Abstract
To study the incidence and management of postoperative hypocalcemia in participants undergoing near-total (NTT) and total thyroidectomy (TT) at a tertiary health care center. This is an observational prospective study. Patients posted for NTT and TT in our institute and meeting the inclusion criteria were included. A total of 45 participants were enrolled. The serum calcium was measured on postoperative day 2, at the time of discharge and on 3 months follow-up. A combination of injectable and oral calcium supplements with or without vitamin D sachet was used for the treatment of hypocalcemia. Hypocalcemia was observed in 49% cases. Women were observed to develop hypocalcemia at a higher rate than men. Incidence of hypocalcemia was more in TT patients than NTT patients. Cases with malignant pathology were more susceptible to develop hypocalcemia than those with benign pathology. Operated TT with concomitant neck dissection were at higher risk for development of hypocalcemia. There was no significant association between age and incidence of hypocalcemia. Serum calcium measured on postoperative day 2 was a reliable indicator of risk of hypocalcemia. The early measurement of serum calcium level is a reliable indicator of the risk of hypocalcemia. Standardized treatment of hypocalcemic patients with calcium and vitamin D supplements can reduce the incidence and morbidity associated with postoperative hypocalcemia.
Keywords: Total thyroidectomy, Hypocalcemia, Near total thyroidectomy
Introduction
Postoperative hypocalcemia is a common complication following total thyroid resection. Its incidence varies in the current available literature. This stems from the fact that serum calcium recovers spontaneously within a few months, although, in a few patients, hypocalcemia can persist and is considered permanent.
Transient and permanent postoperative hypocalcemia are primarily due to the extent of damage to the parathyroid glands during the surgery. Familiarity with the anatomy and blood supply of parathyroid glands is necessary to prevent iatrogenic injury. The major difficulty lies in the fact that they may not be identified during surgery because they could be intrathyroidal, flattened subcapsular, hidden in the internodular grooves, or infiltrated by the thyroid tumor [1]. Despite the several advances, transient hypocalcemia can occur even in the hands of the most experienced thyroid surgeons [2]. This occurs due to the age, parathyroid gland handling, devascularization, venous congestion, post-surgical local site edema and central compartment neck dissection [3].
This leads us to a very important matter of being able to identify patients at risk for developing hypocalcemia due to its severe consequences on the patient’s physical and psychological state. It can be life threatening if acute and can impair the patient’s health, psyche and quality of life thereafter [4]. Care and treatment costs as well as the status of employee’s illness are therefore of economic relevance [4].
A review of the available literature reveals a broad range of criteria, definitions and parameters that have been used to define postoperative patients for hypocalcemia. Various institutional and individual surgeon protocols have been used to prevent, detect, and manage early postoperative hypocalcemia. Nevertheless, there is a lack of a definitive algorithm for its prevention, diagnosis, and treatment.
Thus, our goal is to study the incidence of hypocalcemia and their management in patients undergoing near total thyroidectomy (NTT) and total thyroidectomy (TT) in our institute, and compare the data with the available statistics in the current available literature.
Materials
This observational prospective study was conducted in the Department of ENT, from June 2019 to September 2021. Institutional Ethical Committee approval obtained as per requirements No.GMCS/STU/ETHICS/Approval/16921/19.
Inclusion criteria consisted of patients posted for NTT and TT. Those who underwent concomitant central compartment neck dissection and/ lateral compartment neck dissection (L-ND) were also included. Exclusion criteria consisted of patients who refused to give consent, those with a preoperative serum calcium level < 8 mg/dl and preoperative serum albumin < 3.4 gm/dl, patients that required definitive parathyroid resection, those already on calcium supplements and a history of prior thyroid surgery.
A total of 45 patients comprising 38 females and 7 males were enrolled in the study. Informed written consent was obtained from all participants.
