Abstract
Introduction
Cervical cancer is a preventable yet highly prevalent disease in Africa. Despite female adolescents and young women being a target group for cervical cancer prevention strategies, little research has examined their knowledge of how to prevent the disease. The study aimed to describe: (a) knowledge about cervical cancer prevention and (b) sociodemographic, social, and systemic factors associated with and interacting with knowledge among female senior high school students in Ghana.
Methods
A cross-sectional survey assessed knowledge about (a) risk factors and (b) primary and secondary prevention of cervical cancer among 2,400 female students from 17 public senior high schools in the Ashanti region, Ghana. Descriptive statistics were used to describe knowledge. Linear mixed-effects regression models were used to examine factors associated with knowledge scores.
Results
Knowledge gaps were observed for at least two-thirds (>65%) of students. Most students (mean age = 17) did not know that early sexual debut (before 18 years) is a risk factor for cervical cancer (72%) and that a blood test cannot detect cervical cancer (71%). Students in later stages of senior high school education and those who received sexual health education from teachers and parents had significantly greater cervical cancer knowledge scores than their counterparts. Interactive effects showed that school-based sexual health education was associated with higher knowledge scores than home-based education among students.
Conclusions
Most female senior high school students had gaps in knowledge about cervical cancer prevention. Finding new ways to strengthen the capacity of schools and parents to deliver accurate cervical cancer prevention information is warranted.
Keywords: cervical cancer, prevalence, students, risk factors, correlates, prevention, knowledge
Introduction
Cervical cancer is the fourth most common cancer in women globally and the leading cause of cancer-related death in Africa (Sung et al., 2021). Compared with worldwide estimates, the age-standardized incidence and mortality rate of cervical cancer in Ghana are two times higher (27.4 and 17.8, respectively; Sung et al., 2021). It is also the second most common cancer and the leading cause of cancer deaths among women in Ghana (Sung et al., 2021). The high incidence of cervical cancer could be attributed to increasing exposure to risk factors, including human papillomavirus (HPV) infections (Bruni et al., 2022). Between 2004 and 2018, the percentage of HPV 16/18 infections detected in cervical cancer cases increased from 47% (Awua et al., 2016) to 59% (Bruni et al., 2022) in Ghana. Besides HPV infections, other factors contributing to cervical cancer cases are long-term hormonal contraceptive use, Human Immunodeficiency Virus (HIV), tobacco smoking, multiple sexual partners, multigravida, immunosuppression, and family history of cervical cancer (Bruni et al., 2022).
Despite the growing prevalence of HPV 16/18 infections from 6.2% (Donkoh et al., 2022) to 11.2% (Krings et al., 2019) between 2011 and 2014 among Ghanaian women, the uptake of regular organized cervical screening programs offered by benevolent organizations is less than 12% (Ampofo et al., 2020; Binka et al., 2016). Due to the low coverage of screening services and the absence of symptoms in early-stage cervical cancer, the majority of women with cervical cancer in Ghana have their cancers detected at an advanced stage of the disease (Nartey et al., 2016). Low patronage of cervical screening and late-stage presentation of the disease have been attributed to a number of individual, community and health system barriers, including poor knowledge about the disease (i.e., poor health literacy; Chidyaonga-Maseko et al., 2015; Dunyo et al., 2018). No data exist for HPV vaccination uptake among adolescents and young women, but this is not surprising given that there is no government-mandated HPV vaccination program in Ghana.
Knowledge about cervical cancer prevention is vital for reducing morbidity and mortality associated with the disease. Insufficient knowledge about cervical cancer risk factors, HPV vaccination, and screening is linked to low participation in prevention programs and adverse health outcomes including late diagnosis and treatment (Chidyaonga-Maseko et al., 2015; Ebu et al., 2014; Rugutt, 2014). While previous studies have found inadequate knowledge about cervical cancer risk factors, vaccination, and screening among Ghanaian women, men in the general population, and college students (Binka et al., 2016; Ebu et al., 2014; Gyamfua et al., 2019; Williams & Amoateng, 2012; Zurales et al., 2023), few studies have examined knowledge of the disease among high school students.
There are a disproportionately small number of studies about cervical cancer knowledge among high school girls. Of ten studies identified in the literature (Ayissi et al., 2012; Bardaji et al., 2018; Bowyer et al., 2013; Ifediora & Azuike, 2018; Lee et al., 2014; Mapanga et al., 2019; Martianus et al., 2018; Opoku Agyemang & Manortey, 2018; Poudel & Sumi, 2019; Rashwan et al., 2013), only three were conducted in Western Africa. In Cameroon, more than 70% of girls have been reported to have knowledge about cervical cancer risk factors and HPV vaccination (Ayissi et al., 2012; Bardaji et al., 2018). Conversely, less than 50% of Ghanaian and Nigerian girls have knowledge about cervical cancer risk factors and the Pap test (Ifediora & Azuike, 2018; Opoku Agyemang & Manortey, 2018). While these studies provide some insight, they are limited by the modest sample sizes (<400; Ifediora & Azuike, 2018; Opoku Agyemang & Manortey, 2018) and the use of convenience sampling (Ifediora & Azuike, 2018), which reduces the generalizability and quality of the findings.
Health literacy refers to personal knowledge and competencies that provide the ability to access, comprehend, evaluate, and use the information to improve health and engage in health care services (World Health Organization, 2021). Health literacy is consistently linked with knowledge about sexual and reproductive health (Kilfoyle et al., 2016) and cervical cancer (Kim & Han, 2016) risk behaviors and prevention. According to the adolescent framework for health literacy, three major factors can affect adolescent health literacy: individual characteristics, social environment (i.e., parents and peers), and broader systems (i.e., school and health care; Manganello, 2007). Individual factors crucial to health literacy include age, race, gender, cultural background, and parental education (Fleary et al., 2018). Indeed, previous studies have found that cervical cancer knowledge among high school students may be influenced by individual factors (Li et al., 2009; Mapanga et al., 2019). Evidence suggests that parent-based (Widman et al., 2019), peer-led (Sun et al., 2018), and school-based (Sani et al., 2016) sexual health intervention programs improve adolescent sexual health knowledge of factors such as HIV/acquired immunodeficiency syndrome and contraceptive use. School-based cervical cancer education was found to be effective in improving cervical cancer/HPV infection knowledge among female students in our recent review of English-language publications describing randomized controlled trials (Ampofo et al., 2022). Of the 13 studies included in the review, the majority (n=8) were from the United States and assessed knowledge about cervical cancer risk factors and primary prevention (Ampofo et al., 2022).
The World Health Organization’s Health Promoting Schools (HPS) advocacy framework highlights an integrated approach for improving students’ health and well-being (World Health Organization, 1997). The HPS comprises three broad elements: first, integrating health education in school curricula; second, changing the social and physical environment of schools; and third, schools’ engaging with health and education officials, parents, and community (Langford et al., 2016; World Health Organization, 1997). Understanding the current knowledge of high school students and the factors associated with increased knowledge is important for designing and implementing effective school-based cervical cancer education programs, guiding and targeting strategies including the development of educational materials, and identifying channels to reach students (Glanz et al., 2008).
