Abstract
In recent years, the association between neuroinflammatory markers and dementia, especially Alzheimer’s disease (AD), has attracted much attention. However, the evidence for the relationship between serum-hs-CRP and dementia including AD are inconsistent. Therefore, the relationships of serum high-sensitivity CRP (hs-CRP) with dementia including AD and with regions of interest of brain MRI were investigated. A total of 11,957 community residents aged 65 years or older were recruited in eight sites in Japan (JPSC-AD Study). After applying exclusion criteria, 10,085 participants who underwent blood tests and health-related examinations were analyzed. Then, serum hs-CRP levels were classified according to clinical cutoff values, and odds ratios for the presence of all-cause dementia and its subtypes were calculated for each serum hs-CRP level. In addition, the association between serum hs-CRP and brain volume regions of interest was also examined using analysis of covariance with data from 8614 individuals in the same cohort who underwent brain MRI. After multivariable adjustment, the odds ratios (ORs) for all-cause dementia were 1.04 (95% confidence interval [CI] 0.76–1.43), 1.68 (95%CI 1.08–2.61), and 1.51 (95%CI 1.08–2.11) for 1.0–1.9 mg/L, 2.0–2.9 mg/L, and ≥ 3.0 mg/L, respectively, compared to < 1.0 mg/L, and those for AD were 0.72 (95%CI 0.48–1.08), 1.76 (95%CI 1.08–2.89), and 1.61 (95%CI 1.11–2.35), for 1.0–1.9 mg/L, 2.0–2.9 mg/L, and ≥ 3.0 mg/L, respectively, compared to < 1.0 mg/L. Multivariable-adjusted ORs for all-cause dementia and for AD prevalence increased significantly with increasing serum hs-CRP levels (p for trend < 0.001 and p = 0.001, respectively). In addition, the multivariable-adjusted temporal cortex volume/estimated total intracranial volume ratio decreased significantly with increasing serum hs-CRP levels (< 1.0 mg/L 4.28%, 1.0–1.9 mg/L 4.27%, 2.0–2.9 mg/L 4.29%, ≥ 3.0 mg/L 4.21%; p for trend = 0.004). This study’s results suggest that elevated serum hs-CRP levels are associated with greater risk of presence of dementia, especially AD, and of temporal cortex atrophy in a community-dwelling Japanese older population.
Keywords: Alzheimer’s disease, Dementia, High-sensitivity C-reactive protein, Inflammation, Population-based study
Subject terms: Alzheimer's disease, Alzheimer's disease
Introduction
Vascular inflammation and neuroinflammation have been implicated in increased risks of cognitive impairments, particularly Alzheimer’s disease (AD)1–3. Reports have been accumulating showing that systemic inflammation is directly associated with the development of AD2,4,5. Further, vascular risk factors such as hypertension, diabetes mellitus, and chronic kidney disease have been shown to be associated with AD6–8, and vascular inflammation is assumed to be behind these vascular risk factors9.
Serum high-sensitivity C reactive protein (hs-CRP) is a conveniently measured biomarker of systemic inflammation10, but there is no consensus on the association between serum hs-CRP and dementia including AD. Although serum hs-CRP has been reported to be significantly lower in AD patients than in healthy subjects11, a recent meta-analysis found that serum hs-CRP was significantly higher in AD patients than in healthy older subjects12. In another meta-analysis, serum hs-CRP was associated with all-cause dementia, but not with AD13. The relationship between serum hs-CRP and dementia has also been investigated in middle and old age groups, and many reports suggest that high serum hs-CRP levels in middle age increase the risk of AD14. However, reports on the relationship between serum hs-CRP and AD in older subjects were controversial15,16.
Regarding the association between serum hs-CRP levels and brain atrophy, there are reports that elevated serum hs-CRP levels were associated with atrophy of the frontal and temporal corticies17, and that serum hs-CRP was not significantly associated with brain atrophy after multivariable adjustment18. Thus, the results are inconsistent.
The Japan Prospective Studies Collaboration for Aging and Dementia (JPSC-AD) was a prospective cohort study of dementia. A total of 11,957 community-dwelling older residents were surveyed in eight sites from 2016 to 2018. The aim of this study was to examine the relationship between serum hs-CRP levels and dementia, especially AD, and their association with brain atrophy using cross-sectional data from this group of older Japanese persons.
Methods
Study population
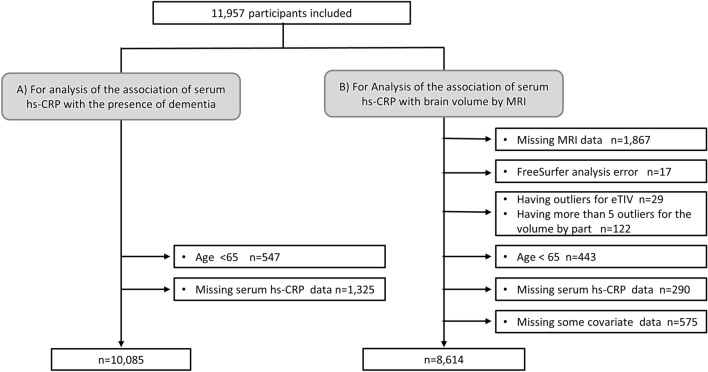
The JPSC-AD Study was a multisite, population-based, prospective, cohort study of dementia involving eight sites in Japan with a pre-specified protocol and standardized measurement methods across the research sites19–22. The study was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist. The Medical Ethics Review Board of Ehime University (approval number 1610004) and Kyushu University Institutional Review Board for clinical research (approval number 686-10) approved this study. Written, informed consent was obtained from all participants. This study was performed in accordance with the Declaration of Helsinki. A total of 11,957 people consented to participate in the study between 2016 and 2018, of which 10,085 were eligible for the present study, excluding 547 participants younger than 65 years and 1325 participants lacking serum hs-CRP levels (Fig. 1A).
