Abstract
Chronic low-degree inflammation is a hallmark of atherosclerotic cardiovascular (CV) disease. To assess the effect of lipid-lowering therapies on C-reactive protein (CRP), a biomarker of inflammation, we conducted a meta-analysis according to the PRISMA guidelines. Databases were searched from inception to July 2023. Inclusion criteria were: (i) randomized controlled trials (RCTs) in human, Phase II, III, or IV; (ii) English language; (iii) comparing the effect of lipid-lowering drugs vs. placebo; (iv) reporting the effects on CRP levels; (v) with intervention duration of more than 3 weeks; (vi) and sample size (for both intervention and control group) over than 100 subjects. The between-group (treatment-placebo) CRP absolute mean differences and 95% confidence intervals were calculated for each drug class separately. A total of 171 668 subjects from 53 RCTs were included. CRP levels (mg/L) were significantly decreased by statins [−0.65 (−0.87 to −0.43), bempedoic acid; −0.43 (−0.67 to −0.20), ezetimibe; −0.28 (−0.48 to −0.08)], and omega-3 fatty acids [omega3FAs, −0.27 (−0.52 to −0.01)]. CRP was reduced by −0.40 (−1.17 to 0.38) with fibrates, although not statistically significant. A slight increase of CRP concentration was observed for proprotein convertase subtilisin/kexin type 9 inhibitors [0.11 (0.07–0.14)] and cholesteryl-ester transfer protein inhibitors [0.10 (0.00–0.21)], the latter being not statistically significant. Meta-regression analysis did not show a significant correlation between changes in CRP and LDL cholesterol (LDL-C) or triglycerides. Statins, bempedoic acid, ezetimibe, and omega3FAs significantly reduce serum CRP concentration, independently of LDL-C reductions. The impact of this anti-inflammatory effect in terms of CV prevention needs further investigation.
Keywords: C-reactive protein, Lipid-lowering therapies, Cardiovascular disease, Inflammation
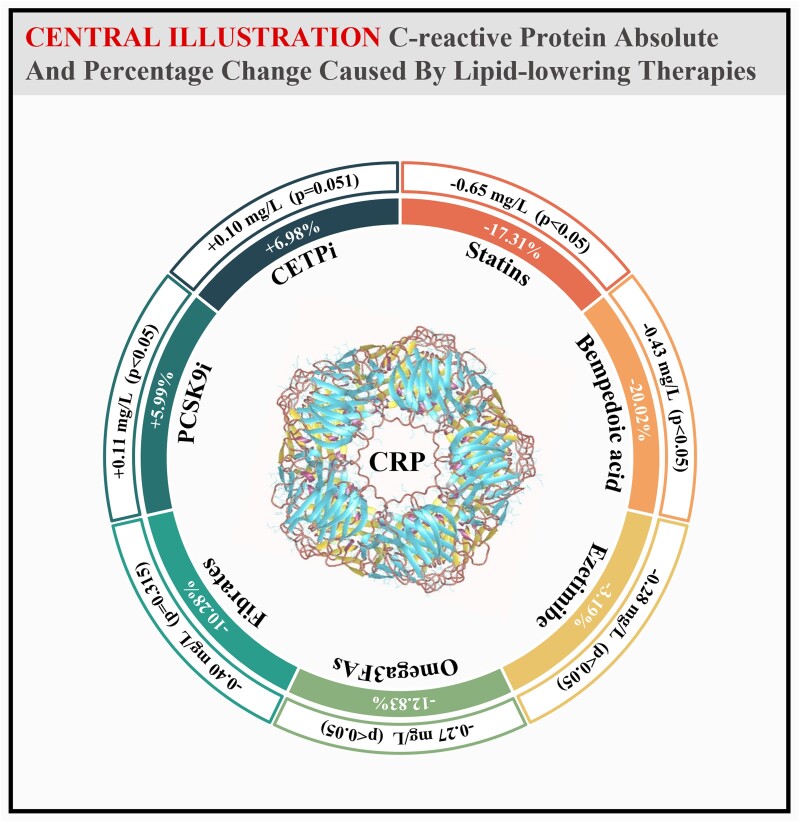
Graphical Abstract
Graphical Abstract.
1. Introduction
Atherosclerotic cardiovascular disease (ASCVD) remains one of the leading causes of death and disability. Controlling LDL cholesterol (LDL-C) levels is the cornerstone of the prevention of cardiovascular (CV) events.1 Lipid-lowering therapy (LLT) with statins as the first choice, is commonly used to improve arterial health and prevent atherosclerosis. Nevertheless, data from both clinical trials and registries highlighted that even under optimized LLT, many patients continue to suffer CV events.2 It has been suggested that the inflammatory state that typically characterizes ASCVD3 could be responsible for this residual CV risk. Thus, the evaluation of inflammatory biomarkers, such as C-reactive protein (CRP), could be critical.4 Indeed, even though the causal role of CRP in the atherosclerotic process has been excluded by Mendelian randomization studies,5 CRP concentration in serum still is a useful marker of the inflammatory status of a given patient. Observational studies reported the link between increased high-sensitivity CRP levels and an elevated risk of CV disease (CVD) in individuals with or without a CVD history.6 Moreover, several clinical trials, including PROVE-IT7 (atorvastatin 80 mg) and IMPROVE-IT8 (ezetimibe plus simvastatin 40 mg), illustrated that patients who met both targets (LDL-C <70 mg/dL and CRP <2 mg/L) had better clinical outcomes.
From this point of view, it is of extreme interest to understand whether LLTs have an effect also on inflammatory markers and how much this could be related to the lipid-lowering effect of these drugs. Therefore, we aimed to perform a comprehensive evaluation of the anti-inflammatory effect, as determined by the effect on CRP plasma levels of several LLTs [including statins, ezetimibe, omega-3 fatty acids (omega3FAs), fibrates, proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9i), cholesteryl-ester transfer protein inhibitors (CETPi), bempedoic acid], and to assess whether this effect is associated to the reduction of LDL-C or triglycerides (TG) levels.
2. Methods
We conducted a meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines9 (see Supplementary material online, Table S1).
2.1. Study selection and eligibility criteria
Inclusion criteria were: (i) randomized controlled trials (RCTs) in humans, Phase II, III, or IV; (ii) English language and full text available (studies published as abstracts were excluded); (iii) comparing the effect of lipid-lowering drugs to placebo (addition of the same drug to both intervention and control group was acceptable); (iv) reporting the effects on CRP levels; (v) with intervention duration of more than 3 weeks; (vi) and sample size (for both intervention and control group at randomization) over than 100 subjects. Patients with inflammatory diseases and autoimmune diseases were excluded.
All selected articles were independently screened by two researchers, with minor differences resolved by discussion and consultation with a third researcher.
2.2. Search strategy and information sources
PubMed, EMBASE, Web of Science, CENTRAL, and ClinicalTrial.gov were searched from inception to July 2023. The following keywords were combined for literature searches: ‘randomized controlled trials’, ‘C-reactive protein’, ‘statins’, ‘bempedoic acid’, ‘ezetimibe’, ‘omega-3 fatty acids’, ‘fibrates’, ‘PCSK9 inhibitors’, ‘CETP inhibitors’ (searching strategies are shown in detail in Supplementary material online, File S1).
2.3. Data extraction and quality assessment
Two independent investigators extracted the data using a predefined data collection form including the first author; year of publication; country; the number of participants and their main characteristics [e.g. sex, mean age; type of prevention (primary or secondary)]; intervention duration; treatment (name and dosage) and control; mean or median values and variance [standard deviation (SD), standard error (SE), interquartile range (IQR), 95% confidence interval (95% CI), the minimum and maximum values (range), P-value (P)] both at baseline and follow-up or absolute change for CRP, LDL-C and TG concentrations.
Authors were contacted by email to obtain information not available in the published articles.
Quality assessment of the included RCTs was performed using the Jadad scale,10 calculating a score ranging from 0 (very poor) to 13 points (rigorous).
2.4. Data synthesis and statistical analysis
The between-group (treatment-placebo) absolute mean differences in CRP, LDL-C, and TG levels and their 95% CI were calculated for each drug class. CRP was recorded in mg/L, whereas LDL-C and TG were recorded in mg/dL (or converted from mmol/L through dividing by 0.0259 or 0.011311 for LDL-C and TG, respectively). All data were presented as mean and SD. We used median values for CRP and TG since they were not normally distributed, and converted SE, IQR, 95% CI, range, and P (when it was displayed as within-group P and a specific number) to SD by using formulas recommended by the Cochrane Handbook.12 Since the within-group absolute mean difference was computed by subtracting the baseline level from the follow-up level, 0.5 was used as the correlation coefficient to calculate pooled SD within groups.13 For trials that reported variances at baseline but without any information for variances at follow-up, the variances at baseline were also used for follow-up. Multiple intervention groups were combined into a single intervention group when they were compared with only one control group in the trial. Pooled estimates were assessed by using both the fixed-effects and the random-effects models. The generic inverse variance method was used to balance the heterogeneity between studies, and the restricted maximum likelihood estimator was used to estimate the between-study variance.14 When significant heterogeneity was discovered (as determined by Cochrane’s Q test and the I2 statistic,15P < 0.05), the results from the random-effects model were presented.