To the authors’ knowledge, no study has comprehensively focused on assessing knowledge about risk factors, primary and secondary prevention of cervical cancer, and how social, family/parental, peer and systemic factors influence knowledge among high school girls across low-, middle-, and high-income settings. Guided by the adolescent health literacy framework and the HPS advocacy framework, this study aimed to describe among female senior high school students: (a) cervical cancer prevention knowledge; (b) individual characteristics, social environment (i.e., parents and peers), and broader systems (i.e., school and health care) associated with cervical cancer prevention knowledge; and (c) how social environment and broader systems interact to affect cervical cancer prevention knowledge.
Material and Method
Study Design, Setting, and Period
The University of Newcastle Human Research Ethics Committee reviewed and approved (#H-2020-0378) the protocol and all study materials. A cross-sectional paper-based survey evaluated knowledge about cervical cancer prevention among 2400 high school students from 17 schools in the Ashanti region of Ghana between February and July 2021. This was part of a larger study examining the prevalence of cervical cancer risk factors and HPV vaccination intentions among high school students. Details of the study methods are described elsewhere (Ampofo et al., 2023; see Appendix A).
Sample Size
A calculated sample of 17 schools with an average of 71 eligible student participants for each school enabled estimation of the proportion of students with sufficient knowledge (defined as a score of 50%, and conservatively assumed to be 50% of the population) with a margin of error of 6%. This calculation assumed an effective sample size of 260 students, resulting from a design effect of 4.55 and an intraclass correlation of 0.05 (Bland, 2015). Allowing for a conservative 50% response rate, an average of 141 students per school was determined and approximated to give a final sample size of 2,400 participants (Bland, 2015).
Measures
Self-administered study-specific surveys were developed in accordance with the Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) guidelines in three phases (Gagnier et al., 2021).
Phase 1: Item Generation and Content Validity
A pool of 23 candidate items drawn from the previous literature and survey instruments assessing cervical cancer and HPV knowledge among adolescents, both in and out of school, were considered for selection (Ayissi et al., 2012; Bardaji et al., 2018; Bowyer et al., 2013; Martianus et al., 2018; Poudel & Sumi, 2019). In line with the recommendations of Lynn (1986), 12 experts including health behavior scientists (n=4), epidemiologists (n=2), nurses (n=2), doctors (n=2), and psychologists (n=2) were purposively selected from the research team’s research and clinical networks. A preliminary list of items was provided by email to the experts who (a) indicated the relevance and comprehensibility of each item on a dichotomous scale of “relevant or not relevant” and “comprehensive or not comprehensive” and (b) suggested any additional items or item modification. Based on the experts’ feedback, new items were added, redundant or duplicate items were deleted, complex items were simplified, and response options were revised. Consensus among experts was required before an item was removed. A summary of feedback from the first round of expert review and the revised list of items were provided to the experts, and the process of item review was repeated. This iterative process of expert review resulted in 11 new items being added (e.g., “Infection with a virus” was added as a response option to “Which of the following can lead to cervical cancer?”), 10 items were deleted (e.g., “Infection with candidiasis” was removed as a response option to “Which of the following can lead to cervical cancer?”), and 9 items were re-worded (e.g., “Having lots of abortions” became “Having more than one abortion”). The resultant 34-item preliminary survey was piloted among students.
Phase 2: Pilot-Testing and Instrument Refinement
One hundred students from a public senior high school in the Ashanti Region were invited to complete the preliminary survey to assess the feasibility of survey administration (completion rate ≥50%, response burden <20 minutes) and data entry. Following completion of the survey, 20 participants were purposively sampled and invited to participate in a qualitative semi-structured telephone interview conducted by one author (AGA). Interviews were recorded with participants’ consent. Interview questions (see Supplemental File 1) elicited general feedback about the survey, as well as knowledge, beliefs, and attitudes regarding cervical cancer, HPV vaccination, and cervical cancer screening, guided by the Integrated Behavior Model (Montaño & Kasprzyk, 2015). Data saturation was achieved after eight interviews, and no further interviews were conducted. Manual codes were identified and developed into themes by one author (AGA) using the Integrated Behavior Model. Based on findings from the pilot testing, two new items were added (“Poor personal hygiene” and “Contact with blood of a person with cervical cancer” were added as response options to “Which of the following can lead to cervical cancer?”), existing items were modified (e.g., “Getting an injection for cervical cancer” became “Getting vaccinated with HPV vaccines to prevent cervical cancer” as a response option to “Which of the following can reduce a woman’s chance of getting cervical cancer?”), and re-ordered. The survey was then reformatted.
Phase 3: Psychometric Evaluation
The psychometric performance of the knowledge scale was evaluated against the following criteria: (a) internal consistency, i.e., acceptable reliability coefficient (Cronbach’s α > 0.7) and acceptable inter-item and item-total correlations (0.2–0.8) and (b) item analysis (i.e., item-by-item frequency). Reliability was acceptable (Cronbach α = 0.82), and inter-item and item-total correlations indicated that item efficiency was good (r = 0.2–0.7). Item-by-item frequency distribution showed a good spread (fairly equal distribution or flat normal distribution) of response options (Streiner et al., 2015). Items below the recommended threshold were assessed for cultural and clinical relevance before deleting them.
This process led to the revised 26-item survey. Components of the final measure are described below and attached as Supplemental File 2.
Cervical Cancer Prevention Knowledge
Cervical cancer prevention knowledge was measured by 26 items across 4 elements. Items consisted of evidence-based and non-evidence-based statements about (a) cervical cancer risk factors (12 items; response options were “Yes/No”), (b) primary prevention strategies (5 items; response options were “True/False”), (c) secondary prevention strategies (5 items; response options were “True/False”); and (d) HPV-related knowledge (4 items; response options were “True/False”). Participants’ answers were scored as “1” for a correct response and “0” for an incorrect or incomplete response to statements. An overall knowledge score was calculated as the sum of all responses, and expressed as a score out of 26, with higher scores indicating more knowledge.
Participant Characteristics
Seven items measured age, grade (SHS 1–3), ethnicity (Akan/Northerner/Ewe and Guan/Ga-Adangbe/Other), program of study (General Arts/Science/Home Economics/Business/Agriculture/Visual Arts), enrollment status (Boarder/Day), mother/female guardian education (No formal education/Primary education/Secondary and Tertiary education) and father/male guardian education (No formal education/Primary education/Secondary and Tertiary education).
Family and Social Factors
Two items measured whether participants had ever received sexual health education from their parents/guardians and friends. Response options were “Yes/No.”
Systemic Factors
School system characteristics were assessed by three items: whether participants had ever received sexual health education from their teachers (response options were “Yes/No”); whether their schools organize sexual health education classes (response options were “Yes/No”); and the schools’ locations (i.e., District or Metropolitan/Municipal). Health system influence was assessed by one item that asked whether participants had ever received sexual health education from a health care professional (response options were “Yes/No”).