Figure 1.
Flowchart of participants selection for the analysis of the association of serum high-sensitivity C-reactive protein with the presence of dementia (A) and brain volume estimated by brain magnetic resonance imaging (B). Abbreviations: MRI, magnetic resonance imaging; eTIV, estimated total intracranial volume.
For the analysis of the association between serum hs-CRP levels and brain volume estimated by brain magnetic resonance imaging (MRI) scan, a total of 8614 participants were included after excluding 1867 participants without available brain MRI data, 17 participants for whom FreeSurfer analysis was errored, 29 participants who had outlier for estimated total intracranial volume (eTIV), 122 participants who had more than 5 outliers for the volume by part, 443 participants aged less than 65 years, 290 participants lacking serum hs-CRP levels, and 575 with missing some covariates data (Fig. 1B).
Measurement of serum hs-CRP
Serum hs-CRP was measured at the central laboratory (LSI Medience Corporation, Tokyo) for all participants using the latex agglutination turbidimetry method. The detailed measurement methods of surum hs-CRP are shown in Supplemental Table 1. Basically, the samples were analyzed once and when abnormal values were found, reassay was carried out. Serum hs-CRP values were categorized into four categories (< 1.0 mg/L, 1.0–1.9 mg/L, 2.0–2.9 mg/L, ≥ 3.0 mg/L) according to clinical cut-off values.
Measurement of other risk factors
Each participant completed a self-administered questionnaire that included education, medical history, alcohol consumption, smoking, medical treatment (antihypertensive medications, diabetes medications), and physical activity. Blood pressure was measured three times with a sphygmomanometer at intervals of at least 5 min, and the average of the three measurements was used for the analysis23. Hypertension was defined by blood pressure greater than 140/90 mmHg or current use of antihypertensive medications. Ischemic heart disease was defined as history of myocardial infarction and/or coronary intervention. Diabetes mellitus was defined by a fasting glucose level ≥ 7.0 mmol/L, glucose level at any time ≥ 11.1 mmol/L, or HbA1c ≥ 6.5%, and/or current use of antidiabetic medications according to the 2010 American Diabetes Association (ADA) criteria24. Serum total cholesterol levels were measured by an enzymatic method. The body mass index (kg/m2) was calculated as an index of obesity. Chronic kidney disease was defined as estimated glomerular filtration rate < 60 ml/min/1.73 m225 and calculated by multiplying the modified Chronic Kidney Disease Epidemiology Collaboration formula by the Japanese coefficient (0.813)26,27. Electrocardiographic abnormalities were defined as ST depression (Minnesota code, 4-1, 2, 3), left ventricular hypertrophy (3-1), and atrial fibrillation (8-3). Regular exercise was defined as physical activity performed for at least 30 min twice a week over the last year. Alcohol consumption and smoking were categorized as ongoing or not. Apolipoprotein E (APOE) ε4 carrier status was defined as the presence of the ε2/ε4, ε3/ε4, and ε4/ε4 alleles. To determine the APOE polymorphism, two single-nucleotide polymorphisms (rs429358 and rs7412) were genotyped using the multiplex PCR-based targeted sequencing method, as previously reported28. Depression was diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders, Third Revised Edition29.
Diagnosis of dementia
Dementia was diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders, Third Revised Edition29. The diagnosis of AD was made based on the following criteria: the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association criteria30. The diagnosis was made by the study team’s expert psychiatrists and neurologists using a standardized diagnostic system across the eight study sites. If the members of the endpoint determination committee agreed, the diagnosis was confirmed; if not, an endpoint determination committee was convened to confirm the diagnosis through discussion. The diagnostic procedure has been previously reported22. Dementia other than AD (isolated type and mixed type) was defined as non- Alzheimer’s dementia (non-AD).
MRI analysis
Brain MRI equipment was set up according to the Alzheimer’s Disease Neuroimaging Initiative (ADNI) study brain MRI protocols31 and T1-weighted image (T1WI) parameters at all study sites. Details of the MRI at each site are provided in Supplemental Table 2.
Segmentation and volumetric measurements of cortical and subcortical brain structures were performed automatically using FreeSurfer software (http://surfer.nmr.mgh.harvard.edu), version 5.3. Total brain volume was calculated from brain segment volumes excluding ventricles. Cortical segmentation was performed using the Desikan-Killiany atlas32. The eTIV of each subject was also calculated using the standard FreeSurfer processing pipeline by exploiting the relationship between the intracranial volume and the linear transformation to the atlas template33. Specifically, FreeSurfer estimates of each brain parameter were fitted with a linear regression model adjusted for age, age squared, and sex. If the residuals of an individual participant’s data were less than − 4 standard deviation (SD) units or greater than + 4 SD units from the linear regression, these data were considered extreme outliers. Extreme outliers in eTIV and volumes of at least five brain regions were excluded.
We selected from the gray matter 4 representative cerebral lobes, i.e., the frontal cortex, parietal cortex, temporal cortex, and occipital cortex, and 3 dementia-related brain regions, i.e., the insular cortex, hippocampus, and amygdala, based on the findings of a previous study34.
