Abstract
Introduction
Extended reality (XR) technologies are an umbrella term for simulated-based learning tools that cover 3-dimensional technologies, including virtual reality (VR), augmented reality (AR), and mixed reality (MR). At King Saud University, first-year pharmacy students are required to experience hospital observational training during the Introductory Pharmacy Practice Experience (IPPE). We aimed to measure the effectiveness and satisfaction of the VR learning experience among IPPE students.
Methods
A Quasi-Experimental study was conducted. The experimental arm included first-year PharmD students. VR headset was used to watch three narrated videos capturing 360° views of the outpatient, inpatient pharmacy, and counseling clinic. A test measuring students’ general knowledge was required prior to and post the experience, followed by a satisfaction survey. The control arm included second-year PharmD students who had traditional hospital visits and were administered a knowledge test and satisfaction survey.
Results
A total of 336 students were enrolled, 174 in the experimental arm and 162 in the control arm. The results showed improvement in the knowledge scores average among the experimental arm, 1.9 vs 3.5 in the pre-test and post-test. The control arm had a comparable score with an average of 3.7. Regarding self-assessment using four 5-likert scales assessing pharmacist role, skills, and responsibilities, 31.8 % and 42 % in the experimental arm compared to 28.9 % and 28.9 % in the control group answered strongly agree and agree, respectively. Regarding satisfaction, using five 5-Likert scales assessing the experience time, quality, and content, 53 % and 25 % in the experimental group compared to 34 % and 23 % in the control group answered strongly agree and agree, respectively.
Conclusion
VR provides pharmacy students with a standardized and effective learning and training experience. The experimental arm reported higher satisfaction rates and self-reported outcomes. Thus, implementing VR experiences within the pharmacy curriculum will provide students with an advanced educational advantage.
Keywords: Pharmacy, Education, Simulation, Experiential, Learning
1. Introduction
Simulation-based learning (SBL) experiences are effective training tools that have been adopted over decades in education (Kaplan et al., 2021). The term “SBL” generally refers to using simulated environments and techniques for learning purposes. For example, scenarios and games are common SBL tools that provide learners with a virtual learning experience and a sense of presence (Frasson and Blanchard, 2012, Landon-Hays et al., 2020). Recently, extended reality (XR) technologies, an umbrella term covering 3-dimensional technologies, including Virtual Reality (VR), Augmented Reality (AR), and Mixed Reality (MR), were actively utilized in SBL (Pomerantz and Rode, 2020, Takemoto et al., 2020). Offers several advantages over traditional learning and training, such as time and cost-saving, safety, and ease of implementation. One of the most critical challenges that XR faces are technical issues, including operational difficulties, audiovisual quality, and wearable gear comfort. Nevertheless, XR technologies are becoming essential tools that complement and overcome the shortcomings of traditional training and education practices. Thus, universities should be encouraged to support colleges in revising their curriculums and creating opportunities to adapt these tools to their maximum benefit.
Virtual reality was developed with the help of other technologies, including the internet, multimedia, and computers, but what makes it special is that it gives a sense of presence and the feeling of being immersed in a virtual experience (Ventola, 2019). The application of VR was reported in art, military settings, and medical practice. However, the implementation of VR in pharmacy education has been slow compared to other professions (Berkman, 2018, Coyne et al., 2019). In didactic pharmacy education, VR technology can help visualize complex pharmacology and chemistry topics in a three-dimensional space, providing students with the opportunity to 'see' the interactions at a molecular level. This visual representation helps simplify abstract concepts, leading to deeper understanding and better academic performance (Grieco, 2022, Norrby et al., 2015, Smith and Friel, 2021, Walters et al., 2022). In experiential pharmacy education, VR can be utilized to train students on various skills, from understanding the workflow of a pharmacy to medication compounding and patient interview skills (Coyne et al., 2019).