The preoperative investigations included serum calcium, serum albumin, ultrasonography neck, fine needle aspiration cytology, thyroid function tests and radiological investigation (if any). Postoperative serum calcium on day 2, at the time of discharge and 3 months after surgery was noted. Serum PTH was done only for those patients whose serum calcium was found to be persistently low (less than 7 mg/dl) on day 2 and had symptoms of hypocalcemia.
Methodology
Serum calcium was measured on postoperative day 2 (POD-2) and the following protocol was followed depending on this value: Patients whose serum calcium was less than 7 mg/dl were given injectable calcium gluconate 1 ampule (10%) intravenously 8 hourly for 3–5 days, tapered and stopped by 7th postoperative day along with tablet calcium gluconate (500 mg) 2-2-2-2 with Vitamin D sachet (cholecalciferol-60,000 IU) once weekly. Simultaneously serum PTH was sent and if serum PTH value was less than 15 pg/ml, they were considered as a risk factor for permanent hypocalcemia and calcium was continued and monitored. Patients with serum calcium between 7–8 mg/dl were put on tablet calcium gluconate (500 mg) 2-2-2 with weekly Vitamin D sachet (cholecalciferol-60,000 IU). Those with serum calcium in the range of 8.1–8.4 mg/dl, were given tablet calcium gluconate (500 mg) 1-1-1 only. Normocalcemic patients were not given any calcium/ vitamin D supplements.
Repeat serum calcium was done at the time of discharge. Those patients whose serum calcium had improved from the POD-2 value and was between 7.5 and 8 mg/dl, were discharged on oral calcium supplements in the form of tablet Calcium gluconate (500 mg) 2-2-2 and Vitamin D sachet (cholecalciferol-60,000 IU) weekly. If the serum calcium was 8.1–8.4 mg/dl at the time of discharge, only tablet calcium gluconate (500 mg) 1-1-1 was given.
All patients were followed up until 3 months after surgery and serum calcium level was measured. Those patients whose serum calcium was between 7–8 mg/dl, were given tablet calcium gluconate (500 mg) 2-2-2 with vitamin D supplement and were stated to have permanent hypocalcemia. Those patients whose serum calcium was 8.1–8.4 mg/dl were given tablet calcium gluconate (500 mg) 1-1-1 with vitamin D sachet (cholecalciferol-60,000 IU) once weekly.
Signs of hypocalcemia in the form of facial paresthesia, tingling and numbness, positive Chvostek and Trousseau’s sign were noted in the post-operative period.
Normal serum calcium levels: 8.6–10.2 mg/dl, normal serum albumin levels: 3.5–5.2 gm/dl and serum PTH reference range: 4.7–130 pg/ml.
Those with serum PTH value less than 15 pg/ml on POD-2 were considered at risk for long term hypocalcemia, need for calcium supplementation and calcium monitoring. Hypocalcemia was defined as postoperative serum calcium less than 8.5 mg/dl. Duration of stay was calculated from the day of the surgery till the day of discharge.
Transient postoperative hypocalcemia was defined as hypocalcemia occurring in the first 48 h after the surgery and permanent hypocalcemia was stated if biochemical evidence of hypocalcemia were present at 3 month follow- up.
The data entry was done using Microsoft Office Excel Sheet (version 2008) and analyzed using SPSS ver.23. Analysis was done using frequency tables and charts. Data was expressed as mean ± standard deviation. The categorical demographic and clinical variables were expressed as number (percentage). Comparison of data was done using paired t tests, independent t test and chi-squared tests. Results were considered statistically significant when the 2-tailed P value was less than 0.05 with a confidence interval of 95%
Results
This study comprised a total of 45 patients operated by NTT 26/45 (58%) and TT 19/45 (42%). A total of 7 (16%) males and 38 (84%) females were studied.
Out of 45 patients, 22 (49%) developed hypocalcemia and 23 (51%) were normocalcemic. Of the 22 hypocalcemia patients, 12 (55%) were observed to have both laboratory (hypocalcemia on POD-2) and symptomatic hypocalcemia. 10 (45%) were observed to have only laboratory hypocalcemia.
