Abstract
Objective:
Anxiety sensitivity and coping motives for substance use are processes implicated in anxiety and substance use disorder (SUD) comorbidity, and are malleable treatment targets. Little is known about whether changes in anxiety sensitivity or coping motives during cognitive behavioral therapy (CBT) for anxiety disorders (with or without CBT for SUD) mediate substance use outcomes among patients with comorbid anxiety disorders and SUD. We examined whether changes in anxiety sensitivity and coping motives during treatment for comorbid SUD and anxiety disorders (either CBT for SUD only or CBT for SUD and anxiety disorders) were associated with substance use outcomes.
Methods:
Repeated measurements of anxiety sensitivity and coping motives throughout treatment were examined from a randomized clinical trial comparing usual, CBT-based treatment at a substance use disorder specialty clinic (UC) to that usual care plus a brief CBT for anxiety program for patients with comorbid anxiety and substance use disorders (CALM ARC).
Results:
Anxiety sensitivity decline during treatment was significantly steeper among those who received CALM ARC than those in UC. Decreases in anxiety sensitivity mediated the effect of treatment group on alcohol use following treatment such that the greater reduction in anxiety sensitivity in CALM ARC explained the superior outcomes for alcohol use in CALM ARC compared to UC. Declines in substance use coping motives were not observed in either condition, and did not differ between CALM ARC and UC. Thus, declines in coping motives did not mediate substance use after treatment.
Conclusions:
These findings provide preliminary evidence suggesting alcohol use outcomes were related to decreasing anxiety sensitivity rather than decreasing coping motives. Implications and future directions are discussed.
Self-medication (Khantzian, 1985), tension-reduction (Conger, 1956), motivational (Cox & Klinger, 1988), mutual-maintenance (Stewart & Conrod, 2008), and negative reinforcement (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004) models posit that individuals use substances to alleviate anxiety, and that the negatively reinforcing effects of substances may lead to a pattern of maladaptive substance use. Therefore, targeting anxiety symptoms among those with comorbid anxiety disorders and SUD should not only improve anxiety symptoms, but decrease substance use as well. Indeed, a small body of research indicates that integrated treatments for anxiety disorders and SUD are effective in reducing substance use (Najavits, 2002; Kushner et al., 2006). We recently demonstrated that the addition of a brief cognitive behavioral therapy (CBT) program for anxiety disorders to usual care at a SUD specialty clinic was superior to usual care alone in reducing anxiety symptoms, drinking, and drug use (Wolitzky-Taylor et al., 2018).
It remains unclear how CBT for anxiety exerts its effects on substance use. Examining treatment mediators can increase understanding about how a treatment works in order to develop more targeted and effective approaches. Moreover, knowledge of the processes leading to change during treatment can help clinicians determine whether the targeted mechanisms are indeed changing for individual patients during treatment and can thus be used as a treatment decision-making tool to enhance outcomes.
1. Anxiety sensitivity as a putative mediator of SUD outcomes
Anxiety sensitivity, implicated in the onset and maintenance of both anxiety disorders and SUD, is characterized by the degree to which an individual is prone to misappraise physiological anxiety symptoms as having harmful physical, social, and mental consequences (Reiss, Peterson, Gursky, & McNally, 1986). Anxiety sensitivity is elevated across many anxiety disorders (Olatunji & Wolitzky-Taylor, 2009), and is associated with SUD onset (Schmidt, Buckner, & Keough, 2007; Schmidt, Eggleston et al., 2007), substance severity and use (Buckner et al., 2011; Comeau, Stewart, & Loba, 2001; Hearon et al., 2011) and poor SUD treatment outcomes (Lejuez et al., 2008). Notably, anxiety sensitivity has been found to mediate the association between anxiety disorder symptoms and substance use (Wolitzky-Taylor et al., 2015), suggesting that the associations between anxiety and substance use may be explained by the degree to which an individual misappraises physiological sensations of arousal as having negative consequences.
Importantly, anxiety sensitivity is malleable. It mediates symptom outcomes in CBT for anxiety disorders, and is thought to be a core process targeted in CBT for anxiety (Meuret, Rosenfield, Seidel, Bhaskara, & Hofmann, 2010; Smits, Powers, Cho, & Telch, 2004; Arch, Wolitzky-Taylor, Eifert, & Craske, 2012). Relatedly, studies have demonstrated the success of brief CBT protocols to reduce anxiety sensitivity for prevention of problem drinking (Conrod, Castellanos-Ryan, & Mackie, 2011; Conrod et al., 2013; Schmidt, Buckner, et al., 2007; Watt, Stewart, Birch, & Bernier, 2006) and in the treatment of SUD (Schmidt, Raines, Allan & Zvolensky, 2016). Although anxiety sensitivity has been demonstrated as a mediator of change in anxiety symptoms during CBT for anxiety disorders, no study to our knowledge has investigated whether changes in anxiety sensitivity during CBT for anxiety disorders predict subsequent improvement in substance use in SUD treatment seekers.
2. Coping motives for substance use as a putative mediator of SUD outcomes
Coping motives for substance use (i.e., using drugs or alcohol to alleviate distress or cope with distressing situations) are implicated in the maintenance of substance use problems and SUDs (Cooper, Kuntsche, Levitt, Barber, & Wolf, 2016). Many cognitive behavioral treatments for SUD aim to provide patients with alternative coping strategies to decrease motivation to use substances as a way to cope with unpleasant emotions or stimuli (McHugh, Hearon, & Otto, 2010). Given that coping motives contribute to substance use for individuals with anxiety symptoms in particular (Buckner, Bonn-Miller, Zvolensky, & Schmidt, 2007; Cooper et al., 2016; Kuntsche, Knibbe, Gmel, & Engels, 2006; Tate, Pomerleau, & Pomerleau, 1994), CBT for anxiety may reduce substance use by providing individuals with new coping skills for managing anxiety. Taken together, decreases in anxiety (or improvements in ability to manage anxiety adaptively) via CBT for anxiety disorders may reduce coping motives, leading to decreased substance use.
Prior studies of CBT for SUD have found that improvements in coping skills play an important role in the reduction of substance use (Cooper et al., 2016; Kiluk, Nich, Babuscio, & Carroll, 2010; Litt, Kadden, Kabela-Cormier, & Petry, 2008; Magill, Kiluk, McCrady, Tonigan, & Longabaugh, 2015). Presumably, improvement in adaptive coping strategies would be associated with decreases in motivations to use substances to cope with distress. Indeed, one study (Banes, Stephens, Blevins, Walker & Roffman, 2014) found that coping motives declined following a CBT intervention for marijuana-dependent participants. Although this study did find that change in coping motives from baseline to a 9-month follow-up (based on scores that those two cross-sectional timepoints) was associated with 9-month marijuana use outcomes, no studies to our knowledge have utilized treatment process data (i.e., repeated measurements of coping motives during treatment) to examine whether decreases in coping motives mediate drug and alcohol treatment outcomes. Examining coping motives for substance as a treatment mediator explaining reduction in substance use outcomes may be particularly relevant to examine in a clinical population with comorbid SUD and anxiety disorders. Although coping motives for substance use are clearly associated with comorbid SUD and anxiety disorders, they are a general treatment target in typical SUD care. Therefore, changes in coping motives may mediate substance use treatment outcomes in both typical SUD treatment and in SUD treatment that include CBT for anxiety disorders. Research to understand the mediational role of coping motives in this comorbid population is lacking.