Pharmacy colleges providing Doctor of Pharmacy (PharmD) degrees are expected to graduate professionals with practice-based competencies. Therefore, it is essential to create opportunities for students to practice what they learned in a safe environment and orient them to different practice settings that enrich their knowledge and experiences (Accreditation Council for Pharmacy Education, 2015, Cheema, 2018). At the College of Pharmacy at King Saud University (KSU), PharmD students are exposed to several Introductory Pharmacy Practice Experiences (IPPE). During the first year, students enrolled in IPPE-1. At the end of the year, students are expected to be able to describe the scope of practice, identify the responsibilities of pharmacists in traditional and non-traditional settings, reflect on various skills needed to function effectively within a practice setting and identify the variety of career opportunities. In order to achieve the previous objectives, several practice area visits and reflections are conducted throughout the year. Groups of 8–10 students and training faculty will visit the different settings weekly, and a reflection assignment is usually required following the experience. Hence, the quality of these visits was not monitored, nor was the expected learning outcome measured. Therefore, we aimed to conduct an experimental study by creating and implementing VR visit experiences during the IPPE-1 and measuring its effectiveness and learners' satisfaction compared to traditional visits.
2. Methods
2.1. Study sample and design
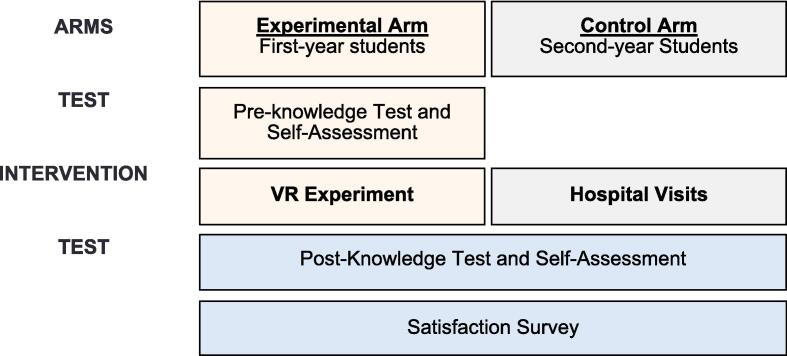
A quasi-experimental study was conducted at King Saud University, College of Pharmacy, to assess the impact of using virtual reality technology during the IPPE (Fig. 1) after obtaining the institutional review board approval. The experimental arm included all first-year pharmacy students who are currently enrolled in the IPPE-1 course. Second-year pharmacy students who completed the traditional IPPE-1 course were identified as the control arm. During the traditional IPPE-1 course, students conducted a hospital visit to orient them to the different pharmacy settings. In contrast to the experimental arm, the VR technology was implemented prior to any hospital visits.
Fig. 1.
VR in IPPE-1 quasi-experimental study design.
2.2. Procedure
The VR experiment was conducted at the pharmacy simulation lab using VR headsets (Fig. 2). A 360-technology camera was used to capture three different settings in King Saud University Medical City, a fifteen-hundred-bed academic tertiary care hospital in Riyadh, Saudi Arabia. Three videos were filmed in settings including inpatient pharmacy, outpatient pharmacy, and counseling clinic. Each video was 2 to 3 min long and narrated with a detailed description of each setting. For example, in the outpatient pharmacy video, the narrator focused on the environment and the dispensing process. Headings were added to the video pointing to the narrated subjects, e.g., unit dose system. Scenes of the videos are shown in Fig. 3.
Fig. 2.
Pharmacy simulation experience.
Fig. 3.
Sample of the VR Videos.
2.3. Questionnaire and knowledge test
A test containing a total of 10 questions was created to measure the student’s knowledge of different pharmacy settings and mapped to the IPPE-1 learning outcomes. First-year pharmacy students were expected to understand the roles, responsibilities, and equipment in each training setting (outpatient, inpatient, and clinic).