“The figure below demonstrates this data (Fig. 1):”
Fig. 1.
Bar graph demonstrating patients with laboratory and/symptomatic hypocalcemia
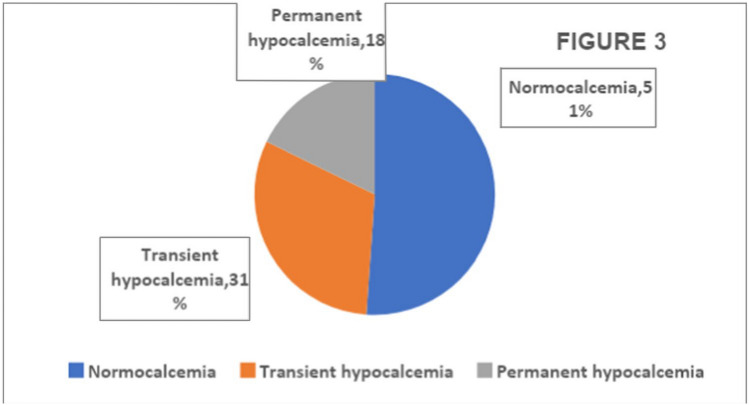
Of the 22/45 patients that developed hypocalcemia, 14 (31%) developed transient hypocalcemia and 8 (18%) developed permanent hypocalcemia.
“This information has been demonstrated in the figure given below (Fig. 2):”
Fig. 2.
Pie chart demonstrating number of patients with normocalcemia, transient and permanent hypocalcemia
Out of 26 NTT patients, 7 (27%) developed hypocalcemia and 18 were normocalcemic. Out of 19 TT patients, 14 (74%) developed hypocalcemia and 5 were normocalcemic.
“This data has been represented in the figure below (Fig. 3):”
Fig. 3.
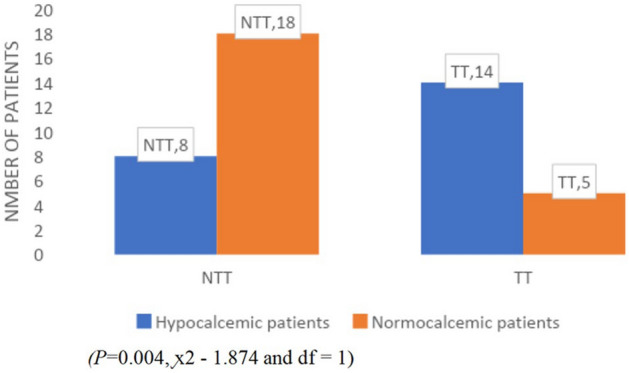
Bar graph demonstrating number of normocalcemic and hypocalcemia patients amongst NTT and TT operated patients
26 patients were operated with NTT. 7 (27%) developed transient hypocalcemia and 1 (4%) developed permanent hypocalcemia. 19 patients were operated with TT. 7 (50%) developed transient hypocalcemia and 7 (50%) developed permanent hypocalcemia.
“This data has been formulated in Table 1”
Table 1.
Data demonstrating number of transient and permanent hypocalcemia patients amongst NTT and TT patients
| Postoperative hypocalcemia | Number of TT patients | Number of NTT patients |
|---|---|---|
| Transient | 07 (27%) | 07 (50%) |
| Permanent | 01 (4%) | 07 (50%) |
| Total | 08 | 14 |
Amongst the 26 NTT patients, there were 23 females and 3 males. 8 females (35%) and zero males developed postoperative hypocalcemia. Amongst the 19 TT patients, there were 15 females and 4 males. 13 females (87%) and 1 male (33%) developed hypocalcemia.
“The table below demonstrates the following data (Table 2):”
Table 2.
