Abstract
Background
Healthy lifestyles are effective means to reduce major cardiovascular events. However, little is known about the association of healthy lifestyles with development of carotid atherosclerosis at the early stage of cardiovascular diseases (CVDs).
Methods
We enrolled participants from Fujian province in the China PEACE MPP project. We calculated a healthy lifestyle score by adherence to non-smoking, sufficient physical activity, healthy diet and healthy body mass index. Cox proportional hazards regression models and restricted cubic splines (RCS) were used to explore the association between the healthy lifestyles and rapid progression of carotid plaque.
Results
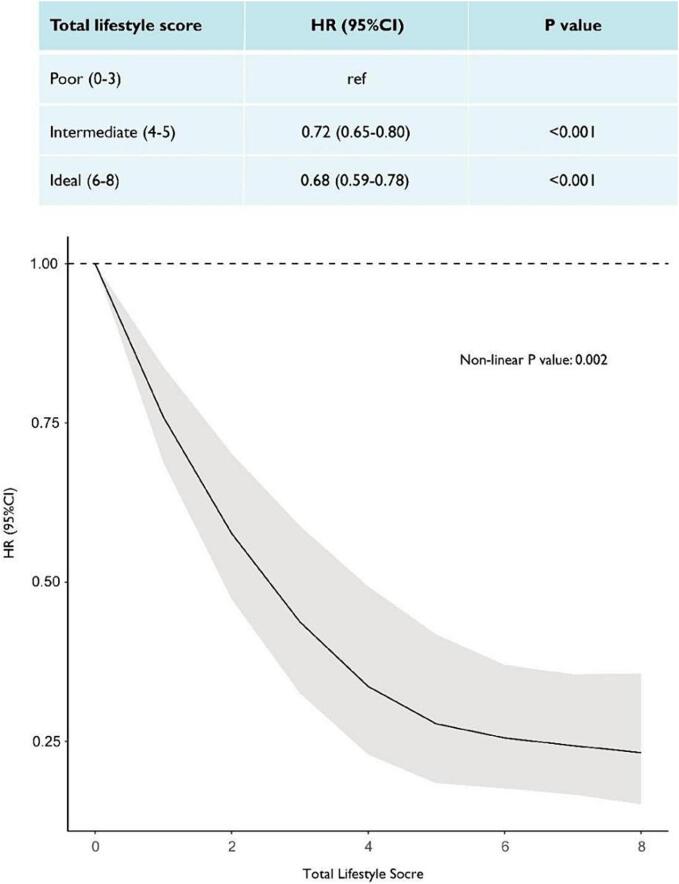
8379 participants were included (mean age: 60.6 ± 8.3 years, 54.6 % female), with a median follow-up of 1.2 years (inter quartile range: 1.0–1.6). RCS showed a significant inverse association between the healthy lifestyle score and progression of carotid plaque. Participants with “intermediate” (HR: 0.72 [95 % confidence interval (CI): 0.65–0.80]) or “ideal” (HR: 0.68 [0.59–0.78]) adherence to healthy lifestyles had a lower risk of progression of carotid plaque compared to those with “poor” adherence. Age, sex, occupation, income, residence type and metabolic status were significant factors influencing the relationship. Farmers benefited more in non-smoking and sufficient physical activity compared to non-farmers, and participants with lower income or without dyslipidaemia benefited more in sufficient physical activity and healthy diet compared to their counterparts (p-for-interaction < 0.05).
Conclusions
Healthy lifestyles were associated with lower risk of progression of carotid plaque in populations with atherosclerosis. Promotion of healthy lifestyles from the early stage of carotid atherosclerosis could reduce the burden of CVDs in China.
Keywords: Healthy lifestyles, Carotid plaque, Atherosclerosis, China
1. Introduction
Cardiovascular disease (CVDs) is the leading cause of deaths in China–approximately 4 million deaths are caused annually by CVDs, accounting for 40 % of overall deaths in the population. (China, NCfCDo, 2021) Atherosclerosis is the main pathological process of most CVDs. (Song et al., 2020) Before cardiovascular events occur, atherosclerosis and sub-clinical atherosclerosis might have begun early in life and remain latent and asymptomatic for long periods. (Hong, 2010, McGill et al., 2000) Carotid plaque (CP), which can be assessed non-invasively using ultrasonography, (Touboul et al., 2004, O'Leary and Bots, 2010) is considered a marker of sub-clinical atherosclerosis. Early detection and early intervention of CP could effectively retard the progress of atherosclerosis, subsequently reducing the burden of CVDs. (Piepoli et al., 2016).
