Abstract
Rhinocerebralmucormycosis, is a progressive fungal invasion of a hard palate, paranasal sinuses, orbit, and brain. Post covid the huge number of mucor cases reported in our institute. To combat them a uniform assessment scale was needed as multiple healthcare workers were involved. Thus, a novel linear grading system on nasal endoscopy was developed for the early management of patients to prevent morbidity and mortality. A Prospective study of 650 patients in Epidemic duration from April to June 2021 in a tertiary health center, Central India. Patients subjected to Nasal Endoscopy with 0degree 4 mm Telescope and classified into 5 categories according to the severity of the disease. In a novel grading system, minimum patients were of grade 0, maximum was in Grade I. Maxillary sinus was most commonly involved. This novel grading system on nasal endoscopy makes the management of patients much easier in an epidemic, reducing human errors, morbidity, and mortality of the fulminant disease.
Keywords: Mucormycosis, Nasal endoscopy, Grading system
Introduction
Coronavirus disease 2019 (COVID-19) is a highly infectious disease caused by newly discovered novel severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2), affecting more than 20 million people in India [1]. India has a high prevalence rate of type 2 diabetes mellitus (8.9% of adults, 77 million patients), which is a well-known risk factor to develop mucormycosis [2]. The widespread use of steroids or monoclonal antibodies, or broad-spectrum antibiotics as part of the armamentarium against COVID-19 infection may lead to the development of fungal disease in covid 19 patients [3]. During the coronavirus disease pandemic, the prevalence of paranasal mucormycosis is on the rise, probably due to systemic immune alterations due to Coronavirus infection [4]. Alternations in innate immunity associated with COVID-19 may be due to the reduced number of T lymphocytes, CD4 + T helper, and CD8 + T cells [5]. It is assumed that the port of entry is a colonization of the nasal mucosa, allowing the fungus to spread via the paranasal sinuses into the orbit [6]. The fungus invades the arteries leading to thrombosis that subsequently causes necrosis of the tissue resulting in gangrene therefore infection spread to orbital and intracranial structures either by direct invasion or through the blood vessels resulting in rhinocerebral mucormycosis, characterized by progressive fungal invasion of the paranasal sinuses, hard palate, orbit and brain [7].
There are various diagnostic modalities for the suspicious Mucor infection namely MRI PNS + Brain + Orbit, wet KOH mount, Biopsy, etc. [8]. Nasal Endoscopy in these cases is an important primary diagnostic tool.
Nasal Endoscopy showing the change within the normal appearance of the nasal mucosa is the most consistent finding [9]. The main findings include black necrotic eschar tissue with underlying purulent exudates with an unpleasant odour [10]. The presence of black discoloration of mucosa indicates tissue ischemia which is secondary to the angiocentric invasion. In high-risk suspected patients, surgeons while performing nasal endoscopy should be careful to inspect the common sites for mucormycosis, which includes middle turbinate (67%), septum (24%), palate (19%), and inferior turbinate (10%) [9]. If there is decreased mucosal bleeding and/or sensation to touch during endoscopy in these areas, then it may be a sign of fungal disease and a biopsy should be performed [11]. To combat these, a uniform assessment scale was needed as multiple healthcare workers were involved. Nasal Endoscopy is the early or can be described as first investigation that can be done in quick time, less manpower, direct real visualization of the mucosal changes and also pocket friendly. In the Novel Grading system used in this study, grade 0 is having normal mucosal findings which are devoid of any kind of disease, grade I is considered when the mucosal lining of nasal cavity is congested erythema present and edematous these cases are to be subjected for wet KOH mount preparation as a gold standard test to differentiate from other allergic and infective disease of nose. Grade II shows thick purulent secretion in middle meatus and choana, this is suspicious so also subjected to wet KOH mount. Grade III having blackening of middle turbinate and nasal mucosa and Grade IV showing black necrotic eschar tissue with underlying purulent exudates, were considered to be cases of mucormycosis and were subjected to debridement without waiting for KOH mount report during epidemic scenario. Thus, this study describes the approach for the primary diagnosis and management of the disease based on the Nasal Endoscopy that optimizes the line, time, and appropriate management to people in this epidemic.