Data demonstrating gender distribution, type of surgery and incidence of hypocalcemia
| Surgery | Number of males | Number of females | ||
|---|---|---|---|---|
| Number of Hypocalcemic patients | Number of normocalcemic patients | Number of Hypocalcemic patients | Number of normocalcemic patients | |
| NTT | 0 | 03 | 08 | 15 |
| TT | 01 | 03 | 13 | 02 |
| Total | 01 | 06 | 21 | 17 |
(P = 0.0.046, χ2–3.972 and degree of freedom (df) = 1)
The histopathology report of all 45 operated patients were classified into benign and malignant and the incidence of hypocalcemia was tabulated.
“Table 3 demonstrates the incidence of hypocalcemia based on the final histopathology report.”
Table 3.
Data to demonstrate final histopathology report and incidence of hypocalcemia
| Nature of thyroid pathology | Number of patients | Number of normocalcemic patients | Number of patients developing hypocalcemia | Percentage observed (%) | |
|---|---|---|---|---|---|
| Benign | 24 | 16 | 07 | 29 | χ2–4.99; df = 1; P = 0.012 |
| Malignant | 21 | 07 | 15 | 71 | |
| Total | 45 | 23 | 22 |
19 patients underwent TT. 10 (22%) underwent only TT. 3 (6%) patients underwent TT with CCND and 6 (13%) patients underwent TT with CCND and L-ND.
“The incidence of hypocalcemia in patients of TT with relation to neck dissection has been demonstrated (Table 4).”
Table 4.
Tabulation showing the type of surgery with/without neck dissection and incidence of hypocalcemia
| Variable | No. of patients | No. of patients developing hypocalcemia | No (%) | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| TT vs | 10 | 05 | 50 | 0.80 | 1.333 | 0.1655,10.74 |
| TT with CCND | 03 | 02 | 66.66 | |||
| TT vs | 10 | 05 | 50 | 0.2085 | 2 | 0.4204,9.515 |
| TT with CCND and SND | 06 | 06 | 1001 | |||
| TT with CND and L-ND vs | 06 | 06 | 100 | 0.3733 | 0.6667 | 0.08027,5.537 |
| TT with CCND | 03 | 02 | 66.66 |
We tabulated the data of NTT and TT patients based on the supplementation they received after postoperative day 2 serum calcium value.
“Table 5 demonstrates the above tabulated data”
Table 5.
Patients receiving intravenous and ora calcium supplementation, with/without vitamin D
| Number of patients | Number of NTT patients (percentage) | Number of TT patients (percentage) | P |
|---|---|---|---|
| No. of patients given intravenous, oral calcium and vitamin D supplementation | 01 (4%) | 06 (32%) |
χ2–7.9 df = 3 P = 0.004 |
| No. of patients given oral calcium and vitamin D supplementation | 06 (23%) | 05 (26%) | |
| No. of patients given oral calcium only | 04 (15%) | 03 (16%) | |
| No. of patients not requiring any calcium supplementation | 15(58%) | 05 (26%) | |
| Total | 26 | 19 |
Discussion
Postoperative hypocalcemia is notorious to increase the morbidity of its patients. Malignancy warrants lymph node dissection, which would entail extensive dissection with increased probability of vascular compromise to the parathyroid end arteries and inadvertent parathyroid injury. This is more noticeable in patients undergoing central compartment lymph node dissection [5]. Identification of such patients and their prompt supplementation with calcium and Vitamin D may be a useful approach in decreasing or preventing hypocalcemic morbidity and serve as a prophylactic tool in the prevention of hypocalcemic crisis [6]. Although in majority, hypocalcemia resolves spontaneously, it can remain prolonged in thyrotoxic osteodystrophy and persistent in devascularization and/or inadvertent removal of the parathyroid glands [6].
From the data we observed, the female to male ratio was 5:1 for the incidence of thyroid pathologies requiring surgeries amongst both the genders. This gross difference in sex distribution is due to the higher prevalence of thyroid disorders in females as reported in the literature [6, 9, 10].
Consequently, we observed that there was a significant association between the incidence of postoperative hypocalcemia and the female sex (P = 0.0.046). Our results are similar to Qubaisi and Haigh et al. [13], who stated that women were at a greater risk of hypocalcemia development compared to men (OR = 2.10; 95% CI = 1.14–3.87; p = 0.017).
