Abstract
Hypervirulent variants of foot-and-mouth disease virus (FMDV) of serotype C arise upon serial cytolytic or persistent infections in cell culture. A specific mutation in the internal ribosome entry site of persistent FMDV was previously associated with enhanced translation initiation activity that could contribute to the hypervirulent phenotype for BHK-21 cells. Here we report that several hypervirulent FMDV variants arising upon serial cytolytic passage show an invariant internal ribosome entry site but have a number of mutations affecting structural and nonstructural viral proteins. The construction of chimeric type O-type C infectious transcripts has allowed the mapping of a major determinant of hypervirulence to the viral capsid. Tissue culture-adapted FMDV displayed enhanced affinity for heparin, but binding to cell surface heparan sulfate moieties was not required for expression of the hypervirulent phenotype in Chinese hamster ovary (CHO) cells. Virulence was identical or even higher for glycosaminoglycan-deficient CHO cells than for wild-type CHO cells. FMDV variants with decreased affinity for heparin were selected from a high-binding parental population and analyzed. Substitutions associated with decreased heparin binding were located at positions 173 of capsid protein VP3 and 144 of capsid protein VP1. These substitutions had a moderate effect on virulence for BHK-21 cells but completely abrogated infection of CHO cells. The comparative results with several FMDV isolates show that (i) increased affinity for heparin and alterations in cell tropism may be mediated by a number of independent sites on the viral capsid and (ii) the same capsid modifications may have different effects on different cell types.
RNA viruses replicate as mutant swarms termed viral quasispecies (16, 18, 30). The continuous generation of mutants provides the basis for fitness gain and adaptation to changing environments (14, 15, 19, 30). In a constant biological environment such as that provided by a clonal cell population grown under defined culture conditions, competitive selection of viral mutants leads to replicative optimization of the viral quasispecies (4, 36, 46, 47). Work with foot-and-mouth disease virus (FMDV), an important animal pathogen of the Picornaviridae family, has documented the emergence of variants which are hypervirulent for BHK-21 cells. Such variants became dominant in the course of persistent infections (7–9, 39) and also during serial cytolytic infections (3, 37, 54). The hypervirulent FMDV variants displayed a shorter replication cycle in BHK-21 cells and an enhanced ability to kill cells compared with the parental viral clone (54).
The genetic alterations associated with the increase of FMDV virulence during persistent and cytolytic viral passages in BHK-21 cells are largely unknown. A pyrimidine transition was identified at the base of stem 3 of the internal ribosome entry site of the hypervirulent FMDV R100, a virus rescued after 100 passages of carrier BHK-21 cells persistently infected with FMDV clone C-S8c1 (9, 21). This mutation caused a 1.5- to 5-fold increase in translation efficiency as measured with bicistronic mRNA constructs in transfected cells (38). It was previously proposed that such a mutation could contribute to the increased virulence of FMDV R100 (38). The length of the poly(C) tract located within the 5′ nontranslated region of the FMDV genome has also been suggested to be a possible virulence determinant (5, 25). However, we have not been able to establish any correlation between the size of the poly(C) tract of FMDV of serotype C and virulence for BHK-21 cells (21, 54).
Amino acid substitutions accumulate in the capsid of FMDV during persistent infections in vivo (5, 24, 53) and upon persistent and cytolytic passages in cell culture (8, 9, 29, 37, 54). In the passages in cell culture, most of the replacements affected sites exposed on the particle surface and resulted in antigenic variation of FMDV in the absence of antibody pressure (2, 10, 13, 55). It was suggested that such substitutions may occur at sites where they are tolerated and that they may be of a neutral character with few phenotypic consequences (13). However, heparan sulfate (HS) has recently been recognized as a cell attachment molecule for FMDV (31). Sa-Carvalho et al. (51) have reported that tissue culture adaptation of FMDV of serotype O selects for variant viruses with positively charged residues situated at antigenically relevant positions on capsid proteins VP3 and VP2. These substitutions result in enhanced binding to HS and in attenuation of the virulence of the virus for cattle (51). In this view, integrins, in particular integrin αvβ3, would be a major receptor group for FMDV (1, 23, 26, 32), but adaptation to cell culture would enhance the affinity of the virus for HS (31, 51).
In the present study, we document that several amino acid substitutions are fixed around the G-H loop of capsid protein VP1 of FMDV clone C-S8c1 in the course of cytolytic infections. Such substitutions enhance the binding of the virus to heparin and contribute to increased virulence for BHK-21 cells and to altered cell tropism. FMDV mutants selected for their inability to bind heparin showed a strong reduction in virulence for some cell types but not others.
MATERIALS AND METHODS
Cells, viruses, cDNA, and plasmids.
The origin of the BHK-21 cells, procedures for infections of cell monolayers, and plaque assays with FMDV have been described previously (12, 56). Wild-type Chinese hamster ovary (CHO) cells and the two glycosaminoglycan-deficient CHO mutants pgsD-677 (N-acetylglucosaminyl and glucuronosyltransferase deficient) and pgsA-745 (xylosyltransferase deficient) were kindly provided by J. D. Esko (22, 34). Mutant pgsD-677 cells produce no detectable HS but threefold more chondroitin sulfate than the wild-type cells do. pgsA-745 mutant cells produce about 1% of the amount of glycosaminoglycan expressed by wild-type cells. CHO cells were grown in Dulbecco’s modified Eagle’s medium (DMEM) (Gibco) supplemented with nonessential amino acids (Gibco) and 5% fetal calf serum (Gibco). For treatment with heparinase I and III, CHO cells were grown in Ham’s F-12 medium (Gibco) supplemented with 10% fetal calf serum.
FMDV C-S8c1 is a plaque-purified derivative of the European serotype C natural isolate C1 Santa Pau-Spain 70 (56). FMDV C-S8c1 was used both to establish a persistent infection in cell culture (7) and to initiate 213 serial cytolytic infections in BHK-21 cells at a multiplicity of infection of 1 to 2 PFU per cell (3). The FMDV population at passage 213 was used to select MARLS, a monoclonal antibody (MAb)-resistant mutant selected with MAb SD6, which includes an L-144 → S substitution in VP1 (44). FMDV C-S8c1p100c1 and C-S8c1p100c10 are two plaque-purified clones derived from FMDV C-S8c1p100 described by Martínez et al. (37). FMDV C-S8c1p100RGG is a C-S8c1p100-derived MAR mutant with a D-143 → G substitution at the integrin recognition Arg-Gly-Asp motif (37). FMDV R100 is a virus rescued after 100 passages of carrier BHK-21 cells persistently infected with FMDV C-S8c1 (9, 21). The proportion of MAR mutants selected with MAb SD6 was 4 × 10−3 in the FMDV C-S8c1 p100 population and 2 × 10−3 in the R100 population (37).
Plasmid pFMDV-YEP-poly(C) containing the cDNA of FMDV strain O1K under the control of the bacteriophage SP6 promoter was constructed by Zibert et al. (60). Plasmid pO1KΔ3242 is a derivative of pFMDV-YEP-poly(C). For its construction, the 3,242-bp NgoMI fragment (FMDV O1K cDNA residues 1102 to 4344) was deleted from pFMDV-YEP-poly(C) and the NgoMI restriction site present in the vector sequence was removed by partial digestion and treatment with mung bean nuclease (New England Biolabs). Plasmid p3,242/O1K was constructed by subcloning the 3,242-bp NgoMI fragment of pFMDV-YEP-poly(C) into the NgoMI site of a pGEM-5Zf(+) derivative (vector position 2695). The pGEM-5Zf(+) vector (Promega) was modified by deleting the NcoI restriction site present in the polylinker: the vector was digested with NcoI (vector position 37) and NotI (vector position 62), treated with mung bean nuclease, and religated.
Single-step growth curves.
Confluent BHK-21 cell monolayers (2 × 106 cells) were inoculated with FMDV at a multiplicity of infection of 5 PFU/cell. After a 1-h absorption period at 37°C, the monolayers were extensively washed, overlaid with 1 ml of culture medium, and further incubated at the same temperature. At different times after infection, samples were taken for determination of infectivity (56).
Tissue culture virulence assay.
Virulence for BHK-21 cells was measured by determining the minimum number of PFU required to kill 104 BHK-21 cells in 24 h (54). For CHO cells, the time of infection was extended to 72 h.
cDNA synthesis, PCR amplification, and nucleotide sequencing.
Viral RNA extraction, cDNA synthesis, and reverse transcription-PCR amplification were performed as previously described (20). Briefly, the supernatant of infected cell monolayers (200 μl) was treated with 1 μg of proteinase K per μl in the presence of 1% sodium dodecyl sulfate for 20 min at 37°C and 10 min at 45°C. Following three phenol extractions, the RNA was recovered by two ethanol precipitations. The oligonucleotides used for FMDV retrotranscription and amplification are described in Table 1. PCR products were purified with the Wizard PCR Preps DNA purification system (Promega).
TABLE 1.
