Abstract
Adults aged 65+ are at highest risk for severe COVID-19 outcomes, and prior to the distribution of vaccines in the U.S., were strongly advised to quarantine at home to reduce risk of infection. This study examines how COVID-19 restrictions impacted various dementia risk factors and social determinants of health among older adults. Data came from the Systematic Multi-Domain Alzheimer's Risk Reduction Trial, a randomized controlled trial of a multi-domain intervention in higher-risk older adults (aged 70-89). A questionnaire was administered to participants (n=156; 90.7% response rate) between May 2020 and March 2021. The data show a significant decline in social activity, physical activity, and mood among respondents. Compared to living with others, living alone was associated with worsened physical activity, diet, and subjective memory/thinking, adjusted for sex and age. These results suggest that the COVID-19 pandemic exacerbated several risk factors for dementia in older adults, particularly in those living alone.
Introduction
The coronavirus pandemic dramatically altered daily life for Americans in unparalleled ways. Physical distancing and stay-at-home measures were abruptly put in place to slow the rate of infection and reduce healthcare burden. Adherence to lockdown restrictions was especially crucial for older adults, who have the highest risk of serious illness from COVID-19 and constitute the vast majority of its death toll (CDC, 2023). Despite the importance of physical-distancing protocols in containing the spread of COVID-19 and protecting the vulnerable, prolonged social isolation puts older adults at higher risk for many age-related diseases, including Alzheimer’s Disease and dementia (Nicholson, 2012).
This study aims to examine how COVID-19 restrictions affected dementia risk factors in the older population to better inform public-health measures in the future. We evaluated pandemic-related changes and their variation by demographic factors in the context of an ongoing pilot trial to test a personalized, multi-domain intervention in an integrated healthcare delivery system (Yaffe et al., 2019). A questionnaire regarding changes in risk factors and social determinants of health (SDOH) due to COVID-19 was administered during the first year of the pandemic and assessed in the current study.
Methods
Research Participants and Setting
Participants were enrolled in the Systematic Multi-Domain Alzheimer’s Risk Reduction Trial (SMARRT) and were all members of Kaiser Permanente Washington, an integrated healthcare system in the Northwest US (Yaffe et al., 2019). Participants were aged 70-89 years, and at increased risk for Alzheimer’s Disease, having at least two of the following modifiable risk factors: physical inactivity, social isolation, high depressive symptoms, poor sleep, taking a medication that may adversely affect cognition, current smoking, uncontrolled hypertension, and uncontrolled diabetes. Nursing home and rehabilitation facility residents were excluded from the SMARRT sample.
In response to the coronavirus pandemic, the state of Washington issued a mandatory stay-at-home order in March 2020 until May 2020 (Moreland et al., 2020). Afterwards, stay-at-home orders remained for certain counties and a phased county-by-county reopening plan was implemented but was paused for several months due to a spike in cases (Governor Jay Inslee, 2021).
Data Collection
The questionnaire was administered to participants over the phone by trained research staff between May 2020 and March 2021 as part of their regular outcome visits for SMARRT. Outcome visits occurred at 6-month intervals throughout the trial and transitioned from in person to telephone visits after the start of the pandemic. For this analysis, we used each participant’s first visit after the start of the pandemic, most of which (86%) were held between May and July 2020. Demographic factors, including age, sex, race and living arrangement, were asked at study baseline.
COVID-19 Questionnaire
The questionnaire contained ten five-point Likert scale questions regarding the impact of coronavirus on subjective memory and thinking and nine modifiable risk factors for dementia: physical activity, cognitive activity, social activity, mood, diet, sleep quality, smoking, ability to manage blood pressure, and ability to manage blood sugar. Respondents were asked how they feel the coronavirus has affected each item on a scale of −2 to 2, with answer choices including increased/improved a lot (=2), increased/improved a little (=1), no change (=0), decreased/worsened a little (=−1), decreased/worsened a lot (=−2), and don’t know/refuse to answer. The choice of not applicable was added for questions on smoking, blood pressure management and blood sugar management.