Materials and Method
A Prospective study was conducted on 650 patients who reported and were admitted in the Epidemic from April 2021 to June 2021 in the tertiary health care center in central India.
Inclusion Criteria: In our study, patients who were admitted to M.Y. Hospital, Indore with symptoms suggestive of mucormycosis like headache, vision abnormality, facial pain, facial weakness, nasal obstruction, nasal discharges, with or without a history of Covid-19 infection.
Exclusion Criteria: Patients who did not give consent for endoscopy, patients having atrophic rhinitis, benign and malignant lesions of the nasal cavity, patients of mucormycosis operated for ESS before the study.
All patients were subjected to diagnostic Nasal Endoscopy with 0 degree 4 mm Nasal Telescope and were classified into 5 categories based on the endoscopic finding.
All patients were subjected to Magnetic Resonance Imaging (MRI) paranasal sinus, brain, and orbit, and wet KOH mount to differentiate congestion and edema present in nasal mucosa of mucor patients pre-operatively. Routine blood investigations were done and patients were taken for Endoscopic Sinus Surgery (ESS) with Nasal Cavity Debridement under TIVA/GA. Biopsy was sent for histopathological examination in an operated patient.
We developed a unique and novel grading system to segregate and triage the patients based on nasal endoscopy findings (Table 1, Fig. 4).
Table 1.
Novel nasal endoscopic grading system
| Grade | Nasal Endoscopy Findings |
|---|---|
| 0 | Normal pink nasal mucosa |
| I | Congestion and edematous nasal mucosa |
| II | Thick purulent secretion in middle meatus and choana |
| III | Blackening of middle turbinate and nasal mucosa |
| IV | Black necrotic eschar tissue with underlying purulent exudates |
Fig. 4.
Nasal Endoscopy view of Grades in Novel Grading System. a Grade 0: Normal pink nasal mucosa. b Grade 1: Congestion and edematous nasal mucosa. c Grade II: Thick purulent secretion in middle meatus and choana. d Grade III: Blackening of middle turbinate and nasal mucosa. e Grade IV: Black necrotic eschar tissue with underlying purulent exudates
Results
The study was conducted on 650 patients who were subjected to Diagnostic Nasal Endoscopy using a 0-degree telescope. Among 650 patients, there were 505 (77.7%) males and 145 (22.3%) females, which is a 3.5:1 ratio (Fig. 1). The Novel grading System for Nasal Endoscopy that was used in the study was classified into 5 grades as described earlier (Table 1). In Grade 0 there were 11(1.7%) patients which were minimum who reported, maximum patients were in Grade I which have 275 (42.3%) followed by Grade II—179 (27.5%), Grade III—115 (17.7%), and Grade IV—70 (10.8%) (Table 2). There were 205(31.5%) patients reported from the 5th decade of life among 650 patients which were followed by the 6th decade having 175(26.9%) and least were from 9th decade 7(1.1%) (Table 3).
Fig. 1.
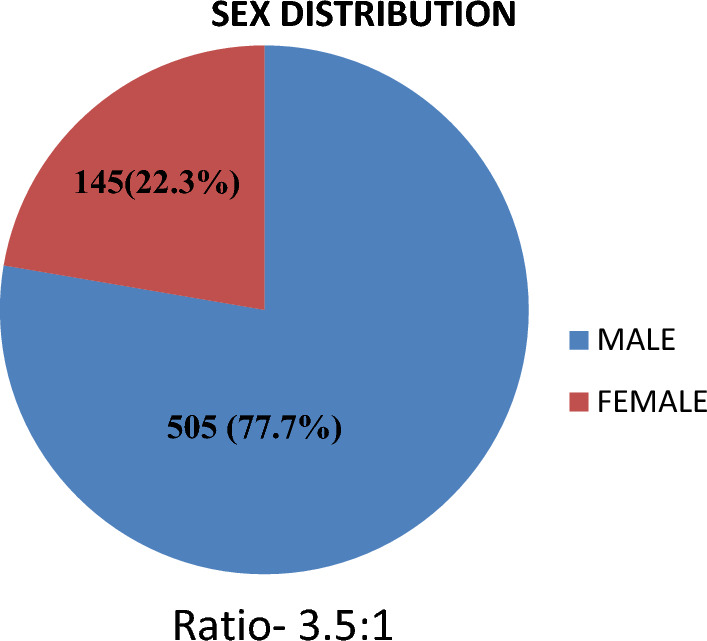
Sex Distribution of total Study patients
Table 2.