The current study aimed to understand the processes of change by which two distinct treatments (i.e., CBT-based usual SUD care, called “usual care”, or UC; and CBT-based usual SUD care + CBT for anxiety disorders, called “CALM for Addiction Recovery Centers”, or “CALM ARC”) leads to reduced substance use in patients with comorbid anxiety disorders and SUD by investigating two hypothesized mediators: 1) decreases in anxiety sensitivity and 2) decreases in coping motives for substance use. A small body of research has evaluated the addition of CBT to usual treatment for SUD for comorbid SUD and anxiety disorders relative to usual treatment alone (Kushner et al., 2006; Randall, Thomas, & Thevos, 2001), and some research has examined whether CBT for SUD improves anxiety symptom outcomes (Buckner & Carroll, 2010). However, no studies to our knowledge have examined theoretical process-based treatment mediators of each approach. This comparison allows for testing of differential mediation between CBT treatment that addresses comorbidity and usual care in this unique population, which can guide the refinement of treatments by identifying active change processes.
Our first hypothesis was that decreases in anxiety sensitivity and in coping motives for substance use would be significantly steeper in the condition that included usual SUD care (UC) plus a brief, CBT program for anxiety disorders (CALM ARC; Wolitzky-Taylor et al., 2018) than UC alone. Our second hypothesis was that changes in anxiety sensitivity and coping motives would mediate treatment outcome such that differences in substance use between UC + CALM ARC and UC would be explained by differential change in anxiety sensitivity and coping motives between the two treatments.
3. Methods
3.1. Design
Data analyzed in this investigation came from a hybrid efficacy/effectiveness randomized clinical trial (RCT) aimed at evaluating the effectiveness of usual care at a community-based, CBT-based Intensive Outpatient Program for SUD (UC) compared to UC plus Coordinated Anxiety Learning and Management for Addiction Recovery Centers (CALM ARC) among patients with comorbid SUD and anxiety disorders. CALM ARC is a brief (orientation + 6 treatment sessions), group-based, computer-assisted but therapist directed cognitive behavioral treatment for anxiety disorders adapted for individuals with anxiety disorder and SUD comorbidity and delivered by SUD counselors (see Wolitzky-Taylor et al., 2018).
During treatment in the Intensive Outpatient Program (IOP), eligible participants were randomized to either (a) UC or (b) UC + CALM ARC. In order to control for therapy time, participants in UC attended family education sessions while participants in UC + CALM ARC received the CALM ARC intervention. After randomization, participants completed a pre-treatment symptom assessment, followed by seven weeks of either CALM ARC with weekly symptom assessment or matched weekly assessment only in the UC condition, post-treatment assessment and 6-month follow-up assessment.
Randomization occurred in a standardized 6-week cycle to one condition or another (NIDA, 2003) in order to accrue sufficient numbers of participants for the CALM ARC groups more quickly. Thus, participants began CALM ARC sessions or matched weekly assessments (if randomized to UC) at varying points in their course of treatment at the IOP depending on when they were assessed for eligibility into the study during the 6-week cycle. As a product of randomization, there were no differences between groups on the time from IOP initiation until study participation began, and no between-group differences in the length of IOP treatment at the addiction treatment clinic (ps > .19).
Anxiety sensitivity and coping motives were measured every other week throughout treatment (i.e., periodically during treatment), whereas substance use (i.e., drinking and drug use days) was measured only during the outcome assessments (i.e., pre-treatment, post-treatment, and follow-up). Details can be found in Wolitzky-Taylor et al. (2018).
3.2. Participants and procedures
Participants were recruited from a community-based SUD Intensive Outpatient Program as part of an RCT described above (N = 97 randomized, N = 75 completed a pre-treatment assessment, with n = 42 in UC + CALM ARC and n = 33 in UC). Only those who completed the post-treatment assessment (regardless of the number of CALM ARC or UC sessions completed; N = 60; n = 32 in UC + CALM ARC and n = 28 in UC) were included in analyses for the present study. These participants were 70% White, 60% male, and had a mean age of 35.15 (SD = 12.35). Participants were eligible if they (1) indicated at least a moderate level of distress or impairment due to anxiety symptoms (≥8 on the Overall Anxiety Severity and Impairment Scale (OASIS; Campbell-Sills et al., 2009)), (2) met the DSM-5 diagnostic criteria for at least one of the following disorders: panic disorder, agoraphobia, social anxiety disorder, specific phobia, generalized anxiety disorder, obsessive compulsive disorder, post-traumatic stress disorder, and (3) met the DSM-5 diagnostic criteria for substance use disorder (SUD), including any alcohol or non-alcohol substance of dependence. Participants were excluded if there was evidence of: (a) marked cognitive impairment; (b) unstable psychotic or manic symptoms; or (c) active suicidality (i.e., patient currently endorsed intent to harm self and was at risk for imminent harm, resulting in an immediate need for a higher level of care).
Of the participants included in these analyses (N = 60) who completed post-treatment assessment, most participants met the DSM-5 diagnostic criteria for more than one anxiety disorder (M = 2.85, SD = 1.41). However, the most common principal anxiety disorder was generalized anxiety disorder (50.0%), followed by social anxiety disorder (31.7%), panic disorder (8.3%), obsessive compulsive disorder (5.0%), posttraumatic stress disorder (3.3%), and specific phobia (1.7%). Similarly, although most participants met the DSM-5 SUD criteria for more than one substance of dependence (61.7%), the most common primary substance of dependence was alcohol (53.3%), followed by stimulants (13.3%), opiates (10.0%), cannabis (10.0%), tranquilizers/sedatives (8.3%), and cocaine (5.0%).
For more information about the participants, procedures, and treatment conditions, see Wolitzky-Taylor et al. (2018).
3.3. Measures
3.3.1. Diagnostic measure
DSM-5 diagnoses were determined using the MINI Neuropsychiatric Interview for DSM-5 (Sheehan, 2016). Interviewers were trained to at least 80% inter-rater reliability using a set of “gold standard” recorded MINI interviews prior to administering the MINI in this study. Inter-rater reliability was assessed on 22.6% of the MINIs administered, with κ = 0.80 across anxiety disorders and κ = 0.84 across SUDs.
3.3.2. Treatment process measures
Treatment process measures were examined as putative mediators. They were administered at pre-treatment, session 2, session 4, and session 6.
