |
| Yang[31] | 20 | 17 | 45.45 ± 10.38 | 44.18 ± 11.5 | Baduanjin + CG | Routine | 6 wk | ①③⑦ |
| Li et al[32] | 20 | 20 | NA | NA | Baduanjin | Blank | 10 mo | ② |
| Rao[33] | 30 | 30 | 54.91 ± 4.65 | 54.32 ± 4.99 | Tai Chi + CG | Routine | 8 wk | ①④⑦ |
| Xiong et al[34] | 30 | 30 | 43.9 ± 6.0 | 42.2 ± 5.6 | Tai Chi | Blank | 6 mo | ①⑦ |
| Wang et al[35] | 30 | 30 | NA | NA | Wuqinxi | Blank | 6 mo | ②④ |
| Long et al[36] | 40 | 40 | 64.3 ± 3.55 | 64.09 ± 3.61 | Baduanjin + CG | Routine | NA | ②④ |
| Zhang et al[37] | 32 | 30 | NA | NA | Tai Chi + CG | Routine | 8 wk | ⑧ |
| Kee-Lee Chou et al[38] | 7 | 7 | NA | NA | Tai Chi | Blank | 3 mo | ⑨ |
| Yeung A et al[39] | 26 | 13 | NA | NA | Tai Chi | Blank | 12 wk | ① |
| María del Carmen Carcelén-Fraile et al[40] | 57 | 60 | 69.70 ± 6.15 | 69.75 ± 6.76 | Baduanjin | Blank | 12 wk | ④ |
| Helen Lavretsky et al[41] | 33 | 35 | 69.1 ± 7.0 | 72 ± 7.4 | Tai Chi + CG | Routine | 14 wk | ① |
| Tsang H. W.[42] | 48 | 34 | 82.74 ± 6.83 | 82.11 ± 7.19 | Baduanjin | Routine | 16 wk | ⑩ |
| Tsang W. W.[43] | 21 | 17 | 79.67 ± 6.55 | 80.65 ± 4.36 | Baduanjin | Routine | 12 wk | ⑥⑩ |
| Liao S. J.[44] | 55 | 52 | 71.84 ± 7.297 | 71.75 ± 8.201 | Tai Chi + CG | Routine | 3 mo | ⑥ |
Note: CG = control group, EG = experimental group, NA = not available.①=24-item Hamilton Rating Scale for Depression; ②=Self-rating Depression Scale; ③=Beck Depression Inventory; ④=Pittsburgh Sleep Quality Index; ⑤=Self-rating Anxiety Scale; ⑥=Geriatric Depression Scale; ⑦=Hamilton Anxiety Rating Scale; ⑧=9-item Patient Health Questionnaire; ⑨=Center for Epidemiological Survey, Depression Scale; ⑩=Chinese General Social Survey.
Data are presented as mean ± SD.
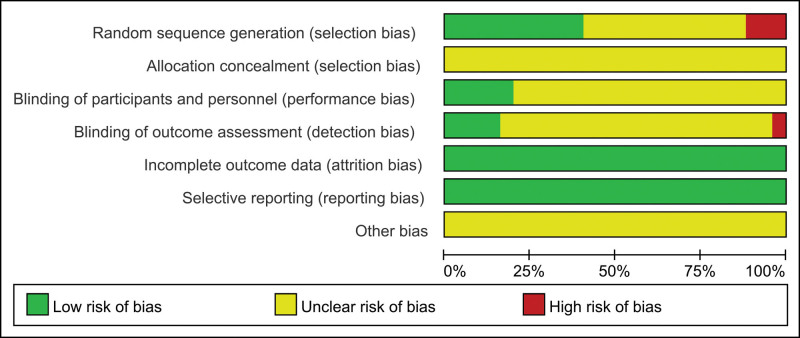
3.2. Evaluation of the quality of the included studies
Eleven studies[21,24,28,30,31,33,34,39,40,43,44]were evaluated as low risk by random number table grouping, 3 studies[22,25,32] were evaluated as high risk by grouping for the order of treatment, and 11 studies[20,23,26,27,29,35–38,41,42] only mentioned “random” evaluation as uncertainty. None of the studies mentioned the use of allocation concealment, which was considered uncertain. Nineteen studies[20–38,40] did not mention whether the implementation of blind method evaluation was uncertain, 5 studies[39,41–44]mentioned double-blind test evaluation as low risk, 1 study[44]was evaluated as low risk by a single-blind method in the implementation stage, and no blind method evaluation was evaluated as high risk in the measurement stage. The data integrity of all studies was good, no selective report was found, and the risk was evaluated as low. Therefore, none of the studies had any other reports of bias and were evaluated as uncertain. The risk assessment results are shown in Figure 2.
Figure 2.
Results of risk of bias evaluation of included studies.