Data Analysis
Knowledge was analyzed using descriptive statistics including percentages, frequencies, means, and standard deviation (SD). Mean (SD) knowledge scores were calculated from the percentage of correct responses. For the purpose of the analysis, the following variables were re-categorized: Ethnicity (Akans vs. Northerner/Ewe/Guans/Ga—Adangbe/Other); and program of study, Science/Home Economics/Agric (STEM—Science, Technology, Engineering and Math,) vs, General Arts/Visual Arts/Business, Non-STEM)).
Linear mixed-effect regression modeling (LMM) was used to analyze the associations between correlates (i.e., demographic characteristics, social factors, and systemic factors) and overall knowledge scores. The LMM included fixed effects for all correlates and a random school-level intercept to model the clustering within schools from the Ashanti Region. Interaction effects between sexual health education received from parents, peers, teachers, school, and health care professionals were included in the LMM to assess whether there was a synergistic effect between any of these prespecified variables. Pairwise interaction terms were formed by multiplying any two variables, with each entered one at a time into the initial model. Interaction terms that improved the model and/or were significant were retained. The formal test of interaction was assessed using the Wald test. Model assumptions were assessed by inspecting residual plots. The confidence interval and significant p value were set at 95% and less than 0.05, respectively. The intra-cluster correlation coefficient (ICC) was calculated and presented as an estimate of the between-school variance divided by the sum of the within-school and between-school variance. For this study, the ICC reflects how similar knowledge scores are for students in the same school. If the ICC is close to zero, it is indicative of homogeneity between students in each school and small to no differences in knowledge scores between the samples across all included schools.
Results
Two thousand four hundred students participated in the study. All 17 schools that were invited agreed to participate, and the target quota of student participants of at least 141 was achieved in each school. Table 1 presents the characteristics of student participants. The average age of participants was 17 years. The most prevalent grade level of participants was SHS level one (46%), and 77% belonged to the Akan tribe. More than half (52%) of participants were General Arts students. Over 60% of participants’ parents had a secondary or tertiary education.
Table 1.
Characteristics, Social and Systemic Factors of Participants, N=2,400.
| Characteristics | N a (%) |
|---|---|
| Age, M ( SD ) | 17.32 (1.22) |
| Grade | |
| SHS 1 | 1,107 (46%) |
| SHS 2 | 573 (24%) |
| SHS 3 | 720 (30%) |
| Ethnicity | |
| Akan | 1,860 (77%) |
| Northerner | 300 (13%) |
| Ewe/Guans | 121 (5%) |
| Ga—Adangbe | 49 (2%) |
| Other | 68 (3%) |
| Program of study | |
| Science | 287 (12%) |
| General arts | 1,251 (52%) |
| Visual arts | 69 (3%) |
| Business | 138 (6%) |
| Home economics | 584 (24%) |
| Agric | 59 (2%) |
| Mother/female guardian education | |
| No formal education | 217 (9%) |
| Primary/Junior High School | 616 (26%) |
| Senior High School or higher | 1,556 (65%) |
| Father/male guardian education | |
| No formal education | 171 (7%) |
| Primary/Junior High School | 553 (23%) |
| Senior High School or higher | 1,640 (69%) |
| Ever received sexual health education by parents/guardians | |
| Yes | 1,732 (72%) |
| No | 661 (28%) |
| Ever received sexual health education by friends | |
| Yes | 1,492 (62%) |
| No | 902 (38%) |
| Ever received sexual health education by teachers | |
| Yes | 1,830 (76%) |
| No | 564 (24%) |
| Provision of sexual health education classes in school | |
| Yes | 834 (35%) |
| No | 1,557 (65%) |
| Ever received sexual health by health care provider | |
| Yes | 1,215 (51%) |
| No | 1,170 (49% |
| Administrative location of school | |
| District | 1,275 (53%) |
| Metropolitan/municipal | 1,123 (47%) |
May not add up to 2,400 due to missing data.
Cervical Cancer Prevention Knowledge
The overall mean knowledge score was 14.57 (median: 15, SD: 2.68, range: 5–23) out of a possible score of 26. No student correctly answered all items, and 68% (95% CI: [66%, 70%]) of students correctly answered more than half of all items. The percentages of correct responses for the items are presented in Table 2. Knowledge gaps reported by at least two-thirds of students included not being aware that: early sexual debut (before 18 years) was a risk factor for cervical cancer (72%); a blood test cannot detect whether you have cervical cancer (71%); and cervical cancer screening should begin in women at age 21 (69%). About half of students incorrectly believed that poor hygienic practices (47%) and activities pertaining to the introduction of foreign substances into the vagina (46%) may lead to cervical cancer, and that cervical cancer can be transmitted through blood (44%) and can be prevented by praying to God (42%).
Table 2.
Participants’ Knowledge About Cervical Cancer Risk Factors, Primary and Secondary Prevention Strategies, and HPV-Related Knowledge. N=2,400.
| Knowledge about cervical cancer risk factors | Correct response | ||
|---|---|---|---|
| N (%) | [95% CI] | ||
| Which of the following can increase chances of getting cervical cancer? | |||
| Evidence-based items | Smoking cigarettes | 921 (38%) | [37%, 40%] |
| Having sexually transmitted infections e.g., HPV, HIV/AIDS | 1,092 (46%) | [44%, 48%] | |
| Using oral contraceptives | 1,059 (44%) | [42%, 46%] | |
| Early sexual intercourse (before 18 years) | 678 (28%) | [26%, 30%] | |
| Having multiple sexual partners | 885 (37%) | [35%, 39%] | |
| Having a family history of cervical cancer | 835 (35%) | [33%, 37%] | |
| Non-evidence-based items | Poor personal hygiene | 1,270 (53%) | [51%, 55%] |
| Blood contact of a person with cervical cancer | 1,336 (56%) | [54%, 58%] | |
| Having one or more abortions | 1,327 (55%) | [53%, 57%] | |
| Vaginal use of Dettol or strong soaps | 1,118 (47%) | [45%, 49%] | |
| Spiritual forces (e.g., witchcraft) | 1,929 (81%) | [79%, 82%] | |
| Vaginal insertion of herbs | 1,294 (54%) | [52%, 56%] | |
| Knowledge about primary prevention of cervical cancer | Correct response | ||
| N (%) | [95% CI] | ||
| Which of the following can reduce a woman’s chance of getting cervical cancer? | |||
| Evidence-based items | Use of condom during sexual intercourse | 1,343 (56%) | [54%, 58%] |
| Having regular cervical check-ups | 1,840 (77%) | [75%, 79%] | |
| Getting HPV vaccines | 1,613 (67%) | [65%, 69%] | |
| Non-evidence-based items | Praying to God | 1,393 (58%) | [56%, 60%] |
| Fasting to God | 1,676 (70%) | [68%, 72%] | |
| Knowledge about secondary prevention of cervical cancer | Correct response | ||
| N (%) | [95% CI] | ||
| Please indicate whether you believe each statement about cervical cancer is TRUE OR FALSE | |||
| Evidence-based items | Cervical cancer screening can find changes to the cervix early | 1,788 (75%) | [73%, 76%] |
| Cervical cancer can be prevented through screening | 1,547 (65%) | [63%, 66%] | |
| Cervical cancer can be cured when detected early. | 1,791 (75%) | [73%, 76%] | |
| Cervical cancer screening should begin in women at age 21. | 737 (31%) | [29%, 33%] | |
| Non-evidence-based items | A blood test can detect whether or not you have cervical cancer. | 705 (29%) | [28%, 31%] |
| HPV-related knowledge | Correct response | ||
| N (%) | [95% CI] | ||
| Please indicate whether you believe each statement about cervical cancer is TRUE OR FALSE | |||
| Evidence-based items | HPV infection can be transmitted during sexual intercourse | 1,895 (79%) | [77%, 81%] |
| HPV infection can cause cervical cancer | 1,837 (77%) | [75%, 78%] | |
| HPV infection can be prevented by a vaccine | 1,628 (68%) | [66%, 70%] | |
| Non-evidence-based items | Only girls should be vaccinated against HPV | 1,395 (58%) | [56%, 60%] |
| Accurate knowledge of more than half of all statements | 1,633 (68%) | [66%, 70%] | |
| Accurate knowledge of all statements | 0% | ||
| Overall knowledge score | M (SD) = 14.57 (2.68) | ||
HPV = human papillomavirus; HIV/AIDs = human immunodeficiency virus infection and acquired immunodeficiency syndrome.