Prior studies reported that healthy lifestyles are proven to be associated with substantially lower risk of ischemic heart disease and stroke. (Lv et al., 2017) These healthy behaviors collectively contribute to reducing systemic inflammation, enhancing endothelial function, and improving metabolic profiles, which are pivotal in slowing the pathophysiological processes underlying atherosclerotic development. Whether the lifestyle factors are associated with reduced risk of early vascular damage is still inconclusive. Prior studies revealed a significantly lower incidence of CP in persons who were never smokers, (Jiang et al., 2010) with higher level of physical activity, (Chen et al., 2022, Walker et al., 2019) having greater consumption of fresh vegetables and fruit, (Blekkenhorst et al., 2018, Zhu et al., 2021) or having a healthy body mass index (BMI). (Botvin Moshe et al., 2020, Imahori et al., 2018) However, these studies were mostly cross-sectional studies, providing insufficient evidence for preventive factors of progression of CP. Moreover, few studies compared the association of healthy lifestyles and CP in population subgroups. It is still unknown that whether there is difference in the association of healthy lifestyles with development of CP across different subgroups of the population in China, such as in people at different socioeconomic status.
Therefore, we used data drawn from China Patient-centered Evaluative Assessment of Cardiac Events (PEACE) Million Persons Project (MPP)-Fujian Project. We aimed to examine the association of healthy lifestyles and rapid progression of CP and investigate the heterogeneity in subgroups of population, which could provide insights for tailored health promotion on CVD prevention in regional China.
2. Methods
2.1. Study design and population
As part of the China PEACE MPP, MPP-Fujian project is a government-funded public health project on screening and management of high-risk subjects with CVD in Fujian Province of China. The study design has been previously published. (Lu et al., 2016) From March 2017 to September 2020, subjects with high CVD risk aged 35 to 75 years were identified through a well-designed screening from 11 rural counties or urban districts in Fujian Province. These high-risk subjects received carotid ultrasonography and a detailed questionnaire survey on lifestyle and medical history at baseline. Since then, they were invited to attend face-to-face follow-up with carotid ultrasonography once a year. We included participants with identified carotid plaque through carotid ultrasonography at baseline, excluding those who reported a history of cardiovascular disease (myocardial infarction, coronary artery bypass graft surgery, percutaneous coronary intervention, or stroke), those who were lost to follow-up, or had missing information on key variables. The project protocol was approved by the central ethics committee at Fuwai Hospital, Beijing, China (Approval No. 2014–574). All enrolled participants provided written informed consent.
2.2. Data collection and variables
Data of four lifestyle factors, namely, smoking, physical activity, diet, and BMI, was collected through the baseline questionnaire interview and anthropometric measurement. The questionnaire was adapted from validated questionnaires used in other large population-based studies. (UKBiobank, 2007, Chen et al., 2011) Briefly, we asked for smoking status (never, former, or current smokers). Ever smokers were further asked for the frequency, type, and amount of cigarette per day. Former smokers were additionally asked for reasons and durations for cessation. Two domains of physical activities (occupational and leisure-time activities), at different intensity (vigorous or moderate), were measured by a standardised questionnaire. For leisure-time activities, participants were asked to choose the most commonly practiced one from Tai-Chi/qigong/leisure walking, jogging/aerobic exercise, ball games, brisk walking/gymnastics/folk dancing, swimming, or other exercise (e.g., mountain hiking, home exercise and rope jumping). The amount of physical activity level was quantified by asking for their exercise frequency and exercise time per week. A food frequency questionnaire (FFQ) was used to collect habitual dietary intake by asking eating frequency of typical food over the previous year. For each food group, the intake frequency was chosen from “never or rarely”, “1–3 days/month”, “1–3 days/week”, “4–6 days/week”, or “daily”. Height and body weight were measured by trained staff using calibrated instruments. BMI was calculated as weight divided by height squared (kg/m2).
According to the metrics of ideal cardiovascular health developed by the American Heart Association (AHA), (Lloyd-Jones et al., 2010) we defined four healthy lifestyles into 3 categories to encompass the entire spectrum of cardiovascular health, poor, intermediate, and ideal, scoring from 0, 1, and 2 accordingly. For non-smoking, ideal is defined as never smoking, whereas intermediate is defined as having quit smoking for ever smokers, and poor is defined by currently smoking. (López-Melgar et al., 2020) For physical activity, those who performed at least 150 min moderate-intensity activities or 75 min vigorous-intensity activities per week were considered ideal, and any level greater than 0 is believed to be better than none, thus defining the intermediate and poor group. (Composing and Editorial Board of Physical Activity Guidelines for Chinese, 2022) For healthy diet, based on the recommendations in the Chinese Dietary Guidelines, (Chinese Nutrition Society, 2022) ideal was defined as a score of at least 3 out of 4 using a healthy diet score calculated by the weekly food intake of four components, including daily intake of fresh fruit, fresh vegetables, whole grains and eating red meat less than seven days per week, whereas intermediate was defined as score 1–2, and poor is defined as score 0. In the case of BMI, intermediate and poor health are defined by the presence of overweight (BMI ≥ 24 kg/m2) or obesity (BMI ≥ 28 kg/m2) respectively. (Department of Disease Control and Prevention MoH, 2006) Thus, the healthy lifestyle score was the sum of the points and ranged between 0 and 8, with higher scores indicating healthier lifestyles. We categorised them into three groups as poor (0–3), intermediate (4–5), and ideal (6–8) accordingly.
