Abstract
Background:
Neonatal sepsis is a serious blood bacterial infection in neonates at the age of equal to or less than 28 days of life, and it’s still the major significant cause of death and long-term morbidity in developing countries.
Objective:
This study aimed to assess the prevalence and related factors with neonatal sepsis among newborns admitted to the neonatal intensive care unit at Hiwot Fana Comprehensive Specialized University Hospital, Harar, Ethiopia.
Methods:
An institutional-based retrospective cross-sectional study design was conducted among 386 neonates admitted to Neonatal Intensive Care Unit from September 2017 to August 2019. A systematic random sampling method was used. Data were analyzed using SPSS V.26. Descriptive summary statistics were done. Bivariate regression and multivariate analysis were computed. Variables with P-value <.05 were declared as having a statistically significant association.
Result:
The prevalence of neonatal sepsis was 53.1%. Among the total neonates who had sepsis, 67.8% had early neonatal sepsis. Among neonatal factors, preterm neonates (AOR: 8.1, 95%CI: 2.1, 31.2), birth asphyxia (AOR: 4.7, 95%CI: 1.6, 13.6); and among maternal factors, urban residence (AOR: 0.26, 95%CI: 0.1, 0.5), antenatal care attendance (AOR: 0.32, 95%CI: 0.2, 0.6), spontaneous vaginal delivery (AOR: 0.047, 95%CI: 0.01, 0.2), and maternal antibiotic use (AOR: 0.39; 95%CI: 0.2, 0.8) were found to have significant association with neonatal sepsis.
Conclusion:
Overall, the magnitude of neonatal sepsis was high. Provision of neonatal and obstetrics care as per standard during prenatal, intranatal, and postnatal periods is needed. Training of health professionals on infection prevention and safe delivery practice should be provided.
Keywords: Neonatal sepsis, intensive care unit, Harar
Introduction
Sepsis is a systemic inflammatory reaction syndrome that occurs as a result of a suspected or confirmed infection. A dysregulated host response to infection causes a life-threatening organ failure. It’s also a prevalent last pathway to death from numerous infectious diseases around the world.1 -3 Neonatal sepsis is a serious blood bacterial infection in neonates at the age of equal to or less than 28 days of life, and it’s still the major significant cause of death and long-term morbidity in developing countries.4,5
Globally, an estimated 1.3 to 3.9 million annual neonatal sepsis cases and 400 000 to 700 000 annual deaths worldwide, of these about 6700 newborns die every day due to sepsis. 6 Among hospital-born infants, hospital-acquired infections account for an estimated 4% to 56% of all deaths in the neonatal period, and 84% of these deaths are preventable.5,7
Developing countries accounted for around 85.0% of sepsis and deaths worldwide. Annually, an estimate of 5.29 to 8.73 million DALYs (disability adjusted life years) are lost due to neonatal sepsis in sub-Saharan African countries.8,9
According to EDHS 2016 and EDHS 2019 report the neonatal mortality rate in Ethiopia was 29 and 33 deaths per 1000 live births, respectively and the major causes of death in neonates are neonatal infections.10 -12 Studies conducted in different parts of Ethiopia from 2015 to 2019 showed that the magnitude of neonatal sepsis ranged from 33.8% to 78% (33.8% in Wolayita, 64.8% in Gondar, 76.8% in Mekele, 77.8% in Shashamane, and 78.3% in Arba Minch).13 -17 The main significant factors associated with neonatal sepsis were maternal factors (meconium-stained amniotic fluid,18,19 UTI during pregnancy,12,14,15,18,19 place of delivery,14,15,20 antenatal follow up,19,20 and PROM12,15,17,20,21) and neonatal factors (birth weight12,17,18 and APGAR score.17,19,21).
As indicated by many studies conducted in different parts of Ethiopia, the magnitude of neonatal sepsis varies geographically. Thus, there is a need to perform a periodic assessment of the problem in each location. In addition, in order to achieve the SDG goal of reducing neonatal mortality in Ethiopia, identifying factors contributing to neonatal sepsis is of paramount importance. There have been no studies in the study area that have investigated the magnitude and variables related to newborn sepsis to our knowledge. Thus, the prevalence of newborn sepsis and the factors that contribute to it have been investigated in this study among neonates admitted to the NICU at Hiwot Fana Comprehensive Specialized University Hospital.
Materials and Methods
Study area and period
The study was conducted in Hiwot Fana Comprehensive Specialized University Hospital, which is located in Harar town, 526 km from Addis Ababa, the capital city of Ethiopia. Harar is one of the most popular historical towns. HFCSUH is a specialized university hospital established in 2006 and provides service to more than 5 million people in the catchment area. Currently, it is the only teaching and referral hospital in Harar city. Annually, around 1400 neonates are admitted to the NICU of HFCSUH.
Study design
An institutional-based cross-sectional study design was conducted.