Moreover, a checkbox question asked participants to indicate which of the following SDOH were negatively affected by the pandemic: ability to pay bills, ability to access transportation or get to places outside your home (i.e., medical appointments, grocery shopping, etc.), employment status, ability to access healthy food, and/or something else. For participants who selected “something else,” a follow-up question asked them to expand on their response. The final question was an open-ended question allowing participants to share any further impacts of COVID-19 on themselves or their community.
Statistical Analysis
Baseline characteristics of the sample are described using means and standard deviations (SD) for continuous variables and numbers and percentages for categorical variables. Linear regression models were used to determine whether there were significant differences in risk factors and behaviors associated with dementia based on sex, race, assigned treatment arm, and living arrangements, all adjusted for age and sex.
Results
Of the 172 SMARRT participants, there was a 90.7% (n=156) response rate to the COVID-19 questionnaire. Characteristics of the participants are shown in Table I. The cohort had a mean age of 75.4 years (SD ± 4.7) and were approximately 67% female. The majority lived with one or more people (n=93, 59.6%) during this period.
Table I:
Characteristics of 156 Participants
| Characteristic | Mean (SD) or No. (%) |
|---|---|
| Age | 75.4 (4.7) |
| Sex | |
| Female | 104 (66.7%) |
| Male | 52 (33.3%) |
| Years of Education | 16.3 (2.5) |
| Living Situation | |
| Living Alone | 53 (34.0%) |
| Living with other(s) | 93 (59.6%) |
| Other | 8 (5.1%) |
| Prefer not to answer | 2 (1.3%) |
| Race | |
| White | 121 (77.5%) |
| Black | 14 (9.0%) |
| Asian | 7 (4.5%) |
| Other | 13 (8.3%) |
| Prefer not to answer | 1 (0.6%) |
| Current smoker | 18 (11.5%) |
| Hypertension | 97 (62.2%) |
| Diabetes | 47 (30.1%) |
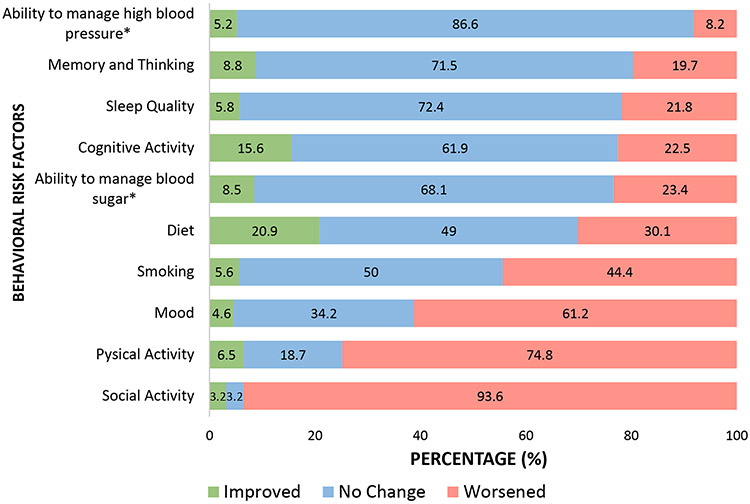
Data on changes in risk factors due to COVID-19 are presented in Figure 1. The factors most reported to have worsened were social activity (93.6%), physical activity (73.7%), and mood (59.6%). “No change” was the most frequent response for the remaining variables, including ability to manage high blood pressure (86.6%), sleep quality (72.4%), memory and thinking (71.5%), ability to manage blood sugar (68.1%), cognitive activity (61.9%) and diet (49%). Diet had the most positive responses, with 20.9% of participants reporting improvement. However, for all factors, more participants reported negative change than positive change.
Figure 1. Change in Behavioral Risk Factors during COVID-19 for All Participants.
