Abstract
Household food insecurity (HFI) during childhood is associated with poor dietary diversity and malnutrition, placing children's growth at risk. Children with growth disorders, such as stunting, are more likely to have poor cognition and educational performance, lower economic status, and an increased risk of nutrition‐related chronic diseases in adulthood. Our study aimed to systematically review and conduct a meta‐analysis of cohort studies investigating the association between HFI and stunting in children aged 0−59 months. Peer‐reviewed and grey literature were systematically searched in electronic databases with no language or date restrictions. Two reviewers independently assessed the studies for pre‐established eligibility criteria. Data were extracted using a standard protocol. Random‐effects meta‐analysis models were used, and I 2 > 40% indicated high heterogeneity across studies. We used the Grading of Recommendations Assessment, Development, and Evaluation system to assess the quality of the evidence. Nine cohort studies comprising 46,300 children were included. Approximately 80% (n = 7) of the studies found a positive association between HFI and stunting. Pooled odds ratio was 1.00 (95% confidence interval [CI]: 0.87−1.14; I 2: 76.14%). The pooled hazard ratio between moderate and severe HFI and stunting was 1.02 (95% CI: 0.84−1.22; I 2: 85.96%). Due to high heterogeneity, the quality of evidence was very low. Individual studies showed an association between HFI and stunting in children aged 0–59 months; however, this association was not sustained in the pooled analysis, possibly because of high heterogeneity across studies.
Keywords: child preschool, growth, household food insecurity, infant, meta‐analysis, stunting
Individual studies showed an association between Household food insecurity (HFI) and stunting in children aged 0–59 months. This association was not sustained in the pooled analysis. Based on scientific evidence in the literature to date, other factors contribute to delayed linear growth.
Key messages
Household food insecurity (HFI) was associated with stunting in children aged 0–59 months; however this association was not observed in a pooled analysis.
Based on the scientific evidence in the literature to date, HFI alone does not explain growth problems in the 0–59 months age group.
Because other factors were found to be associated with delayed linear growth in light of the available evidence, it is recommended that another systematic review be conducted to expand this investigation.
There is a need for continued and effective monitoring of factors affecting child growth.
1. INTRODUCTION
Childhood, particularly the first 2 years of life, provides opportunities for growth and development. Human growth is defined as a dynamic and continuous process, involving physical enlargement of the body, which is related to a gradual increase in the number and size of cells. Growth patterns vary throughout life (Black et al., 2022). During the first 2 years of life, growth is intense, and adequate food and nutrition during this period are the basis for child survival, growth, and development. Therefore, adverse childhood experiences, such as poverty and food insecurity, are risk factors for suboptimal growth (Inzaghi et al., 2022; Schwarzenberg et al., 2018).
Intrinsic (genetic) and extrinsic (environmental) factors, such as insufficient or inadequate food access and consumption, general care and hygiene, housing conditions, and basic sanitation, influence child growth (Schwarzenberg et al., 2018). Faltering growth contributes to higher rates of infant morbidity and mortality, predisposing children to various diseases during adulthood, including non‐communicable diet‐related diseases, such as obesity and other cardiometabolic diseases; this negatively interferes with cognitive, motor, and social development (de Oliveira et al., 2020; UNICEF/WHO/WORLD BANK, 2021). Therefore, linear growth is an important indicator of a child's overall health and should be monitored continuously (Inzaghi et al., 2022).
Recent scientific evidence suggests that linear growth in childhood can have lifelong consequences and can be associated with HFI (Gallegos et al., 2021; Mistry et al., 2019). HFI is defined as a lack of physical, social, and economic access to sufficient, safe, and nutritious food that meets the dietary needs and food preferences for an active and healthy life (FAO, IFAD, UNICEF, WFP, & WHO, 2022). According to ‘The State of Food and Nutrition Security in the World 2022’ report, 828 million individuals were hungry globally (approximately 9.8% of the world's population), and 2.3 billion individuals (29.3% of the world's population) experienced moderate or severe HFI (FAO, IFAD, UNICEF, WFP, & WHO, 2022).
Children with HFI are more likely to be stunted, wasted, and underweight than those in food security households (Hasan et al., 2022). Globally, approximately 148.1 million children <5 years were reported to be stunted, which corresponds to 22% of this population, and a further 6.8% (45.4 million) children aged <5 years were wasted in 2020. The highest prevalence of short stature in children is in Asia (52%) and Africa (43%) (World Health Organization, 2023). Given the health and economic consequences of HFI on early childhood development, understanding the relationship between HFI and child nutrition is critical.
A systematic review (Lye et al., 2023) that included 36 studies found that HFI is significantly associated with undernutrition, especially stunting and underweight; however, no meta‐analysis was performed. Moreover, the authors did not assess the certainty of the evidence for each exposure–outcome association, restricted the publication period between 2012 and 2022, and limited the search to English‐language studies, and most studies included were cross‐sectional studies. New reviews in this area should take a more comprehensive approach, such as not limiting the publication date and language, which allows for capturing the whole body of evidence. Specifically, it is important to investigate group‐based trajectory models to understand the changes that occur in responses over time and to compare them between individuals (Fitzmaurice et al., 2012). Cohort studies are recommended because this design allows the observation of repeated measures in similar groups of individuals over time, observation of individual changes, and consideration of time for the development of the outcome of interest, thereby establishing a causal relationship (Laird, 2022). Therefore, we aimed to systematically review cohort studies to investigate the relationship between HFI and stunting in children aged 0–59 months.
2. METHODS
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) for reporting systematic reviews (Page et al., 2021). The study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO; number CRD42022353737). The Population, Exposure, Comparison, Outcome, and Study design was used to elaborate the guiding study question as follows: ‘Is HFI associated with stunting in children aged 0–59 months?’
2.1. Eligibility criteria
Cohort designs (prospective and retrospective) that reported a measure of association (relative risk [RR], odds ratio [OR], hazard ratio [HR], or coefficients with confidence intervals [CI]) between HFI and stunting in children up to 59 months of age were included. Studies were not eligible if they were as follows: (a) letters to editors, reviews, personal opinions, book chapters, commentaries, editorials, or any publication without primary data; (b) animal studies; (c) children with comorbidities that affect growth; and (d) studies that evaluated developmental outcomes, such as cognitive abilities, language, motor, socioemotional, and social interactions.
2.2. Exposure
The key exposure was the HFI, which was measured according to the results reported by studies using their assessment instruments. When studies reported different levels of HFI, a meta‐analysis was performed for each study using a fixed‐effects inverse‐variance model so that it could be included in the statistical combination of individual results.
2.3. Outcome
Stunting was measured using z‐scores, according to sex and age at the time of the measurement, calculated for length‐for‐age z‐score (LAZ) for infants between 0 and 24 months, and height‐for‐age (HAZ) for toddlers between 2 and 5 years, according to the World Health Organization (WHO) Child Growth Standards (WHO Child Growth Standards, 2006). Children with LAZ or HAZ score below −2 standard deviation (SD) were considered stunted. Children with LAZ or HAZ scores ≥ −2SD were considered to have adequate growth (WHO Child Growth Standards, 2006). Furthermore, the length‐for‐age and stature‐for‐age, fifth percentile, and tenth percentile were considered based on the Center for Disease Control age‐sex specific growth standards (Kuczmarski et al., 2002).