Distribution of patients according to novel grading system
| Grade | Nasal endoscopy findings | No. of patient | % Distribution |
|---|---|---|---|
| 0 | Normal nasal mucosa | 11 | 1.7 |
| I | Congestion and edematous nasal mucosa | 275 | 42.3 |
| II | Thick purulent secretion in Middle meatus and Choana | 179 | 27.5 |
| III | Blackening of middle turbinate and nasal mucosa | 115 | 17.7 |
| IV | Black necrotic eschar tissue with underlying purulent exudates | 70 | 10.8 |
| Total | 650 |
Table 3.
Age distribution
| Age group (in years) | Total = 650 | Grade 0 | Grade 1 | Grade 2 | Grade 3 | Grade 4 |
|---|---|---|---|---|---|---|
| 20–30 | 26 (4%) | 5 | 10 | 8 | 2 | 1 |
| 31–40 | 74 (11.4%) | 2 | 25 | 35 | 9 | 3 |
| 41–50 | 205 (31.5%) | 3 | 112 | 41 | 32 | 17 |
| 51–60 | 175 (26.9%) | 1 | 77 | 50 | 28 | 19 |
| 61–70 | 129 (19.9%) | 0 | 49 | 40 | 24 | 16 |
| 71–80 | 34 (5.2%) | 0 | 2 | 4 | 18 | 10 |
| 81–90 | 7 (1.1%) | 0 | 0 | 1 | 2 | 4 |
In Grade 0 maximum patients were from the 3rd decade having 5 patients, Grade I and Grade III have maximum from 5th decade having 112 and 32 patients respectively while Grade II and Grade IV has maximum from 6th decade having 50 and 19 patients respectively (Table 3). Surprisingly Grade I was a common and mostly seen nasal endoscopy finding in all decades of life that were under the study (Table 3).
The MRI PNS out of 650 patients shows the involvement of Maxillary sinus in 479 patients, showing the commonest sinus to be involved is maxillary sinus, ethmoid sinus was involved in 401 patients, sphenoid sinus in 282 patients, and frontal sinus was least involved in 128 patients. The sinus involvement in MRI PNS in different 5 grades is shown in Table 4.
Table 4.
Nasal endoscopy grade and paranasal sinus status on MRI
| Grade | Maxillary sinus | Ethmoid sinus | Sphenoid sinus | Frontal sinus |
|---|---|---|---|---|
| Grade 0 | 2 (18%) | 2 (18%) | 1 (9%) | 0 (0%) |
| Grade I | 158 (57.4%) | 104 (37.8%) | 58 (21%) | 15 (5%) |
| Grade II | 136 (76%) | 117 (65.3%) | 78 (43.5%) | 27 (15%) |
| Grade III | 113 (98.2%) | 111 (96.5%) | 86 (74.8%) | 43 (37.4%) |
| Grade IV | 70 (100%) | 67 (95.7%) | 59 (84.3%) | 43 (61.4%) |
| Total | 479 (73.7%) | 401(61.7%) | 282(43.4%) | 128(19.7%) |
Wet KOH mount test was done only in Grade 0, I, II showing positive results 0, 81(30%), and 90 (50.2%) respectively (Fig. 2).
Fig. 2.
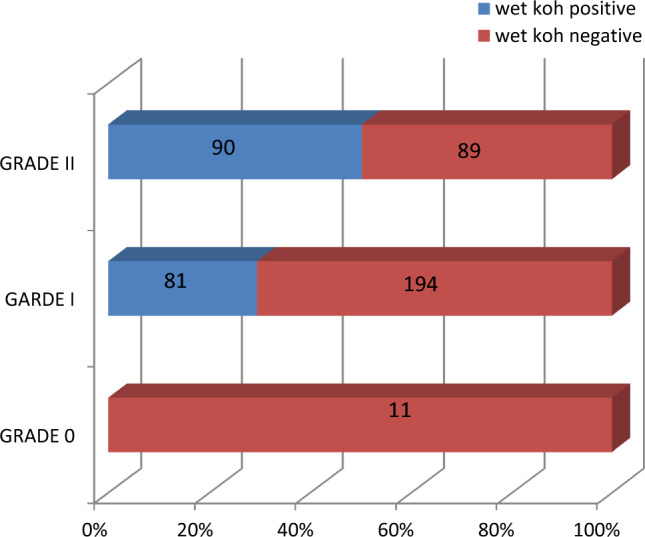
Wet KOH mount status in Grade 0, I and II
The 380 patients out of 650 were operated on for nasal cavity debridement and Endoscopic Sinus Surgery (ESS). In Grade 0 none of the patients were operated, Grade I 91(33.1%) out of 275 patients, Grade II 104(58.1%) out of 179 patients while in Grade III and Grade IV 100% that is 115 and 70 patients respectively were operated (Fig. 3).