Adding to the above results, we observed that the same female predominance in the development of transient and permanent hypocalcemia. These results were consistent with Noureldine et al. [19] who observed postoperative permanent hypocalcemia in only 2 patients (0.7%); both were females and both developed significant transient postoperative hypocalcemia. Male sex was found to be independently protective against postoperative hypocalcemia.
“Therefore, female gender appears to be a predisposing factor for the development of both transient and permanent hypocalcemia.”
Arumugam et al. [7] showed that thyroid diseases that required thyroid surgeries were frequent in the middle age group between 30 and 40 years. Tolone et al. [8], stated that the risk for postoperative hypocalcemia was increased 20-fold for patients older than 50 years (odds ratio [OR] 20.2; 95% confidence interval [CI] 10.4–58.3). In our study the incidence of postoperative hypocalcemia was observed to be higher in the age group of 41–50 years in NTT patients whereas in TT patients, the incidence was observed to increase with advancing age groups. We were unable to find a significant association between age and incidence of hypocalcemia.
In our study due to a small sample size, we were unable to find a correlation between the sub-classified thyroid pathologies (based on their final postoperative histopathology report) and incidence of transient and permanent hypocalcemia. However, when we grouped the thyroid pathologies into benign and malignant, we found that there was a significant association between incidence of hypocalcemia and benign or malignant nature of the thyroid pathology (P = 0.012; χ2–4.99; df = 1;)(Table 3). The reason for this was probably the rich vascularity of malignant tumors and the inability to find a proper plane of dissection which might lead to jeopardization of the vascular supply and/or damage to the parathyroid glands. Dhiman et al. [11] stated that the higher incidence of hypocalcemia in malignant conditions was because of excessive dissection required for resection of thyroid and clearance of lymph nodes. In contrast to this, Khazaeni and Mousavi et al. [12] said that the thyroid pathology was not significantly predictive of hypocalcemia.
There was observed to be a statistically significant association between incidence of hypocalcemia and the type of surgery (NTT/TT) (P = 0.004, χ2–1.874 and df = 1). Thus, we can say that the incidence of hypocalcemia was found to be greater in patients operated for TT than NTT (Table 1). These findings were very similar to those by Unalp et al. [2], Hosseini et al. [14] and Wang et al. [15].
From our study we observed that 7 out of 12 (58.3%) patients developed symptoms of hypocalcemia in less than 24 h of surgery. 5 participants developed hypocalcemia between 24 and 48 h after surgery. Also, as per Fig. 1, we observed that all asymptomatic postoperative participants need not be normocalcemic. Thus, to diagnose hypocalcemia, laboratory measurement is helpful in asymptomatic patients. Tredici et al. [16], found that a maximum of 36 h (morning of the second postoperative day) was necessary to observe a decrease in serum calcium levels. Sperlongano et al. [17] stated that the peak of hypocalcemia was on the first postoperative day. Ravikumar et al. [6] observed that the mean duration of onset of hypocalcemia was 27.43 ± 12.34 h.
Roh et al. [5] stated that postoperative hypocalcemia occurred far more commonly in neck dissection patients than no neck dissection participants (30.5 vs. 9.6%, P = 0.001). Tripathi et al. [18] stated more importantly that permanent hypocalcemia was more frequent in TT with neck dissection than in TT only (8.5 vs. 2.8%). We observed that the incidence of hypocalcemia was higher in patients who underwent TT with concomitant neck dissection (89%) than only TT (50%). We could not find a significant association (P = 0.09; OR-0.13; 0.004–1.38 CI).