An influence analysis was conducted by omitting one study at a time, to determine how much a single study influenced the overall results.16 Potential publication bias was visually assessed through funnel plot asymmetry,17 also quantitatively evaluated by Begg’s rank correlation18 and Egger’s weighted regression tests.19
Subgroup analyses were conducted based on the background of patients (primary or secondary prevention, or mixed), and baseline CRP levels [low (<3 mg/L) or high (≥3 mg/L)].
Finally, we performed mixed-effects meta-regression analyses to investigate the potential link between LDL-C or TG absolute change and CRP absolute change, also adjusting for relevant covariates (including age, sex, and intervention duration), for each drug class separately.
All tests were considered statistically significant for P-value <0.05. The analyses and the corresponding graphical visualization of forest and funnel plots were conducted using R (version 4.0.5).
3. Results
3.1. Characteristics of included studies
The flow chart indicating the procedure of literature searching and study screening is shown in Supplementary material online, Figure S1, while a list of excluded trials is provided in Supplementary material online, Table S2. A total of 171 668 subjects from 53 RCTs were included in our meta-analysis (15 RCTs for statins, 9 RCTs for omega3FAs, 8 RCTs for ezetimibe, 7 RCTs for PCSK9i, 6 RCTs for fibrates and CETPi, and 5 RCTs for bempedoic acid). Table 1 and Supplementary material online, Table S3 summarize the main characteristics of included studies. Sample sizes of the included studies ranged from 200 to 26 145 participants. The intervention duration ranged between 1.5 and 60 months. All studies were shown in high methodological quality, with the Jadad score ranging from 8 to 13 points (see Supplementary material online, Table S4).
Table 1.
Characteristics of the 53 trials included in the analysis
| Trial name | Year published | Primary or secondary prevention | Experimental group | Control group | Intervention duration (months) | Baseline CRP levels (mg/L) | ||
|---|---|---|---|---|---|---|---|---|
| N | Intervention | N | Intervention | |||||
| Statins | ||||||||
| CARE | 1999 | Secondary | 258 | Pravastatin 40 mg | 214 | Placebo | 60 | 2.30 |
| AFCAPS/TexCaps | 2001 | Primary | 2885 | Lovastatin 20–40 mg | 2834 | Placebo | 12 | 1.60 |
| PRINCE | 2001 | Primary | 865 | Pravastatin 40 mg | 837 | Placebo | 6 | 2.00 |
| MIRACL | 2003 | Secondary | 1186 | Atorvastatin 80 mg | 1216 | Placebo | 4 | 11.50 |
| Athyros et al. (2005) | 2005 | Primary | 100 | Atorvastatin 20 mg + fenofibrate 200 mg | 100 | Fenofibrate 200 mg | 12 | 4.50 |
| DIACOR | 2006 | Primary | 100 | Simvastatin 20 mg + fenofibrate 160 mg | 100 | Fenofibrate 160 mg | 3 | 2.24 |
| 4D | 2008 | Mixed | 539 | Atorvastatin 20 mg | 544 | Placebo | 6 | 5.80 |
| GISSI-HF | 2008 | Secondary | 336 | Rosuvastatin 10 mg | 314 | Placebo | 3 | 2.68 |
| JUPITER | 2008 | Primary | 8901 | Rosuvastatin 20 mg | 8901 | Placebo | 12 | 4.20 |
| AURORA | 2009 | Mixed | 1389 | Rosuvastatin 10 mg | 1384 | Placebo | 3 | 4.80 |
| CORONA(1) | 2009 | Secondary | 777 | Rosuvastatin 10 mg | 779 | Placebo | 3 | 1.10 |
| CORONA(2) | 2009 | Secondary | 1711 | Rosuvastatin 10 mg | 1694 | Placebo | 3 | 5.50 |
| ASTRONOMER | 2010 | Primary | 134 | Rosuvastatin 40 mg | 135 | Placebo | 3 | 1.60 |
| CARDS | 2015 | Primary | 1174 | Atorvastatin 10 mg | 1148 | Placebo | 12 | 1.30 |
| LIPID | 2015 | Secondary | 3854 | Pravastatin 40 mg | 3889 | Placebo | 12 | 2.47 |
| HOPE-3 | 2016 | Primary | 785 | Rosuvastatin 10 mg | 769 | Placebo | 36 | 3.60 |
| Bempedoic acid | ||||||||
| CLEAR harmony | 2019 | Mixed | 1421 | Bempedoic acid 180 mg | 724 | Placebo | 3 | 1.49 |
| CLEAR serenity | 2019 | Mixed | 218 | Bempedoic acid 180 mg | 103 | Placebo | 3 | 2.92 |
| CLEAR wisdom | 2019 | Mixed | 467 | Bempedoic acid 180 mg | 240 | Placebo | 3 | 1.61 |
| Ballantyne et al. (2020)—BA | 2020 | Mixed | 101 | Bempedoic acid 180 mg | 52 | Placebo | 3 | 2.95 |
| Ballantyne et al. (2020)—BA + EZE | 2020 | Mixed | 102 | Bempedoic acid + ezetimibe 10 mg | 102 | Ezetimibe 10 mg | 3 | 3.12 |
| CLEAR outcomes | 2023 | Primary | 2100 | Bempedoic acid 180 mg | 2106 | Placebo | 12 | 2.39 |
| Ezetimibe | ||||||||
| ENHANCE | 2008 | Mixed | 357 | Ezetimibe 10 mg + simvastatin 80 mg | 363 | Simvastatin 80 mg | 24 | 1.70 |
| Kouvelos et al. (2013) | 2013 | Mixed | 126 | Ezetimibe 10 mg + rosuvastatin 10 mg | 136 | Rosuvastatin 10 mg | 12 | 3.15 |
| IMPROVE-IT | 2015 | Secondary | 6954 | Ezetimibe 10 mg + simvastatin 40 mg | 7019 | Simvastatin 40 mg | 12 | 9.60 |
| PRECISE-IVUS | 2015 | Secondary | 100 | Ezetimibe 10 mg + atorvastatin | 102 | Atorvastatin | 10 | 3.00 |
| CuVIC | 2017 | Secondary | 109 | Ezetimibe 10 mg + statins | 112 | Statins | 6 | 4.46 |
| HIJ-PROPER | 2017 | Secondary | 673 | Ezetimibe 10 mg + pitavastatin 2 mg | 691 | Pitavastatin 2 mg | 12 | 9.20 |
| I-ROSETTE | 2018 | Mixed | 195 | Ezetimibe 10 mg + rosuvastatin 5/10/20 mg | 194 | Rosuvastatin 5/10/20 mg | 2 | 0.70 |
| Ballantyne et al. (2020)—EZE | 2020 | Mixed | 102 | Ezetimibe 10 mg | 52 | Placebo | 3 | 3.03 |
| Ballantyne et al. (2020)—EZE + BA | 2020 | Mixed | 102 | Ezetimibe 10 mg + bempedoic acid 180 mg | 101 | Bempedoic acid 180 mg | 3 | 3.12 |
| Omega-3 fatty acids | ||||||||
| GISSI-HF | 2008 | Secondary | 551 | EPA/DHA 1 g | 559 | Placebo | 36 | 2.39 |
| DO IT | 2009 | Mixed | 247 | EPA/DHA 2.4 g | 239 | Placebo | 36 | 3.58 |
| ANCHOR | 2012 | Mixed | 444 | E-EPA 2/4 g | 219 | Placebo | 3 | 2.05 |
| ALPHA OMEGA | 2014 | Secondary | 601 | EPA/DHA 0.4 g | 609 | Placebo | 40 | 1.46 |
| ESPRIT | 2015 | Secondary | 416 | OM3-CA 2/4 g | 211 | Placebo | 1.5 | 4.05 |
| HEARTS | 2017 | Secondary | 129 | EPA/DHA 3.36 g | 111 | Placebo | 30 | 0.90 |
| VITAL | 2019 | Primary | 1644 | EPA/DHA 1 g | 1636 | Placebo | 48 | 1.60 |
| STRENGTH | 2020 | Mixed | 1467 | OM3-CA 4 g | 1499 | Placebo | 12 | 2.10 |
| REDUCE-IT | 2022 | Mixed | 3322 | E-EPA 4 g | 3229 | Placebo | 24 | 2.18 |
| Fibrates | ||||||||
| Athyros et al. (2005) | 2005 | Primary | 100 | Fenofibrate 200 mg + atorvastatin 20 mg | 100 | Atorvastatin 20 mg | 12 | 4.50 |
| DIACOR | 2006 | Primary | 100 | Fenofibrate 160 mg + simvastatin 20 mg | 100 | Simvastatin 20 mg | 3 | 2.24 |
| Zhu et al. (2006) | 2006 | Primary | 115 | Fenofibrate 160 mg + hypotensive agents | 110 | Hypotensive agents | 24 | 6.73 |
| BIP | 2007 | Secondary | 1319 | Bezafibrate 400 mg | 1297 | Placebo | 24 | 3.40 |
| DAIS | 2016 | Mixed | 108 | Fenofibrate 200 mg | 96 | Placebo | 36 | 1.80 |
| Ihm et al. (2020) | 2020 | Mixed | 174 | Fenofibrate 160 mg + pitavastatin 2 mg | 173 | Pitavastatin 2 mg | 2 | 7.00 |
| PCSK9 inhibitors | ||||||||
| DESCARTES | 2014 | Mixed | 535 | Evolocumab 420 mg | 276 | Placebo | 13 | 1.00 |
| RUTHERFORD-2 | 2015 | Mixed | 210 | Evolocumab 140 or 420 mg | 101 | Placebo | 3 | 1.01 |
| GLAGOV | 2016 | Secondary | 484 | Evolocumab 420 mg | 484 | Placebo | 19 | 1.60 |
| FOURIER | 2018 | Secondary | 13 091 | Evolocumab 140 or 420 mg | 13 054 | Placebo | 12 | 1.70 |
| SPIRE-1 and 2 | 2018 | Mixed | 9738 | Bococizumab 150 mg | 9785 | Placebo | 3.5 | 1.88 |
| EVOPACS | 2019 | Secondary | 141 | Evolocumab 420 mg | 150 | Placebo | 2 | 6.68 |
| PACMAN-AMI | 2022 | Secondary | 126 | Alirocumab 150 mg | 132 | Placebo | 13 | 6.40 |
| CETP inhibitors | ||||||||
| ILLUMINATE | 2007 | Mixed | 7533 | Torcetrapib 60 mg | 7534 | Placebo | 3 | 1.30 |
| ILLUSTRATE | 2007 | Secondary | 464 | Torcetrapib 60 mg | 446 | Placebo | 24 | 2.10 |
| RADIANCE 1 | 2007 | Mixed | 423 | Torcetrapib 60 mg | 427 | Placebo | 24 | 0.80 |
| DEFINE | 2010 | Mixed | 779 | Anacetrapib 100 mg | 773 | Placebo | 6 | 1.40 |
| dal-VESSEL | 2012 | Mixed | 206 | Dalcetrapib 600 mg | 209 | Placebo | 9 | 2.65 |
| ACCELERATE | 2017 | Secondary | 4558 | Evacetrapib 130 mg | 4565 | Placebo | 3 | 1.52 |
DHA, docosahexaenoic acid; EPA, eicosapentaenoic acid; E-EPA, eicosapentaenoic acid ethyl ester; OM3-CA, omega-3 carboxylic acid.