Participants’ demographic characteristics and medical history were collected through the questionnaire interview. Blood pressure, fasting blood glucose and blood lipid were measured by uniform equipment and standard operating procedures. Blood pressure was measured twice on the right upper arm after 5 min of rest in a seated position (Omron HEM-7430, Omron Corporation, Japan). Fasting vein blood glucose (FPG) and lipid profile were assessed by a rapid glucose analyser (BeneCheck PD-G001-2; General Life Biotechnology Co., Ltd., Taiwan, China) and a rapid lipid analyzer (CardioChek PA Analyzer; Polymer Technology Systems, Indiana, USA), respectively.
2.3. Ascertainment of outcomes
All carotid ultrasound examinations at baseline and at follow-up visits were obtained by registered ultrasound physicians (certificates issued by Fujian Commission of Health), performing with a 5–12 MHz linear array transducer ultrasound system. Ultrasound assessment technique followed the recommendations in ultrasound measurement guidelines approved by the National Center for Cardiovascular Disease (NCCD). Participants at high CVD risk were examined in a supine position. Registered ultrasound physicians scanned from common carotid artery (CCA) to carotid bifurcation, internal carotid artery, and external carotid artery in transverse and longitudinal sections to check for carotid intima-media thickness (CIMT) and presence of CP. Presence of CP was defined as a region with CIMT ≥ 1.5 mm, protruding into the arterial lumen, or an endoluminal protrusion of more than 0.5 mm or 50 % of the surrounding intima-media thickness value. Atherosclerosis was defined as CIMT ≥ 1.0 mm, or the presence of CP. Progression of CP was defined as occurrence of CP transformation, including increased number of CP or the change of plaque shape from regular type to irregular type (irregular plaque length > 0.4 mm, ulcerated plaque with uneven surface and local tissue defect, or crater-like defect).
2.4. Statistical analysis
We described the characteristics of the participants according to their total score of healthy lifestyles. Categorical variables were summarized as frequencies and percentages, and continuous variables as means ± standard deviations or medians [interquartile range (IQR)]. Chi-square test was used for categorical variables, and one-way ANOVA test (Kruskal-Wallis test when abnormal distributed) was used for continuous variables to compare differences between groups. We also used restricted cubic splines (RCS) with three knots at the 5th, 50th, and 95th centiles to flexibly model the association of total score of the adherence to healthy lifestyles with progression of carotid plaque. Cox proportional hazard models (crude, adjusting for age and sex, or multivariable adjusted models) were used to calculate hazard ratio (HR) and 95 % confidence interval (CI) for the overall and individual healthy lifestyles with progression of carotid plaque. Multivariable adjusted models included most of the demographic and socioeconomic characteristics, i.e., age, sex, occupation, education, annual household income, alcohol use, self-reported history of hypertension, diabetes, and dyslipidaemia, blood pressure, blood glucose, and blood lipid. All models satisfied the proportional hazards assumptions. Stratified analyses were performed to verify the major findings in various subgroups. Competing risk models were adopted as a sensitivity analysis by taking all-cause death as the competing risk event for the progression of carotid plaque. We also conducted a sensitivity analysis by excluding those with less than one year of follow-up. In addition, a mixed-effects Cox regression was conducted incorporating residential location as a random effect. Python 3.9 (Python Software Foundation) and R 4.2.0 (The R Foundation for Statistical Computing, Vienna, Austria) were used for statistical analyses. A two-sided P < 0.05 was considered to be statistically significant.
3. Results
3.1. Participant characteristics
From March 2017 to September 2020, we enrolled 9565 individuals with carotid plaque identified in ultrasound examination at baseline. We excluded those with established CVD history (n = 479), those died or lost to follow-up (n = 250), and those with missing information on lifestyle factors (n = 457). Finally, a total of 8379 participants were included in the analysis (Appendix Figure S1).
Among the included participants, 2115(25.2 %) were defined “poor” in adherence to healthy lifestyles, 4499 (53.7 %) were “intermediate”, and 1765 (21.1 %) were “ideal”. Participants with “ideal” adherence to healthy lifestyles were more likely to be female, elders, non-farmers, with higher education and income, and had self-reported dyslipidemia, while less likely to currently married, currently drinking alcohol, and hypertensive or diabetic (Table 1). For individual lifestyle factors, 6115 (73.0 %) had “ideal” non-smoking status, 3121 (37.2 %) had “ideal” sufficient physical activity, and 1347 (16.1 %) had “ideal” healthy diet, 4761 (56.8 %) had “ideal” healthy BMI (Appendix 1, Table S1).
Table 1.
