Abstract
Background
A retained coronary guidewire following coronary angiography is an extremely rare complication. We present a case of a retained coronary guidewire from a percutaneous coronary intervention done 2 years ago.
Case summary
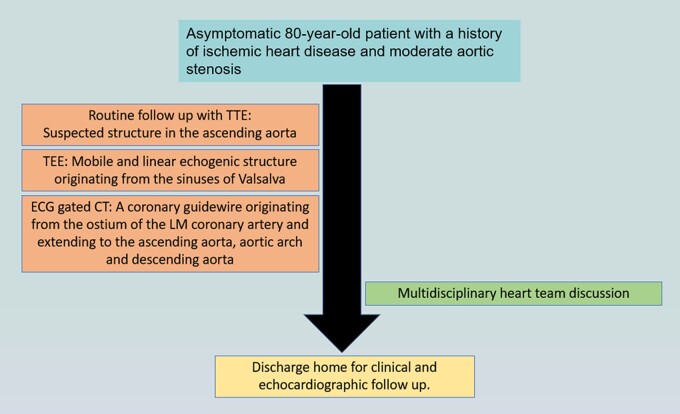
An 80-year-old asymptomatic man with a history of ischemic heart disease and moderate aortic stenosis presented to the echocardiography lab for routine follow-up. Transthoracic echocardiography showed Moderate aortic stenosis and a suspected linear echogenic structure in the ascending aorta. trans-esophageal echocardiography was performed to reveal a mobile and linear echogenic structure originating from the sinuses of Valsalva/Sinotubular junction and extending to the ascending aorta. An electrocardiogram gated cardiac computed tomography was performed and showed A linear well-defined structure originating from the ostium of the left main coronary artery and extending to the ascending aorta—a coronary guidewire from an earlier procedure. A second look at the last invasive coronary angiography record demonstrated the same finding. A multidisciplinary heart team discussion was obtained and concluded that the risk of surgical or endovascular intervention outweighed the potential benefit. The patient was discharged home for a close clinical and echocardiographic follow-up.
Discussion
A retained coronary guidewire is a rare complication that operators should be aware of. Management should be case-specific depending on clinical presentation.
Keywords: Case report, Coronary guidewire, Cardiac computed tomography, Echocardiography, Aortic dissection
Learning points.
A retained coronary guidewire is a rare complication that operators should be aware of following percutaneous coronary intervention (PCI).
The use of multi-modality imaging is essential for accurate diagnosis and a multidisciplinary heart team discussion is important for appropriate treatment decisions.
Introduction
Invasive coronary angiography and percutaneous coronary intervention (PCI) have become the standard of care for all non-ST segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI) as well as for part of the patients with chronic coronary syndromes.1,2,3 Complications may occur during percutaneous coronary procedures or subsequently. Some of the common complications include coronary artery dissection or perforation, hyper-acute stent thrombosis, contrast-induced nephropathy or anaphylaxis, and vascular access site-related complications.4,5 A retained coronary guidewire is an extremely rare complication. We present a case of a retained coronary guidewire from a PCI done 2 years ago.
Summary figure
Case presentation
An 80-year-old male presented to the echocardiography lab for routine follow-up for moderate aortic stenosis (AS). His medical comorbidities included hyperlipidaemia, hypertension, and type 2 diabetes mellitus. In the past, the patient underwent multiple PCI’s due to ischemic heart disease (IHD). His last coronary intervention involved implanting a drug eluting stent (DES) to the left main (LM) and proximal left anterior descending (LAD) coronary arteries, at an outside institution 2 years ago.