2.4. Search strategy
A systematic literature search was performed on August 25, 2022, and updated on May 12, 2023, using the Medline, Embase, Scopus, Web of Science, and Lilacs (BVS) databases. Furthermore, a gray literature search was performed using ProQuest Dissertations and Theses Global and Google Scholar (limited to the first 200 most relevant results in the first search and first 100 in the update) (Biete et al., 2023; Paula et al., 2022). Reference lists of selected articles were manually searched to identify additional relevant publications. The search strategy comprised free‐text words and identified terms in medical subject headings and health science descriptors for participants, exposure, and outcomes. The following terms were used in combination using boolean operators, such as ‘OR’ or ‘AND’: (‘Infant’ OR ‘Child’ OR ‘Children’ OR ‘child preschool’ OR ‘Preschool Child’ OR ‘children preschool’ OR ‘Preschool Children’ OR ‘infant newborn’ OR ‘infants newborn’ OR ‘Newborn Infant’ OR ‘Newborn Infants’ OR ‘Newborns’ OR ‘Newborn’ OR ‘Neonate’ OR ‘Neonates’ OR ‘Toddler’ OR ‘boy’ OR ‘girl’) AND (‘Food Insecurity’ OR ‘Food Insecurities’ OR ‘insecurity food’ OR ‘Food Rationing’ OR ‘rationing food’ OR ‘nutrition insecurity’ OR ‘Food and nutrition insecurity’ OR ‘household food insecurity’ OR ‘Food and Nutrition Security’ OR ‘Food Supply’ OR ‘Food Supplies’ OR ‘supplies food’ OR ‘supply food’ OR ‘Food Security’ OR ‘security food’ OR ‘Food Insecurity Scale’ OR ‘Household Food Insecurity Measurement Scale’) AND (‘Growth Charts’ OR ‘chart growth’ OR ‘charts growth’ OR ‘Growth’ OR ‘Child undernutrition’ OR ‘infant undernutrition’ OR ‘Growth and Development’ OR ‘Development and Growth’ OR ‘Postnatal growth’ OR ‘Postnatal development’ OR ‘Growth Disorders’ OR ‘disorder growth’ OR ‘Growth Disorder’ OR ‘Stunting’ ‘Stunted Growth’ OR ‘growth stunted’ OR ‘Physical Development’ OR ‘Nutritional Status’ OR ‘status nutritional’ OR ‘Child Nutrition Disorders’ OR ‘Child Nutrition Disorder’ OR ‘Child Malnutrition’ OR ‘malnutrition child’ OR ‘Malnutrition in Children’ OR ‘Infant Malnutrition’ OR ‘Malnutrition in Infant’ OR ‘Malnutrition in Infants’ OR ‘malnutrition infant’ OR ‘Infantile Malnutrition’ OR ‘malnutrition infantile’ OR ‘Malnutrition’ OR ‘Nutritional Deficiency’ OR ‘Nutritional Deficiencies’ OR ‘Undernutrition’ OR ‘Malnourishment’).
The quality of the search strategy was assessed by an investigator with experience in systematic reviews and expertise in child nutrition, following the Peer Review of Electronic Search Strategies checklist (McGowana et al., 2016). The full search strategy for each database is presented in Table S1.
2.5. Study selection
The review selection process was independently conducted by two reviewers in two steps. First, the titles and abstracts of all retrieved articles were screened, according to the eligibility criteria. Potentially eligible studies were submitted for a full‐text analysis. Articles that met the eligibility criteria were included in this review. Any disagreements were resolved by consensus. Duplicates were identified and removed using the Mendeley Desktop Reference Management Tool (version 1.19.8). The Rayyan QCRI software (Qatar Computing Research Institute®) was used for the screening of articles.
2.6. Data extraction
For data extraction, the two reviewers independently extracted data using a standard predefined protocol, including authors, year of publication, data collection year, follow‐up time, study design, country in which the study was conducted, sample size, age of participants, criteria for stunting, method for assessing the degree and prevalence of HFI, measures of effect size with CI, details of adjustment for confounding factors, and study funding/support information. When multiple estimates were reported, the results adjusted for the highest number of confounders were used. The authors were contacted to retrieve additional information when necessary. At least two attempts were made to request for missing or additional information.
2.7. Risk of bias assessment of individual studies
The two investigators independently assessed the methodological quality of each included study using the Joanna Briggs Institute Critical Appraisal Checklist for Cohort Studies (Moola et al., 2020). The tool consists of questions answered as ‘yes’, ‘no’, ‘unclear’, or ‘not applicable’. In this study, the risk of bias was considered low when all items were answered ‘yes’ or ‘not applicable’. If the response to any item was ‘no’ or ‘unclear’, a high risk of bias was expected. Any disagreements were resolved by consensus. An analysis of the relative frequency of each investigated domain was presented, and no scores were assigned.
2.8. Data analysis
2.8.1. Descriptive analysis
Description of the characteristics of the included studies, such as type of study, sample size, age, and key findings (severity, prevalence, and association between HFI and growth). Regarding country classification by income level, the countries in which the studies were conducted were classified as high‐income countries, upper‐middle‐income countries, low‐ and middle‐income countries (LMICs), or low‐income countries (LICs), according to the World Bank Open Data (The World Bank, 2023).
2.8.2. Effect size
The primary outcome was the association between HFI and stunting, along with their respective 95% CI. Based on data availability, RR, OR, HR, and coefficients with their respective 95% CI were measured for stunting outcomes. If studies reported a measure of the coefficient beta (β) of the regression, it was converted to OR and HR using the proposed methods of Zhang and Yu (1998).
2.8.3. Meta‐analysis
Meta‐analysis was conducted when at least three studies reported data that could be included in the statistical combination of results. No studies were included in the meta‐analysis in which the OR or HR could not be calculated using the available data. Owing to the studies with different measures of association, such as OR and HR, a meta‐analysis was performed to summarize the results of mild and moderate HFI exposure presented in studies with OR and beta measures. Additionally, and another meta‐analysis was performed to summarize the results of moderate and severe HFI exposure presented in studies with HR and beta measures. Overall associations were analyzed using the DerSimonian and Laird random‐effect models. Statistical heterogeneity between studies was measured using I‐square (I 2). Heterogeneity was considered important if I 2 values were >40% (Deeks et al., 2021). Publication bias and meta‐regression analyses were not conducted because a minimum of 10 studies were not available for the measure (Deeks et al., 2021). Data analysis was performed using the Stata software (StataCorp. 2019. Stata Statistical Software: Release 16.1.; StataCorp, LLC).
2.9. Quality of meta‐evidence
The Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system was used to evaluate the certainty of the evidence for each exposure–outcome association based on the major domains of study limitations. The quality of the evidence was downgraded based on five criteria: risk of bias, inconsistency of results, indirectness of evidence, imprecision, and publication bias when it was assessed (Schünemann et al., 2013).
3. RESULTS
3.1. Characteristics of studies
A PRISMA flowchart of the study selection process is shown in (Figure 1). A database search retrieved 8791 articles. After removing duplicates, 4339 articles and abstracts were screened. Of these, 20 full‐text articles were further assessed for eligibility. Finally, nine studies (Belayneh et al., 2020; Cook et al., 2006; Harper et al., 2023; Kabalo & Lindtjørn, 2022; Koyratty et al., 2022; Mutisya et al., 2015; Na et al., 2020; Namirembe et al., 2022; Oduro et al., 2022) met the inclusion criteria and were included in this systematic review. A complete list of the reasons for the exclusion of articles is presented in Table S2.
Figure 1.