*Ability to manage blood sugar and high blood pressure was collected among participants with diabetes and hypertension, respectively.
The figure displays combined Likert scale responses, where ‘1’ and ‘2’ indicate an increase and ‘−1’ and ‘−2’ indicate a decrease.
We identified significant associations between changes in risk factors and living arrangement. In our sample, 34% (n=53) lived alone while 59.6% (n=93) lived with a spouse/partner, family, or others, and 6.4% (n=10) selected “other” or declined to answer. Participants who lived alone were more likely to be older and female. Compared to living with others, living alone was associated with worsened physical activity (p=0.005), subjective memory and thinking (p=0.02), and diet (p=0.05) after adjusting for sex and age. Average values of risk factors on the Likert scale by living situation are presented in Table II. Among people living alone, 84.9% reported worse physical activity compared to 65.6% of people cohabitating; 24.5% reported worse subjective memory and thinking compared to 11.8% cohabitating; and 45.3% reported worse diet compared to 21.5% of people cohabitating. We also examined the risk factors by sex, race, and assigned treatment arm, but found no significant differences (all p>0.05).
Table II:
Scale Values of Health Variables by Living Situation
| Living Alone Mean (SD) |
Living with Other(s) Mean (SD) |
P-value | P-value (sex + age) |
|
|---|---|---|---|---|
| Physical activity | −1.5 (0.7) | −0.9 (1.1) | 0.01 | 0.003 |
| Cognitive activity | −0.3 (0.9) | 0 (0.8) | 0.10 | 0.09 |
| Social activity | −1.7 (0.9) | −1.7 (0.7) | 0.72 | 0.70 |
| Smoking | 0.4 (0.8) | 0.6 (0.9) | 0.40 | 0.50 |
| Memory and thinking | −0.2 (0.7) | 0 (0.7) | 0.02 | 0.04 |
| Mood | −0.7(0.9) | −0.7 (0.8) | 0.82 | 0.82 |
| Diet | −0.4 (1.1) | 0.1 (0.9) | 0.05 | 0.04 |
| Quality of sleep | −0.2 (0.8) | −0.3 (0.7) | 0.44 | 0.47 |
| Ability to manage blood pressure | 0 (0.7) | 0 (0.4) | 0.68 | 0.66 |
| Ability to manage blood sugar | −0.3 (0.8) | −0.2 (0.8) | 0.50 | 0.50 |
Values represent answers using a Likert scale (−2 to 2); −2 = worsened a lot, 2 = improved a lot. P-values were determined from linear regression analysis.
Regarding the SDOH negatively affected by COVID-19, ability to access transportation or get to places outside your home was most reported (44.9%). “Something else” ranked second (32.7%), with most responses referring to limited social engagement. Other factors were less reported, including ability to access healthy food (16%), employment status (13.5%) and ability to pay bills (12.18%).
In the last survey question, which invited participants to elaborate on the pandemic’s impact on their lives, most responses described struggling with social isolation from family and friends and a yearning to hug their children and grandchildren. Multiple responses also reported increased levels of fear and anxiety, primarily about the well-being of their loved ones and/or the existing political uncertainty in the United States.
Discussion
Older adults in the SMARRT trial reported that their physical activity, social interactions, and mood deteriorated significantly during the pandemic.
Physical inactivity is a well-established risk factor for dementia and cognitive impairment. Substantial evidence suggests that regular aerobic exercise in old age provides neuroprotective effects that can enhance cognitive function and delay brain aging (Ahlskog et al., 2011). Lack of social connection and perceived loneliness are also associated with worse cognitive outcomes (Nicholson, 2012). A recent meta-analysis of 10 longitudinal studies (all prior to COVID-19) found that older adults experiencing social isolation and loneliness have a 49-60% higher risk of developing dementia (Lazzari & Rabottini, 2022). Moreover, low mood as a symptom of depression has been linked to higher incidence of mild cognitive impairment and dementia (Diniz et al., 2013).
