Abstract
Surgical management of a diseased thyroid depends on sonological and pathological evaluation and thereby, planning of the surgery. The definite surgery has two objectives: removal of the diseased gland and preservation of the nerves, namely EBSLN (External Branch of Superior Laryngeal Nerve) and RLN (Recurrent Laryngeal Nerve) and the Parathyroid glands. The objectives of the study were: (1) To identify the course of the RLN and EBSLN of both sides, during Thyroidectomy. (2) To discern various anatomical landmarks, the relations of the two nerves with them and anatomical variations, if any. In this Prospective observational study, fifty selected goitre patients underwent various types of thyroidectomies based on sonological and cytological criteria. The course and anatomical variations of EBSLN and RLN were photo-documented and results were analysed. Most of the EBSLN were found as Cernea type 1 type (25 out of 50), followed by Cernea type 2a (comprising 36%). The least common was type 2b. It was found that 36 out of 50 (72%) of RLN passed posterior to Inferior Thyroid Artery (ITA). Moreover, before piercing cricothyroid joint, the RLN showed bifurcation in 13 out of 50 subjects (26%), 1 participant had trifurcation and the remaining 36 (72%) had a single trunk. The EBSLN shows relation to the horizontal plane passing through the upper pole of the thyroid gland and it is more prone to get damaged when it passes within less than 1 cm to the plane. The RLN has various relations to the distinct anatomical landmarks thereby helping in safe dissection of the nerve. The study also noted the RLN in relation to ITA and branching before entering into the cricothyroid joint.
Keywords: Recurrent laryngeal nerve, Supeior laryngeal nerve, Thyroidectomy, Anatomical landmarks, Cricothyroid joint
Introduction
The thyroid gland - a bilobed gland with an isthmus is very vital for maintaining normal homeostasis of the body. Any dysfunction in its structure or function prompts an individual to visit an endocrinologist or an otolaryngologist for consultation. The increase in size of the gland leads to social dilemma for the bearer. For an otolaryngologist, the concern is more than the cosmetic aspect of the swelling of the neck. Cytological and radiological tools are helpful in arriving at a definite diagnosis and thereby in treatment planning.
Once the definite surgery is planned, understanding the anatomy of the gland with its surrounding structures is very important for any ENT surgeon. The thyroid gland is closely associated with parathyroid glands and the two nerves - recurrent laryngeal nerve and external branch of superior laryngeal nerve. The vessels supplying the gland should be carefully lighted to ensure the vitality of the parathyroid glands.
Preservation of the recurrent laryngeal nerve is of paramount importance as unilateral damage can lead to hoarseness, breathiness or may go unnoticed in one-third of the patients. Bilateral damage can lead to fixity of the vocal cords in the para-median position leading to aspiration. Hence, knowledge of the anatomy and variations in the course of the nerve help us prevent catastrophe. External branch of superior laryngeal nerve - nerve of Amelita Galli-Curci is an important nerve for professional voice users like singers. Damage to the nerve leads to failure in sustaining high notes and voice fatigue after prolonged use.
Thus, the purpose of this study is to observe the course of the recurrent laryngeal nerve and external branch of superior laryngeal nerve during thyroidectomy. The study will also take into account the relation of the two nerves with various anatomical landmarks, thereby helping in better delineation of the nerves and prevention of injuries during thyroidectomy.
The course of External Branch of Superior Laryngeal Nerve (EBSLN) and Recurrent Laryngeal Nerve (RLN) has been described below.
EBSLN
Superior laryngeal nerve arises from the inferior ganglion of the vagus nerve. It passes downwards and forwards on the superior constrictor muscle medial to the internal carotid artery and divides into external and internal branches.
The external laryngeal nerve is motor, accompanies the superior thyroid artery, pierces the inferior constrictor and ends by supplying the cricothyroid muscle. The internal laryngeal nerve passes downwards and forwards, pierces the thyrohyoid membrane with the superior laryngeal vessels and enters the larynx. It supplies the mucous membrane of the larynx upto the mucosal folds.