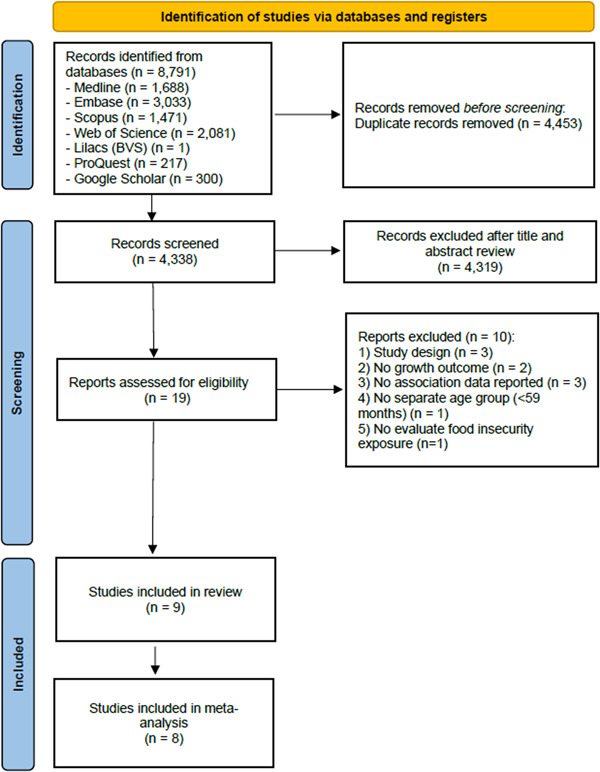
Flowchart of the study selection process. Adapted from PRISMA. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta‐Analyses.
The articles were published between 2006 (Cook et al., 2006) and 2022 (Harper et al., 2023; Kabalo & Lindtjørn, 2022; Koyratty et al., 2022; Namirembe et al., 2022; Oduro et al., 2022). The included studies were conducted in Africa (Belayneh et al., 2020; Harper et al., 2023; Kabalo & Lindtjørn, 2022; Koyratty et al., 2022; Mutisya et al., 2015; Namirembe et al., 2022; Oduro et al., 2022), America (Cook et al., 2006), and Asia (Harper et al., 2023). The sample size ranged from 692 (Oduro et al., 2022) to 17,130 (Cook et al., 2006), with a total of 46,300 children evaluated. The ages of the children ranged from 0 (Harper et al., 2023; Koyratty et al., 2022; Mutisya et al., 2015; Oduro et al., 2022) to 55 months (Harper et al., 2023). Four studies were conducted in the LMICs (Koyratty et al., 2022; Mutisya et al., 2015; Na et al., 2020; Oduro et al., 2022), three in the LICs (Belayneh et al., 2020; Kabalo & Lindtjørn, 2022; Namirembe et al., 2022), one in upper‐middle‐income country (Harper et al., 2023), and one in high‐income countries (Cook et al., 2006).
Five studies were conducted in rural areas (Belayneh et al., 2020; Kabalo & Lindtjørn, 2022; Koyratty et al., 2022; Na et al., 2020; Namirembe et al., 2022), three in urban areas (Cook et al., 2006; Mutisya et al., 2015; Oduro et al., 2022), and one in a traditional area (communally owned land under the jurisdiction of traditional leaders. Settlements within these areas included villages, urban areas, and rural areas (Harper et al., 2023).
3.2. HFI across studies
The prevalence of HFI ranged between 15.4% (Belayneh et al., 2020) and 100% (Koyratty et al., 2022), with a higher prevalence in African countries. Regarding exposure to HFI, one cohort used the Multidimensional Family Feeding Insecurity Tools developed specifically for rural households in Zimbabwe, including three dimensions: poor food access, household shocks, and low food availability and quality (Koyratty et al., 2022). Two cohorts used nine Household Food Insecurity Access Scale (HFIAS) items, validated for Ethiopia (Belayneh et al., 2020; Kabalo & Lindtjørn, 2022). This tool is adapted to estimate seasonal variations in food insecurity and assesses four levels of food insecurity: food secure, mild food insecurity, moderate food insecurity, and severe food insecurity. One cohort used an 18‐item food security measure referred to as the Family Food Safety Research (HFSS) module (Cook et al., 2006).
Namirembe et al. (2022) used the HFIAS to measure food access published by the US Agency for International Development through the Food and Nutrition Technical Assistance III Project. Through the households' responses, the categorization of household food insecurity (HFI) (access) was assessed on four levels: food secure, mildly food insecure, moderately food insecure, or severely food insecure. Na et al. (2020) examined food security, mild food insecurity, moderate food insecurity, and severe food insecurity using the 9‐item Food Access Survey Tool developed and tested by the Food and Nutrition Technical Assistance Project in Bangladesh. Mutisya et al. (2015) evaluated the severity of the three levels of HFI severity using a Radimer framework. One cohort did not include a validated measure of food security (Harper et al., 2023), and another did not report which tool was used in the evaluation (Oduro et al., 2022).
3.3. Description of the relationship between stunting and HFI
A summary of the characteristics and main results of each study is presented in Table 1. The overall prevalence of stunting ranged between 32.1% (Kabalo & Lindtjørn, 2022) and 79% (Namirembe et al., 2022).
Table 1.
Summary of included studies characteristics.
| Author, year country | Year of data collection | Study design | Subjects (n) | Age (months) | Prevalence of HFI | Prevalence of outcome | Main results | |
|---|---|---|---|---|---|---|---|---|
| (Belayneh et al., 2020) Ethiopia | March to December 2017 | Prospective cohort | 935 | 6−47 months |
Food secure: 3.2%; Food insecurity mild: 3.8%; Food insecurity moderate: 5.0%; Food insecurity severe: 6.6% |
Stunting: 43% |
Food insecurity severe: Ref Food security associated with stunting: (aOR: 1.28; 95% CI: 0.72−2.26) Food security mild associated with stunting: (aOR: 1.35; 95% CI: 0.78−2.35) Food insecurity moderate associated with stunting: (aOR: 1.01; 95% CI: 0.71−1.45) |
|
| (Cook et al. 2006) United States (US) | 1998 to 2004 | Prospective cohort | 17,130 | ≤36 months |
Food Secure: 78%; HFI: 10%; H& CFI:12%. |
Children with risk for growth problems: 44% |
HFI: (aOR, TANF controlled: 1.09; 95% CI: 0.93−1.28) (aOR, FSP controlled: 1.10; 95% CI: 0.94−1.30) H&CFI: (aOR, TANF controlled: 1.02; 95% CI: 0.88−1.19) (aOR, FSP controlled: 1.02; 95% CI: 0.87−1.19) |
|
| (Harper et al. 2023) South Africaa | 2008 to 2012 | Prospective cohort | 1391 | Birth to 55 months | Food poverty line (R274) (equivalent to 42.16 USD): 81.2% |
Stunted: 17.8%; Severely stunted: 14.4% |
Food poverty line (R274) and stunting: (aRR: 2.31; 95% CI: 1.27−4.22; p = 0.006) Food poverty line (R274) and severe stunting: (aRR: 1.21; 95% CI: 0.69−2.12; p = 0.498) |
|
| (Kabalo & Lindtjørn, 2022) Ethiopia | June 2017 to June 2018 | Prospective cohort | 907 | Mean: 33.4 (SD: 11.7) months | HFI: 74.2% | Stunting: 32.1% | Household food insecurity associated with stunting: (β = 0.063; 95% CI: −0.066 to 0.192) | |
| (Koyratty et al., 2022) Zimbabwean | November 2012 to March 2015 | Retrospective cohort | 1166 | 1 at 18 months | HFI: 100% | Stunting: 35.6% | From M1 to M18 (β = −0.09; 95% CI: −0.17 to 0.01) | |
| (Mutisya et al., 2015) Kenya | 2006 to 2012 | Prospective cohort | 6858 | Between 6 and 23 months |
Food secure: 28%; Moderate food insecure: 50%; Severely food insecure: 22%. |
Stunting: 49% |
Food secure: 1 (reference) Moderate food insecure: (HR: 1.12; 95% CI: 1.02−1.22) Severely food insecure: (HR: 1.15; 95% CI: 1.02−1.22) |
|
| (Na et al., 2020) Bangladesh | Not reported | Prospective cohort | 12,693 | Birth at 6 months |
Food‐secure: 48.7%; Mild food insecurity: 20.4%; Moderate food insecurity: 15.7%; Severe food insecurity: 15.2%. |
Stunting: not reported |
Food‐secure households: (reference group) Adjusted for infant and maternal factors Mild food insecurity (aOR: 1.05; 95% CI: 0.94−1.16) Moderate food insecurity (aOR: 1.24; 95% CI: 1.11−1.39) Severe food insecurity (aOR: 1.39; 95% CI: 1.24−1.56) |
|
| (Namirembe et al., 2022) Uganda | Between 2014 and 2016 | Prospective cohort | 4528 | 0 at 12 months |
Food secure: 38.2%; Mildly food insecure: 24.8%; Moderately food insecure: 23.2%; Severely food insecure: 13.8%. |
Stunting: 79% |