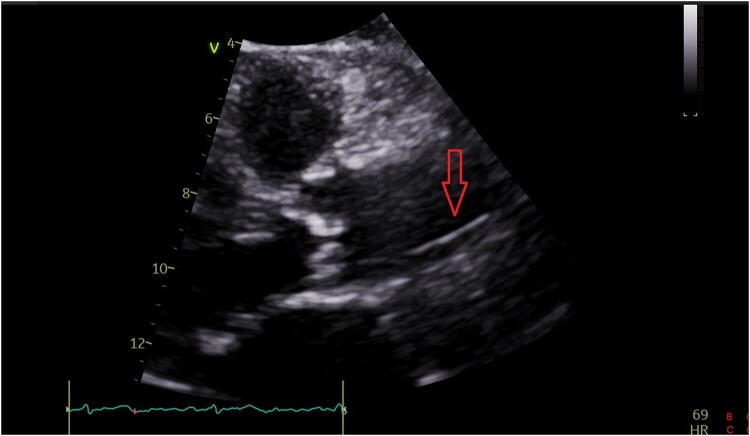
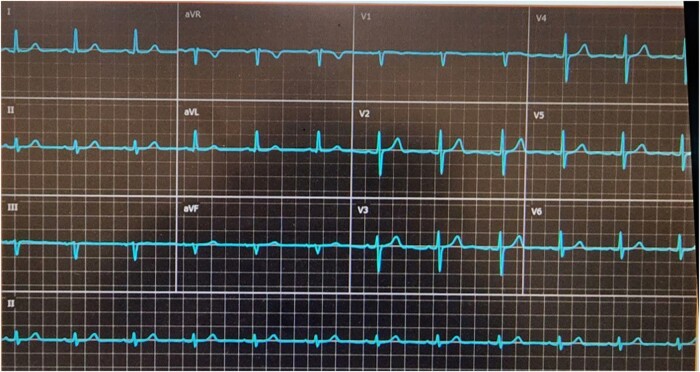
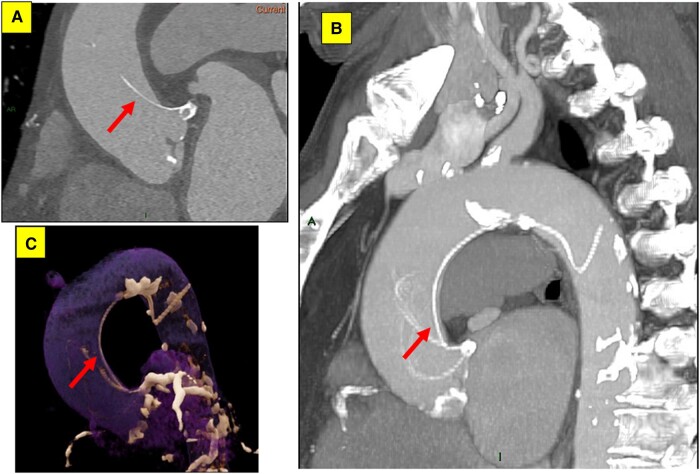
The patient was hemodynamically stable and reported no chest pain, back pain, or dyspnoea. Cardiac auscultation demonstrated regular heart sounds with crescendo-decrescendo systolic murmur heard best at the right upper sternal border, radiating to the neck. His lungs were clear and he had no signs of heart failure. Initial Transthoracic echocardiography (TTE) showed normal left ventricular systolic function with moderate AS (aortic valve area: 1.1 cm², max and mean aortic gradients: 46 and 30 mmHg, respectively), moreover, a suspected linear echogenic structure was noted in the ascending aorta, which was suspicious for a dissection flap or an artefact (Figure 1, Supplementary material online, Videos S1 and S2). As mentioned above, the patient was completely asymptomatic and for better visualization, evaluation, and characterization of the findings seen on TTE, trans-esophageal echocardiography (TEE) was immediately performed to reveal a mobile and linear echogenic structure originating from the sinuses of Valsalva/Sinotubular junction (STJ) and extending to the ascending aorta and the aortic arch (Figure 2, Supplementary material online, Video S3), highly suspicious for Stanford type A aortic dissection. No aortic regurgitation was noted (see Supplementary material online, Video S4). Electrocardiogram (ECG) showed normal sinus rhythm with no signs of acute ischaemia (Figure 3). Blood tests for high-sensitivity cardiac Troponin T (hs-cTnT) and Creatine Kinase-Myocardial Band (CK-MB) were negative. Immediate ECG-gated cardiac computed tomography (CT) was performed. In CT images the aortic endothel was intact and no false lumen was noticed, thus ruling out aortic dissection. A linear well-defined structure was noted originating from the ostium of the LM coronary artery and extending to the ascending aorta, aortic arch, and descending aorta, most probably a coronary guidewire from an earlier procedure (Figure 4). A second look at the last invasive coronary angiography record demonstrated the same finding at the end of the procedure—a coronary guidewire originating from the LM coronary artery and extending to the ascending aorta (see Supplementary material online, Video S5). A multidisciplinary heart team discussion, including an invasive cardiologist, a cardiothoracic surgeon, and a cardiac imaging specialist, was obtained, and concluded that the risk of surgical or endovascular intervention outweighed the potential benefit, particularly since the patient was completely asymptomatic, at advanced age and with multiple comorbidities. Discharge home followed several detailed explanations to the patient and his family regarding his condition and a recommendation for a close clinical and echocardiographic follow-up.
Figure 1.
Transthoracic echocardiography.
Figure 2.
Trans-esophageal echocardiography.
Figure 3.
Twelve lead electrocardiogram.
Figure 4.
Electrocardiogram gated cardiac computed tomography.
