Abstract
Objectives
Robotic knee arthroplasty procedures have emerged as a new trend, garnering attention from orthopedic surgeons globally. It has been hypothesized that the use of robotics enhances the accuracy of prosthesis positioning and alignment restoration. The objective of this study was to provide a high-level, evidence-based comparison between robotic total knee replacements and conventional methods, focusing on radiological and functional outcomes.
Methods
We searched five databases from their inception until June 1, 2022, specifically targeting randomized controlled trials (RCTs) that compared the outcomes of robotic and conventional total knee replacements. We were interested in outcomes such as knee range of motion, clinical and function knee society scores, the Western Ontario and McMaster University score (WOMAC), the Hospital of Special Surgery score, complications, and radiological alignment. This review was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes guidelines. We assessed the risk of bias using the revised Cochrane risk-of-bias tool for randomized trials (RoB 2).
Results
Our search returned seven RCTs suitable for our analysis, which included a total of 1942 knees; 974 of these knees were implanted using robotic arms while the remaining 968 utilized jig-based knee systems. Our findings indicated that robotic knees had significantly better post-operative anatomical (OR − 0.82; 95% CI, − 1.027 to − 0.58, p value < 0.00001) and mechanical restoration (OR − 0.95; 95% CI, − 1.49 to − 0.41, p value < 0.0006). While knee range of motion (OR − 2.23; 95% CI − 4.89–0.43, p value 0.1) and femoral prosthesis position (OR − 0.98; 95% CI, − 2.03–0.08, p value 0.07) also favored robotic knees, these differences did not reach statistical significance. Both clinical and functional outcomes, as well as the rate of complications, were found to be statistically similar between the groups undergoing robotic and traditional knee replacement surgeries.
Conclusion
This meta-analysis indicates that robotic total knee replacements offer superior post-operative anatomical and mechanical alignment compared to conventional total knee replacements. Despite this, clinical and functional outcomes, as well as complication rates, were similar between the two. These findings should be considered in light of potential confounding factors. More randomized controlled trials with the latest robotic systems are needed to confirm any superior functional and clinical outcomes from robotic-assisted surgeries.
Level of evidence
I.
Keywords: Total knee arthroplasty, Robotic arthroplasty, Jig-based arthroplasty, Conventional knee arthroplasty
Introduction
Over the last few decades, total knee replacement has experienced significant growth as an orthopedic procedure. From 2017 to 2019 alone, the UK recorded 312,167 primary knee replacements, constituting 24% of the national joint registry [1]. This surge can largely be linked to the increasing prevalence and economic impact of osteoarthritis among different populations [2].
Despite the proven effectiveness and replicability of traditional knee arthroplasty methods, paired with advancements in prosthesis technology, a considerable number of patients are still unhappy with their knee replacements for various known and undetermined reasons [3, 4]. Factors such as soft tissue balance and implant placement have been identified to influence patient satisfaction with the procedure [5, 6]. Though precise component alignment is often achievable and replicable in today's conventional total knee arthroplasty (CTKA), it can be challenging and intricate to obtain, particularly in more complex cases [7].
The development of robotic total knee arthroplasty (RTKA) was aimed at eliminating potential inaccuracies in implant positioning and alignment, thus reducing patient dissatisfaction. The first-ever RTKA was performed in the UK as early as 1988, utilizing the Acrobat system [8]. Given that most robotic systems employed in knee arthroplasty use 3-dimensional imaging, it is suggested that these robotic procedures offer higher precision in positioning and balancing. Some reports even suggest that they outperform traditional jig-based methods in clinical settings [9, 10]. However, this claim has not yet been conclusively validated [11].
Over the past decades, various robotic arms have been developed and incorporated into medical practice. These include systems such as ROBODOC by Curexo Technology in Fremont, CA [12], Mako by Stryker in Mahwah, NJ [13], CASPAR by URS Ortho GMBH and Co in Rastatt, Germany [14], and NAVIO by Smith and Nephew in Memphis, TN [15].
