Abstract
Introduction
Lemmel's syndrome is a rare disease presenting with obstructive jaundice, secondary to common bile duct compression by duodenal diverticulum.
Presentation of case
A 79-year-old female was admitted to our emergency department with cholangitis and obstructive jaundice, due to choledocal compression by two periampullary diverticula, with major papilla opening near the biggest one (periampullary diverticulum type III). Endoscopic retrograde cholangiopancreatography didn't succeed sphincterotomy, therefore laparoscopic rendez-vous was performed.
Discussion
This case is an example of an unusual cause of obstructive jaundice, which should be mentioned along with choledocolithiasis and biliary or ampullary neoplasms, in order to avoid delay in diagnosis and management.
Conclusion
The commonest treatment of Lemmel's syndrome reported in literature is ERCP with sphincterotomy, but when endoscopic management fails, interventional radiology and surgery should also be considered.
Keywords: Lemmel'syndrome, Obstructive jaundice, Sphinterectomy, Rendez-vous
Highlights
-
•
Lemmel's syndrome is a rare disease presenting with obstructive jaundice, secondary to common bile duct compression by duodenal diverticulum
-
•
In a 79-year-old female with cholangitis and obstructive jaundice, due to choledocal compression by two periampullary diverticula, endoscopic retrograde cholangiopancreatography didn’t succeed sphincterotomy, therefore laparoscopic rendez-vous was performed
-
•
When endoscopic management fails, interventional radiology and surgery should also be considered.
1. Introduction
In Lemmel's syndrome, duodenal diverticulum compresses the distal tract of common bile duct causing obstructive jaundice [1]. Due to its rarity, this syndrome should be suspected in patients with direct hyperbilirubinemia, after ruling out choledocholithiasis and pancreato-biliary or duodenal tumors [2]. The initial management is endoscopic retrograde cholangiopancreatography (ERCP), but in case of failure, interventional radiology and surgery can be an option [3].
We present the case of a 79-year-old female admitted to the emergency department with cholangitis, secondary to periampullary diverticulum (PAD type III e.g. major papilla opening near diverticulum). The endoscopic treatment failed and rendez-vous technique was performed.
2. Case description
A 79-year-old female was admitted to the emergency department with abdominal pain in right hypochondrium, obstructive jaundice and fever. Her past medical history were hypertension and Hashimoto's thyroiditis; she also referred familiarity for pancreatic cancer (younger sister). Blood exams revealed an increased total bilirubin (5.9 mg/dL with direct bilirubin of 5.3 mg/dL), elevated liver enzymes (AST 135 U/L, ALT 223 U/L) and cholestatic pattern (ALP 491 U/L, GGT 595 U/L); she underwent abdominal CT-scan, that showed dilated intra and extrahepatic bile ducts, idropic gallbladder, a dilatated PPD without apparent solid lesions (Fig. 1).
Fig. 1.

CT-scan.
The patient was then admitted to our General Surgery unit for further investigations.
During hospital stay she underwent:
-
•
tumoral markers measurement (CA19–9 negative)
-
•
MRCP, which revealed the presence of dilated hepatocholedocus (14 mm), lithiasis of its middle part and compression of its distal end by iuxta-ampullary diverticulum located in the medial wall of second part of duodenum (diameter 45 mm) (Fig. 2).
Fig. 2.
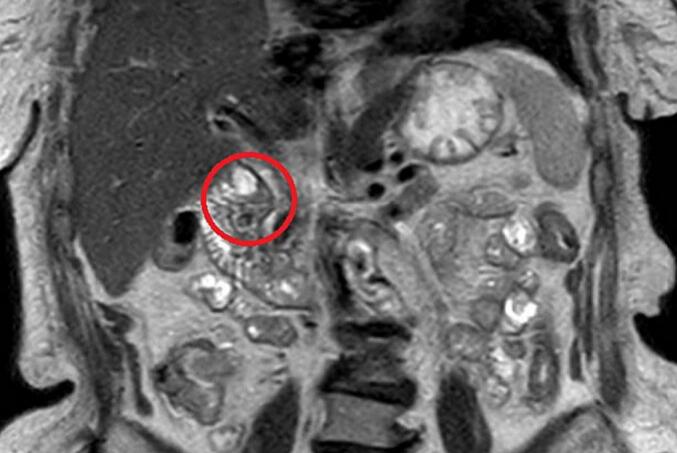
MRI image.