Anxiety sensitivity was assessed with the Anxiety Sensitivity Index (ASI; Reiss et al., 1986), which assesses misappraisals of physiological anxiety-related sensations of arousal as having social, physical, or mental consequences. Examples of items include, “It scares me when I feel faint,” and “When I cannot keep my mind on a task, I worry that I am going crazy.” The ASI is comprised of three factors: social, physical, and mental concerns about bodily sensations of anxiety. Psychometrically, the ASI has good internal consistency and stable test-retest reliability (Maller & Reiss, 1992). In the present sample, the Cronbach’s α was 0.87.
Drinking and drug use coping motives were measured using the 5-item subscale from the Drinking Motives Questionnaire (DMQ; Cooper, Russell, Skinner, & Windle, 1992). The coping motives subscale of the DMQ has been validated with adequate internal consistency and reliability in samples of older adults and university students (Cooper et al., 1992; Gilson et al., 2013; Stewart, Zeitlin, & Samoluk, 1996). Instructions (but not items) on the measure were adapted to assess coping motives for both drinking and drug use. Specifically, the instructions stated, “Below is a list of reasons why some people drink alcohol or use drugs. If you ever drink alcohol or use drugs, please indicated how often you drink or use for each of the following reasons, by circling whichever number applies.” Examples of items include, “To relax,” and “To forget your worries.” Responses were rated on a 4-point scale from 1 (almost never/never) to 5 (almost always) and averaged with higher scores indicating more use of coping motives when drinking or using drugs. In the present sample, the Cronbach’s α = 0.92.
3.3.3. Outcome measure
Substance use was assessed with the Timeline Followback (TLFB; Sobell & Sobell, 1995). The TLFB was used to gather information about the number of drinking days and the number of drug use days in the past 30 days. Any type of drug use on any day was combined to form a single indicator (i.e., if someone used more than one drug on a given day, the day was only counted once). The TLFB was administered at pre-treatment and post-treatment assessment, which occurred during a face-to-face visit scheduled after the session 6 questionnaires were completed online. Therefore, change in anxiety sensitivity and coping motives for substance use (including the final measurement of each of these constructs) preceded the post-treatment TLFB assessment, thus establishing temporal precedence of the putative mediators (see Kraemer, Wilson, Fairburn, & Agras, 2002). However, it is important to note that the period in question (i.e., the past month) overlapped with the time in which participants were finishing the last few weeks of treatment (with no differences between groups). Trained interviewers (who independently conducted assessments after achieving at least 80% inter-rater reliability on a set of “gold standard” TLFB assessment recordings) assessed the number of drinking days and number of days of drug use (specifying drug type) in the past 30 days. Inter-rater reliability was assessed on 22.9% of the TLFB interviews from the larger original sample, with 100% agreement.
3.4. Treatment conditions
Detailed descriptions of each treatment condition can be found in Wolitzky-Taylor et al. (2018). To summarize, CALM ARC was a therapist-directed but computer-assisted group treatment, such that SUD treatment counselors presented the material directly from the Web-based program (projected onto a screen for the group). CALM ARC materials were adapted from traditional CBT for anxiety disorders to be relevant for a population with comorbid anxiety disorders and SUD, and consisted of an orientation session plus six sessions of group CBT for anxiety disorders. Orientation presented educational information about anxiety and substance use as mutually maintaining each other; session 1 included education about anxiety and cognitive restructuring; session 2 focused on setting up a plan for in vivo, interoceptive, or imaginal exposure, and assigning the first exposure home practice; sessions 3–5 focused primarily on in-session exposure and assigning and reviewing home practice of exposure; and session 6 addressed relapse prevention.
Usual care (UC) consisted of the Matrix Model of addiction treatment, an Intensive Outpatient Program which combines CBT and 12-step facilitation for SUD. Participants completed 9 h of treatment per week for approximately 2–4 months. Treatment was conducted in groups and focused on traditional CBT for SUD, including education about addiction, identifying triggers for use, developing coping plans for high risk situations, scheduling free time and increasing pleasurable (non-substance using) activities, healthy living, addressing relapse justification thoughts/beliefs, and developing coping strategies for handling emotions such as anger, guilt, or depression. Sessions also provided information about 12-step recovery and encouraged engagement in the 12-step process.
3.5. Data analysis
Analyses were conducted using Stata 14. To extract slope and intercept parameters for the ASI and the DMQ (coping subscale), hierarchical linear models (HLM) were conducted with Time (pretreatment = 0, session 2 = 1, session 4 = 2, session 6 = 3) as the level 1 predictor, treatment Condition (CALM ARC vs. UC) as the level 2 predictor, a cross-level interaction between Time and Condition, and ASI or DMQ coping scores as the outcome variables (in separate models). Least squares estimates of level 2 residuals were used to compute individual ASI intercepts and slopes for each participant. These datasets contain the ordinary least squares (OL) residuals and fitted values (FV) for each level 1 coefficient. Adding the OL residuals to the corresponding FVs produces the OL estimate of the corresponding level 1 coefficient. The OL and FV residuals are estimated for the intercept and slope.
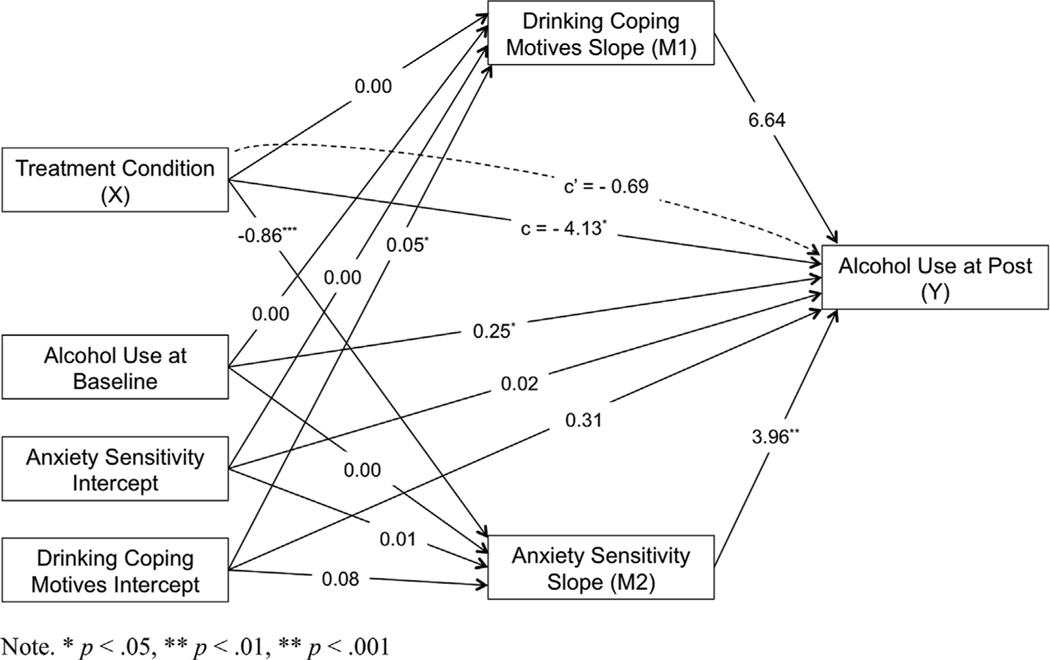
After generating individual slope and intercept parameters, we used structural equation modeling (SEM) in Stata 14 to test the slopes as mediators of the effect of treatment group on the outcome of interest (i.e., drinking days at post-treatment, drug use at post-treatment). The mediation model is shown in Fig. 1. The predictor (or X variable) was treatment condition (UC v. UC + CALM ARC), the mediators (M1 and M2) were the DMQ and ASI slopes respectively (derived from the HLM models), and covariates in the model were baseline values of the outcome of interest, and the ASI and DMQ intercepts (derived from the HLM models). A parallel set of models was run with TLFB drinking days and drug use days separately as the dependent variables, for a total of two SEM models. For the TLFB outcome measures, Satorra-Bentler robust standard errors were used, which are robust to nonnormality in SEM. Significance of indirect effects for DMQ and ASI slopes was determined using percentile bootstrapped confidence intervals with 2000 repetitions according to the guidelines of Hayes and Scharkow (2013).
