Abstract
To study the presentation and plan of treatment of patient with Rosai Dorfman Disease. Rosai-Dorfman disease(RDD), is rare, non-neoplastic, multisystemic histiocytic disorder. Nodal form is more common. It’s self-limiting disorder of unknown etiology. Symptomatic treatment is mainstay. Bardet–Biedl syndrome (BBS) is rare ciliopathic, autosomal-recessive disorder, affecting multiple organs. Characterized by marked central obesity, retinal dystrophy, polydactyly, mental retardation, hypogonadism and renal dysfunction. Treatment is symptomatic with hormone supplementation & regular follow-ups. 10 year male presented with swelling over left side of neck and intermittent fever since 2 years, diminished vision in night since 5 years. History of similar complaints on right side 5 years back. Fine needle aspiration cytology(FNAC)-features consistent with Rosai Dorfman Disease. Examination showed short stature, squint eyes, polydactyly. Multiple palpable neck nodes of variable sizes. Ophthalmic evaluation showed Retinitis Pigmentosa. Paediatric consultation for syndromic evaluation, features were consistent with Bardet Biedel syndrome. Since the presentation is same as that of opposite side in past, because of recurrence of symptoms even with regular antibiotic and steroid therapy, and no local recurrence of disease on right side, surgical excision is planned for the patient. Rosai-Dorfman disease and Bardet–Biedl syndrome are rare disorders presenting many diagnostic and therapeutic challenges. High degree of clinical suspicion (RDD & BBS) with typical histopathological features (RDD) are diagnostic. Symptomatic treatment is useful and surgical excision can be done for recurrent/ complicated cases of RDD while symptomatic treatment with regular follow-up for BBS.
Keywords: Rosai dorfman disease, Bardet-biedel syndrome, Emperipolesis, Sinus histiocytosis
Introduction
Rosai-Dorfman disease(RDD), is rare, non-neoplastic, multisystemic histiocytic disorder, caused by histiocytic proliferation in sinusoids leading to massive lyphadenopathy. Occurs in first two decades of life commonly in males(58% [2]).
The literature says that 70% of patients are in stable condition, 20% are self-limiting and only 10% results in aggressive local or systemic disease which may be fatal if compression of vital structures is present [1]. No standard treatment is available till date, various treatment modalities in the form of corticosteroids, chemotherapy, radiotherapy & surgical excision have been tried with variable outcomes.
Bardet–Biedl syndrome (BBS) is autosomal-recessive ciliopathic disorder. < 15 cases have been reported in India with disease frequency of 1:1,60,000 [3]. Primary features of disease include marked central obesity, retinal dystrophy, polydactyly, mental retardation, hypogonadism and renal dysfunction [4]. Symptomatic treatment with hormone supplementation & regular follow-ups is generally followed [5].
More than 1000 reports of Rosai Dorfman disease are available with varied presentations and treatment modalities. While only < 15 cases of Bardet Biedel syndrome are reported in India. But there is no literature found till date on Rosai Dorfman Disease associated with Bardet Biedl Syndrome & hence this case report was done to study different presentation of our patient & to plan treatment.
Case Report
We present a case report of 10 year old male child who presented with swelling over left side of neck since 2 years. It was insidious in onset and gradually progressive in nature. Started as a betel nut sized swelling which gradually progressed to present size of a lemon, aggravating gradually in size over 2–3 days during which it is associated with pain and fever and subsides on taking medications.
Patient had similar complaints 5 years back on right side for which got admitted with history of fever, pain and swelling over right side of neck and was treated medically during episodes for about an year after which frequency of symptoms increased. Patient was subjected to ultrasonography(USG) of neck which revealed bilateral sub-mandibular, left jugular chain and posterior triangle lymphadenopathy.
Fine needle aspiration cytology(FNAC) showed dense acute inflammatory cell infiltrate, cellular debris and occasional macrophages with haemorrhagic background suggestive of suppurative inflammation.
Contrast enhanced Computerized Tomography(CECT) scan showed bilateral cervical lymphadenopathy with focal areas of necrosis/abscess-granulomatous infection, possibility of tuberculosis.
Tuberculin test was done to rule out tuberculosis and the test was positive(> 25 mm). Patient was put on anti-tubercular therapy for 6 months and had completed the treatment course. As the symptoms recurred after about an year, repeat aspiration cytology of lymph node was done which showed non-specific lymphadenitis on one node aspirate while other node aspirate showed necrotizing lymphadenitis. Since symptoms were recurring thereafter, excisional biopsy was planned.