The external branch of superior laryngeal nerve lies deep to the upper pole of the thyroid gland as it passes superficial to the cricothyroid muscle in the sternothyrolaryngeal triangle (Joll’s triangle). This triangle is formed laterally by the upper pole of the thyroid gland and the superior thyroid vessels, superiorly by the attachment of the strap muscles and deep investing layer of fascia to the hyoid and medially by the midline. Its floor is formed by the cricothyroid muscle and its roof is made up of strap muscles, it contains the EBSLN running on cricothryroid.
EBSLN can have variations with its relations to the superior pole of the thyroid gland. This relationship was described by Cernea et al. [1] in his paper titled ‘Surgical Anatomy of External Branch of Superior Laryngeal Nerve’. He performed dissection on 30 cadavers and proposed a classification system as follows:
Type 1- Nerve crossing the superior thyroid vessels 1 or more cm above a horizontal plane passing the upper border of the superior thyroid pole.
Type 2-Nerve crossing the vessels less than 1 cm above or below that horizontal plane.
Type 2a-Nerve less than 1 cm above the plane.
Type 2b-Nerve below the plane (Fig. 1).
Fig. 1.
Types of branching of EBSLN as proposed by Cernea et al.
RLN
It is a branch of vagus, the tenth cranial nerve. On the right side, it arises from the vagus anterior to the first part of the subclavian artery. It then curves backwards below and behind the artery to ascend obliquely to the side of the trachea behind the common carotid artery. Near the lower pole of the lateral lobe of the thyroid gland, it is closely related to the inferior thyroid artery. The recurrent laryngeal nerve crosses either in front of, behind or between the branches of inferior thyroid artery.
On the left, the nerve arises from the vagus on the left of the aortic arch. It then curves below it immediately behind the attachment of the ligamentum arteriosum to the concavity of the aortic arch and ascends to the side of the trachea.
On both sides, the recurrent laryngeal nerve ascends in or near a groove between the trachea and oesophagus. It is closely related to the medial surface of the thyroid gland before it passes under the lower border of the inferior constrictor, enters the larynx behind the articulation of the inferior thyroid cornu with the cricoid cartilage.
The nerve enters the larynx by passing either deep to (two-third cases) or between the fibres of cricopharyngeus (one-third of cases) at its attachment to the lateral aspect of the cricoid cartilage. It supplies cricopharyngeus as it passes through it. At this point, the nerve is in intimate proximity to the postern-medial aspect of the thyroid gland.
The nerve may supply extralaryngeal branches to the larynx which arise before it passes behind the inferior thyroid cornu.
Variation
A very rare anomaly that is of relevance to laryngeal innervation, is the so-called ‘non-recurrent’ laryngeal nerve,where the right recurrent laryngeal nerve arises directly from the vagus trunk high up in the neck and enters the larynx close to the inferior pole of the thyroid gland. Only the right side is affected, and it is always associated with an abnormal origin of the right subclavian artery from the aortic arch on the left side. If unrecognised, a non recurrent laryngeal nerve may be at risk to injury during surgery. It may also potentially be compressed by tumours of the thyroid gland.
Materials and methods
It is a prospective observational study conducted over twelve months in the study period July 2021-July 2022. Fifty patients, belonging to the age group 15–70 years, diagnosed with thyroid disorders like neoplasms, goitre, indeterminate nodules of thyroid, thyroiditis were admitted at a tertiary care hospital for undergoing thyroidectomy (hemi-thyroidectomy, total thyroidectomy, completion thyroidectomy). The inclusion criteria was USG or FNAC/biopsy proven thyroid disorder amenable to surgery and those who were fit to undergo surgery. The exclusion criterion only being patient’s refusal to participate in the study.
During the surgery, intra-operative pictures were taken demonstrating the variable course of EBSLN and RLN of the left and right side(depending on the extent of the surgery). The results were obtained and statistical analysis was done.
Results
Applying chi-square tests, p value of 0.290 was obtained and it is is not statistically significant. Therefore, we can say that both the sides of EBSLN run their own course and are developmentally independent of each other (Table 1; Fig. 2).
Table 1.