The objective of this meta-analysis was to provide the most robust evidence currently available that compares these two techniques. To the best of our knowledge, this is the only meta-analysis that draws upon randomized controlled trials to compare robotic total knee arthroplasty with its conventional equivalent in the existing literature.
Our hypothesis was that there would be no significant difference between the two groups concerning functional results, knee range of motion and rates of complications.
Materials and methods
This meta-analysis was conducted in line with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA), utilizing both a PRISMA checklist and algorithm [16].
Search strategy
PubMed/Medline, CINAHL, Cochrane, Embase, and Google Scholar databases were systematically searched from inception until June 1, 2022, to identify articles in peer-reviewed journals. The search was performed using the following keywords and their derivatives: “Knee arthroplasty,” “Knee replacement,” “Joint replacement,” “Total knee,” “Robotic-assisted,” “Conventional,” “Robotic-arm,” “Randomized,” and “RCT.” Two authors independently sifted through search results, assessing them against the eligibility criteria based on their titles and/or abstracts. Any disagreements were addressed in a resolution meeting with a third senior author. A comprehensive review of the full-text articles that met the eligibility criteria was conducted, and references from these articles were manually checked to guarantee the inclusion of all pertinent studies.
Eligibility criteria
Inclusion criteria
All original comparative level I of evidence randomized controlled trials (RCTs) reporting primary TKA indicated in robotic total knee arthroplasty with its conventional equivalent.
The primary indication for TKA is primary osteoarthritis.
English full-text manuscript with available data.
RCTs that published clear outcome measures with attached data presented as or can be transferred to mean and standard deviation values.
Exclusion criteria
Studies involving patients with inflammatory arthritis or post-traumatic arthritis.
Non-comparative or not reporting outcomes.
Review articles, cross-sectional, case series and reports.
Preclinical or animal studies.
Data collection process and data items
A pre-designed data collection sheet in Microsoft Excel was utilized by two independent reviewers to extract data. The collected data items comprised: surname of the first author, year of study, age, gender, patient count, prosthesis type, robotic system used, points of follow-up, revision rates for any cause, complications encountered.
Outcomes of interest
The study evaluated several outcomes of interest, including scores for knee society pain and function, the Western Ontario and McMaster University score (WOMAC), the Hospital of Special Surgery score (HSS), knee range of motion, and alignment parameters. Additionally, we were successful in obtaining data related to sagittal and coronal knee alignments, which included the anterior–posterior (AP) tibial angle (varus–valgus), tibial slope angle, femoral flexion angle, and tibiofemoral angle.
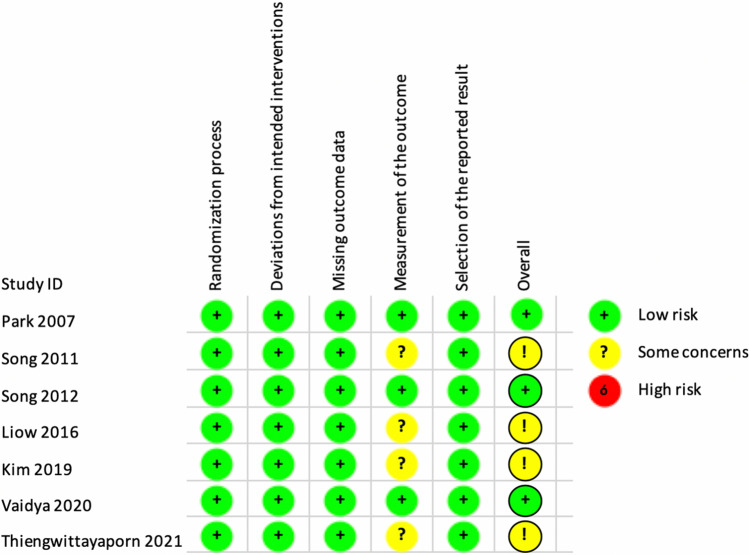
Qualitative assessment (risk of bias)
The qualitative analysis was conducted using the revised Cochrane risk-of-bias tool for randomized trials (RoB 2) [17]. This tool evaluates five key areas: randomization, adherence to intended treatments, missing outcomes, measurement bias, and reporting bias. Two authors independently assessed each study using the RoB 2, and the final evaluation of each study was reviewed in conjunction with the senior author to arrive at a mutual agreement.