Fig. 3.
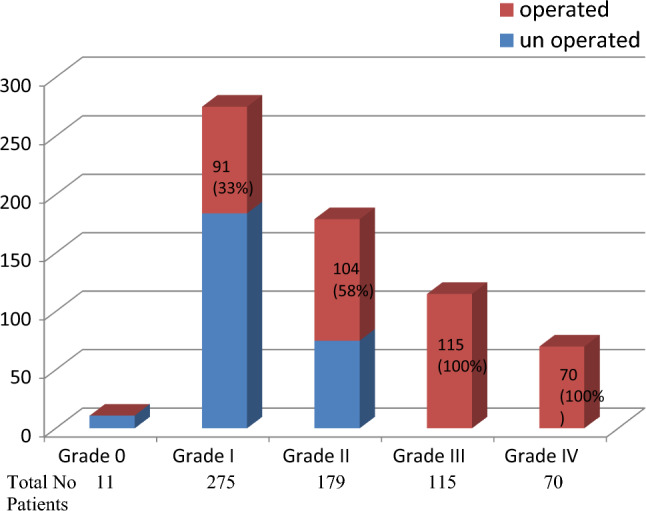
ESS and Debridment from Grading System. NS- Nasal Septum, LNW- Lateral Nasal Wall, MT- Middle Turbinate
Discussion
The Rhino-orbital- cerebral infection is the most typical presentation of mucormycosis where there is an invasion of the fungal infection from paranasal sinuses to palate, orbit, and brain [7], 12. Mucormycosis is caused by fungi in the order Mucorales, including Mucor, Rhizopus, and Absidia species [13]. The spores invade the nasal mucosa and are not phagocytized which then germinate, forming angioinvasive hyphae that cause infarction of the involved tissue, which leads to gangrene. Invasion occurs with spread to the maxillary sinuses and subsequent orbital spread through the ethmoid sinuses [14]. Extension of the disease leads to vascular thrombosis, including the cavernous sinus and other cerebral vessels due to fibrin reaction and thrombus formation. Subsequent thrombosis may develop eschar formation or cerebral infarctions which eventually in some cases can lead to coma or death. The morbidity and mortality rate of mucormycosis is high and within as little as 2 weeks death may occur. Cranial nerve palsies and blindness are major sequelae of the disease because of its aggressively invasive nature. Thus, early detection and treatment are important factors resulting in the disposition of the patient with a substantial decrease in mortality. Diseased tissues are more susceptible to necrosis and devitalization, which leads to a lack of contrast enhancement seen on Magnetic Resonance Imaging (MRI) scan "the black turbinate sign," a feature that can aid in earlier detection of the disease [15] (Fig. 4, 5).
Fig. 5.
MRI Scan showing the Paranasal Sinuses involvement. a Coronal view showing Frontal, Ethamoid and Maxillary Sinus involvement. b Coronal view showing bilateral Ethmoid and Maxillary Sinus involvement. c Axial view showing sphenoid sinus involvement
Nasal Endoscopy aids in the early detection and management of the disease [9].
In our study, 650 patients were considered out of which 505 (77.7%) were males and females were 145(22.3%). In a study, Singh et al. [16] also show male dominance of 78.9%. The maximum mucormycosis patients in this epidemic come from the 5th decade of life which accounts for 31.5% followed by the 6th decade 26.9%. The incidence increases from 3rd decade to 5th decade then start decreasing to 9th-decade accounts only 1.1% of the total study population.