Food insecurity associated with chronically stunted: (β = 0.183; 95% CI: −0.129 to 0.495) Food insecurity associated with recovery group: (β = −0.107; 95% CI: −0.426 to 0.212) Food insecurity associated with borderline stunted: (β = −0.354; 95% CI: −0.623 to −0.085) |
|
| (Oduro et al., 2022) Kenya | Between 2010 and 2014 | Prospective cohort | 692 | 0 and 36 months |
Food secure: 25%; Moderately food insecure: 17%; Severely food insecure: 58%. |
Normal: 23%; Marginally stunted: 26%; Moderately stunted: 21%; Severely stunted: 30%. |
Transition (state normal‐marginally stunted): Hunger scale (ref = Food secure) Moderately food insecure: (HR: 0.8622; 95% CI: 0.3189−2.331) Severely food insecure: (HR: 0.3934; 95% CI: 0.1445, 1.0708) Transition (state marginally stunted‐normal): Hunger scale (ref = Food secure) Moderately food insecure: (HR: 0.8376; 95% CI: 0.3262−2.151) Severely food insecure: (HR: 0.3487; 95% CI: 0.1351−0.8997) Transition (state marginally stunted‐moderately stunted): Hunger scale (ref = Food secure) Moderately food insecure: (HR: 2.4362; 95% CI: 1.3037−4.552) Severely food insecure:(HR: 1.2696; 95% CI: 0.7795−2.0679) Transition (state moderately stunted‐ marginally stunted): Hunger scale (ref = Food secure) Moderately food insecure: (HR: 2.8500; 95% CI: 1.5761−5.154) Severely food insecure: (HR: 1.6450; 95% CI: 1.0643−2.5427) Transition (state moderately stunted‐severely stunted): Hunger scale (ref = Food secure) Moderately food insecure: (HR: 0.4177; 95% CI: 0.1172−1.489) Severely food insecure: (HR: 0.4033; 95% CI: 0.1313−1.2387) Transition (state severely stunted‐ moderately stunted): Hunger scale (ref = Food secure) Moderately food insecure: (HR: 0.9433; 95% CI: 0.2503−3.555) Severely food insecure: (HR: 0.4642; 95% CI: 0.1423−1.5142) |
|
Abbreviations: aRR, adjusted relative risk; aOR, odds ratio adjusted; CI, confidence interval; FSP, food stamp program (FSP); HFI, household food insecurity; H&CFI, household and child food insecurity; HR, hazard ratio; OR, odds ratio; SE, standard error; TANF, temporary assistance to needy families; β, Beta.
Not included in the meta‐analysis because it was not possible to calculate the OR with the data available.
A prospective cohort study conducted by Mutisya et al. (2015) assessed the effect of household food security status and its interaction with household wealth status on stunting among children aged 6–23 months in a resource‐poor urban setting in Kenya. The growth delay was greater between 10 and 15 months, reaching a peak at around 12 months of age, and the risk of a child being stunted if he came from a household with moderate and severe food insecurity increased by 16% (HR: 1.16; 95% CI: 1.07−1.26) and 23% (HR: 1.23; 95% CI: 1.11−1.35), respectively, compared to that in children from a household with food security. In other words, family security and the asset wealth index are associated with delayed growth. After adjusting for other variables, such as the asset wealth index, the characteristics of the mother and child (age at birth, level of education, birth parity, breastfeeding, and birth weight), and household characteristics (head education, sex, age, and size) remained positive and significant (Mutisya et al., 2015).
The retrospective cohort study (Koyratty et al., 2022) conducted in rural districts of Zimbabwe between November 2012 and March 2015 showed that the dimension of ‘low food availability and quality' was the only one associated with LAZ from 1 month to month 18 (M1 to M18) of age (β: −0.09; 95% CI: −0.17 to –0.01). Na et al. (2020) identified components and likely mechanisms explaining the observed associations between HFI and infant size at 6 months of age in rural Bangladesh. Compared with the food‐secure group, mild, moderate, and severe HFI were associated with a 5% (adjusted OR [aOR]: 1.05; 95% CI: 0.94−1.16), 24% (aOR: 1.24; 95% CI: 1.11−1.39), and 39% (aOR: 1.39; 95% CI: 1.24−1.56) increased risk of stunting, respectively (Na et al., 2020).
A longitudinal study in South Africa (Harper et al., 2023) assessed the relationship between HFI indicators with birth weight and stunting in the first 5 years of life and showed that household food expenditure below the poverty line, a food security indicator, was significantly associated with an increased risk of stunting.
Oduro et al. (2022) described transitions between stunting states and associated factors among children aged 0−3 years and showed that when in a marginally stunted state, children living in moderately food insecure and severely food insecure households are 2.4 times more at risk of moving into a moderately stunted state than children in food secure households. Additionally, the risk of back transitioning from moderately stunted to marginally stunted state for children in moderately food secured and severely food households are, respectively, 2.8 and 1.6 times the risk for children in food secured households (Oduro et al., 2022).
Namirembe et al. (2022) followed a cohort of Ugandan infants from birth through 1 year of age, applied group‐based trajectory modeling to assess diverse patterns of growth, and assessed the pre‐and postnatal factors associated with each pattern. Child growth patterns followed four distinct trajectory groups in rural Ugandan children: chronically stunted (group one), recovery (group two), borderline stunted (group three), and normal (group four). Group one had the highest proportion of children from poorest (41.3%) and most food‐insecure (68.1%) households. The HFI was a risk factor to borderline stunted (β = −0.354; 95% CI: −0.623 to −0.085; p ≤ 0.01) (Namirembe et al., 2022).
Belayneh et al. (2020) evaluated seasonal patterns of HFI on stunting and showed that the prevalence increased with age, with a higher prevalence among children aged > 36 months. Additionally, compared to the severe HFI group, the mild HFI group showed increased odds of child stunting (OR: 2.94; 95% CI: 1.18−7.31; p < 0.05) and moderate HFI (OR: 1.56; 95% CI: 1.02−2.39; p < 0.05). The other studies included in this review showed no association between HFI and stunting (Cook et al., 2006; Kabalo & Lindtjørn, 2022).
3.4. Risk of bias within individual studies
Figure 2 outlines the risk of bias (see Table S3 for a full appraisal). Of nine cohort studies, five (55.5%) were considered low risk of bias (Belayneh et al., 2020; Kabalo & Lindtjørn, 2022; Mutisya et al., 2015; Na et al., 2020; Namirembe et al., 2022), two studies were at high risk of bias due to not presenting a validated method for measuring HFI (Harper et al., 2023; Koyratty et al., 2022). Among the sources of bias, one study did not detail whether the method used to measure exposure was validated and did not control for confounding factors (Oduro et al., 2022), Another study did not recruit groups from the same population (Cook et al., 2006).