Descriptive statistics of participant characteristics by healthy lifestyle scores among adults in Fujian Province, China, 2017–2020.
|
Overall M ± SD or n(%) |
Poor (0–3) M ± SD or n(%) |
Intermediate (4–5) M ± SD or n(%) |
Ideal (6–8) M ± SD or n(%) |
P value | |
|---|---|---|---|---|---|
| Total | 8379 | 2115 | 4499 | 1765 | |
| Sex: female | 4575 (54.6) | 452 (21.4) | 2812 (62.5) | 1311 (74.3) | <0.001 |
| Age, year | 60.6 ± 8.3 | 60.1 ± 8.6 | 60.6 ± 8.3 | 61.3 ± 8.0 | <0.001 |
| 35–44 | 246 (2.9) | 75 (3.5) | 135 (3.0) | 36 (2.0) | |
| 45–54 | 1880 (22.4) | 542 (25.6) | 990 (22.0) | 348 (19.7) | |
| 55–64 | 3136 (37.4) | 752 (35.6) | 1701 (37.8) | 683 (38.7) | |
| 65–75 | 3117 (37.2) | 746 (35.3) | 1673 (37.2) | 698 (39.5) | |
| Occupation: Farmer | 2851 (34.0) | 878 (41.5) | 1652 (36.7) | 321 (18.2) | <0.001 |
| Education: High school or above | 2190 (26.1) | 542 (25.6) | 1009 (22.4) | 639 (36.2) | <0.001 |
| Annual household income: >50 000 yuan | 2451 (29.3) | 569 (26.9) | 1188 (26.4) | 694 (39.3) | <0.001 |
| Marriage: currently married | 7568 (90.3) | 1988 (94.0) | 4027 (89.5) | 1553 (88.0) | <0.001 |
| Alcohol use: currently drinking | 1994 (23.8) | 771 (36.5) | 936 (20.8) | 287 (16.3) | <0.001 |
| Hypertension | 5982 (71.4) | 1612 (76.2) | 3270 (72.7) | 1100 (62.3) | <0.001 |
| SBP, mmHg | 146.4 ± 22.6 | 147.8 ± 21.9 | 147.6 ± 22.5 | 141.8 ± 23.2 | <0.001 |
| DBP, mmHg | 85.4 ± 12.5 | 88.1 ± 12.5 | 85.6 ± 12.4 | 81.9 ± 12.1 | <0.001 |
| Diabetes | 1904 (22.7) | 504 (23.8) | 1003 (22.3) | 397 (22.5) | 0.368 |
| Fasting blood glucose, mmol/L | 6.32 ± 1.82 | 6.39 ± 1.76 | 6.31 ± 1.84 | 6.26 ± 1.85 | 0.103 |
| Dyslipidemia | 2816 (33.6) | 542 (25.6) | 1479 (32.9) | 795 (45.0) | <0.001 |
| TC, mmol/L | 5.39 ± 1.29 | 5.12 ± 1.25 | 5.43 ± 1.27 | 5.61 ± 1.34 | <0.001 |
3.2. Healthy lifestyles and progression of carotid plaque
During a median follow-up time 1.2 years (IQR: 1.0–1.6 years), there were 2236 (26.7 %) observed progression of carotid plaque, among which 650 (30.7 %) were from participants who were “poor” in adherence to healthy lifestyles, 1156 (25.7 %) who were “intermediate”, and 430 (24.4 %) who were “ideal”. When the healthy lifestyle behaviours were combined, according to the results of restricted cubic spline analysis, the total score of healthy lifestyles were inversely associated with the progression of carotid plaque in a non-linear manner (p < 0.001, Fig. 1). This association was non-linear, with the curve being steeper in the 0–5 score interval than in the 5–8 score interval (p for nonlinearity = 0.002). Compared with the participants defined “poor”, those with “intermediate” (HR: 0.72 [95 % confidence interval (CI): 0.65–0.80], p < 0.001) or “ideal” (HR: 0.68 [0.59–0.78], p < 0.001) adherence to healthy lifestyles were less likely to had progression of carotid plaque (Fig. 1; Appendix 1, Table S2). Similar findings were observed in the competing risk models and other sensitivity analyses (Appendix 1, Table S3-5, Figure S3).
Fig. 1.
Association between total healthy lifestyle score and carotid plaque progression using restricted cubic splines among adults in Fujian Province, China, 2017–2020. * Models were adjusted for age, sex, occupation, education, annual household income, residence type, alcohol use, hypertension, diabetes, dyslipidaemia blood pressure, fasting blood glucose, and blood lipid.
For individual healthy lifestyles that were used to fit multivariable adjusted Cox regression models separately, lower risks of progression of carotid plaque were observed in “intermediate” (HR: 0.42 [0.35–0.51], p < 0.001) and “ideal” sufficient physical activity (HR: 0.37 [0.30–0.45], p < 0.001), “intermediate” (HR: 0.52 [0.45–0.60], p < 0.001) and “ideal” healthy diet (HR: 0.52 [0.44–0.63], p < 0.001). “Ideal” non-smoking status was associated with lower risk of development of carotid plaque in crude models (HR: 0.83 [0.76–0.92], p < 0.001), while the correlation was insignificant after multivariable adjustment. No significant results were observed in healthy BMI with or without adjustment (Table 2).