There is always a need for protocol and guidelines to manage an epidemic so we have tried to develop a new grading system for the condition based on the data available at our center to manage the bulk of patients reported for sake of appropriate treatment. According to the Novel Grading System that we used in this epidemic in our center for Diagnostic Nasal Endoscopy, 1.7%(11) patients were in Grade 0, 42.3%(275) in Grade I, 27.5%(179) in Grade II, 17.7%(115) in Grade III, 10.8%(70) in Grade IV shows the maximum number of patients were in Grade I and II having a very mild disease in which progression of the disease is slow and can be managed on a medical basis with amphotericin B, surgical management is least required in these patients that is why only 33% and 58% of patients were taken for surgical nasal debridement and ESS based on several grounds which are:-
MRI suggestive of paranasal sinus involvement.
Wet KOH mount if found to be positive.
The sensitivity of wet KOH mount in mucormycosis is 84% [17]. The wet KOH mount was only done in Grade 0, I and II, and positive patients were operated on. In Garde III and IV the fungal appearance was clear in the endoscopy picture therefore all patients were managed surgically. Most of the patients were from the 5th decade of life 205(31.5%), while the least was seen from the 9th decade only 1.1%. In the 3rd to 7th decade of life except for the 4th decade most of the patients were having Grade I, while in the 4th decade Grade II was common. In the 8th decade of life, most of the patients were having Grade III, whereas in the 9th decade most belongs to Grade IV.
On MR imaging, there is variable intensity within the sinuses on T1- and T2-weighted images are usually seen. Fungal elements themselves can cause a low signal intensity on T2 sequences [15]. Tamijeselvan [18] show that most patients had a primary disease infection involving the ethmoid sinus air cells. In most of the cases, the maxillary sinus was affected. Sphenoid and frontal involvement was less common. The maxillary sinus is a common sinus involved found in 73.7% of patients in overall grades. The frontal sinus is the least common sinus involved only in 19.7%. Ethmoid sinus in 61.7% while sphenoid sinus in 43.4%. In our Novel grading system also Maxillary sinus is commonly involved in all grades and the least is the frontal sinus.
Based on the Grading system the patients were grouped and subjected to ESS and nasal cavity debridement. Grade III and IV all 100% patients were operated, in grade 0 none of the patients were taken and were discharged. In grades, I and II based on criteria cited above 33% (91) and 58% (104) were operated. In this epidemic, this grading system makes the management of a large number of patients easier. Appropriate time, treatment, and resources can be given to the required patients. All patients after this management protocol stood well and were successfully discharged with only an 8% mortality rate.
Conclusion-
Mucormycosis is a rapidly growing epidemic disease with high morbidity and mortality rate in a covid era. Presently, the triad of clinician's awareness, prompt diagnosis, and timely surgical treatment of rhino-orbital mucormycosis is the "sine qua non" as antifungal drugs and surgical debridement can successfully control the infection and thus reduce the high mortality and morbidity associated with mucormycosis represent the effective way of managing the disease for which this Novel Grading System is useful. ENT surgeons with nasal endoscopy can make early diagnoses and immediately classify the severity of disease, this grading system can help to develop uniformity in treatment protocol in the massive number of patients in an epidemic. As there are multiple health workers and teams involved, this grading system can also be used by ophthalmologists and maxillofacial surgeons for the management.
Summary
Mucormycosis was reported in large number in post covid patients with high morbidity and mortality rate
At present, there is no Nasal endoscopic grading system for categorizing the severity of the Mucormycosis.
The triad of clinician's awareness, prompt diagnosis, and timely surgical treatment of rhinoorbital mucormycosis is the "sine qua non" as antifungal drugs and surgical debridement can successfully control the infection.
ENT surgeons with nasal endoscopy can make early diagnoses and can immediately classify the severity of disease based on this novel grading system and can help multiple health team members involved like ophthalmologists and maxillofacial surgeons to take needful interventions for the management.
This grading system can help to develop uniformity in treatment protocol in the bulk number of patients in an epidemic resulting in the reduction of human errors, higher mortality, and morbidity of the fulminant disease.
Acknowledgements
The Authors acknowledge Dr. Sanjay Dixit, Dean and CEO of MGMMC, Indore and Dr. PS Thakur, Superintendent, MYH, Indore for providing advice and support for management of these cases.