Source and study population
The source populations for the study were all neonates who were admitted and treated at Hiwot Fana Comprehensive Specialized University Hospital neonatal intensive care unit regardless of cause of admission. All neonates who were admitted and treated at Hiwot Fana Comprehensive Specialized University Hospital neonatal intensive care unit regardless of cause of admission from September 2017 to August 2019 were study population and all medical charts of neonates who were admitted to NICU which were selected using systematic random sampling were enrolled in the study. The data were reviewed from April 2 to 6, 2020.
Eligibility criteria
All neonates’ charts (records of patients) and ages equal to or less than 28 days who were admitted to the NICU of HFCSUH were included and neonates’ charts (records of patients) with incomplete information were excluded.
Sample size determination
A single population proportion formula was used to calculate the required sample size with the assumption of taking 95% confidence interval (CI), 5% marginal error, and taking a proportion of 64.8 % from research done in Gondar, 2019. 14
Where: n = required sample size; z = the standard normal deviation at 95% confidence interval = 1.96; P = prevalence of neonatal sepsis 64.8% (0.648); d = margin of error 5% (0.05), by adding 10% (35.1) for non-response rate. Then, the total sample size to assess the prevalence of Neonatal Sepsis and associated factors was 386.
Sampling technique and procedure
A list of 2 years admitted neonates were taken from the database and the K value was calculated as K = N/n → 2600/386 = 7 and samples were selected using a systematic random sampling method by every kth interval according to the registration order. Then the first number was selected by the lottery method. So, every 7 intervals were selected until the completion of the sample size. An incomplete sample was dropped out and replacement was done for it.
Measurement
Study variables
The dependent variable was neonatal sepsis and the independent variables included sociodemographic characteristics, maternal, and neonatal factors.
Data collection tools
After reviewing relevant literature, a semi-structured data extraction tool was developed to obtain information on sociodemographic characteristics (age, sex, residence, and place of delivery); maternal factors (parity, mode of delivery, maternal diseases, maternal age, history of UTI, ANC follow-up, history of maternal fever, history of foul-smelling liquor, history of chorioamnionitis, meconium-stained amniotic fluid, history of PROM, duration of rupture of membrane, duration of labor, and previous maternal use of medication); and Neonatal variables (birth weight, gestational age, birth asphyxia, and APGAR score).
Data processing and analysis
After the data was extracted from the charts (records of patients) into the extraction sheet, it was checked manually for completeness and inconsistency. Then the data was coded and entered into Epidata v.3 and transported to SPSS version 26.0 for analysis. To describe the data, summary statistics were done. Bivariate regression analysis was used with a P-value <.25 to check the existence of an association between each independent variable with the outcome variable. A multivariate logistic regression model was used to adjust the effects of possible cofounders on the outcome variable. Variables with a P-value < 0.05 were declared as having a statistically significant association. We have checked for collinearity using VIF and the result was all down to satisfactory values which means they’re all less than 5. This was not problematic or not fatal (it was not high). Hosmer-Lemeshow test was used to determine the goodness of fit of the logistic regression model.
Data quality assurance
First, a data extraction tool was prepared in English. Before starting the actual data collection, the quality of the data was assured by pre-testing the data extraction tool on 10% of the total sample in Dilchora hospital, Dire Dawa. A 1-day training was given to data collectors. Daily, the collected data were reviewed by supervisors and authors to check for completeness and consistency before data entry.
Operational definitions
Inborn
Neonate who was born in the maternity ward of HFCSUH and admitted to the NICU of HFCSUH.
Out born
Those neonates born outside of HFCSUH and admitted to the NICU of HFCSUH.
Neonatal sepsis
Neonatal sepsis is a serious blood bacterial infection in neonates at the age of equal to or less than 28 days of life.4,5
But, in this study neonatal sepsis is measured as when a medical diagnosis of the neonate is stated as “neonatal sepsis” by ithe physician in the neonate’s medical record chart.
ANC attendance
Pregnant women that received antenatal care provided by skilled health personal at least once during pregnancy. 22
Birth asphyxia
Birth asphyxia is a medical diagnosis of neonates by midwives/physicians based on the Apgar score at birth. Apgar score of > 7 at 1 minute of age was classified as no birth asphyxia, and an Apgar score of <7 at 1 minute of age, metabolic acidosis (pH ⩽ 7.0), or no breathing at 1 minute was recorded as mild/moderate to severe birth asphyxia. 23
History of UTI
If the mother has history of diagnosis of urinary tract infection during her pregnancy period.
Result
Sociodemographic characteristics of neonate and mothers
A total of 386 neonate charts (records of patients) were reviewed, which is a 100% response rate. The majority of the mothers’ age ranged between 20 and 29 years. Regarding residence, 64.8% and 35.2% of mothers were from rural and urban, respectively. Out of 386, the majority, 234 (60.6%) were male. Regarding their age, the vast majority, 90.4% were 0 to 7 days (Table 1).
