Abstract
Myringoplasty is still the most performed otological surgery. Nevertheless, the underlay vs. overlay approaches have yet to be determined. The purpose of this study is to compare the surgical and audiological outcomes of underlay and overlay myringoplasty in perforated tympanic membrane patients. A systematic review and meta-analysis synthesizing randomized controlled trials (RCTs), which were retrieved by systematically searching of Web of Science, SCOPUS, PubMed, and Google Scholar until January 25th, 2023. RevMan version 5.4 software was used to pooled dichotomous outcomes using the risk ratio (RR) with the corresponding 95% confidence interval (CI). We registered our protocol in PROSPERO with ID: [CRD42023387432]. We included eight RCTs with 656 tympanic perforation membrane patients. Four RCTs had a low risk of overall bias, two had some concerns, and two had a high risk of bias. The underlay technique was significantly associated with a higher surgical success rate (n = 7 RCTs, RR: 1.21 with 95% CI [1.02, 1.43], P = 0.03) and audiological success rate (n = 4 RCTs, RR: 1.31 with 95% CI [1.18, 1.44], P < 0.00001). This meta-analysis underscores the potential superiority of the underlay technique in managing tympanic membrane perforations, with significant implications for surgical and audiological outcomes. However, more investigations are still necessary to confirm this result.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12070-023-04425-6.
Keywords: Myringoplasty, Underlay, Overlay, Tympanoplasty, Surgical Success rate
Introduction
Tympanic membrane (TM) perforations pose a challenging clinical scenario in otolaryngology. Different etiologies, such as chronic otitis media, traumatic injuries, or previous surgeries, can cause these perforations, which frequently result in conductive hearing loss, recurrent infections, and decreased quality of life for those affected. Although TM perforations mostly heal spontaneously (about 80% of the cases), many cases require surgical intervention to waterproof the ear, and to improve conductive hearing loss. The decision to perform surgical intervention for TM perforations depends on many factors, including the location, size, and chronicity of the perforation, in addition to the severity of the patient’s symptoms and their personal preferences.
Myringoplasty is a surgical intervention used to restore the damaged TM and avoid future consequences of chronic otitis media [1]. It is also known as tympanoplasty type-I, in which the middle ear components are exposed and evaluated for functional integrity throughout the procedure [1, 2]. Myringoplasty can be performed using various surgical approaches, which include postaural, endaural, and endomeatal techniques [3, 4]. A range of graft materials, such as temporalis fascia, vein grafts, and perichondrium, may be employed in these procedures [5, 6]. While the medical literature presents several myringoplasty procedures, encompassing methods like the underlay technique, the “Swinging Door” technique, the overlay technique, the tipple “C” technique, the “Gelfilm Sandwich” technique, and others [1, 3, 4, 6–11], it is worth noting that there are two established and widely recognized methods of myringoplasty: the overlay technique and the underlay technique [4, 7, 12, 38].
Underlay myringoplasty includes inserting the graft material beneath the borders of the tympanic membrane perforation, forming a seal between the graft and the surrounding tissue [13, 14]. The goal of this procedure is to restore the tympanic membrane’s integrity while minimizing the danger of graft displacement and failure [3, 14]. On the other hand, the overlay myringoplasty procedure inserts the graft material directly over the perforation, allowing it to adhere to the residual eardrum [13]. This method attempts to directly cover the perforation, potentially simplifying the surgical operation [13, 15]. These two surgical procedures have been used with various degrees of success, and the best choice of them remains a source of debate among otolaryngologists.
While the underlay approach may exhibit a higher success rate, the determination of which surgical procedure yields superior outcomes remains a subject of debate [12]. The overlay approach demonstrates a propensity for achieving superior anatomical outcomes, whereas the underlay technique tends to excel in functional outcomes [12]. Some professionals believe that the overlay approach is better for healing large and anterior perforations, whereas the underlay technique is better for treating posterior perforations [16]. However, an alternative study has reported that a combination method incorporating both techniques yielded the highest overall success rate [17].
The aim of this systematic review and meta-analysis is to resolve this controversy by comparing the outcome of graft uptake by underlay and overlay techniques in myringoplasty patients.
Methods and Materials
Protocol Registration
The methodological plan of this systematic review and meta-analysis was registered and published on PROSPERO with ID: [CRD42023387432]. We followed the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [18] and the Cochrane Handbook of Systematic reviews and meta-analysis version 6.2 [updated February 2021] [19].
