Abstract
Background:
International travellers may seek care abroad to address health problems that arise during their trip or plan healthcare outside their country of residence as medical tourists.
Methods:
Data were collected on travellers evaluated at GeoSentinel Network sites who reported healthcare during travel. Both unplanned and planned healthcare were analysed, including the reason and nature of healthcare sought, characteristics of the treatment provided and outcomes. Travellers that presented for rabies post-exposure prophylaxis were described elsewhere and were excluded from detailed analysis.
Results:
From May 2017 through June 2020, after excluding travellers obtaining rabies post-exposure prophylaxis (n = 415), 1093 travellers reported care for a medical or dental issue that was an unanticipated part of the travellers’ planned itinerary (unplanned healthcare). Travellers who sought unplanned healthcare abroad had frequent diagnoses of acute diarrhoea, dengue, falciparum malaria and unspecified viral syndrome, and obtained care in 131 countries. Thirty-four (3%) reported subsequent deterioration and 230 (21%) reported no change in condition; a third (n = 405; 37%) had a pre-travel health encounter. Forty-one travellers had sufficient data on planned healthcare abroad for analysis. The most common destinations were the US, France, Dominican Republic, Belgium and Mexico. The top reasons for their planned healthcare abroad were unavailability of procedure at home (n = 9; 19%), expertise abroad (n = 9; 19%), lower cost (n = 8; 17%) and convenience (n = 7; 15%); a third (n = 13; 32%) reported cosmetic or surgical procedures. Early and late complications occurred in 14 (33%) and 4 (10%) travellers, respectively. Four travellers (10%) had a pre-travel health encounter.
Conclusions:
International travellers encounter health problems during travel that often could be prevented by pre-travel consultation. Travellers obtaining planned healthcare abroad can experience negative health consequences associated with treatments abroad, for which pre-travel consultations could provide advice and potentially help to prevent complications.
Keywords: Medical tourism, illness, travellers, international, treatment, procedure, outcome
Introduction
International tourist arrivals had been increasing at a rate of 4–6% annually for several years before the SARS-CoV-2 pandemic occurred, reaching 1.5 billion arrivals in 2019.1 During 2020, international tourist arrivals declined by 73% compared with 2019 but have been rebounding.1 High travel volume is likely associated with a substantial number of travellers that encounter health problems during travel. Although many of these health problems may be mild and may resolve spontaneously, some travellers need to, or choose to seek medical evaluation in foreign countries.2–5 However, the characteristics, clinical illness patterns and outcome of travellers who visit healthcare facilities abroad have rarely been described systematically or at a global level.
At the same time, planned travel abroad for healthcare has also increased rapidly in recent years, driven by a variety of motivations including economic, cultural, ethical and legal constraints.6–8 Popular interventions include joint, cosmetic and dental procedures, cardiac surgery, reproductive care (e.g. in vitro fertilization, abortion, surrogacy) and organ transplantation.6,9 Travel to another country for the purpose of obtaining medical care is referred to by various terms including medical tourism, cross-border healthcare and preplanned international travel for medical care.10,11 A standardized approach to collect data including demographics, procedures sought and outcomes can provide insight into anticipated healthcare challenges that medical providers can use to advise patients seeking healthcare abroad or to evaluate them after returning from their treatments abroad.
This prospective project aimed to describe the epidemiological and clinical pattern of travel-related healthcare encounters among travellers seen in the GeoSentinel Network, a global network of travel and tropical medicine providers that monitors travel-related morbidity and collects data on international travellers, including travel exposure and diagnoses.12 This descriptive analysis included data both from travellers whose main purpose of travel was to obtain healthcare abroad (planned healthcare) and travellers who obtained healthcare abroad that was not the main purpose of travel (unplanned healthcare). The analysis aimed to describe the travellers who obtained healthcare abroad and reasons for healthcare visits during travel, types of treatment, antibiotic use, response to treatment and relationship of the healthcare abroad with the subsequent reason for care at a GeoSentinel Network site.
Methods
Data source
The GeoSentinel network consists of 68 specialized travel and tropical medicine clinical sites in 28 countries on 6 continents at the time of this enhanced surveillance project.12 All sites see international travellers either pre-, during and also post travel. These sites collect de-identified data on international travellers, including demographics, trip details, region and country of exposure, clinical information and diagnoses; clinical treatment and outcomes are not reported routinely.
The GeoSentinel Network developed supplemental data collection forms to collect additional information specifically for patients presenting to GeoSentinel sites during or after a trip outside of their country of residence from 1 May 2017 to 30 June 2020, and who had received medical or dental care during travel. Data collected included the destination where healthcare was obtained (i.e. destination country), country where a disease or injury occurred (i.e. country of exposure), type of facility, nature of healthcare sought, type of procedure, treatment or surgery received, the outcome and the patients’ purpose for seeking care outside of their country of residence. GeoSentinel’s data collection protocol has been reviewed by a human subjects’ advisor at CDC’s National Center for Emerging and Zoonotic Infectious Diseases and is classified as public health surveillance and not human subjects’ research.
Inclusion and exclusion criteria
Patients presenting at a GeoSentinel clinic from 1 May 2017 to 30 June 2020, who reported unplanned or planned healthcare during their recent trip, regardless of reason for attendance at the clinic, and for whom a supplemental data collection form was completed, were included. Presentation could be during, or after travel. Healthcare included medical care, dental care, surgical care or other health services that were provided by healthcare professionals or at local healthcare facilities during travel. Patients who self-treated with over-the-counter medications were excluded. Excluded from detailed analysis were patients that consulted a GeoSentinel site whose only diagnosis was a reported bite, scratch, sting or other exposure to animals during travel for which they received rabies post-exposure prophylaxis during or after travel, because they were previously analysed and reported.13,14
Statistical analysis
Data for unplanned and planned travel were analysed separately. Descriptive analyses were performed using Microsoft Excel and SAS Enterprise Guide v7.1 (SAS Institute Inc., Cary, NC, USA).