Figure 2.
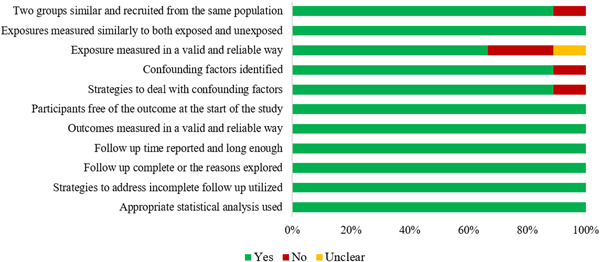
Risk of bias of the included articles according to study design.
3.5. Meta‐analysis
Six articles were pooled in the meta‐analysis, including 37.359 participants, but no association was found between the mild and moderate HFI exposition and stunting (OR: 1.00; 95% CI: 0.87−1.14; I 2: 76.14%) (Figure 3) (Belayneh et al., 2020; Cook et al., 2006; Kabalo & Lindtjørn, 2022; Koyratty et al., 2022; Na et al., 2020; Namirembe et al., 2022). The association between moderate and severe HFI and stunting was also explored using HR in five articles, including 14.151 children (Kabalo & Lindtjørn, 2022; Koyratty et al., 2022; Mutisya et al., 2015; Namirembe et al., 2022; Oduro et al., 2022); however, no significant association was found (HR: 1.02; 95% CI: 0.84−1.22; I 2: 85.96%) (Figure 4).
Figure 3.
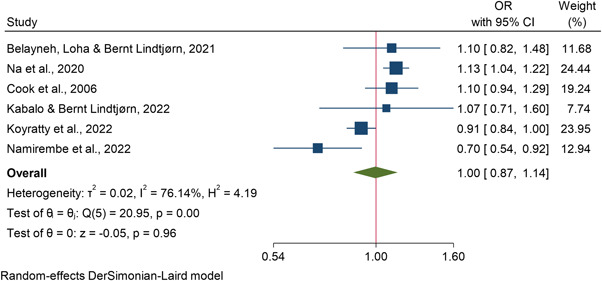
Meta‐analysis of HFI mild and moderate versus stunting. HFI, household food insecurity.
Figure 4.
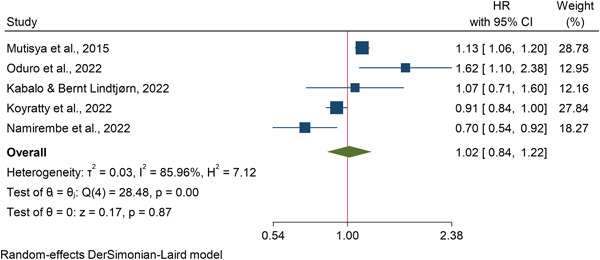
Meta‐analysis of HFI moderate and severe versus stunting. HFI, household food insecurity.
3.6. Certainty of evidence
The GRADE assessment was very low for mild and moderate HFI and stunting and moderate and severe HFI and stunting (⊕◯◯◯). The full GRADE assessment of each meta‐analysis is shown in Table S4.
4. DISCUSSION
The present systematic review highlighted the association between HFI and stunting in children aged 0−59 months across individual studies; however, this association was not observed in the pooled analysis. The results of our meta‐analysis should be interpreted with caution because of the small number of cohort studies investigating this association. Stunting affects 148.1 million (22.3%) children aged <5 years worldwide. Almost all the affected children live in Asia (52% of the global population) and Africa (43% of the global proportion) (World Health Organization, 2023). A systematic review conducted to describe the prevalence and predictive factors in children aged <5 years of age found a combined prevalence of growth retardation of 39.11% (Rafique & Afzal, 2023). The data reported in the literature are consistent with the high prevalence of stunting observed among participants in the studies included in this review.
Of the nine studies included in this review, 78% found a significant association between HFI and stunting. The data demonstrate the important impact on public health in children and may support future recommendations and strategies for these populations. HFI is recognized as a standard underlying determinant of stunting (United Nations Children's Fund UNICEF, 2020). A cross‐sectional study of children aged 2−5 years in Indonesia found that households with severe food insecurity increased the likelihood of child stunting (Mahmudiono et al., 2018). Other studies have presented contrasting findings, indicating no correlation between HFI and stunting in the respective contexts in which the study was conducted (Motbainor et al., 2015; Roesler et al., 2019).
When attempting to statistically combine the results of individual studies, this association was not sustained in the pooled meta‐analyses. This may be explained by the fact that these studies had regional differences. Food security inequalities exist both within and between countries. Furthermore, the HFI has a geographical concentration in impoverished urban neighborhoods, large metropolitan areas, and remote rural regions (FAO, IFAD, UNICEF, WFP, & WHO, 2022).
The high prevalence of HFI found among children in studies conducted in sub‐Saharan Africa (Harper et al., 2023; Kabalo & Lindtjørn, 2022; Koyratty et al., 2022; Mutisya et al., 2015; Namirembe et al., 2022; Oduro et al., 2022) can be explained by the civil conflict in these regions and heavy dependence of the Near East and North African diets on imported wheat (FAO, IFAD, UNICEF, WFP, & WHO, 2022). In 2021, the prevalence of HFI is significantly higher in African populations than that in Asian, Latin American, and Caribbean populations; Oceania; North America; and Europe (FAO, IFAD, UNICEF, WFP, & WHO, 2022). In contrast, in addition to these regional and socioeconomic differences within and between countries, the influence of other factors on child growth must also be considered.
Childhood stunting is influenced by several contextual factors originating at different levels that may interact or correlate with each other (Lukwa et al., 2020). Namirembe et al., 2022 reported that stunting occurred before birth, citing maternal education, height, age, human immunodeficiency virus serology, and gestational age as possible prenatal risk factors. Na et al. (2020) found that increasing the severity of HFI had a significant dose–response association with infant weight and linear growth at 6 months of age. A systematic review examining the relationship between HFI, dietary diversity, and stunting in children aged <5 years found that these factors are significantly associated with stunting in sub‐Saharan Africa (Gassara & Chen, 2021).
According to the WHO conceptual framework on childhood stunting (Stewart et al., 2013), stunted growth and development are at the center of the framework, and the contextual factors are organized in the category ‘Community/Nation’, which includes the following groups: political economy, health and healthcare, education, society and culture, agriculture and food systems, and water, sanitation and environment. As causes of stunted growth and development, household and family factors include maternal outcomes before and during pregnancy and the home environment (Stewart et al., 2013).
In Ethiopia, stunting shows seasonal variations, and the HFI increases during the preharvest season when there is a greater shortage of food. However, the patient developed stunting a few months later. Additionally, household characteristics such as poverty level, education, occupation, HFI, and dietary diversity have been associated with subsequent wasting or stunting (Belayneh et al., 2020).
A significant proportion of the studies included in this review were conducted in LMICs. Despite the progress made in recent years in reducing global poverty and HFI, particularly in LMICs, the prevalence of HFI remains unacceptably high. Moreover, stunting and wasting remain public health problems associated with LICs (Victora et al., 2021). Food expenditure below the Stats SA poverty line and low dietary diversity are associated with stunting and severe stunting, respectively (Harper et al., 2023). There is growing evidence that HFI interferes with physical, economic, biological, and social access to food, and its consequences can affect the nutritional status of both children and adults (Militao et al., 2022; Potochnick et al., 2019; Schmeer & Piperata, 2017).