Statistical analyses
For patient background, comparisons among the four groups of serum hs-CRP < 1.0 mg/L, 1.0–1.9 mg/L, 2.0–2.9 mg/L, ≥ 3.0 mg/L were evaluated with the logistic regression analysis for binary variables and linear regression analysis for continuous variables. Age- and sex-adjusted prevalence of all-cause dementia and its subtypes was estimated by the direct method with 5-year age groups. Age- and sex-adjusted and multivariable-adjusted odds ratios for presence of all-cause dementia and its subtypes were calculated by logistic regression analysis. Trends between serum hs-CRP levels were calculated using multiple regression analysis. Multivariable adjustment was performed for age, sex, education, hypertension, ischemic heart disease, diabetes mellitus, serum total cholesterol level, BMI, chronic kidney disease, abnormal electrocardiogram (ECG), previous stroke, smoking, alcohol consumption, exercise habits, APOE ε4 carrier status, depression, and research site. Of the participants selected for this analysis, 7.7% (= 774/10,085) were excluded from the multivariable-adjusted analysis due to missing data for any covariates. Mean values of brain volume were adjusted for the same adjustment factors and subjected to analysis of covariance. Two-tailed p value < 0.05 were considered significant. In the analysis for the association between serum hs-CRP levels and each regional brain volume, false discovery rate (FDR)-corrected p values (i.e., q values) was calculated by using the Benjamini–Hochberg methods35 in consideration of multiple comparisons, and a q-value < 0.05 was considered statistically significant. All analyses were conducted using the Statistical Package for the Social Sciences (version 23; SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics of the study population
The patient background of the study population is summarized in Table 1. Age, low education, current smoker, BMI, hypertension, diabetes mellitus, ischemic heart disease, chronic kidney disease, stroke, and ECG abnormalities were significantly higher with higher serum hs-CRP levels. Frequency of female, serum total cholesterol levels, regular exercise, and frequency of APOE ε4 carriers were significantly lower with higher serum hs-CRP levels.
Table 1.
Clinical characteristics of the study participants according to serum high-sensitivity C-reactive protein level (n = 10,085).
| Variable | Serum hs-CRP level, mg/L | ||||
|---|---|---|---|---|---|
| < 1.0 | 1.0–1.9 | 2.0–2.9 | ≥ 3.0 | P for trend | |
| n = 7465 | n = 1379 | n = 442 | n = 799 | ||
| Age, y | 73.5 (6.5) | 74.0 (6.8) | 74.2 (7.2) | 75.4 (7.3) | < 0.001 |
| Female, % | 60.0 | 52.1 | 48.2 | 49.2 | < 0.001 |
| Education ≤ 9 y, % | 31.4 | 31.6 | 33.6 | 37.2 | 0.002 |
| Hypertension, % | 72.0 | 78.6 | 77.9 | 78.0 | < 0.001 |
| Diabetes mellitus, % | 15.2 | 19.82 | 22.5 | 21.5 | < 0.001 |
| Serum total cholesterol, mmol/L | 5.4 (0.9) | 5.3 (0.9) | 5.2 (0.9) | 5.0 (0.9) | < 0.001 |
| BMI, kg/m2 | 23.0 (3.2) | 24.4 (3.5) | 24.3 (3.6) | 23.9 (3.9) | < 0.001 |
| Ischemic heart disease, % | 4.2 | 5.2 | 5.4 | 7.0 | < 0.001 |
| Chronic kidney disease, % | 17.4 | 23.8 | 24.7 | 26.7 | < 0.001 |
| ECG abnormalities, % | 13.5 | 14.2 | 18.8 | 16.6 | 0.001 |
| History of stroke, % | 5.5 | 8.5 | 7.0 | 10.9 | < 0.001 |
| Current smoker, % | 7.1 | 11.0 | 10.0 | 10.8 | < 0.001 |
| Current drinker, % | 41.9 | 44.0 | 46.2 | 35.8 | 0.08 |
| Regular exercise, % | 43.3 | 38.0 | 35.4 | 36.9 | < 0.001 |
| APOE ε4 carrier, % | 20.2 | 13.0 | 12.9 | 15.6 | < 0.001 |
| Depression, % | 1.1 | 0.9 | 1.1 | 1.8 | 0.16 |
Values are shown as means (standard deviation) or frequencies.
hs-CRP high-sensitivity C-reactive protein, BMI body mass index, ECG electrocardiogram, APOE apolipoprotein E.
Associations of serum hs-CRP levels with all-cause dementia and dementia subtypes
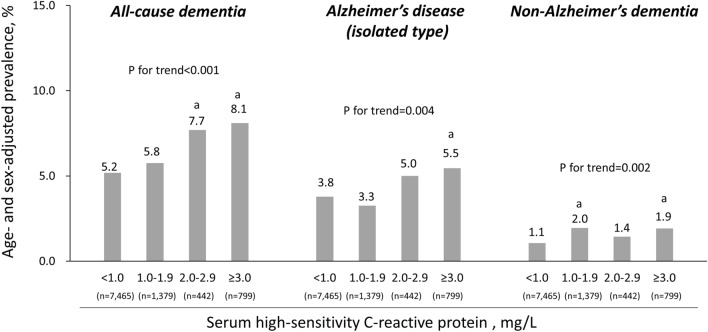
First, the age- and sex-adjusted prevalence of all-cause dementia, AD and non-AD are shown in Fig. 2. The age- and sex-adjusted prevalence of all-cause dementia, AD and non-AD increased significantly with rising serum hs-CRP levels (p for trend < 0.001, p for trend = 0.004, p for trend = 0.002, respectively). Moreover, the odds ratios of the presence of all-cause dementia, AD and non-AD according to serum hs-CRP level were calculated; as shown in Table 2. The multivariable-adjusted odds ratios for the presence of all-cause dementia were 1.04 (95% confidence interval [CI] 0.76–1.43), 1.68 (95%CI 1.08–2.61), and 1.51 (95%CI 1.08–2.11) for 1.0–1.9 mg/L, 2.0–2.9 mg/L, and ≥ 3.0 mg/L, respectively, compared to < 1.0 mg/L, with a significant increase with higher serum hs-CRP levels (p for trend < 0.001). Similarly, as shown in Table 2, the multivariable-adjusted odds ratios for the presence of AD were 0.72 (95%CI 0.48–1.08), 1.76 (95%CI 1.08–2.89), and 1.61 (95%CI 1.11–2.35), for 1.0–1.9 mg/L, 2.0–2.9 mg/L, and ≥ 3.0 mg/L, respectively, compared to < 1.0 mg/L, increasing significantly with higher serum hs-CRP levels (p for trend = 0.001). On the other hand, there was no evidence of significant associations between serum hs-CRP levels and the multivariable-adjusted odds ratio of non-AD (p for trend = 0.47). In a sensitivity analysis excluding 491 patients with serum hs-CRP ≥ 5.0 mg/L, the significant association between serum hs-CRP and not only all-cause dementia, but also AD, remained (Supplemental Table 3).