Moreover, to definitely rule-out periampullary tumor, EUS was performed. Endoscopic ultrasound showed two diverticula in second duodenal portion, ampulla located near the biggest one, and compression with consequent dilatation of biliary and Wirsung ducts (PAD type III).
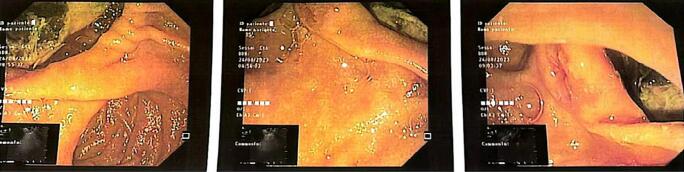
ERCP was attempted but didn't achieved sphincterotomy, due to difficult cannulation of papilla (Fig. 3).
Fig. 3.
Endoscopic images.
Therefore, a combined approach with laparoscopic cholecistectomy and ERCP was performed, with so-called rendez-vous technique. Intraoperative cholangiography confirmed the radiological diagnose of concomitant common bile duct stones: sphincterotomy and basket catheter were used, achieving effective clearance and safe common bile duct stone removal as confirmed by post-procedural cholangiography.
The postoperative course was uneventful and patient was discharged on postoperative day 2. After 6 months follow-up in out-patient setting, no recurrence of jaundice or cholangitis was observed: in particular, routine laboratory exams, including liver function tests, were within normal range.
3. Discussion
Duodenum is the second most common site of diverticula, after colon. Acquired or extraluminal diverticula are outpouching of mucosa and muscolaris mucosa through duodenal wall, in opposition to rarest intraluminal or congenital diverticula. Most diverticula are located within 2 cm of papilla of Vater (so called periampullary diverticula) and are usually incidental findings during upper endoscopy; in fact, only 5 % of them presents with symptoms, such as diverticulitis, ulceration, bleeding or jaundice. Literature provides several classification of periampullary duodenal diverticula [[1], [2], [3]]: Boix classification, published in 2006, is adopted in our center and classifies PAD as follows: PAD type I, with major papilla opening inside the diverticulum; PAD type II, opening in the margin of the diverticulum; and PAD type III, opening near the diverticulum. The main causes of obstructive jaundice are choledocholithiasis and pancreato-biliary or periampullary tumors [4]. Lemmel's syndrome is an uncommon form of jaundice, caused by biliary duct compression by periampullary diverticulum [[5], [6], [7]].
A recent literature review reports that hyperbilirubinemia is the most common laboratory abnormality in Lemmel's syndrome, followed by elevation of hepatic enzymes, alkaline phosphatase and gamma-glutamyl transferase; thirdly, elevation of C reactive protein is present [8,9]. Imaging is pivotal to diagnose Lemmel's syndrome accurately. Ultrasound could reveal biliary tract dilatation but cannot identify duodenal diverticula, which could be assessed by CT, MRI or ERCP. In CT and MRI, periampullary diverticula could appear as cavitary lesions of the second part of duodenum, arising from its medial wall, as in our case [10]. Regarding ERCP, literature report that lateral-vision endoscope during procedure is considered as the gold standard for the diagnosis [7]; ERCP is also the simplest treatment of Lemmel's syndrome described in literature [4,10]. Yet, cannulation of papilla can be difficult, as in our case; rendez-vous techniques can be an alternative, since they facilitate cannulation of papilla with guide wire insertion during laparoscopic cholecystectomy, or previous PTBD positioning in patients who already had cholecystectomy. Currently, there is no consensus about optimal surgical technique [7]. Diverticulum resection, duodenectomy, Roux en Y hepaticojejunostomy with or without duodenojejunostomy have also been reported, but should be limited only to symptomatic cases after failure of endoscopic and conservative treatments.