Results
Among >60000 records in the GeoSentinel database during 1 May 2017 to 30 June 2020, 1549 travellers had enhanced data forms on medical or dental issues abroad and met the inclusion criteria (Figure 1). Excluding 415 travellers that presented for rabies post-exposure prophylaxis and described elsewhere,13,14 1134 travellers were assessed for healthcare received abroad. Among these travellers, 1093 had unplanned healthcare abroad and 41 had planned healthcare abroad.
Figure 1.
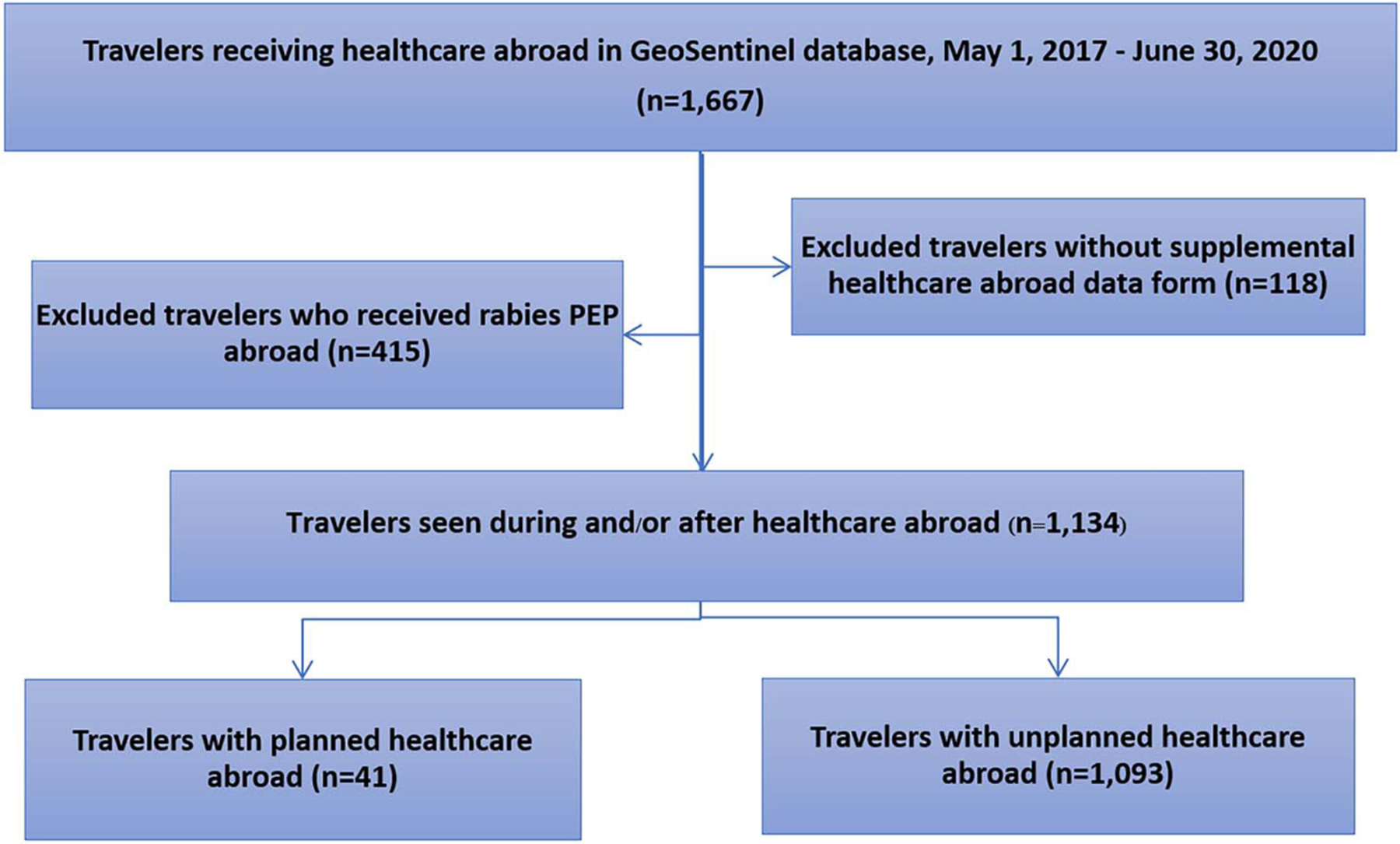
Travellers with healthcare abroad seen at GeoSentinel Network sites 1 May 2017–30 June 2020.
Travellers with unplanned healthcare abroad
During the study period, 1093 travellers received unplanned healthcare in 131 countries (Figure 2). Median age was 36 years (range: <1–94); 597 (55%) were female, and children under 18 years of age accounted for 116 (11%) travellers (Table 1). About a third of travellers (n = 405; 37%) reported having a pre-travel healthcare encounter. The most common reasons for travel were tourism (n = 493; 45%), visiting friends or relatives (n = 240; 22%) and volunteerism (n = 119; 11%), including missionary, humanitarian or community service work. Among 979 travellers with data available on the geographic region where disease was acquired or the adverse health event took place that required healthcare, the regions visited most commonly were sub-Saharan Africa (n = 288; 29%), Southeast Asia (n = 170; 17%) and South-Central Asia (n = 140; 14%) (Table 1). Among the 1093 travellers who received unplanned healthcare abroad, the most frequently reported destination countries for healthcare were India (n = 110; 10%), Thailand (n = 60; 5%) and Mexico (n = 45; 4%) (Table 2).
Figure 2.