Table 1.
Sociodemographic characteristics of study participants in Hiwot Fana comprehensive specialized University Hospital, Harar, eastern Ethiopia, 2021.
| Sociodemographic variables | Frequency (%) |
|---|---|
| Age of mother (y) | |
| <19 | 23 (6) |
| 20-24 | 129 (33.4) |
| 25-29 | 167 (43.3) |
| 30-34 | 17 (4.4) |
| ⩾35 | 50 (13) |
| Residence | |
| Urban | 136 (35.2) |
| Rural | 250 (64.8) |
| Age of neonate (d) | |
| 0-7 | 349 (90.4) |
| 8-28 | 37 (9.6) |
| Sex of neonate | |
| Male | 234 (60.6) |
| Female | 152 (39.4) |
Maternal and neonatal health related characteristics
Out of 386 mothers of neonates, 250 (64.8%) of them had attended ANC during their pregnancy and 169 (43.8%) had a history of UTI. Of the total neonates, 233 (60.4%) of them were born in the hospital. Most, 229 (59.3%) of them were born with SVD, and 231 (59.8%) them were born at term. Regarding the duration of labor majority, 256 (66.3%) of neonates were born within less than 12 hours from the onset of labor. Among the total neonates, 213 (55.2%) were born with a weight of 2.5 to 4 kg. The initial assessment of neonates at birth indicated that the majority, 209 (54.1%) of them had <7 APGAR scores, while 237 (61.4%) and 104 (26.9%) of them had birth asphyxia and meconium-stained amniotic fluid, respectively (Table 2).
Table 2.
Maternal and neonatal health related factors among neonates admitted at Hiwot Fana Comprehensive Specialized University Hospital, Harar, eastern Ethiopia, 2021.
| Maternal and neonatal health related factors | Frequency (%) |
|---|---|
| ANC history | |
| Yes | 250 (64.8) |
| No | 136 (35.2) |
| Maternal fever history | |
| Yes | 58 (15) |
| No | 328 (85) |
| History of UTI | |
| Yes | 169 (43.8) |
| No | 217 (56.2) |
| History of foul-smelling liquor | |
| Yes | 46 (11.9) |
| No | 340 (88.1) |
| History of chorioamnionitis | |
| Yes | 52 (13.5) |
| No | 334 (86.5) |
| History of PROM | |
| Yes | 52 (13.5) |
| No | 334 (86.5) |
| Duration of rupture of membrane (h) | |
| <12 | 197 (51) |
| 12-17 | 94 (24.4) |
| ⩾18 | 95 (24.6) |
| Parity | |
| Primigravida | 164 (42.5) |
| Multigravida | 222 (57.5) |
| Place of delivery | |
| In born | 233 (60.4) |
| Out born | 153 (39.6) |
| Mode of delivery | |
| SVD | 229 (59.3) |
| Cesarean section | 135 (35) |
| Instrumental | 22 (5.7) |
| Duration of labor (h) | |
| <12 | 256 (66.3) |
| 12-24 | 100 (25.9) |
| >24 | 30 (7.8) |
| Maternal antibiotic use | |
| Yes | 74 (19.2) |
| No | 312 (80.8) |
| Birth weight (kg) | |
| <2.5 | 150 (38.9) |
| 2.5-4 | 213 (55.2) |
| >4 | 23 (6) |
| Gestational age (weeks) | |
| <37 | 138 (35.8) |
| 37-42 | 231 (59.8) |
| >42 | 17 (4.4) |
| Meconium-stained amniotic fluid | |
| Yes | 104 (26.9) |
| No | 282 (73.1) |
| APGAR score | |
| <7 score | 209 (54.1) |
| ⩾7 score | 177 (45.9) |
| Birth asphyxia | |
| Yes | 237 (61.4) |
| No | 149 (38.6) |
Prevalence of neonatal sepsis among hospital admitted neonates
Out of the total 386 admitted neonates, 205 (53.1%) of them had neonatal sepsis (Figure 1). Among these, the majority, 139 (67.8%) of them had early-onset neonatal sepsis and the rest had late onset of neonatal sepsis. Among the neonates who had sepsis, 122 (59.5%) were males.
Figure 1.
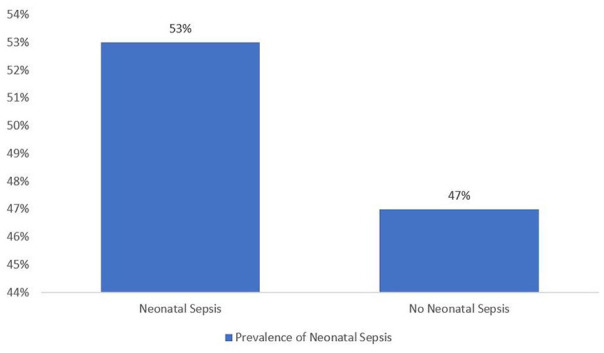
Prevalence of neonatal sepsis among neonates admitted in NICU at Hiwot Fana comprehensive specialized University Hospital, Harar, eastern Ethiopia, 2021.