Other factors associated with growth and development disorders include inadequate breastfeeding, inadequate complementary feeding (Stewart et al., 2013). An Ethiopian demographic and health survey conducted in 2019 with children aged 6–23 months found that the factors that had a significant negative association with length‐for‐age were agrarian region of residence, poor household wealth category, unimproved household toilet facility, male sex, age, not currently breastfeeding, and small birth size. In contrast, vitamin A supplementation, higher meal frequency, and dietary diversity scores showed significant positive associations with length‐for‐age, confirming its multifactorial nature (Mohammed et al., 2019).
It is essential to implement both clinical interventions aimed at the prevention and treatment of growth disorders and social protection policies aimed at reducing HFI and stunting in children (Mohammed et al., 2019). From a clinical practice perspective, targeted interventions may include the promotion of growth status, tailored counseling, micronutrient supplementation, detection and treatment of common conditions, and referral to healthcare providers as needed (Daelmans et al., 2015).
At the social protection policy level, various policies and programs can be formulated or reformulated to address child food insecurity in households. Unconditional and conditional cash transfer programs can improve food security and dietary diversity. Food vouchers can also reduce stunting (Durao et al., 2020; Reeves et al., 2021). These social protection measures contribute directly or indirectly to improving the socioeconomic status of families, consequently reducing HFI. Additionally, measures must be implemented that include educating vulnerable groups, such as women and girls, improving access to drinking water, and changing access to maternal and child health care (Durao et al., 2020; Reeves et al., 2021).
Between 2006 and 2016, India reported that modifications in health and nutrition services, household socioeconomic status, and sanitation led to advancements in reducing childhood stunting. Shared programs between the state and district governments, development partners, and civil society included a set of interventions aimed at health and nutrition care during pregnancy and childbirth, neonatal protection against tetanus, deworming, nutritional interventions for children (complete immunization, folic acid and vitamin A supplementation), massive community health worker programs, right‐to‐food campaigns, improvements in sanitation, and universalization of the Integrated Child Development Services program (Kohli et al., 2020).
Brazil's policies for income redistribution and the provision of basic services, including universal access to education, health, water supply, and sanitation services, played a fundamental role in improving child growth indicators from 1996 to 2007, highlighting the need to maintain economic and social policies (Monteiro et al., 2009; Monteiro et al., 2010). Another study that presented results from countries with exemplary progress in providing guidelines for reducing child stunting highlighted the importance of interventions both within and outside the health sector. These interventions include improvements in parental education, maternal nutrition, maternal and neonatal care, economic conditions, and fertility control/interval between pregnancies (Bhutta et al., 2020).
This systematic review and meta‐analysis highlight that HFI and stunting are prominent global health problems that are interrelated. Thus, they require attention from both researchers and health policymakers in the production of more homogeneous studies, formulation of health policies, and decision‐making to reduce stunting. This study has several strengths. To our knowledge, this is the first study to conduct a meta‐analysis on this topic. A comprehensive search strategy was carried out using robust and appropriate methodology according to Cochrane Handbook and PRISMA guidelines. Moreover, many participants were included in each pooled outcome, which increases the generalizability of the results. The methodological quality of the included studies was assessed independently, and the GRADE system was used to assess the certainty of the evidence for each exposure–outcome association.
This study has some notable limitations. First, considering the nature of observational studies, high heterogeneity between studies was observed in many analyses. Additionally, variations in the HFI measurement instruments used in the studies and discrepancies in the incidence of food security based on the level of development of the countries may have contributed to heterogeneity. Although we performed a meta‐regression to explore the possible sources of heterogeneity, this was not possible because of the limited number of studies. For further cohort studies, since a wide variety of covariates were used in the included studies, it is recommended that multivariable analyses be performed to adjust for other factors associated with growth that may be confounding covariates, such as differences in age at exposure assessment, maternal age and education level, income level, and breastfeeding. Second, we focused only on the association between HFI and stunting. As other factors were found to be associated with delayed linear growth in light of the available evidence, another systematic review is recommended to expand this investigation. Third, few longitudinal studies have examined the relationship between HFI and stunting in children aged <5 years, indicating the need for further studies with robust methodological quality.
5. CONCLUSIONS
This study indicated that most of the studies included in the review found a significant association between HFI and stunting; however, this was not maintained in the meta‐analysis results. These study findings highlight that HFI alone does not explain growth problems in this age group based on scientific evidence in the literature to date and point to the need for continued and effective monitoring of factors affecting child growth.
AUTHOR CONTRIBUTIONS
Érika S. O. Patriota, Lívia C. S. Abrantes Vivian S. S. Gonçalves and Nathalia Pizato were involved in conceptualization. Érika S. O. Patriota, Lívia C. S. Abrantes and Vivian S. S. Gonçalves were involved in methodology. Érika S. O. Patriota and Lívia C. S. Abrantes were involved inconducting the systematic literature search. Érika S. O. Patriota and Lívia C. S. Abrantes were involved inperformed the data extraction and quality assessment. Érika S. O. Patriota and Ana C. M. G. Figueiredo were involved formal analysis. Érika S. O. Patriota was involved in writing—original draft preparation. Érika S. O. Patriota, Vivian S. S. Gonçalves and Gabriela Buccini were involved inwriting‐review and editing. Vivian S. S. Gonçalves was involved insupervision. All authors have read and agreed to the published version of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Supporting information
Supporting information.
Supporting information.
Supporting information.
Supporting information.
ACKNOWLEDGEMENTS
We would like to thank to Roberta Borges Silva for the “Peer Review of Electronic Search Strategies” validation. Furthermore, we thank all authors who we contacted and sent us their data for the meta‐analysis.