Synthetic oligonucleotides used for retrotranscription and amplification of FMDV genomes
| Fragmenta | Oligonucleotide sequence (5′ to 3′) | Orientation |
|---|---|---|
| F1 (1–367) | TTGAAAGGGGGCGCTAGGGTC | Sense |
| GTTAACTGAAAGGCGGGTTTCGGGTG | Antisense | |
| F2 (368–973) | TAAGTTTTACCGTCTGTCCCG | Sense |
| AAACCGAGCGCTTTTATAG | Antisense | |
| F3 (569–1643) | CACGATCTAAGCAGGTTTCC | Sense |
| CCCTTGAGCTTTCGCT | Antisense | |
| F4 (1002–4189) | CGGAGGTCGGCACCTTTCCTTTAC | Sense |
| CAAACGTGCTGTCCAGAATCTC | Antisense | |
| F5 (3988–5699) | TTGGTGTCTGCTTTTGAGGAAC | Sense |
| GCCTTCTGACCTGGAAGAGTTC | Antisense | |
| F6 (5344–7156) | AAAGGCCAACACGAGGCAGC | Sense |
| CGTCGACAATGCGAGTCTTGCCG | Antisense | |
| F7 (6610–8115) | GGGTTGATCGTTGATACCAGAGA | Sense |
| GGATTAAGGAAGCCGGGAAAGCCC | Antisense | |
| C1 (3573–4189) | ACACCGTGTGTTGGCTACGGCG | Sense |
| CAAACGTGCTGTCCAGAATCTC | Antisense | |
| C2 (2817–4189) | CTTGGCCGGTTTGGCCCAGTAC | Sense |
| CAAACGTGCTGTCCAGAATCTC | Antisense | |
| C3 (1009–3534) | CGGCACCTTTCCTTTTATAACC | Sense |
| CTTGTGGTAGGCAGTGGGATTGGTT GTGTTGTTAAGTG | Antisense |
Amplified fragments of FMDV serotype C and chimeric type O-type C genomes are designated by F and C, respectively; numbers in parentheses indicate the oligonucleotide positions in the C-S8c1 genome, numbered as described in Materials and Methods (20).
Consensus nucleotide sequences were determined on PCR-amplified DNA with either the Thermo Sequenase cycle sequencing kit (Amersham) or the fmol method (Promega) followed by terminal deoxynucleotidyltransferase treatment (6). The oligonucleotides used for nucleotide sequencing are described in Table 2.
TABLE 2.
Synthetic oligonucleotides used for nucleotide sequence determination of FMDV genomes
| Oligonucleotide sequence (5′ to 3′) | Positiona | Orientation |
|---|---|---|
| TTGAAAGGGGGCGCTAGGGTC | 1 | Sense |
| CAGCGCTAACAACCAAGTAG | 236 | Antisense |
| GTTAACTGAAAGGCGGGTTTCGGGTG | 367 | Antisense |
| TAAGTTTTACCGTCTGTCCCG | 368 | Sense |
| CACGATCTAAGCAGGTTTCC | 569 | Sense |
| TGTCAGTTGGGGAAACCTGC | 599 | Antisense |
| CTTGGTAACAAGGACCCAC | 750 | Sense |
| CGGAGGTCGGCACCTTTCCTTTAC | 1002 | Sense |
| GCCTTCCACCCTTCATTGAGTGGC | 1619 | Antisense |
| AACCAGTCGTTGGTCTGG | 1844 | Antisense |
| CAACCTTGTGCATGTGTCC | 2140 | Antisense |
| GGGTTGATGAACTGGTGGGG | 2345 | Antisense |
| CAGTTGTCACCATGTTGCC | 2602 | Antisense |
| CTTGGCCGGTTTGGCCCAGTAC | 2817 | Sense |
| GTACTGTGTGTAGTACTGCGC | 2850 | Antisense |
| GTTTCAGCCTCGTGGGACGC | 3077 | Antisense |
| CTTGTGGTAGGCAGTGGGATTGG TTGTGTTGTTAAGTG | 3534 | Antisense |
| ACACCGTGTGTTGGCTACGGCG | 3573 | Sense |
| CTGCACCAAAGTTGAACGAT | 3697 | Antisense |
| GAGAAGAAGAAGGGCCCAGGGTT GGACT | 3896 | Antisense |
| CAAACGTGCTGTCCAGAATCTC | 4189 | Antisense |
| GAAGACCTTGAGAGAGCAGAG | 4338 | Sense |
| CTCTTCTGAGGCGATCCATGC | 4158 | Antisense |
| CGCTCACGTCGATGTCAAAGTG | 5047 | Antisense |
| AAAGGCCAACACGAGGCAGC | 5363 | Sense |
| GAGTCGTGTACCATGCCCTC | 5396 | Antisense |
| GAACTCTTCCAGGTCAGAAGGC | 5677 | Sense |
| GTAAGTGGTGCCCCACCGACCGAC | 5971 | Sense |
| CATGACCATCTTTTGCAGGTCAG | 6009 | Antisense |
| CCCCCGTCGTTGGCGTGATTAAC | 6308 | Sense |
| GGGTTGATCGTTGATACCAGAGA | 6610 | Sense |
| ACCACTGCAGCGATGCCATGAAC | 7349 | Sense |
| GGCATCGCTGCAGTGGTTTGC | 7365 | Antisense |
| CTTGCCACCACGATGTCGTC | 7640 | Antisense |
| GGATTAAGGAAGCCGGGAAAGCCC | 8115 | Antisense |
Positions refer to the C-S8c1 genomic residues, numbered as described in Materials and Methods (20).
Construction of full-length cDNAs of FMDV O1K encoding type C capsid proteins.
FMDV C-S8c1 and MARLS genomic residues are numbered from the 5′ end, ignoring the poly(C) tract because of its variable length (3, 21). With this numbering, the adenosine residue of the first functional AUG initiation codon is at nucleotide 1039; the capsid-coding region spans nucleotides 1642 to 3834. Amino acid residues have been numbered independently for each protein. cDNA fragments encoding FMDV type C capsid proteins were obtained by reverse transcription-PCR amplification of viral RNA with oligonucleotides described in Table 1 (fragment F4). To perform mutagenesis, a KpnI-Hind III cDNA fragment (FMDV genomic positions 1388 and 4066) was cloned in the pALTER-1 vector (Promega).
Full-length cDNAs were constructed in two steps. First, the NcoI-HindIII fragment encoding C-S8c1 or MARLS capsid proteins (FMDV genomic positions 1739 and 4066) was substituted for the corresponding type O1K sequence in plasmid p3242/O1K. Second, full-length chimeric cDNAs, named pO1K/C-S8c1 and pO1K/MARLS, were produced by inserting the NgoMI fragment of the corresponding derivatives of p3242/O1K in the NgoMI site of plasmid pO1KΔ3242. The region transferred to the O1K genetic background spans Ser-33 of VP4 to Lys-62 of protein 2B. Since the amino acid sequence of capsid protein VP4 is conserved between FMDV serotypes O and C, chimeric constructions encode capsid proteins VP1 to VP4 and protease 2A of serotype C. Protein 2B is predicted to be a chimeric translation product containing the amino-terminal region of the serotype C protein and the carboxy-terminal region of the O1K protein.
To facilitate the construction of pO1K/C-S8c1, a silent mutation, C-2826 to T, was introduced by mutagenesis in the C-S8c1 cDNA to eliminate a NgoMI restriction site. This silent mutation was present in the FMDV MARLS genome (see Results). The amino acid substitution Thr-52 → Ala identified in MARLS protein 2B was reverted for the construction of pO1K/MARLS. To this aim, the BstXI-ClaI fragment of the C-S8c1 pALTER-derived construct (spanning FMDV genomic residues 3924 to 4066, followed by vector residues 56 to 479) was substituted for the corresponding fragment of the MARLS pALTER-derived construct. Nucleotide sequence analysis of the plasmidic constructions revealed the presence of a C-2363 → T mutation in the FMDV MARLS cDNA clone compared to the MARLS virus consensus sequence. This mutation predicts an Ala-156 → Val substitution in capsid protein VP2. Mutation T-2363 was reverted for the construction of pO1K/MARLS. To this end, the NcoI-SfiI fragment (FMDV genomic positions 1739 to 2827), generated by restriction of PCR-amplified cDNA of FMDV MARLS (Table 1, fragment F4), was substituted for the corresponding fragment of the p3242/O1K-derived preparation. The resulting plasmid pO1K/MARLS includes a capsid-coding region identical to the consensus sequence of FMDV MARLS. The construction containing the T-2363 mutation was named pO1K/MARLST2363.
Mutagenesis.
Site-directed mutagenesis was carried out with the Altered Sites in vitro mutagenesis system kit (Promega) as specified by the manufacturer. The single-stranded DNA template used in the mutagenesis reaction was obtained from Escherichia coli DH5αF′ cultures harboring the pALTER-derived construct. The sequence of the mutagenic oligonucleotide used was 5′-CTTGGCCGGTTTGGCCCAGTAC-3′ (the mutated nucleotide is underlined).
In vitro transcription and cell transfection.
Plasmid constructions were linearized by digestion with HpaI. Transcription was performed in 40 mM HEPES-KOH (pH 7.7)–6 mM magnesium acetate–20 mM spermidine–1 mM each nucleoside triphosphate–10 mM dithiothreitol–0.1 mg of bovine serum albumin per ml in the presence of 2 U of RNasin (Promega) per μl, 1 U of SP6 RNA polymerase (Promega) per μl, and 5 to 50 ng of linearized plasmid per μl. The RNA concentration was estimated by agarose gel electrophoresis and ethidium bromide staining. BHK-21 cell monolayers at about 75% confluency were transfected with 0.1 to 1 μg of RNA by using Lipofectin (38).
Heparin-Sepharose binding assay and selection of FMDV variants with decreased affinity for heparin.
Heparin-Sepharose CL-6B and control Sepharose CL-6B beads (Pharmacia Biotech; ligand density, ∼2 mg of porcine heparin/ml of drained gel) were resuspended as a 10% (wt/vol) slurry in phosphate-buffered saline (PBS) containing 0.1% azide. A 500-μl volume of the viral suspension diluted in DMEM to a final concentration of 0.2% fetal calf serum was incubated with the equivalent of 200 μl of beads previously washed with DMEM. The virus was allowed to bind for 1 h at room temperature with gentle rocking, and then the titer of unbound virus was determined by a plaque assay. Binding of serial dilutions of FMDV was analyzed to ensure that saturation of heparin binding sites was not reached. FMDV variants with decreased affinity for heparin were selected by using serial rounds of binding to heparin-Sepharose CL-6B beads. Viral particles remaining in the supernatant of the viral suspension after three rounds of incubation (30 min each) in the presence of 100 μl of heparin-Sepharose beads were amplified in BHK-21 cells. Rounds of selection-amplification were repeated 10 times until variants with undetectable affinity for heparin were obtained (Fig. 1).