3.3. Results of reticulated meta-analysis
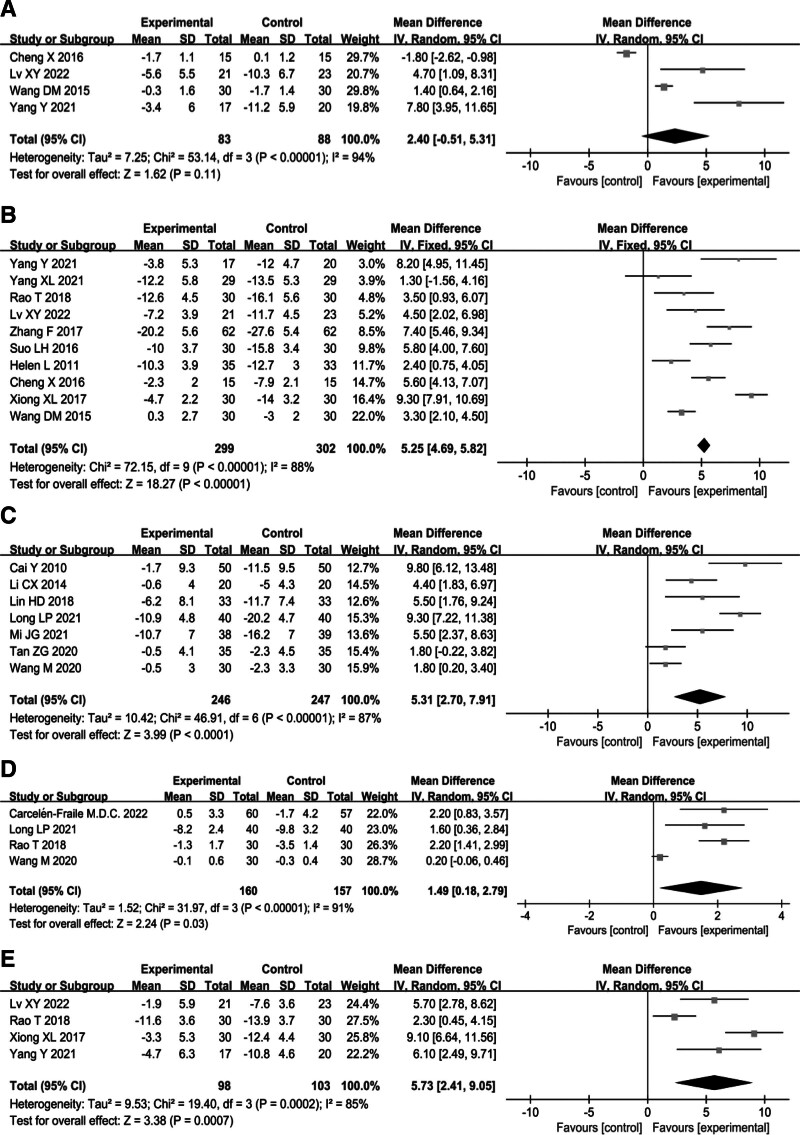
3.3.1. Assessment of heterogeneity.
The results of the heterogeneity estimates are presented as forest plots. Publication bias was measured for heterogeneous outcome indicators: I-square (I2). Figure 3 shows that the I2 of the 5 scores is greater than 50%, and the P value of the test for overall effect is less than .05, which indicates that the heterogeneity of all outcome indicators is high and significantly different. The I2 of the BDI score was 94%, and the composite MD was 2.40, with a 95% CI from −0.51 to 5.31, due to the better intervention effect of the control group than the experimental group in the first article (Fig. 3A). After we eliminated the first article, I2 was reduced to 84%, MD versus 95% CI was 4.30 [0.27, 8.32], and P value of .04 (please see the optimized picture in the attachment). The MD versus 95% CI for the HAMD score was 5.25 [4.69, 5.82], with an I2 of 88% (Fig. 3B). The MD versus 95% CI for the SDS score was 5.31 [2.70, 7.91], with an I2 of 87% (Fig. 3C). The MD versus 95% CI of the PSQI score was 1.49 [0.18, 2.79], with an I2 of 91% and a P value of .03 (Fig. 3D). The MD versus 95% CI of HAMA score was 5.73 [2.41, 9.05], with an I2 of 85% and a P value of .0007 (Fig. 3E).
Figure 3.
Forest plot for outcome indicators.
3.3.2. Consistency testing.
The 3 interventions in this study did not form a closed loop and do not require consistency testing.