Histopathology of excised lymph node revealed multiple lymph nodes exhibiting dilated sinuses filled with large histiocytes containing intact lymphocytes- Emperipolesis. Cells exhibited large and round morphology with vesicular nuclei with delicate nuclear membrane and prominent nucleoli. Reactive lymphoid follicles along with plasma cells were also noted. Features were suggestive of Rosai Dorfman disease.
Systemic examination, haematological investigations were normal. Ultrasonography of abdomen and pelvis was normal. Radiology of chest showed trachea deviated to right.
Patient has history of diminished vision in night since birth. Had ophthalmologic consultation and was diagnosed to have Retinitis Pigmentosa.
Head to toe examination revealed short stature, squint eyes, post-axial polydactyly of both upper and lower limb digits (Fig. 1).
Fig. 1.
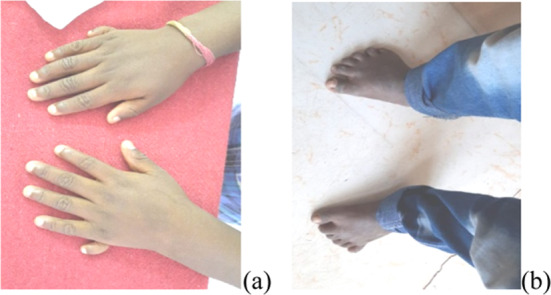
a Bilateral upper limb post-axial polydactyly; b Bilateral lower limb post-axial polydactyly
Examination of Neck
On inspection, swelling was present over left side of neck extending from about 1 cm below the lobule of ear to about 3–4 cms above the level of clavicle vertically. Swelling extended from mid and along the posterior border of sternocleidomastoid, upto the level of hairline posteriorly. Size of swelling was about 5*6 cms, overlying sternocleidomastoid. There was scar mark over right side of neck. (Fig. 2).
Fig. 2.

Left sided posterior neck swelling
On palpation, swelling was non-tender with no local rise of temperature, firm in consistency. All inspector findings were confirmed. Swellings were multiple and mobile in both vertical and horizontal planes. Skin over the swelling was normal and pinchable. Swelling was non-pulsatile.
There was another swelling present anterior to the first swelling. It extended from the angle of mandible on the left side diagonally down and medially till midline upto the level of thyroid cartilage. It was about 5cms below the lower margin of mandible and about 5 cms above the clavicle. Swelling was bout 6*1cms. Swelling was non-tender to touch with no local rise of temperature. All inspectory findings were confirmed on palpation. There were multiple swellings which were mobile. Skin over swelling was normal (Fig. 3).
Fig. 3.

Left sided anterior neck swelling
Trachea appeared to be pushed to right side (Fig. 4). There were no other swellings present in the neck.
Fig. 4.

Right sided tracheal deviation
With differential diagnosis of Rosai Dorfman disease, Tubercular lymphadenitis, Reactive lymphadenitis, Hodgkin’s/ non- Hodgkin’s lymphoma, Secondaries in neck and Immunological disorders, patient was subjected to ultrasonography of swelling & neck which showed lymphadenopathy. USG abdomen and pelvis, chest X-ray were normal. FNAC of node revealed features consistent with Rosai Dorfman Disease.
Patient was sent for syndromic evaluation to Paediatrician & was diagnosed with? Bardet Biedel Syndrome. The list of investigations patient underwent is listed in Table 1.
Table 1.
List of investigations
| Investigations | Reports |
|---|---|
| Complete haemogram | Hb: 10.4gm/dl |
| WBC: 17,300 cells/cumm | |
| Platelet count: 4.54 lakhs/cumm | |
| Neutrophils: 65% | |
| Lymphocytes: 30% | |
| Other tests | RBS: 80 mg/dl |
| Blood Urea: 17 mg/dl | |
| Sr. Creatinine: 0.8 mg/dl | |
| TSH: 1.11 mU/ml | |
| HIV: Negative | |
| Urine routine & microscopy: normal | |
| USG of swelling | Lymphadenopathy |
| USG of abdomen & pelvis | Normal |
| Chest X-Ray | Rotational deviation of trachea to right |
| FNAC of nodes | Features consistent with RDD |
| Ophthalmologic consultation: | |
| • Visual acuity | 6/12 |
| • Fundoscopy | Retinitis Pigmentosa changes |
| Paediatric consultation for syndromic evaluation | Clinical features consistent with ?Bardet Biedl Syndrome |
Discussion
RDD is histiocytic disorder described by Destombes for the first time in 1965 and later as ‘sinus histiocytosis with massive lymphadenopathy by Rosai and Dorfman in 1969. Disease is more common in first two decades of life [1]. 1/3rd cases show extra nodal involvement(43%) [2], skin lesions being more common contributing to 10%, with predilection for eyelids and malar area [1].