Quantitative analysis
RevMan V.5.0.18.33 (The Cochrane Collaboration, Copenhagen, Denmark) was used to perform the meta-analysis. Mean and standard variations were extracted to present continuous variables. Dichotomous variables were analyzed by Relative risk (RR) with 95% CI. Heterogeneity was measured using I2, and results were considered statistically significant at p < 0.05.
Results
Study selection
The initial search resulted in 651 articles; among these, 318 were duplicates and were removed both manually and electronically. The remaining articles were screened based on title and abstract, resulting in the exclusion of 79. The full text of the 333 remaining articles was evaluated against the inclusion criteria. Ultimately, seven studies fulfilled the eligibility criteria and were incorporated into both the qualitative and quantitative synthesis [18–24]. In instances where studies provided details on approximately the same cohort at two different time points, only results from the later study were included [19, 25]. The PRISMA flowchart detailing this process is displayed in Fig. 1.
Fig. 1.
Search strategy flowchart
Characteristics of the included studies
In our final qualitative and quantitative analysis, seven randomized controlled trials met our inclusion criteria and were thus eligible for our analysis. The study included 1942 knees; of these, 974 were implanted using robotic arms and the remaining 968 were conventionally implanted. Although different prosthesis designs and brands were used in total, each included study compared outcomes using the same knee brand and design. The studies included in this analysis did not contain data on cementless TKAs. All TKAs in the included RCTs were cemented. In terms of robotic systems, five papers [18–22] utilized the ROBODOC system (Integrated Surgical Systems, Sacramento, CA) for the robotically assisted knee group, while the other two studies [23, 24] used the NAVIO® system (Smith and Nephew, Andover, TX, USA).
All the trials included in our study matched their study groups in terms of participant age and gender. However, there was a variation in the follow-up periods, so we reported our results at the final follow-up. Two studies [23, 24] provided post-operative radiological outcomes without specifying a follow-up interval, which is understandable given that their outcome measures were solely radiological assessments. We also examined common outcomes between the studies. Despite the variation in follow-up periods, we analyzed the data based on the final patient visits (Table 1).
Table 1.
Characteristics of the included studies
| Study | LoE | Number of knees | RTKA | CTKA | Follow up (month) | Type of prosthesis | Robot system |
|---|---|---|---|---|---|---|---|
| Park [20] | I | 62 | 32 | 30 | 47.17 | Zimmer LPS | ROBODOC |
| Song [21] | I | 60 | 30 | 30 | 12 | NexGen CR prosthesis (Zimmer, Warsaw, Indiana) | ROBODOC |
| Song [22] | I | 100 | 50 | 50 | 36 | NexGen CR prosthesis (Zimmer, Warsaw, Indiana) | ROBODOC |
| Liow [19] | I | 60 | 31 | 29 | 24 | NexGen LPS-Flex; Zimmer, Inc, Warsaw, IN, USA | ROBODOC |
| Kim [18] | I | 1448 | 724 | 724 | 120 | Duracon® posterior cruciate-substituting total knee prosthesis (Stryker Orthopedics, Mahawh, NJ, USA) | ROBODOC |
| Vaidya [24] | I | 60 | 32 | 28 | 0 | posterior-stabilized prosthesis (Anthem, Smith and Nephew Inc.) | Navio |
| Thiengwittayaporn [23] | I | 152 | 75 | 77 | 0 | (Legion® PS Total Knee System, Smith and Nephew, Memphis, TN, USA) | Navio |
LoE level of evidence, RTKA robotic total knee arthroplasty, CTKA conventional total knee arthroplasty
Quality assessment
Three studies demonstrated a low risk of bias, while five studies exhibited some concern for bias. Notably, none of the included studies showed a high risk of bias. All studies maintained their groups according to the original randomization, and no study experienced a high dropout rate or failed to report outcomes. A graphic representation of the qualitative assessment can be found in Table 2.
Table 2.