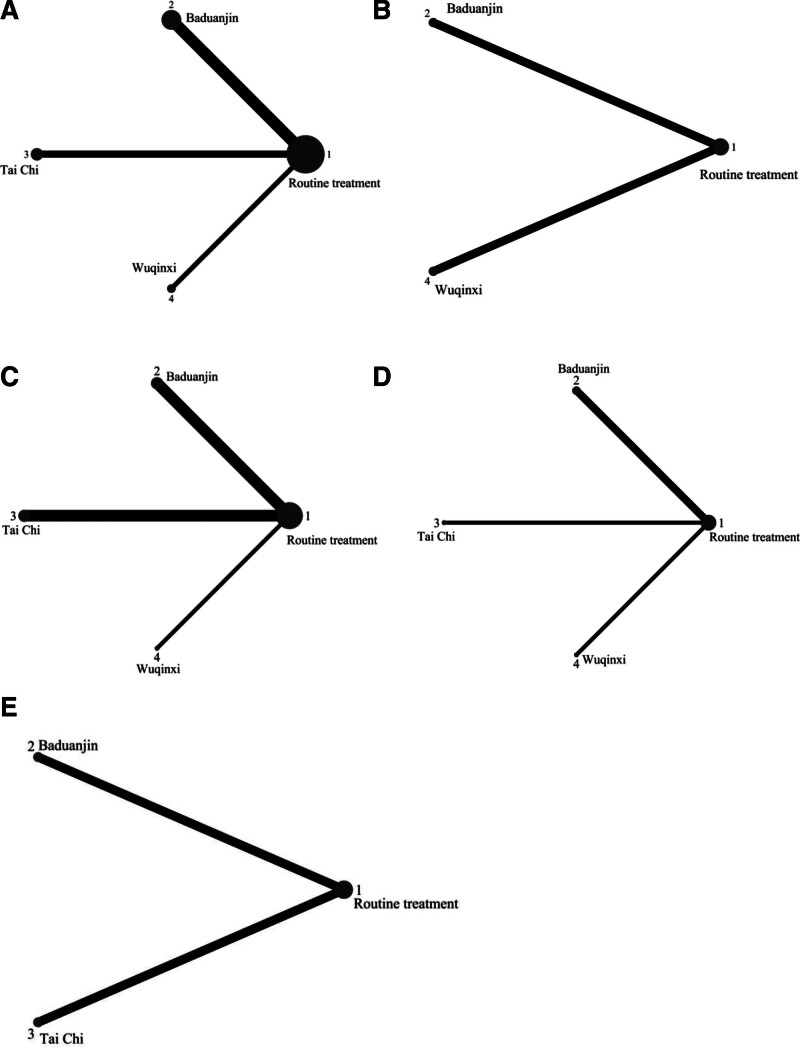
3.3.3. 24-Item Hamilton depression scale score.
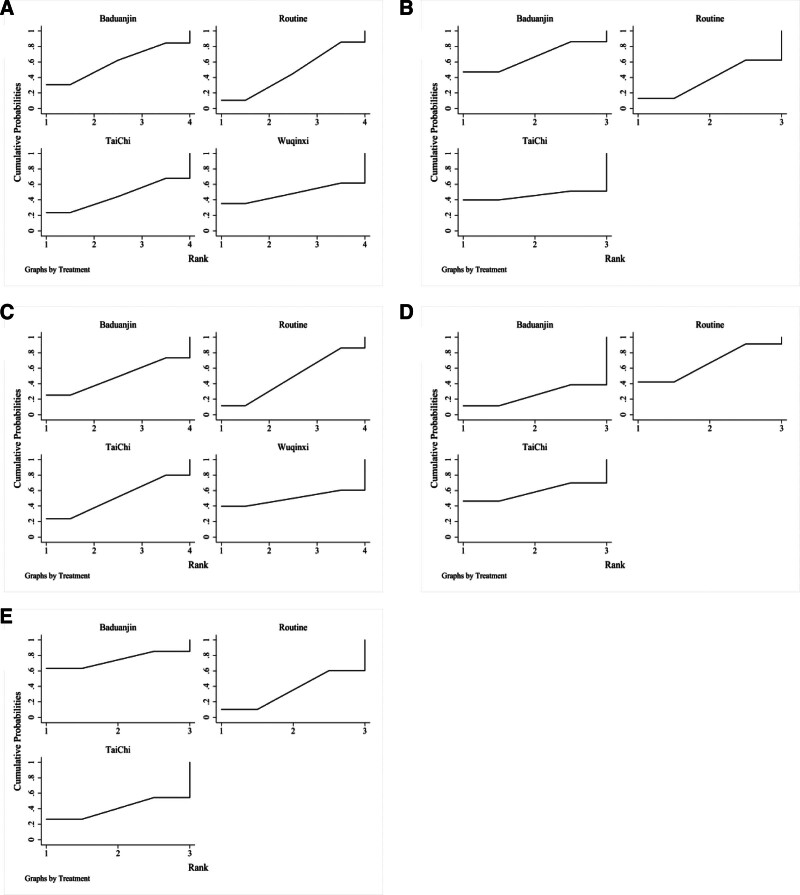
Ten studies[20,22–24,29–31,33,34,41]were included to compare HAMD alterations after traditional Chinese exercise treatment for depression. The evidence plot is shown in Figure 4A. The results of the network meta-analysis showed that the addition of Baduanjin compared with routine therapy only SMD = 0.10, 95% CI [−0.47, 0.67]; the addition of Tai Chi compared with routine therapy only SMD = −0.05, 95% CI [−0.88, 0.79]; and the addition of Wuqinxi compared with routine therapy only SMD = −0.00, 95% CI [−1.33, 1.33]. Regarding the change in HAMD values, the difference in variability was not statistically significant (Table 2). The improvement effects of the 3 exercises on HAMD variation in descending order of specific ranking (rank) were as follows: Baduanjin (SUCRA = 59.2), Wuqinxi (SUCRA = 48.4), routine treatment (SUCRA = 47.1), and Tai Chi (SUCRA = 45.2), as shown in Figure 5A.