Factors associated with neonatal sepsis among hospital admitted neonates
Neonatal related factors associated with neonatal sepsis
Preterm neonates were 8 (AOR: 8.1; 95% CI: 2.1,31.2) times more likely to develop neonatal sepsis than post-term neonates. The odds of neonatal sepsis were 5 (AOR: 5.4; 95%CI: 1.5, 19.3) times among neonates born with < 2.5 kg than neonates born with >4 kg. Neonates with birth asphyxia were 4 (AOR: 4.7; 95%CI: 1.6, 13.6) times more likely to get sepsis than those who had no birth asphyxia (Table 3).
Table 3.
Factors associated with neonatal sepsis among neonates admitted in NICU at Hiwot Fana Comprehensive Specialized University Hospital, Harar, eastern Ethiopia, 2021.
| Neonatal Factors related with neonatal sepsis | Neonatal sepsis (N = 386) | COR (95%: CI) | P-value | AOR (95%: CI) | P-value | |
|---|---|---|---|---|---|---|
| Yes (n = 205) | No (n = 181) | |||||
| Age of neonates (d) | ||||||
| 0-7 | 189 (92.2%) | 160 (88.4%) | 1.5 (0.8, 3.1) | .209 | 0.97 (0.4, 2.6) | .95 |
| 8-28 | 16 (7.8%) | 21 (11.6%) | 1 | |||
| Sex of neonates | ||||||
| Male | 122 (59.5%) | 112 (61.9%) | 0.9 (0.6, 1.4) | .63 | 1.1 (0.6, 2.0) | .67 |
| Female | 83 (40.5%) | 69 (38.1%) | 1 | |||
| Gestational age (weeks) | ||||||
| <37 | 131 (63.9%) | 7 (3.9%) | 13 (3.8, 44.8) | .0001 | 8.1 (2.1, 31.2) | .003* |
| 37-42 | 64 (31.2%) | 167 (92.2%) | 0.26 (0.1, 0.7) | .011 | 0.3 (0.1, 0.8) | .021* |
| >42 | 10 (4.9%) | 7 (3.9%) | 1 | 1 | ||
| Birth weight (kg) | ||||||
| <2.5 | 121 (59%) | 29 (16%) | 19.8 (6.3, 62.7) | .0001 | 5.4 (1.5, 19.3) | .01* |
| 2.5-4 | 80 (39%) | 133 (73.5%) | 2.8 (0.9, 8.7) | .065 | 1.4 (0.4, 4.7) | .57 |
| >4 | 4 (2%) | 19 (10.5%) | 1 | |||
| History of meconium-stained amniotic fluid | ||||||
| Yes | 69 (33.7%) | 35 (19.3%) | 2.12 (1.3, 3.4) | .002 | 1.4 (0.7, 2.8) | .27 |
| No | 136 (66.3%) | 146 (80.7%) | 1 | 1 | ||
| APGAR score | ||||||
| <7 APGAR score | 132 (64.4%) | 77 (42.5%) | 2.4 (1.6, 3.7) | .0001 | 0.6 (0.2, 1.5) | .28 |
| >7 APGAR score | 73 (35.6%) | 104 (57.5%) | 1 | |||
| Birth asphyxia | ||||||
| Yes | 151 (73.7%) | 86 (47.5%) | 3.1 (2.0, 4.7) | .0001 | 4.7 (1.6, 13.6) | .004* |
| No | 54 (26.3%) | 95 (52.5%) | 1 | |||
| Place of delivery | ||||||
| Inborn | 138 (67.3%) | 95 (52.5%) | 1.9 (1.2, 2.8) | .003 | 1.7 (0.9, 3.2) | .068 |
| Out born | 67 (32.7%) | 86 (47.5%) | 1 | |||
Abbreviations: AOR, adjusted odds ratio; COR, crude odds ratio; CI, confidence interval; N: sample size; n: sub group sample.
Bold, significant at <.05.
Maternal related factors associated with neonatal sepsis
Neonates born from mothers living in urban areas were 74% (AOR: 0.26; 95%CI: 0.1, 0.5) less likely to develop neonatal sepsis than neonates whose mothers lived in rural areas. Neonates born from mothers who had attended ANC were 68% (AOR: 0.32; 95%CI: 0.2, 0.6) less likely to develop neonatal sepsis than those neonates whose mothers had not attended ANC. Neonates born with spontaneous vaginal delivery were 95.3% (AOR: 0.047; 95%CI: 0.01, 0.2) less likely to develop neonatal sepsis than neonates born with instrumental delivery. Similarly, neonates born by the cesarian section were 95% (AOR: 0.05; 95%CI: 0.01, 0.3) less likely to develop neonatal sepsis than neonates born by instrumental delivery.