Figure 2.
The age- and sex-adjusted prevalence of all-cause dementia and dementia subtypes according to serum high-sensitivity C-reactive protein level. The data are expressed as the prevalence after adjusting for age and sex. (a) p < 0.05, compared to the lowest serum high-sensitivity C-reactive protein group.
Table 2.
Age- and sex-adjusted and multivariable-adjusted odds ratios for the presence of all-cause dementia and dementia subtypes according to serum high-sensitivity C-reactive protein level.
| Serum hs-CRP, mg/L | No. of cases/participants | Age- and sex-adjusted | Multivariable-adjusteda | ||
|---|---|---|---|---|---|
| OR (95%CI) | p | OR (95%CI) | p | ||
| All-cause dementia | |||||
| < 1.0 | 367/7465 | 1.00 (reference) | 1.00 (reference) | ||
| 1.0–1.9 | 82/1379 | 1.08 (0.82–1.41) | 0.60 | 1.04 (0.76–1.43) | 0.80 |
| 2.0–2.9 | 38/442 | 1.57 (1.06–2.32) | 0.03 | 1.68 (1.08–2.61) | 0.02 |
| ≥ 3.0 | 86/799 | 1.70 (1.28–2.25) | < 0.001 | 1.51 (1.08–2.11) | 0.02 |
| P for trend | < 0.001 | < 0.001 | |||
| Alzheimer’s disease (isolated type) | |||||
| < 1.0 | 269/7465 | 1.00 (reference) | 1.00 (reference) | ||
| 1.0–1.9 | 46/1379 | 0.77 (0.55–1.09) | 0.14 | 0.72 (0.48–1.08) | 0.11 |
| 2.0–2.9 | 25/442 | 1.33 (0.84–2.11) | 0.23 | 1.76 (1.08–2.89) | 0.02 |
| ≥ 3.0 | 58/799 | 1.47 (1.06–2.04) | 0.02 | 1.61 (1.11–2.35) | 0.01 |
| P for trend | 0.004 | 0.001 | |||
| Non-Alzheimer’s dementia | |||||
| < 1.0 | 75/7465 | 1.00 (reference) | 1.00 (reference) | ||
| 1.0–1.9 | 28/1379 | 1.84 (1.18–2.88) | 0.007 | 2.02 (1.19–3.44) | 0.009 |
| 2.0–2.9 | 7/442 | 1.32 (0.60–2.91) | 0.50 | 0.64 (0.19–2.17) | 0.48 |
| ≥ 3.0 | 20/799 | 1.80 (1.08–3.01) | 0.03 | 1.06 (0.53–2.14) | 0.87 |
| P for trend | 0.002 | 0.47 | |||
Mixed types including Alzheimer’s disease are not included in either Alzheimer’s disease (isolated) or non-Alzheimer’s dementia groups.
hs-CRP high-sensitivity C-reactive protein, OR odds ratio, CI confidence interval.
aAdjusted for age, sex, low education, hypertension, ischemic heart disease, diabetes mellitus, serum total cholesterol, body mass index, chronic kidney disease, electrocardiogram abnormalities, history of stroke, smoking habit, alcohol intake, regular exercise, apolipoprotein E ε4 carrier status, depression, and research site.
Associations of serum hs-CRP levels with brain volume
Next, Table 3 shows the relationships between serum hs-CRP levels and each brain volume/total intracranial volume ratio. In all subjects included in the imaging analysis, the multivariable-adjusted mean value of total brain volume/eTIV ratio decreased significantly with increasing serum hs-CRP levels (p for trend = 0.02) (Table 3). With regard to regional brain volume, higher serum hs-CRP levels were associated significantly with lower multivariable-adjusted mean values of temporal cortex volume/eTIV ratio (p for trend = 0.004). This significant association was also observed, even after FDR correction (q-value = 0.03). Sensitivity analysis after excluding 353 participants with dementia found a similar negative association between serum hs-CRP levels and mean values of temporal cortex volume/eTIV ratio (%): serum hs-CRP < 1.0 mg/L, 4.33 (95%CI 4.24–4.42); 1.0–1.9 mg/L, 4.33 (4.24–4.42); 2.0–2.9 mg/L, 4.36 (4.26–4.46); ≥ 3.0 mg/L, 4.27 (4.18–4.37); p for trend = 0.02 (data not shown).