Correlates of Cervical Cancer Prevention Knowledge
Compared with participants in SHS Level 1, those in SHS Levels 2 and 3 had statistically significantly higher knowledge scores. Participants who received sexual health education from their parents/guardians (mean difference = 0.51 points, 95% CI: [0.18, 0.84]) and teachers (mean difference = 0.63 points, 95% CI: [0.31, 0.94]) had statistically significantly higher knowledge scores than participants who did not receive sexual health education from their parents/guardians and teachers respectively (see Table 3). Participants whose school provided sexual health education classes had statistically significant higher knowledge scores (mean difference = 0.68 points, 95% CI: [0.16, 1.20]) than those who did not have sexual health education classes in their school.
Table 3.
Linear Mixed-Effects Regression of Overall Cervical Cancer Prevention Knowledge Score and Interactive Effects.
| Variables | |
|---|---|
| Participant characteristics | Mean difference [95% CI] |
| Age (per year) | 0.04 [−0.08, 0.16] |
| Grade | |
| SHS two | 0.85 [0.47, 1.22]* |
| SHS three | 0.58 [0.21, 0.95]* |
| SHS one | 1 |
| Ethnicity | |
| Akan | −0.17 [−0.44, 0.10] |
| Northerner/Ewe/Guans/Ga—Adangbe/Other | 1 |
| Program of study | |
| General arts/Visual arts/Business (Non-STEM) | −0.16 [−0.41, 0.09] |
| Science/ /Home economics/Agric (STEM) | 1 |
| Mother/female guardian education | |
| Primary/Junior High School | 0.00 [−0.45, 0.45] |
| Senior High School or higher | −0.19 [−0.62, 0.24] |
| No formal education | 1 |
| Father/male guardian education | |
| Primary/Junior High School | 0.32 [−0.12, 0.82] |
| Senior High School or higher | 0.41 [−0.07, 0.89] |
| No formal education | 1 |
| Family and social factors | |
| Ever received sexual health education from parents/guardians | |
| Yes | 0.51 [0.18, 0.84] * |
| No | 1 |
| Ever received sexual health education from friends | |
| Yes | 0.06 [−0.19, 0.32] |
| No | 1 |
| School-based system factors | |
| Ever received sexual health education from teachers | |
| Yes | 0.63 [0.31, 0.94] * |
| No | 1 |
| Provision of sexual health education classes in school | |
| Yes | 0.68 [0.16, 1.20] * |
| No | 1 |
| Administrative location of school | |
| District | −0.15 [−0.47, 0.16] |
| Metropolitan/municipal | 1 |
| Healthcare system factors | |
| Ever received sexual health education by health care provider | |
| Yes | 0.05 [−0.19, 0.29] |
| No | 1 |
| Interactive effects | |
| Provision of sexual health education classes in school × Receive sexual health education from parents/guardians | −0.73 [−1.30, −0.15]* |
Note. ICC = intraclass correlation; STEM = science, technology, engineering and math.
Unadjusted ICC = 0.04; adjusted ICC= 0.01.
Significant.
However, the interactive effect between receiving sexual health education from parents/guardians and the provision of sexual health education classes in schools was statistically significant (p < 0.05). Among students who did not receive sexual health education from their parents/guardians, those from schools that provided sexual health education classes had knowledge scores that were 0.68 points higher compared with students from schools who did not receive sexual health education classes, while the effect of school sexual health education among students who had received sexual health education from their parent/guardian was 0.73 points lower (see Table 3). This means that participants who received sexual health education from schools had higher cervical cancer knowledge scores than those who received sexual health education from parents/guardians (see Figure 1; and Table 3). A complementary interpretation of this interaction effect is that in the absence of school-based health education, parental education can increase knowledge scores. The group that received no education from school or from their parents was worse off in terms of knowledge scores (see bottom left of Figure 1). Using the Wald test, the p value assessed the null hypothesis that the difference in knowledge scores between those who had sexual health education at school does not differ depending on whether they had education at home. The p value was < 0.05, indicating a difference in knowledge scores between those who received sexual health education at school and those who received it from parents.
Figure 1.
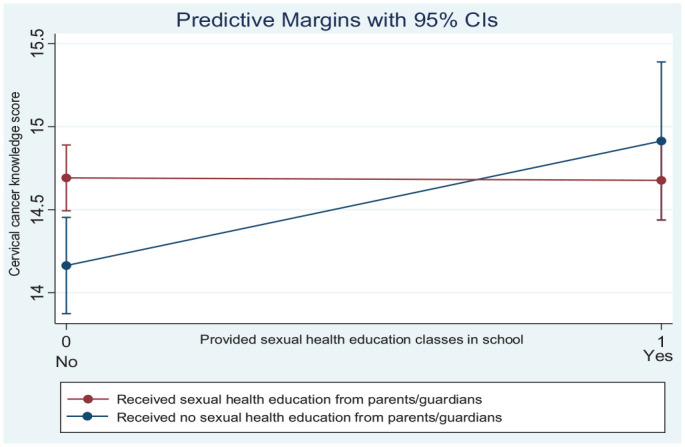
Predictive Margins of the Interactive Effects.