Risk of bias in individual studies
Clinical knee society score (KSS clinical)
The clinical knee society score was documented in two studies [19, 20]. These studies reported their outcomes at varying follow-up periods, ranging from 24 to 47 months. We reported our meta-analysis outcome at the final follow-up. None of the included studies, nor our fixed model analysis, reported a statistically significant difference. Figure 2 presents the forest plot of the clinical knee society score, revealing no statistical difference between the two groups (OR 0.11; 95% CI − 1.82–2.04, p value 0.91) and high heterogeneity across the results (I2 = 74%).
Fig. 2.
Forest plot of clinical knee society score at the final follow up between RTKA and CTKA, CI confidence interval
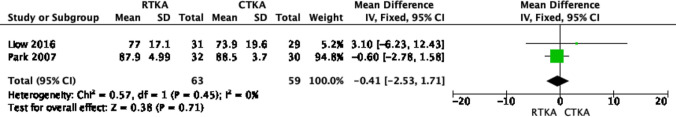
Functional knee society score (KSS functional)
The functional knee society score was outlined in two studies [19, 20]. Due to variations in follow-up periods among the included studies, we reported the outcome at the final follow-up. Figure 3 shows the forest plot of the clinical knee society score, which demonstrates no statistical difference between the two groups (OR − 0.41; 95% CI − 2.53, 1.71, p value 0.71). The results also displayed low heterogeneity (I2 = 0%).
Fig. 3.
Forest plot of functional knee society score at the final follow up between RTKA and CTKA, CI confidence interval
Hospital of special surgery score (HSS)
Two studies [21, 22] reported the HSS score at 12 and 36 months, respectively. Our fixed model analysis, conducted at the final follow-up, did not reveal any differences between the two groups. This is represented in Fig. 4 (OR − 0.22; 95% CI − 1.72, 1.28, p value 0.14).
Fig. 4.
Forest plot of hospital of special surgery score at the final follow up between RTKA and CTKA, CI confidence interval
The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) functional score
The WOMAC score was examined in two papers [21, 22], with neither reporting any differences between RTKA and CTKA at 12 and 36 months, respectively. Our fixed model analysis, conducted at the final follow-up, also showed no significant differences. These findings are illustrated in Fig. 5 (OR − 1.47; 95% CI − 3.32–0.37; p value 0.12), with the results demonstrating low heterogeneity (I2 = 0%).
Fig. 5.
Forest plot of WOMAC score at the final follow up between RTKA and CTKA, CI confidence interval
Knee range of motion
Four studies [19–22] reported on the post-operative range of motion, with their analysis being conducted at the final follow-up, which ranged from 12 to 47 months. The fixed effect meta-analysis indicated a superiority of RTKA knees in terms of range of motion; however, this was not statistically significant, as shown in Fig. 6 (OR − 2.23; 95% CI − 4.89–0.43, p value 0.1). The results showed low heterogeneity (I2 = 1%).
Fig. 6.
Forest plot of range of motion score at the final follow up between RTKA and CTKA, CI confidence interval
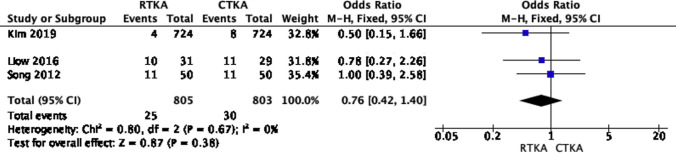
Complications
Three studies [18, 19, 22] reported on complication events, with respective follow-up periods ranging from 36 to 120 months. Neither the included studies nor our fixed model analysis at the final follow-up reported any significant differences between RTKA and CTKA. This is displayed in Fig. 7 (OR 0.76; 95% CI, 0.42–1.4, p value 0.38). The results showed low heterogeneity (I2 = 0%). The pooled complications primarily consisted of infection, aseptic loosening, and knee stiffness.
Fig. 7.