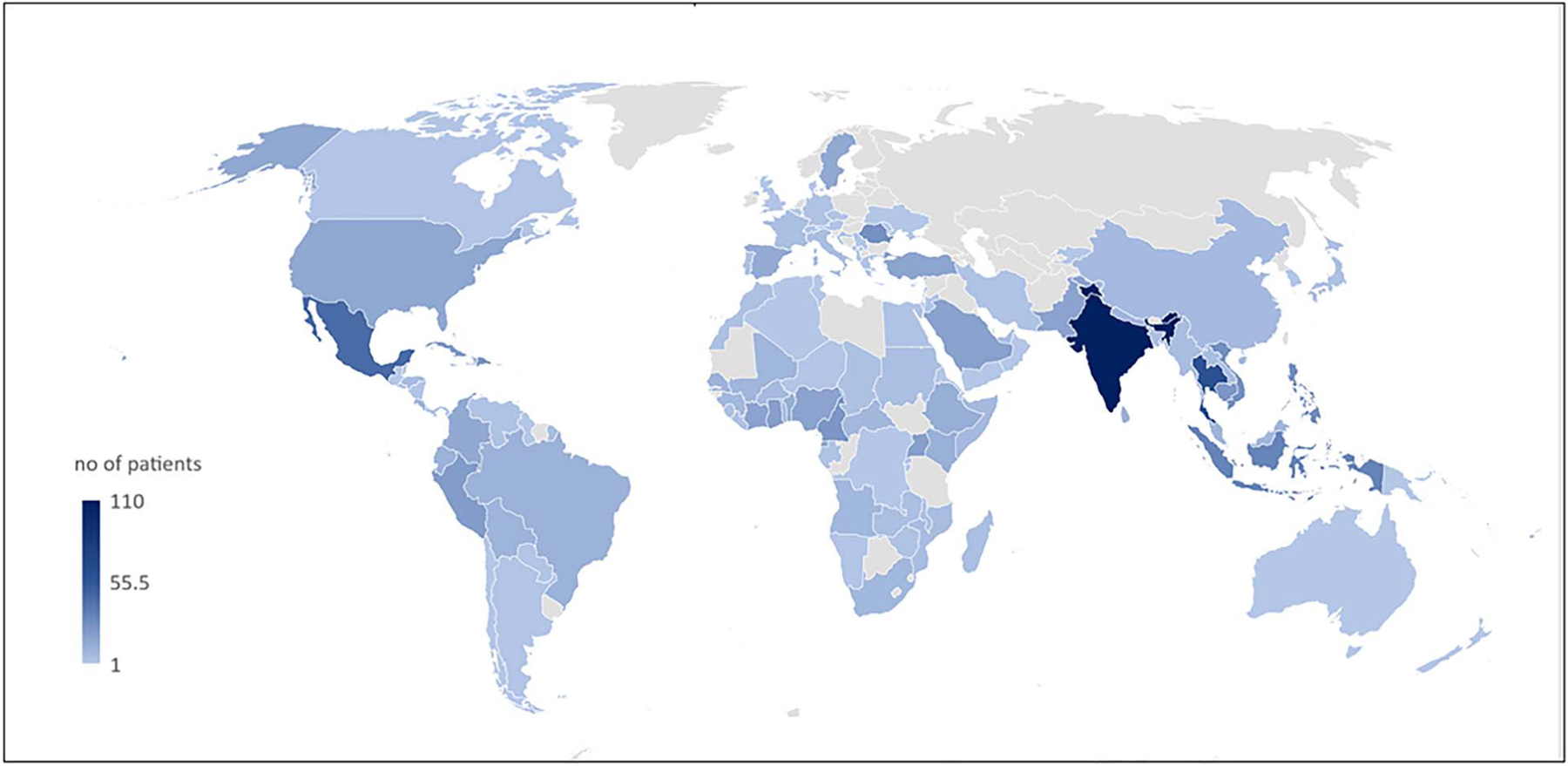
Destinations where travellers reported unplanned healthcare (n = 131)*. *This map reflects absolute numbers of travellers presented to the GeoSentinel Network only and should not be interpreted as true risk levels or distribution of travellers.
Table 1.
Demographic and trip characteristics of travellers with planned and unplanned healthcare abroad
| Unplanned (n = 1093) | Planned (n = 41) | |
|---|---|---|
| Age, years | ||
| Median (range) | 36 (<1–94) | 41 (2–81) |
| Age Group n = 1091 (col %) | ||
| <1–17 years | 116 (11) | 6 (15) |
| 18–25 | 169 (15) | 2 (5) |
| 26–39 | 321 (29) | 12 (29) |
| 40–49 | 161 (15) | 7 (17) |
| 50–64 | 185 (17) | 10 (24) |
| ≥65 | 139 (13) | 4 (10) |
| Sex | ||
| Female | 597 (55) | 25 (63) |
| Reason for planned healthcare abroad | ||
| Procedure unavailable in home country | 9 (22) | |
| Clinical expertise abroad | 9 (22) | |
| Lower cost | 8 (20) | |
| Greater convenience | 7 (17) | |
| Seeking a second opinion | 4 (10) | |
| Care provided by trusted known doctor | 3 (7) | |
| Anonymity | 1 (2) | |
| Reason for travel | ||
| Tourism | 493 (45) | |
| Visiting Friends or Relatives | 240 (22) | |
| Volunteerism (missionary, humanitarian, or community service work) | 119 (11) | |
| Corporate/Professional | 92 (8) | |
| Research | 43 (4) | |
| Othera | 43 (4) | |
| Migration | 34 (3) | |
| Business/Occupational | 29 (3) | |
| Pre-travel encounter | 405 (37) | 4 (10) |
| Region where disease was acquired, or adverse health event took place that required healthcare | Unplanned (n = 979b) | Planned (n = 41) |
| Sub-Saharan Africa | 288 (29) | 10 (24) |
| Southeast Asia | 170 (17) | 1 (2) |
| South-Central Asia | 140 (14) | 2 (5) |
| South America | 65 (7) | 6 (15) |
| Central America | 56 (6) | 3 (7) |
| Caribbean | 54 (6) | 4 (10) |
| Middle East | 47 (5) | 3 (7) |
| Eastern Europe | 41 (4) | 1 (2) |
| Western Europe | 32 (3) | 0 (0) |
| Northeast Asia | 16 (2) | 3 (7) |
| North Africa | 14 (1) | 3 (7) |
| North America | 9 (1) | 2 (5) |
| Oceania | 8 (1) | 1 (2) |
| Australia/New Zealand | 2 (<1) | 0 (0) |
| Not Ascertainable | 36 (4) | 2 (5) |
| Clinical outcomes | Unplanned (n = 1093) | Planned (n = 41) |
| Hospitalized | 364 (33) | 22 (54) |
| Deaths | 2 (<1)c | 0 (0) |
Other reported reasons for travel: Unspecified (30), Not Ascertainable (7), Military (2), Providing medical care (2), Planned Medical Care (1), Retirement (1)
About 114 (10%) of 1093 travellers had missing region where disease was acquired, or adverse health event took place that required unplanned healthcare
Cause of death: Pulmonary tuberculosis (1), skin and soft tissue infection with an antibiotic resistant organism (1)
Table 2.