Discussion
This large, cross-sectional multi-site study of female senior high school students in Ghana revealed knowledge gaps about risk factors, as well as primary and secondary prevention of cervical cancer including HPV transmission and prevention. Encouragingly, about two-thirds of students correctly responded to more than half of all knowledge items. More than half of the students correctly answered questions about cervical cancer primary prevention, and HPV infection transmission and prevention. There appeared to be more knowledge about general prevention strategies than specific cervical cancer risk factors, suggesting that students generally understand the prevention of sexually transmitted infections (STIs)-related conditions (incidentally including cervical cancer) but not the specific risk factors for this disease. This is consistent with findings for student samples from other regions of Sub-Saharan Africa (Bardaji et al., 2018; Opoku Agyemang & Manortey, 2018), Asia (Poudel & Sumi, 2019) and Europe (Bowyer et al., 2013).
Less than half of the participants had correct knowledge of the six specific cervical cancer risk factors assessed in this study: having STIs, using oral contraceptives, sexual debut before 18 years, having a family history of cervical cancer, having multiple sexual partners, and smoking cigarettes. While available evidence suggests that these modifiable lifestyle risk factors may increase the risk of cervical cancer, the risk is lower for long-term use of oral contraceptives (>5 years) than for the remaining risk factors (World Health Organization, 2014). Importantly, the effectiveness of oral contraceptives in preventing unplanned and unwanted pregnancies (with consequent prevention of burden associated with these pregnancies) far outweighs the potential risk of cervical cancer (World Health Organization, 2014). While it is important to emphasize cervical cancer risk factors during health education, the risk associated with long-term use of oral contraceptives should be communicated cautiously.
Despite the higher level of knowledge about the prevention of cervical cancer and HPV, most students did not know how cervical cancer screening was conducted or the minimum age for cervical cancer screening. The lack of understanding about the procedure and eligible age for cervical cancer screening may negatively affect screening uptake (Ampofo et al., 2020; Kirubarajan et al., 2021). These findings suggest that risk factors and prevention should be emphasized during cervical cancer education.
Misconceptions about cervical cancer risk factors and prevention strategies were prevalent. The most common of these misconceptions were that students believed activities pertaining to the introduction of foreign substances into the vagina and poor hygienic practices may lead to cervical cancer, and that cervical cancer can be transmitted through blood. These misconceptions have been previously reported by adolescents, men, and women in Africa (Mapanga et al., 2019; Moore & Driver, 2014), the United States (Morales-Campos et al., 2021), and Asia (Poudel & Sumi, 2019). While these activities are unhealthy, they are not risk factors for cervical cancer, and not unexpectedly, the latter misconceptions can lead to stigmatization of people with cervical cancer (Williams & Kenu, 2017).
A striking finding was that a large proportion of the students believed cervical cancer could be prevented by praying to God. With over 80% of the Ghanaian population being religious (including Christians and Muslims; Ghana Statistical Service, 2012), a spiritual dimension to diseases is very common. Most West Africans believe God is a supreme being who prevents diseases (Mwambazambi, 2021), making prayer and faith in God an integral part of disease prevention (Mwambazambi, 2021; Okyerefo & Fiaveh, 2017). This finding emphasizes the need to involve and partner with churches to promote the dissemination of cervical cancer messages.
Students with higher levels of education were likely to have a good understanding of cervical cancer. This can be explained by students in levels two and three having completed modules on sexual and reproductive health (SRH), substance abuse, and other general health conditions, which have been integrated into the Ghanaian senior high school curriculum (i.e., integrated science and social studies). Two main co-curricular programs are also offered as additional programs outside the regular curriculum, either during or after school: the Enhanced School Health Education Program (E-SHEP) of the Ghana Education Service; and the HIV Alert program (Awusabo-Asare et al., 2017). Given the potential benefits of these programs, their scope could be broadened (to include cervical cancer and HPV infection) and introduced early at the basic education level or right at the commencement of SHS, thus adopting a more participatory approach.
Parent and teacher communication about sexual health may play a significant role in improving cervical cancer and HPV infection knowledge. The study revealed that sexual health education provided to students by parents and teachers improved cervical cancer knowledge. Some students were able to translate this information to cervical cancer and HPV infection. This finding is consistent with previous studies that found parent-based sexual health education (Widman et al., 2019), communication about sex (Usonwu et al., 2021), and teacher-based sexual health education (Mathews et al., 2012) improved sexual health knowledge. This finding is not surprising as students spend a substantial amount of time with their teachers. Parents/guardians, on the contrary, play a critical role as socialization agents in communicating sexual health information and shaping adolescent sexual behavior. They often initiate and emphasize sexual heath discussions from a place of fear of unwanted pregnancy and STIs and the stigma of unmarried adolescents, given they have reached puberty (Usonwu et al., 2021). Female adolescents mostly believe sexual health education should be initiated by mothers at home (Shams et al., 2017) and view them as a trustworthy source of information (Awusabo-Asare et al., 2017). Collectively, these findings emphasize the need to provide parents with the skills to confidently start important but sensitive conversations about sex-related topics with their children. Sexual health training and investment in resources (including learning materials) for teachers should also be prioritized to enhance their teaching skills.
Schools and parents play significant roles in improving cervical cancer knowledge. The interaction analysis revealed that among students who have not received sexual health education from parents or guardians, sexual health education received from schools through health classes is associated with higher knowledge scores (compared with having received no sexual health education from schools). However, among students who have not received sexual health education in schools, those who received education at home had higher knowledge scores than those who did not receive education at home. Overall, these findings suggest that receiving sexual health education from either schools or parents increases cervical cancer knowledge among students, compared with not receiving any sexual health education from any source. As advocated by the World Health Organization’s HPS framework, parents should be engaged alongside incorporation and strengthening school-based cervical cancer education into the Ghanaian senior high school curriculum. School-based education improves knowledge about cervical cancer and HPV infection if there are consistent follow-up sessions (Ampofo et al., 2022). However, there is no evidence for the effectiveness of parent-based cervical cancer education, and future studies should explore this potential method. Allocating specific times for school-based SRH education will allow adequate time for students to understand and apply the information received (Awusabo-Asare et al., 2017). In addition, schools should be supported with adequate resources to provide curriculum-based SRH and extra-curricular SRH. In Ghana, schools provide extra-curricular SRH activities whereby health care providers, religious persons and peer educators commonly visit schools to teach SRH education (Awusabo-Asare et al., 2017).
Strengths and Limitations
This is the first study to use a large multisite sample of senior high school students to comprehensively describe the extent of knowledge about cervical cancer and identify individual characteristics, the social environment (e.g., parents and peers), and broader systems (e.g., education and health) influencing knowledge. Nevertheless, there are some limitations. First, the findings of this study were restricted to public senior high school students aged 16 years and above in the Ashanti region, reducing the Generalizability of the results across other school settings in Ghana. As adequate representation of students is important for generalizing study findings, more than 65% of senior high schools are government-managed and admit the highest number of students, and the Ashanti region records the highest number of senior high schools in Ghana (Nyabor, 2017).