The negative effects of quarantine restrictions on physical and mental health observed in our study is consistent with some but not all other studies investigating pandemic-related changes in older adults. Most studies found that pandemic-mandated social isolation was associated with diminished physical activity, increased feelings of loneliness, and overall decline in quality of life and well-being (Bailey et al., 2021; Rising et al., 2022; Di Gessa & Zaninotto, 2023). However, some large-scale studies conflict with our findings. For instance, results from the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability COVID-19 survey found no drastic changes in lifestyle factors, with the most notable change being a decrease in physical activity for 34% of participants (Lehtisalo et al., 2021). Similarly, a longitudinal study investigating the impact of the COVID-19 lockdown on 1,671 older Australian adults found no significant effects on any dementia risk factors (Bartlett et al., 2021). Interestingly, both studies were based in countries with different COVID-19 policies than the United States, and specifically the state of Washington, which was one of the earliest states to institute a lockdown and had relatively strict COVID-19 restrictions.
Living alone was associated with more adverse changes compared to cohabitating, specifically regarding physical activity, subjective memory/thinking, and diet. Our results align with prior research, including Lehtisalo et al. (2021) and Bartlett et al. (2021), demonstrating that older people living alone during the pandemic were more susceptible to negative health outcomes. Older adults living alone are at higher risk of social isolation, which is linked to a range of physical and mental health issues (Donovan et al., 2020). Social connectedness is thus crucial for this population’s well-being, particularly during a pandemic lockdown, as it can protect against the detrimental effects of stress and instill a sense of obligation to engage in healthy behaviors (Shah et al., 2022).
This study’s strengths include a community-based sample and significant participation from minority groups, offering meaningful insights for developing effective public health policies. The limitations to this study include potential biases in self-reported survey data, limited generalizability due to the sample being from one health care system in Washington state, and the increased likelihood of inaccurate correlations from multiple comparisons. Additionally, most of the data in this study were collected within a short timeframe early in the pandemic. Examining the variations in outcome variables over time could be an interesting avenue for future research.
In summary, this study found that the COVID-19 restrictions negatively impacted physical activity, social activity, and mood in older adults. The striking decline of these factors may lay the groundwork for a potential rise in dementia incidence among the older population. In addition, living alone was associated with worsened physical activity, diet, and memory/thinking compared to living with others. These findings highlight the need for pandemic emergency responses to incorporate programs that help older adults maintain healthy behaviors while adhering to safety measures.
What this paper adds
Provides a glimpse into the firsthand experiences of a diverse group of older adults during a pandemic-mandated lockdown.
Identifies several dementia health risk factors significantly impacted by the COVID-19 pandemic
Identifies older adults who live alone as a particularly vulnerable group in periods of stay-at-home measures
Applications of study findings
Informs public health strategies to maintain and promote well-being among older adults in the event of another mandated lockdown.
Provides insight on specific dementia risk factors to target in developing interventions to reduce cognitive decline post-pandemic.
Highlights need for public health initiatives that address loneliness, especially for older adults living alone.
Funding
This work was supported by the National Institute on Aging (1R01 AG057508)
Footnotes
IRB Approval Numbers:
SMARRT: 17-22940, Kaiser: 1220346-50
COI:
None of the authors of this manuscript have related conflicts of interests to disclose.