Top destinations where travellers received unplanned and planned healthcare abroad
| Countrya | Unplanned (1093) column% | Countryb | Planned (n = 41) column % |
|---|---|---|---|
| India | 110 (10) | United States | 6 (15) |
| Thailand | 60 (5) | France | 5 (12) |
| Mexico | 45 (4) | Dominican Republic | 4 (10) |
| Indonesia | 33 (3) | Belgium | 3 (7) |
| Philippines | 28 (3) | Mexico | 3 (7) |
| Romania | 27 (2) | Colombia | 2 (5) |
| Viet Nam | 27 (2) | Japan | 2 (5) |
| Tanzania | 26 (2) | South Africa | 2 (5) |
| Dominican Republic | 25 (2) | Thailand | 2 (5) |
| Cambodia | 24 (2) | Turkey | 2 (5) |
Additional destinations where ≥10 travellers reported unplanned healthcare: Cameroon (24), Cuba (21), Peru (21), Ghana (20), Uganda (20), Saudi Arabia (19), Cote d’Ivoire (18), Democratic Republic of the Congo (18), Nigeria (18), Pakistan (18), Turkey (17), Equatorial Guinea (16), United States (16), Colombia (15), Sweden (15), Spain (14), Benin (13), Ethiopia (13), Kenya (12), Brazil (11), Ecuador (11), Sri Lanka (11), Bolivia (10), Senegal (10). In 97 destinations, <10 travellers each reported receiving unplanned healthcare.
Additional destinations where travellers reported planned healthcare (1 each): Chile, Ecuador, French Guiana, Guinea, India, Israel, Morocco, Myanmar, Peru, Serbia
Unplanned healthcare was obtained most frequently for evaluation of medical conditions (n = 1058; 97%), followed by injury (n = 30; 3%) and dental care (n = 5; 0.5%). The most common interventions received abroad were diagnostic procedures (n = 810; 35%), antimicrobials (n = 771; 33%), medical observation (n = 394; 17%) and injection/infusions (n = 302; 13%). The most frequent healthcare settings were hospitals (n = 617; 56%), outpatient clinics (n = 211; 19%) and private physician’s offices (n = 111; 10%). Few patients had complications (n = 13; 1%) from the healthcare they obtained abroad. Patients reported that their presenting conditions were completely resolved (n = 176; 16%), improved (n = 640; 59%) or unchanged (n = 230; 21%); few patients (n = 34; 3%) subsequently deteriorated. Among 1488 diagnoses made in 1093 patients, the top four diagnoses were acute diarrhoea (n = 119), uncomplicated dengue (n = 88), falciparum malaria (n = 81) and unspecified viral syndrome with or without rash (n = 66) (Table 3). Completed reports on healthcare exposure during travel were more frequently obtained from travellers evaluated at GeoSentinel sites after travel (n = 1004; 92%) rather than during travel (n = 87; 8%).
Table 3.
Top diagnoses among travellers with unplanned healthcare received abroad
| Diagnosis | n = 1093 travellers |
|---|---|
| Acute unspecified diarrhoea | 119 (11) |
| Uncomplicated dengue fever | 88 (8) |
| Falciparum malaria | 81 (7) |
| Unspecified viral syndrome with or without rash | 66 (6) |
| Chronic unspecified diarrhoea | 55 (5) |
| Unspecified febrile illness (< 3 weeks) | 46 (4) |
| Upper respiratory tract infection | 30 (3) |
| Skin and soft tissue infection: erysipelas, cellulitis, gangrene | 26 (2) |
| Pyelonephritis | 21 (2) |
| Skin and soft tissue infection: skin abscess or secondary bacterial infection of existing lesion | 18 (2) |
Travellers with planned healthcare abroad
Forty-one travellers sought planned healthcare abroad in 20 countries. Median age was 41 years (range: 2–81); 25 (63%) were female (Table 1). The most common reasons for planned travel were unavailability of the procedure where the patient resided (n = 9; 22%), clinical expertise abroad (n = 9; 22%), lower cost (n = 8; 20%), greater convenience (n = 7; 17%), seeking a second opinion (n = 4; 10%), care provided by a trusted known doctor (n = 3; 7%) and anonymity (n = 1; 2%). Despite planning for healthcare abroad, only four travellers (10%) reported having a pre-travel healthcare encounter (Table 1). The most common destination countries where travellers obtained planned healthcare were the United States (n = 6; 15%), France (n = 5; 12%), the Dominican Republic (n = 4; 10%), Belgium (n = 3;7%) and Mexico (n = 3; 7%) (Table 2). The most frequent types of planned healthcare were for medical care (n = 19; 46%), cosmetic procedures (n = 9; 22%), surgical care (n = 4; 10%) and check-up or consultation (n = 4; 10%). Procedures included surgeries (cosmetic, cardiac, cholecystectomy, herniorrhaphy, ophthalmologic, orthopaedic and laryngomalacia surgery), obstetric care and dental care.