Our observation was that patients who were put on a combination of calcium gluconate and vitamin D (cholecalciferol) supplements immediately after POD-2 calcium value, had a marked improvement in their calcium levels. Similarly Alhefdhi et al. [20], from the meta-analysis showed a significant decrease in the rate of symptomatic postoperative hypocalcemia between the groups treated with vitamin D along with calcium as compared to no prophylaxis or calcium alone. Bellantone et al. [21] also suggested that the administration of calcium supplements prevented the development of hypocalcemia after thyroid surgery. They also demonstrated that the combination of vitamin D and oral calcium supplements resulted in significantly higher serum calcium concentrations on the second and the third postoperative days thus, decreasing the incidence of hypocalcemia.
From our study we observed that all participants (6 out of 45) who had a postoperative serum PTH level on day 2 less than 15 pg/ml were at high risk for the development of permanent hypocalcemia. However, Kim et al. [22] said that a single PTH measurement on postoperative day 1 could accurately predict which patients were at risk of transient and permanent hypoparathyroidism after TT.
Clinical Significance
Early measurement of serum calcium levels on development of the signs/symptoms and/or on postoperative day 2 can enable the operating surgeon to detect hypocalcemia early. The early diagnosis of hypocalcemia will prompt the surgeon for the proper and immediate management of the same. Standardization of treatment of hypocalcemia can prevent morbidity associated with hypocalcemia.
Limitations
The emergence of the COVID-19 epidemic in India between 2020 and 2022 caused a temporary cessation of all planned surgeries for a significant period of 6–8 months. This was a major reason that affected the sample size of our study. The cessation of surgical procedures, conversion of our institute into a designated COVID care centre and the inability of several patients to come for follow- up due to the imposed lockdown further led to the shrinkage of the sample size. Secondly the association of other electrolytes (example magnesium) on the postoperative calcium levels could not be assessed due to a limitation in resources and the economic status of the patients catered at this center.
Funding
The authors did not receive support from any organisation for the submitted work.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Institutional Ethical Committee approval was obtained as per requirements No.GMCS/STU/ETHICS/Approval/16921/19.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rajinikanth J, Paul MJ, Abraham DT, Selvan CKB, Nair A. Surgical audit of inadvertent parathyroidectomy during total thyroidectomy: incidence, risk factors, and outcome. MedGenMed Medscape Gen Med. 2009;11(1):1–10. [PMC free article] [PubMed] [Google Scholar]
- 2.Unalp HR, Erbil Y, Akguner T, Kamer E, Derici H, Issever H. Does near total thyroidectomy offer advantage over total thyroidectomy in terms of postoperative hypocalcemia? Int J Surg. 2009;7(2):120–125. doi: 10.1016/j.ijsu.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Malik MZ, Mirza AA, Farooqi SA, Chaudhary NA, Waqar M, Bhatti HW. Role of preoperative administration of vitamin D and calcium in postoperative transient hypocalcemia after total thyroidectomy. Cureus. 2019;11(4):1–8. doi: 10.7759/cureus.4579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maschuw K, Schlosser K, Lubbe D, Nies C, Bartsch DK. Total versus near-total thyroidectomy in Graves ’ disease and their outcome on postoperative transient hypoparathyroidism: study protocol for a randomized controlled trial ? Trials. 2020;13:1–7. doi: 10.1186/1745-6215-13-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roh JL, Park JY, Il Park C. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg. 2007;245(4):604–610. doi: 10.1097/01.sla.0000250451.59685.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ravikumar K, Sadacharan D, Muthukumar S, Sundarram T, Periyasamy S, Suresh RV. A prospective study on role of supplemental oral calcium and Vitamin D in prevention of postthyroidectomy hypocalcemia. Indian J Endocrinol Metab. 2017;21(4):498–503. doi: 10.4103/ijem.IJEM_402_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arumugam S, Mohankumar A, Muthukumaraswamy A, Anandan H. Clinical study of hypocalcemia following thyroid surgery. Int J Sci Study. 2017;37:11. doi: 10.17354/ijss/2017/44. [DOI] [Google Scholar]