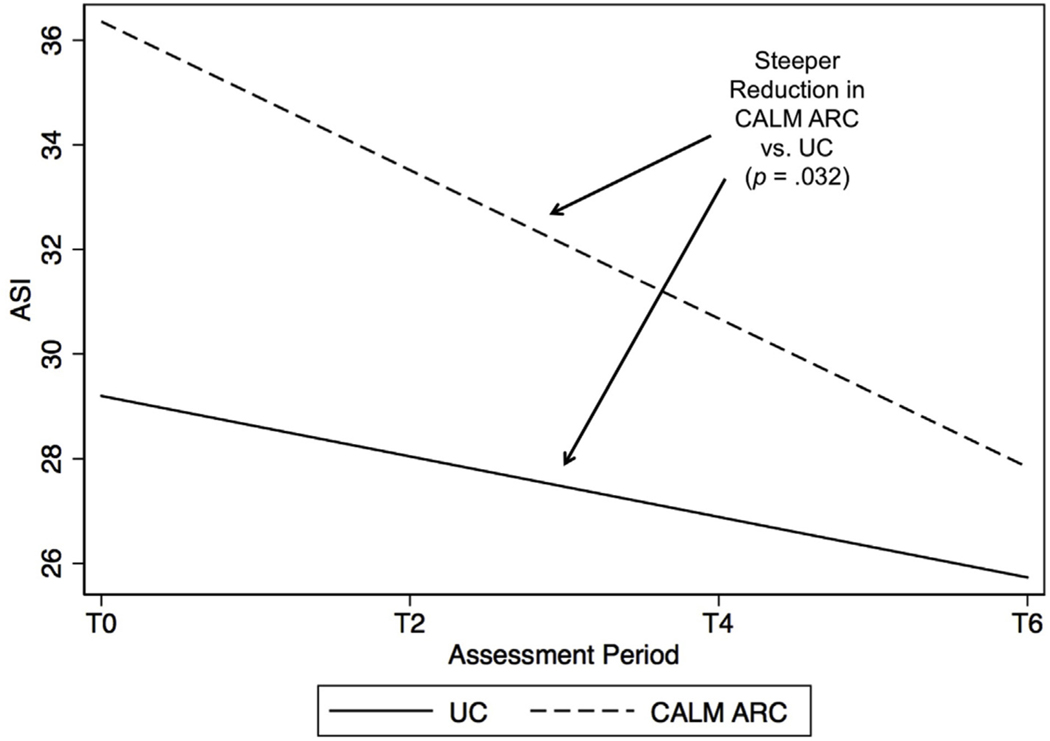
Fig. 1.
ASI decline slopes by condition.
4. Results
For descriptive information on each measure, as well as information about treatment adherence, attrition, credibility, and more detail about treatment outcomes, see Wolitzky-Taylor et al. (2018). Means for mediators and outcomes examined in the current study are shown in Table 1.
Table 1.
Means of mediators and outcomes by time point.
| Anxiety Sensitivity Mean (SD) | Coping Motives Mean (SD) | TLFB Drinking Mean (SD) | TLFB Drug Mean (SD) | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| UC | CALM ARC | UC | CALM ARC | UC | CALM ARC | UC | CALM ARC | |
|
| ||||||||
| T0 | 28.7 (12.6) | 35.9 (12.8) | 3.3 (.7) | 3.2 (1.0) | 3.3 (5.2) | 4.9 (7.9) | 2.0 (4.2) | 3.5 (6.4) |
| T2 | 28.5 (12.5) | 34.7 (12.2) | 3.3 (0.7) | 3.2 (0.9) | – | – | – | – |
| T4 | 25.0 (13.2) | 27.6 (15.9) | 3.0 (1.1) | 2.9 (1.2) | – | – | – | – |
| T6 | 25.3 (11.8) | 27.4 (12.2) | 3.0 (1.0) | 2.8 (1.1) | 5.2 (8.1) | 1.7 (3.3) | 4.6 (9.0) | 1.4 (3.7) |
Note. TLFB = Timeline Followback; T = Time; UC = Usual Care; CALM ARC = Coordinated Anxiety Learning and Management for Addiction Recovery Centers.
4.1. Slopes in the putative mediators during treatment
Decline in anxiety sensitivity during treatment: Comparison of UC to UC + CALM ARC. As shown in Fig. 1, ASI significantly declined during treatment in both UC, b = −0.58, CI = −1.15, −0.01 p = .046 and in UC + CALM ARC, b = −1.42, CI = −1.94, −0.90, p < .001. However, ASI decline slopes were significantly steeper in UC + CALM ARC compared to UC, b = −0.84, CI = −1.61, −0.07, p = .032. It should be noted that at baseline, participants in UC + CALM ARC had higher ASI scores than participants in UC (b = 7.16, CI = 1.08, 13.23, p = .021). No group differences emerged at any subsequent timepoint (ps > .066).