Table 2.
Hazard ratios for carotid plaque progression by healthy lifestyle factors among adults in Fujian Province, China, 2017–2020.
|
Non-smoking |
Sufficient Physical activity |
Healthy diet |
Healthy BMI |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR (95 %CI) | P value | HR (95 %CI) | P value | HR (95 %CI) | P value | HR (95 %CI) | P value | |||||
| Model 1: no adjustment | ||||||||||||
| Poor | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | ||||||||
| Intermediate | 0.89(0.72–1.11) | 0.308 | 0.41(0.35–0.49) | <0.001 | 0.47(0.41–0.54) | <0.001 | 0.94(0.78–1.14) | 0.549 | ||||
| Ideal | 0.83(0.76–0.92) | <0.001 | 0.30(0.25–0.36) | <0.001 | 0.37(0.31–0.43) | <0.001 | 0.97(0.80–1.16) | 0.722 | ||||
| Model 2: adjusted for age and sex | ||||||||||||
| Poor | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | ||||||||
| Intermediate | 0.87(0.70–1.09) | 0.227 | 0.40(0.34–0.48) | <0.001 | 0.47(0.41–0.54) | <0.001 | 0.95(0.78–1.14) | 0.562 | ||||
| Ideal | 0.90(0.80–1.02) | 0.088 | 0.29(0.24–0.35) | <0.001 | 0.38(0.32–0.45) | <0.001 | 0.96(0.80–1.15) | 0.663 | ||||
| * Model 3: multivariable adjusted model | ||||||||||||
| Poor | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | ||||||||
| Intermediate | 0.88(0.71–1.10) | 0.276 | 0.33(0.28–0.40) | <0.001 | 0.43(0.37–0.49) | <0.001 | 0.96(0.80–1.17) | 0.707 | ||||
| Ideal | 0.92(0.82–1.03) | 0.149 | 0.28(0.23–0.33) | <0.001 | 0.42(0.35–0.49) | <0.001 | 0.97(0.81–1.17) | 0.746 | ||||
| # Model 4: multivariable adjusted model | ||||||||||||
| Poor | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | ||||||||
| Intermediate | 0.93(0.75–1.17) | 0.546 | 0.42(0.35–0.51) | <0.001 | 0.52(0.45–0.60) | <0.001 | 0.96(0.79–1.16) | 0.679 | ||||
| Ideal | 0.95(0.85–1.07) | 0.417 | 0.37(0.30–0.45) | <0.001 | 0.52(0.44–0.63) | <0.001 | 0.95(0.79–1.15) | 0.594 | ||||
*Model 3: adjusted for age, sex, occupation, education, annual household income, residence type, and alcohol use.
# Model 4: adjusted for hypertension, diabetes, dyslipidaemia, blood pressure, fasting blood glucose, and blood lipid, based on model 3.
3.3. Stratified analyses by potential effect modifiers
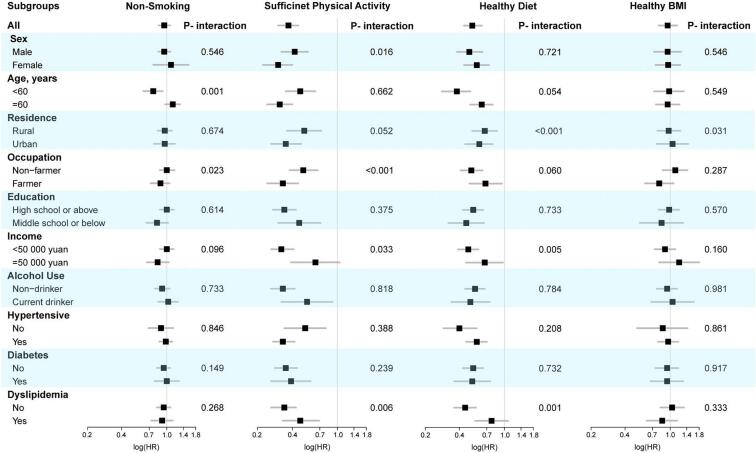
Stratified analyses showed that the strength of the association between healthy lifestyles and progress of CP varied among population subgroups (Appendix1, Figure S2). Among the participants who had deal adherence to healthy lifestyles, female participants benefited more in progression of carotid plaque compared to the males (females, HR: 0.30 [0.22–0.40]; males, HR:0.42 [0.32–0.55]; p for interaction = 0.016) when adhering to sufficient physical activity. Participants age below 60 benefited more compared to elders when adhering to non-smoking (aged below 60, HR: 0.76 [0.62–0.92]; aged above 60, HR:1.13 [0.97–1.31]; p for interaction < 0.001). Rural citizens benefited more compared to urban residents when adhering to healthy diet (rural, HR:0.60 [0.45–0.79]; urban, HR: 0.67 [0.52–0.86]; p for interaction < 0.001). Similarly, farmers benefited more in sufficient physical activity compared to non-farmers. Participants with lower income or without dyslipidaemia benefited more in sufficient physical activity and healthy diet compared to their counterparts (Fig. 2, Appendix1, Table S6,7).