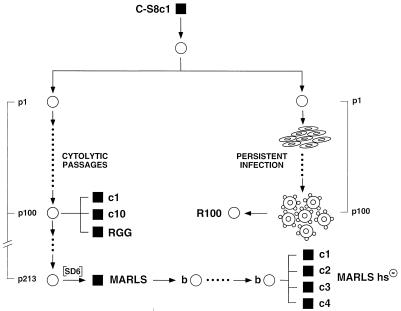
FIG. 1.
Passage history of serotype C FMDV variants analyzed in this study. Plaque-purified FMDV C-S8c1 (▪) passaged once cytolytically in BHK-21 cells (○) was further propagated in BHK-21 cells either in cytolytic or in persistent infections. C-S8c1-derived populations p100 and p213 were obtained after 100 and 213 serial cytolytic passages, respectively. Clones c1 and c10 were isolated from C-S8c1 p100 (37). RGG and MARLS are two mutants resistant to MAb SD6 (3, 37). FMDV MARLS was subjected to 10 rounds of selection and amplification (b○) with heparin-Sepharose binding and infection of BHK-21 cells, to eliminate viruses with high affinity for heparin. This led to the isolation of clones MARLS/hs− c1, c2, c3, and c4 (bottom right). Procedures for cytolytic infections and isolation of virus from single plaques are described in Materials and Methods. Persistent FMDV infections and the R100 population were described previously (8, 9, 21).
Heparinase treatment.
CHO cells were detached from their culture surface with PBS containing 0.5 mM EDTA, centrifuged, washed with PBS, and resuspended in PBSB (PBS, 0.1% bovine serum albumin) to a final concentration of 106 cells/ml. A mixture of 1 U of heparinase I (EC 4.2.2.7) and 0.5 U of heparinase III (EC 4.2.2.8) (Sigma) was added to 105 cells and incubated at 35°C for 1 h. Enzyme-treated cells were washed with PBSB and resuspended in 100 μl of PBSB containing 0.5 mM MgCl2 and 1 mM CaCl2. Virus was added to the cells, and the mixture was incubated for 30 min at 37°C in the presence of fresh heparinase I and III. Extracellular virus was neutralized with 0.1 M phosphate buffer (pH 6.0), and the cells were resuspended in DMEM containing 2% fetal calf serum. The sensitivity of treated and untreated cells to virus infection was estimated (i) as the minimum number of infected cells required to kill 104 wild-type CHO cells in 72 h (cell-killing assay) and (ii) by plaque formation on a wild-type CHO cell monolayer (plating assay).
Molecular modeling.
The crystallographic coordinates of FMDV C-S8c1 (33) have been used as starting model. The conformation of the G-H loop of VP1 and its position in the viral capsid has been taken from the structure of the complex with MAb SD6 (27, 57). The substitutions found in the capsid of variant FMDVs have been modeled with the program TURBO (49) by placing the side chain atoms of the substituted amino acids in their standard conformations. The structure was then optimized by removing the close contacts with the same program.
RESULTS
Multiply passaged FMDV MARLS displays hypervirulence for BHK-21 cells.
Prolonged serial cytolytic passage of FMDV C-S8c1 in BHK-21 cells resulted in selection of hypervirulent variants together with defective FMDV genomes lacking part of the leader (L) protease gene (3). A MAb-resistant mutant isolated from passage 213 (MARLS) (Fig. 1) was compared with the parental C-S8c1 virus with regard to replication kinetics (Fig. 2A) and virulence for BHK-21 cells (Table 3). In the standard infection protocol, complete cytopathic effect was observed 4 to 6 h after infection of BHK-21 cells with FMDV MARLS and 16 to 20 h after infection with C-S8c1. Also, the maximum virus titer observed was 10-fold higher for MARLS than for C-S8c1. These titers correspond to an average infectious-virus production of 200 and 20 PFU/cell, respectively. It is remarkable that the ability to kill BHK-21 cells in a standard virulence assay was about 103-fold greater for MARLS than for the parental FMDV C-S8c1 (Table 3).
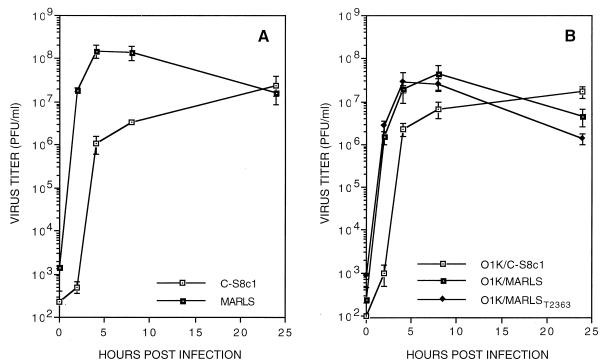
FIG. 2.
Comparison of the virus production upon infection of BHK-21 cell monolayers with (A) FMDV C-S8c1 and the MARLS variant (A) and chimeric FMDVs O1K/C-S8c1, O1K/MARLS, and O1K/MARLST2363, including the capsid of C-S8c1 or its hypervirulent derivatives (described in Materials and Methods) (B). In all cases, BHK-21 cells were infected at a multiplicity of infection of 5 PFU per cell. Virus titers at different times after infection were determined by plaque assays on BHK-21 cells monolayers (12). Each value represents the mean and standard deviation from triplicate assays.
TABLE 3.
Phenotypic traits of FMDV variants with different passage histories in BHK-21 cell cultures
| FMDV straina | Binding to heparinb | Virulence forc:
|
|||
|---|---|---|---|---|---|
| BHK-21 cells | CHO cells
|
||||
| Wild type | pgsA-745 | pgsD-677 | |||
| C-S8c1 | − | 105 | − | − | − |
| O1K | ++ | 103 | 104 | − | − |
| MARLS | +++ | 102 | 104 | 102 | 104 |
| MARLS/hs−c1 | − | 103 | − | − | − |
| MARLS/hs−c2 | − | 103 | − | − | − |
| MARLS/hs−c3 | − | 102 | − | − | − |
| MARLS/hs−c4 | − | 103 | − | − | − |
| O1K/C-S8c1 | − | 104 | − | − | − |
| O1K/MARLS | +++ | 102 | 102 | 10 | 102 |
| O1K/MARLST2363 | ++ | 102 | 103 | 10 | 102 |
| C-S8c1p100c1 | ++ | 102 | 105 | 103 | 105 |
| C-S8c1p100c10 | ++ | 102 | 105 | 103 | 105 |
| C-S8c1p100RGG | + | 103 | 105 | 104 | 105 |
| R100 | ++ | 103 | − | − | − |
The origin of each FMDV strain is shown in Fig. 1 and is described in Materials and Methods. FMDV C-S8c1p100c1 and C-S8c1p100c10 are two plaque-purified clones derived from C-S8c1 after 100 serial passages in BHK-21 cells; C-S8c1p100RGG is a C-S8c1p100-derived MAR mutant with a substitution at the Arg-Gly-Asp motif; FMDV R100 was rescued after 100 passages of carrier BHK-21 cells persistently infected with C-S8c1. FMDV O1K was obtained by transfection of BHK-21 cells with infectious O1K transcripts derived from plasmid pFMDV-YEP-poly(C) (60). FMDV O1K used was at passage 1.
Binding to heparin was estimated as the ratio of PFU remaining in the supernatant of a viral suspension after incubation with control beads (without heparin) relative to heparin-Sepharose beads. Binding was classified as follows: +, 2 < ratio < 50, where 2 is the limit of positive detection; ++, 50 ≤ ratio < 5 × 102; +++, 5 × 102 ≤ ratio < 5 × 103; −, no detectable binding (ratio, ∼1). Further details on heparin binding assays are given in Materials and Methods.
Minimum number of PFU required for complete cell killing of 104 BHK-21 cells in 24 h or 104 CHO cells in 72 h. Thus, a large number corresponds to low virulence; −, no cytopathic effect in the presence of the following PFU for the different FMDVs: 1 × 106 (C-S8c1), 2 × 105 (O1K), 7 × 106 (MARLS/hs− c1 to c4), 2 × 106 (O1K/C-S8c1), 6 × 105 (R100). Each value represents the average of triplicate determinations.
Analysis of the MARLS virus genome.
The nucleotide sequence of the entire MARLS genome was compared with that of C-S8c1 (Table 4). Interestingly, mutations at the 5′ nontranslated region were located outside the internal ribosome entry site element, indicating that the hypervirulence phenotype of FMDV does not require substitutions at this regulatory domain. The amino acid substitutions at the nonstructural proteins 2C, 3C, and 3D affected regions which are considerably variable when different picornaviruses are compared (61; current alignments in GenBank). Only the Glu-165 → Gly substitution in the L protease affected a position which is conserved among the sequenced FMDVs of serotypes A, C, O, and SAT-2 (50). Amino acids substituted in the capsid were located at exposed sites, as defined by accessibility to a probe with a radius of 2 Å (33, 43). Antigenic site A was affected by the VP1 Leu-144 → Ser replacement (the substitution responsible of the MAR phenotype), and the His-197 → Arg and Pro-200 → Gln substitutions were located in antigenic site C (33, 41) (Table 4).
TABLE 4.