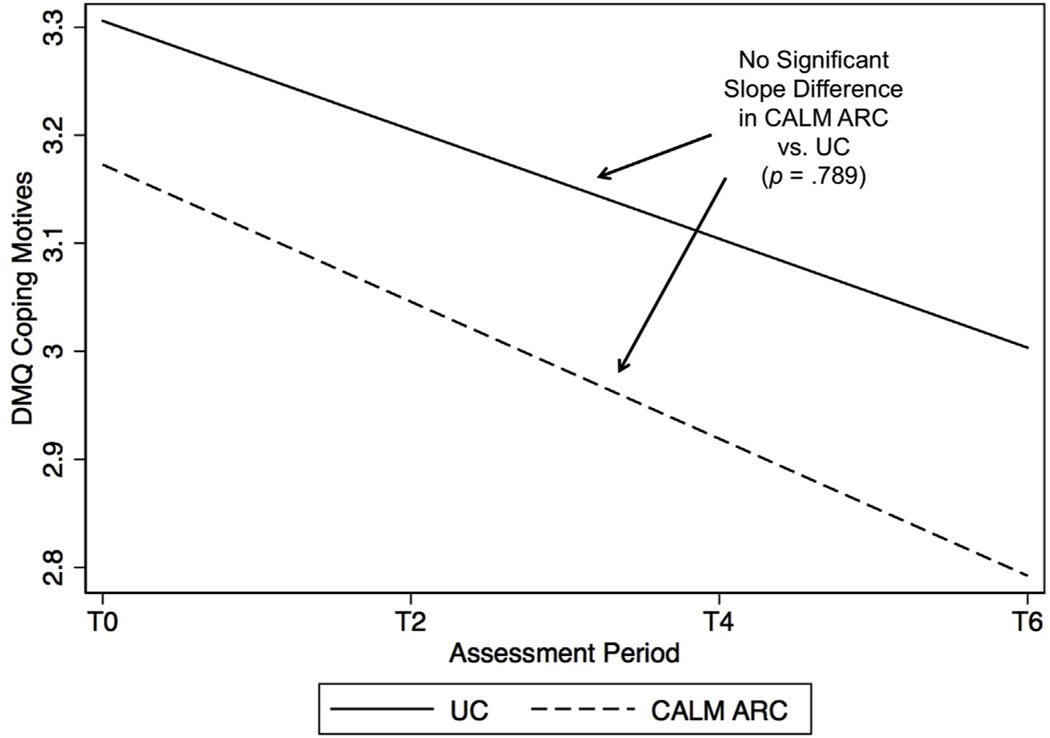
Decline in substance use coping motives during treatment: Comparison of UC to UC + CALM ARC. As shown in Fig. 2, DMQ coping did not significantly decline in UC, b = −0.05, CI = −0.12, 0.02, p = .160, or in UC + CALM ARC, b = −0.06, CI = −0.13, 0.00, p = .053. There were no significant differences between conditions on DMQ coping decline slopes, b = −0.01, CI = −0.11, 0.08, p = .789. Further, no group differences emerged at any timepoint (ps > .397).
Fig. 2.
Coping motives decline slopes by condition.
4.2. Anxiety sensitivity and substance use coping motives as mediators of substance use outcomes
Do changes in anxiety sensitivity and substance use coping motives during treatment mediate effects of treatment on number of drinking days? Model parameter estimates are shown in Fig. 3. Treatment condition was significantly associated with ASI slope with participants in UC + CALM ARC showing more negative ASI slopes compared to participants in UC. ASI slope was significantly associated with number of drinking days such that more negative ASI slopes predicted fewer drinking days. More drinking days at baseline predicted more drinking days post treatment, but no other covariates significantly predicted ASI slope or drinking days. The total effect of condition on number of drinking days was significant. However, when ASI slope was included in the model, the direct effect was no longer significant. The indirect effect of condition on number of drinking days via ASI slope was significant (b = −3.26, Percentile 95% CI = −5.88 to −0.65, p = .011). The percentage of the total effect mediated by ASI slope was 81%. Thus, ASI slope was a significant mediator of the effect of condition on number of drinking days with 81% of the condition effect explained by ASI slope.
Fig. 3.
Mediation model with parameter estimates for number of drinking days outcome. Note. *p < .05, **p < .01, **p < .001.
Treatment condition was not significantly associated with DMQ slope, and DMQ slope was not significantly associated with number of drinking days. The indirect effect of condition on number of drinking days via DMQ slope was not significant (p = .911). Thus, DMQ slope was not a significant mediator of the effect of condition on number of drinking days.
Do changes in anxiety sensitivity or coping motives during treatment mediate effects of treatment on number of drug use days? Treatment condition was significantly associated with ASI slope with participants in UC + CALM ARC showing more negative ASI slopes compared to participants in UC (b = −0.88, p < .001), but ASI slope was not significantly associated with number of drug use days (p = .129). More drug use days at baseline predicted more drug use days post treatment (b = 0.50, p = .010) and more positive ASI slopes (b = 0.01, p = .018). No other covariates significantly predicted number of drug use days (ps > .071) or ASI slopes (p > .09). The total effect of condition on number of drug use days was significant (b = −4.98, p = .012). However, when ASI slope was included in the model, the direct effect was no longer significant (p = .262). The indirect effect of condition on number of drug use days via ASI slope was not significant (p = .160). Thus, ASI slope was not a significant mediator of the effect of condition on number of drug use days.
Treatment condition was not significantly associated with DMQ slope (p = .711), and DMQ slope was not significantly associated with number of drug use days (p = .247). The indirect effect of condition on number of drug use days via DMQ slope was not significant (p = .783). Thus, DMQ slope was not a significant mediator of the effect of condition on number of drug use days.
5. Discussion
This study aimed to understand theory-driven processes of change in treatment consisting of usual care with or without adjunctive CBT for comorbid anxiety and substance use disorders. Our findings were partially consistent with our hypotheses. Decreases in anxiety sensitivity during treatment mediated changes in alcohol (but not drug) use, with greater reductions in anxiety sensitivity predictive of less alcohol use post treatment. In contrast, coping motives for substance use did not mediate drug or alcohol outcome. Anxiety sensitivity decline slopes were significantly steeper in the condition that received adjunctive CBT for anxiety disorders. Consequently, the greater improvement in alcohol use among those receiving the adjunctive anxiety treatment during SUD treatment compared to those receiving only treatment for their SUD is explained by changes in anxiety sensitivity rather than coping motives for substance use.
These findings build upon prior work demonstrating that CBT for anxiety disorders decreases anxiety sensitivity and is related to anxiety outcomes (Meuret et al., 2010; Smits et al., 2004), and that cross-sectional associations between anxiety symptoms and alcohol use problems are statistically accounted for by anxiety sensitivity (Wolitzky-Taylor et al., 2015). The current findings use longitudinal treatment process data to demonstrate that decreases in anxiety sensitivity during treatment are associated with subsequent decreases in substance use outcomes (particularly drinking days), lending support to theories suggesting that treating underlying anxiety (and in this case, reducing core processes known to mediate anxiety outcomes) improves substance use outcomes among those with comorbid anxiety and substance use disorders (e.g., Stewart & Conrod, 2008). These findings also demonstrate that anxiety sensitivity remains a malleable and critical treatment target even among complex, treatment seeking patients with SUD comorbidity.