Forest plot of complications at the final follow up between RTKA and CTKA, CI confidence interval
Post-operative alignment
Post-operative alignment parameters were extensively studied in the included papers. The tibiofemoral [18, 20, 23] and mechanical axes [21, 22, 24] were reported in three studies each. As demonstrated in Fig. 8 (OR − 0.82; 95% CI, − 1.027 to − 0.58, p value < 0.00001) and Fig. 9 (OR − 0.95; 95% CI, − 1.49 to − 0.41, p value < 0.0006), the robotic knee was statistically superior in restoring the tibiofemoral and mechanical axes, respectively. However, the results for the tibiofemoral axis demonstrated high heterogeneity.
Fig. 8.
Forest plot of tibiofemoral axis at final follow up between RTKA and CTKA, CI confidence interval
Fig. 9.
Forest plot of mechanical axis at final follow up between RTKA and CTKA, CI confidence interval
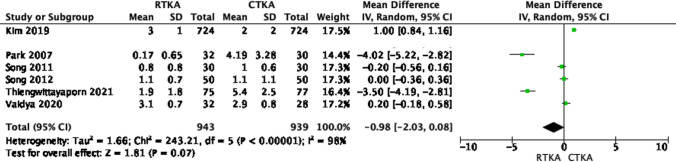
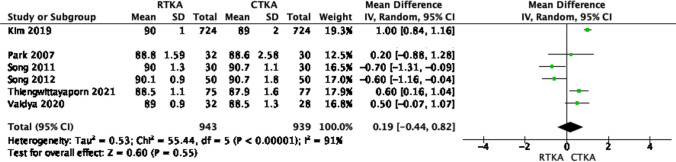
On the other hand, other parameters such as the femoral flexion angle, and the anteroposterior and lateral tibial angles were reported in six studies [18, 20–24]. Our fixed model analysis did not reveal any significant differences between the anteroposterior and lateral tibial angles in both knee arthroplasty techniques (p value > 0.05), as shown in Figs. 10 and 11. The restoration of the femoral flexion angle favored robotic knees, but this was not statistically significant, as shown in Fig. 12 (OR − 0.98; 95% CI, − 2.03–0.08, p value 0.07), with high heterogeneity across the results (I2 = 98%).
Fig. 10.
Forest plot of femoral flexion angle at final follow up between RTKA and CTKA, CI confidence interval
Fig. 11.
Forest plot of anteroposterior tibial angle at final follow up between RTKA and CTKA, CI confidence interval
Fig. 12.
Forest plot of lateral tibial angle at final follow up between RTKA and CTKA, CI confidence interval
Discussion
The increase in knee replacement surgeries, mainly due to osteoarthritis, has advanced both conventional and robotic techniques. Despite technological advancements, achieving optimal patient satisfaction remains a challenge, with precise implant placement and soft tissue balance being key factors. RTKA emerged to address these issues, promising enhanced accuracy. This meta-analysis was crucial as it sought to compare the RTKA with CTKA methods.
The most significant result from this meta-analysis was the markedly improved restoration of mechanical alignment in robotic-assisted knee arthroplasty compared to jig-based methods. This finding, which was a unique outcome of our level I study, could likely be credited to the accuracy of knee balancing in robotic surgeries [26, 27]. Furthermore, our study findings concur with prior acknowledgments concerning the superior performance of robotic-assisted knee arthroplasty in terms of implant placement and reduction of radiological outliers.
The precision of robotic knees concerning balancing and implant placement has been shown to positively influence knee outcomes in a few cohorts [7, 28–30]. However, this meta-analysis was unable to demonstrate any superiority in patient-reported outcome scores. Furthermore, the introduction of kinematic alignment, which can be replicated in robotic knees, has increased the popularity of robotic arthroplasty among surgeons [31]. This contrasts with traditional knees that are balanced through measured resection, gap balancing, or a combination of techniques. While kinematic alignment seems to be a promising direction for knee balancing, no long-term studies currently confirm its superiority over other balancing techniques. On the other hand, while RTKA promises theoretical precision, the substantial learning curve and extended operative times present notable concerns. The requirement for preoperative CT imaging with certain systems further adds to the duration, cost, and radiation exposure, complicating its widespread adoption [32–34].