Table 3.
Multivariable-adjusted mean values (95% confidence intervals) of total brain volume and each regional brain volume to estimated total intracranial volume ratios according to serum high-sensitivity C-reactive protein level in all participants.
| Brain region | Serum hs-CRP levels | |||||
|---|---|---|---|---|---|---|
| < 1.0 mg/L (n = 6412) | 1.0–1.9 mg/L (n = 1178) | 2.0–2.9 mg/L (n = 387) | ≥ 3.0 mg/L (n = 637) | P for trend | q-value of FDR correction | |
| Total brain volume/eTIV | 54.59 (53.95 to 55.24) | 54.51 (53.85 to 55.17) | 54.56 (53.84 to 55.27) | 54.24 (53.56 to 54.91) | 0.02 | – |
| Each regional braina | ||||||
| Frontal cortex volume/eTIV | 6.85 (6.73 to 6.98) | 6.86 (6.73 to 6.99) | 6.84 (6.70 to 6.99) | 6.79 (6.66 to 6.93) | 0.051 | 0.18 |
| Parietal cortex volume/eTIV | 4.34 (4.24 to 4.43) | 4.34 (4.24 to 4.44) | 4.33 (4.22 to 4.43) | 4.30 (4.20 to 4.49) | 0.13 | 0.23 |
| Temporal cortex volume/eTIV | 4.28 (4.19 to 4.37) | 4.27 (4.18 to 4.37) | 4.29 (4.19 to 4.39) | 4.21 (4.12 to 4.31) | 0.004 | 0.03 |
| Occipital cortex volume/eTIV | 1.73 (1.68 to 1.77) | 1.73 (1.68 to 1.78) | 1.74 (1.69 to 1.79) | 1.72 (1.67 to 1.76) | 0.56 | 0.78 |
| Insular cortex volume/eTIV | 0.75 (0.73 to 0.76) | 0.75 (0.73 to 0.76) | 0.76 (0.74 to 0.77) | 0.75 (0.73 to 0.76) | 0.78 | 0.91 |
| Hippocampal volume/eTIV | 0.31 (0.30 to 0.32) | 0.31 (0.30 to 0.32) | 0.31 (0.30 to 0.33) | 0.31 (0.30 to 0.32) | 0.08 | 0.19 |
| Amygdala volume/eTIV | 0.018 (0.013 to 0.023) | 0.018 (0.013 to 0.024) | 0.019 (0.013 to 0.025) | 0.018 (0.012 to 0.023) | 0.91 | 0.91 |
Values are shown as multivariable-adjusted mean values (95% confidence intervals), where values are calculated as follows: ([left + right] volumes of total brain or each regional brain/eTIV) × 100 (%), where values were adjusted for the following covariates: age, sex, low education, hypertension, ischemic heart disease, diabetes mellitus, serum total cholesterol, body mass index, chronic kidney disease, electrocardiogram abnormalities, history of stroke, smoking habit, alcohol intake, regular exercise, apolipoprotein E ε4 carrier status, depression, and research site.
hs-CRP high-sensitivity C-reactive protein, eTIV estimated total intracranial volume, FDR false discovery rate.
aThe number of missing data for each regional brain volume are 93 for fontal cortex, 20 for parietal cortex, 81 for temporal cortex, 33 occipital cortex, 10 for insular cortex, 11 for hippocampus, and 11 for amygdala.
Discussion
In this large cohort study of Japanese older people, the odds ratios for the presence of all-cause dementia and of AD were positively correlated with serum hs-CRP levels. In addition, the temporal cortex volume/eTIV ratio was inversely correlated with serum hs-CRP levels. This significant relationship also was maintained in a sensitivity analysis after excluding patients with dementia.
Though recent reports that vascular inflammation and neuroinflammation are risk factors for AD have accumulated1–3, reports on the association between serum hs-CRP levels and dementia including AD are inconsistent. A recent meta-analysis found that serum hs-CRP was associated with all-cause dementia, but not with AD13. In contrast, the present study showed that elevated levels of serum hs-CRP contributed to an increased odds ratio not only for all-cause dementia, but also for AD alone, and furthermore did not contribute to a significant increased odds ratio for non-AD. The multivariable-adjusted odds ratios for the presence of all-cause dementia and AD for every 1 SD increment in log (serum hs-CRP) were 1.06 (95% confidence interval [CI] 0.97–1.15) and 1.05 (95%CI 0.95–1.15), respectively, which were not significant. The results show that there may not be a linear relationship between hs-CRP and dementia and between hs-CRP and AD, but there is a relationship between elevated hs-CRP and dementia, especially AD. Regarding the association between serum hs-CRP and brain atrophy, previous studies have reported that elevated serum hs-CRP is associated with temporal lobe atrophy17,35, and the present results were consistent with those findings. A longitudinal study using data from the Framingham Offspring Study found no significant association between elevated serum hs-CRP levels and brain atrophy after multivariable adjustment (adjustment factors: age, sex, time to MRI scan, educational history, and APOE ε4 carrier status), and elevated serum hs-CRP levels were significantly associated with temporal lobe atrophy in APOE ε4 carriers18. The present study had a larger sample size than these existing studies, and it included potential confounders not addressed in other studies as adjustment factors.