Frequency distribution table of external branch of superior laryngeal nerve as per Cernea’s classification
| Frequency | Percent | Valid percent | Cumulative percent | |
|---|---|---|---|---|
| Type 1 | 25 | 50.0 | 50.0 | 50.0 |
| Type 2a | 18 | 36.0 | 36.0 | 86.0 |
| Type 2b | 7 | 14.0 | 14.0 | 100.0 |
| Total | 50 | 100.0 | 100.0 |
Fig. 2.

Intra-operative picture showing EBSLN (right side) while dissecting the superior pole of the thyroid
On comparison of the relation of recurrent laryngeal nerve with inferior thyroid artery on the left side and right side, 26 out of 36 nerves on the right side were posterior to ITA and while 10 on the left side were in posterior relation to ITA. 8 nerves on the right side were anterior to ITA whereas 6 nerves on the left side were so (Table 2).
Table 2.
Frequency distribution table showing relation of RLN to ITA
| Side | Total | ||
|---|---|---|---|
| Left | Right | ||
| RLN relation to ITA | |||
| Anterior | 6 | 8 | 14 |
| Posterior | 10 | 26 | 36 |
| Total | 16 | 34 | 50 |
After applying chi-square test to compare left and right side of RLN in relation to ITA, p-value obtained was 0.305 (statistically insignificant). Therefore, we can deduce that the left and right side of the nerve are not significantly different from each other in their course.
Extra-laryngeal Branching of RLN
As per the study, 13 out of 50 participants had bifurcation of recurrent laryngeal nerve whereas one participant showed trifurcation too. The remaining 36 out of 50 show a single trunk of recurrent laryngeal nerve (Table 3; Fig. 3).
Table 3.
Extra laryngeal branching of RLN
| Frequency | Percent | Valid percent | Cumulative percent | |
|---|---|---|---|---|
| 2 branches | 13 | 26.0 | 26.0 | 26.0 |
| 3 branches | 1 | 2.0 | 2.0 | 28.0 |
| single trunk | 36 | 72.0 | 72.0 | 100.0 |
| Total | 50 | 100.0 | 100.0 |
Fig. 3.
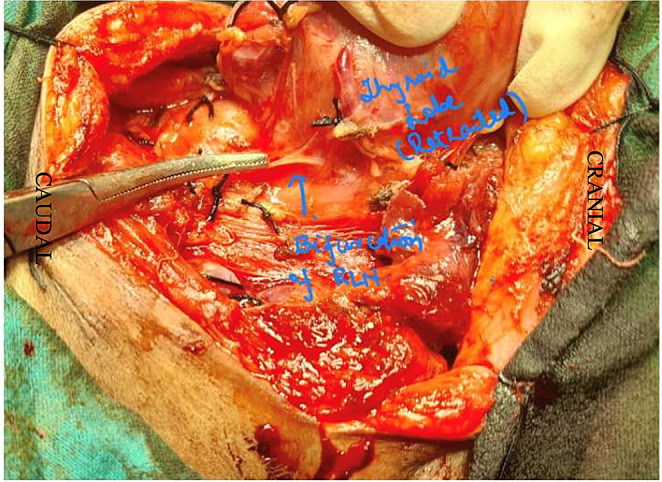
Intra-operative picture showing RLN (left side) bifurcating before entering cricothyroid joint
Discussion
After analyzing the patients affected with benign and malignant disorders of thyroid in this study, it is found that the most common age group affected was 15–30 years (34%), followed by 31–40 years (26%). The remaining 20% were in the age group 41–50 years, followed by 16% in the age group 51–60 years while just 4% were above 60 years of age.
Out of fifty patients, 47 were females and 3 were males constituting 94% and 6% respectively. This is very much in synchrony to other studies conducted on the prevalence of disorders of thyroid gland.
The distribution of External Branch of Laryngeal Nerve as per Cernea’s classification was analysed. It was found that the most common type found was Cernea type 1 (50%), followed by Cernea type 2A (36%) and least common was type 2B (14%). Therefore, the risk of damage to EBSLN was least in our study with the majority of the EBSLN passing about more than 1 cm above the superior thyroid pole, which the most common variety to get injured i.e. type 2B was least predominant.