Interestingly, anxiety sensitivity declined (albeit less steeply) in UC as well, a typical SUD treatment that utilized cognitive and behavioral strategies and principles for SUD. Although threat-laden misappraisals of physiological arousal associated with anxiety are not a target in typical SUD treatment, it is possible that as SUD treatment reduces alcohol use, individuals may experience fewer bodily sensations of arousal due to fewer experiences of intoxication and withdrawal. Possibly, this may lead to less concern about sensations that may have previously been experienced as having harmful consequences during times of more frequent substance use. Also, although UC did not explicitly address anxiety sensitivity, there were components that may have led to new ways of thinking about or managing unpleasant emotions. For example, tools presented for managing unpleasant emotions included journaling, disclosure/talking to someone about it, meditation, and assertiveness. These activities, although not framed as corrective learning experiences, may have led to decreases in anxiety sensitivity. It is also possible that the acceptance-based model of addiction as a disease to manage may have unintentionally had a positive impact on patients’ acceptance of their own emotions, as well as their ability to tolerate and manage them. Still, it is important to note that the extent to which an intervention decreases anxiety sensitivity is associated with superior alcohol use outcome, and that usual SUD treatment plus CBT for anxiety disorders (i.e., UC + CALM ARC) showed steeper decline slopes compared to SUD treatment alone (i.e., UC). Therefore, treatments for comorbid anxiety disorders and SUD that maximize reductions in anxiety sensitivity are warranted. At present, there is a large body of evidence suggesting that exposure-based CBT for anxiety disorders leads to large changes in anxiety sensitivity (see Olatunji & Wolitzky-Taylor, 2009, for a review). Medication-assisted SUD treatments that reduce anxiety-related withdrawal symptoms (e.g., Mason, Quello, Goodell, Shadan, & Kyle, 2015) may also be a promising intervention, or adjunctive component, of treatment for comorbid anxiety disorders and SUD.
The specificity of decreases in anxiety sensitivity associated with decreases in alcohol but not drug use is worth noting. The heterogeneity of drugs of dependence in this sample increases the complexity of these associations. Possibly, decreasing anxiety sensitivity via treatment may lead to decreases particularly of those substances that may be more functionally related to reduction of negative affect (e.g., alcohol, sedatives), as opposed to having anxiogenic effects (e.g., stimulants). Future research with larger samples is needed to evaluate this by examining specific drug types separately.
In contrast to hypotheses, coping motives for substance use did not significantly mediate substance use outcomes. SUD treatment directly targets coping motives for substance use, but CBT for anxiety disorders, while not directly targeting coping motives, presumably decreases anxiety and provides more adaptive ways of managing it. We interpret null findings cautiously, particularly given the relatively small sample size that may have limited our ability to detect small effects as statistically significant. Still, although this is the first study to specifically examine the mediational role of coping motives in substance use outcomes among real-world treatment seekers with comorbid SUD and anxiety disorders, these findings are somewhat inconsistent with prior work finding that coping motives are related to high levels of substance use (see Cooper et al., 2016 for a review), that increases in coping skills are associated with greater improvement in substance use symptoms (Kiluk et al., 2010; Litt et al., 2008; Magill et al., 2015), and that in one study, change in coping motives over a long-term follow-up was associated with marijuana use following treatment (Banes et al., 2014). However, in this study (Banes et al., 2014), pre-to post-treatment change in coping motives was not associated with post-treatment marijuana use. This finding only emerged at the 9-month follow-up, suggesting that more work is needed to understand what change is occurring following treatment, and why. Surprisingly, in the current study, even baseline substance use coping motives were not significantly associated with substance use outcomes. Future work is needed to examine whether these findings replicate.
Because decreases in coping motives for substance use during treatment were minimal and non-significant across participants in both conditions, it reasons that mediation was not observed. Possibly, the use of a heterogeneous sample of substance users, with over half meeting the diagnostic criteria for two or more SUDs (see Wolitzky-Taylor et al., 2018) resulted in a similarly heterogeneous sample with regard to motives for use. Although the majority of anxiety and SUD comorbidity can be explained by tension-reduction and self-medication hypotheses (Kushner, Krueger, Frye, & Peterson, 2008), substance use may have preceded anxiety in some individuals who then experienced anxiogenic effects from intoxication or withdrawal (e.g., stimulant intoxication, alcohol withdrawal; see Kushner et al., 2008, for a review). Relatedly, polysubstance users may use some substances to cope with anxiety and others for enhancement or conformity motives, thus making it difficult to respond to a measure that asked respondents to consider all substance use together. Thus, coping motives may be more relevant and easily targeted in a homogenous group of SUD patients who initially endorse that they use substances to cope with anxiety, or among those whose primary substances of dependence have stress-dampening effects (e.g., central nervous system depressants). Large samples will be needed to examine moderated mediation (e.g., whether coping motives mediate outcomes more among those who primarily use central nervous system depressants compared to those who use stimulants).
Notably, most work demonstrating a link between anxiety, coping motives, and substance use has examined homogenous samples of patients with alcohol problems or community samples of primarily young adults with varying levels of alcohol and other substance use (see DeMartini & Carey, 2011 for a review) or community samples of marijuana users (e.g., Johnson, Mullin, Marshall, Bonn-Miller, & Zvolensky, 2010). Similarly, most psychometric studies of the Drinking Motives Questionnaire have used undergraduate student samples (e.g., Stewart et al., 1996; Read, Wood, Kahler, Maddock, & Palfai, 2003), suggesting that work may be needed to evaluate the extent to which this remains a psychometrically sound measure for assessing substance use motives among complex and severe treatment-seeking samples. We did not consider other motives questionnaires for specific substances of dependence due to the heterogeneous, polysubstance using sample in this study, and because the Drinking Motives Questionnaire has long been established in the literature. Still, other motives measures may have yielded different findings and are worth exploring in future research. It is also worth noting that this study is the first to our knowledge to gather repeated measurements of coping motives throughout treatment for SUD. Possibly, coping motives remain stable despite treatment. Even if new coping skills are developed and negative affect and substance use decrease, individuals may still consider that if they were to use a substance, it would be for the same reasons as when they used more often. More work is needed to better understand the extent to which coping motives are malleable.
The use of repeated measurements throughout treatment, use of a real-world sample of patients with comorbid anxiety disorders and SUD, and examination of mediation between two distinct, evidence-based treatment approaches (i.e., CBT-based treatment for SUD v. CBT-based treatment for SUD + a full integrated, brief CBT program for anxiety disorders) are strengths of the current study. Still, there are some limitations. Most notably, the sample size was relatively small and may have precluded us from detecting small effects as statistically significant. Thus, future replication research is needed with larger samples. In addition, larger samples sizes will allow for a more fine-grained analysis of whether mediational effects are observed differently with certain principal anxiety disorder/primary substance of dependence combinations. Second, although the measurement of the mediators temporally preceded that of the substance use variables, the period of time assessed in the Timeline Followback likely had some overlap with the last few weeks of active participation in the treatment phase of the study (either CALM ARC sessions or weekly assessments in UC). Therefore, scores on the mediator measures during the later assessment periods may have been present concurrently with the drinking and drug use recorded for that time period. Third, psychometric properties of the Drinking Motives Questionnaire have only been established for its use in assessing motives for drinking alcohol. Due to the heterogeneous nature of our sample (which is a strength from an effectiveness framework), we modified the questionnaire instructions such that participants were asked to consider their motives across any substances they may have used. Although there is no theoretical reason to suspect that the construct of coping motives would differ as a function of the type of substance being considered, it is possible that there may be psychometric flaws with broadening the instructions in this way. Possibly, polysubstance using participants had difficulties completing the questionnaire accurately when an item might have been endorsed for one substance but not another. Future research should investigate the psychometric properties of a broader motives questionnaire. Fourth, replication studies are needed to see whether anxiety sensitivity consistently mediates alcohol outcome. Specifically, despite randomization, anxiety sensitivity was significantly higher in CALM ARC than UC, and thus regression to the mean remains a possible explanation for these findings. Finally, this study lacked measures assessing functioning or the consequences of substance use. Future research would benefit from additional work utilizing such measures.