Neonates born from mothers who had used antibiotics during pregnancy were 61% (AOR: 0.39; 95%CI: 0.2, 0.8) less likely to develop neonatal sepsis than neonates born from mothers who had not used antibiotics. Neonates born from mothers with a duration of rupture of membrane <12 and 12 to 17 hours were 89% (AOR: 0.11; 95%CI: 0.05, 0.2), and 79% (AOR: 0.2; 95%CI: 0.1, 0.5) less likely to develop neonatal sepsis than neonates born from mothers with a duration of rupture of membrane > 18 hours, respectively (Table 4).
Table 4.
Maternal factors associated with neonatal sepsis among neonates admitted in NICU at Hiwot Fana Comprehensive Specialized University Hospital, Harar, eastern Ethiopia, 2021.
| Factor related with neonatal sepsis | Neonatal sepsis (N = 386) | COR (95%: CI) | P-value | AOR (95%: CI) | P-value | |
|---|---|---|---|---|---|---|
| Yes (n = 205) | No (n = 181) | |||||
| Age of mother (y) | ||||||
| <19 | 12 (3.1%) | 11 (2.83%) | 1.1 (0.4, 2.9) | .86 | 1.44 (0.3, 6.3) | .625 |
| 20-24 | 66 (17.1%) | 63 (16.3%) | 1.05 (0.5, 2) | .88 | 1.45 (0.6, 3.8) | .449 |
| 25-29 | 92 (23.8%) | 75 (19.4%) | 1.2 (0.6, 2.3) | .52 | 1.9 (0.8, 4.4) | .142 |
| 30-34 | 10 (2.6%) | 7 (1.8%) | 1.4 (0.5, 4.3) | .53 | 1.2 (0.3, 5.1) | .83 |
| >35 | 25 (6.5%) | 25 (6.5%) | 1 | 1 | ||
| Residence | ||||||
| Urban | 48 (12.4%) | 88 (22.8%) | 0.3 (0.2, 0.5) | .0001 | 0.26 (0.1, 0.5) | <.001* |
| Rural | 157 (40.7%) | 93 (24.1%) | 1 | 1 | ||
| History of ANC | ||||||
| Yes | 112 (29%) | 138 (35.8%) | 0.3 (0.2, 0.6) | .0001 | 0.32 (0.2, 0.6) | <.001* |
| No | 93 (24.1%) | 43 (11.1%) | 1 | 1 | ||
| History of maternal fever | ||||||
| Yes | 40 (10.4%) | 18 (4.7%) | 1 | .01 | 1 | .546 |
| No | 165 (42.7%) | 163 (42.2%) | 0.46 (0.2, 0.8) | 1.3 (0.5, 3.4) | ||
| History of UTI | ||||||
| Yes | 116 (30.1%) | 53 (13.7%) | 3.1 (2.1, 4.8) | .0001 | 3.6 (2.1, 6.1) | <.001* |
| No | 89 (23%) | 128 (33.2%) | 1 | 1 | ||
| History of foul smelling | ||||||
| Yes | 33 (8.5%) | 13 (3.4%) | 1 | .008 | 1 | .125 |
| No | 172 (44.6%) | 168 (43.5%) | 0.4 (0.2, 0.8) | 0.4 (0.1, 1.3) | ||
| History of chorioamnionitis | ||||||
| Yes | 40 (10.4%) | 12 (3.1%) | 1 | .0001 | 1 | .079 |
| No | 165 (42.7%) | 169 (43.8%) | 0.3 (0.1, 0.6) | 0.34 (0.1, 1.1) | ||
| History of PROM | ||||||
| Yes | 29 (7.5%) | 23 (6%) | 1 | .68 | 1 | .254 |
| No | 176 (45.6%) | 158 (40.9%) | 0.9 (0.5, 1.6) | 1.7 (0.7, 4.1) | ||
| Duration of labor (h) | ||||||
| <12 | 134 (34.8%) | 122 (31.6%) | 1.2 (0.6, 2.6) | .55 | 1.9 (0.6, 5.3) | .24 |
| 12-24 | 57 (14.8%) | 43 (11.1%) | 1.5 (0.6, 3.4) | .32 | 1.6 (0.5, 4.7) | .433 |
| >24 | 14 (3.6%) | 16 (4.3%) | 1 | 1 | ||
| Parity | ||||||
| Primigravida | 87 (22.5%) | 77 (20%) | 0.9 (0.7, 1.5) | .98 | (0.6, 2.1) | .79 |
| Multigravida | 118 (30.6%) | 104 (26.9%) | 1 | 1 | ||
| Mode of delivery | ||||||
| SVD | 122 (31.6%) | 107 (27.7%) | 0.11 (0.03, 0.5) | .004 | 0.047(0.01, 0.2) | <.001* |
| Cesarean section | 63 (16.3%) | 72 (18.7%) | 0.09 (0.02, 0.4) | .001 | 0.05 (0.01, 0.3) | .001* |
| Instrumental delivery | 20 (5.2 %) | 2 (0.52%) | 1 | 1 | ||
| Maternal antibiotic use | ||||||
| Yes | 27 (7%) | 47 (12.2%) | 0.43 (0.3, 0.7) | .002 | 0.39 (0.2, 0.8) | <.001* |
| No | 178 (46.1%) | 134 (34.7%) | 1 | 1 | ||
| Duration of rapture of membrane (h) | ||||||
| <12 | 76 (19.7%) | 121 (31.3%) | 0.11 (0.6, 0.2) | .0001 | 0.11 (0.05, 0.2) | <.001* |
| 12-17 | 48 (12.4%) | 46 (11.9%) | 0.18 (0.1, 0.4) | .0001 | 0.21 (0.1, 0.5) | <.001* |
| >18 | 81 (21%) | 14 (3.6%) | 1 | 1 | ||
Abbreviations: AOR, adjusted odds ratio; COR, crude odds ratio; CI, confidence interval; N, sample size; n, sub group sample.