While robotics may yield improved clinical and radiological outcomes, it is necessary to weigh these potential benefits against the increased cost of robotic surgery. The crucial question is whether the possible clinical advantage justifies the incremental cost per knee. Certain robotic systems employ CT scans, which can further escalate costs [28, 35]. Several studies have estimated an increased cost per knee of $1000–1350, and this does not take into account any additional radiological studies that may be required [36, 37].
Several meta-Analyzes in the existing literature compare Robotic Total Knee Arthroplasty (RTKA) to Conventional Total Knee Arthroplasty (CTKA), with none qualifying as a Level I study. For example, Ren et al. [38], in their meta-analysis, which considered 517 knees across 6 RCTs and one cohort study, reported superior restoration of mechanical alignment in RTKA procedures. On the other hand, Onggo et al. [39] reviewed the outcomes of 6500 knees from 18 studies (only 4 RCTs) and intriguingly reported better mechanical alignment restoration, reduced blood loss, and superior clinical outcomes in RTKA surgeries. Additionally, Zhang et al. [40] included 16 studies (no RCT) in their relatively recent meta-analysis, with results favoring RTKA in terms of implant position and early patient-reported outcomes, though the latter was not statistically significant. Our study, in contrast, provides the highest level of evidence on this topic, as it includes the only seven available RCTs in the literature that compare both techniques. The statistical significance reported for post-operative alignment with robotic knee arthroplasty suggests that this method can more accurately achieve the desired alignment compared to conventional methods particularly in mechanical axis and tibiofemoral axis results. However, the presence of heterogeneity in the results for the tibiofemoral axis warrants cautious interpretation. Moreover, the clinical importance of these findings and their impact on patient outcomes and satisfaction remains uncertain. A recent review [41], despite including studies of lower evidence levels, suggests that both neutral (0°–3°) and mild varus (3°–6°) alignments post-TKA result in similar patient outcomes in patients with preoperative varus knees. This highlights the necessity for a more comprehensive exploration of the role alignment plays in the success of TKA.
While this report presented data from studies with high levels of evidence, we acknowledge a few limitations. First, there was variability in the follow-up periods among the included RCTs, and some of the outcomes were analyzed at the final follow-up, which ranged from 2 to 5 years. Second, we were only able to include two robotic systems in our study, one of which, ROBODOC (Curexo Technology, Fremont, CA) [12], is a first-generation robotic system. It is not as widely used currently in comparison to the newer and more advanced robotics. There were no RCTs comparing the use of other robotic systems, such as Mako, which might be more commonly used in certain regions. Lastly, the number of patients involved in the included studies is relatively small, limiting the generalizability of our results. Therefore, further high-powered randomized trials using newer robotic systems are needed to provide a definitive statement about robotic knees.
Conclusion
This meta-analysis indicates that robotic total knee replacements offer superior post-operative anatomical and mechanical alignment compared to conventional total knee replacements. Despite this, clinical and functional outcomes, as well as complication rates, were similar between the two. These findings should be considered in light of potential confounding factors. More randomized controlled trials with the latest robotic systems are needed to confirm any superior functional and clinical outcomes from robotic-assisted surgeries.
Acknowledgements
None.
Author contributions
AE contributed to data collection, statistical analysis, manuscript writing; RA contributed to data collection, statistical analysis; OA contributed to data collection, manuscript review and submission; MZ contributed to data collection; ZS contributed to manuscript writing; GA contributed to data reviewing.
Funding
Open Access funding provided by the Qatar National Library. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Data and code availability
Not applicable as this is a review article. However, happy to provide access to any statistical data (coding) upon request.
Declarations
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Consent to participate
Not applicable as this is a review article.