Our patient was 10 year old, presenting with cervical lymphadenopathy with occasional fever which was comparable with study done by Silky et al. [1] in study done by Ashutosh et al. [5], patient presented with lymphadenopathy but without fever. While in study done by Hashimoto et al. [6], 53 year old patient presented with massive cervical lymphadenopathy with fever (Table 2).
Table 2.
Discusssion for Rosai Dorfman Disease
| References | Presentation/ Investigations | Treatment |
|---|---|---|
| Our study |
Neck swelling, fever Normal blood tests Montoux test positive |
Symptomatic treatment: Antibiotics, antipyretics, analgesics, steroids Surgical excision of nodes for recurrence |
| Ashutosh et al. [5] |
Neck swelling Blood tests normal Montoux negative |
Oral steroids 4 months |
| Silky et al. [1] |
Neck swelling Montoux negative |
Oral steroids 1 month |
| Hashimoto et al. [6] |
Neck swelling CT- mediastinal, inguinal nodes MRI brain- malignant lesions |
Oral steroids Craniotomy |
| Karajgikar et al. [7] | Subcutaneous nodule, Soft tissue mass in pancreas, sacral mass | Clofarabine |
| Karajgikar et al. [7] | Medial left arm mass | Radiotherapy |
Disease is self-limited with unknown etiology; but, Herpes, Ebstein Barr, Cytomegalo and Human Immuno Deficiency virus could be causative organisms [2]. Most affected are lymph nodes, but multiple organs can be affected at same time.
Our patient had only involvement of lymph nodes while in study by Hashimoto et al. [6], along with cervical nodes, mediastinal & inguinal nodes with intracranial lesions was noted. In study by Karajgikar et al. [7], mass on medial arm & pancreas was noted (extra nodal involvement).
Typical pathological findings of disease show mature and immature lymphocytes and histiocytes with immunocytes, centroblasts, plasma cells and tingible body macrophages. Emperipolesis is a common histopathological finding which was similar to study done by Farooq Ahmed et al. [8] & Hashimoto et al. [6].
Several forms of therapy have been described like corticosteroids, chemotherapy for steroid refractory disease, early recurrence or when steroids are contraindicated. Radiotherapy is beneficial in refractory cases or to palliate local symptoms. Doses between 30 and 50 Gy have been employed. Partial or total surgical excision can be curative for unifocal disease and for upper airway obstruction. Surgery is indicated in symptomatic patients or in those with involvement of critical structures [5].
In our study, patient received corticosteroid therapy with tapering dose during acute episodes & symptoms subsided, which was similar with study done by Hashimoto et al. [3] where Prednisolone was used for cervical node while craniotomy & resection of intracranial mass was done (Table 2).
In our study, because of non-availability & denial by patient attender for chemotherapy or radiotherapy & as symptoms were frequently recurring, surgical excision was planned.
Bardet–Biedl syndrome (BBS) is ciliopathic human autosomal-recessive disorder. Primary features of disease include marked central obesity, retinal dystrophy, polydactyly, mental retardation, hypogonadism and renal dysfunction.
While secondary features of disease includes developmental delay, brachydactyly/syndactyly, delayed speech,cataract/strabismus/astigmatism, polyuria/polydipsia, diabetes mellitus, congenital heart disease, hepatic problems, dental crowding/hypodontia, high arched palate [4].
Our patient had short stature, low intelligence quotient(IQ), diminished vision in night(Retinitis Pigmentosa), post-axial polydactyly & squint eyes which are features of Bardet Biedel Syndrome which is comparable with study done by Kumar et al. [3] & Khan PA et al. [9] (Table 3).
Table 3.