Mutations and corresponding amino acid substitutions found in the FMDV MARLS genome as compared to FMDV C-S8c1
| Genomic region | Mutationa | Amino acid substitutionb | Secondary structurec |
|---|---|---|---|
| 5′ nontranslated region | C-247 → T | NCR | |
| C-338 → T | NCR | ||
| G-476 → A | NCR | ||
| T-518 → C | NCR | ||
| L protease | G-1091 → T | Arg-18 → Ile | |
| C-1105 → T | Pro-23 → Ser | ||
| A-1532 → G | Glu-165 → Gly | ||
| VP2 | G-2285 → A | Gly-130 → Asp | E-F loop |
| VP3 | T-2622 → C | − | |
| C-2624 → T | Ala-25 → Val | N terminus | |
| C-2826 → T | − | ||
| G-3067 → A | Glu-173 → Lys | G-H loop | |
| T-3082 → A | Cys-178 → Ser | G-H loop | |
| C-3202 → A | Gln-218 → Lys | C terminus | |
| VP1 | A-3328 → G | Lys-41 → Glu | βB strand |
| C-3423 → T | − | ||
| T-3638 → C | Leu-144 → Ser | G-H loop, antigenic site A | |
| A-3797 → G | His-197 → Arg | C terminus, antigenic site C | |
| C-3806 → A | Pro-200 → Gln | C terminus, antigenic site C | |
| 2B | A-4036 → G | Thr-52 → Ala | |
| 2C | G-4583 → A | Ser-80 → Asn | |
| A-5110 → G | Thr-256 → Ala | ||
| G-5133 → C | Gln-263 → His | ||
| A-5191 → G | Met-283 → Val | ||
| 3A | A-5364 → C | − | |
| 3C | T-6225 → C | − | |
| A-6295 → C | Met-109 → Leu | ||
| 3D | T-6744 → C | − | |
| A-7305 → C | Gln-232 → His | ||
| G-7554 → T | − | ||
| T-7564 → C | − | ||
| T-7932 → C | − |
Procedures for sequencing the entire FMDV genome are described in Materials and Methods. The first letter corresponds to the nucleotide found in the parental FMDV C-S8c1, and the number gives the nucleotide position in the C-S8c1 genome, according to reference 20. Mutation T-3638 → C (Leu-144 → Ser) is responsible for resistance to neutralization by MAb SD6 (37). Except for this mutation, the capsid coding sequence of C-S8c1 p213 is indistinguishable from that of MARLS.
The first amino acid is the one found in C-S8c1; amino acid residues are numbered independently for each protein. NCR, noncoding region; −, silent mutation.
RNAs derived from chimeric O1K full-length cDNAs encoding type C capsid proteins are infectious.
To investigate whether the capsid of FMDV could influence its virulence for BHK-21 cells, it was important to transfer the capsid-coding regions of C-S8c1 and MARLS into the same viral genetic background. Entire infectious cDNA clones of FMDV serotype C have not been described. In contrast, complete infectious cDNA clones have been obtained for serotypes O1K and A12 (48, 60). Therefore, to analyze the possible implication of type C structural proteins in hypervirulence for BHK-21 cells, chimeric type O-type C FMDVs including the capsid of serotype C were constructed. The capsid-coding regions located between the NcoI (position 1739) and HindIII (position 4066) restriction sites of FMDV C-S8c1 and MARLS cDNAs were substituted for the corresponding sequence in the type O1K full-length cDNA (60), as detailed in Materials and Methods (Fig. 3). BHK-21 cells were transfected with the transcription products of each of the chimeric cDNAs (Fig. 3). RNA derived from the FMDV O1K cDNA clone [pFMDV-YEP-poly(C)] was used as a control. A complete cytopathic effect was observed at 20 to 24 h posttransfection in BHK-21 monolayers transfected with RNA transcripts from pO1K/MARLS or pO1K/MARLST2363. Viral titers in the supernatant of transfected cells ranged from 2 × 107 to 4 × 107 PFU/ml. In contrast, transcripts from pO1K/C-S8c1 or pFMDV-YEP-poly(C) resulted in cytopathologic changes at about 48 h posttransfection. Viral titers ranged from 3 × 105 to 4 × 106 PFU/ml. No cytopathic effect was observed in parallel transfections carried out in the absence of RNA. The chimeric virus progeny was neutralized by serotype C-specific MAbs directed to antigenic site D (33).
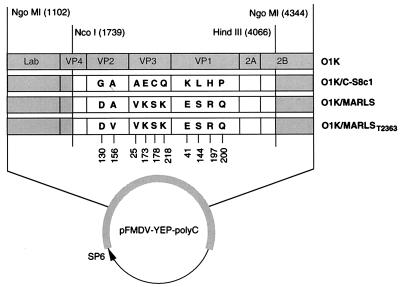
FIG. 3.
Schematic representation of the capsid coding region of FMDV O1K and of C-S8c1 and its variant derivatives, as inserted in the parental type O1 plasmid pFMDV-YEP-poly(C) (60). Type C genomic regions are represented by open boxes. NgoMI restriction sites and their numbering refer to FMDV O1K cDNA (60). NcoI and Hind III sites and their numbering refer to the C-S8c1 genome (20). Amino acid residues differing in the compared chimeric genomes are indicated. The vertical numbers at the bottom refer to the corresponding positions in each protein. Infectious transcripts were produced with plasmid pFMDV-YEP-poly(C), and derived constructs encoding the cDNA of FMDV O1K or type O-type C chimeras under the control of the SP6 promoter. The amino acid sequence of protein VP4 is conserved among the FMDVs of serotypes O and C analyzed here. Procedures for the construction of chimeric viruses and confirmatory sequence analysis of chimeric progeny are described in Materials and Methods. O1K/MARLS includes a capsid-coding region identical to the consensus sequence of FMDV MARLS. T-2363 indicates an Ala-156 → Val mutation in protein VP2 that was accidentally selected during the cloning procedure. Infectious transcripts were produced with plasmid pFMDV-YEP-poly(C) and derived constructs encoding the cDNA of FMDV O1K or type O-type C chimeras under the control of the SP6 promoter. The amino acid sequence of protein VP4 is conserved among the FMDVs of serotypes O and C analyzed here. Procedures for the construction of chimeric viruses and confirmatory sequence analysis of chimeric progeny are described in Materials and Methods.
RNA from chimeric viruses resulting from one round of replication after transfection were copied into cDNA and amplified by PCR, and the regions encoding the capsid proteins and neighboring viral products were sequenced. Nucleotide sequences diagnostic of serotype O FMDV were found at the regions around those encoding the capsid. Apart from the silent mutation T-2826 introduced by mutagenesis (see Materials and Methods), the nucleotide sequence encoding the capsid proteins of the O1K/C-S8c1 chimera was identical to the corresponding sequence of C-S8c1. Mutations present in the capsid-coding regions of MARLS were found in the viral progeny derived from the O1K/MARLS and O1K/MARLST2363 chimeras. As expected, the O1K/MARLST2363 genome included a thymidine residue at position 2363. The virus production of the chimeric O1K/MARLS viruses was about 10-fold lower than that of the authentic MARLS. The times at which maximum cytopathic effect and maximum virus titers were reached were shorter for the MARLS-containing than for the C-S8c1-capsid containing chimeras (Fig. 2B). The results indicate that type C structural proteins are expressed in a functional form in the genetic context of a serotype O FMDV and are able to encapsidate chimeric type O-type C FMDV genomes. The chimeric viruses manifest a different replication kinetics, which is dependent on the nature of the capsid-coding regions.
Phenotypic characterization of FMDV chimeric progeny and comparative analysis of additional mutant FMDVs.
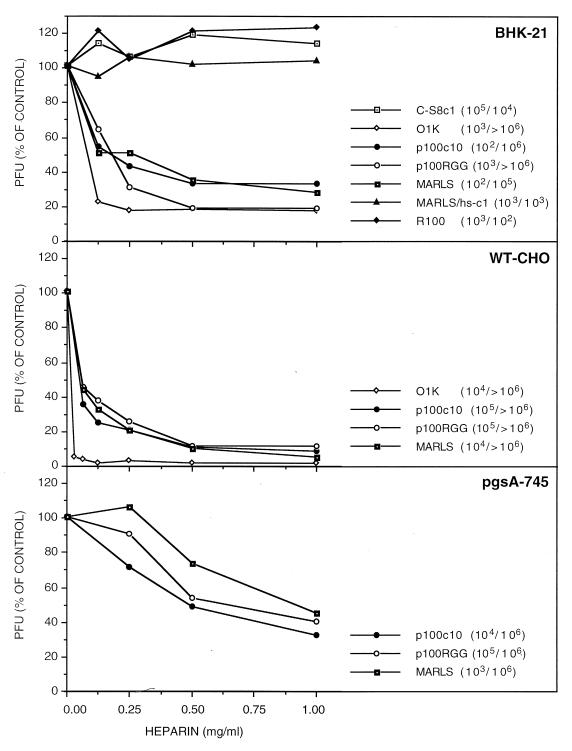
A number of mutants of FMDV with various amino acid substitutions in their capsid proteins have been isolated in our laboratory over the last decade (17, 37) (Fig. 1). They differ in the number of passages in BHK-21 cells and thus in the degree of adaptation to this cell line, as evidenced by an increase in relative fitness values with passage number (28, 36). Since it has been suggested that an increase in heparin binding may be associated with adaptation of FMDV of serotype O to cell culture (31, 51), it was of interest to analyze our collection of mutant FMDVs as well as the chimeric type O-type C viruses with regard to binding to heparin and its possible association with virulence for cells in culture. The results (Table 3) show that all variants derived from passage of C-S8c1 in BHK-21 cells displayed enhanced virulence for this cell line and acquired the ability to bind heparin, albeit to different extents. Likewise, the O1K/MARLS chimeras were also able to bind heparin, in contrast to FMDV C-S8c1 and to the O1K/C-S8c1 chimera (Table 3). The O1K/MARLS chimeras were 100-fold more virulent for BHK-21 cells than the O1K/C-S8c1 chimera, in agreement with the results of the single-step growth experiments (Fig. 2B) and reflecting the origin of the capsid proteins (Table 3). The conclusions were also supported by the results of heparin inhibition assays (Fig. 4). Both the infectivity and virulence for BHK-21 cells of FMDV O1K, p100c10, p100RGG, and MARLS, but not of C-S8c1 or MARLS/hs-c1, were reduced by soluble heparin (Fig. 4). Interestingly, the infectivity of R100 was not affected by heparin despite its positive heparin binding (compare Fig. 4 and Table 3).