As per the original study done by Cernea et al. [1], the nerve distribution pattern seen were as follows: Type 1 pattern was seen in 18 subjects (60%), Type 2a constituted 5 (17%), while Type 2b were 6 in number(20%). 3% remain unidentified.
As per the study conducted by Furlan et al. [2], 34 were Type 1 nerves, 22 were Type 2a nerves, and 16 were Type 2b nerves found in the bilateral dissections performed in 36 human cadavers.
As per this current study, 18 nerves out of 25 belong to type 1 on the right side, whereas it is 7 out of 25 on the left side. 10 out of 18 on the right side belong to Cernea type 2a, while 8 out of 18 on the left side are type 2a type. The least common type 2b variety, 6 out of 7 on the right and 1 out of 7 on the left side.
In our study, we found that 14 out of 50 subjects have recurrent laryngeal nerve passing anterior to inferior thyroid artery whereas the majority 36 out of 50 (72%) pass posterior to inferior thyroid artery. On comparison of the relation of recurrent laryngeal nerve with inferior thyroid artery on the left side and right side, we found that 26 out of 36 nerves on the right side were posterior to ITA and while 10 on the left side were in posterior relation to ITA. 8 nerves on the right side were anterior to ITA whereas 6 nerves on the left side were so.
The findings are similar to the study done in cadavers by Dr.Swapnali and Dr Bhuiyan [3], out of total 120 RLN identified, the RLN was found anterior to ITA in 44 (36.52%) cases and posterior to ITA in 68(56.44%) cases. In the remaining 6(4.98%) cases the nerve was serve to be traversing a route within the branches of ITA.
As per the study done by Amana et al. [4] in 2019 on 227 thyroidectomies, RLN was posterior to ITA in 75.08% of cases with prevalence of the truncal, anterior in 16.07% and inter-arterial in 3.28% cases. One non-recurrent laryngeal nerve was also found on the right.
As per the works of Zada et al. [5] to find correlation between RLN and ITA during thyroidectomy. It was observed that out of total 398 RLNs identified, the nerve was found to be anterior to ITA in 220 (55.27%) cases while it was posterior to ITA in 138 (34.67) % cases. In the remaining 40 (10.05%) cases the nerve was seen to be traversing within the branches of inferior thyroid artery. This finding is quite contrary to what we found in our study.
The study also took into consideration the branching pattern (if any) of the recurrent laryngeal nerve. It was found 13 out of 50 participants had bifurcation of recurrent laryngeal nerve whereas one participant showed trifurcation too; thereby accounting for 28% cases of extra-laryngeal branching. The remaining 36 out of 50 show a single trunk of recurrent laryngeal nerve. Hence, it is important to identify the branching pattern of RLN while doing thyroidectomy as injuring any division inadvertently may lead to hoarseness post-operatively or weakness of one/more laryngeal muscles.
In a study done by Nemiroff et al. [6], a total of 153 recurrent laryngeal nerves were observed. Out of 153, 63 (41.2%) bifurcated or trifurcated into extralaryngeal branches. Of these, there were four instances of trifurcations. The remaining 59 nerves bifurcated.
In a surgical case series done by Piperos et al. [7], the most common pattern of RLN extralaryngeal division is bifurcation with an incidence of 51%. When the RLN bifurcates extralangyngeally, the motor branch is the anterior one and the sensory branch runs posteriorly.
As per the study done by Yin et al. [8] in 292 patients undergoing thyroidectomy, about 30.9% of the RLNs gave off multiple branches into the larynx. Two branches of RLNs into the larynx were found in 25.5% of the case whereas three branches were found in 5.4% of the cases.
Conclusion
In this study, we conclude that majority of the study participants were females (94%) while only 6% were males. This further reinforces the fact that thyroid disorders are common in females.
The age group affected were almost in synchrony to other studies, though in our study the females affected were more in the age group fifteen to thirty years followed by thirty to forty years.
The anatomical distribution of the two nerves were compared with previous classification system. According to the study, most of the EBSLN were Cernea type 1 type (25 out of 50), followed by Cernea type 2a (comprising 36%). The least common was Cernea type 2b, thereby there were least chances of damage to the nerve in our study population. If injury occurs, it can lead to loss in timbre.