It is widely known that an inflammatory response occurs in the brains of AD patients. Activation of microglia, immunocompetent cells that release inflammatory cytokines, has been reported to occur around the senile plaque in AD brains36. The association of peripherally derived serum hs-CRP with AD may be explained by the fact that peripheral inflammation transfers into the brain via disruption of the blood–brain barrier37,38. Recent studies have also shown that the migration of immune cells of peripheral origin, such as T cells and neutrophils, into the brain is involved in the brain aging and neurodegeneration39–41. Interestingly, serum hs-CRP itself was reported to increase the permeability of the cerebral blood–brain barrier42. In addition, an association between cerebral small vessel disease (white matter lesions, perivascular space, etc.) and risk of dementia, especially AD, has recently been reported43–46, and vascular risk factors are associated with the development of cerebral small vessel disease47. The background of the involvement of vascular risk factors in AD can be related to vascular inflammation, i.e., inflammatory markers.
The fact that elevated levels of inflammation were associated with temporal cortex atrophy in the present study suggests that the temporal cortex is particularly vulnerable to inflammation among brain regions. Differences in the distribution pattern of inflammatory cytokine receptors may underlie why some brain regions are more vulnerable to inflammation. In AD, the density and expression of inflammatory cytokine receptors has been reported to be increased in neurodegenerative regions, including the prefrontal cortex and medial temporal lobes48. Interestingly, plasma inflammation predicted phenotypic conversion and clinical progression of autosomal dominant frontotemporal lobar degeneration49. It has also been reported that higher serum hs-CRP levels were associated with decreased frontotemporal functional network connectivity in community-dwelling older adults50.
The strengths of this study are the large sample size and the ability to adjust for potential confounding factors. However, there are some limitations. First, because this was a cross-sectional study, the causal relationships among serum hs-CRP, dementia including AD, and brain volume cannot be addressed. In addition, the ability to generalize the results of this study to other racial groups is limited due to differences in lifestyle and background. Longitudinal, world-wide, and basic medical studies are needed to clarify the mechanism of the association between inflammation and AD.
Conclusions
This study’s results suggest that elevated serum hs-CRP levels are associated with greater risk of presence of dementia, especially AD, and of temporal cortex atrophy in a community-dwelling Japanese older population.
Supplementary Information
Acknowledgements
The authors would like to acknowledge the diligent work and contributions of all researchers and investigators in the JPSC-AD Study Group. They would also like to thank the participants for their time in taking part in the JPSC-AD study.
Author contributions
A.T., J.I., and T.N. designed the research; T.O., T.Y., Y.Y., H.S., T.M., Y.T., T.M., T.M., K.O., M.M., K.N., J.I., T.N., and M.T. contributed to the acquisition of data and the critical revision of the manuscript. Y.F., M.S., T.O., and J.H. contributed to the critical revision of the manuscript; A.T., J.I., and S.U. wrote the paper with input from all authors. All authors read and approved the final manuscript.
Funding
This study was supported by the Japan Agency for Medical Research and Development (JP22dk0207053) and Suntory Holdings Limited (Osaka, Japan). The funders had no role in the design of the study, the collection, analysis, and interpretation of data, or the writing of the manuscript.
Data availability
All the processed data generated during this study are provided in the main article and Supplementary Information. The raw data are not openly available to protect the confidentiality of participants and to comply with the terms of participant consent. Requests related to the raw data should be addressed to the principal investigator, Toshiharu Ninomiya (Department of Epidemiology and Public Health, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan) [t.ninomiya.a47@m.kyushu-u.ac.jp], and the Japan Agency for Medical Research and Development.
Competing interests
This study was supported by the Japan Agency for Medical Research and Development (JP22dk0207053) and Suntory Holdings Limited (Osaka, Japan). The funders had no role in the design of the study, the collection, analysis, and interpretation of data, or the writing of the manuscript. Toshiharu Ninomiya received funds from the Japan Agency for Medical Research and Development and Suntory Holdings Limited (Osaka, Japan). The other authors assert that they have no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Jun-ichi Iga, Email: iga.junichi.it@ehime-u.ac.jp.
the JPSC-AD study group:
Takanori Honda, Masato Akiyama, Shigeyuki Nakaji, Koichi Murashita, Kaori Sawada, Shintaro Yokoyama, Naoki Ishizuka, Hiroshi Akasaka, Yasuo Terayama, Hisashi Yonezawa, Junko Takahashi, Moeko Noguchi-Shinohara, Kazuo Iwasa, Sohshi Yuki-Nozaki, Masahito Yamada, Shogyoku Bun, Hidehito Niimura, Ryo Shikimoto, Hisashi Kida, Yasuyo Fukada, Hisanori Kowa, Toshiya Nakano, Kenji Wada, Masafumi Kishi, Tomohisa Ishikawa, Seiji Yuki, Ryuji Fukuhara, Asuka Koyama, Mamoru Hashimoto, Manabu Ikeda, Yoshihiro Kokubo, Kazuhiro Uchida, Midori Esaki, Yasuko Tatewaki, Benjamin Thyreau, Koji Yonemoto, Hisako Yoshida, Kaori Muto, Yusuke Inoue, Izen Ri, Yukihide Momozawa, Chikashi Terao, Michiaki Kubo, and Yutaka Kiyohara
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-57922-1.