Second, knowledge scores may have been under/overestimated given that an author-developed study-specific survey was used because there is no standardized tool to measure cervical cancer prevention knowledge. While the reliability and validity of a measure is essential, efforts were made to develop a robust tool with minimal errors through broad consultation with participants and experts, an integrative review, and an evaluation of psychometric properties. Researchers are encouraged to validate the knowledge scale in other regions in Ghana or similar settings.
Implications for Practice
This study’s findings provide an opportunity to broaden the scope and review the content and strategies for the teaching of sexual health education on cervical cancer in Ghanaian schools. While the content of the curricula in the core subjects is limited in scope, it appears the limited range of topics included in the integrated and social science courses are promising and could provide the basis for cervical cancer education. To reduce students’ knowledge gaps about cervical cancer, the Government of Ghana, Ministry of Education, and the E-SHEP Unit of the Ghana Education Service could introduce cervical cancer education at the primary or junior high school level, provide teachers with in-service training about cervical cancer, and equip them with appropriate resources (such as providing teaching and learning materials and more classroom time). In addition, due to the historic taboo nature of sexuality discussions, teacher communication skills about sex should be enhanced by providing a level of comfort, and empowerment to engage adolescents in interactive discussions (Usonwu et al., 2021). Alternatively, the Ghana Education Service could liaise with the Ghana Health Service to provide health educators to deliver cervical cancer education during health education classes.
Conclusion
Female senior high school students have limited knowledge and some misconceptions about cervical cancer risk factors as well as primary and secondary prevention of cervical cancer. In particular, knowledge gaps about risk factors and secondary prevention were reported. Parents and teachers education about sexual health by parents and teachers, and school-based sexual health education increased cervical cancer knowledge. However, interactive effects indicated that sexual health education received from schools or homes alone may be adequate. Strategies to support and strengthen school- and parent-based programs to provide students with accurate cervical cancer prevention information are needed. Future research should develop and test strategies for effective implementation of cervical cancer prevention programs among female students, particularly those in the lower levels of high school.
Supplemental Material
Supplemental material, sj-docx-1-heb-10.1177_10901981231217978 for Prevalence and Correlates of Cervical Cancer Prevention Knowledge Among High School Students in Ghana by Ama Gyamfua Ampofo, Lisa J Mackenzie, Shadrack Osei Asibey, Christopher Oldmeadow and Allison W Boyes in Health Education & Behavior
Supplemental material, sj-docx-2-heb-10.1177_10901981231217978 for Prevalence and Correlates of Cervical Cancer Prevention Knowledge Among High School Students in Ghana by Ama Gyamfua Ampofo, Lisa J Mackenzie, Shadrack Osei Asibey, Christopher Oldmeadow and Allison W Boyes in Health Education & Behavior
Supplemental material, sj-docx-3-heb-10.1177_10901981231217978 for Prevalence and Correlates of Cervical Cancer Prevention Knowledge Among High School Students in Ghana by Ama Gyamfua Ampofo, Lisa J Mackenzie, Shadrack Osei Asibey, Christopher Oldmeadow and Allison W Boyes in Health Education & Behavior
Acknowledgments
The authors wish to extend their thanks to the teachers and principals at participating schools for their collaboration; the students who completed the questionnaire; and the research assistants who undertook recruitment, data collection and data entry.
Footnotes
Author Contributions: AGA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Funding acquisition, Project administration, Writing—original draft, Writing—review & editing. LJM: Conceptualization, Investigation, Methodology, Funding acquisition, Project administration, Supervision, Validation, Writing—review & editing. SOA: Investigation, Resources, Data curation, Writing—review & editing. CO: Methodology, Supervision, Validation, Writing—review & editing. AWB: Conceptualization, Investigation, Methodology, Funding acquisition, Project administration, Supervision, Validation, Writing—review & editing.
Availability of Data and Material: The data sets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by a University of Newcastle College of Health, Medicine and Wellbeing Strategic Research Pilot Grant. Ama Gyamfua Ampofo is supported by a University of Newcastle Postgraduate Research Scholarship (UNIPRS) and University of Newcastle Research Scholarship Central (UNRSC). Allison Boyes was supported by a National Health & Medical Research Council Early Career Fellowship (APP1073317). Lisa Mackenzie was supported by an Australian National Breast Cancer Foundation Post-Doctoral Fellowship Grant (PF-16-011). This research was supported by infrastructure funding from the University of Newcastle and Hunter Medical Research Institute. The funding sources had no involvement in study design; in the collection; analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Ethics Approval and Consent to Participate: The study was approved by the Human Research Ethics Administration of the University of Newcastle (#H-2020-0378). All procedures were performed in accordance with the ethical standards of the institutional and/or national research committee and as laid down in the 1964 Helsinki declaration and later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants and/or legal guardians of participants to be included in the study.
Consent for Publication: All the authors consent to publish the study.
ORCID iD: Ama Gyamfua Ampofo  https://orcid.org/0000-0003-3730-6313
https://orcid.org/0000-0003-3730-6313
Supplemental Material: Supplemental material for this article is available online.