Figure 4.
Evidence network for outcome indicators.
Table 2.
Results of the network meta-analysis of the score of 24-item Hamilton depression scale (standardized mean difference with 95% confidence intervals).
| Intervention | Baduanjin | Wuqinxi | Tai Chi | Routine |
|---|---|---|---|---|
| Baduanjin | 1 | |||
| Wuqinxi | 0.10 (−1.35, 1.54) | 1 | ||
| Tai Chi | 0.14 (−0.87, 1.15) | 0.05 (−1.53, 1.62) | 1 | |
| Routine | 0.10 (−0.47, 0.67) | −0.00 (−1.33, 1.33) | −0.05 (−0.88, 0.79) | 1 |
Figure 5.
Probability ranking of outcome indicators.
3.3.4. Beck depression inventory score.
Four studies[22,23,30,31]compared BDI alterations after traditional Chinese exercise treatment for depression. The evidence plot is shown in Figure 4B. The results of the network meta-analysis showed that the addition of Baduanjin compared with routine therapy only SMD = 0.28, 95% CI [−0.53, 1.08], and the addition of Wuqinxi compared with routine therapy only SMD = −0.00, 95% CI [−2.59, 2.59]. Regarding the change in the BDI values, the difference in variability was not statistically significant (Table 3). The improvement effect of exercises on BDI variation in descending order of specific ranking (rank) was Baduanjin (SUCRA = 66.4), Wuqinxi (SUCRA = 46.4), and routine treatment (SUCRA = 37.2; Fig. 5B).
Table 3.
Results of the network meta-analysis of the score of beck depression inventory (standardized mean difference with 95% confidence intervals).
| Intervention | Baduanjin | Wuqinxi | Routine |
|---|---|---|---|
| Baduanjin | 1 | ||
| Wuqinxi | 0.28 (−2.43, 2.98) | 1 | |
| Routine | 0.28 (−0.53, 1.08) | 0.00 (−2.59, 2.59) | 1 |
3.3.5. Self-rating depression scale score.
Seven studies[21,25,27,28,32,35,36]were included to compare SDS changes after traditional exercise treatment for depression. An evidence plot is shown in Figure 4C. The results of the network meta-analysis showed that the addition of Baduanjin compared with routine therapy only SMD = −0.00, 95% CI [−0.76, 0.76]; the addition of Tai Chi compared with routine therapy only SMD = 0.02, 95% CI [−0.54, 0.58]; and the addition of Wuqinxi compared with routine therapy only SMD = 0.00, 95% CI [−1.56, 1.56]. Regarding the change in the HAMD values, the difference in variability was not statistically significant (Table 4). The improvement effect of the 3 exercises on SDS variation in descending order of specific ranking was: Tai Chi (SUCRA = 52), Wuqinxi (SUCRA = 49.6), Baduanjin (SUCRA = 49.3), Routine treatment (SUCRA = 49.1), shown in Figure 5C.
Table 4.
Results of the network meta-analysis of the score of self-rating depression scale (standardized mean difference with 95% confidence intervals).
| Intervention | Tai Chi | Wuqinxi | Baduanjin | Routine |
|---|---|---|---|---|
| Tai Chi | 1 | |||
| Wuqinxi | 0.02 (−1.64, 1.68) | 1 | ||
| Baduanjin | 0.02 (−0.93, 0.97) | 0.00 (−1.74, 1.74) | 1 | |
| Routine | 0.02 (−0.54, 0.58) | 0.00 (−1.56, 1.56) | −0.00 (−0.76, 0.76) | 1 |
3.3.6. Pittsburgh sleep quality index score.
Four of the 25 studies[33,35,36,40]reported PSQI scores including routine treatment combined with Baduanjin, Tai Chi, and Wuqinxi. However, the fourth data point intersected with the invalid line and was excluded. The evidence plot is shown in Figure 4D. The results of the network meta-analysis showed that the addition of Baduanjin compared with routine therapy only SMD = −0.88, 95% CI [−2.77, 1.01]; the addition of Tai Chi compared with routine therapy only SMD = −0.00, 95% CI [−2.95, 2.95]. Regarding the change in PSQI values, the difference in variability was not statistically significant (P > .05; Table 5). The improvement effect of exercise on PSQI variation in the descending order of specific ranking (rank) was as follows: routine treatment (SUCRA = 65.4), Tai Chi (SUCRA = 59.1), and Baduanjin (SUCRA = 25.6), as shown in Figure 5D.