4. Conclusion
In patients with cholangitis, in absence of choledocholithiasis or neoplastic obstruction, Lemmel's syndrome has to be considered to avoid misdiagnosis or overtreatment. The presence of periampullary diverticula can cause difficult cannulation of major papilla during ERCP. In the cases in which endoscopic treatment fails, rendez-vous techniques can be an alternative.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Methods
The paper has been written according to SCARE criteria [11]. Consent to the processing of data for scientific purposes is requested and signed at the time of admission and kept in the medical record; the authors confirm that the patient's parents have signed consent to the publication of the data.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Disclosure statement
The authors have nothing to disclose.
Ethical approval
In our institute, the approval of the ethics committee for the retrospective analysis of a clinical case report is not required.
Sources of funding
No fundings were used.
Author contribution
William Sergi: design of work and manuscript writing.
Annarita Libia: co-author.
Elisa Stasi, Stefano D'Ugo, Norma Depalma: data collection.
Marcello Spampinato: supervisors.
Guarantor
Marcello Spampinato.
Registration of research studies
The submitted case report is not a research study.
Declaration of competing interest
The authors declare no conflict of interests.
References
- 1.Lobo D.N., Balfour T.W., Iftikhar S.Y. Periampullary diverticula: consequences of failed ERCP. Ann. R. Coll. Surg. Engl. 1998 Sep;80(5):326–331. PMID: 9849331; PMCID: PMC2503106. [PMC free article] [PubMed] [Google Scholar]
- 2.Boix J., Lorenzo-Zúñiga V., Añaños F., Domènech E., Morillas R.M., Gassull M.A. Impact of periampullary duodenal diverticula at endoscopic retrograde cholangiopancreatography: a proposed classification of periampullary duodenal diverticula. Surg. Laparosc. Endosc. Percutan. Tech. 2006 Aug;16(4):208–211. doi: 10.1097/00129689-200608000-00002. (PMID: 16921297) [DOI] [PubMed] [Google Scholar]
- 3.Yue P., Zhu K.X., Wang H.P., Meng W.B., Liu J.K., Zhang L., Zhu X.L., Zhang H., Miao L., Wang Z.F., Zhou W.C., Suzuki A., Tanaka K., Li X. Clinical significance of different periampullary diverticulum classifications for endoscopic retrograde cholangiopancreatography cannulation. World J. Gastroenterol. 2020 May 21;26(19):2403–2415. doi: 10.3748/wjg.v26.i19.2403. PMID: 32476801; PMCID: PMC7243649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carmona Agúndez M., Lopez Guerra D., Fernandez Perez J., Blanco Fernandez G. Síndrome de Lemmel: ictericia obstructiva secundaria a divertículo duodenal. Cir. Esp. [Internet] 2017 Nov;95(9):550–551. doi: 10.1016/j.ciresp.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Frauenfelder G., Maraziti A., Ciccone V., Maraziti G., Caleo O., Giurazza F., et al. Computed tomography imaging in lemmel syndrome: a report of two cases. J. Clin. Imaging Sci. 2019;9(23):1–4. doi: 10.25259/JCIS-17-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberto R.F., Hector P.L., Gabriela E.S., de Lemmel Síndrome. Una causa rara de obstrucci’on biliar no neoplasica de la vía biliar. Presentacion de un caso. Rev. Colomb. Gastroenterol. 2017;32(1):60–64. [Google Scholar]
- 7.Khan B., Khan S., Sharma A. Lemmel’s syndrome: a rare cause of obstructive jaundice secondary to periampullary diverticulum. Eur. J. Case Rep. Int. Med. [Internet] 2017 May;5:2. doi: 10.12890/2017_000632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Love J.S., Yellen M., Melitas C., Yazici C., Zar F. Diagnosis and management of Lemmel syndrome: an unusual presentation and literature review. Case Rep. Gastroenterol. 2022 Dec 16;16(3):663–674. doi: 10.1159/000528031. PMID: 36605730; PMCID: PMC9808136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernshteyn M., Rao S., Sharma A., Masood U., Manocha D. Lemmel’s syndrome: usual presentation of an unusual diagnosis. Cureus. 2020;12(4) doi: 10.7759/cureus.7698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Desai K., Wermers J.D., Beteselassie N. Lemmel syndrome secondary to duodenal diverticulitis: a case report. Cureus. 2017;9(3):1–6. doi: 10.7759/cureus.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]