The most frequent healthcare settings were hospitals (n = 25; 61%), outpatient clinics (n = 8; 20%) and free-standing surgical facilities (n = 3; 7%); for five patients (12%) the healthcare facility was not reported. Median length of stay at hospitals was 6.5 days (range 0–30). Twenty-three (57%) patients reported uneventful courses, 14 (33%) experienced early complications (infection, pain, repeat procedures within 30 days of healthcare encounter) and 4 (10%) reported late complications (infection, fistula 30 days or more after healthcare encounter). Among 16 patients given antimicrobial therapy, the most common agents received were cephalosporin (n = 5) and penicillin (n = 3) antibiotics. Twenty-two (54%) patients who received planned healthcare abroad were hospitalized; 13 (32%) of the 41 were hospitalized after return from travel. The diagnoses for which travellers were seen at GeoSentinel sites after their planned healthcare abroad included: atypical mycobacterial skin lesion (3), skin and soft tissue infection (3), bacteremia (2), cutaneous leishmaniasis (2) and schistosomiasis (2) (Table 4).
Table 4.
Diagnoses among travellers with planned healthcare received abroada
| Diagnosis | n = 41 travellers |
|---|---|
| Atypical mycobacterium skin lesion | 3 (7) |
| Skin and soft tissue infection: skin abscess or secondary bacterial infection of existing lesion | 3 (7) |
| Bacteremia | 2 (5) |
| Cutaneous leishmaniasis | 2 (5) |
| Schistosomiasis, human species unknown | 2 (5) |
These diagnoses may or may not related to the planned healthcare abroad Note: Twenty-nine more diagnoses were identified to affect one traveller each
Discussion
International travellers may encounter healthcare abroad because of health problems that arise as a result of acute travel-related illness, exacerbations of pre-existing conditions or from plans made in advance to obtain care at the destination. This study provides a more in-depth understanding about the type of facilities where travellers sought care, interventions received, invasive procedures and antibiotics used, and outcomes. Reasons for obtaining unplanned healthcare during travel frequently included conditions that could have potentially been prevented through a comprehensive travel consultation with vaccinations and preventive advice, including use of malaria prophylaxis, insect avoidance methods, self-treatment of diarrhoea and injury prevention. Reasons for obtaining planned healthcare abroad varied. Among all who obtained care in another country, most reported favourable outcomes of their condition although some deterioration or associated complications were reported.
Previous studies have found that a substantial proportion of travellers developed health problems during travel and a broad range may obtain healthcare abroad.2–5 Among 628 travellers from the Boston area surveyed, 49% reported health problems during travel, 7% sought medical care and 1% required hospitalization abroad.3 Similarly, among 460 travellers recruited in a Finnish travel clinic, 76% reported illness during travel; 13% sought medical evaluation and 0.9% were hospitalized abroad.4 Among 198 short-term volunteers from Europeto Cambodia, 57% sought medical assistance.5 However, details of the travellers’ healthcare abroad were not studied. In a recent study of 517 U.S. residents travelling internationally for a planned medical or dental surgery, treatment or procedure, 24 (5%) reported an unexpected or undesirable oucome as a result; 18 (64%) of the 24 needed to see a healthcare provider after returning to the United States.11
Unplanned healthcare
Among this cohort of travellers seen in GeoSentinel clinics during or after their trip, 1093 travellers sought care for a medical or dental issue that was an unanticipated part of the travellers’ planned itinerary (unplanned healthcare). Unplanned healthcare was received in a diverse range of 131 countries reflecting both the broad capture of travel destination among the GeoSentinel network and the wide geographical risks of health problems during travel (Figure 2).
The diagnosis of health problems abroad and treatment received was also varied. Dengue, malaria and unspecified febrile illnesses were among the common diagnoses abroad, which substantiate other studies that highlighted fever as a major problem among travellers.15,16 Our study identified the receipt of an antimicrobial agent while abroad in up to one-third of travellers and up to 13% received injections or infusion. There are potential risks especially if given in resource-limited locations with suboptimal quality healthcare and limited means for infection prevention and control, including the use of improper medications, poor medication quality or procedure-related infection.17–19 Moreover, unnecessary use of antibiotics during travel may contribute to increasing antimicrobial resistance in the global context as previously reported in several studies.20–23
In our study, only 37% of those reporting unplanned healthcare abroad obtained pre-travel advice, raising concerns about knowledge regarding how to choose optimal healthcare facilities if the need arose. Pre-travel consultation might have prevented the need for care abroad, especially when considering the top three diagnoses in our study: acute diarrhoea, uncomplicated dengue and falciparum malaria. The pre-travel consultation would include a discussion about what to do if a traveller becomes ill and how to select optimal care abroad. Travellers should be advised to investigate the quality and accreditation of healthcare facilities, utilizing resources such as the ISTM Global Travel Clinic Directory (https://www.istm.org/AF_CstmClinicDirectory.asp) or the Joint Commission International for accredited organizations (https://www.jointcommissioninternational.org/about-jci/accredited-organizations/), and to seek information from the traveller’s own national agency (e.g. US Department of State; https://travel.state.gov/content/travel/en/international-travel/before-you-go/your-health-abroad.html). Furthermore, travellers should be advised to seek care from providers with Certificate in Travel Health™ if possible.
The Covid-19 pandemic has raised more uncertainty about travel and concern about potentially unexpected need for medical evaluation and treatment during travel. During this period, travellers may have secured travel assistance programs such as travel health insurance and medical evacuation insurance that might help to locate appropriate providers and healthcare facilities for the traveller. Hence, travel assistance programs may be underutilized sources that could contribute detailed understanding about during-travel unplanned healthcare needs. Moreover, the digital era has led to the development of many mobile applications related to travellers’ health, which should be explored as possible solutions to improve healthcare during travel.