Data Sources and Search Strategy
Two reviewers independently conducted an electronic systematic search on PubMed, Web of Science, SCOPUS, Google Scholar, and Cochrane Central Register of Controlled Trials (CENTRAL) until January 25th, 2023. The search strategy for each database is illustrated in Table S1.
Eligibility Criteria
Randomized control trials (RCTs) comparing underlay and overly techniques were included. A PICO criterion was used to include RCTs: population (P): Patients with dry ears and central tympanic membrane perforation, undergoing myringoplasty; intervention (I): underlay technique regardless the graft material; control (C): overlay technique regardless the graft material; and outcomes (O): surgical success rate (%) and audiological success rate (%).
Animal studies, pilot studies, case reports, case series, cohort studies, case-control studies, single-arm clinical trials, non-randomized trials, in vitro studies (tissue and culture studies), book chapters, editorials, press articles, and conference abstracts were excluded from our analysis.
Selection Process
Two reviewers individually screened the title and abstract via Rayyan website [20] after excluding duplicates. Then, full-text screening was conducted by the same reviewers using the previously stated eligibility criteria. A third reviewer was added to resolve any conflicts.
Data Extraction
Two independent investigators extracted the following data from the included studies using a previously pilot-tested extraction excel sheet: summary characteristics (first author last name, year of publication, country, total participants, recruitment period, and type of technique, surgery type, and graft type); baseline data (sex, age, perforation size, type of anesthesia, and follow-up); and outcomes [surgical and audiological success rates (%)]. Disputes were discussed and solved through consensus.
Risk of bias and Quality Assessment
Two independent investigators assessed the quality of the studies independently using the Cochrane RoB-2 tool [21]. The evaluated domains included the risk of bias resulting from the randomization process, the risk of bias due to deviation from the intended intervention, the risk of bias due to missing outcome data, the risk of bias in measuring the outcome, and the risk of bias in selecting the reported results. In the event of any disagreements, the reviewers discussed and resolved them through consensus.
Statistical Analysis
RevMan version 5.4 [22] was used to pool dichotomous outcomes using risk ratio (RR) presented with the corresponding 95% confidence interval (CI). We used a random-effect model in case of significant heterogeneity. Heterogeneity was evaluated using two methods: I-square and Chi-square tests; the Chi-square test assesses whether there is significant heterogeneity, while the I-square evaluates the magnitude of heterogeneity. According to the Cochrane Handbook (chapter nine) [19], an alpha level below 0.1 is considered to be a significant heterogeneity for the Chi-square test, while in the I-square test, a value of ≥ 50% suggests significant heterogeneity. Finally, we did not investigate the publication bias by funnel plots as we included less than ten RCTs [23].
Results
Search Results and Study Selection
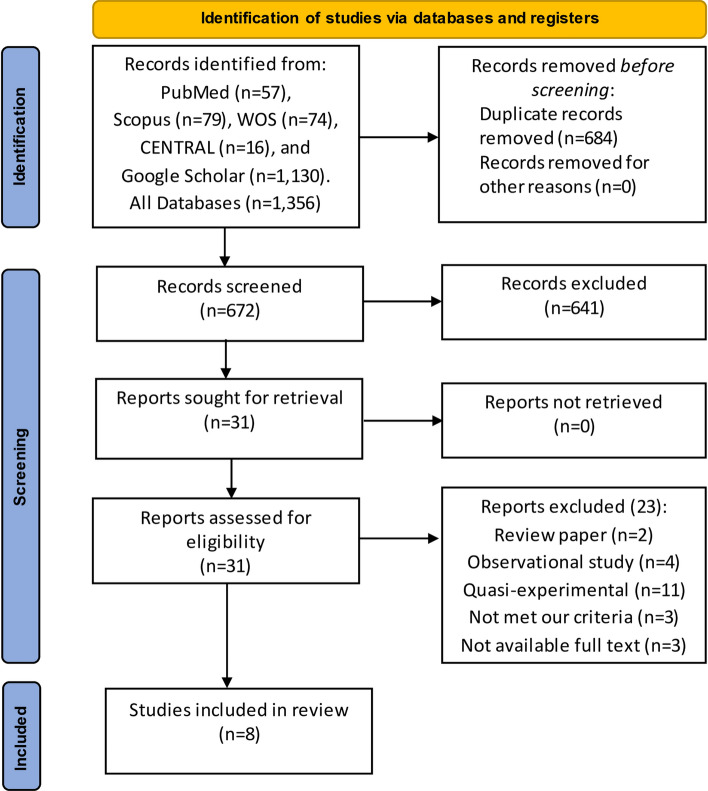
We retrieved 1356 studies after searching databases, then 684 duplicates were excluded, leaving 672 records to be screened. After title and abstract screening, we proceeded with 31 articles for full-text screening, and irrelevant studies. Finally, we included eight RCTs Fig. 1.