Taken together, this novel examination of changes in anxiety sensitivity and coping motives for substance use during treatment revealed that anxiety sensitivity, but not coping motives, significantly mediated alcohol use outcome (but not drug). Moreover, adding brief CBT for anxiety disorders to usual, CBT-based SUD treatment resulted in steeper anxiety sensitivity decline slopes compared to usual SUD treatment. Therefore, treatment augmentation strategies that enhance the reduction of anxiety sensitivity (e.g., via exposure) should result in greater decreases in alcohol use. Anxiety sensitivity should be assessed as a regular part of care in SUD treatment settings, and interventions including interoceptive exposure should be delivered.
Acknowledgements
This study was supported by grant funds from a National Institute on Drug Abuse (NIDA; 5K23DA031677) Early Career Development Award (PI: Wolitzky-Taylor). The study was approved by the UCLA Institutional Review Board and was registered at clinicaltrials.gov, NCT01764698.
References
- Arch JJ, Wolitzky-Taylor KB, Eifert GH, & Craske MG. (2012). Longitudinal treatment mediation of traditional cognitive behavioral therapy and acceptance and commitment therapy for anxiety disorders. Behaviour Research and Therapy, 50, 469–478. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC. (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111, 33–51. [DOI] [PubMed] [Google Scholar]
- Banes KE, Stephens RS, Blevins CE, Walker DD, & Roffman RA. (2014). Changing motives for use: Outcomes from a cognitive-behavioral intervention for marijuana-dependent adults. Drug and Alcohol Dependence, 139, 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Bonn-Miller MO, Zvolensky MJ, & Schmidt NB. (2007). Marijuana use motives and social anxiety among marijuana-using young adults. Addictive Behaviors, 32(10), 2238–2252. 10.1016/j.addbeh.2007.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, & Carroll KM. (2010). Effect of anxiety on treatment presentation and outcome: Results from the Marijuana Treatment Project. Psychiatry Research, 178(3), 493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Smits JA, Norton PJ, Crosby RD, Wonderlich SA, et al. (2011). Anxiety sensitivity and marijuana use: An analysis from ecological momentary assessment. Depression and Anxiety, 28(5), 420–426. 10.1002/da.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, Norman SB, Craske MG, Sullivan G, Lang AJ, Chavira DA, & Stein MB. (2009). Validation of a brief measure of anxiety-related severity and impairment: The Overall Anxiety Severity and Impairment Scale (OASIS). Journal of Affective Disorders, 112(1), 92–101. 10.1016/j.jad.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comeau N, Stewart SH, & Loba P. (2001). The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addictive Behaviors, 26(6), 803–825. 10.1016/S0306-4603(01)00238-6. [DOI] [PubMed] [Google Scholar]
- Conger JJ. (1956). Alcoholism: Theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. The Quarterly Journal of Social Affairs, 17, 296–305. [PubMed] [Google Scholar]
- Conrod PJ, Castellanos-Ryan N, & Mackie C. (2011). Long-term effects of a personality-targeted intervention to reduce alcohol use in adolescents. Journal of Consulting and Clinical Psychology, 79(3), 296–306. 10.1037/a0022997. [DOI] [PubMed] [Google Scholar]
- Conrod PJ, O’Leary-Barrett M, Newton N, Topper L, Castellanos-Ryan N, Mackie C, et al. (2013). Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: A cluster randomized controlled trial. JAMA Psychiatry, 70(3), 334–342. 10.1001/jamapsychiatry.2013.651. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Kuntsche E, Levitt A, Barber LL, & Wolf S. (2016). Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco. In Sher KJ (Vol. Ed.), The oxford handbook of substance use and substance use disorders: Vol. 1, (pp. 375–421). New York, NY: University of Oxford Press. [Google Scholar]
- Cooper ML, Russell M, Skinner JB, & Windle M. (1992). Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment, 4(2), 123–132. 10.1037/1040-3590.4.2.123. [DOI] [Google Scholar]
- Cox WM, & Klinger E. (1988). A motivational model of alcohol use. Journal of Abnormal Psychology, 97(2), 168–180. 10.1037/0021-843X.97.2.168. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, & Carey KB. (2011). The role of anxiety sensitivity and drinking motives in predicting alcohol use: A critical review. Clinical Psychology Review, 31(1), 169–177. 10.1016/j.cpr.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Gilson KM, Bryant C, Bei B, Komiti A, Jackson H, & Judd F. (2013). Validation of the Drinking Motives Questionnaire (DMQ) in older adults. Addictive Behaviors, 38(5), 2196–2202. [DOI] [PubMed] [Google Scholar]
- Hayes AF, & Scharkow M. (2013). The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: Does method really matter? Psychological Science, 24(10), 1918–1927. [DOI] [PubMed] [Google Scholar]
- Hearon BA, Calkins AW, Halperin DM, McHugh RK, Murray HW, & Otto MW. (2011). Anxiety sensitivity and illicit sedative use among opiate-dependent women and men. The American Journal of Drug and Alcohol Abuse, 37(1), 43–47. 10.3109/00952990.2010.535581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K, Mullin JL, Marshall EC, Bonn-Miller MO, & Zvolensky M. (2010). Exploring the mediational role of coping motives for marijuana use in terms of the relation between anxiety sensitivity and marijuana dependence. American Journal on Addictions, 19(3), 277–282. 10.1111/j.1521-0391.2010.00041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ. (1985). The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry, 142(11), 1259–1264. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Nich C, Babuscio T, & Carroll KM. (2010). Quality versus quantity: Acquisition of coping skills following computerized cognitive–behavioral therapy for substance use disorders. Addiction, 105(12), 2120–2127. 10.1111/j.1360-0443.2010.03076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Wilson T, Fairburn CG, & Agras WS. (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59, 877–883. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R. (2006). Who drinks and why? A review of socio-demographic, personality, and contextual issues behind the drinking motives in young people. Addictive Behaviors, 31(10), 1844–1857. 10.1016/j.addbeh.2005.12.028. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Donahue C, Sletten S, Thuras P, Abrams K, Peterson J, et al. (2006). Cognitive behavioral treatment of comorbid anxiety disorder in alcoholism treatment patients: Presentation of a prototype program and future directions. Journal of Mental Health, 15(6), 697–707. 10.1080/09638230600998946. [DOI] [Google Scholar]