Fig. 2.
Stratified analyses by potential effect modifiers for the association of four healthy lifestyles with progression of carotid plaque among adults in Fujian Province, China, 2017–2020. Compared with the participants who were “poor”and “ideal” adherence to healthy lifestyles. * Models were adjusted for age, sex, occupation, education, annual household income, residence type, alcohol use, hypertension, diabetes, dyslipidaemia blood pressure, fasting blood glucose, and blood lipid.
4. Discussion
In this study, we found that among people with carotid atherosclerosis, only one fifth had an ideal adherence to four healthy lifestyles, including non-smoking, sufficient physical activity, healthy diet and healthy BMI. Compared to individuals with poor adherence to four healthy lifestyles, those with intermediate adherence and ideal adherence had 28 % and 32 % lower risk in progression of carotid plaque respectively. The association was non-linear, and was stronger in some population subgroups such as females, adults aged below 60, rural residents.
To our knowledge, this paper is one of the few studies comprehensively analysed the combined effect of multiple lifestyle factors on progression of atherosclerosis. A number of prior studies have investigated the association between lifestyles and atherosclerosis, while most of them usually focused on one or two individual lifestyle factors and defined them dichotomously. (Blekkenhorst et al., 2018, Kiechl et al., 1994, Mury et al., 2020) In comparison, our study defined each lifestyle into 3 categories to encompass the entire spectrum of cardiovascular health and attached importance on the overall performance of multiple lifestyles by calculating an overall lifestyle score. We exhibited a considerably proportional reduction in risk of atherosclerosis progression in those with ideal adherence to four healthy lifestyles. Although some individual healthy lifestyles showed insignificant results, nevertheless, the combined effects of multiple healthy lifestyles were overwhelming, which highlighted the necessity of integrated interventions.
On the basis, we further verified that the association between overall lifestyle score and the atherosclerosis progression were non-linear. Compared with individuals having an intermediate adherence to four healthy lifestyles, those with poor adherence would gain much greater risk reduction by minimal lifestyle modification. The non-linear association might be related to clustering effect of multiple healthy lifestyles in population which have been verified in prior studies. (Schuit et al., 2002, Zhang et al., 2021) This finding can yet be regarded as a kind of encouragement for people with poor adherence to healthy lifestyles.
It is worth noting that, this study filled the gaps about prevention of atherosclerosis by providing evidence on the health effects of lifestyles in individuals who had already have atherosclerosis. Prior studies had revealed that healthy lifestyles could stop early formation of carotid plaque in healthy populations. In one large-scale cohort study of menopausal women, Wang D et al found the lower incidence of carotid plaque was associated with non-smoking, healthy dietary patterns, and higher level of physical activity. (Wang et al., 2018) Another study in China showed that a healthy BMI was associated with lower presence of carotid plaque. (Ma et al., 2022) In this study, we detected the effects of healthy lifestyles in a patient population with established atherosclerosis and clearly showed the healthy lifestyles were still on working. These health effects persist throughout one’s life cycle, in sickness or in health.
What’s more, we observed that the protective effects of healthy lifestyles were stronger in some certain population subgroups, which is consistent with prior reports. (Chen et al., 2022) Age plays a key role in the progression of atherosclerosis. Aging physiology and cardiovascular pathophysiology may have common biological pathways, which explain the interaction between age and risk of atherosclerosis progression. The sex differences in risk factors for atherosclerosis have also been discussed in prior studies, (Cheng et al., 2022) which explains the interaction in our study. Individuals in different socio-economic status (SES) have different adherence to healthy lifestyles. In general, people of low SES, such as those living in rural areas, having low income or education, tend to have a lower adherence to healthy lifestyles. (Zhang et al., 2021) This may be attributed to the interaction of socio-economic factors in our study. However, the exact mechanism of these interaction is still unclear, and should be further investigated in well-designed population-based prospective studies.
Our findings have significant policy implications for primary prevention of CVDs. First, instead of relying solely on medication, lifestyle improvement programs should be more actively offered to patients who have had atherosclerotic plaque. It is never too late to start the lifestyle modification even though atherosclerotic plaque has been formed. Second, integrated health education and health promotion programs would be more effective and practical ways to maximize the impact of healthy lifestyle on stopping the atherosclerosis progression. Particular attention should be attached to those with poorer adherence with more room for improvement. Third, the results of the stratified analysis showed that similar lifestyle pattern can be associated with different risk of plaque progression in different populations. In a large country like China, customized interventions for various subgroups, such as focused improvements for males, elderly adults, or rural residents should be further promoted.