References
- 1.Xie J, Van Hoecke L, Vandenbroucke RE. The impact of systemic inflammation on Alzheimer’s disease pathology. Front. Immunol. 2021;12:796867. doi: 10.3389/fimmu.2021.796867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bradburn S, Murgatroyd C, Ray N. Neuroinflammation in mild cognitive impairment and Alzheimer's disease: A meta-analysis. Ageing Res. Rev. 2019;50:1–8. doi: 10.1016/j.arr.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Akiyama H, et al. Inflammation and Alzheimer’s disease. Neurobiol. Aging. 2000;21:383–421. doi: 10.1016/s0197-4580(00)00124-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butchart J, Birch B, Bassily R, Wolfe L, Holmes C. Male sex hormones and systemic inflammation in Alzheimer disease. Alzheimer Dis. Assoc. Disord. 2013;27:153–156. doi: 10.1097/WAD.0b013e318258cd63. [DOI] [PubMed] [Google Scholar]
- 5.Holmes C. Review: systemic inflammation and Alzheimer’s disease. Neuropathol. Appl. Neurobiol. 2013;39:51–68. doi: 10.1111/j.1365-2990.2012.01307.x. [DOI] [PubMed] [Google Scholar]
- 6.Zhang CY, He FF, Su H, Zhang C, Meng XF. Association between chronic kidney disease and Alzheimer’s disease: An update. Metab. Brain Dis. 2020;35:883–894. doi: 10.1007/s11011-020-00561-y. [DOI] [PubMed] [Google Scholar]
- 7.Shah NS, et al. Midlife blood pressure, plasma beta-amyloid, and the risk for Alzheimer disease: The Honolulu Asia Aging Study. Hypertension. 2012;59:780–786. doi: 10.1161/HYPERTENSIONAHA.111.178962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Noguchi-Shinohara M, et al. Diabetes mellitus, elevated hemoglobin A1c, and glycated albumin are associated with the presence of all-cause dementia and Alzheimer’s disease: The JPSC-AD study. J. Alzheimers Dis. 2022;85:235–247. doi: 10.3233/JAD-215153. [DOI] [PubMed] [Google Scholar]
- 9.Kawakami I, Iga JI, Takahashi S, Lin YT, Fujishiro H. Towards an understanding of the pathological basis of senile depression and incident dementia: Implications for treatment. Psychiatry Clin. Neurosci. 2022;76:620–632. doi: 10.1111/pcn.13485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pepys MB, et al. Targeting C-reactive protein for the treatment of cardiovascular disease. Nature. 2006;440:1217–1221. doi: 10.1038/nature04672. [DOI] [PubMed] [Google Scholar]
- 11.O'Bryant SE, et al. Decreased C-reactive protein levels in Alzheimer disease. J. Geriatr. Psychiatry Neurol. 2010;23:49–53. doi: 10.1177/0891988709351832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krance SH, et al. The complement cascade in Alzheimer’s disease: A systematic review and meta-analysis. Mol. Psychiatry. 2021;26:5532–5541. doi: 10.1038/s41380-019-0536-8. [DOI] [PubMed] [Google Scholar]
- 13.Darweesh SKL, et al. Inflammatory markers and the risk of dementia and Alzheimer’s disease: A meta-analysis. Alzheimers Dement. 2018;14:1450–1459. doi: 10.1016/j.jalz.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt R, et al. Early inflammation and dementia: A 25-year follow-up of the Honolulu-Asia Aging Study. Ann. Neurol. 2002;52:168–174. doi: 10.1002/ana.10265. [DOI] [PubMed] [Google Scholar]
- 15.Kravitz BA, Corrada MM, Kawas CH. Elevated C-reactive protein levels are associated with prevalent dementia in the oldest-old. Alzheimers Dement. 2009;5:318–323. doi: 10.1016/j.jalz.2009.04.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gabin JM, Saltvedt I, Tambs K, Holmen J. The association of high sensitivity C-reactive protein and incident Alzheimer disease in patients 60 years and older: The HUNT study, Norway. Immun. Ageing. 2018;15:4. doi: 10.1186/s12979-017-0106-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Conole ELS, et al. DNA methylation and protein markers of chronic inflammation and their associations with brain and cognitive aging. Neurology. 2021;97:e2340–e2352. doi: 10.1212/WNL.0000000000012997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tao Q, et al. Association of chronic low-grade inflammation with risk of Alzheimer disease in ApoE4 carriers. JAMA Netw. Open. 2018;1:e183597. doi: 10.1001/jamanetworkopen.2018.3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thyreau B, et al. Higher-resolution quantification of white matter hypointensities by large-scale transfer learning from 2D images on the JPSC-AD cohort. Hum. Brain Mapp. 2022;43:3998–4012. doi: 10.1002/hbm.25899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maki K, et al. CKD, brain atrophy, and white matter lesion volume: The Japan prospective studies collaboration for aging and dementia. Kidney Med. 2023;5:100593. doi: 10.1016/j.xkme.2022.100593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu Y, et al. Altruistic social activity, depressive symptoms, and brain regional gray matter volume: Voxel-based morphometry analysis from 8695 old adults. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:1789–1797. doi: 10.1093/gerona/glac093. [DOI] [PubMed] [Google Scholar]
- 22.Ninomiya T, et al. Study design and baseline characteristics of a population-based prospective cohort study of dementia in Japan: The Japan Prospective Studies Collaboration for Aging and Dementia (JPSC-AD) Environ. Health Prev. Med. 2020;25:64. doi: 10.1186/s12199-020-00903-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pickering TG, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: A statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111:697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kimura K. Preface: Evidence-based clinical practice guidelines for CKD: an abridged English version. Clin. Exp. Nephrol. 2014;18:339–340. doi: 10.1007/s10157-014-0948-3. [DOI] [PubMed] [Google Scholar]
- 26.Levey AS, et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gottesman RF, et al. Blood pressure and white-matter disease progression in a biethnic cohort: Atherosclerosis risk in communities (ARIC) study. Stroke. 2010;41:3–8. doi: 10.1161/STROKEAHA.109.566992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Momozawa Y, et al. Low-frequency coding variants in CETP and CFB are associated with susceptibility of exudative age-related macular degeneration in the Japanese population. Hum. Mol. Genet. 2016;25:5027–5034. doi: 10.1093/hmg/ddw335. [DOI] [PubMed] [Google Scholar]
- 29.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 3rd Revised Edition (1987).