Bold, significant at <.05.
Discussion
In our findings, the prevalence of neonatal sepsis was 53.1%. Other similar studies conducted in different parts of Ethiopia indicated a higher prevalence of neonatal sepsis, 78.3% in Arba Minch., 17 77.9% in Shashamane, 16 76.8% in Mekelle, 15 64.8% in Gondar. 14 The reason for the low prevalence of neonatal sepsis in our finding compared to the above studies could be due to differences in population variation and due to the fact that our study was conducted in a specialized university referral hospital that has relatively better facilities and human resources. On the contrary, our study finding was higher than the finding reported from Wolaita Sodo, Ethiopia 33.8%, 13 Nairobi, Kenya 28.6%, 24 and Johannesburg, South Africa 20.5%. 25 These differences might be due to quality of care, sociodemographic variation and sample size differences.
In our study, the prevalence of neonatal sepsis was higher among males than females 31.6%. This finding was consistent with studies conducted in Bahar Dar, Gondar, and Arba Minch, 64%, 26 41.1%, 14 and 58.2%, 17 respectively.
From the total cases of neonatal sepsis, early neonatal sepsis was found to be high, 67.9%. A similar finding was also reported from other studies in West Showa, Arba Minch, Bahar Dar, Gondar, and Wolaita Sodo, which reported 94.9%, 20 84%, 17 72.9%, 26 48.2%, 14 and 40.4%, 13 respectively. This could be due to the fact that most new born who harbor different infectious agents during intra uterine life, intra-partum, and immediate postpartum period manifest clinical symptoms during early period (0-7 days).
In our finding, the odds of developing neonatal sepsis were 8 times among preterm neonates than post-term neonates. This is consistent with a study conducted in Debre Markos, Ethiopia, and Nairobi, Kenya where preterm neonates were found to be 6 times more likely to develop neonatal sepsis. In addition, other studies also reported similar findings.21,25,27,28 This could be due to the fact that neonates born before term have immature immune system which render them at high risk for acquring infections.
Our study revealed that the odds of neonatal sepsis was 5 times higher among neonates born with low birth weight. This is consistent with studies conducted in different parts of Ethiopia, in Durame, Arsi, Arba Minch, Jimma, and Gondar.12,17,18,28,29 This could be due to the fact that neonates who are born under weight have poor immune system which put them at a higher risk for acquring infections.
According to this study, the odds of developing neonatal sepsis were 4 times among neonates with birth asphyxia than those who had no birth asphyxia. This is consistent with a study conducted in Shashamane. 16
In our study, the odds of developing neonatal sepsis were 68% less among neonates born from mothers who had at least 1 ANC follow-up than those neonates whose mothers had not at least 1 ANC follow-up. This result was consistent with a study conducted in West Shewa, Oromia Region. 20
Our study revealed that the odds of developing neonatal sepsis were 3 times among neonates born from mothers who had a history of UTI than neonates born from mothers who had no history of UTI. This finding was consistent with similar studies conducted in Durame, 18 Gondar, 14 Mekelle, 15 Ethiopia, and Nairobi, Kenya. This is due to the fact that, an infectious agent colonization in the birth canal may contaminate newborns as they emerge and predispose them to early sepsis, which is 1 reason for this connection.
Our study findings indicated that neonates who were born by SVD and the Cesarian section were found to be 95.3% and 95% less likely to get neonatal sepsis than children born by instrumental delivery, respectively. This finding was contradictory to the finding reported in Gondar, which reported that the odds of developing neonatal sepsis were higher among neonates born by cesarian section than neonates born by SVD and instrumental delivery. 29 This difference could be due to a difference in implementation procedure of infection prevention and patient safety guideline.