Planned healthcare
Travellers who received planned healthcare abroad (some also known as medical tourists) are well known in the tourism and hospitality sector. However, there has been limited research conducted by the travel medicine community and there are few published data on the actual health risks of this population. Although the patient numbers were relatively small in this analysis, the data showed that travellers sought planned healthcare for a wide range of reasons as well as in diverse countries, and characterized the frequency and severity of complications after receiving healthcare abroad. The most frequently reported reasons were attributed to the expertise at destination (i.e. procedure/medication unavailable at home, clinical expertise abroad, second opinion and trusted doctor) and lower cost.
Up to one-third (n = 14; 33%) of the 41 travellers who received planned healthcare abroad developed early complications, whereas four (10%) developed late complications which may have impacted the trip. Prior studies have documented some risk for hospital-associated and procedure-related infections as well as for locally endemic infections for certain medical tourists.24–26 We found that some complications were directly related to healthcare received abroad such as wound infections, repeat procedures and fistula—the risks of which may be reduced by choosing higher quality healthcare facilities with high standard of care including adequate infection prevention and control procedures. In this analysis, up to half of the travellers that planned healthcare abroad received a procedure abroad such as body contouring, breast surgery and cholecystectomy; therefore, it is important that medical tourists are aware of infection-related complications. Only four (10%) of the travellers in our cohort with planned healthcare sought pre-travel advice, far less than other types of travellers.27–29 Several possible reasons included the concern for stigma resulting in withholding information from their primary care provider, or that they entrusted the treatment provider abroad or medical tourism organizer to inform them of travel-related health preparations and risks. Proper pre-travel consultation could potentially prevent complications and provide advice regarding strategies if complications arise. Although excellent reviews on pre-travel advice have focused on many types of travellers (e.g. backpacker, business travellers),30 travellers with planned healthcare abroad were rarely explored. Unfortunately, our small sample size did not allow any conclusions, and this is worth exploring in future research.
Fortunately, in this cohort of travellers with planned healthcare abroad, none developed serious or life threatening complications after receiving care abroad. However, serious or even fatal complications among medical tourists have been reported in several studies.31–34
Despite the dramatically reduced volume of international travel due to the Covid-19 pandemic, medical tourism will likely resume and increase in the near future. In addition to conventional medical tourism, some recent phenomena include travel for Covid-19 vaccination or even death tourism (travel for euthanasia).35,36 Apart from health-related issues, medical tourism will inevitably be associated with diverse financial, legal, moral and ethical issues.8
Limitations
Data may not be representative of all travellers who received healthcare abroad or representative of all travellers who received healthcare abroad in the GeoSentinel Network as some sites did not submit supplemental data on the travellers’ planned or unplanned care. Patients may not have disclosed important details about care abroad unless clinicians inquired specifically. The data contain nuances that complicate the interpretation. For instance, this analysis considers ‘home’ to be the country where a traveller is living, which may differ from the ‘country of origin’ and the ‘country of permanent residence.’ Also, the planned healthcare cohort includes expatriates who may have been diagnosed with diseases endemic in the countries in which they were living, but who sought healthcare in their countries of origin or permanent residence. Additionally, data on disease outcomes (e.g. requiring hospital or ICU admission) were limited to travellers with unplanned healthcare; for travellers with planned healthcare, hospital admissions reflected the facility type where a procedure was performed not severity of disease.
The GeoSentinel network analysis is not a systematic analysis of healthcare during travel among all international travellers but is a convenience sample of patients presenting to one of the large number of network clinics with wide ranging patient catchment. As such, these data may be biased towards travellers who sought evaluation in specialized travel and tropical medicine clinics, whereas patients without complications would likely not have sought medical attention. The database does not include insurance coverage information, which may influence a traveller’s decision regarding obtaining care abroad. The study period was mainly prior to the Covid-19 pandemic; therefore, these findings would not reflect occurrences during the pandemic. Finally, it is important to note that accident and injury are also major risks for travellers.37 However, since most Geosentinel clinics do not specialize in trauma/injury, travellers that encountered accidents and injuries abroad may not be represented in this study.
Conclusion
Travellers who sought healthcare during travel for unexpected health problems often had conditions for which pre-travel consultation could provide vaccinations, chemoprophylaxis or advice that may have mitigated the need to present to a healthcare facility during the trip. Analysing healthcare needs during travel provides useful insights to inform priorities for pre-travel advice. Furthermore, travellers undertaking planned healthcare abroad are diverse and have been rarely studied in the travel medicine community. We have described some adverse health consequences that can occur from treatments received abroad, conditions for which pre-travel consultations could provide advice and prevent complications. This analysis provided a framework for evaluating medical tourists with suspected infections and reinforces the need for improvement to ensure broad access to high quality health services, continuity of care and surveillance for post-procedure complications.
Supplementary Material
Acknowledgement
The authors thank Mary E. Wilson and Kristina Angelo for their suggestions and Charles Miller for technical support.