Funding
The authors did not receive support from any organization for the submitted work.
Declarations
Conflict of interests
The author(s) declare none.
Ethical Approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation (please name) and with the Helsinki Declaration of 1975, as revised in 2008.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.India: WHO Coronavirus Disease (COVID-19) Dashboard with vaccination data [Internet]. [cited 2023 Nov 3]. Available from: https://covid19.who.int
- 2.International Diabetes Federation. [Jul;2020 ]; https://idf.org/our-network/regions-members/south-east-asia/members/94-india.html 2020.
- 3.Rhino-Orbital Mucormycosis Associated With COVID-19 [Internet]. [cited 2021 Apr 30]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7599039/
- 4.Mehta S, Pandey A. Rhino-orbital mucormycosis associated with COVID-19. Cureus. 2020;12(9):e10726. doi: 10.7759/cureus.10726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gangneux JP, Bougnoux ME, Dannaoui E, Cornet M, Zahar JR. Invasive fungal diseases during COVID-19: we should be prepared. J Mycol Med. 2020;30:100971. doi: 10.1016/j.mycmed.2020.100971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hosseini SMS, Borghei P. Rhinocerebral mucormycosis: pathways of spread. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg. 2005;262(11):932–938. doi: 10.1007/s00405-005-0919-0. [DOI] [PubMed] [Google Scholar]
- 7.Garlapati K, Chavva S, Vaddeswarupu RM, Surampudi J. Fulminant mucormycosis involving paranasal sinuses: a rare case report. Case Rep Dent. 2014;2014:1–4. doi: 10.1155/2014/465919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Awal SS, Biswas SS, Awal SK. Rhino-orbital mucormycosis in COVID-19 patients—a new threat? Egypt J Radiol Nucl Med. 2021;52(1):152. doi: 10.1186/s43055-021-00535-9. [DOI] [Google Scholar]
- 9.Singh VP, Bansal C, Kaintura M. Sinonasal Mucormycosis: A to Z. Indian J Otolaryngol Head Neck Surg. 2019;71(Suppl 3):1962–1971. doi: 10.1007/s12070-018-1384-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lunge SB, Sajjan V, Pandit AM, Patil VB. Rhinocerebrocutaneous mucormycosis caused by Mucor species: a rare causation. Indian Dermatol Online J. 2015;6(3):189–192. doi: 10.4103/2229-5178.156393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spellberg B, Edwards J, Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005;18(3):556–569. doi: 10.1128/CMR.18.3.556-569.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferguson BJ. Mucormycosis of the nose and paranasal sinuses. Otolaryngol Clin North Am. 2000;33(2):349–365. doi: 10.1016/S0030-6665(00)80010-9. [DOI] [PubMed] [Google Scholar]
- 13.Hibbett DS, Binder M, Bischoff JF, et al. A higher-level phylogenetic classification of the fungi. Mycol Res. 2007;111(pt 5):509–547. doi: 10.1016/j.mycres.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Horger M, Hebart H, Schimmel H, Vogel M, Brodoefel H, Oechsle K, et al. Disseminated mucormycosis in haematological patients: CT and MRI findings with pathological correlation. Br J Radiol. 2006;79(945):e88–95. doi: 10.1259/bjr/16038097. [DOI] [PubMed] [Google Scholar]
- 15.Safder S, Carpenter JS, Roberts TD, Bailey N. The, “black turbinate” sign: an early MR imaging finding of nasal mucormycosis. Am J Neuroradiol. 2010;31(4):771–774. doi: 10.3174/ajnr.A1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15(4):102146. doi: 10.1016/j.dsx.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bala K, Chander J, Handa U, Punia RS, Attri AK. A prospective study of mucormycosis in north India: experience from a tertiary care hospital. Med Mycol. 2015;53(3):248–257. doi: 10.1093/mmy/myu086. [DOI] [PubMed] [Google Scholar]
- 18.Tamijeselvan S. CT and MR Imaging in the diagnosis of mucormycosis in COVID-19 era - an overview. Int J Sci Healthc Res. 2021;6(2):222–227. doi: 10.52403/ijshr.20210440. [DOI] [Google Scholar]