References
- Ampofo A. G., Adumatta A. D., Owusu E., Awuviry-Newton K. (2020). A cross-sectional study of barriers to cervical cancer screening uptake in Ghana: An application of the health belief model. PLOS ONE, 15(4), e0231459. 10.1371/journal.pone.0231459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ampofo A. G., Boyes A. W., Asibey S. O., Oldmeadow C., Mackenzie L. J. (2023). Prevalence and correlates of modifiable risk factors for cervical cancer and HPV infection among senior high school students in Ghana: A latent class analysis. BMC Public Health, 23(1), 340. 10.1186/s12889-022-14908-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ampofo A. G., Boyes A. W., Khumalo P. G., Mackenzie L. (2022). Improving knowledge, attitudes, and uptake of cervical cancer prevention among female students: A systematic review and meta-analysis of school-based health education. Gynecologic Oncology, 164(3), 675–690. 10.1016/j.ygyno.2021.12.021 [DOI] [PubMed] [Google Scholar]
- Awua A. K., Sackey S. T., Osei Y. D., Asmah R. H., Wiredu E. K. (2016). Prevalence of human papillomavirus genotypes among women with cervical cancer in Ghana. Infectious Agents and Cancer, 11(1), 4. 10.1186/s13027-016-0050-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awusabo-Asare K., Stillman M., Keogh S., Doku D. T., Kumi-Kyereme A., Esia-Donkoh K., Bankole A. (2017). From paper to practice: Sexuality education policies and their implementation in Ghana. Guttmacher Institute. https://www.guttmacher.org/report/sexuality-education-ghana [Google Scholar]
- Ayissi C. A., Wamai R. G., Oduwo G. O., Perlman S., Welty E., Welty T., Ogembo J. G. (2012). Awareness, acceptability and uptake of human papilloma virus vaccine among Cameroonian school-attending female adolescents. Journal of Community Health, 37(6), 1127–1135. 10.1007/s10900-012-9554-z [DOI] [PubMed] [Google Scholar]
- Bardaji A., Mindu C., Augusto O. J., Casellas A., Cambaco O., Simbine E., Munguambe K. (2018). Awareness of cervical cancer and willingness to be vaccinated against human papillomavirus in Mozambican adolescent girls. Papillomavirus Research, 5, 156–162. 10.1016/j.pvr.2018.04.004 [DOI] [PMC free article] [PubMed]
- Binka C., Nyarko S. H., Doku D. T. (2016). Cervical cancer knowledge, perceptions and screening behaviour among female university students in Ghana. Journal of Cancer Education, 31(2), 322–327. [DOI] [PubMed] [Google Scholar]
- Bland M. (2015). An introduction to medical statistics. Oxford University Press. [Google Scholar]
- Bowyer H. L., Marlow L. A., Hibbitts S., Pollock K. G., Waller J. (2013). Knowledge and awareness of HPV and the HPV vaccine among young women in the first routinely vaccinated cohort in England. Vaccine, 31(7), 1051–1056. 10.1016/j.vaccine.2012.12.038 [DOI] [PubMed] [Google Scholar]
- Bruni L., Albero G., Serrano B., Mena M., Collado J., Gómez D., de Sanjosé S. (2022). Human Papillomavirus and related diseases in Ghana. Summary report. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre; ). [Google Scholar]
- Chidyaonga-Maseko F., Chirwa M. L., Muula A. S. (2015). Underutilization of cervical cancer prevention services in low and middle income countries: A review of contributing factors. Pan African Medical Journal, 21(1), 231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donkoh E. T., Asmah R. H., Agyemang-Yeboah F., Dabo E. O., Wiredu E. K. (2022). Prevalence and distribution of vaccine-preventable genital human Papillomavirus (Hpv) genotypes in Ghanaian women presenting for screening. Cancer Control, 29, 10732748221094721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunyo P., Effah K., Udofia E. A. (2018). Factors associated with late presentation of cervical cancer cases at a district hospital: A retrospective study. BMC Public Health, 18(1), 1156–1156. 10.1186/s12889-018-6065-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebu N. I., Mupepi S. C., Siakwa M. P., Sampselle C. M. (2014). Knowledge, practice, and barriers toward cervical cancer screening in Elmina, Southern Ghana. International Journal of Women’s Health, 7, 31–39. 10.2147/IJWH.S71797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleary S. A., Joseph P., Pappagianopoulos J. E. (2018). Adolescent health literacy and health behaviors: A systematic review. Journal of Adolescence, 62, 116–127. 10.1016/j.adolescence.2017.11.010 [DOI] [PubMed] [Google Scholar]
- Gagnier J. J., Lai J., Mokkink L. B., Terwee C. B. (2021). COSMIN reporting guideline for studies on measurement properties of patient-reported outcome measures. Quality of Life Research, 30(8), 2197–2218. 10.1007/s11136-021-02822-4 [DOI] [PubMed] [Google Scholar]
- Ghana Statistical Service. (2012). Population and housing census report, 2010. Sakoa Press. [Google Scholar]
- Glanz K., Rimer B. K., Viswanath K. (2008). Health behavior and health education: Theory, research, and practice. John Wiley & Sons. [Google Scholar]
- Gyamfua A. A., Nkrumah I., Ibitoye B. M., Agyemang B. A., Ofosu E. S., Tsoka-Gwegweni J. M., Cumber S. N. (2019). The level of knowledge and associated socio-demographic factors on cervical cancer among women: A cross-sectional study at Kenyase Bosore community, Ghana. The Pan African Medical Journal, 34, 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ifediora C. O., Azuike E. C. (2018). Knowledge and attitudes about cervical cancer and its prevention among female secondary school students in Nigeria. Tropical Medicine & International Health, 23(7), 714–723. 10.1111/tmi.13070 [DOI] [PubMed] [Google Scholar]
- Kilfoyle K. A., Vitko M., O’Conor R., Bailey S. C. (2016). Health literacy and women’s reproductive health: A systematic review. Journal of Women’s Health, 25(12), 1237–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K., Han H.-R. (2016). Potential links between health literacy and cervical cancer screening behaviors: A systematic review. Psycho-Oncology, 25(2), 122–130. 10.1002/pon.3883 [DOI] [PubMed] [Google Scholar]
- Kirubarajan A., Leung S., Li X., Yau M., Sobel M. (2021). Barriers and facilitators for cervical cancer screening among adolescents and young people: A systematic review. BMC Women’s Health, 21(1), 122. 10.1186/s12905-021-01264-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krings A., Dunyo P., Pesic A., Tetteh S., Hansen B., Gedzah I., Kaufmann A. M. (2019). Characterization of Human Papillomavirus prevalence and risk factors to guide cervical cancer screening in the North Tongu District, Ghana. PLOS ONE, 14(6), e0218762. 10.1371/journal.pone.0218762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langford R., Bonell C., Komro K., Murphy S., Magnus D., Waters E., Campbell R. (2016). The health promoting schools framework: Known unknowns and an agenda for future research. Health Education & Behavior, 44(3), 463–475. 10.1177/1090198116673800 [DOI] [PubMed] [Google Scholar]
- Lee A., Ho M., Cheung C. K. M., Keung V. M. W. (2014). Factors influencing adolescent girls’ decision in initiation for human papillomavirus vaccination: A cross-sectional study in Hong Kong. BMC Public Health, 14(1), 925. 10.1186/1471-2458-14-925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Li L.-K., Ma J.-F., Wei L.-H., Niyazi M., Li C.-Q., Belinson J. (2009). Knowledge and attitudes about human papillomavirus (HPV) and HPV vaccines among women living in metropolitan and rural regions of China. Vaccine, 27(8), 1210–1215. [DOI] [PubMed] [Google Scholar]
- Lynn M. R. (1986). Determination and quantification of content validity. Nursing Research, 35(6), 382–386. [PubMed] [Google Scholar]