*Additional members of the GeoSentinel Surveillance Network who contributed data but did not author this article are: Carsten Schade Larsen and Christian Wejse (Aarhus, Denmark), Emmanuel Bottieau (Antwerp, Belgium), Jesse Waggoner and Henry Wu (Atlanta, USA), Israel Molina and Fernando Salvador Velez (Barcelona, Spain), Frank Mockenhaupt and Gundel Harms-Zwingenberg (Berlin, Germany), Denis Malvy and Alexandre Duvignaud (Bordeaux, France), Elizabeth Barnett and Dan Bourque (Boston, USA), Francesco Castelli and Alberto Matteelli (Brescia, Italy), Simin Aysel Florescu and Corneliu Petru Popescu (Bucharest, Romania), Stephen Vaughan and Susan Kuhn (Calgary, Canada), Tari Papavarnavas and Salim Parker (Cape Town, South Africa), Loïc Epelboin (Cayenne, French Guiana), Francoise Chappuis and Gilles Eperon (Geneva, Switzerland), Matteo Bassetti and Federica Toscanini (Genova, Italy), Jasper Chan and Kwok-Yung Yuen (Hong Kong, China), Johnnie Yates (Honolulu, USA), Lucille Blumberg and Albie de Frey (Johannesburg, South Africa), Michael Beadsworth and Nicolas Beeching (Liverpool, United Kingdom), Jose Perez-Molina and Francesca Norman (Madrid, Spain), Philippe Gautret and Emilie Javelle (Marseille, France), Bill Stauffer (Minnesota, USA), Sapha Barkati and Cedric Yansouni (Montreal, Canada), Christina Greenaway (Montreal, Canada), Arpita Chakravarti (Montreal, Canada), Federico Gobbi and Andrea Rossanese (Negrar, Italy), Christina Coyle (New York, USA), Stefan Hagmann (New York, USA), Carmelo Licitra (Orlando, USA), Frank Patterson (Oslo, Norway), Anne McCarthy (Ottawa, Canada), Eric Caumes and Paul Henri Consigny (Paris, France), Bronx Lebanon (Peekskill, USA), Els Van Nood (Rotterdam, the Netherlands), Daniel Leung and Jakrapun Pupaibool (Salt Lake City, USA), Cecilia Perret Perez (Santiago, Chile), Mugen Ujiie and Kei Yamamoto (Tokyo, Japan), Andrea Boggild and Kevin Kain (Toronto, Canada), Pierre Plourde and Jackie Shackel (Winnipeg, Canada), Yukihiro Yoshimura and Natsuo Tachikawa (Yokohama, Japan).
Source of funding
GeoSentinel, the Global Surveillance Network of the International Society of Travel Medicine (ISTM), is supported by a cooperative agreement (U50CK00189) from the Centers for Disease Control and Prevention (CDC), as well as funding from the ISTM and the Public Health Agency of Canada.
Footnotes
Conflict of interest/Disclosure
The authors have declared no conflicts of interest.
This study, in part, was presented at 69th Annual meeting of the American Society of Tropical Medicine and Hygiene, 15–19 November 2020 and at the 17th Congress of the International Society of Travel Medicine (CISTM17), 19–22 May 2021. The abstract was also presented at the International Congress on Infectious Diseases (ICID) 2022, Kuala Lumpur, Malaysia, November 17–20, 2022.
Data availability
The data underlying this article were provided by GeoSentinel Surveillance Network by permission. Data will be shared on request to the corresponding author with permission of GeoSentinel.
References
- 1.UNWTO. World Tourism Barometer 2022; January 18. https://www.unwto.org/news/tourism-grows-4-in-2021-but-remains-far-below-pre-pandemic-levels. 17 April 2022, date last accessed.
- 2.Angelo KM, Kozarsky PE, Ryan ET et al. What proportion of international travellers acquire a travel-related illness? A review of the literature. J Travel Med 2017; 24. 10.1093/jtm/tax046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen LH, Han PV, Wilson ME et al. Self-reported illness among Boston-area international travelers: a prospective study. Travel Med Infect Dis 14:604–13. 10.1016/j.tmaid.2016.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vilkman K, Pakkanen SH, Lääveri T et al. Travelers’ health problems and behavior: prospective study with post-travel follow-up. BMC Infect Dis 2016; 16:328. 10.1186/s12879-016-1682-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barrio-Cortes J, Rojas-Muñoz C, Acosta-Benito MÁ et al. Health problems encountered by short-term European volunteers in a non-governmental Organization in Cambodia. Am J Trop Med Hyg 2022; 106:985–92. 10.4269/ajtmh.21-0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen LH, Wilson ME. The globalization of healthcare: implications of medical tourism for the infectious diseases clinician. Clin Infect Dis 2013; 57:1752–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crooks VA, Kingsbury P, Snyder J, Johnston R. What is known about the patient’s experience of medical tourism? A scoping review. BMC Health Serv Res 2010; 10:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen IG. Patients with Passports: Medical Tourism, Law, and Ethics. New York: Oxford University Press; 2015. 10.1093/acprof:oso/9780199975099.001.0001. [DOI] [Google Scholar]
- 9.Lunt N, Smith R, Exworthy M et al. Medical tourism: treatments, markets and health system implications: a scoping review. OECD 2011. http://www.oecd.org/els/health-systems/48723982.pdf 8 July 2022, date last accessed. [Google Scholar]
- 10.Foley BM, Haglin JM, Tanzer JR, Eltorai AEM. Patient care without borders: a systematic review of medical and surgical tourism. J Travel Med 2019; 26:taz049. 10.1093/jtm/taz049. [DOI] [PubMed] [Google Scholar]
- 11.Stoney RJ, Kozarsky PE, Walker AT, Gaines JL. Population-based surveillance of medical tourism among US residents from 11 states and territories: findings from the Behavioral risk factor surveillance system. Infect Control Hosp Epidemiol 2022;43(7):870–75. 10.1017/ice.2021.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamer DH, Rizwan A, Freedman DO et al. GeoSentinel: past, present and future. J Travel Med 2020; 27:taaa219. 10.1093/jtm/taaa219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muehlenbein MP, Angelo KM, Schlagenhauf P et al. Traveller exposures to animals: a GeoSentinel analysis. J Travel Med 2020; 27:taaa010. 10.1093/jtm/taaa010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gautret P, Angelo KM, Asgeirsson H et al. Rabies post-exposure prophylaxis started during or after travel: a GeoSentinel analysis. PLoS Negl Trop Dis 2018; 12:e0006951. 10.1371/journal.pntd.0006951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Camprubí-Ferrer D, Cobuccio L, Van Den Broucke S et al. Causes of fever in returning travelers: a European multicenter prospective cohort study. J Travel Med 2022; 29:taac002. 10.1093/jtm/taac002. [DOI] [PubMed] [Google Scholar]