3.2. Meta-analysis results
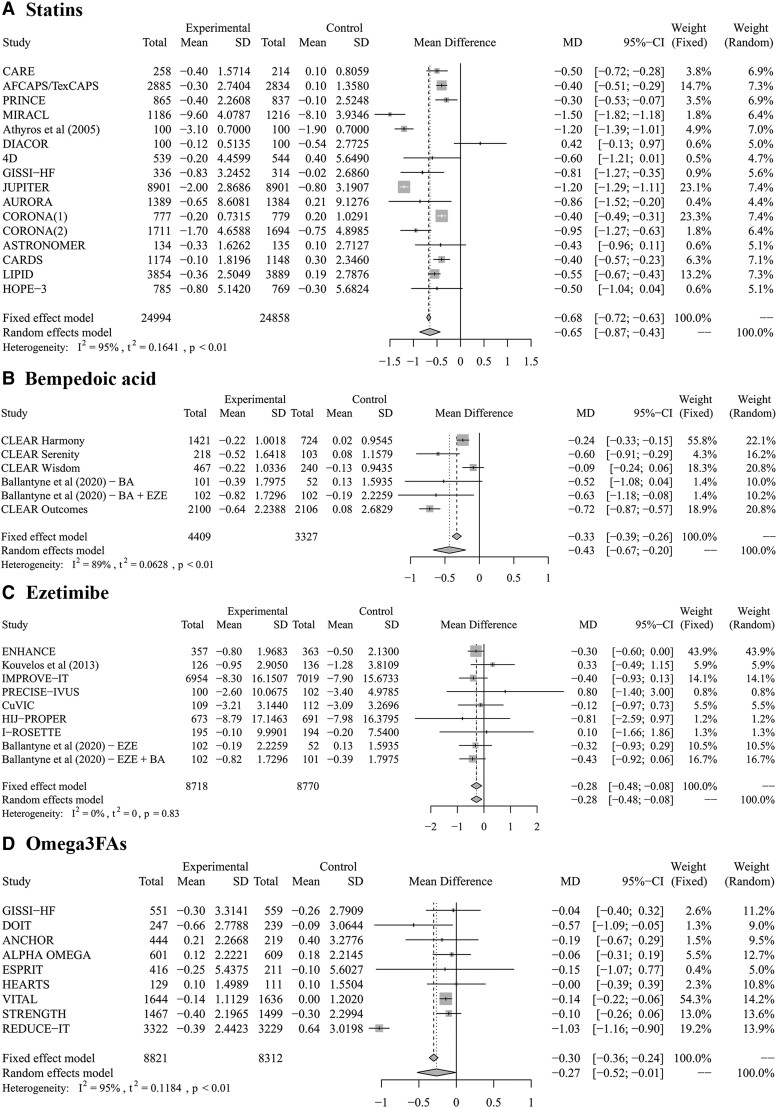
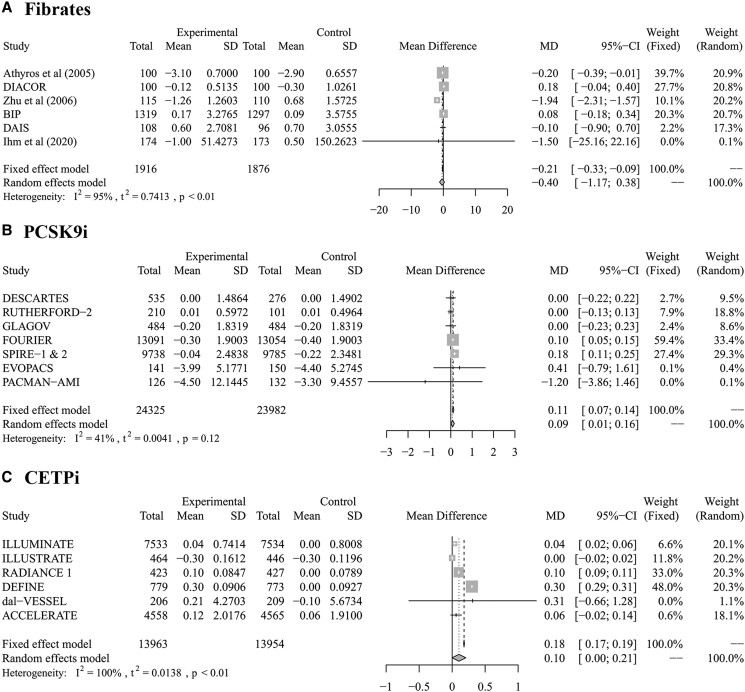
The different effects on CRP concentration among LLTs are shown in Figures 1 and 2. An additional −0.65 mg/L (−0.87 to −0.43) absolute reduction of CRP concentration was observed with statins compared with the placebo group. Bempedoic acid showed a considerable lowering effect on CRP levels as well [−0.43 mg/L (−0.67 to −0.20)]. CRP was also reduced by −0.28 mg/L (−0.48 to −0.08) in the ezetimibe-combined treatment group compared with the single-statin treatment group. A similar absolute decrease was obtained with omega3FAs [−0.27 mg/L (−0.52 to −0.01)] compared with placebo. In addition, a −0.40 mg/L (−1.17 to 0.38) lowering in CRP level was observed in patients treated with fibrates, although not statistically significant. PCSK9i [0.11 mg/L (0.07–0.14)] and CETPi [0.10 mg/L (0.00–0.21)] both showed a small rise in CRP levels; however, the latter was not statistically significant.
Figure 1.
Forest plots indicate the significant lowering effect on CRP levels caused by statins (A), bempedoic acid (B), ezetimibe (C), and omega3FAs (D). The trials are sorted by published year. The pooled estimate and 95% CIs were represented by the centre line and lateral tips of the diamond and shown in absolute mean differences (mg/L). CI, confidence interval; MD, mean difference; SD, standard deviation.
Figure 2.
Forest plots indicate the not significant lowering or increasing effect on CRP levels related to fibrates (A), PCSK9 inhibitors (B), and CETPi (C). The trials are sorted by published year. The pooled estimate and 95% CIs were represented by the centre line and lateral tips of the diamond and shown in absolute mean differences (mg/L). CI, confidence interval; MD, mean difference; SD, standard deviation.
Supplementary material online, Figures S2 and S3 report the pooled analyses on absolute differences in LDL-C and TG levels, respectively. LDL-C concentration was markedly reduced by PCSK9i [−61.98 mg/dL (−73.53 to −50.42) and statins −48.37 mg/dL (−55.71 to −41.03)]. Bempedoic acid, ezetimibe, and CETPi reduced LDL-C levels by −25.04 mg/dL (−30.96 to −19.12), −22.09 mg/dL (−30.10 to −14.08) and −21.90 mg/dL (−30.19 to −13.61), respectively. A slight decrease in LDL-C was shown with fibrates [−5.56 mg/dL (−10.38 to −0.75)], while the change of LDL-C with omega-3FAs was not significant [−0.96 mg/dL (−3.84 to 1.92)]. All these LLTs significantly reduced TG levels from −10.58 mg/dL (−12.40 to −8.76) with ezetimibe to −53.55 mg/dL (−78.91 to −28.20) with fibrates, except for bempedoic acid [0.61 mg/dL (−1.64 to 2.86)].