References
- Yaffe K, Barnes DE, Rosenberg D, Dublin S, Kaup AR, Ludman EJ, Vittinghoff E, Peltz CB, Renz AD, Adams KJ, Larson EB. Systematic Multi-Domain Alzheimer's Risk Reduction Trial (SMARRT): Study Protocol. J Alzheimers Dis. 2019;70(s1):S207–S220. doi: 10.3233/JAD-180634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahlskog JE, Geda YE, Graff-Radford NR, & Petersen RC (2011). Physical exercise as a preventive or disease-modifying treatment of dementia and brain aging. Mayo Clinic Proceedings, 86(9), 876–884. 10.4065/mcp.2011.0252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey L, Ward M, DiCosimo A, Baunta S, Cunningham C, Romero-Ortuno R, Kenny RA, Purcell R, Lannon R, McCarroll K, Nee R, Robinson D, Lavan A, & Briggs R (2021). Physical and mental health of older people while cocooning during the COVID-19 pandemic. QJM: An International Journal of Medicine, 114(9), 648–653. 10.1093/qjmed/hcab015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett L, Brady JJ, Farrow M, Kim S, Bindoff A, Fair H, Vickers JC, & Sinclair D (2021). Change in modifiable dementia risk factors during COVID-19 lockdown: The experience of over 50s in Tasmania, Australia. Alzheimer's & Dementia: Translational Research & Clinical Interventions, 7(1). 10.1002/trc2.12169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2023, February). Covid-19 risks and information for older adults. https://www.cdc.gov/aging/covid19/index.html [Google Scholar]
- Di Gessa G, & Zaninotto P (2023). Health Behaviors and Mental Health during the COVID-19 Pandemic: Evidence from the English Longitudinal Study of Aging. Journal of Applied Gerontology, 42(7), 1541–1550. 10.1177/07334648231159373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diniz BS, Butters MA, Albert SM, Dew MA, & Reynolds CF (2013). Late-life depression and risk of vascular dementia and alzheimer's disease: Systematic review and meta-analysis of community-based cohort studies. British Journal of Psychiatry, 202(5), 329–335. 10.1192/bjp.bp.112.118307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan NJ, & Blazer D (2020). Social isolation and loneliness in older adults: Review and commentary of a National Academies Report. The American Journal of Geriatric Psychiatry, 28(12), 1233–1244. 10.1016/j.jagp.2020.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Governor Jay Inslee. (2021, May). Inslee announces two-week pause on phases. https://governor.wa.gov/news/2021/inslee-announces-two-week-pause-phases
- Lazzari C, & Rabottini M (2021). Covid-19, loneliness, social isolation and risk of dementia in older people: A systematic review and meta-analysis of the relevant literature. International Journal of Psychiatry in Clinical Practice, 26(2), 196–207. 10.1080/13651501.2021.1959616 [DOI] [PubMed] [Google Scholar]
- Lehtisalo J, Palmer K, Mangialasche F, Solomon A, Kivipelto M, & Ngandu T (2021). Changes in lifestyle, behaviors, and risk factors for cognitive impairment in older persons during the first wave of the coronavirus disease 2019 pandemic in Finland: Results from the finger study. Frontiers in Psychiatry, 12. 10.3389/fpsyt.2021.624125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreland A, Herlihy C, Tynan MA, Sunshine G, … Popoola A (2020). Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement — United States, March 1–May 31, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(35), 1198–1203. 10.15585/mmwr.mm6935a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson NR (2012). A review of social isolation: An important but underassessed condition in older adults. The Journal of Primary Prevention, 33(2-3), 137–152. 10.1007/s10935-012-0271-2 [DOI] [PubMed] [Google Scholar]
- Rising KL, Salcedo VJ, Amadio G, Casten R, Chang A, Gentsch A, O’Hayer CV, Sarpoulaki N, Worster B, & Gerolamo AM (2022). Living Through the Pandemic: The Voices of Persons With Dementia and Their Caregivers. Journal of Applied Gerontology, 41(1), 30–35. 10.1177/07334648211036399 [DOI] [PubMed] [Google Scholar]
- Shah SJ, Fang MC, Wannier SR, Steinman MA, & Covinsky KE (2022). Association of social support with functional outcomes in older adults who live alone. JAMA Internal Medicine, 182(1), 26. 10.1001/jamainternmed.2021.6588 [DOI] [PMC free article] [PubMed] [Google Scholar]