Patriota, É. S. O. , Abrantes, L. C. S. , Figueiredo, A. C. M. G. , Pizato, N. , Buccini, G. , & Gonçalves, V. S. S. (2024). Association between household food insecurity and stunting in children aged 0−59 months: Systematic review and meta‐analysis of cohort studies. Maternal & Child Nutrition, 20, e13609. 10.1111/mcn.13609
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Belayneh, M. , Loha, E. , & Lindtjørn, B. (2021). Seasonal variation of household food insecurity and household dietary diversity on wasting and stunting among young children in A drought prone area in South Ethiopia: A cohort study. Ecology of Food and Nutrition, 60(1), 44–69. 10.1080/03670244.2020.1789865 [DOI] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Akseer, N. , Keats, E. C. , Vaivada, T. , Baker, S. , Horton, S. E. , Katz, J. , Menon, P. , Piwoz, E. , Shekar, M. , Victora, C. , & Black, R. (2020). How countries can reduce child stunting at scale: lessons from exemplar countries. The American Journal of Clinical Nutrition, 112(Suppl. 2), 894S–904S. 10.1093/ajcn/nqaa153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biete, A. , Gonçalves, V. S. S. , Franceschini, S. C. C. , Nilson, E. A. F. , & Pizato, N. (2023). The prevalence of nutritional anaemia in Brazilian pregnant women: A systematic review and meta‐analysis. International Journal of Environmental Research and Public Health, 20(2), 1519. 10.3390/ijerph20021519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, R. E. , Liu, L. , Hartwig, F. P. , Villavicencio, F. , Rodriguez‐Martinez, A. , Vidaletti, L. P. , Perin, J. , Black, M. M. , Blencowe, H. , You, D. , Hug, L. , Masquelier, B. , Cousens, S. , Gove, A. , Vaivada, T. , Yeung, D. , Behrman, J. , Martorell, R. , Osmond, C. , … Victora, C. G. (2022). Health and development from preconception to 20 years of age and human capital. The Lancet, 399(10336), 1730–1740. 10.1016/s0140-6736(21)02533-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook, J. T. , Frank, D. A. , Levenson, S. M. , Neault, N. B. , Heeren, T. C. , Black, M. M. , Berkowitz, C. , Casey, P. H. , Meyers, A. F. , Cutts, D. B. , & Chilton, M. (2006). Child food insecurity increases risks posed by household food insecurity to Young Children's Health. The Journal of Nutrition, 136, 1073–1076. [DOI] [PubMed] [Google Scholar]
- Daelmans, B. , Black, M. M. , Lombardi, J. , Lucas, J. , Richter, L. , Silver, K. , Britto, P. , Yoshikawa, H. , Perez‐Escamilla, R. , MacMillan, H. , Dua, T. , Bouhouch, R. R. , Bhutta, Z. , Darmstadt, G. L. , Rao, N. , & Steering committee of a new scientific series on early child, development . (2015). Effective interventions and strategies for improving early child development. BMJ (Clinical Research Ed.), 351, 4029. 10.1136/bmj.h4029 [DOI] [PubMed] [Google Scholar]
- Deeks, J. , Higgins, J. , & Altman, D. (2021). Chapter: Analysing data and undertaking meta‐analyses, Cochrane Handbook for Systematic Reviews of Interventions Version 6.2, 3 (pp. 1–48). https://training.cochrane.org/handbook/current/chapter-10 [Google Scholar]
- Durao, S. , Visser, M. E. , Ramokolo, V. , Oliveira, J. M. , Schmidt, B. M. , Balakrishna, Y. , Brand, A. , & Kristjansson, E. S. A. (2020). Community‐level interventions for improving access to food in low‐ and middle‐income countries (Review). Cochrane Database of Systematic Reviews, 7, 1. 10.1002/14651858.CD011504.pub2.www.cochranelibrary.com [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO, IFAD, UNICEF, WFP, & WHO . (2022). The State of Food Security and Nutrition in the World 2022, In The State of Food Security and Nutrition in the World 2022. 10.4060/cc0639en [DOI] [Google Scholar]
- Fitzmaurice, G. M. , Laird, N. M. , & Ware, J. (2012). In Sons J. W. (Ed.), Applied Longitudinal Analysis (2nd ed). [Google Scholar]
- Gallegos, D. , Eivers, A. , Sondergeld, P. , & Pattinson, C. (2021). Food insecurity and child development: A state‐of‐the‐art review, International Journal of Environmental Research and Public Health, 18, 8990. 10.3390/ijerph18178990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gassara, G. , & Chen, J. (2021). Household food insecurity, dietary diversity, and stunting in Sub‐Saharan Africa: A systematic review. Nutrients, 13(13), 4401. 10.3390/nu1312440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper, A. , Rothberg, A. , Chirwa, E. , Sambu, W. , & Mall, S. (2023). Household food insecurity and demographic factors, low birth weight and stunting in early childhood: Findings from a longitudinal study in South Africa. Maternal and Child Health Journal, 27(1), 59–69. 10.1007/s10995-022-03555-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan, M. M. , Kader, A. , Asif, C. A. A. , & Talukder, A. (2022). Seasonal variation in the association between household food insecurity and child undernutrition in Bangladesh: Mediating role of child dietary diversity. Maternal & Child Nutrition, 19(2), e13465. 10.1111/mcn.13465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inzaghi, E. , Pampanini, V. , Deodati, A. , & Cianfarani, S. (2022). The effects of nutrition on linear growth. Nutrients, 14(9), 1752. 10.3390/nu14091752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabalo, B. Y. , & Lindtjørn, B. (2022). Seasonality and predictors of childhood stunting and wasting in drought‐prone areas in Ethiopia: A cohort study. BMJ Open, 12(11), e060692. 10.1136/bmjopen-2021-060692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohli, N. , Nguyen, P. H. , Avula, R. , & Menon, P. (2020). The role of the state government, civil society and programmes across sectors in stunting reduction in Chhattisgarh, India, 2006–2016. BMJ Global Health, 5(7), e002274. 10.1136/bmjgh-2019-002274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koyratty, N. , Ntozini, R. , Mbuya, M. N. , Jones, A. D. , Schuster, R. C. , Kordas, K. , Li, C. S. , Tavengwa, N. V. , Majo, F. D. , Humphrey, J. , & Smith, L. E. (2022). Growth and growth trajectory among infants in early life: Contributions of food insecurity and water insecurity in rural Zimbabwe. BMJ Nutrition, Prevention & Health, 5(2), 332–343. 10.1136/bmjnph-2022-000470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski, R. J. , Ogden, C. L. , Guo, S. S. , Grummer‐Strawn, L. M. , Flegal, K. M. , Mei, Z. , Wei, R. , Curtin, L. R. , Roche, A. F. , & Johnson, C. L. (2002). 2000 CDC growth charts for the United States: Methods and development. vital and health statistics. Vital and Health Statistics 11, 246, 1–190. [PubMed] [Google Scholar]
- Laird, N. M. (2022). Statistical analysis of longitudinal studies. International Statistical Review, 90(S1), S2–S16. 10.1111/insr.12523 [DOI] [Google Scholar]
- Lukwa, A. T. , Siya, A. , Zablon, K. N. , Azam, J. M. , & Alaba, O. A. (2020). Socioeconomic inequalities in food insecurity and malnutrition among under‐five children: Within and between‐group inequalities in Zimbabwe. BMC Public Health, 20(1), 1199. 10.1186/s12889-020-09295-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lye, C. W. , Sivasampu, S. , Mahmudiono, T. , & Majid, H. A. (2023). A systematic review of the relationship between household food insecurity and childhood undernutrition. Journal of Public Health, 45, e677–e691. 10.1093/pubmed/fdad070 [DOI] [PubMed] [Google Scholar]