No publication bias was found when evaluating funnel plot asymmetry through quantitative analysis (Begg’s rank correlation and Egger’s linear regression tests) for each outcome (see Supplementary material online, Figures S4–S6 and Table S5).
Influence analyses illustrated that no appreciable impact on pooled estimates for CRP concentration was observed omitting one study at a time for statin, bempedoic acid, ezetimibe, or fibrate trials, respectively. However, the effect on CRP levels caused by omega3FAs became smaller but still statistically significant after removing the REDUCE-IT trial [−0.13 mg/L (−0.19 to −0.06)]. The increase in CRP level caused by PCSK9i became not statistically significant after removing FOURIER [0.07 mg/L (−0.04 to 0.18)] or SPIRE-1 and 2 [0.06 mg/L (−0.01 to 0.13)], while the increase in CRP level caused by CETPi turned out to be statistically significant after removing ILLUSTRATE trial [0.13 mg/L (0.01–0.25)] (see Supplementary material online, Figures S7 and S8).
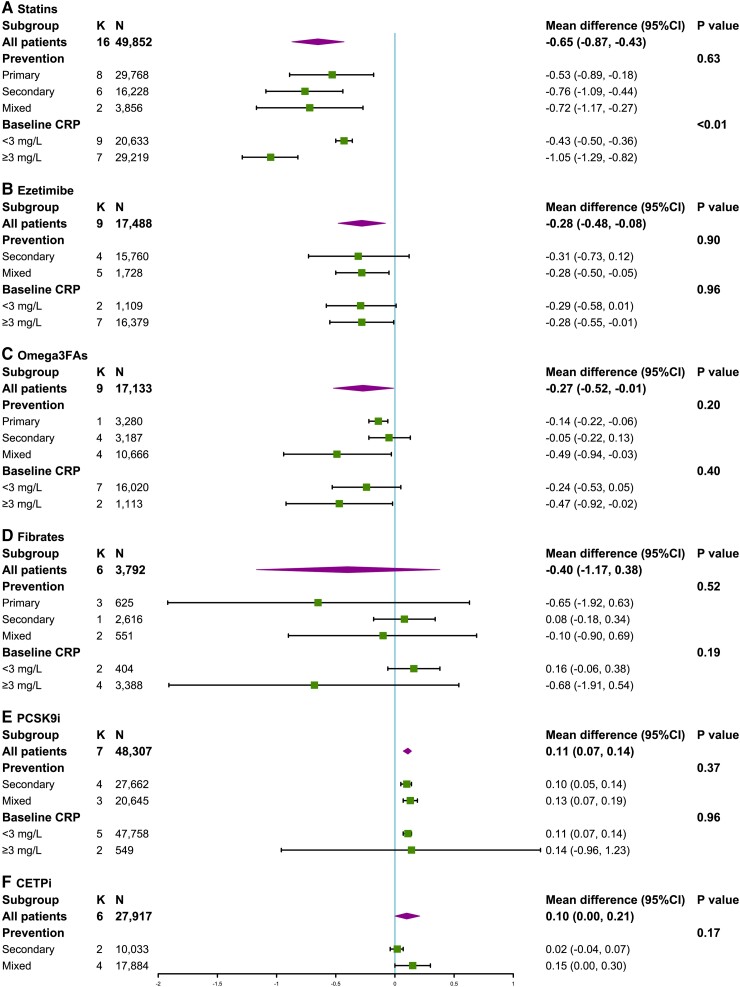
3.3. Subgroup analyses
For statins, subgroup analyses illustrated a slight difference in CRP reduction between patients in primary or secondary prevention [−0.53 mg/L (−0.89 to −0.18) vs. −0.76 mg/L (−1.09 to −0.44), respectively], albeit not statistically significant (P = 0.63). After statins therapy, the decrease in CRP level in the group of participants with higher CRP levels at baseline was greater than the reduction in subjects with a baseline CRP level of <3 mg/L [−1.05 mg/L (−1.29 to −0.82) vs. −0.43 mg/L (−0.50 to −0.36); P < 0.01].
For omega3FAs, subgroup analyses discovered little difference in CRP lowering among patients in primary or secondary prevention and patients with low or high CRP levels at baseline, but none of them were statistically significant. Similar results were also found for ezetimibe, fibrates, and PCSK9i.
Additionally, subgroup analysis of CETPi failed to show a statistically significant difference between trials involving only patients in secondary prevention and trials involving patients either in primary or secondary prevention (P = 0.17). All these data are shown in Figure 3.
Figure 3.
Forest plots illustrate the different changes in CRP levels among patients in primary CV prevention, secondary CV prevention, or mixed, and patients with low (<3 mg/L) or high (≥3 mg/L) CRP levels at baseline in each drug class. The results are shown in absolute change (mg/L). Only LLTs with more than one trial in at least two subgroups were subjected to subgroup analysis (bempedoic acid was not eligible). CETPi were not included in the subgroup analysis by baseline CRP levels as in all the trials patients had a baseline CRP <3 mg/L. CI, confidence interval; K, number of included trials; N, number of participants.
3.4. Meta-regression analysis
Among LLTs with a significant effect on CRP levels, mixed-effects meta-regression did not show a significant correlation between changes in CRP and LDL-C levels or between changes in CRP and TG levels even after adjustment by age, sex, and intervention duration, except for omega3FAs (slope for the adjusted model: 0.0879, P < 0.0001, Supplementary material online, Table S6, and slope for the adjusted model: 0.0371, P < 0.0001, Supplementary material online, Table S7). However, when the REDUCE-IT trial was removed from the meta-regression analyses, both the correlations became not statistically significant (data not shown).
4. Discussion
Atherosclerosis is now considered to be primarily a progressive inflammatory disease. As some reports suggested modulating effects on inflammatory markers by LLTs, we systematically evaluated evidence in literature and conducted the largest, most comprehensive, and up-to-date meta-analysis (53 RCTs) on the effect of LLTs on CRP, in addition to lipid reduction. The results from our meta-analysis indicate statins, bempedoic acid, ezetimibe, and omega3FAs as the drugs with a significant impact on lowering CRP levels.
Statins thus emerge as the class with the largest anti-inflammatory effect, leading to an additional −0.65 mg/L absolute decrease of CRP concentrations (−17.31% from CRP value of ∼3.75 mg/L at baseline in the 15 included trials) compared with the placebo group. The reduction was even more marked in the pooled analysis of trials with higher CRP levels at baseline. CRP levels in the MIRACL trial20 including patients with acute coronary syndrome (ACS) were reported to be 11.25 mg/L at baseline and to have been reduced by 1.50 mg/L (−13.33%). However, we did not observe a significant change in our results after deleting this trial, according to the influence analysis (see Supplementary material online, Figure S7). Similarly, the CRP decreased by 1.18 mg/L from 4.47 mg/L at baseline when we combined the data from the JUPITER21 and CORONA(2)22 studies, which only included patients with baseline CRP of 2 mg/L or above. The result became −0.58 mg/L (−0.81 to −0.35) from 3.59 mg/L at baseline (−16.16%) after removing these two trials. This effect has already been suggested by a previously published meta-analysis,23 in which the CRP reduction observed in the pooled analysis of statin-only trials was comparable. In the recent meta-analysis by Kandelouei et al.24 on more than 40 studies, statins reduced the serum levels of CRP [−0.97 mg/L (95% CI −1.26 to −0.68)] in patients with CVD. This effect of statins has also been discussed to rely upon mechanisms beyond lipid control in CV prevention. The review by Lv et al.25 reported that statins can attenuate disease activity markedly in patients with rheumatoid arthritis, with CRP declining significantly during the treatment. It was also suggested that the greater effect occurred in patients with higher baseline CRP levels. Horiuchi et al.26 in 2010 showed that statin therapy reduced inflammatory markers in hypercholesterolaemic patients, with anti-inflammatory activity limited to subjects with elevated inflammatory markers at baseline.
Asher et al.27 clearly illustrated that clinical trials with statins demonstrated a decrease in CRP levels of up to −43%,28 but the relative reductions in CRP levels appear to be independent of the magnitude of LDL-C lowering; indeed, statin trials that produced similar LDL-C reductions showed heterogenous changes in CRP levels. Similarly, in our meta-regression, we failed to find an association between reductions in LDL-C and changes in CRP levels with this drug class.