- Manganello J. A. (2007). Health literacy and adolescents: A framework and agenda for future research. Health Education Research, 23(5), 840–847. [DOI] [PubMed] [Google Scholar]
- Mapanga W., Girdler-Brown B., Singh E. (2019). Knowledge, attitudes and practices of young people in Zimbabwe on cervical cancer and HPV, current screening methods and vaccination. BMC Cancer, 19(1), 845–845. 10.1186/s12885-019-6060-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martianus R., Putri R. C., Satyarsa A. B. S., Brahmantya Y. B., Abdulhadi A. F. (2018). Correlation between knowledge and attitudes of female high school students regarding cervical cancer in Denpasar, Bali. Annals of Oncology, 29, 5. 10.1093/annonc/mdy436.005 [DOI] [Google Scholar]
- Mathews C., Aarø L., Grimsrud A., Flisher A., Kaaya S., Onya H., Klepp K.-I. (2012). Effects of the SATZ teacher-led school HIV prevention programmes on adolescent sexual behaviour: Cluster randomised controlled trials in three sub-Saharan African sites. International Health, 4(2), 111–122. [DOI] [PubMed] [Google Scholar]
- Montaño D. E., Kasprzyk D. (2015). Health behavior: Theory, research and practice (5th ed. Vol. 70). SAGE. [Google Scholar]
- Moore A. R., Driver N. (2014). Knowledge of cervical cancer risk factors among educated women in Lomé, Togo: Half-truths and misconceptions. Sage Open, 4(4), 2158244014557041. [Google Scholar]
- Morales-Campos D. Y., Snipes S., Villarreal E. K., Crocker L., Guerrero A., Fernandez M. (2021). Cervical cancer, human papillomavirus (HPV), and HPV vaccination: Exploring gendered perspectives, knowledge, attitudes, and cultural taboos among Mexican American adults. Ethnicity & Health, 26(2), 206–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwambazambi K. (2021). A West African perspective on god and disease. All creation groans: Toward a theology of disease and global health, 141. https://journal.cjgh.org/index.php/cjgh/article/view/589
- Nartey Y., Hill P. C., Amo-Antwi K., Nyarko K. M., Yarney J., Cox B. (2016). Cervical cancer in the greater Accra and Ashanti Regions of Ghana. Journal of Global Oncology, 3(6), 782–790. 10.1200/JGO.2016.005744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyabor J. (2017). Regional distribution of Senior High Schools in Ghana. https://citifmonline.com/2017/09/regional-distribution-of-senior-high-schools-in-ghana-infographic/
- Okyerefo M. P. K., Fiaveh D. Y. (2017). Prayer and health-seeking beliefs in Ghana: Understanding the “religious space” of the urban forest. Health Sociology Review, 26(3), 308–320. 10.1080/14461242.2016.1257360 [DOI] [Google Scholar]
- Opoku Agyemang D., Manortey S. (2018). Awareness and knowledge of cervical cancer among female senior high school students in Lower Manya Krobo Municipal in Ghana. Journal of Scientific Research and Reports, 19, 1–11. 10.9734/JSRR/2018/41116 [DOI] [Google Scholar]
- Poudel K., Sumi N. (2019). Analyzing Awareness on Risk Factors, Barriers and prevention of cervical cancer among Pairs of Nepali high school students and their mothers. International Journal of Environmental Research and Public Health, 16(22). 10.3390/ijerph16224382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashwan H., Ishak I., Sawalludin N. (2013). Knowledge and views of secondary school students in Kuala Lumpur on cervical cancer and its prevention. Asian Pacific Journal of Cancer Prevention, 14(4), 2545–2549. 10.7314/apjcp.2013.14.4.2545 [DOI] [PubMed] [Google Scholar]
- Rugutt K. A. (2014). Barriers to early diagnosis of invasive cervical cancer among patients receiving treatment at Kenyatta National Hospital: Kenyatta University [Unpublished Master’s thesis], Nairobi, Kenya. [Google Scholar]
- Sani A. S., Abraham C., Denford S., Ball S. (2016). School-based sexual health education interventions to prevent STI/HIV in sub-Saharan Africa: A systematic review and meta-analysis. BMC Public Health, 16(1), 1–26. doi.org/10.1186/s12889-016-3715-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shams M., Parhizkar S., a Mousavizadeh A., Majdpour M. (2017). Mothers’ views about sexual health education for their adolescent daughters: A qualitative study. Reproductive Health, 14(1), 24. 10.1186/s12978-017-0291-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streiner D. L., Norman G. R., Cairney J. (2015). Health measurement scales: A practical guide to their development and use. Oxford University Press. [Google Scholar]
- Sun W. H., Miu H. Y. H., Wong C. K. H., Tucker J. D., Wong W. C. W. (2018). Assessing participation and effectiveness of the peer-led approach in youth sexual health education: Systematic review and meta-analysis in more developed Countries. The Journal of Sex Research, 55(1), 31–44. 10.1080/00224499.2016.1247779 [DOI] [PubMed] [Google Scholar]
- Sung H., Ferlay J., Siegel R. L., Laversanne M., Soerjomataram I., Jemal A., Bray F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209–249. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- Usonwu I., Ahmad R., Curtis-Tyler K. (2021). Parent–adolescent communication on adolescent sexual and reproductive health in sub-Saharan Africa: A qualitative review and thematic synthesis. Reproductive Health, 18(1), 202. 10.1186/s12978-021-01246-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widman L., Evans R., Javidi H., Choukas-Bradley S. (2019). Assessment of parent-based interventions for adolescent sexual health: A systematic review and meta-analysis. JAMA Pediatrics, 173(9), 866–877. 10.1001/jamapediatrics.2019.2324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams M., Amoateng P. (2012). Knowledge and beliefs about cervical cancer screening among men in Kumasi, Ghana. Ghana Medical Journal, 46(3), 147. [PMC free article] [PubMed] [Google Scholar]
- Williams M. S., Kenu E. (2017). Abstract B25: Sometimes it’s spiritual: A mixed-methods study of cervical cancer stigma among women in Ghana, West Africa. Cancer Research, 77(22 Suppl.), B25–B25. 10.1158/1538-7445.NEWFRONT17-B25 [DOI] [Google Scholar]
- World Health Organization. (1997). Promoting health through schools: Report of a WHO Expert Committee on Comprehensive School Health Education and Promotion. [PubMed] [Google Scholar]
- World Health Organization. (2014). Comprehensive Cervical Cancer Control A guide to essential practice (2nd ed., pp. 23–190). [PubMed] [Google Scholar]
- World Health Organization. (2021). Health promotion glossary of terms. [Google Scholar]
- Zurales K. R., Appiah-Kubi A., Bell S. G., Konney T., Tawiah A., Kobernik E. K., Lawrence E. R. (2023). Attitudes and knowledge about HPV vaccination among Ghanaian women with cervical cancer. Reproductive, Female and Child Health, 2(1), 11–18. 10.1002/rfc2.24 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-heb-10.1177_10901981231217978 for Prevalence and Correlates of Cervical Cancer Prevention Knowledge Among High School Students in Ghana by Ama Gyamfua Ampofo, Lisa J Mackenzie, Shadrack Osei Asibey, Christopher Oldmeadow and Allison W Boyes in Health Education & Behavior
Supplemental material, sj-docx-2-heb-10.1177_10901981231217978 for Prevalence and Correlates of Cervical Cancer Prevention Knowledge Among High School Students in Ghana by Ama Gyamfua Ampofo, Lisa J Mackenzie, Shadrack Osei Asibey, Christopher Oldmeadow and Allison W Boyes in Health Education & Behavior
Supplemental material, sj-docx-3-heb-10.1177_10901981231217978 for Prevalence and Correlates of Cervical Cancer Prevention Knowledge Among High School Students in Ghana by Ama Gyamfua Ampofo, Lisa J Mackenzie, Shadrack Osei Asibey, Christopher Oldmeadow and Allison W Boyes in Health Education & Behavior