In our study, neonates born of mothers who had a duration of rupture membrane <12 and 12 to 17 hours were 89% and 79% less likely to have neonatal sepsis than those neonates born of mothers with a duration of rupture of membrane ⩾18 hours. Similar findings also reported from studies in Arba Minch, 17 Debre Markos, Ethiopia, 21 and Nairobi, Kenya. 25 This might be explained by the fact that during Early membrane rupture can increase the risk of neonatal sepsis following delivery because it exposes the baby to bacteria that are rising from the birth canal into the amniotic sac.
In our study, neonates born from mothers who had a history of antibiotic use were 61% less likely to have neonatal sepsis than those born from mothers who had no history of antibiotic use. This is consistent with study conducted in Dhaka, 30 Bangladesh, however it is not statistically significant.
Similarly, neonates born from mothers who lived in urban areas were 74% less likely to have neonatal sepsis than neonates born from mothers living in rural areas. These factors were the only variables that had a significant association with neonatal sepsis and which were not reported in other similar studies.
Conclusion
Overall, the magnitude of neonatal sepsis was high and it was prevalent among male neonates. Neonatal factors; being preterm, low birth weight, and having birth asphyxia were found to significantly increase the odds of neonatal sepsis. Among maternal factors; urban residence, having ANC follow up, giving birth by SVD and CS, history of antibiotic use, and having rupture of membrane <18 hours were found to significantly decrease the odds of neonatal sepsis.
Provision of neonatal and obstetrics care as per standard during prenatal, intranatal, and postnatal periods should be strengthened. Training for health professionals on obstetrics care standards and delivery practice should be provided.
Limitations of the Study
The research was conducted using secondary data, which is difficult to generalize to the general population. The study used a cross-sectional study design. Therefore, there is a temporal relationship issue. Also, 1 variable shows a wide confidence interval, so we recommend for future direction for researchers to overcome or get out of such type of issue they have to try to study this topic using a cohort study design.
Acknowledgments
We thank the Almighty God. Also, we would like to thank Hiwot Fana Comprehensive Specialized University Hospital.
Abbreviations: ANC, Antenatal Care; CS, Cesarian Section; NICU, Neonatal Intensive Care Unit; HFCSUH, Hiwot Fana Comprehensive Specialized University Hospital; IHREC, Institutional Health Research Ethical Committee; PROM, Premature Rupture of Membrane; SDGs, Sustainable Developmental Goals; SVD, Spontaneous Vaginal Delivery; SPSSs, Statistical Package for Social Science; UTI, Urinary Tract Infection
ORCID iDs: Astawus Alemayehu  https://orcid.org/0000-0003-1384-7123
https://orcid.org/0000-0003-1384-7123
Mohammed Yusuf  https://orcid.org/0000-0002-1091-9235
https://orcid.org/0000-0002-1091-9235
Abebaw Demissie  https://orcid.org/0000-0001-8322-2570
https://orcid.org/0000-0001-8322-2570
Mekuria Edae Muleta  https://orcid.org/0000-0003-2113-7076
https://orcid.org/0000-0003-2113-7076
Declarations
Ethics approval and consent to participate: An ethical Approval letter was obtained from Rift Valley University IHREC with reference no. IHREC 0015/02/01/2020, and an official letter was written from Rift Valley University to obtain consent from the Hiwot Fana Comprehensive Specialized University Hospital to review patient charts and collect data. Confidentiality of all information had been maintained.
Consent for publication: Not applicable.
Author contributions: Astawus Alemayehu: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing— – original draft. Mohammed Yusuf: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft. Abebaw Demissie: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing—original draft. Mekuria Edae Muleta: Formal analysis; Validation; Visualization; Writing—review & editing.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Any time, the corresponding author provides an additional resource on request.