Statins have been reported to exert in vitro properties that may contribute to a direct protective influence on the arterial wall in vivo,29 and these pleiotropic properties appear to be derived from the inhibition of isoprenylation of the Rho kinase pathway.30 Other hypothesized mechanisms for statin-mediated CRP reduction include a decrease in monocyte expression of inflammatory cytokines and in turn a downregulation of CRP gene transcription.31 An in vivo study provided evidence for a direct activating effect of statins of the peroxisome proliferator-activated receptor (PPARα) and downstream suppressive effect on CRP gene expression independent of cholesterol lowering.32 Another in vitro study further demonstrated that statins could inhibit protein geranylgeranylation, reduce the IL-6-induced phosphorylation of signal transducer and activator of transcription 3 in hepatocytes, and eventually decrease CRP gene expression.33
CRP levels were also reduced in response to bempedoic acid treatment, resulting in a −0.43 mg/L absolute decrease (−20.02% from baseline CRP value of ∼2.15 mg/L) compared with the placebo. Our pooled results are consistent with a secondary biomarker analysis of the CLEAR harmony trial on patients with known atherosclerotic disease and residual inflammatory risk (defined as a baseline CRP ≥2 mg/L), showing a −26.5% (95% CI −34.8 to −18.4) reduction for CRP that was not correlated with bempedoic acid-associated lipid changes.34 Bempedoic acid is a new hypolipidemic drug blocking the ATP citrate lyase enzyme, which in turn inhibits cholesterol synthesis through the same biosynthetic pathway as statins do. In addition, it targets the AMP-activated protein kinase pathway, resulting in strong anti-inflammatory effects proven by both in vivo35,36 and in vitro37,38 studies. In a previously published meta-analysis of seven RCTs, patients treated with bempedoic acid compared with placebo experienced a −13.2% (95% CI −16.7 to −9.79%) decrease in CRP levels.39
The other drug showing a significant effect in CRP lowering was ezetimibe, with a −0.28 mg/L decrease in the ezetimibe-combined treatment group compared with the single-statin treatment group (−3.19% reduction). It has to be acknowledged that the baseline CRP values in ezetimibe trials included in our analysis were much higher (∼8.77 mg/L) than trials with other lipid-lowering drugs, and this was due to the inclusion of the IMPROVE-IT8 and HIJ-PROPER40 trials, the former on 18 144 patients stabilized after ACS (median CRP at randomization 10.2 mg/L, measured as mean of 5 days after presentation with ACS), and the latter on 1734 patients hospitalized for ST-segment elevation myocardial infarction or non-ST-segment elevation myocardial infarction or unstable angina within 72 h before randomization (median CRP at baseline 9.00 mg/L). Importantly, when we performed a sensitivity analysis omitting these two trials, the main results were confirmed [−0.26 mg/L (95% CI −0.47 to −0.04) with baseline CRP of 2.39 mg/L, −10.88%]. Combining these two trials, the CRP was reduced by −0.43 mg/L from 9.50 mg/L at baseline (−6.35%).
The pooled analyses by Pearson et al.41 (six trials on ezetimibe as monotherapy and seven trials as an add-on to baseline statin therapy), confirmed the reduction in CRP both by ezetimibe monotherapy (−6% from a baseline of 2.5 mg/L, P = 0.09) and when added to statin therapy (−10% from a baseline of 2.7 mg/L, P < 0.001). However, other studies showed that ezetimibe alone did not modify CRP.42,43
The meta-analysis on omega3FAs also showed a considerable effect in reducing CRP levels [−0.27 mg/L (95% CI −0.52 to −0.01) compared with placebo]. For this drug class, there is a strong pre-clinical evidence base demonstrating the efficacy of omega3FAs for ameliorating inflammation and thereby reducing disease burden, but clinical trials have not provided compelling evidence that omega-3 supplementation reduces established inflammation.44,45 Recently, an umbrella meta-analysis46 on 32 eligible meta-analyses conducted from 2012 to 2021 reported a significant effect [effect size: −0.40 (95% CI −0.56 to −0.24), P < 0.001].
Different mechanisms have been proposed for the possible impacts of n−3 polyunsaturated fatty acids (PUFAs) on inflammation:47n−3 PUFAs can affect innate and adaptive immune system responses,48 act as the natural agonists of PPARα,49 or replace arachidonic acid in the cell membrane.50 Notably, in our analysis, this reduction was less evident [−0.13 mg/L (95% CI −0.19 to −0.06)] in the sensitivity analysis where the REDUCE-IT trial was excluded. REDUCE-IT51 randomly allocated 8179 statin-treated patients with triglyceride levels >135 and <500 mg/dL to treatment with 2 g twice daily of icosapent ethyl or a comparator (mineral oil). The levels of biomarkers associated with atherosclerosis increased over time among those allocated to the comparator (+21.95% for CRP at 12 months), while in the icosapent ethyl group, there were minimal changes (−1.03 mg/L). This led to the hypothesis that part of the net clinical benefit observed with icosapent ethyl might have been a consequence of adverse biomarker effects attributable to mineral oil. The result is smaller but still significant once we nulled the inflammatory effect of mineral oil (i) defining the CRP change in the placebo group as 0 [−0.18 mg/L (95% CI −0.29 to −0.06)]; (ii) considering the CRP change in the placebo group as the mean of changes in placebo arms across all omega3FA trials [−0.17 mg/L (95% CI −0.23 to −0.11)]; (iii) using the effect of corn oil in the STRENGTH trial52 as control value [−0.12 mg/L (95% CI −0.18 to −0.06)].
Our meta-analysis also showed that the effect of fibrates on CRP was limited as they showed an only marginal, nonsignificant reduction of CRP levels. The influence analysis highlighted that this reduction was mainly driven by the study by Zhu et al., as excluding this trial in the influence analysis, the effect became null [0.00 mg/L (95% CI −0.21 to 0.22)]. In this trial, 594 enrolled patients with essential hypertension were randomized to 160 mg of micronized fenofibrate daily in combination with hypotensive agents or to hypotensive therapy alone. Treatment with micronized fenofibrate in combination with antihypertensive agents for 24 months showed a significant lipid-lowering and anti-inflammatory effect [CRP, mean (SD), from 6.73 (1.38) to 5.47 (1.09) mg/L]. In the meta-analysis by Hao et al.53 on 16 RCTs, treatment with fibrates significantly decreased CRP concentrations [weighted mean difference: 0.47 mg/L (95% CI −0.93 to −0.01)]. The possible mechanism is under debate.54 In patients with metabolic syndrome, fibrates were shown to reduce CRP independent of lipid-lowering effects,55 suggesting that PPARα mediated the effect of fenofibrate could have a direct effect on the inflammation pathway. Evidence in vivo showed that changes in CRP with fenofibrate were significantly and inversely associated with changes in adiponectin.56
PCSK9i and CETPi showed a slight or null effect on CRP levels, as already reported.57–59 Our findings were consistent with results from a recent meta-analysis60 reporting that PCSK9i had no significant impact on circulating CRP levels irrespective of PCSK9-monoclonal antibody types, participant characteristics, and treatment duration. Interestingly, the analysis stratified by treatment also showed no differential effect with PCSK9i as monotherapy [0.00 mg/L (95% CI −0.08 to 0.07)] or combination therapy [−0.08 mg/L (95% CI −0.37 to 0.21)], with meta-regression confirming no significant linear correlation with LDL-C reduction. This effect, when compared with that of statins within the context of the two drug classes’ ability to reduce LDL-C, aligns with the evidence found in the literature and is further confirmed by our meta-regression analysis. In other words, it underscores that the reduction of CRP is not correlated with the LDL-C reduction. It is worth noting, however, that the design of the included trials for these two treatments frequently containing a run-in phase with statin therapy, which is known to alleviate vascular inflammation. Taking this, both the low CRP levels at baseline and the lack of reduction in this biomarker after treatment could be partially explained, making further investigation necessary.
CRP is the classical acute-phase response protein, with its role in atherosclerotic plaque formation and progression of atherosclerosis is long debated.61 Although Mendelian randomization studies refuted the causal association between CRP and the risk of CV events,5 elevated CRP concentrations have been consistently associated with CVD,62,63 indicating that CRP may be rather a marker than a mediator of CVD risk. Even if CRP has demonstrated value as a predictor of CV risk, it remains yet unclear whether targeting CRP levels improves CV outcomes. The risk of CV events was significantly lower among individuals treated with colchicine (an anti-inflammatory drug) compared with placebo, according to the COLCOT64 and LoCoDo265 trials. Canakinumab, a monoclonal antibody against IL-1β evaluated in the trial CANTOS,66 was shown to reduce the risk of secondary CV events, providing conclusive evidence that targeting the inflammatory processes of atherosclerosis alone improves CV outcomes. On the other hand, a recent meta-analysis on 15 RTCs that measured CRP before and after administration of therapies for CVD and measured incidence of CV events found that a greater magnitude of CRP reduction was not associated with better clinical outcomes, as improvements in clinical outcomes were largely accounted for by reduction in LDL-C.67 Authors clearly stated that targeting CRP does not offer additional benefit over targeting LDL-C across the general population in terms of CV risk reduction, as confirmed by other studies in literature.68,69 However, there is value in targeting CRP in patients at high residual inflammatory risk despite non-elevated lipid levels.4 Indeed, a recently published study showed that among patients receiving statins, inflammation assessed by high-sensitivity CRP was a stronger predictor for risk of future CV events and death than LDL-C.70 In September 2023, the use of low-dose (0.5 mg) colchicine had been approved in the US in patients with ASCVD. Meta-analyses illustrated that low-dose colchicine (0.5–1.0 mg) could reduce CRP by −0.36 mg/L [95% CI (−0.51 to −0.20)] in patients with CAD71 and by −0.66 mg/L [95% CI (−0.98 to −0.35)] in patients post MI,72 translating into a 35% [odds ratio 0.65 (95% CI 0.51–0.83)] and 44% [risk ratio 0.56 (95% CI 0.48–0.67)] reduction in major CV events, respectively.