The recurrent laryngeal nerve has various relations to the distinct anatomical landmarks thereby helping in safe dissection of the nerve. In our study, we observed the nerve in relation to ITA and if it is showing any branching before the entry into the cricothyroid joint.
It was found that 14 out of 50 subjects have recurrent laryngeal nerve passing anterior to inferior thyroid artery whereas the majority 36 out of 50 (72%) pass posterior to inferior thyroid artery. The RLN before piercing crico-thyroid joint showed bifurcation in 26% of cases (i.e. 13 out of 50 subjects), 1 participant had trifurcation and the remaining 74% had a single trunk of RLN. Two of the nerves showed tortuosity of the main trunk. The nerves which show division need careful observation, as any one of the branches which might get injured during dissection can lead to post-operative hoarseness.
Therefore, we conclude that understanding the anatomical distribution of the recurrent laryngeal nerve and external branch of superior laryngeal nerve is pertinent while operating on a thyroid gland. The safest way is to proceed, keeping the anatomical landmarks in view and to dissect out both the nerves meticulously before ligating the superior and inferior pole vessels; thereby preventing any undue entrapment of the nerve leading to post operative voice change.
Acknowledgements
We would like to acknowledge all OT sisters and technicians who have helped us during the surgeries, and institution for constant encouragement and support.
Funding
All the authors declare they have not received any funding.
Declarations
Informed Consent
Written informed consent was obtained from the concerned patient.
Conflict of Interest
All the authors declare they have no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cernea CR, Ferraz AR, Nishio S, Dutra A Jr, Hojaij FC, dos Santos LR (1992) Sep-Oct;14(5):380-3 Surgical anatomy of the external branch of the superior laryngeal nerve. Head Neck. 10.1002/hed.2880140507. PMID: 1399571 [DOI] [PubMed]
- 2.Furlan JC, Cordeiro AC, Brandão LG. Study of some intrinsic risk factors that can enhance an iatrogenic injury of the external branch of the superior laryngeal nerve. Otolaryngol Head Neck Surg. 2003;128(3):396–400. doi: 10.1067/mhn.2003.11. [DOI] [PubMed] [Google Scholar]
- 3.Swapnali S, Bhuiyan PS. Relationship between the recurrent laryngeal nerve and the inferior thyroid artery: a study in cadavers. Int J Curr Res. 2016;9(09):38855–38557. [Google Scholar]
- 4.Amana B, Foma W, Pegbessou E, Darré T, Boko E, Kpemissi E (2019) Apr Relationship between the recurrent laryngeal nerve and the inferior thyroid artery in the Togolese subject: Surgical anatomy study from 227 thyroidectomies. BJOHNS. 30 ;27(1)
- 5.Zada B, Anwar K, Malik SA, Niamatullah, Khan N, Salam F (2014 Jul-Sep) Anatomical relationship between recurrent laryngeal nerve and inferior thyroid artery in thyroidectomy patients. J Ayub Med Coll Abbottabad 26(3):380–383 [PubMed]
- 6.Nemiroff PM, Katz AD. Extralaryngeal divisions of the recurrent laryngeal nerve. Surgical and clinical significance. Am J Surg. 1982;144(4):466–469. doi: 10.1016/0002-9610(82)90425-1. [DOI] [PubMed] [Google Scholar]
- 7.Piperos T, Kaklamanos I, Chrysikos D, Zarokosta M, Boumpa E, Zoulamoglou M, Kalles V, Gkogka GI, Mariolis-Sapsakos T (2018) Abnormal distance of the extralaryngeal bifurcation point of the recurrent laryngeal nerve from the cricothyroid joint. J Surg Case Rep 2018(1) [DOI] [PMC free article] [PubMed]
- 8.Yin C, Song B, Wang (2020) Xiaoyan. Anatomical variations in recurrent laryngeal nerves in thyroid surgery. Ear, Nose Throat J 100:014556132092756. 10.1177/0145561320927565 [DOI] [PubMed]