The test was administered before and after the experiment to ensure accuracy and validity and to measure first-year students’ knowledge gain. Additionally, a five-point Likert scale satisfaction survey was distributed following the experience among both arms to assess the students’ satisfaction with the time, approach, content, and environment of the experience. A pilot was done prior to implementation to ensure the validity and reliability of the testing tools.
2.4. Statistical analysis
All statistical analyses were performed using STATA 15.1 (StataCorp LP, College Station, Texas, USA). A paired t-test was performed for numerical data to analyze pre-test vs post-test scores. Furthermore, an unpaired t-test and Chi-Square test for numerical and ordinal data were used to compare 1st year and 2nd-year satisfaction survey scores.
3. Results
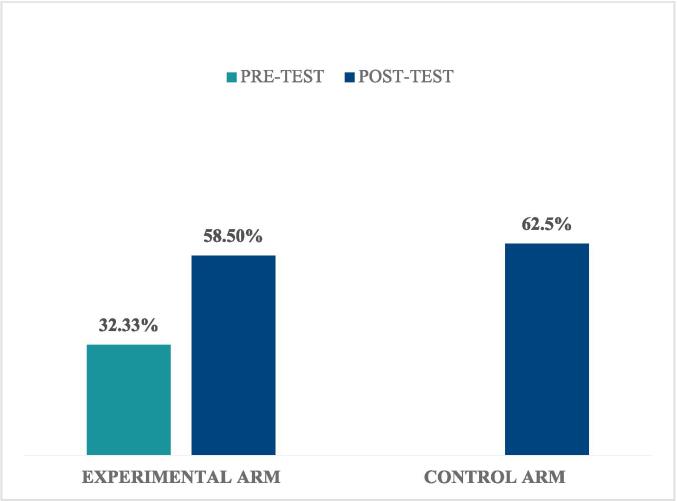
A total of 336 students were enrolled. The experimental arm included 174 students, and 162 students were in the control arm. The test results showed an improvement in the knowledge gained among the experimental arm, with an average of 1.94 ± 1.18 out of 6 scores in the pre-test and an average of 3.51 ± 1.24 out of 6 scores in the post-test. The post-test average in the control arm was 3.75 ± 1.24 out of 6 (Fig. 4).
Fig. 4.
Knowledge-test scores.
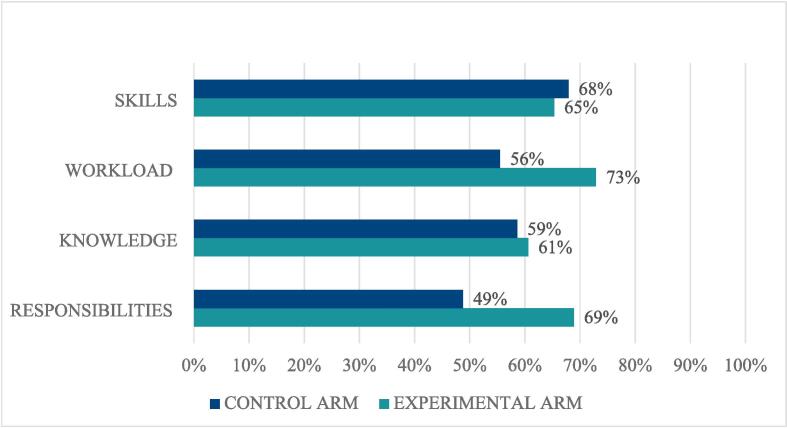
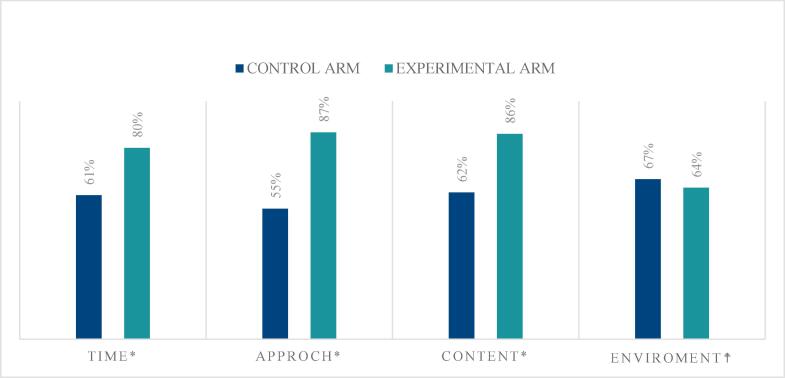
Paired t-test was performed to compare experimental arm scores in the pre-test vs post-test, resulting in a significant P value of < 0.0001 (Table 1). An Unpaired t-test/Welch two-sample t-test was performed to compare the experimental arm vs control arm knowledge scores, which showed a nonsignificant P value of 0.07 (Table 2). The test discussed simple tasks and definitions, such as “Who is responsible for labeling and preparing the Medication?” in question (1), and multiple answers were given [(A) The pharmacist, (B) The technician, (C) A machine, (D) The nurse], 11 % of experimental arm chose the correct answer in the pre-test compared to 60 % in the post-test. Similar improvement is shown throughout the entire test questions (Table 3). Moreover, students in the experimental arm scored higher in self-assessment statements than those in the control arm (Fig. 5). Finally, a significantly higher number of students were satisfied or strongly satisfied in the experimental arm vs control arm using the five-point Likert scale in all of the variables (p-value < 0.001), except for the environment variable (p-value = 0.493) (Fig. 6).