5. Strengths and limitations
Our meta-analysis is a comprehensive and updated evaluation of seven main LLTs, counting 171 668 participants in a total of 53 trials. To the best of our knowledge, this is the first comprehensive meta-analysis to illustrate the absolute changes in CRP across several lipid-lowering drugs, including unpublished data, directly provided by authors. In addition, by converting absolute changes into percentage changes, we eliminated the influence of the baseline values on the absolute changes and got a clearer picture of the extent to which the various LLTs have an impact on CRP reduction. However, some limitations exist. First, there were always some dropouts at follow-up, in this case, CRP and lipids may not have been measured for the same sample. Second, the small number of trials included for bempedoic acid and CETPi prevented conducting all the sub-analyses that could lead to more robust and reliable results. Third, we could not obtain the required data from authors of some RCTs reporting CRP levels (see Supplementary material online, Table S8), which may influence the results.
6. Conclusions
Among LLTs, statins, bempedoic acid, ezetimibe, and omega3FAs reduced serum CRP concentration, independently of LDL-C or TG changes. The CRP reduction seems to be greater in some specific groups of patients, mainly those with high CRP levels at baseline. While it is evident that the reduction in CV risk is primarily linked to the decrease in LDL-C levels, the existence of a remaining CV risk attributed to an underlying inflammatory condition could influence the selection of the hypolipidaemic therapy among those having an equivalent effect on LDL-C reduction.
Further investigation is required to clearly demonstrate how this potential anti-inflammatory action may influence CV protection, and whether new therapies targeting inflammation pathways (such as the recently approved colchicine) could be added to lipid treatment and used to help reduce CV risk in selected groups of individuals.
Supplementary material
Supplementary material is available at Cardiovascular Research online.
Supplementary Material
Acknowledgements
The authors thank the members of the META-LIPID Group who provided unpublished data: Christoph Wanner (for 4D trial), Salim Yusuf (for HOPE-3 trial), Aldo Maggioni (for GISSI-HF trial), Adrienne Kirby (for LIPID trial), Hiroshi Ogawa (for HIJ-PROPER trial), Ellen K. Hoogeveen (for ALPHA OMEGA trial), Ingebjørg Seljeflot (for DOIT trial), Francine K. Welty (for HEARTS trial), Michal Benderly (for BIP trial), JoAnn E. Manson (for VITAL trial), Kathy Wolski (for ACCELERATE trial), Christopher P. Cannon (for DEFINE trial), Frederick J. Raal (for RUTHERFORD-2 trial), David Kallend (for dal-VESSEL trial), JoAnne Foody and Michael Louie (for bempedoic acid trials). For additional information please see the Supplementary material online, File S2.
Contributor Information
Sining Xie, Epidemiology and Preventive Pharmacology Service (SEFAP), Department of Pharmacological and Biomolecular Sciences, University of Milan, via Balzaretti 9, 20033 Milan, Italy.
Federica Galimberti, IRCCS MultiMedica, via Milanese 300, 20099 Sesto San Giovanni (Milan), Italy.
Elena Olmastroni, Epidemiology and Preventive Pharmacology Service (SEFAP), Department of Pharmacological and Biomolecular Sciences, University of Milan, via Balzaretti 9, 20033 Milan, Italy; IRCCS MultiMedica, via Milanese 300, 20099 Sesto San Giovanni (Milan), Italy.
Thomas F Luscher, Center for Molecular Cardiology, University Zurich, Wagistrasse 12, 8952 Schlieren (Zurich), Switzerland; Cardiac Unit, Royal Brompton and Harefield Hospitals GSTT, Imperial College and King’s College London, Sydney Street, SW3 6NP London, UK.
Stefano Carugo, Department of Clinical Sciences and Community Health, University of Milan, via della Commenda 19, 20122 Milan, Italy; Cardiology Unit, Department of Internal Medicine, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico of Milan, via Francesco Sforza 28, 20122 Milan, Italy.
Alberico L Catapano, Epidemiology and Preventive Pharmacology Service (SEFAP), Department of Pharmacological and Biomolecular Sciences, University of Milan, via Balzaretti 9, 20033 Milan, Italy; IRCCS MultiMedica, via Milanese 300, 20099 Sesto San Giovanni (Milan), Italy.
Manuela Casula, Epidemiology and Preventive Pharmacology Service (SEFAP), Department of Pharmacological and Biomolecular Sciences, University of Milan, via Balzaretti 9, 20033 Milan, Italy; IRCCS MultiMedica, via Milanese 300, 20099 Sesto San Giovanni (Milan), Italy.
META-LIPID Group:
Alberico L Catapano, Manuela Casula, Federica Galimberti, Elena Olmastroni, Sining Xie, Christoph Wanner, Salim Yusuf, Aldo Maggioni, Adrienne Kirby, Hiroshi Ogawa, Ellen K Hoogeveen, Ingebjørg Seljeflot, Francine K Welty, Michal Benderly, JoAnn E Manson, Kathy Wolski, Christopher P Cannon, Frederick J Raal, David Kallend, JoAnne Foody, and Michael Louie
Funding
No funding was received for this project. The work of Manuela Casula has been supported by Ministero della salute italiano - IRCCS MultiMedica GR-2016-02361198. The work of A.L.C. has been supported by Ministero della salute italiano - IRCCS MultiMedica RF-2019-12370896, SISA Lombardia, and Fondazione SISA. The work of A.L.C., M.C., and F.G. has been also supported by Ministero della salute italiano - Ricerca Corrente - IRCCS MultiMedica.
Data availability
The data underlying this study are derived from published articles (available in the main text or in the supplementary materials), or unpublished data directly provided by the authors (this data will be shared on request to the corresponding author with permission of the original article's authors).
References
- 1. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, Chapman MJ, De Backer GG, Delgado V, Ference BA, Graham IM, Halliday A, Landmesser U, Mihaylova B, Pedersen TR, Riccardi G, Richter DJ, Sabatine MS, Taskinen MR, Tokgozoglu L, Wiklund O; ESC Scientific Document Group . 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J 2020;41:111–188. [DOI] [PubMed] [Google Scholar]
- 2. Ridker PM. How common is residual inflammatory risk? Circ Res 2017;120:617–619. [DOI] [PubMed] [Google Scholar]
- 3. Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005;352:1685–1695. [DOI] [PubMed] [Google Scholar]
- 4. Aday AW, Ridker PM. Targeting residual inflammatory risk: a shifting paradigm for atherosclerotic disease. Front Cardiovasc Med 2019;6:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zacho J, Tybjærg-Hansen A, Jensen JS, Grande P, Sillesen H, Nordestgaard BG. Genetically elevated C-reactive protein and ischemic vascular disease. N Engl J Med 2008;359:1897–1908. [DOI] [PubMed] [Google Scholar]
- 6. Ballantyne CM. Clinical Lipidology: A Companion to Braunwald’s Heart Disease. 2nd ed. Houston, TX: Elsevier; 2014. p138. [Google Scholar]
- 7. Ridker PM, Cannon CP, Morrow D, Rifai N, Rose LM, McCabe CH, Pfeffer MA, Braunwald E; Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 (PROVE IT-TIMI 22) Investigators . C-reactive protein levels and outcomes after statin therapy. N Engl J Med 2005;352:20–28. [DOI] [PubMed] [Google Scholar]
- 8. Bohula EA, Giugliano RP, Cannon CP, Zhou J, Murphy SA, White JA, Tershakovec AM, Blazing MA, Braunwald E. Achievement of dual low-density lipoprotein cholesterol and high-sensitivity C-reactive protein targets more frequent with the addition of ezetimibe to simvastatin and associated with better outcomes in IMPROVE-IT. Circulation 2015;132:1224–1233. [DOI] [PubMed] [Google Scholar]
- 9. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–12. [DOI] [PubMed] [Google Scholar]
- 11. Rabinowitz H, Vogel S. The Manual of Scientific Style: A Guide for Authors, Editors, and Researchers. Burlington: Elsevier; 2009. p870. [Google Scholar]
- 12. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch V. Cochrane Handbook for Systematic Reviews of Interventions version 6.3. Cochrane. 2022. www.training.cochrane.org/handbook.