- 8.Tolone S, et al. The impact of age and oral calcium and vitamin D supplements on postoperative hypocalcemia after total thyroidectomy. A prospective study. BMC Surg. 2013;13(Suppl 2):S11. doi: 10.1186/1471-2482-13-S2-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baldassarre RL, Chang DC, Brumund KT, Bouvet M. Predictors of hypocalcemia after thyroidectomy: results from the nationwide inpatient sample. ISRN Surg. 2012;2012:1–7. doi: 10.5402/2012/838614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edafe O, Prasad P, Harrison BJ, Balasubramanian SP. Incidence and predictors of post-thyroidectomy hypocalcaemia in a tertiary endocrine surgical unit. Ann R Coll Surg Engl. 2014;96(3):219–223. doi: 10.1308/003588414X13814021679753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dhiman B, Dalal S, Dalal N, Raman S. Study of the incidence of hypocalcemia in patients undergoing bilateral thyroid surgery. Int Surg J. 2020;7(9):2914–2918. doi: 10.18203/2349-2902.isj20203767. [DOI] [Google Scholar]
- 12.Khazaeni K, Mousavi V. Surgical and clinical risk factors of postoperative hypocalcemia after total thyroidectomy. Am J Otolaryngol Head Neck Surg. 2019;2(1):2–6. [Google Scholar]
- 13.Al Qubaisi M, Haigh PI. Hypocalcemia after total thyroidectomy in graves disease. The Permanente J. 2020;23:1–9. doi: 10.7812/TPP/18-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosseini M, Otaghvar HA, Tizmaghz A, Shabestanipour G, Vahid PA. Evaluating the time interval for presenting the signs of hypocalcaemia after thyroidectomy. J Clin Diagnostic Res. 2016;10(3):PC19–PC22. doi: 10.7860/JCDR/2016/15274.7445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Orloff LA, et al. American thyroid association statement on postoperative hypoparathyroidism: diagnosis, prevention, and management in adults. Thyroid. 2018;28(7):830–841. doi: 10.1089/thy.2017.0309. [DOI] [PubMed] [Google Scholar]
- 16.Tredici P, Grosso E, Gibelli B, Massaro MA, Arrigoni C, Tradati N. Identification of patients at high risk for hypocalcemia after total thyroidectomy. Acta Otorhinolaryngol Italica. 2019;31(3):144–148. [PMC free article] [PubMed] [Google Scholar]
- 17.Sperlongano P, et al. Postoperative hypocalcemia: assessment timing. Int J Surg. 2014;12(S1):S95–S97. doi: 10.1016/j.ijsu.2014.05.042. [DOI] [PubMed] [Google Scholar]
- 18.Tripathi M, Karwasra RK, Parshad S. Effect of preoperative vitamin D deficiency on postoperative hypocalcemia after thyroid surgery. Thyroid Res. 2014;7(1):1–9. doi: 10.1186/1756-6614-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noureldine SI, Genther DJ, Lopez M, Agrawal N, Tufano RP. Early predictors of hypocalcemia after total thyroidectomy: an analysis of 304 patients using a short-stay monitoring protocol. JAMA Otolaryngol Head Neck Surg. 2014;140(11):1006–1013. doi: 10.1001/jamaoto.2014.2435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alhefdhi A, Mazeh H, Chen H. Role of postoperative vitamin D and/or calcium routine supplementation in preventing hypocalcemia after thyroidectomy: a systematic review and meta-analysis. Oncologist. 2013;18(5):533–542. doi: 10.1634/theoncologist.2012-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bellantone R, et al. Is routine supplementation therapy (calcium and vitamin D) useful after total thyroidectomy? Surgery. 2002;132(6):1109–1113. doi: 10.1067/msy.2002.128617. [DOI] [PubMed] [Google Scholar]
- 22.Kim H, et al. Prediction of transient and permanent hypoparathyroidism after total thyroidectomy using the postoperative serum parathyroid hormone test: when is the best time to check? J Endocr Surg. 2017;17(3):104. doi: 10.16956/jes.2017.17.3.104. [DOI] [Google Scholar]