FIG. 4.
The effect of soluble heparin on the infectivity of FMDV. Mixtures of the indicated FMDV (50 to 300 PFU) and the amount of heparin (Sigma; from bovine lung, sodium salt) were incubated in DMEM for 10 min at 25°C. Then the mixtures were applied to confluent monolayers of either BHK-21, wild-type CHO (WT-CHO), or pgsA-745 CHO cells. After an adsorption period of 1 h at 37°C, the monolayers were washed and overlaid with DMEM containing 1% fetal calf serum and 0.5% agar. Plaques were visualized by staining with crystal violet. Plaque formation by mutant p100RGG required the presence of DEAE-dextran (0.08 mg/ml) in the semisolid medium. Percent plaque reduction was calculated relative to parallel assays with each virus and cell type in the absence of heparin. In addition, virulence assays were performed, as described in Materials and Methods, in the absence or presence of heparin (1 mg/ml) in the virus to be tested. Virulence values are given in parentheses (absence or presence of heparin) and are defined as indicated in Materials and Methods. Some viruses were tested only in BHK-21 cells because they do not infect CHO cells under the assay conditions used (see the text and Table 3).
To further investigate the involvement of GAG in the acquisition of virulence in tissue culture, wild-type CHO cells and mutant CHO cell lines deficient in GAG biosynthesis (22, 34) (described in Materials and Methods) were tested in the virulence assay (Table 3). The chimeras containing the MARLS capsid were able to replicate in both wild-type CHO cells and GAG-deficient CHO cell lines pgsA-745 and pgsD-677. Replication of MARLS in CHO cells did not entail selection of a variant with substitutions in the capsid, as documented by sequencing of the capsid-coding region of progeny from an infection of wild-type CHO cells and mutant pgsA-745 cells with MARLS. The deduced amino acid sequences of the capsid proteins of the parental and progeny viruses were identical. The virulence of all these viruses for pgsA-745 cells was 10- to 100-fold higher than for wild-type and mutant pgsD-677 CHO cells (Table 3). In parallel assays, FMDV O1K was able to kill wild-type CHO cells but not mutant CHO cells, as previously described for other O1 isolates (31, 51) (Table 3). All FMDV C-S8c1p100-derived viruses (Fig. 1) (37) were able to infect wild-type and mutant CHO cells (Table 3). Only the FMDV mutant p100RGG showed a slightly diminished ability to bind heparin and a somewhat lower virulence for BHK-21 and pgsA-745 CHO cells (Table 3). Finally, the persistent FMDV R100 was also tested. This population acquired high virulence for BHK-21 cells as a result of coevolution with the host cells (8, 9, 52) (Fig. 1). Interestingly, R100 showed moderate heparin binding and was not capable of replicating in CHO cells (Table 3) (see Discussion). For viruses that infect wild-type CHO cells, heparin caused a strong inhibition of both infectivity and virulence (Fig. 4). The inhibition was 10- to 30-fold lower in parallel assays employing with pgsA-745 cells (Fig. 4).
To further document that HS is not required for infection of CHO cells by FMDV MARLS, wild-type and GAG-deficient CHO cells were treated with mixtures of heparinase I and III, as described in Materials and Methods. No reduction of the infectivity of MARLS was observed after heparinase treatment of pgsA-745 or pgsD-677 CHO cells; only a twofold reduction was measured upon heparinase treatment of wild-type CHO cells. In parallel treatments of wild-type CHO cells, a reduction of 5-fold (plating assay) and 25-fold (cell killing assay) in the infectivity and 25-fold in the virulence of FMDV O1K was observed. Furthermore, in contrast to the FMDVs of serotype C tested, plaque development of FMDV O1K on wild-type CHO cell monolayers in semisolid agar medium (12) was completely inhibited in the presence of DEAE-dextran (0.08 mg/ml).
These results suggest that the affinity for heparin is a phenotypic property of tissue culture-adapted FMDV of serotype C and that infection of CHO cells by FMDV MARLS and C-S8c1p100-derived viruses does not require the presence of cell surface HS moieties.
Selection and characterization of FMDV MARLS variants with decreased affinity for heparin.
Variants with decreased affinity for heparin were selected from the MARLS population by using heparin-Sepharose beads, as described in Materials and Methods. After 10 rounds of selection for negative binding, a total reversion of the heparin-binding phenotype was observed. Four FMDV clones were isolated from the subpopulation MARLS/hs−, which were unable to bind heparin (Fig. 1). The four individual clones (c1, c2, c3, and c4) did not show detectable binding to heparin (Table 3). In addition, heparin inhibition was tested with clone c1, with negative results, as expected (Fig. 4). Sequencing of the capsid-coding region revealed that clones c1, c2, c3, and c4 had the same two amino acid replacements on the capsid: Lys-173 → Met in VP3 and Ser-144 → Leu in VP1. The latter replacement represents the reversion of the substitution responsible for resistance to MAb SD6. The presence of an uncharged Met residue in position 173 of VP3 in MARLS/hs− and of Glu in the corresponding position of C-S8c1 suggests that the positively charged Lys-173 in VP3 is essential for binding to heparin and for infection of CHO cells (compare Tables 3 and 5). The results provide evidence that VP1 position 144 may also play a role in heparin binding and infectivity for CHO cells (see Discussion).
TABLE 5.
Amino acid substitutions found in capsid proteins of FMDV variants with different passage histories in BHK-21 cell culturesa
| Viral protein | Positionb | Amino acid in:
|
|||
|---|---|---|---|---|---|
| C-S8c1 | C-S8c1 p100c10 | MARLS | R100 | ||
| VP2 | 130 | Gly | −c | Asp | − |
| 192 | Ala | − | − | Thr | |
| 193 | Gly | − | − | Ser | |
| VP3 | 7 | Cys | − | − | Val |
| 9 | Asp | − | − | Ala | |
| 13 | Asn | − | − | His | |
| 14 | Met | − | − | Leu | |
| 25 | Ala | Val | Val | − | |
| 173 | Glu | Lys | Lys | − | |
| 178 | Cys | − | Ser | − | |
| 194 | Asp | − | − | − | |
| 218 | Gln | Lys | Lys | − | |
| VP1 | 41 | Lys | Glu | Glu | − |
| 46 | Asp | Glu | − | − | |
| 83 | Thr | − | − | Ala | |
| 144 | Leu | − | Ser | − | |
| 145 | Ala | − | − | − | |
| 148 | Thr | − | − | Lys | |
| 164 | Val | − | − | − | |
| 194 | Gly | − | − | Asp | |
| 197 | His | Arg | Arg | − | |
| 200 | Pro | − | Gln | − | |
All variant FMDVs compared are derived from clone C-S8c1, as depicted in Fig. 1 and as described in Materials and Methods.
Amino acid residues are numbered independently for each protein, and the positions refer to clone C-S8c1 (20). No mutations were found in the VP4 coding region.
−, no substitution found in the virus.
All MARLS/hs− clones tested lost the ability to infect CHO cells, and three of four clones displayed a virulence for BHK-21 cells which was 10-fold lower than that of MARLS but still 102-fold higher than that of the parental C-S8c1 (Table 3). This suggests that the BHK-21 cell-specific virulent phenotype displayed by FMDV MARLS does not have identical determinants to those of the virulent phenotype for CHO cells.
Location of the amino acid residues involved in heparin binding and cell tropism.
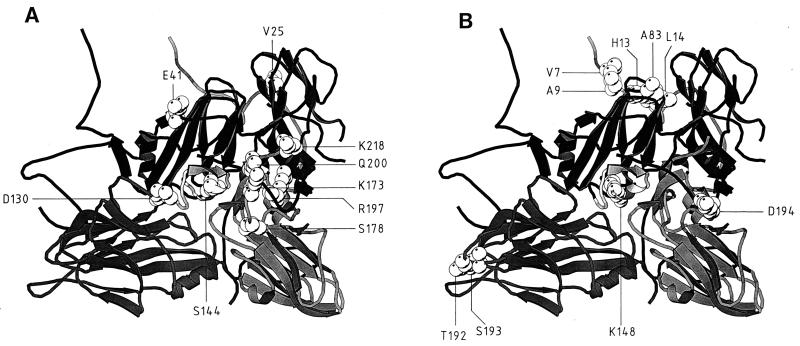
The atomic coordinates of FMDV C-S8c1 obtained by X-ray crystallography (33, 57) were used (i) to model the amino acid substitutions found in the capsid of FMDV MARLS and R100 on the capsid of C-S8c1 and (ii) to position the residues responsible for heparin binding on the three-dimensional structure of the virion (Fig. 5). With the exception of the VP1 residue Glu-46, all mutations fixed in the capsid of FMDV C-S8c1p100c10 upon serial passages in BHK-21 cells were maintained in the MARLS mutant (Table 5). Of the five conserved replacements, four mutations (Glu-173 → Lys and Gln-218 → Lys in VP3, Lys-41 → Glu and His-197 → Arg in VP1) were clustered around the position occupied by the G-H loop of VP1 (27, 37). In particular, a 4.7-Å minimal side chain-side chain distance was measured between residues R-141 (Nɛ) of the VP1 G-H loop and K-173 (Cδ) of VP3, which is involved in heparin binding and cell tropism modification. Additional amino acid substitutions found in the capsid of FMDV MARLS (VP2 Gly-130 → Asp, VP3 Cys-178 → Ser, and VP1 Pro-200 → Gln) (Table 5) also mapped close to the loop (Fig. 5). The SD6 MAR mutation Leu-144 → Ser is located at antigenic site A within G-H the loop of VP1 (Fig. 5).
FIG. 5.
