Key Findings.
-
▪
Existing guidelines recommend explantation of an implantable loop recorder (ILR) either upon battery depletion or reaching a diagnosis, taking into account patient preferences.
-
▪
ILR localization through palpation may be unreliable in individuals with high body mass index, often necessitating the use of fluoroscopy.
-
▪
Ultrasound-guided ILR explantation is a highly efficient and radiation-free technique that provides real-time device localization and minimizes incision size, with the potential to improve patient care.
An implantable loop recorder (ILR) has become a vital diagnostic tool for continuous monitoring of heart rhythm, especially in cases of unexplained syncope, recurrent palpitations, or suspected atrial fibrillation. ILRs have gained popularity in recent years for ambulatory cardiac monitoring because of their small size, absence of external leads, and extended battery life. In the latest UK National Audit of Cardiac Rhythm Management, over 11,000 ILRs were implanted annually.1 Current guidelines from the British Heart Rhythm Society recommend explantation of ILRs at completion of battery life, or explantation once diagnosis is reached, according to patient preference.2
Obesity introduces unique challenges to ILR explantation. Palpation alone for device localization may be unreliable in individuals with high body mass index (BMI), particularly in cases of device migration. In such instances, the use of fluoroscopy may be necessary but exposes patients to ionizing radiation. With no established guidelines for challenging ILR explantation, ultrasound offers a safer alternative modality of imaging to localize the device prior to or during ILR explantation. Here, we outline a simple technique of ultrasound-guided explantation of an ILR, emphasizing its practicality and benefits in patients with high BMI.
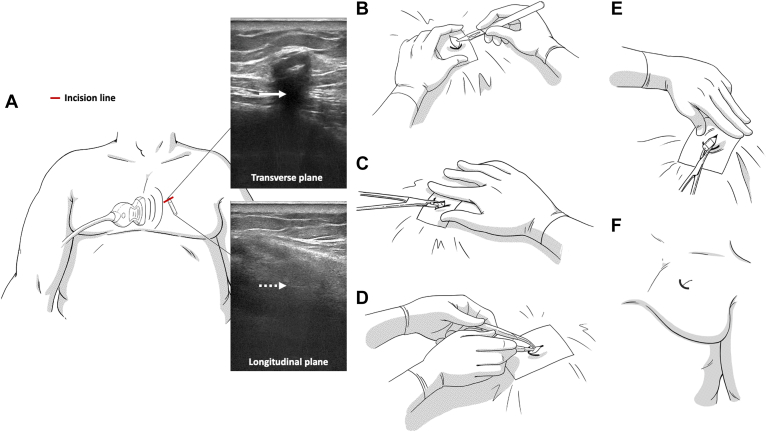
Our technique is illustrated in Figure 1. We have summarized a few practical points that could be helpful during ILR explantation in patients with high BMI. First, the use of ultrasound facilitates real-time visualization of the position of the device. This is particularly relevant in this group of patients as the device can be mobile in adipose tissue and ultrasound enables precise incision marking directly above the device. This approach facilitates easier access to the device, minimizes the size of the incision, and facilitates precise administration of local anesthetic for optimal pain control. Additionally, ultrasound enables visualization of adjacent structures, such as blood vessels and pleura, minimizing risk of complications. Second, we advocate the use of absorbable subcutaneous sutures followed by adhesive strips or absorbable subcuticular sutures, as obesity is associated with poor wound healing and increased risk of wound dehiscence. Furthermore, incision along Langer's lines yields superior healing and aesthetic results. We achieved satisfactory hemostasis in all cases through manual compression and/or local adrenaline.
Figure 1.