- Mahmudiono, T. , Nindya, T. , Andrias, D. , Megatsari, H. , & Rosenkranz, R. (2018). Household food insecurity as a predictor of stunted children and overweight/obese mothers (SCOWT) in urban Indonesia. Nutrients, 10(5), 535. 10.3390/nu10050535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan, J. , Sampson, M. , Salzwedel, D. M. , Cogo, E. , Foerster, V. , & Lefebvre, C. (2016). PRESS peer review of electronic search strategies: 2015 guideline statement. Journal of Clinical Epidemiology, 75, 40–46. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- Militao, E. M. A. , Salvador, E. M. , Uthman, O. A. , Vinberg, S. , & Macassa, G. (2022). Food insecurity and health outcomes other than malnutrition in Southern Africa: A descriptive systematic review. International Journal of Environmental Research and Public Health, 19(9), 5082. 10.3390/ijerph19095082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistry, S. K. , Hossain, M. B. , Khanam, F. , Akter, F. , Parvez, M. , Yunus, F. M. , Afsana, K. , & Rahman, M. (2019). Individual, maternal‐ and household‐level factors associated with stunting among children aged 0–23 months in Bangladesh. Public Health Nutrition, 22(1), 85–94. 10.1017/S1368980018002926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammed, S. H. , Habtewold, T. D. , Tegegne, B. S. , Birhanu, M. M. , Sissay, T. A. , Larijani, B. , & Esmaillzadeh, A. (2019). Dietary and non‐dietary determinants of linear growth status of infants and young children in Ethiopia: Hierarchical regression analysis. PLoS One, 14(1), e0209220. 10.1371/journal.pone.0209220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteiro, C. A. , Benicio, M. H. D. , Conde, W. L. , Konno, S. , Lovadino, A. L. , Barros, A. J. , & Victora, C. G. (2010). Narrowing socioeconomic inequality in child stunting: The Brazilian experience, 1974–2007. Bulletin of the World Health Organization, 88(4), 305–311. 10.2471/blt.09.069195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteiro, C. A. , Benicio, M. H. D. , Konno, S. C. , Silva, A. C. F. , Lima, A. L. L. , & Conde, W. L. (2009). Causas do declínio da desnutrição infantil no Brasil, 1996–2007. Revista de Saúde Pública, 43(1), 35–43. 10.1590/s0034-89102009000100005 [DOI] [PubMed] [Google Scholar]
- Moola, S. , Munn, Z. , Tufanaru, C. , Aromataris, E. , Sears, K. , Sfetcu, R. , Currie, M. , Lisy, K. , Qureshi, R. , & Mattis, P. M. P. (2020). Systematic Reviews of Etiology and Risk. In Aromataris E. & Munn Z. (Eds.), JBI Manual for Evidence Synthesis. JBI. 10.46658/JBIMES-20-08 [DOI] [Google Scholar]
- Motbainor, A. , Worku, A. , & Kumie, A. (2015). Stunting is associated with food diversity while wasting with food insecurity among underfive children in east and west Gojjam zones of Amhara region, Ethiopia. PLoS One, 10(8), e0133542. 10.1371/journal.pone.0133542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutisya, M. , Kandala, N. , Ngware, M. W. , & Kabiru, C. W. (2015). Household food (in)security and nutritional status of urban poor children aged 6 to 23 months in Kenya. BMC Public Health, 15(1), 1052. 10.1186/s12889-015-2403-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Na, M. , Shamim, A. A. , Mehra, S. , Labrique, A. , Ali, H. , Wu, L. S. F. , Shaikh, S. , Klemm, R. , Christian, P. , & West, K. P. (2020). Maternal nutritional status mediates the linkage between household food insecurity and mid‐infancy size in rural Bangladesh. British Journal of Nutrition, 123(12), 1415–1425. 10.1017/S0007114520000707 [DOI] [PubMed] [Google Scholar]
- Namirembe, G. , Ghosh, S. , Ausman, L. M. , Shrestha, R. , Zaharia, S. , Bashaasha, B. , Kabunga, N. , Agaba, E. , Mezzano, J. , & Webb, P. (2022). Child stunting starts in utero: Growth trajectories and determinants in Ugandan infants. Maternal & child nutrition, 18(3), 1–12. 10.1111/mcn.13359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oduro, M. S. , Iddi, S. , Asiedu, L. , Asiki, G. , & Kadengye, D. T. (2022). A multi‐state transition model for child stunting in two urban slum settlements of Nairobi: A longitudinal analysis, 2011–2014. MedRxiv. https://www.medrxiv.org/content/10.1101/2022.07.26.22278058.abstract%0Ahttps://www.medrxiv.org/content/10.1101/2022.07.26.22278058.full.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Oliveira, K. H. D. , de Almeida, G. M. , Gubert, M. B. , Moura, A. S. , Spaniol, A. M. , Hernandez, D. C. , Pérez‐Escamilla, R. , & Buccini, G. (2020). Household food insecurity and early childhood development: Systematic review and meta‐analysis. Maternal & child nutrition, 16(3), 1–27. 10.1111/mcn.12967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paula, W. O. , Patriota, E. S. O. , Gonçalves, V. S. S. , & Pizato, N. (2022). Maternal consumption of Ultra‐Processed Foods‐Rich diet and perinatal outcomes: A systematic review and Meta‐Analysis. Nutrients, 14(15), 3242. 10.3390/nu14153242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potochnick, S. , Perreira, K. M. , Bravin, J. I. , Castañeda, S. F. , Daviglus, M. L. , Gallo, L. C. , & Isasi, C. R. (2019). Food insecurity among Hispanic/Latino youth: who is at risk and what are the health correlates? Journal of Adolescent Health, 64(5), 631–639. 10.1016/j.jadohealth.2018.10.302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafique, S. , & Afzal, S. (2023). Prevalence and predictors of stunting in children under five years of age. Journal of the College of Physicians and Surgeons Pakistan, 33(4), 449–456. 10.29271/jcpsp.2023.04.449 [DOI] [PubMed] [Google Scholar]
- Reeves, A. , Loopstra, R. , & Tarasuk, V. (2021). Family policy and food insecurity: An observational analysis in 142 countries. The Lancet Planetary Health, 5(8), e506–e513. 10.1016/S2542-5196(21)00151-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roesler, A. L. , Smithers, L. G. , Wangpakapattanawong, P. , & Moore, V. (2019). Stunting, dietary diversity and household food insecurity among children under 5 years in ethnic communities of Northern Thailand. Journal of Public Health, 41(4), 772–780. 10.1093/pubmed/fdy201 [DOI] [PubMed] [Google Scholar]
- Schmeer, K. K. , & Piperata, B. A. (2017). Household food insecurity and child health. Maternal & Child Nutrition, 13(2), 1–13. 10.1111/mcn.12301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schünemann, H. , Brozek, J. , Guyatt, G. , & Oxman, A. (2013). Quality of Evidence. In Schünemann H., Brozek J., Guyatt G., & Oxman A., (Eds.), GRADE Handbook. GRADE Working Group. [Google Scholar]
- Schwarzenberg, S. J. , Georgieff, M. K. , Corkins, M. , Golden, N. H. , Kim, J. H. , Lindsey, C. W. , & Magge, S. N. , Committee on nutrition . (2018). Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics, 141(2), e20173716. 10.1542/peds.2017-3716 [DOI] [PubMed] [Google Scholar]
- Stewart, C. P. , Iannotti, L. , Dewey, K. G. , Michaelsen, K. F. , & Onyango, A. W. (2013). Contextualising complementary feeding in a broader framework for stunting prevention. Maternal & child nutrition, 9(S2), 27–45. 10.1111/mcn.12088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank . (2023). World Bank Open Data, Free and open access to global development data. https://data.worldbank.org/ [Google Scholar]
- UNICEF/WHO/WORLD BANK . (2021). Levels and trends in child malnutrition UNICEF/WHO/World Bank Group Joint Child Malnutrition Estimates Key findings of the 202 edition (pp. 1–32). World Health Organization. https://www.who.int/publications/i/item/9789240025257 [Google Scholar]
- United Nations Children's Fund (UNICEF) . (2020). Nutrition, for Every Child: UNICEF Nutrition Strategy 2020–2030. UNICEF. [Google Scholar]
- World Health Organization, United Nations Children's Fund (UNICEF) & International Bank for Reconstruction and Development/The World Bank . (2023). Levels and trends in child malnutrition: UNICEF/WHO/World Bank Group Joint Child Malnutrition Estimates: Key findings of the 2023 edition. UNICEF and WHO. [Google Scholar]
- Victora, C. G. , Christian, P. , Vidaletti, L. P. , Gatica‐Domínguez, G. , Menon, P. , & Black, R. E. (2021). Revisiting maternal and child undernutrition in low‐income and middle‐income countries: Variable progress towards an unfinished agenda. The Lancet, 397(10282), 1388–1399. 10.1016/S0140-6736(21)00394-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Child Growth Standards: Growth velocity based on weight, length and head circumference: Methods and development . (2006). Developmental Medicine & Child Neurology, 51(12), 1002. 10.1111/j.1469-8749.2009.03503.x [DOI] [Google Scholar]
- Zhang, J. , & Yu, K. F. (1998). What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. Journal of the American Medical Association, 280(19), 1690–1691. 10.1001/jama.280.19.1690 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