Table 1.
Experimental arm pre-test vs post-test results.
| Knowledge Test | Score | p-value |
|---|---|---|
| Pre-test | 1.94 ± 1.18 | <0.0001 |
| Post-test | 3.51 ± 1.24 |
Table 2.
Experimental arm vs control arm post-test results.
| Knowledge Test | Score | p-value |
|---|---|---|
| Experimental Arm | 3.51 ± 1.24 | 0.07 |
| Control Arm | 3.75 ± 1.24 |
Table 3.
Knowledge-test results.
| N | Questions | Control Arm |
Experimental arm |
|
|---|---|---|---|---|
|
Post-test only N = 162 |
Pre-test N = 172 |
Post-test N = 170 |
||
| 1 | “Who is responsible for labeling and preparing the medication?” | 35 (21.6 %) | 19 (11 %) | 102 (60 %) |
| 2 | “The process of providing important information, advice and assistance regarding medications to the patient is called” | 125 (77.2 %) | 60 (35 %) | 131 (77 %) |
| 3 | “All of the following are components of the medication label except” | 147 (90 %) | 80 (46.5 %) | 75 (44.4 %) |
| 4 | “What type of medication distribution system(s) is/are available at the inpatient pharmacy?” | 68 (42 %) | 32 (18.6 %) | 101 (59.4 %) |
| 5 | “The inpatient pharmacy has all the following except” | 102 (63 %) | 43 (25 %) | 58 (34 %) |
| 6 | “The pharmacist can receive the prescription through” | 131 (80.9 %) | 100 (58 %) | 129 (75.9 %) |
Fig. 5.
Self-assessment survey results.
Fig. 6.
Satisfaction survey results. *P-value < 0.001,  P-value = 0.493.
P-value = 0.493.
4. Discussion
In this study, VR provided students with a realistic, safe, immersed reality experience. The gain in students’ knowledge was observed in the post-test scores in the experimental arm, which was comparable to the knowledge test results in the control arm. VR experience students were much more confident about their knowledge of the self-assessment scales and had higher satisfaction scores when compared to regular hospital visits.
The effectiveness of different SBL technologies was proven in multiple studies in pharmacy education (Benedict et al., 2013, Gustafsson et al., 2017, Lichvar et al., 2016, Smith and Benedict, 2015). One of the notable applications was in the University of Pittsburgh College of Pharmacy, where they introduced simulated case software to final-year pharmacy students. Students found the simulated cases engaging and helpful in therapeutic education (Bernaitis et al., 2018). Using VR technology in SBL was studied in other healthcare disciplines, including nursing (Smith et al., 2018). However, to our knowledge, this study was the first to explore the use of VR SBL in delivering experiential pharmacy practice experiences.