Step-by-step procedure for ultrasound-guided explantation of an implantable loop recorder (ILR). A: Identify and locate ILR using ultrasound; obtain images in transverse and longitudinal planes. Note the acoustic shadowing (arrow) and reverberation artifacts below the device (dashed arrow). B: A 10- to 15-mm incision is made directly above the device, ideally along a Langer’s line following administration of a local anesthetic. C: Dissection is performed to free up subcutaneous and/or fibrous tissue from the proximal end of the device (typically using Halsted mosquito forceps). D: If a capsule is attached to the device, cut the capsule with a scalpel to release the device. E: Once the device is visible, the proximal end of the device is grasped with forceps, and the device is pulled out of the pocket with gentle traction. F: Finally, the skin is closed with absorbable subcutaneous sutures (usually 1 or 2) followed by adhesive strips or absorbable subcuticular sutures.
Between January 2022 and January 2023, a total of 113 patients underwent ILR explantation at our institution. In 5 of these cases (4 females and 1 male), ultrasound was employed due to difficulties in locating the device, obviating any need for fluoroscopy. These patients had BMI values ranging from 33.3 to 40.5 kg/m2. The median time from implantation to explantation was 50 months, and all patients had Medtronic Reveal LINQ devices (Medtronic, Minneapolis, MN). We successfully explanted all devices with no immediate complications. All patients were discharged with comprehensive postprocedure advice. No complications, including wound dehiscence, infection, bleeding, or tissue ischemia, were reported.
The process of ILR explantation can pose challenges, particularly in cases in which palpation alone is not sufficient for localization, often due to large body habitus and/or device migration. To address this, ultrasound-guided explantation is a simple and effective strategy. It enables real-time localization of the device and its surrounding structures without exposing patients to ionizing radiation. This technique can be especially valuable at the point of care in identifying device migration or adherence to deeper structures, such as pleural space and abdomen, although such occurrences are relatively rare and may require complex surgical explantation.3, 4, 5, 6 The prevalence of obesity has nearly tripled since 1975 and has become a global pandemic.7 In light of this, the adoption of our technique offers potential to improve patient care.
In summary, ultrasound-guided explantation of ILRs is a simple, yet effective, approach that enables accurate device localization in patients with high BMI without exposure to ionizing radiation. This method holds the potential to enhance patient care, but additional training may be required.
Acknowledgments
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures
The authors have no conflicts to disclose.
Authorship
All authors attest they meet the current ICMJE criteria for authorship.
Patient Consent
The author/s confirm that written consent for submission and publication of the clinical case including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Ethics Statement
Ethical approval was not required.
Data Availability
Data are available upon reasonable request from the author at chokanan.thaitirarot@nhs.net.
References
- 1.National Institute for Cardiovascular Outcome Research National Cardiac Programme National Audit of Cardiac Rhythm Management (NACRM). 2023 Summary Report (2021/22 data) https://www.nicor.org.uk/wp-content/uploads/2023/06/10633-NICOR-Annual-Summary_Reports_NACRM_domain_Report_v5.pdf Available at:
- 2.British Heart Rhythm Society Standards for insertion, follow up and explant of implantable loop recorders [ILRs] by non-medical staff. 2020. https://bhrs.com/wp-content/uploads/2020/10/BHRS-ILR-Standards-for-Insertion-revised.pdf Available at:
- 3.Preminger M.W., Musat D.L., Sichrovsky T., Bhatt A.G., Mittal S. Migration of an implantable loop recorder into the pleural space. HeartRhythm Case Rep. 2017;3:539–541. doi: 10.1016/j.hrcr.2017.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahkovich M., Laish-Farkash A. Migration of a new generation implantable loop recorder: a case report. Eur Heart J Case Rep. 2021;5:ytab043. doi: 10.1093/ehjcr/ytab043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasnie A.A., Hasnie A.A., Assaly R.A. The case of the migrating loop recorder. J Am Coll Cardiol Case Rep. 2019;1:156–160. doi: 10.1016/j.jaccas.2019.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brignole M., Donateo P., Oddone D. Migration of an 'injectable' loop recorder in the dorsal pleural cavity. Europace. 2018;20:24. doi: 10.1093/europace/eux222. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization Obesity and overweight 2023. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request from the author at chokanan.thaitirarot@nhs.net.