Locations of the amino acid substitutions found in FMDV MARLS (A) and FMDV R100 (B) on a ribbon protein diagram of a crystallographic protomer of C-S8c1 (33). The capsid proteins VP1, VP2, and VP3 are represented as dark, medium, and light grey, respectively. VP1 from a neighboring protomer is shown at the upper right. The position of the G-H loop of VP1 in C-S8c1 corresponding to that found in the complex with MAb SD6 is shown in light grey at the center of each structure (27). The substituted residues are depicted in van der Waals spheres. The amino acids indicated are those listed in Table 5 for MARLS and R100. The minimal side chain-side chain distances measured between critical amino acid residues of MARLS and were 3.6 Å between VP2 D-130 (Cδ2) and VP1 A-145 (N), 4.5 Å between VP3 K-173 (Nζ) and VP1 Q-200 (Oɛ1), 4.7 Å between VP3 K-173 (Cδ) and VP1 R-141 (Nɛ), 5.1 Å between VP1 Q-200 (Cα) and VP1 R-141 (Cζ), 12.7 Å between VP1 R-197 (Cα) and VP1 R-141 (Nη2), and 15.0 Å between VP3 S-178 (Cβ) and VP1 P-156 (Cγ). The corresponding Cα-Cα distances were 6.8, 5.6, 9.5, 9.7, 17.9, and 16.5 Å, respectively. A minimal side chain distance of 13.3 Å was measured between R100 VP1 D-194 (Oδ2) and VP1 R-141 (Nη2). The corresponding Cα-Cα distance was 21.1 Å. The origin of the viruses and the procedures used to locate amino acids on the capsid structure are described in Materials and Methods.
Mutations found in the capsid of FMDV R100 differed drastically from those of FMDV MARLS and C-S8c1p100c10 (Table 5). Whereas capsid alterations accumulated around the VP1 G-H loop in the course of cytolytic infections, evolution in persistently infected carrier cells led to substitutions around the pore located at the fivefold axis of symmetry (Fig. 5). In addition, the Thr-148 → Lys and Gly-194 → Asp substitutions in VP1 and the Ala-192 → Thr and Gly-193 → Ser substitutions in VP2 are fixed in R100. The results suggest that multiple sites which are distant on the capsid of FMDV of serotype C can modulate the affinity of FMDV for heparin.
DISCUSSION
Viral quasispecies replicating under conditions which ensure competitive rating of genomes from the mutant spectra move toward high-fitness peaks (15). For viruses replicating in cell culture under a constant environment, an increased ability to kill cells and produce progeny will be strongly selected (54). This ability may be associated with optimization of any limiting step in the viral replication cycle: recognition of the cell receptor, virus entry, uncoating, expression of viral genes, genome replication, particle assembly, or release of virus particles from cells.
Cell receptor recognition is an essential step in any infection process, and it is currently recognized that many viruses are capable of using several cellular receptors and coreceptors. This may contribute to an expanded host range and to an increased probability of virus survival. For FMDV, integrins, in particular αvβ3, were the first receptors to be identified (1, 23, 32, 40). Recently, Jackson et al. (31) found that, in common with other natural ligands of some integrins, binding to the ubiquitous cell surface GAG was required for efficient infection of cultured cells by FMDV of serotype O. These results were confirmed and extended by Sa-Carvalho et al. (51) working with chimeric type A-type O FMDVs. Their results showed that tissue culture-adapted variants included positively charged residues exposed in capsid proteins VP2 and VP3 that mediated heparin binding and the ability to infect CHO cells. These observations revealed that entry of FMDV type O into cells is a complex process and that HS may mediate the first contact between the cell and the virus in tissue culture (31, 51).
In the present study, we have analyzed a collection of FMDV serotype C variants which were obtained as a result of either persistent or serial cytolytic infections of clone C-S8c1 (56) in BHK-21 cell cultures (Fig. 1). Our initial aim was to map the hypervirulent phenotype for BHK-21 cells, first described for persistent virus R100 (8, 9) and later found to be a trait also selected upon serial cytolytic passage of the same viral clone (3, 54). With the construction of chimeric type O-type C viruses (Fig. 3), it has been possible to assign major determinants of hypervirulence for BHK-21 cells to the viral capsid. Indeed, several chimeras including the capsid of the tissue culture-adapted MARLS variant were 102-fold more virulent for BHK-21 cells than were the same constructs including the capsid of the parental clone C-S8c1 (Fig. 2; Table 3).
The use of several FMDV mutants, all derived from clone C-S8c1 but with different, albeit controlled evolutionary histories (Fig. 1), has established that the increase in virulence for BHK-21 cells paralleled an enhanced ability to bind heparin. For all FMDV C-S8c1-derived variants selected upon cytolytic passages in BHK-21 cells (MARLS, chimeras with the MARLS capsid, and clones derived from C-S8c1 p100 [Table 3]), an enhanced affinity for heparin correlated with the inhibition of infectivity by soluble heparin and with the ability to infect CHO cells. However, in contrast to FMDV of serotype O, the presence of cell surface HS was dispensable for infection of CHO cells, since these tissue culture-adapted C-S8c1 variants replicate in CHO mutant derivatives pgsA-745 and pgsD-677, which are deficient in GAG biosynthesis (22, 34). In assays carried out in parallel with the same cells at the same passage number, wild-type CHO cells, but not the mutant cells pgsA-745 and pgsD-677, were infected with FMDV O1K, a result which agrees with the observations of Jackson et al. (31). The distinct levels of virulence displayed by FMDV in each cell line document that the virulence determinants for different cell lines in culture are not identical. Virulence levels may be influenced by a number of variables affecting the virus and the cells (growth rate, cell density at confluency, etc.).
The evolutionary history, which in this case is distinguished by adaptation of FMDV either to cytolytic infections or to persistent infections, influenced the host range of FMDV. The hypervirulent R100 FMDV mutant, rescued after prolonged persistence in BHK-21 cells, was unable to replicate in CHO cells despite its relative high affinity for heparin. Therefore, the acquisition of heparin-binding capacity does not entail an ability to infect CHO cells or to use HS as coreceptor. Studies are now in progress to identify the step in the replication cycle of FMDV R100 that is blocked in CHO cells. The results reported here suggest that adaptation of FMDV to cell culture involves multiple virulence determinants. The acquisition of elevated virulence during persistent infections clearly depends on mechanisms other than those operating during cytolytic passages.
Biological selection in vitro was exploited to identify the amino acid residues associated with binding of MARLS to heparin. Reversion of the heparin-binding phenotype of MARLS was accompanied by two substitutions, Lys-173 → Met in VP3 and Ser-144 → Leu in the G-H loop of VP1. Interestingly, these mutations abolished the replication of the virus in wild-type and mutant CHO cells. Lys-173 of VP3 was present in all FMDV variants with cytolytic passage histories in BHK-21 cell cultures, suggesting that this positively charged amino acid played a central role in the interaction of the virus with heparin. In contrast, the presence of the Ser-144 in VP1 was not required for binding to heparin. Positioning of the critical residues in the three-dimensional structure of C-S8c1 (33) indicated that Lys-173 of VP3 was one of a cluster of amino acid replacements surrounding the G-H loop of VP1 (Fig. 4). These replacements may also affect integrin recognition by FMDV, since viable mutants with substitutions within the RGD triplet were selected from C-S8c1 p100—a population which included the cluster of replacements on VP1 and VP3—but not from C-S8c1 (37). However, only Asp-130 of VP2, which is present in MARLS but not in C-S8c1p100 or C-S8c1p100c10 (Table 5), could potentially form a hydrogen bond with the main chain of Ala-145 in VP1, assuming that the position of the G-H loop of VP1 is that recently defined in a complex with MAb SD6 (27). The distances measured between the sites of other capsid replacements and the G-H loop of VP1 preclude a direct interaction between the relevant residues. The ability to infect CHO cells may therefore be the result of an interaction of the VP3 Lys-173 and other residues surrounding the G-H loop with structures (heparin-like or other) present at the cell surface that could act as receptors or coreceptors for FMDV on these cells. Because of the likely hinge movement of the G-H loop of VP1 (27, 35), it cannot be excluded that certain loop positions could bring into contact some loop residues with those found substituted in the variant FMDVs. This possibility is currently under investigation.
Some of the evidence presented here suggests that the protruding, mobile G-H loop of VP1 may exert some influence in the interaction with heparin. First, all four MARLS/hs− mutant clones included Ser-144 → Leu substitutions in the loop (Table 5). It cannot be totally excluded that Ser-144 conferred some selective disadvantage to FMDV during the process of negative selection for heparin binding for reasons unrelated to this phenotype. However, this seems unlikely in view of the high fitness and stability of the MARLS mutant upon repeated passages in BHK-21 cells (3). Second, mutant C-S8c1p100RGG displayed decreased binding to heparin compared to mutant C-S8c1p100c10 (Table 3). The capsids of these two viruses differ only in the presence of a Gly residue instead of an Asp in the RGG variant. Additional selection experiments for FMDV mutants with decreased affinity for heparin are in progress to determine whether mutations affecting the G-H loop of VP1 may influence heparin binding. It is noteworthy that the capsid residues which affect heparin binding in the populations derived from clone C-S8c1 are located at completely different positions than the relevant residues identified for FMDV serotype O (51). This means either that a variety of different capsid modifications may lead to the same heparin-binding phenotype or that different FMDV serotypes require different capsid modifications to achieve the same phenotypic result. This would not be the only biologically relevant difference among FMDV serotypes. We have recently documented the critical participation of the Asp-143 residue of the Arg-Gly-Asp triplet in the binding of neutralizing antibodies directed to the major antigenic site A (located within the G-H loop of VP1) of serotype C FMDV (57–59). This critical participation of the Arg-Gly-Asp triplet in antibody binding does not seem to apply to FMDV of serotype A (40, 45). This illustrates how evolution may drive individual representatives of a single viral genus to adopt different biological solutions for similar processes.