- 16.Buss I, Genton B, D’Acremont V. Aetiology of fever in returning travellers and migrants: a systematic review and meta-analysis. J Travel Med 2020; 27:taaa207. 10.1093/jtm/taaa207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kolars JC. Rules of the road: a consumer’s guide for travelers seeking health care in foreign lands. J Travel Med 2002; 9:198–201. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Medicines: spurious/falsely-labelled/falsified/counterfeit (SFFC) medicines [fact sheet no. 275]. Geneva: World Health Organization; 2012. www.who.int/mediacentre/factsheets/fs275/en/17 June 2022, date last accessed. [Google Scholar]
- 19.Centers for Disease Prevention and Control. CDC Health Information for International Travel 2020. The Yellow Book, New York: Oxford University Press; 2020. [Google Scholar]
- 20.Kuenzli E, Jaeger VK, Frei R et al. High colonization rates of extended-spectrum β-lactamase (ESBL)-producing Escherichia coli in Swiss travellers to South Asia- a prospective observational multicentre cohort study looking at epidemiology, microbiology and risk factors. BMC Infect Dis 2014; 14:528. 10.1186/1471-2334-14-528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paltansing S, Vlot JA, Kraakman ME et al. Extended-spectrum β-lactamase-producing enterobacteriaceae among travelers from the Netherlands. Emerg Infect Dis 2013; 19:1206–13. 10.3201/eid.1908.130257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kajova M, Khawaja T, Kangas J et al. Import of multidrug-resistant bacteria from abroad through interhospital transfers, Finland, 2010–2019. Euro Surveill 2021; 26:2001360. 10.2807/1560-7917.ES.2021.26.39.2001360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kantele A, Lääveri T, Mero S et al. Antimicrobials increase travelers’ risk of colonization by extended-spectrum betalactamase-producing Enterobacteriaceae. Clin Infect Dis 2015; 60:837–46. 10.1093/cid/ciu957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pavli A, Maltezou HC. Infectious complications related to medical tourism. J Travel Med 2021; 28:taaa210. 10.1093/jtm/taaa210. [DOI] [PubMed] [Google Scholar]
- 25.Nelwan EJ, Andayani D, Clarissa G, Pramada T. Vancomycin-resistant staphylococcus aureus infection post-liposuction in South Korea. Cureus 2021; 13:e14357. 10.7759/cureus.14357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cusumano LR, Tran V, Tlamsa A et al. Rapidly growing mycobacterium infections after cosmetic surgery in medical tourists: the Bronx experience and a review of the literature. Int J Infect Dis 2017; 63:1–6. 10.1016/j.ijid.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 27.Pfeil A, Mütsch M, Hatz C, Szucs TD. A cross-sectional survey to evaluate knowledge, attitudes and practices (KAP) regarding seasonal influenza vaccination among European travellers to resource-limited destinations. BMC Public Health 2010; 10:402. 10.1186/1471-2458-10-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang M, Zhang J, Hao Y et al. Vaccination knowledge, attitude and practice among Chinese travelers who visit travel clinics in preparation for international travel. J Travel Med 2016; 23:taw051. 10.1093/jtm/taw051. [DOI] [PubMed] [Google Scholar]
- 29.Toovey S, Jamieson A, Holloway M. Travelers’ knowledge, attitudes and practices on the prevention of infectious diseases: results from a study at Johannesburg international airport. J Travel Med 2004; 11:16–22. 10.2310/7060.2004.13587. [DOI] [PubMed] [Google Scholar]
- 30.Kain D, Findlater A, Lightfoot D et al. Factors affecting pre-travel health seeking behaviour and adherence to pre-travel health advice: a systematic review. J Travel Med 2019; 26:taz059. 10.1093/jtm/taz059. [DOI] [PubMed] [Google Scholar]
- 31.Mason A, Bhati S, Jiang R, Spencer EA. Medical tourism patient mortality: considerations from a 10-year review of global news media representations. In: Merviö M ed. Global Issues and Innovative Solutions in Healthcare, Culture, and the Environment. Hershey, PA: IGI Global, 2020. 10.4018/978-1-7998-3576-9. [DOI] [Google Scholar]
- 32.Turner L News media reports of patient deaths following ‘medical tourism’ for cosmetic surgery and bariatric surgery. Dev World Bioeth 2012; 12:21–34. 10.1111/j.1471-8847.2012.00320.x. [DOI] [PubMed] [Google Scholar]
- 33.Večerić-Haler Ž, Borštnar Š, Luzar B et al. Multiorgan failure with fatal outcome after stem cell tourism. Eur J Med Res 2021; 26:5. 10.1186/s40001-020-00477-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kracalik I, Ham DC, McAllister G et al. Extensively drug-resistant Carbapenemase-producing Pseudomonas aeruginosa and medical tourism from the United States to Mexico, 2018–2019. Emerg Infect Dis 2022; 28:51–61. 10.3201/eid2801.211880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bauer IL. Death as attraction: the role of travel medicine and psychological travel health care in ‘dark tourism’. Trop Dis Travel Med Vaccines 2021; 7:24. 10.1186/s40794-021-00149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steele S, Worswick D. Destination death: a review of Australian legal regulation around international travel to end life. J Law Med 2013; 21:415–28. [PubMed] [Google Scholar]
- 37.Wyler BA, Young HM, Hargarten SW, Cahill JD. Risk of deaths due to injuries in travellers: a systematic review. J Travel Med 2022; 29:taac074. 10.1093/jtm/taac074. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article were provided by GeoSentinel Surveillance Network by permission. Data will be shared on request to the corresponding author with permission of GeoSentinel.