Several strengths were identified. In this scientific study, we explored the role of VR in experiential pharmacy education in a controlled environment using a large sample size. Thus, eliminating any extraneous variables and increasing the generalizability of the study. The design incorporated the use of a control group, which is essential for minimizing biases and drawing accurate conclusions. Lastly, the study was well structured to measure the experiential course objectives, hence enhancing its replicability within pharmacy schools’ curriculums.
Some limitations were identified during the study. First, the single-center design may limit its generalizability. Additionally, it is important to notice that using VR technology in pharmacy education is in its early stages, where it lacks standardization of the content, evaluation process, and its place within the pharmacy curricula. Secondly, there are some technical difficulties, especially in the early implementation stages. Software glitches and hardware malfunctions led to disruption of the learning experience; however, less than 5 % of the captured information was missing. Thirdly, VR technology has limited capabilities when it comes to practical skills. Since VR might not fully replicate the complexity of actual pharmacy practice, its applicability is limited until now in advanced experiential education, such as hands-on skills such as counseling and communication with other healthcare professionals. Finally, accessibility might be an issue for students with disabilities or other health conditions (e.g., motion sickness and vertigo). While VR technology holds the potential to enhance pharmacy education, these limitations must be considered when implementing it in a curriculum.
5. Conclusion
VR provides a standardized learning experience in pharmacy practice when compared to traditional visits, with comparable education outcomes. Higher satisfaction rates and self-reported outcomes were observed among the VR arm. Thus, implementing VR experiences within the pharmacy curriculum will provide students with an advanced educational advantage. However, further studies are needed to assess long-term retention and skill gain.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of King Saud University [No. E-21-6084]. Written informed consent from the participants was obtained per the national legislation and the institutional requirements.
Funding
This Project was funded by the Center for Excellence in Learning and Teaching at King Saud University for funding the project as part of the Center’s Teaching Excellence grant initiative, which aims to support students’ skills in the job market. All data used in this research were collected from a project supported by the center. Additional funding was provided by Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2023R319), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
CRediT authorship contribution statement
Nora Alkhudair: Conceptualization, Methodology, Visualization, Formal analysis, Investigation, Writing – original draft, Funding acquisition. Fatma Alrayes: Conceptualization, Methodology, Formal analysis, Writing – review & editing. Dalal Alsehli: Conceptualization, Methodology, Visualization, Formal analysis, Investigation, Writing – original draft. Shahad AlRayes: Conceptualization, Methodology, Visualization, Formal analysis, Investigation, Writing – original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors thank the Center for Excellence in Learning and Teaching at King Saud University for supporting the project as part of the Center’s Teaching Excellence grant initiative, which aims to support students’ skills in the job market. All data used in this research were collected from a project supported by the center.
References
- Accreditation Council for Pharmacy Education, 2015. Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree, ACPE.
- Benedict N., Schonder K., McGee J. Promotion of self-directed Learning using virtual patient cases. Am. J. Pharm. Educ. 2013;77:151. doi: 10.5688/ajpe777151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman M.I. Encyclopedia of Computer Graphics and Games. Springer International Publishing; Cham: 2018. History of virtual reality; pp. 1–9. [DOI] [Google Scholar]
- Bernaitis N., Baumann-Birkbeck L., Alcorn S., Powell M., Arora D., Anoopkumar-Dukie S. Simulated patient cases using DecisionSimTM improves student performance and satisfaction in pharmacotherapeutics education. Curr. Pharm. Teach. Learn. 2018;10:730–735. doi: 10.1016/j.cptl.2018.03.020. [DOI] [PubMed] [Google Scholar]
- Cheema E. The need to introduce simulation-based teaching in pharmacy education in Saudi Arabia. Pharmacy. 2018;6:60. doi: 10.3390/pharmacy6030060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne L., Merritt T.A., Parmentier B.L., Sharpton R.A., Takemoto J.K. The past, present, and future of virtual reality in pharmacy education. Am. J. Pharm. Educ. 2019;83:7456. doi: 10.5688/ajpe7456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frasson, C., Blanchard, E.G., 2012. Simulation-Based Learning, in: Encyclopedia of the Sciences of Learning. Springer US, Boston, MA, pp. 3076–3080. Doi: 10.1007/978-1-4419-1428-6_129.