Although the observations on the use of integrin and HS receptors by FMDV have involved studies in cell cultures, it is by no means unlikely that changes in cell tropism could play a role in the infection process of FMDV in vivo. Sequestration of virus to particular cell types (esopharyngeal region during persistence or stratum spinosum of the vascular dermis during formation of the typical vesicles [reviewed in reference 17]) may depend on very few amino acid substitutions in capsid amino acid residues. Mutants with few substitutions relative to a dominant genomic sequence are likely to occur within the range of genomic fluctuations in quasispecies mutant spectra (11). The elucidation of possible variations of cell tropism in vivo poses an important challenge in view of the ample antigenic diversity of FMDV even within serotype C (42). The amino acid substitutions responsible for the antigenic differences may also exert some effect on the recognition of different cell types.
ACKNOWLEDGMENTS
We are indebted to C. Escarmís and E. Martínez-Salas for valuable discussions and unpublished information and to M. Dávila and G. Gómez Mariano for expert technical assistance. The CHO cell lines were kindly provided by J. D. Esko and were obtained through the courtesy of R. Snoeck.
Work in Madrid was supported by grant PB94-0034-C02-01 from DGICYT and Fundación Ramón Areces. Work at CID in Barcelona was supported by grant PB 95-0218 from DGICYT. Work in Giessen was supported by grant SFB 535 from Deutsche Forschungsgemeinschaft.
REFERENCES
- 1.Berinstein A, Roivainen M, Hovi T, Mason P W, Baxt B. Antibodies to the vitronectin receptor (integrin αvβ3) inhibit binding and infection of foot-and-mouth disease virus to cultured cells. J Virol. 1995;69:2664–2666. doi: 10.1128/jvi.69.4.2664-2666.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Borrego B, Novella I S, Giralt E, Andreu D, Domingo E. Distinct repertoire of antigenic variants of foot-and-mouth disease virus in the presence or absence of immune selection. J Virol. 1993;67:6071–6079. doi: 10.1128/jvi.67.10.6071-6079.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Charpentier N, Dávila M, Domingo E, Escarmís C. Long-term, large-population passage of aphthovirus can generate and amplify defective noninterfering particles deleted in the leader protease gene. Virology. 1996;223:10–18. doi: 10.1006/viro.1996.0450. [DOI] [PubMed] [Google Scholar]
- 4.Clarke D K, Duarte E A, Moya A, Elena S F, Domingo E, Holland J J. Genetic bottlenecks and population passages cause profound fitness differences in RNA viruses. J Virol. 1993;67:222–228. doi: 10.1128/jvi.67.1.222-228.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costa Giomi M P, Bergmann I E, Scodeller E A, Augé de Mello P, Gómez I, La Torre J L. Heterogeneity of the polyribocytidylic acid tract in aphthoviruses: biochemical and biological studies of viruses carrying polyribocytidylic acid tracts of different lengths. J Virol. 1984;51:799–805. doi: 10.1128/jvi.51.3.799-805.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeBorde D C, Naeve C W, Herlocher M L, Maassab H. Resolution of a common RNA sequencing ambiguity by terminal deoxynucleotidyl transferase. Anal Biochem. 1986;157:275–282. doi: 10.1016/0003-2697(86)90626-3. [DOI] [PubMed] [Google Scholar]
- 7.de la Torre J C, Dávila M, Sobrino F, Ortín J, Domingo E. Establishment of cell lines persistently infected with foot-and-mouth disease virus. Virology. 1985;145:24–35. doi: 10.1016/0042-6822(85)90198-9. [DOI] [PubMed] [Google Scholar]
- 8.de la Torre J C, Martínez-Salas E, Díez J, Villaverde A, Gebauer F, Rocha E, Dávila M, Domingo E. Coevolution of cells and viruses in a persistent infection of foot-and-mouth disease virus in cell culture. J Virol. 1988;62:2050–2058. doi: 10.1128/jvi.62.6.2050-2058.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Díez J, Dávila M, Escarmís C, Mateu M G, Dominguez J, Perez J J, Giralt E, Melero J A, Domingo E. Unique amino acid substitutions in the capsid proteins of foot-and-mouth disease virus from a persistent infection in cell culture. J Virol. 1990;64:5519–5528. doi: 10.1128/jvi.64.11.5519-5528.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Díez J, Mateu M G, Domingo E. Selection of antigenic variants of foot-and-mouth disease virus in the absence of antibodies, as revealed by an in situ assay. J Gen Virol. 1989;70:3281–3289. doi: 10.1099/0022-1317-70-12-3281. [DOI] [PubMed] [Google Scholar]
- 11.Domingo E. Biological significance of viral quasispecies. Viral Hepatitis Rev. 1996;2:247–261. [Google Scholar]
- 12.Domingo E, Dávila M, Ortín J. Nucleotide sequence heterogeneity of the RNA from a natural population of foot-and-mouth disease virus. Gene. 1980;11:333–346. doi: 10.1016/0378-1119(80)90073-6. [DOI] [PubMed] [Google Scholar]
- 13.Domingo E, Díez J, Martínez M A, Hernández J H, Holguín A, Borrego B, Mateu M G. New observations on antigenic diversification of RNA viruses. Antigenic variation is not dependent on immune selection. J Gen Virol. 1993;74:2039–2045. doi: 10.1099/0022-1317-74-10-2039. [DOI] [PubMed] [Google Scholar]
- 14.Domingo E, Escarmís C, Sevilla N, Moya A, Elena S F, Quer J, Novella I S, Holland J J. Basic concepts in RNA virus evolution. FASEB J. 1996;10:859–864. doi: 10.1096/fasebj.10.8.8666162. [DOI] [PubMed] [Google Scholar]
- 15.Domingo E, Holland J J. RNA virus mutations and fitness for survival. Annu Rev Microbiol. 1997;51:151–178. doi: 10.1146/annurev.micro.51.1.151. [DOI] [PubMed] [Google Scholar]
- 16.Domingo E, Holland J J, Biebricher C, Eigen M. Quasispecies: The concept and the word. In: Gibbs A, Calisher C, García-Arenal F, editors. Molecular basis of virus evolution. Cambridge, United Kingdom: Cambridge University Press; 1995. pp. 171–180. [Google Scholar]
- 17.Domingo E, Mateu M G, Martínez M A, Dopazo J, Moya A, Sobrino F. Genetic variability and antigenic diversity of foot-and-mouth disease virus. Appl Virol Res. 1990;2:233–266. [Google Scholar]
- 18.Domingo E, Sabo D L, Taniguchi T, Weissmann C. Nucleotide sequence heterogeneity of an RNA phage population. Cell. 1978;13:735–744. doi: 10.1016/0092-8674(78)90223-4. [DOI] [PubMed] [Google Scholar]
- 19.Eigen M, Biebricher C K. Sequence space and quasispecies distribution. In: Domingo E, Holland J J, Ahlquist P, editors. RNA genetics. Vol. 3. Boca Raton, Fla: CRC Press, Inc.; 1988. pp. 211–245. [Google Scholar]
- 20.Escarmís C, Dávila M, Charpentier N, Bracho A, Moya A, Domingo E. Genetic lesions associated with Muller’s ratchet in an RNA virus. J Mol Biol. 1996;264:255–267. doi: 10.1006/jmbi.1996.0639. [DOI] [PubMed] [Google Scholar]
- 21.Escarmís C, Toja M, Medina M, Domingo E. Modifications of the 5′ untranslated region of foot-and-mouth disease virus after prolonged persistence in cell culture. Virus Res. 1992;26:113–125. doi: 10.1016/0168-1702(92)90151-x. [DOI] [PubMed] [Google Scholar]
- 22.Esko J D, Stewart T E, Taylor W H. Animal cell mutants defective in glycosaminoglycans biosynthesis. Proc Natl Acad Sci USA. 1985;82:3197–3201. doi: 10.1073/pnas.82.10.3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fox G, Parry N, Barnett P V, McGlinn B, Rowlands D J, Brown F. The cell attachment site on foot-and-mouth disease virus includes the amino acid sequence RGD (argine-glycine-aspartic acid) J Gen Virol. 1989;70:625–637. doi: 10.1099/0022-1317-70-3-625. [DOI] [PubMed] [Google Scholar]
- 24.Gebauer F, de la Torre J C, Gomes I, Mateu M G, Barahona H, Tiraboschi B, Bergmann I, Augé de Mello P, Domingo E. Rapid selection of genetic and antigenic variants of foot-and-mouth disease virus during persistence in cattle. J Virol. 1988;62:2041–2049. doi: 10.1128/jvi.62.6.2041-2049.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris T J R, Brown F. Biochemical analysis of a virulent and an avirulent strain of foot-and-mouth disease virus. J Gen Virol. 1977;34:87–105. doi: 10.1099/0022-1317-34-1-87. [DOI] [PubMed] [Google Scholar]
- 26.Hernández J, Valero M L, Andreu D, Domingo E, Mateu M G. Antibody and host cell recognition of foot-and-mouth disease virus (serotype C) cleaved at the Arg-Gly-Asp (RGD) motif: a structural interpretation. J Gen Virol. 1996;77:257–264. doi: 10.1099/0022-1317-77-2-257. [DOI] [PubMed] [Google Scholar]
- 27.Hewat E A, Verdaguer N, Fita I, Blakemore W, Brookes S, King A, Newman J, Domingo E, Mateu M G, Stuart D. Structure of the complex of an Fab fragment of a neutralizing antibody with foot-and-mouth disease virus: positioning of a highly mobile antigenic loop. EMBO J. 1997;16:1492–1500. doi: 10.1093/emboj/16.7.1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holguín A. Variantes genéticos y fenotípicos en cuasiespecies del virus de la fiebre aftosa y del virus de la inmunodeficiencia humana. Ph.D. thesis. Madrid, Spain: Universidad Autónoma de Madrid; 1996. [Google Scholar]