The study also has some limitations. First of all, we assumed four healthy lifestyles with equal weight when calculating the overall lifestyle score, which may lead to some bias. Second, some recall bias was inevitable since the lifestyle factors were self-reported; although we used standardized electronic questionnaires with real-time logic check. Third, residual confounding due to unmeasured or unknown factors cannot be completely ruled out, for example, we did not collect detailed information on cardiovascular medications, HbA1C, and Fitness. Fourth, there is a very small proportion of loss of follow-up and incomplete data, which might lead to a slight underestimation of the atherosclerosis progression, but probably not biases in the correlation analyses. Last, given the high-quality data source, rigorous statistical analyses, and proper handling of confounders, the internal validity of the findings can be guaranteed. However, the lacking diversity of our population might limit our findings when generalizing to population in other countries or regions.
In conclusion, healthy lifestyles were associated with lower risk of progression of carotid plaque in populations with established atherosclerosis. Promotion of healthy lifestyles from the early stage of carotid atherosclerosis could reduce the burden of CVDs in China.
5. Lay summary
Healthy lifestyles are associated with a lower risk of progression of carotid plaque in populations with atherosclerosis. Participants with intermediate or ideal adherence to healthy lifestyles had a lower risk of progression of carotid plaque compared to those with poor adherence. The study concluded that promoting healthy lifestyles from the early stage of carotid atherosclerosis could reduce the burden of cardiovascular diseases in China.
6. Previous presentations of the work presented in the article
The study design has been previously published in BMJ open (Ref. (Lu et al., 2016). The results in this article have not been presented or disseminated in any form prior to its submission to Preventive Medicine Reports.
Funding
This work was supported by the Fujian Province Pilot Project (2020Y0060), the Fujian Provincial Health Youth Project (2020QNB017), the Construction of Fujian Provincial Scientific and Technological Innovation Platform (2019Y2001), the Chinese Academy of Medical Sciences Innovation Fund for Medical Science (2021-I2M-1–011), the National High Level Hospital Clinical Research Funding (2022-GSP-GG-4), the Ministry of Finance of China and National Health Commission of China, and the 111 Project from the Ministry of Education of China (B16005).
CRediT authorship contribution statement
Xin Fang: Writing – review & editing, Writing – original draft, Project administration, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Xingyi Zhang: Writing – review & editing, Writing – original draft, Formal analysis, Data curation, Conceptualization. Ze Yang: Project administration, Investigation, Data curation. Ling Yu: . Kaiyang Lin: Writing – review & editing, Data curation, Conceptualization. Tiehui Chen: Writing – review & editing, Data curation, Conceptualization. Wenling Zhong: Writing – review & editing, Project administration, Funding acquisition, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We appreciate the multiple contributions made by study teams at the Fujian Provincial Center for Disease Control and Prevention, National Center for Cardiovascular Diseases (NCCD), and all the staff from the 11 project counties in Fujian province for their work and support on providing the data for this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2024.102697.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Blekkenhorst L.C., Bondonno C.P., Lewis J.R., et al. Cruciferous and total vegetable intakes are inversely associated with subclinical atherosclerosis in older adult women. J. Am. Heart Assoc. 2018;7(8) doi: 10.1161/JAHA.117.008391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botvin Moshe C., Haratz S., Ravona-Springer R., et al. Long-term trajectories of BMI predict carotid stiffness and plaque volume in type 2 diabetes older adults: a cohort study. Cardiovasc. Diabetol. 2020;19(1):138. doi: 10.1186/s12933-020-01104-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Bi Y., Su J., et al. Physical activity and carotid atherosclerosis risk reduction in population with high risk for cardiovascular diseases: a cross-sectional study. BMC Public Health. 2022;22(1):250. doi: 10.1186/s12889-022-12582-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z., Chen J., Collins R., et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int. J. Epidemiol. 2011;40(6):1652–1666. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Q., Zhou D., Wang J., et al. Sex-specific risk factors of carotid atherosclerosis progression in a high-risk population of cardiovascular disease. Clin. Cardiol. 2022 doi: 10.1002/clc.23931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- China, NCfCDo. Annual Report on Cardiovascular health and diseases in China 2021. Beijing, China: Science Press; 2022.