Discussion for Bardet Biedel Syndrome
| References | Presentation | Treatment |
|---|---|---|
| Our study | Short stature, diminished vision, polydactyly, low IQ |
Regular follow-up Symptomatic treatment |
| Kumar et al. [3] |
Underdeveloped genitalia, diminished night vision, delayed development of milestones, low IQ, severe obesity Fatty liver, renal changes |
Regular follow-up Testosterone supplementation |
| Mahesh Dave et al. [4] |
Fever, vomiting, giddiness Diminished vision, polydactyly, obesity, low IQ |
Symptomatic treatment with regular follow-up |
| Khan et al. [9] | Weakness of both lower limbs, progressive loss of vision, obesity, polydactyly, developmental delay, low IQ, hypogonadism |
Testosterone supplementation Symptomatic treatment Regular follow-up |
Symptomatic treatment with testosterone hormone supplementation for hypogonadism & regular follow-ups is generally advised [3, 4, 9].
Syndromic association of Rosai Dorfman Disease with Bardet Biedel Syndrome is not found in any literature available, which needs further research.
Conclusion
Rosai Dorfman Disease & Bardet Biedel Syndrome are rare disorders presenting variably & imposing many diagnostic and therapeutic challenges.
Being a rare entity, high degree of clinical suspicion(RDD & BBS) with typical histopathological features(RDD) are diagnostic.
Medical line of treatment using antibiotics, steroids, chemotherapeutic agents are useful and surgical excision can be done for recurrent/complicated cases of RDD.
Regular follow-up and symptomatic treatment is important for BBS.
Multidisciplinary involvement is often important for evaluation and management of both disorders.
Cases presenting with RDD in association with BBS are rarer and needs further research.
Acknowledgements
None.
Abbreviations
- RDD
Rosai dorfman disease
- BBS
Bardet biedel syndrome
- FNAC
Fine needle aspiration cytology
- USG
Ultra sonography
- CECT
Contrast enhanced computed tomography
- IQ
Intelligence quotient
Funding
None.
Declarations
Conflict of interest
None.
Ethical approval
Study was approved by Institutional Ethical Committee (IEC).
Informed consent
Obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Silky S, Singh V, Kumar R, Chaudhary AK. Rosai Dorfman disease: a case report with nodal involvement. Int J Otorhinolaryngol Head Neck Surg. 2022;8(3):263–266. doi: 10.18203/issn.2454-5929.ijohns20220480. [DOI] [Google Scholar]
- 2.Kumar MB, Somaiah SA, Mohan M, Vittal R. Cutaneous emperipolesis: rosai–dorfman disease–an uncommon entity. Clin Dermatol Rev. 2023;7:80–83. doi: 10.4103/cdr.cdr_23_21. [DOI] [Google Scholar]
- 3.Kumar S, Mahajan BB, Mittal J. Bardet-Biedl syndrome: a rare case report from North India. Indian J Dermatol Venereol Leprol. 2012;78:228. doi: 10.4103/0378-6323.93656. [DOI] [PubMed] [Google Scholar]
- 4.Dave M, Goyal A, Saini RG, Dave G. Laurence-moon-bardet-biedl syndrome: a rare case report. Indian J Clin Pract. 2023;34(3):38–41. doi: 10.59793/ijcp.v34i3.573. [DOI] [Google Scholar]
- 5.Singh A, Kanaujiya SK. The rosai-dorfman disease: a differential diagnosis in cervical swelling. Indian J Otolaryngol Head Neck Surg. 2019;71(1):107–112. doi: 10.1007/s12070-017-1133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hashimoto K, Kariya S, Onoda T, Ooue T, Yamashita Y, Naka K, et al. Rosai-Dorfman disease with extranodal involvement. Laryngoscope. 2014;124:701–704. doi: 10.1002/lary.24290. [DOI] [PubMed] [Google Scholar]
- 7.Karajgikar J, Grimaldi G, Friedman B, Hines J. Abdominal and pelvic manifestations of Rosai-Dorfman disease: a review of four cases. Clin Imaging. 2016;40:1291–1295. doi: 10.1016/j.clinimag.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed F, Moinuddin M, Devani RG. Rosai-Dorfman disease (Sinus Histiocytosis With Massive Lymphadenopathy): a case report. RGUHS J Med Sci. 2018;8(1):37–39. [Google Scholar]
- 9.Khan PA, Nishaat J, Noor S, Fatima N. Laurence moon bardet biedl syndrome: a rare case report in a tertiary care teaching hospital, Hyderabad, Telangana. India Int J Med Public Health. 2017;7(1):68–71. doi: 10.5530/ijmedph.2017.1.13. [DOI] [Google Scholar]