- 29.Holguin A, Hernandez J, Martinez M A, Mateu M G, Domingo E. Differential restrictions on antigenic variation among antigenic sites of foot-and-mouth disease virus in the absence of antibody selection. J Gen Virol. 1997;78:601–609. doi: 10.1099/0022-1317-78-3-601. [DOI] [PubMed] [Google Scholar]
- 30.Holland J J, de la Torre J C, Steinhauer D A. RNA viral populations as quasispecies. Curr Top Microbiol Immunol. 1992;176:1–20. doi: 10.1007/978-3-642-77011-1_1. [DOI] [PubMed] [Google Scholar]
- 31.Jackson T, Ellard F M, Abu Ghazaleh R, Brookes S M, Blakemore W E, Corteyn A H, Stuart D I, Newman J W I, King A M Q. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J Virol. 1996;70:5282–5287. doi: 10.1128/jvi.70.8.5282-5287.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jackson T, Sharma A, Ghazaleh R A, Blakemore W E, Ellard F M, Simmons D F L, Newman J W I, Stuart D I, King A M Q. Arginine-glycine-aspartic acid binding by foot-and-mouth disease viruses to the purified integrin αvβ3 in vitro. J Virol. 1997;71:8357–8361. doi: 10.1128/jvi.71.11.8357-8361.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lea S, Hernandez J, Blakemore W, Brocchi E, Curry S, Domingo E, Fry E, Abu-Ghazaleh R, King A, Newman J, Stuart D, Mateu M G. The structure and antigenicity of a type C foot-and-mouth disease virus. Structure. 1994;2:123–139. doi: 10.1016/s0969-2126(00)00014-9. [DOI] [PubMed] [Google Scholar]
- 34.Lidholt K, Weinke J L, Kiser C S, Lugemwa F N, Bame K J, Cheifetz S, Massagué J, Lindahl U, Esko J D. A single mutation affects both N-acetylglucosaminyltransferase and glucuronosyltransferase activities in a chinese hamster ovary cell mutant defective in heparin sulfate biosynthesis. Proc Natl Acad Sci USA. 1992;89:2267–2271. doi: 10.1073/pnas.89.6.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Logan D, Abu-Ghazaleh R, Blakemore W, Cyrry S, Jackson T, King A, Lea S, Lewis R, Newman J, Parry N, Rowlands D, Stuart D, Fry E. Structure of a major immunogenic site of foot-and-mouth disease virus. Nature. 1993;362:566–568. doi: 10.1038/362566a0. [DOI] [PubMed] [Google Scholar]
- 36.Martínez M A, Carrillo C, González-Candelas F, Moya A, Domingo E, Sobrino F. Fitness alteration of foot-and-mouth disease virus mutants: measurement of adaptability of viral quasispecies. J Virol. 1991;65:3954–3957. doi: 10.1128/jvi.65.7.3954-3957.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martínez M A, Verdaguer N, Mateu M G, Domingo E. Evolution subverting essentiality: dispensability of the cell attachment Arg-Gly-Asp motif in multiply passaged foot-and-mouth disease virus. Proc Natl Acad Sci USA. 1997;94:6798–6802. doi: 10.1073/pnas.94.13.6798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martínez-Salas E, Saiz J C, Dávila M, Belsham G J, Domingo E. A single nucleotide substitution in the internal ribosome entry site of foot-and-mouth disease virus leads to enhanced cap-independent translation in vivo. J Virol. 1993;67:3748–3755. doi: 10.1128/jvi.67.7.3748-3755.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martin-Hernández A M, Carrillo E C, Sevilla N, Domingo E. Rapid cell variation can determine the establishment of a persistent viral infection. Proc Natl Acad Sci USA. 1994;91:3705–3709. doi: 10.1073/pnas.91.9.3705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mason P W, Rieder E, Baxt B. RGD sequence of foot-and-mouth disease virus in essential for infecting cells via the natural receptor but can be bypassed and antibody-dependent enhancement pathway. Proc Natl Acad Sci USA. 1994;91:1932–1936. doi: 10.1073/pnas.91.5.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mateu M G. Antibody recognition of picornaviruses and escape from neutralization: a structural view. Virus Res. 1995;38:1–24. doi: 10.1016/0168-1702(95)00048-u. [DOI] [PubMed] [Google Scholar]
- 42.Mateu M G, Da Silva J J, Rocha E, De Brum D L, Alonso A, Enjuanes L, Domingo E, Barahona H. Extensive antigenic heterogeneity of foot-and-mouth disease virus of serotype C. Virology. 1988;166:113–124. doi: 10.1016/0042-6822(88)90060-8. [DOI] [PubMed] [Google Scholar]
- 43.Mateu M G, Hernández J, Martínez M A, Feigelstock D, Lea S, Peréz J J, Giralt E, Stuart D, Palma E L, Domingo E. Antigenic heterogeneity of foot-and-mouth disease virus serotype in the field is mediated by very limited sequence variation at several antigenic sites. J Virol. 1994;68:1407–1417. doi: 10.1128/jvi.68.3.1407-1417.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mateu M G, Martínez M A, Capucci L, Andreu D, Girald E, Sobrino F, Brocchi E, Domingo E. A single amino acid substitution affect multiple overlapping epitopes in the major antigenic site of foot-and-mouth disease virus of serotype C. J Gen Virol. 1990;71:629–637. doi: 10.1099/0022-1317-71-3-629. [DOI] [PubMed] [Google Scholar]
- 45.McKenna T S C, Lubroth J, Rieder E, Baxt B, Mason P W. Receptor binding-site-deleted foot-and-mouth disease (FMD) virus protects cattle from FMD. J Virol. 1995;69:5787–5790. doi: 10.1128/jvi.69.9.5787-5790.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Novella I S, Clarke D K, Quer J, Duarte E A, Lee C H, Weaver S C, Elena S F, Moya A, Domingo E, Holland J J. Extreme fitness differences in mammalian and insect hosts after continuous replication of vesicular stomatitis virus in sandfly cells. J Virol. 1995;69:6805–6809. doi: 10.1128/jvi.69.11.6805-6809.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Novella I S, Duarte E A, Elena S F, Moya A, Domingo E, Holland J J. Exponential increases of RNA virus fitness during large population transmission. Proc Natl Acad Sci USA. 1995;92:5841–5844. doi: 10.1073/pnas.92.13.5841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rieder E, Bunch T, Brown F, Mason P W. Genetically engineered foot-and-mouth disease viruses with poly(C) tracts of two nucleotides are virulent in mice. J Virol. 1993;67:5139–5145. doi: 10.1128/jvi.67.9.5139-5145.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roussel A, Cambillau C. Silicon Graphics geometry partners directory Silicon Graphics. 1989. TURBO-FRODO; pp. 77–78. Mountain View, Calif. [Google Scholar]
- 50.Ryan M D, Flint M. Virus-encoded proteinases of the picornavirus super-group. J Gen Virol. 1997;78:699–723. doi: 10.1099/0022-1317-78-4-699. [DOI] [PubMed] [Google Scholar]
- 51.Sa-Carvalho D, Rieder E, Baxt B, Rodarte R, Tanuri A, Mason P. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J Virol. 1997;71:5115–5123. doi: 10.1128/jvi.71.7.5115-5123.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sáiz J C, Domingo E. Virulence as a positive trait in viral persistence. J Virol. 1996;70:6410–6413. doi: 10.1128/jvi.70.9.6410-6413.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Salt J S. The carrier state in foot-and-mouth disease—an immunological review. Br Vet J. 1993;149:207–223. doi: 10.1016/S0007-1935(05)80168-X. [DOI] [PubMed] [Google Scholar]
- 54.Sevilla N, Domingo E. Evolution of a persistent aphthovirus in cytolytic infections: partial reversion of phenotypic traits accompanied by genetic diversification. J Virol. 1996;70:6617–6624. doi: 10.1128/jvi.70.10.6617-6624.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sevilla N, Verdaguer N, Domingo E. Antigenically profound amino acid substitutions occur during large population passages of foot-and-mouth disease virus. Virology. 1996;225:400–405. doi: 10.1006/viro.1996.0615. [DOI] [PubMed] [Google Scholar]
- 56.Sobrino F, Dávila M, Ortin J, Domingo E. Multiple genetic variants arise in the course of replication of foot-and-mouth disease virus in cell culture. Virology. 1983;128:310–318. doi: 10.1016/0042-6822(83)90258-1. [DOI] [PubMed] [Google Scholar]
- 57.Verdaguer N, Mateu M G, Andreu D, Giralt E, Domingo E, Fita I. Structure of the major antigenic loop of foot-and-mouth disease virus complexed with a neutralizing antibody: direct involvement of the Arg-Gly-Asp motif in the interaction. EMBO J. 1995;14:1690–1696. doi: 10.1002/j.1460-2075.1995.tb07158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Verdaguer N, Mateu M G, Bravo J, Domingo E, Fita I. Induced pocket to accommodate the cell attachment Arg-Gly-Asp motif in a neutralizing antibody against foot-and-mouth disease virus. J Mol Biol. 1996;256:364–376. doi: 10.1006/jmbi.1996.0092. [DOI] [PubMed] [Google Scholar]
- 59.Verdaguer N, Sevilla N, Valero M L, Stuart D, Brocchi E, Andreu D, Giralt E, Domingo E, Mateu M G, Fita I. A similar pattern of interaction for different antibodies with a major antigenic site of foot-and-mouth disease virus: implications for intratypic antigenic variation. J Virol. 1998;72:739–748. doi: 10.1128/jvi.72.1.739-748.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zibert A, Maass G, Strebel K, Falk M M, Beck E. Infectious foot-and-mouth disease virus derived from a cloned full-length cDNA. J Virol. 1990;64:2467–2473. doi: 10.1128/jvi.64.6.2467-2473.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zimmern D. Evolution of RNA viruses. In: Domingo E, Holland J J, Ahlquist P, editors. RNA genetics. Vol. 2. Boca Raton, Fla: CRC Press, Inc.; 1988. pp. 211–240. [Google Scholar]