Table 5.
Results of the network meta-analysis of the score of Pittsburgh sleep quality index (standardized mean difference with 95% confidence intervals).
| Intervention | Baduanjin | Tai Chi | Routine |
|---|---|---|---|
| Baduanjin | 1 | ||
| Tai Chi | −0.88 (−4.39, 2.62) | 1 | |
| Routine | −0.88 (−2.77, 1.01) | −0.00 (−2.95, 2.95) | 1 |
3.3.7. Hamilton anxiety scale score.
Four studies[30,31,33,34]compared HAMA alterations after traditional exercise treatments for depression. An evidence plot is shown in Figure 4E. The results of the network meta-analysis showed that the addition of Baduanjin compared with routine therapy only (SMD = 0.36, 95% CI [−0.53, 1.26]) and the addition of Tai Chi compared with routine therapy only (SMD = −0.00, 95% CI [−0.95, 0.95]). Regarding the changes in HAMA values, the difference in variability was not statistically significant (Table 6). The improvement effect of exercise on HAMA variation in the descending order of specific ranking (rank) was as follows: Baduanjin (SUCRA = 74.8), Tai Chi (SUCRA = 39.3), and routine treatment (SUCRA = 35.9), as shown in Figure 5E.
Table 6.
Results of the network meta-analysis of the score of Hamilton anxiety scale (standardized mean difference with 95% confidence intervals).
| Intervention | Baduanjin | Tai Chi | Routine |
|---|---|---|---|
| Baduanjin | 1 | ||
| Tai Chi | 0.36 (−0.94, 1.67) | 1 | |
| Routine | 0.36 (−0.53, 1.26) | −0.00 (−0.95, 0.95) | 1 |
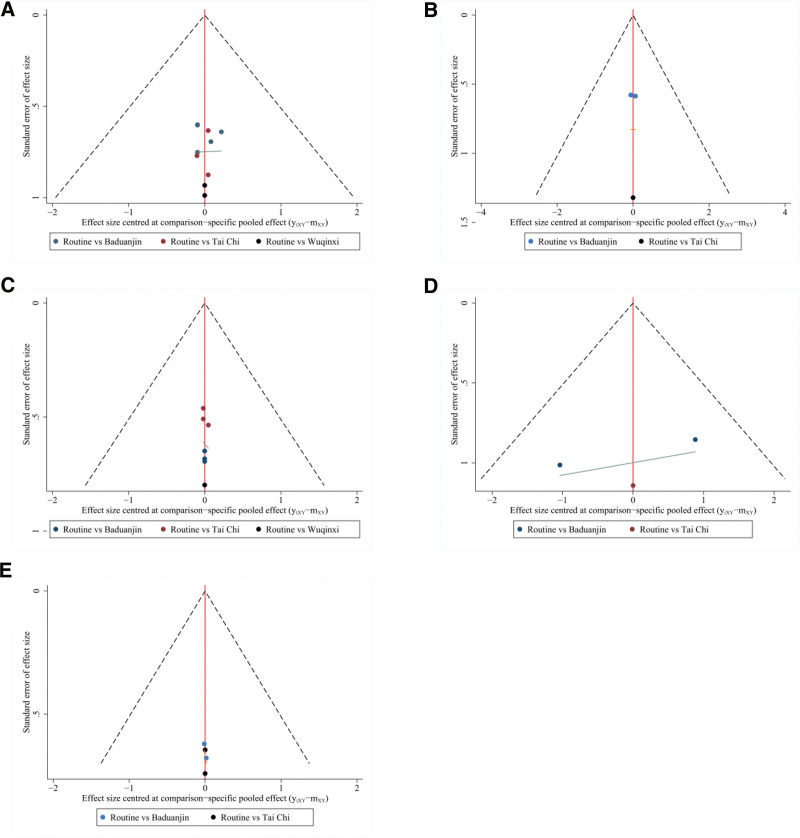
3.3.8. The small sample effect and publication bias.
Studies with HAMD, BDI, SDS, PSQI, and HAMA as indicators were included to compare and correct funnel charts to assess small-sample effects (Fig. 6). The results showed that the comparison–correction funnel plot of HAMD, BDI, and PSQI values showed basic symmetry, and that the studies were roughly symmetrically distributed on either side of the midline, indicating that a small sample effect is less likely to exist. The symmetry of the SDS and HAMA values was poor, indicating a high possibility of a small sample effect. The reasons for this may be related to the low quality of the included studies, small sample sizes, and types of traditional exercises used.
Figure 6.
Comparison–correction funnel plot of each outcome indicator.