References
- 1. Geme RMKJS. Nelson Textbook of Pediatrics, 2-Volume Set. Elsevier; 2019. [Google Scholar]
- 2. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. Sepsis. 2020. https://www.who.int/news-room/fact-sheets/detail/sepsis
- 4. Seale AC, Blencowe H, Manu AA, et al. Estimates of possible severe bacterial infection in neonates in sub-Saharan Africa, south Asia, and Latin America for 2012: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14:731-741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. Global report on the epidemiology and burden of sepsis: Current evidence, identifying gaps and future directions. World Health Organization; 2020. [Google Scholar]
- 6. IGME UNI-aGfCMEU. Levels and Trends in Child Mortality: Report 2019; 2020. [Google Scholar]
- 7. Lawn JE, Blencowe H, Oza S, et al. Every Newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384:189-205. [DOI] [PubMed] [Google Scholar]
- 8. Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395:200-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ranjeva SL, Warf BC, Schiff SJ. Economic burden of neonatal sepsis in sub-Saharan Africa. BMJ Glob Health. 2018;3:e000347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ethiopian Public Health Institute E, Federal Ministry of Health F and Icf. Ethiopia Mini Demographic and Health Survey 2019. EPHI/FMoH/ICF; 2021. [Google Scholar]
- 11. Central Statistical Agency aI. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. CSA and ICF, 2016. [Google Scholar]
- 12. Debelew GT, Afework MF, Yalew AW. Determinants and causes of neonatal mortality in Jimma zone, southwest Ethiopia: a multilevel analysis of prospective follow up study. PLOS ONE. 2014;9:e107184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mersha A, Worku T, Shibiru S, et al. Neonatal sepsis and associated factors among newborns in hospitals of Wolaita Sodo Town, Southern Ethiopia. Res Rep Neonatol. 2019;9:1. [Google Scholar]
- 14. Agnche Z, Yeshita HY, Gonete KA. Neonatal sepsis and its associated factors among neonates admitted to neonatal intensive care units in primary hospitals in central Gondar zone, northwest Ethiopia, 2019. Infect Drug Resist. 2020;13:3957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gebremedhin D, Berhe H, Gebrekirstos K. Risk factors for neonatal sepsis in public hospitals of Mekelle City, North Ethiopia, 2015: unmatched case control study. PLOS ONE. 2016;11:e0154798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Getabelew A, Aman M, Fantaye E, et al. Prevalence of neonatal sepsis and associated factors among neonates in neonatal intensive care unit at selected governmental hospitals in Shashemene Town, Oromia Regional State, Ethiopia, 2017. Int J Pediatr. 2018;2018:7801272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mustefa A, Abera A, Aseffa A. Prevalence of neonatal sepsis and associated factors amongst neonates admitted in arbaminch general hospital, arbaminch, southern Ethiopia, 2019. J Pediatr Neonatal Care. 2020;10:1-7. [Google Scholar]
- 18. Dirirsa DE, Dibaba Degefa B, Gonfa AD. Determinants of neonatal sepsis among neonates delivered in Southwest Ethiopia 2018: a case-control study. SAGE Open Med. 2021;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Akalu TY, Gebremichael B, Desta KW, et al. Predictors of neonatal sepsis in public referral hospitals, Northwest Ethiopia: a case control study. PLOS ONE. 2020;15:e0234472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bulto GA, Fekene DB, Woldeyes BS, et al. Determinants of neonatal sepsis among neonates admitted to public hospitals in central Ethiopia: unmatched case-control study. Glob Pediatr Health. 2021;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Alemu M, Ayana M, Abiy H, et al. Determinants of neonatal sepsis among neonates in the northwest part of Ethiopia: case-control study. Ital J Pediatr. 2019;45:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Unicef. Antenatal care: Antenatal care is essential for protecting the health of women and their unborn children. 2022. Accessed April 18 2023. https://data.unicef.org/topic/maternal-health/antenatal-care/
- 23. Locatelli A, Lambicchi L, Incerti M, et al. Is perinatal asphyxia predictable? BMC Pregnancy Childbirth. 2020;20:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Okube OT, Komen M. Prevalence and predictors of neonatal sepsis among neonates admitted at the newborn unit of Kenyatta National Hospital, Nairobi, Kenya. Open J Obstetr Gynecol. 2020;10:1216. [Google Scholar]
- 25. Clotilde TS, Motara F, Laher AE. Prevalence and presentation of neonatal sepsis at a paediatric emergency department in Johannesburg, South Africa. Afr J Emerg Med. 2022;12:362-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tewabe T, Mohammed S, Tilahun Y, et al. Clinical outcome and risk factors of neonatal sepsis among neonates in Felege Hiwot referral Hospital, Bahir Dar, Amhara Regional State, North West Ethiopia 2016: a retrospective chart review. BMC Res Notes. 2017;10:265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gebrehiwot A, Lakew W, Moges F, et al. Bacterial profile and drug susceptibility pattern of neonatal sepsis in Gondar University Hospital, Gondar Northwest Ethiopia. Der Pharmacia Lettre. 2012;4:1811-1816. [Google Scholar]
- 28. Sorsa A. Epidemiology of neonatal sepsis and associated factors implicated: observational study at neonatal intensive care unit of Arsi University Teaching and Referral Hospital, South East Ethiopia. Ethiop J Health Sci. 2019;29:333-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Moges F, Eshetie S, Yeshitela B, et al. Bacterial etiologic agents causing neonatal sepsis and associated risk factors in Gondar, Northwest Ethiopia. BMC Pediatr. 2017;17:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chan GJ, Stuart EA, Zaman M, et al. The effect of intrapartum antibiotics on early-onset neonatal sepsis in Dhaka, Bangladesh: a propensity score matched analysis. BMC Pediatr. 2014;14:104. [DOI] [PMC free article] [PubMed] [Google Scholar]