- Grieco P. Virtual and augmented reality applications in medicinal chemistry. Future Med. Chem. 2022;14:1417–1419. doi: 10.4155/FMC-2022-0213. [DOI] [PubMed] [Google Scholar]
- Gustafsson M., Englund C., Gallego G. The description and evaluation of virtual worlds in clinical pharmacy education in Northern Sweden. Curr. Pharm. Teach. Learn. 2017;9:887–892. doi: 10.1016/j.cptl.2017.06.002. [DOI] [PubMed] [Google Scholar]
- Kaplan A.D., Cruit J., Endsley M., Beers S.M., Sawyer B.D., Hancock P.A. The effects of virtual reality, augmented reality, and mixed reality as training enhancement methods: a meta-analysis. Hum. Factors J. Hum. Factors Ergon. Soc. 2021;63:706–726. doi: 10.1177/0018720820904229. [DOI] [PubMed] [Google Scholar]
- Landon-Hays M., Peterson-Ahmad M.B., Frazier A.D. Learning to teach: how a simulated learning environment can connect theory to practice in general and special education educator preparation programs. Educ. Sci. 2020;10:184. doi: 10.3390/educsci10070184. [DOI] [Google Scholar]
- Lichvar A.B., Hedges A., Benedict N.J., Donihi A.C. Combination of a flipped classroom format and a virtual patient case to enhance active learning in a required therapeutics course. Am. J. Pharm. Educ. 2016;80:175. doi: 10.5688/ajpe8010175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norrby, M., Grebner, C., Eriksson, J., Boströ, J., 2015. Molecular Rift: Virtual Reality for Drug Designers. Doi: 10.1021/acs.jcim.5b00544. [DOI] [PubMed]
- Pomerantz J., Rode R. Exploring the future of extended reality in higher education. Educ. Rev. 2020 [Google Scholar]
- Smith, C., Friel, C.J., 2021. Experiences in Teaching and Learning Development and use of augmented reality models to teach medicinal chemistry. Doi: 10.1016/j.cptl.2021.06.008. [DOI] [PubMed]
- Smith M.A., Benedict N. Effectiveness of educational technology to improve patient care in pharmacy curricula. Am. J. Pharm. Educ. 2015;79:15. doi: 10.5688/ajpe79115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S.J., Farra S.L., Ulrich D.L., Hodgson E., Nicely S., Mickle A. Effectiveness of two varying levels of virtual reality simulation. Nurs. Educ. Perspect. 2018;39:E10–E15. doi: 10.1097/01.NEP.0000000000000369. [DOI] [PubMed] [Google Scholar]
- Takemoto, J., Parmentier, B., Bratelli, R., Merritt, T., California Health Sciences University, L., 2020. Extended reality in patient care and pharmacy practice: A viewpoint. J. Contemp. Pharm. Pract. 66, 22–27. Doi: 10.37901/jcphp18-00030.
- Ventola C.L. Virtual reality in pharmacy: opportunities for clinical, research, and educational applications. P T. 2019;44:267–276. [PMC free article] [PubMed] [Google Scholar]
- Walters R.K., Gale E.M., Barnoud J., Glowacki D.R., Mulholland A.J. The emerging potential of interactive virtual reality in drug discovery. Expert Opin. Drug Discov. 2022;17:685–698. doi: 10.1080/17460441.2022.2079632. [DOI] [PubMed] [Google Scholar]