Discussion
A retained coronary guidewire is an extremely rare complication that occurs in 0.1–0.2% of PCI procedures.6 In some cases of wire entrapment, over-rotation, or excessive bending—a wire fracture may occur.7 A retained coronary guidewire or guidewire remnants can lead to various complications including acute thrombosis or perforation of the coronary artery involved and systemic thrombo-embolization, leading to cerebrovascular accident (CVA).8,9
Most reported cases of entrapped guidewires were cases discovered during PCI.10 This is a rare case of a jailed wire behind the LM stent struts protruding the aorta, discovered years after the procedure. The use of multi-modality imaging was essential for accurate diagnosis and for further risk stratification. Management of patients with retained fractured guidewire fragments during PTCA remains particularly challenging due to the lack of data regarding clinical outcomes. There are no specific guidelines as to how this complication should be managed. Treatment options include conservative treatment and close follow-up (if the patient is completely asymptomatic), medical treatment with anticoagulation (in case of systemic embolization),11 and endovascular retrieval or surgical extraction (in case of acute thrombosis, perforation, or embolic phenomena threatening coronary artery occlusion).10
In conclusion, a retained coronary guidewire is a rare complication that operators should be aware of. Management should be case-specific depending on clinical presentation.
Supplementary Material
Acknowledgements
The authors thank Osnat Benvenisti for her support in the image acquisition and processing.
Consent: The authors confirm that written consent for the submission and publication of this case report, including images, Videos, and associated text, was obtained from the patient in accordance with COPE guidance.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Ziad Arow, Cardiology Department, Meir Medical Center, Tchernichovsky St 59, Kfar Saba 4418001, Israel; Sackler Faculty of Medicine, Tel-Aviv University, Kiryat HaUniversita, Ramat Aviv Tel Aviv 6139001, Israel.
Avigdor Bar Sef, Cardiology Department, Meir Medical Center, Tchernichovsky St 59, Kfar Saba 4418001, Israel; Sackler Faculty of Medicine, Tel-Aviv University, Kiryat HaUniversita, Ramat Aviv Tel Aviv 6139001, Israel.
Abid Assali, Cardiology Department, Meir Medical Center, Tchernichovsky St 59, Kfar Saba 4418001, Israel; Sackler Faculty of Medicine, Tel-Aviv University, Kiryat HaUniversita, Ramat Aviv Tel Aviv 6139001, Israel.
Yoav Arnson, Cardiology Department, Meir Medical Center, Tchernichovsky St 59, Kfar Saba 4418001, Israel; Sackler Faculty of Medicine, Tel-Aviv University, Kiryat HaUniversita, Ramat Aviv Tel Aviv 6139001, Israel.
Lead author biography
Ziad Arow is currently a resident in the cardiology department at Meir Medical Center in Israel. Ziad Arow finished his medical school (Technion, Israel) in 2016 and completed his internal medicine residency (Rabin Medical Center, Israel) in 2021.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports online.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur Heart J 2018;39:119–177. [DOI] [PubMed] [Google Scholar]
- 2. Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289–1367. [DOI] [PubMed] [Google Scholar]
- 3. Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41:407–477. [DOI] [PubMed] [Google Scholar]
- 4. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 2019;40:87–165.30165437 [Google Scholar]
- 5. Kandan SR, Johnson TW. Management of percutaneous coronary intervention complications. Heart 2019;105:75–86. [DOI] [PubMed] [Google Scholar]
- 6. Hartzler GO, Rutherford BD, McConahay DR. Retained percutaneous transluminal coronary angioplasty equipment components and their management. Am J Cardiol 1987;60:1260–1264. [DOI] [PubMed] [Google Scholar]
- 7. Lotan C, Hasin Y, Stone D, Meyers S, Applebaum A, Gotsman MS. Guide wire entrapment during PTCA: a potentially dangerous complication. Cathet Cardiovasc Diagn 1987;13:309–312. [DOI] [PubMed] [Google Scholar]
- 8. Ghosh PK, Alber G, Schistek R, Unger F. Rupture of guide wire during percutaneous transluminal coronary angioplasty. Mechanics and management. J Thorac Cardiovasc Surg 1989;97:467–469. [PubMed] [Google Scholar]
- 9. Khonsari S, Livermore J, Mahrer P, Magnusson P. Fracture and dislodgment of floppy guidewire during percutaneous transluminal coronary angioplasty. Am J Cardiol 1986;58:855–856. [DOI] [PubMed] [Google Scholar]
- 10. Al-Moghairi AM, Al-Amri HS. Management of retained intervention guide-wire: a literature review. Curr Cardiol Rev 2013;9:260–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Karan A, Omar M, Velarde G, Sattiraju S. An unusual case of an incidentally detected angioplasty wire in the aorta. AIM Clinical Cases 2022;1:e220047. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.