- 13. Sahebkar A, Di Giosia P, Stamerra CA, Grassi D, Pedone C, Ferretti G, Bacchetti T, Ferri C, Giorgini P. Effect of monoclonal antibodies to PCSK9 on high-sensitivity C-reactive protein levels: a meta-analysis of 16 randomized controlled treatment arms. Br J Clin Pharmacol 2016;81:1175–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Veroniki AA, Jackson D, Viechtbauer W, Bender R, Bowden J, Knapp G, Kuss O, Higgins JPT, Langan D, Salanti G. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res Synth Methods 2016;7:55–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Viechtbauer W, Cheung MWL. Outlier and influence diagnostics for meta-analysis. Res Synth Methods 2010;1:112–125. [DOI] [PubMed] [Google Scholar]
- 17. Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 2001;54:1046–1055. [DOI] [PubMed] [Google Scholar]
- 18. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–1101. [PubMed] [Google Scholar]
- 19. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kinlay S, Schwartz GG, Olsson AG, Rifai N, Leslie SJ, Sasiela WJ, Szarek M, Libby P, Ganz P. High-dose atorvastatin enhances the decline in inflammatory markers in patients with acute coronary syndromes in the MIRACL study. Circulation 2003;108:1560–1566. [DOI] [PubMed] [Google Scholar]
- 21. Ridker PM, Danielson E, Fonseca FAH, Genest J, Gotto AM Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ; JUPITER Study Group . Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008;359:2195–2207. [DOI] [PubMed] [Google Scholar]
- 22. McMurray JJV, Kjekshus J, Gullestad L, Dunselman P, Hjalmarson A, Wedel H, Lindberg M, Waagstein F, Grande P, Hradec J, Kamenský G, Korewicki J, Kuusi T, Mach F, Ranjith N, Wikstrand J; CORONA Study Group . Effects of statin therapy according to plasma high-sensitivity C-reactive protein concentration in the controlled rosuvastatin multinational trial in heart failure (CORONA): a retrospective analysis. Circulation 2009;120:2188–2196. [DOI] [PubMed] [Google Scholar]
- 23. Kinlay S. Low-density lipoprotein-dependent and -independent effects of cholesterol-lowering therapies on C-reactive protein: a meta-analysis. J Am Coll Cardiol 2007;49:2003–2009. [DOI] [PubMed] [Google Scholar]
- 24. Kandelouei T, Abbasifard M, Imani D, Aslani S, Razi B, Fasihi M, Shafiekhani S, Mohammadi K, Jamialahmadi T, Reiner Ž, Sahebkar A. Effect of statins on serum level of hs-CRP and CRP in patients with cardiovascular diseases: a systematic review and meta-analysis of randomized controlled trials. Mediators Inflamm 2022;2022:8732360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lv S, Liu Y, Zou Z, Li F, Zhao S, Shi R, Bian R, Tian H. The impact of statins therapy on disease activity and inflammatory factor in patients with rheumatoid arthritis: a meta-analysis. Clin Exp Rheumatol 2015;33:69–76. [PubMed] [Google Scholar]
- 26. Horiuchi Y, Hirayama S, Soda S, Seino U, Kon M, Ueno T, Idei M, Hanyu O, Tsuda T, Ohmura H, Miida T. Statin therapy reduces inflammatory markers in hypercholesterolemic patients with high baseline levels. J Atheroscler Thromb 2010;17:722–729. [DOI] [PubMed] [Google Scholar]
- 27. Asher J, Houston M. Statins and C-reactive protein levels. J Clin Hypertens 2007;9:622–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ballantyne CM, Houri J, Notarbartolo A, Melani L, Lipka LJ, Suresh R, Sun S, LeBeaut AP, Sager PT, Veltri EP; Ezetimibe Study Group . Effect of ezetimibe coadministered with atorvastatin in 628 patients with primary hypercholesterolemia. Circulation 2003;107:2409–2415. [DOI] [PubMed] [Google Scholar]
- 29. Takemoto M, Liao JK. Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors. Arterioscler Thromb Vasc Biol 2001;21:1712–1719. [DOI] [PubMed] [Google Scholar]
- 30. Laufs U, Liao JK. Post-transcriptional regulation of endothelial nitric oxide synthase mRNA stability by rho GTPase. J Biol Chem 1998;273:24266–24271. [DOI] [PubMed] [Google Scholar]
- 31. Ferro D, Parrotto S, Basili S, Alessandri C, Violi F. Simvastatin inhibits the monocyte expression of proinflammatory cytokines in patients with hypercholesterolemia. J Am Coll Cardiol 2000;36:427–431. [DOI] [PubMed] [Google Scholar]
- 32. Kleemann R, Verschuren L, de Rooij BJ, Lindeman J, de Maat MM, Szalai AJ, Princen HMG, Kooistra T. Evidence for anti-inflammatory activity of statins and PPARα activators in human C-reactive protein transgenic mice in vivo and in cultured human hepatocytes in vitro. Blood 2004;103:4188–4194. [DOI] [PubMed] [Google Scholar]
- 33. Arnaud C, Burger F, Steffens S, Veillard NR, Nguyen TH, Trono D, Mach F. Statins reduce interleukin-6–induced C-reactive protein in human hepatocytes. Arterioscler Thromb Vasc Biol 2005;25:1231–1236. [DOI] [PubMed] [Google Scholar]
- 34. Ridker PM, Lei L, Ray KK, Ballantyne CM, Bradwin G, Rifai N. Effects of bempedoic acid on CRP, IL-6, fibrinogen and lipoprotein(a) in patients with residual inflammatory risk: a secondary analysis of the CLEAR harmony trial. J Clin Lipidol 2023;17:297–302. [DOI] [PubMed] [Google Scholar]
- 35. Samsoondar JP, Burke AC, Sutherland BG, Telford DE, Sawyez CG, Edwards JY, Pinkosky SL, Newton RS, Huff MW. Prevention of diet-induced metabolic dysregulation, inflammation, and atherosclerosis in Ldlr−/− mice by treatment with the ATP-citrate lyase inhibitor bempedoic acid. Arterioscler Thromb Vasc Biol 2017;37:647–656. [DOI] [PubMed] [Google Scholar]
- 36. Galic S, Fullerton MD, Schertzer JD, Sikkema S, Marcinko K, Walkley CR, Izon D, Honeyman J, Chen ZP, van Denderen BJ, Kemp BE, Steinberg GR. Hematopoietic AMPK β1 reduces mouse adipose tissue macrophage inflammation and insulin resistance in obesity. J Clin Invest 2011;121:4903–4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Pinkosky SL, Filippov S, Srivastava RAK, Hanselman JC, Bradshaw CD, Hurley TR, Cramer CT, Spahr MA, Brant AF, Houghton JL, Baker C, Naples M, Adeli K, Newton RS. AMP-activated protein kinase and ATP-citrate lyase are two distinct molecular targets for ETC-1002, a novel small molecule regulator of lipid and carbohydrate metabolism. J Lipid Res 2013;54:134–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Filippov S, Pinkosky SL, Lister RJ, Pawloski C, Hanselman JC, Cramer CT, Srivastava RAK, Hurley TR, Bradshaw CD, Spahr MA, Newton RS. ETC-1002 regulates immune response, leukocyte homing, and adipose tissue inflammation via LKB1-dependent activation of macrophage AMPK. J Lipid Res 2013;54:2095–2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Di Minno A, Lupoli R, Calcaterra I, Poggio P, Forte F, Spadarella G, Ambrosino P, Iannuzzo G, Di Minno MND. Efficacy and safety of bempedoic acid in patients with hypercholesterolemia: systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc Cardiovasc Cerebrovasc Dis 2020;9:e016262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hagiwara N, Kawada-Watanabe E, Koyanagi R, Arashi H, Yamaguchi J, Nakao K, Tobaru T, Tanaka H, Oka T, Endoh Y, Saito K, Uchida T, Matsui K, Ogawa H. Low-density lipoprotein cholesterol targeting with pitavastatin + ezetimibe for patients with acute coronary syndrome and dyslipidaemia: the HIJ-PROPER study, a prospective, open-label, randomized trial. Eur Heart J 2017;38:2264–2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pearson TA, Ballantyne CM, Veltri E, Shah A, Bird S, Lin J, Rosenberg E, Tershakovec AM. Pooled analyses of effects on C-reactive protein and low density lipoprotein cholesterol in placebo-controlled trials of ezetimibe monotherapy or ezetimibe added to baseline statin therapy. Am J Cardiol 2009;103:369–374. [DOI] [PubMed] [Google Scholar]
- 42. Oh MS, Min YJ, Kwon JE, Cho EJ, Kim JE, Lee WS, Lee KJ, Kim SW, Kim TH, Kim CJ, Ryu WS. Effects of ezetimibe added to ongoing statin therapy on C-reactive protein levels in hypercholesterolemic patients. Korean Circ J 2011;41:253–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Barbosa SP, Lins LC, Fonseca FA, Matos LN, Aguirre AC, Bianco HT, Amaral JB, França CN, Santana JM, Izar MC. Effects of ezetimibe on markers of synthesis and absorption of cholesterol in high-risk patients with elevated C-reactive protein. Life Sci 2013;92:845–851. [DOI] [PubMed] [Google Scholar]
- 44. Skulas-Ray AC. Omega-3 fatty acids and inflammation: a perspective on the challenges of evaluating efficacy in clinical research. Prostaglandins Other Lipid Mediat 2015;116–117:104–111. [DOI] [PubMed] [Google Scholar]