- Chinese Nutrition Society . People's Medical Publishing House; Beijing: 2022. The chinese dietary guidelines. [Google Scholar]
- Composing and Editorial Board of Physical Activity Guidelines for Chinese. Physical activity guidelines for Chinese. Chinese Journal of Epidemiology 2022; 43(1): 5-6. [DOI] [PubMed]
- Department of Disease Control and Prevention MoH . People’s Medical Publishing House; Beijing, China: 2006. People's Republic of China, chinese adults prevention and control of overweight and obesity guidelines. [Google Scholar]
- Hong Y.M. Atherosclerotic cardiovascular disease beginning in childhood. Korean Circulation Journal. 2010;40(1):1–9. doi: 10.4070/kcj.2010.40.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imahori Y., Mathiesen E.B., Leon D.A., et al. The contribution of obesity to carotid atherosclerotic plaque burden in a general population sample in Norway: the Tromsø study. Atherosclerosis. 2018;273:15–20. doi: 10.1016/j.atherosclerosis.2018.04.014. [DOI] [PubMed] [Google Scholar]
- Jiang C.Q., Xu L., Lin J.M., et al. Dose-response relationship between smoking status and carotid atherosclerosis. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi. 2010;31(9):983–987. [PubMed] [Google Scholar]
- Kiechl S., Willeit J., Egger G., Oberhollenzer M., Aichner F. Alcohol consumption and carotid atherosclerosis: evidence of dose-dependent atherogenic and antiatherogenic effects. Results from the Bruneck Study. Stroke. 1994;25(8):1593–1598. doi: 10.1161/01.str.25.8.1593. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D.M., Hong Y., Labarthe D., et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- López-Melgar B., Fernández-Friera L., Oliva B., et al. Short-term progression of multiterritorial subclinical atherosclerosis. J. Am. Coll. Cardiol. 2020;75(14):1617–1627. doi: 10.1016/j.jacc.2020.02.026. [DOI] [PubMed] [Google Scholar]
- Lu J., Xuan S., Downing N.S., et al. Protocol for the China PEACE (patient-centered evaluative assessment of cardiac events) million persons project pilot. BMJ Open. 2016;6(1):e010200. doi: 10.1136/bmjopen-2015-010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv J., Yu C., Guo Y., et al. Adherence to healthy lifestyle and cardiovascular diseases in the chinese population. J. Am. Coll. Cardiol. 2017;69(9):1116–1125. doi: 10.1016/j.jacc.2016.11.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma X., Chen L., Hu W., He L. Association between a body shape index and subclinical Carotid atherosclerosis in population free of cardiovascular and cerebrovascular diseases. J. Atheroscler. Thromb. 2022;29(8):1140–1152. doi: 10.5551/jat.62988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGill H.C., Jr., McMahan C.A., Herderick E.E., Malcom G.T., Tracy R.E., Strong J.P. Origin of atherosclerosis in childhood and adolescence. Am. J. Clin. Nutr. 2000;72(5 Suppl):1307s–s1315. doi: 10.1093/ajcn/72.5.1307s. [DOI] [PubMed] [Google Scholar]
- Mury P., Mura M., Della-Schiava N., et al. Association between physical activity and sedentary behaviour on carotid atherosclerotic plaques: an epidemiological and histological study in 90 asymptomatic patients. Br. J. Sports Med. 2020;54(8):469–474. doi: 10.1136/bjsports-2018-099677. [DOI] [PubMed] [Google Scholar]
- O'Leary D.H., Bots M.L. Imaging of atherosclerosis: carotid intima-media thickness. Eur. Heart J. 2010;31(14):1682–1689. doi: 10.1093/eurheartj/ehq185. [DOI] [PubMed] [Google Scholar]
- Piepoli M.F., Hoes A.W., Agewall S., et al. 2016 european guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and Other Societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & rehabilitation (EACPR) Atherosclerosis. 2016;252:207–274. doi: 10.1016/j.atherosclerosis.2016.05.037. [DOI] [PubMed] [Google Scholar]
- Schuit A.J., van Loon A.J., Tijhuis M., Ocke M. Clustering of lifestyle risk factors in a general adult population. Prev. Med. 2002;35(3):219–224. doi: 10.1006/pmed.2002.1064. [DOI] [PubMed] [Google Scholar]
- Song P., Fang Z., Wang H., et al. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study. Lancet Glob. Health. 2020;8(5):e721–e729. doi: 10.1016/S2214-109X(20)30117-0. [DOI] [PubMed] [Google Scholar]
- Touboul, P.J., Hennerici, M.G., Meairs. S. et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovascular diseases (Basel, Switzerland) 2012; 34(4): 290-6. [DOI] [PMC free article] [PubMed]
- UKBiobank. Protocol for a large-scale prospective epidemiological resource. 2007. https://www.ukbiobank.ac.uk/media/gnkeyh2q/study-rationale.pdf (accessed 20 March 2021).
- Walker T.J., Heredia N.I., Lee M., et al. The combined effect of physical activity and sedentary behavior on subclinical atherosclerosis: a cross-sectional study among Mexican Americans. BMC Public Health. 2019;19(1):161. doi: 10.1186/s12889-019-6439-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Jackson E.A., Karvonen-Gutierrez C.A., et al. Healthy lifestyle during the midlife is prospectively associated with less subclinical carotid atherosclerosis: the study of women's health across the nation. J. Am. Heart Assoc. 2018;7(23):e010405. doi: 10.1161/JAHA.118.010405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X., Lu, J., Wu, C. et al. Healthy lifestyle behaviours and all-cause and cardiovascular mortality among 0.9 million Chinese adults. The international journal of behavioral nutrition and physical activity 2021; 18(1): 162. [DOI] [PMC free article] [PubMed]
- Zhu F., Qin Y., Bi Y., et al. Fresh vegetable and fruit consumption and carotid atherosclerosis in high-cardiovascular-risk population: a cross-sectional study in Jiangsu, China. Cad. Saude Publica. 2021;37(5):e00033020. doi: 10.1590/01021-311X00033020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.