- 30.McKhann G, et al. Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 31.Jack CR, Jr, et al. The Alzheimer’s disease neuroimaging initiative (ADNI): MRI methods. J. Magn. Reson. Imaging. 2008;27:685–691. doi: 10.1002/jmri.21049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Desikan RS, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31:968–980. doi: 10.1016/j.neuroimage.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 33.Buckner RL, et al. A unified approach for morphometric and functional data analysis in young, old, and demented adults using automated atlas-based head size normalization: Reliability and validation against manual measurement of total intracranial volume. Neuroimage. 2004;23:724–738. doi: 10.1016/j.neuroimage.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 34.Nakazawa T, et al. Multiple-region grey matter atrophy as a predictor for the development of dementia in a community: the Hisayama Study. J. Neurol. Neurosurg. Psychiatry. 2022;93:263–271. doi: 10.1136/jnnp-2021-326611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taki Y, et al. Correlation between high-sensitivity C-reactive protein and brain gray matter volume in healthy elderly subjects. Hum. Brain Mapp. 2013;34:2418–2424. doi: 10.1002/hbm.22073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meda L, et al. Activation of microglial cells by beta-amyloid protein and interferon-gamma. Nature. 1995;374:647–650. doi: 10.1038/374647a0. [DOI] [PubMed] [Google Scholar]
- 37.Jaeger LB, et al. Lipopolysaccharide alters the blood-brain barrier transport of amyloid beta protein: A mechanism for inflammation in the progression of Alzheimer’s disease. Brain Behav. Immun. 2009;23:507–517. doi: 10.1016/j.bbi.2009.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang X, Hussain B, Chang J. Peripheral inflammation and blood-brain barrier disruption: Effects and mechanisms. CNS Neurosci. Ther. 2021;27:36–47. doi: 10.1111/cns.13569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smyth LCD, et al. Neutrophil-vascular interactions drive myeloperoxidase accumulation in the brain in Alzheimer’s disease. Acta Neuropathol. Commun. 2022;10:38. doi: 10.1186/s40478-022-01347-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liston A, Yshii L. T cells drive aging of the brain. Nat. Immunol. 2023;24:12–13. doi: 10.1038/s41590-022-01390-0. [DOI] [PubMed] [Google Scholar]
- 41.Chou ML, et al. Blood-brain crosstalk: the roles of neutrophils, platelets, and neutrophil extracellular traps in neuropathologies. Trends Neurosci. 2023;46:764–779. doi: 10.1016/j.tins.2023.06.005. [DOI] [PubMed] [Google Scholar]
- 42.Hsuchou H, Kastin AJ, Mishra PK, Pan W. C-reactive protein increases BBB permeability: Implications for obesity and neuroinflammation. Cell Physiol. Biochem. 2012;30:1109–1119. doi: 10.1159/000343302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smeijer D, Ikram MK, Hilal S. Enlarged perivascular spaces and dementia: A Systematic review. J. Alzheimers Dis. 2019;72:247–256. doi: 10.3233/JAD-190527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paradise M, et al. Association of dilated perivascular spaces with cognitive decline and incident dementia. Neurology. 2021;96:e1501–e1511. doi: 10.1212/WNL.0000000000011537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gertje EC, van Westen D, Panizo C, Mattsson-Carlgren N, Hansson O. Association of enlarged perivascular spaces and measures of small vessel and Alzheimer disease. Neurology. 2021;96:e193–e202. doi: 10.1212/WNL.0000000000011046. [DOI] [PubMed] [Google Scholar]
- 46.Banerjee G, et al. MRI-visible perivascular space location is associated with Alzheimer's disease independently of amyloid burden. Brain. 2017;140:1107–1116. doi: 10.1093/brain/awx003. [DOI] [PubMed] [Google Scholar]
- 47.Tachibana A, et al. Late-life high blood pressure and enlarged perivascular spaces in the putaminal regions of community-dwelling Japanese older persons (JPSC-AD) J. Geriatr. Psychiatry Neurol. 2023;37(1):61–72. doi: 10.1177/08919887231195235. [DOI] [PubMed] [Google Scholar]
- 48.Hampel H, et al. Pattern of interleukin-6 receptor complex immunoreactivity between cortical regions of rapid autopsy normal and Alzheimer’s disease brain. Eur. Arch. Psychiatry Clin. Neurosci. 2005;255:269–278. doi: 10.1007/s00406-004-0558-2. [DOI] [PubMed] [Google Scholar]
- 49.Asken BM, et al. Plasma inflammation for predicting phenotypic conversion and clinical progression of autosomal dominant frontotemporal lobar degeneration. J. Neurol. Neurosurg. Psychiatry. 2023;94:541–549. doi: 10.1136/jnnp-2022-330866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bang M, et al. Associations of systemic inflammation with frontotemporal functional network connectivity and out-degree social-network size in community-dwelling older adults. Brain Behav. Immun. 2019;79:309–313. doi: 10.1016/j.bbi.2019.01.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the processed data generated during this study are provided in the main article and Supplementary Information. The raw data are not openly available to protect the confidentiality of participants and to comply with the terms of participant consent. Requests related to the raw data should be addressed to the principal investigator, Toshiharu Ninomiya (Department of Epidemiology and Public Health, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan) [t.ninomiya.a47@m.kyushu-u.ac.jp], and the Japan Agency for Medical Research and Development.