4. Discussion
Traditional Chinese exercise is widely used in hospitals to treat various diseases. Among the 4 exercises expected to be found, except for Wuqinxi and Yijinjing, Tai Chi and Baduanjin were the most frequently used to prevent and treat depression. Many meta-analyses have been conducted; however, only a few studies have compared the efficacy of each method. In practice, only one method was selected for intervention. For example, Dong Y explored the effect of 5 traditional Chinese exercises on depression and anxiety in the elderly, and the statistical data showed that the effect of Tai Chi exercise was significantly better than that of other exercises (including Baduanjin, Wuqinxi, Yijinjing, and Liuzijue).[45] Our study conducted a network meta-analysis of various exercises for the treatment of depression, which is compatible with modern medicine and broadens clinical treatment ideas.
This study summarizes the intervention effects of 3 traditional exercises in patients with depression. The results showed that the 3 functional groups were superior to the conventional treatment group in reducing HAMD, BDI, SDS, and HAMA scores, and the difference was statistically significant. The network diagram showed that each index group was a double-arm study compared to the conventional group, and no closed loop was formed. The rank probability ranking showed that the Baduanjin exercise method had the best effect in reducing the HAMD, BDI, and HAMA scores. Tai Chi method has the best effect in improving SDS score, and HAMD score is the worst. Wuqinxi exercise has a good effect in reducing the HAMD and SDS scores.
However, conventional treatments are more effective in improving sleep quality. The inconsistency between this result and that of the meta-analysis may be attributed to several reasons. On one hand, the patient’s depression level may have been affected by other potential factors during treatment. However, the differences in interpersonal communication and exercise may have been caused by the small sample size. As shown in the league table, there were no statistically significant differences between the exercise and conventional treatment groups. In addition, the adjusted funnel plot showed that the SDS and HAMA scores were relatively unbalanced and the remaining groups were balanced symmetrically on the midline, indicating that there may be a small sample effect in this study.
5. Limitations
This study had some limitations: There may be some language bias if only the Chinese and English databases are searched. The included studies did not fully specify the generation of random sequences, allocation concealment, double-blind method, and selective reporting, which may have selection and measurement bias. There were some differences between the methods included in the study and the expected setting. Literature on the application of the Yijinjing method is not included, and the number of studies is small owing to the strict standards, which may affect the reliability of the conclusion. Due to the large number of indicators, the study did not include all the indicators of the entire literature, which weakened the argument to a certain extent. The safety indicators were not reported in the literature, so the safety conclusions of each exercise could not be drawn.
6. Conclusion
In this study, we evaluated the effects of 3 commonly used traditional exercises on the treatment of depression using 5 different outcome indicators. The results of the network meta-analysis showed that there was no significant difference in each exercise method compared with conventional treatment or blank intervention alone. In terms of reducing the scores of each index, Baduanjin ranked the highest in the improvement probability of HAMD, BDI, and HAMA; Tai Chi ranked the highest in the reduction probability of SDS; and routine treatment or blank intervention was the best in improving the PSQI score. In summary, the intervention effect of Baduanjin was better than that of Tai Chi, and we believe that Baduanjin exercise can be used as an intervention for depression in clinical practice. However, the effects of Wuqinxi and unstudied Yijinjing remain unclear and need to be studied in the future.
Although the current research has confirmed the unique effect of traditional Chinese exercises in the intervention of depression, the standardization of their clinical application still needs to be further studied. In the future, we intend to the supervision of the effect evaluation of traditional Chinese exercises, distinguishing the time and intensity of intervention, and completing more high-quality RCT studies to further verify the improvement effect of various exercises on patients with depression and strive to promote the standardized and extensive application of traditional Chinese exercises.
Author contributions
Conceptualization: Yang Feng.
Data curation: Yang Feng, Jin Liu.
Formal analysis: Jin Liu, Peng Liu.
Funding acquisition: Jing Teng.
Investigation: Jin Liu, Peng Liu.
Methodology: Yang Feng.
Project administration: Jing Teng.
Resources: Jin Liu, Jing Teng.
Software: Yang Feng.
Supervision: Peng Liu, Jing Teng.
Validation: Jin Liu, Peng Liu.
Visualization: Yang Feng.
Writing – original draft: Yang Feng, Jin Liu.
Writing – review & editing: Peng Liu, Jing Teng.
Abbreviations:
- BDI
- beck depression inventory
- CI
- confidence intervals
- HAMA
- Hamilton anxiety scale
- HAMD-24
- 24-item Hamilton depression scale
- HAMD
- Hamilton depression scale
- MD
- weighted mean difference
- PSQI
- Pittsburgh sleep quality index
- SDS
- self-rating depression scale
- SMD
- standardized mean difference
- SUCRA
- surface under the cumulative ranking curve
- TCM
- traditional Chinese medicine
The authors have no funding and conflicts of interest to disclose.
How to cite this article: Feng Y, Liu J, Liu P, Teng J. Traditional Chinese exercises on depression: A network meta-analysis. Medicine 2024;103:13(e37319).