- Kushner MG, Krueger R, Frye B, & Peterson J. (2008). Epidemiological perspectives on co-occurring anxiety disorder and substance use disorder. In Stewart SH, & Conrod PJ (Eds.). Anxiety and substance use disorders: The vicious cycle of comorbidity (pp. 3–17). New York, NY: Springer Science+Business Media. [Google Scholar]
- Lejuez CW, Zvolensky MJ, Daughters SB, Bornovalova MA, Paulson A, Tull MT, & Otto MW. (2008). Anxiety sensitivity: A unique predictor of dropout among inner-city heroin and crack/cocaine users in residential substance use treatment. Behaviour Research and Therapy, 46(7), 811–818. 10.1016/j.brat.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, & Petry NM. (2008). Coping skills training and contingency management treatments for marijuana dependence: Exploring mechanisms of behavior change. Addiction, 103(4), 638–648. 10.1111/j.1360-0443.2008.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, Kiluk BD, McCrady BS, Tonigan JS, & Longabaugh R. (2015). Active ingredients of treatment and client mechanisms of change in behavioral treatments for alcohol use disorders: Progress 10 years later. Alcoholism: Clinical and Experimental Research, 39(10), 1852–1862. 10.1111/acer.12848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maller RG, & Reiss S. (1992). Anxiety sensitivity in 1984 and panic attacks in 1987. Journal of Anxiety Disorders, 6(3), 241–247. 10.1016/0887-6185(92)90036-7. [DOI] [Google Scholar]
- Mason BJ, Quello S, Goodell V, Shadan F, & Kyle M. (2015). Gabapentin treatment for alcohol dependence: A randomized controlled trial. JAMA Internal Medicine, 174, 70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Hearon BA, & Otto MW. (2010). Cognitive behavioral therapy for substance use disorders. Psychiatric Clinics of North America, 33(3), 511–525. 10.1016/j.psc.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Rosenfield D, Seidel A, Bhaskara L, & Hofmann SG. (2010). Respiratory and cognitive mediators of treatment change in panic disorder: Evidence for intervention specificity. Journal of Consulting and Clinical Psychology, 78(5), 691–704. 10.1037/a0019552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits LM. (2002). Seeking safety: Therapy for post-traumatic stress disorder and substance use disorder. In Follette VM, & Ruzek JI (Eds.). Cognitive-behavioral therapies for trauma(2nd ed.). New York, NY: Guilford. [Google Scholar]
- National Institute on Drug Abuse (2003). State of the science of group therapy research for drug abuse and dependence: Workshop summary. [Google Scholar]
- Olatunji BO, & Wolitzky-Taylor KB. (2009). Anxiety sensitivity and the anxiety disorders: A meta-analytic review and synthesis. Psychological Bulletin, 135(6), 974–999. 10.1037/a0017428. [DOI] [PubMed] [Google Scholar]
- Randall CL, Thomas S, & Thevos AK. (2001). Concurrent alcoholism and social anxiety disorder: A first step toward developing effective treatments. Alcoholism: Clinical and Experimental Research, 25(2), 210–220. 10.1111/j.1530-0277.2001.tb02201.x. [DOI] [PubMed] [Google Scholar]
- Read JP, Wood MD, Kahler CW, Maddock JE, & Palfai TP. (2003). Examining the role of drinking motives in college student alcohol use and problems. Psychology of Addictive Behaviors, 17(1), 13. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, & McNally RJ. (1986). Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy, 24(1), 1–8. 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Buckner JD, & Keough ME. (2007a). Anxiety sensitivity as a prospective predictor of alcohol use disorders. Behavior Modification, 31(2), 202–219. 10.1177/0145445506297019. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, & Richey JA. (2007b). Anxiety Sensitivity Amelioration Training (ASAT): A longitudinal primary prevention program targeting cognitive vulnerability. Journal of Anxiety Disorders, 21(3), 302–319. 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Raines AM, Allan NP, & Zvolensky MJ. (2016). Anxiety sensitivity risk reduction in smokers: A randomized control trial examining effects on panic. Behaviour Research and Therapy, 77, 138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D. (2016). The MINI international neuropsychiatric interview. (Version 7.0.2) for DSM-5. [Google Scholar]
- Smits JA, Powers MB, Cho Y, & Telch MJ. (2004). Mechanism of change in cognitive-behavioral treatment of panic disorder: Evidence for the fear of fear mediational hypothesis. Journal of Consulting and Clinical Psychology, 72(4), 646–652. 10.1037/0022-006X.72.4.646. [DOI] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB. (1995). Alcohol timeline Followback users’ manual. Toronto, Canada: Addiction Research Foundation. [Google Scholar]
- Stewart SH, & Conrod PJ. (2008). Anxiety disorder and substance use disorder comorbidity: Common themes and future directions. In Stewart SH, & Conrod PJ (Eds.). Anxiety and substance use disorders: The vicious cycle of comorbidity (pp. 239–257). New York, NY: Springer Science+Business Media. [Google Scholar]
- Stewart SH, Zeitlin SB, & Samoluk SB. (1996). Examination of a three-dimensional drinking motives questionnaire in a young adult university student sample. Behaviour Research and Therapy, 34(1), 61–71. [DOI] [PubMed] [Google Scholar]
- Tate JC, Pomerleau CS, & Pomerleau OF. (1994). Pharmacological and non-pharmacological smoking motives: A replication and extension. Addiction, 89(3), 321–330. 10.1111/j.1360-0443.1994.tb00899.x. [DOI] [PubMed] [Google Scholar]
- Watt M, Stewart S, Birch C, & Bernier D. (2006). Brief CBT for high anxiety sensitivity decreases drinking problems, relief alcohol outcome expectancies, and conformity drinking motives: Evidence from a randomized controlled trial. Journal of Mental Health, 15(6), 683–695. 10.1080/09638230600998938. [DOI] [Google Scholar]
- Wolitzky-Taylor K, Guillot CR, Pang RD, Kirkpatrick MG, Zvolensky MJ, Buckner JD, et al. (2015). Examination of anxiety sensitivity and distress tolerance as transdiagnostic mechanisms linking multiple anxiety pathologies to alcohol use problems in adolescents. Alcoholism: Clinical and Experimental Research, 39(3), 532–539. 10.1111/acer.12638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor K, Krull JL, Rawson R, Roy-Byrne P, Ries R, & Craske MG. (2018). Randomized clinical trial evaluating the preliminary effectiveness of an integrated anxiety disorder treatment in substance use disorder specialty clinics. Journal of Consulting and Clinical Psychology, 86, 81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]