Consent for publication
Not applicable as this is a review article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ben-Shlomo Y, Blom A, Boulton C. The national joint registry 17th annual report 2020 [Internet] London: National Joint Registry; 2020. [PubMed] [Google Scholar]
- 2.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 3.Choi YJ, Ra HJ. Patient satisfaction after total. Knee Arthroplasty Knee Surg Relat Res. 2016;28(1):1–15. doi: 10.5792/ksrr.2016.28.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE. Patient satisfaction after total knee replacement: a systematic review. HSS J. 2018;14(2):192–201. doi: 10.1007/s11420-018-9614-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clement ND, Calliess T, Christen B, Deehan DJ. An alternative technique of restricted kinematic alignment of the femur and gap balanced alignment of the tibia using computer aided navigation. Bone Jt Res. 2020;9(6):282–284. doi: 10.1302/2046-3758.96.BJR-2020-0119.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meloni MC, Hoedemaeker RW, Violante B, Mazzola C. Soft tissue balancing in total knee arthroplasty. Joints. 2014;2(1):37–40. [PMC free article] [PubMed] [Google Scholar]
- 7.Matsuda Y, Ishii Y, Noguchi H, Ishii R. Varus–valgus balance and range of movement after total knee arthroplasty. J Bone Jt Surg Br. 2005;87(6):804–808. doi: 10.1302/0301-620X.87B6.15256. [DOI] [PubMed] [Google Scholar]
- 8.Jakopec M, Harris SJ, Rodriguez y Baena F, Gomes P, Cobb J, Davies BL. The first clinical application of a “hands-on” robotic knee surgery system. Comput Aided Surg. 2001;6(6):329–339. doi: 10.3109/10929080109146302. [DOI] [PubMed] [Google Scholar]
- 9.Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR. Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Jt J. 2013;95(1):115–121. doi: 10.1302/0301-620X.95B1.29835. [DOI] [PubMed] [Google Scholar]
- 10.Khlopas A, Sodhi N, Sultan AA, Chughtai M, Molloy RM, Mont MA. Robotic arm-assisted total knee arthroplasty. J Arthroplasty. 2018;33(7):2002–2006. doi: 10.1016/j.arth.2018.01.060. [DOI] [PubMed] [Google Scholar]
- 11.Agarwal N, To K, McDonnell S, Khan W. Clinical and radiological outcomes in robotic-assisted total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2020;35(11):3393–3409.e2. doi: 10.1016/j.arth.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Think surgical (2022) https://thinksurgical.com. Accessed 20 Oct 2022
- 13.- “Mako.” Stryker (2022) https://www.stryker.com/us/en/portfolios/Orthopedics/joint-replacement/mako-robotic-arm-assisted-surgery.html. Accessed 20 Oct 2022
- 14.Minimally invasive surgery in orthopedics (2012) Springer, New York
- 15.NAVIO Surgical System - Robotics-assisted Knee Replacement | Smith & Nephew (2022) https://www.smith-nephew.com/professional/microsites/navio/. Accessed 20 Oct 2022
- 16.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-Analyzes of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 18.Kim YH, Yoon SH, Park JW. Does robotic-assisted TKA result in better outcome scores or long-term survivorship than conventional TKA? A randomized controlled trial. Clin Orthop Relat Res. 2020;478(2):266–275. doi: 10.1097/CORR.0000000000000916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liow MHL, Goh GS, Wong MK, Chin PL, Tay DK, Yeo SJ. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2942–2951. doi: 10.1007/s00167-016-4076-3. [DOI] [PubMed] [Google Scholar]
- 20.Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty. 2007;22(7):1054–1059. doi: 10.1016/j.arth.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 21.Song EK, Seon JK, Park SJ, Jung WB, Park HW, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1069–1076. doi: 10.1007/s00167-011-1400-9. [DOI] [PubMed] [Google Scholar]
- 22.Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013;471(1):118–126. doi: 10.1007/s11999-012-2407-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thiengwittayaporn S, Uthaitas P, Senwiruch C, Hongku N, Tunyasuwanakul R. Imageless robotic-assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve: a randomized controlled trial. Int Orthop. 2021;45(11):2851–2858. doi: 10.1007/s00264-021-05179-y. [DOI] [PubMed] [Google Scholar]