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Contributor Information
Yang Feng, Email: 715512591@qq.com.
Jin Liu, Email: 1500205546@qq.com.
Peng Liu, Email: 1500205546@qq.com.
References
- [1].Jaeschke R, Siwek M, Dudek D. Neurobiology of suicidal behavior. Psychiatr Pol. 2011;45:573–88. [PubMed] [Google Scholar]
- [2].Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wu ZJ, Liu QY. Psychological state and quality of life of the major depressed patients’ relatives. Chin J Health Psychol. 2018;26:330–3. [Google Scholar]
- [4].Yan XN, Chen TY, Peng SQ, et al. Intervention effect of five-element music therapy for patients with depression: a meta-analysis. J Clin Nurs Pract. 2019;5:1–5. [Google Scholar]
- [5].Yuan CR, Tao P. The role of traditional exercise therapy in overall health. Chin J Gerontol. 2020;40:5344–8. [Google Scholar]
- [6].Zhou J, Xiang FM. The inheritance of traditional Chinese medicine classics and the application of innovative models for patient chronic disease management. J Tradit Chin Med. 2021;29:350–1. [Google Scholar]
- [7].Lu Y, Li J, Jiang J, et al. The effect of Baduanjin on depression: a systematic review. Chin Prev Med. 2021;22:434–44. [Google Scholar]
- [8].Lou H, Liu P. A meta-analysis of the effect of physical exercise as a treatment on depression. J Tianjin Univ Sport. 2018;33:500–7. [Google Scholar]
- [9].Zhang JY, Li Z, Xiao T. A meta-analysis of the influence of traditional Chinese medicine fitness on anxiety and depression symptoms in college students. Mod Prev Med. 2021;48:4324–30. [Google Scholar]
- [10].Easton K, Coventry P, Lovell K, et al. Prevalence and measurement of anxiety in samples of patients with heart failure: meta-analysis. J Cardiovasc Nurs. 2016;31:367–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Xiao Q, Zhang DL. Similarities and differences between the diagnostic criteria of ICD-11 and DSM-5 for depression disorder. Sichuan Ment Health. 2019;32:543–7. [Google Scholar]
- [12].Tong P, Dong LP, Yang Y, et al. Traditional Chinese acupuncture and postpartum depression: a systematic review and meta-analysis. J Chin Med Assoc. 2019;82:719–26. [DOI] [PubMed] [Google Scholar]
- [13].Ji CF, Wu GH, Du XD, et al. Factors that contribute to trait mindfulness level among hospitalized patients with major depressive disorder. Front Psychiatry. 2023;14:1144989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Luo H, Gong R, Zheng R, et al. Dose-effect of long-snake-like moxibustion for chronic fatigue syndrome: a randomized controlled trial. J Transl Med. 2023;21:430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Wang Y, Jia NX, Zhou Y, et al. A comparison of the effects of remote coaching HIIT training and combined exercise training on the physical and mental health of university students. Front Psychol. 2023;14:1182332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Craba A, Marano G, Kotzalidis GD, et al. Resilience and attachment in patients with major depressive disorder and bipolar disorder. J Pers Med. 2023;13:969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Martos-Cobo E, Mayoral-Sanz P, Expósito-Delgado AJ, et al. Effect of rapid maxillary expansion on the apnoeahypopnoea index during sleep in children, Systematic review. J Clin Exp Dent. 2022;14:e769–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Li JX, Zhang XM, Wang WR, et al. Network Meta-Analysis of oral Chinese patent medicine in treatment of type 2 diabetic peripheral neuropathy. Chin Tradit Herbal Drugs. 2023;54:5677–95. [Google Scholar]
- [19].Dersimonlan R, Laird N. Meta-analysis of clinical trials. Control Clin Trials. 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- [20].Zhang F, Lin ZH, Zhang L, et al. Observation of clinical Effect by paroxetine combined with eight trigrams boxing exercise therapy for depression patients. Chin J Mod Drug Appl. 2017;11:109–11. [Google Scholar]
- [21].Tan ZG, Tan QW. A study on the psychological and physical effects of fitness qigong Baduanjin on depressed college students. Contemp Sports Technol. 2020;10:182–3 + 185. [Google Scholar]
- [22].Wang DM, Qin QZ. Evaluation of health qigong: five animal games intervene in college students with mild depression. Contemp Sports Technol. 2015;5:29–30. [Google Scholar]
- [23].Cheng X, Wang DM, Chen X, et al. Health qigong Wuqinxi improves hydrogen proton magnetic resonance spectra in prefrontal cortex and hippocampus in college students with mild depression. J South Med Univ. 2016;36:1468–76. [PubMed] [Google Scholar]