- 45. Rangel-Huerta OD, Aguilera CM, Mesa MD, Gil A. Omega-3 long-chain polyunsaturated fatty acids supplementation on inflammatory biomakers: a systematic review of randomised clinical trials. Br J Nutr 2012;107:S159–S170. [DOI] [PubMed] [Google Scholar]
- 46. Kavyani Z, Musazadeh V, Fathi S, Hossein Faghfouri A, Dehghan P, Sarmadi B. Efficacy of the omega-3 fatty acids supplementation on inflammatory biomarkers: an umbrella meta-analysis. Int Immunopharmacol 2022;111:109104. [DOI] [PubMed] [Google Scholar]
- 47. Ruscica M, Penson PE, Ferri N, Sirtori CR, Pirro M, Mancini GBJ, Sattar N, Toth PP, Sahebkar A, Lavie CJ, Wong ND, Banach M; International Lipid Expert Panel (ILEP) and International Lipid Expert Panel Experts (alphabetically) . Impact of nutraceuticals on markers of systemic inflammation: potential relevance to cardiovascular diseases—a position paper from the International Lipid Expert Panel (ILEP). Prog Cardiovasc Dis 2021;67:40–52. [DOI] [PubMed] [Google Scholar]
- 48. Brown AL, Zhu X, Rong S, Shewale S, Seo J, Boudyguina E, Gebre AK, Alexander-Miller MA, Parks JS. Omega-3 fatty acids ameliorate atherosclerosis by favorably altering monocyte subsets and limiting monocyte recruitment to aortic lesions. Arterioscler Thromb Vasc Biol 2012;32:2122–2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Faghfouri AH, Khajebishak Y, Payahoo L, Faghfuri E, Alivand M. PPAR-gamma agonists: potential modulators of autophagy in obesity. Eur J Pharmacol 2021;912:174562. [DOI] [PubMed] [Google Scholar]
- 50. Al-Taan O, Stephenson JA, Spencer L, Pollard C, West AL, Calder PC, Metcalfe M, Dennison AR. Changes in plasma and erythrocyte omega-6 and omega-3 fatty acids in response to intravenous supply of omega-3 fatty acids in patients with hepatic colorectal metastases. Lipids Health Dis 2013;12:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ridker PM, Rifai N, MacFadyen J, Glynn RJ, Jiao L, Steg PG, Miller M, Brinton EA, Jacobson TA, Tardif JC, Ballantyne CM, Mason RP, Bhatt DL. Effects of randomized treatment with icosapent ethyl and a mineral oil comparator on interleukin-1β, interleukin-6, C-reactive protein, oxidized low-density lipoprotein cholesterol, homocysteine, lipoprotein(a), and lipoprotein-associated phospholipase A2: a REDUCE-IT biomarker substudy. Circulation 2022;146:372–379. [DOI] [PubMed] [Google Scholar]
- 52. Nicholls SJ, Lincoff AM, Garcia M, Bash D, Ballantyne CM, Barter PJ, Davidson MH, Kastelein JJP, Koenig W, McGuire DK, Mozaffarian D, Ridker PM, Ray KK, Katona BG, Himmelmann A, Loss LE, Rensfeldt M, Lundström T, Agrawal R, Menon V, Wolski K, Nissen SE. Effect of high-dose omega-3 fatty acids vs corn oil on major adverse cardiovascular events in patients at high cardiovascular risk: the STRENGTH randomized clinical trial. JAMA 2020;324:2268–2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hao Y, Zhang H, Yang X, Wang L, Gu D. Effects of fibrates on C-reactive protein concentrations: a meta-analysis of randomized controlled trials. Clin Chem Lab Med 2012;50:391–397. [DOI] [PubMed] [Google Scholar]
- 54. Angles-Cano E. How statins and fibrates lower CRP. Blood 2004;103:3996–3997. [Google Scholar]
- 55. Belfort R, Berria R, Cornell J, Cusi K. Fenofibrate reduces systemic inflammation markers independent of its effects on lipid and glucose metabolism in patients with the metabolic syndrome. J Clin Endocrinol Metab 2010;95:829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rosenson RS. Effect of fenofibrate on adiponectin and inflammatory biomarkers in metabolic syndrome patients. Obesity 2009;17:504–509. [DOI] [PubMed] [Google Scholar]
- 57. Ruscica M, Tokgözoğlu L, Corsini A, Sirtori CR. PCSK9 inhibition and inflammation: a narrative review. Atherosclerosis 2019;288:146–155. [DOI] [PubMed] [Google Scholar]
- 58. Tardif JC, Rhainds D, Brodeur M, Feroz Zada Y, Fouodjio R, Provost S, Boulé M, Alem S, Grégoire JC, L’Allier PL, Ibrahim R, Guertin MC, Mongrain I, Olsson AG, Schwartz GG, Rhéaume E, Dubé MP. Genotype-dependent effects of dalcetrapib on cholesterol efflux and inflammation: concordance with clinical outcomes. Circ Cardiovasc Genet 2016;9:340–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bloomfield D, Carlson GL, Sapre A, Tribble D, McKenney JM, Littlejohn TW III, Sisk CM, Mitchel Y, Pasternak RC. Efficacy and safety of the cholesteryl ester transfer protein inhibitor anacetrapib as monotherapy and coadministered with atorvastatin in dyslipidemic patients. Am Heart J 2009;157:352–360.e2. [DOI] [PubMed] [Google Scholar]
- 60. Cao YX, Li S, Liu HH, Li JJ. Impact of PCSK9 monoclonal antibodies on circulating hs-CRP levels: a systematic review and meta-analysis of randomised controlled trials. BMJ Open 2018;8:e022348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Nordestgaard BG, Lipids ZJ. Lipids, atherosclerosis and CVD risk: is CRP an innocent bystander? Nutr Metab Cardiovasc Dis 2009;19:521–524. [DOI] [PubMed] [Google Scholar]
- 62. Ridker PM. C-reactive protein: eighty years from discovery to emergence as a major risk marker for cardiovascular disease. Clin Chem 2009;55:209–215. [DOI] [PubMed] [Google Scholar]
- 63. Danesh J, Wheeler JG, Hirschfield GM, Eda S, Eiriksdottir G, Rumley A, Lowe GD, Pepys MB, Gudnason V. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med 2004;350:1387–1397. [DOI] [PubMed] [Google Scholar]
- 64. Tardif JC, Kouz S, Waters DD, Bertrand OF, Diaz R, Maggioni AP, Pinto FJ, Ibrahim R, Gamra H, Kiwan GS, Berry C, López-Sendón J, Ostadal P, Koenig W, Angoulvant D, Grégoire JC, Lavoie MA, Dubé MP, Rhainds D, Provencher M, Blondeau L, Orfanos A, L’Allier PL, Guertin MC, Roubille F. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med 2019;381:2497–2505. [DOI] [PubMed] [Google Scholar]
- 65. Nidorf SM, Fiolet ATL, Mosterd A, Eikelboom JW, Schut A, Opstal TSJ, The SHK, Xu XF, Ireland MA, Lenderink T, Latchem D, Hoogslag P, Jerzewski A, Nierop P, Whelan A, Hendriks R, Swart H, Schaap J, Kuijper AFM, van Hessen MWJ, Saklani P, Tan I, Thompson AG, Morton A, Judkins C, Bax WA, Dirksen M, Alings M, Hankey GJ, Budgeon CA, Tijssen JGP, Cornel JH, Thompson PL; LoDoCo2 Trial Investigators . Colchicine in patients with chronic coronary disease. N Engl J Med 2020;383:1838–1847. [DOI] [PubMed] [Google Scholar]
- 66. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ; CANTOS Trial Group . Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 2017;377:1119–1131. [DOI] [PubMed] [Google Scholar]
- 67. Berkley A, Ferro A. Changes in C-reactive protein in response to anti-inflammatory therapy as a predictor of cardiovascular outcomes: a systematic review and meta-analysis. JRSM Cardiovasc Dis 2020;9:2048004020929235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Zhang X, Lan R, Zhang X, Xu W, Wang L, Kang LN, Xu B. Association between baseline, achieved, and reduction of CRP and cardiovascular outcomes after LDL cholesterol lowering with statins or ezetimibe: a systematic review and meta-analysis. J Am Heart Assoc 2019;8:e012428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Savarese G, Rosano GMC, Parente A, D’Amore C, Reiner MF, Camici GG, Trimarco B, Perrone-Filardi P. Reduction of C-reactive protein is not associated with reduced cardiovascular risk and mortality in patients treated with statins. A meta-analysis of 22 randomized trials. Int J Cardiol 2014;177:152–160. [DOI] [PubMed] [Google Scholar]
- 70. Ridker PM, Bhatt DL, Pradhan AD, Glynn RJ, MacFadyen JG, Nissen SE. Inflammation and cholesterol as predictors of cardiovascular events among patients receiving statin therapy: a collaborative analysis of three randomised trials. Lancet 2023;401:1293–1301. [DOI] [PubMed] [Google Scholar]
- 71. Sethuramalingam S, Maiti R, Hota D, Srinivasan A. Effect of colchicine in reducing inflammatory biomarkers and cardiovascular risk in coronary artery disease: a meta-analysis of clinical trials. Am J Ther 2023;30:e197–e208. [DOI] [PubMed] [Google Scholar]
- 72. Zhou Y, Liu Y, Zeng R, Qiu W, Zhao Y, Zhou Y. Early long-term low-dosage colchicine and major adverse cardiovascular events in patients with acute myocardial infarction: a systematic review and meta-analysis. Front Cardiovasc Med 2023;10:1194605. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this study are derived from published articles (available in the main text or in the supplementary materials), or unpublished data directly provided by the authors (this data will be shared on request to the corresponding author with permission of the original article's authors).