- 24.Vaidya NV, Deshpande AN, Panjwani T, Patil R, Jaysingani T, Patil P. Robotic-assisted TKA leads to a better prosthesis alignment and a better joint line restoration as compared to conventional TKA: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2022;30(2):621–626. doi: 10.1007/s00167-020-06353-2. [DOI] [PubMed] [Google Scholar]
- 25.Liow MH, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty. 2014;29(12):2373–2377. doi: 10.1016/j.arth.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 26.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Jt Surg Br. 1991;73(5):709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 27.Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Jt Surg Am. 2003;85(2):259–265. doi: 10.2106/00004623-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Decking J, Theis C, Achenbach T, Roth E, Nafe B, Eckardt A. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthop Scand. 2004;75(5):573–579. doi: 10.1080/00016470410001448. [DOI] [PubMed] [Google Scholar]
- 29.Hantouly AT, Ahmed AF, Alzobi O, Toubasi A, Salameh M, Elmhiregh A, Hameed S, Ahmed GO, Alvand A, Al Dosari MAA. Mobile-bearing versus fixed-bearing total knee arthroplasty: a meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol. 2022;32(3):481–495. doi: 10.1007/s00590-021-02999-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elmhiregh A, Abuodeh Y, Alzobi O, Zikria B, Alkhayarin M, Morrey BF. All-polyethylene versus metal-backed tibial components in total knee arthroplasty: a meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol. 2023;33:3611–3622. doi: 10.1007/s00590-023-03594-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1132–1141. doi: 10.1007/s00167-018-5138-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marchand KB, Ehiorobo J, Mathew KK, Marchand RC, Mont MA. Learning curve of robotic-assisted total knee arthroplasty for a high-volume surgeon. J Knee Surg. 2022;35(4):409–415. doi: 10.1055/s-0040-1715126. [DOI] [PubMed] [Google Scholar]
- 33.Savov P, Tücking LR, Windhagen H, Ettinger M. Comparable surgery time for robotic assisted total knee arthroplasty after initial learning curve. Orthop J Sports Med. 2020 doi: 10.1177/2325967120s00312. [DOI] [Google Scholar]
- 34.Yap CH, Colson ME, Watters DA. Cumulative sum techniques for surgeons: a brief review. ANZ J Surg. 2007;77(7):583–586. doi: 10.1111/j.1445-2197.2007.04155.x. [DOI] [PubMed] [Google Scholar]
- 35.Salman LA, Khatkar H, Al-Ani A, Alzobi OZ, Abudalou A, Hantouly AT, et al. Reliability of artificial intelligence in predicting total knee arthroplasty component sizes: a systematic review. Eur J Orthop Surg Traumatol. 2023 doi: 10.1007/s00590-023-03784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chun YS, Kim KI, Cho YJ, Kim YH, Yoo MC, Rhyu KH. Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty. 2011;26(4):621–625. doi: 10.1016/j.arth.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 37.Swank ML, Alkire M, Conditt M, Lonner JH. Technology and cost-effectiveness in knee arthroplasty: computer navigation and robotics. Am J Orthop (Belle Mead NJ) 2009;38(2 Suppl):32–36. [PubMed] [Google Scholar]
- 38.Ren Y, Cao S, Wu J, Weng X, Feng B. Efficacy and reliability of active robotic-assisted total knee arthroplasty compared with conventional total knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J. 2019;95(1121):125–133. doi: 10.1136/postgradmedj-2018-136190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Onggo JR, Onggo JD, De Steiger R, Hau R. Robotic-assisted total knee arthroplasty is comparable to conventional total knee arthroplasty: a meta-analysis and systematic review. Arch Orthop Trauma Surg. 2020;140(10):1533–1549. doi: 10.1007/s00402-020-03512-5. [DOI] [PubMed] [Google Scholar]
- 40.Zhang J, Ndou WS, Ng N, Gaston P, Simpson PM, Macpherson GJ, Patton JT, Clement ND. Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30(8):2677–2695. doi: 10.1007/s00167-021-06464-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wan XF, Yang Y, Wang D, Xu H, Huang C, Zhou ZK, Xu J. Comparison of outcomes after total knee arthroplasty involving postoperative neutral or residual mild varus alignment: a systematic review and meta-analysis. Orthop Surg. 2022;14(2):177–189. doi: 10.1111/os.13155. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable as this is a review article. However, happy to provide access to any statistical data (coding) upon request.