- [24].Yang XL, Li YN, Xu XT, et al. Effect of Baduanjin combined with ago melatonin in patients with depression and insomnia. J Int Psychiatry. 2021;48:258–60. [Google Scholar]
- [25].Cai Y, Zhou HF. Taijiquan sport to depression patient mood influence. Med J Chin Peoples Health. 2010;22:2051–2112. [Google Scholar]
- [26].Zhao GZ, Cheng RH, Jie CC, et al. Study on the influence of shadowboxing on mild depression among middle aged and senior people. Chin J Convalescent Med. 2015;24:452–4. [Google Scholar]
- [27].Lin HD, Yu J, Zhang F. Influence of shadowboxing on mood of elderly patients with depression during convalescence. Chin Community Doctors. 2018;34:168–170. [Google Scholar]
- [28].Mi JG. Clinical effect of modified Chaihu Longgu Muli decoction combined with Tai Chi exercise in the treatment of depression: an analysis of 40 cases. Hunan J Tradit Chin Med. 2021;37:6–9 + 13. [Google Scholar]
- [29].Suo LH, Yu HJ. Jieyu decoction with psychological intervention and Ba Duan Jin exercises improved depressive symptoms in perimenopausal patients. J Changchun Univ Chin Med. 2016;32:131–3. [Google Scholar]
- [30].Lyu XY, Yang Y, Lin YN, et al. Modulation of rumination response for mild to moderate depression by traditional Chinese medicine relaxing and calming exercises. Liaoning J Tradit Chin Med. 2022;49:119–23. [Google Scholar]
- [31].Yang Y, Li GX. The effect of Baduanjin combined with relaxation skill on the psychological status of mild to moderate depression patients. China Pharm. 2021;30:237–8. [Google Scholar]
- [32].Li CX, Tan ZG, Liu S. Research on Baduanjin exercise treating depression in college students. Sports Sci Res. 2014;18:72–5. [Google Scholar]
- [33].Rao T, Ni HJ. The effect of Tai Chi on sleep and mood in patients with depression related insomnia. Chin Prim Health Care. 2018;32:66–78. [Google Scholar]
- [34].Xiong XL, Moue CY, Feng YN. Discussion on the effect of Tai Chi exercise on depression and heart rate variability in middle and elderly people. China Med Devices. 2017;32:148–9. [Google Scholar]
- [35].Wang M, Zhao QW, Wu H, et al. Study on Hua Tuo’s five mimic-animal boxing intervention therapies for college students with mild psychological problems. J Liaoning Med Univ Soc Sci Ed. 2020;18:60–2. [Google Scholar]
- [36].Long LP, Liu J, Jing JY, et al. Experimental study of Ba Duan Jin fitness qigong to improve depression in retirees. Diet Health. 2021;37:7–8. [Google Scholar]
- [37].Zhang JY, Qin SD, Zhou Y, et al. A randomized controlled trial of mindfulness-based Tai Chi Chuan for subthreshold depression adolescents. Neuropsychiatr Dis Treat. 2018; 14:2313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Chou KL, Lee PW, Yu EC, et al. Effect of Tai Chi on depressive symptoms amongst Chinese older patients with depressive disorders: a randomized clinical trial. Int J Geriatr Psychiatry. 2004;19:1105–7. [DOI] [PubMed] [Google Scholar]
- [39].Yeung A, Lepoutre V, Wayne P, et al. Tai chi treatment for depression in Chinese Americans: a pilot study. Am J Phys Med Rehabil. 2012;91:863–70. [DOI] [PubMed] [Google Scholar]
- [40].Carcelén-Fraile MDC, Aibar-Almazán A, Martínez-Amat A, et al. Qigong for mental health and sleep quality in postmenopausal women: a randomized controlled trial. Medicine (Baltimore). 2022;101:e30897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Lavretsky H, Alstein LL, Olmstead RE, et al. Complementary use of Tai Chi chih augments escitalopram treatment of geriatric depression: a randomized controlled trial. Am J Geriatr Psychiatry. 2011;19:839–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Tsang HWH, Fung KMT, Chan ASM, et al. Effect of a qigong exercise programme on elderly with depression. Int J Geriatr Psychiatry. 2006;21:890–7. [DOI] [PubMed] [Google Scholar]
- [43].Tsang HW, Tsang WW, Jones AY, et al. Psycho-physical and neurophysiological effects of qigong on depressed elders with chronic illness. Aging Ment Health. 2013;17:336–48. [DOI] [PubMed] [Google Scholar]
- [44].Liao SJ, Tan MP, Chong MC, et al. The impact of combined music and Tai Chi on depressive symptoms among community-dwelling older persons: a cluster randomized controlled trial. Issues Ment Health Nurs. 2018;39:398–402. [DOI] [PubMed] [Google Scholar]
- [45].Dong Y, Kuang X, Dong L, et al. Exploring the efficacy of traditional Chinese medicine exercise in alleviating anxiety and depression in older adults: a comprehensive study with a randomized controlled trial and network meta-analysis. Front Psychol. 2023;14:e1290471. [DOI] [PMC free article] [PubMed] [Google Scholar]