Fig. 1.
PRISMA flow diagram for study selections and screening process
Characteristics of the Included Studies
We included eight RCTs with a total of 656 tympanic perforation membrane patients. Five studies were conducted in Pakistan [24, 26–28, 28] and three in India [29, 31, 31]. The type of grafts that are used were temporalis fascia in five studies [24, 25, 28, 30, 31] while the other studies did not report the graft type. The detailed summary and baseline characteristics of the included studies are illustrated in Tables 1and 2.
Table 1.
Summary of the included trials
| Study ID | Country | Recruitment | N | Trial arms | Type of surgery | Type of graft | |
|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||
| Akhtar 2022 | Pakistan | January 2021-June 2021 | n = 80 | Underlay technique | Overlay technique | Myringoplasty | Not reported |
| Arif 2022 | Pakistan | January 2019-December 2019 | n = 164 | Underlay technique | Overlay technique | Myringoplasty | Temporalis fascia |
| Arshad 2019 | Pakistan | March 2017-February 2018 | n = 27 | Underlay technique | Overlay technique | Myringoplasty | Temporalis fascia and tragus |
| Arumugam 2016 | India | April 2014-June 2015 | n = 103 | Underlay technique | Overlay technique | Myringoplasty | Not reported |
| Habib-ur-Rehman 2011 | Pakistan | January 2008-December 2009 | n = 86 | Underlay technique | Overlay technique | Myringoplasty | Temporalis fascia |
| Kawatra 2014 | India | January 2013-June 2014 | n = 60 | Underlay technique | Overlay technique | Myringoplasty | Temporalis fascia |
| Khawaja 2020 | Pakistan | April 2016-September 2017 | n = 80 | Underlay technique | Overlay technique | Myringoplasty | Not reported |
| Singh 2003 | India | Not reported | n = 56 | Underlay technique | Overlay technique | Myringoplasty | Temporalis fascia |
Table 2.
Baseline characteristics of the included patients
| Study ID | Group | N | Sex, n(%) | Age (years) | Perforation size, n(%) | Type of anesthesia | Follow-up | |||
| Male | Female | Large (> 50) | Medium (25–50) | Small (< 25) | ||||||
| Akhtar 2022 | Overlay | n = 40 | 22 (55%) | 22 (55%) | 29.68 ± 5.54 | 9 (22.5%) | 9 (22.5%) | 22 (55%) | Not reported | Not reported |
| Underlay | n = 40 | 18 (45%) | 18 (45%) | 29.48 ± 6.35 | 9 (22.5%) | 10 (25%) | 21 (52.5%) | |||
| Arif [24] | Overlay | n = 82 | 44 (53.65%) | 38 (46.34%) | 32 ± 6.36 | 35 (42.6%) | 34 (41.4%) | 13 (18.8%) | General | Three months |
| Underlay | n = 82 | 38 (46.34%) | 34 (41.46%) | 31 ± 8.37 | 35 (42.6%) | 35 (42.6%) | 12 (14.6%) | |||
| Arshad 2019 | Overlay | n = 13 | 10 (37%) | 17 (62%) | < 20–40 (range) | Not reported | Not reported | Not reported | General | Six weeks |
| Underlay | n = 14 | < 20–40 (range) | Not reported | Not reported | Not reported | |||||
| Arumugam 2016 | Overlay | n = 51 | 24 (%) | 27 (%) | 15–60 (range) | Not reported | Not reported | Not reported | General | Six months |
| Underlay | n = 52 | 24 (%) | 28(%) | 15–60 (range) | Not reported | Not reported | Not reported | |||
| Habib-ur-Rehman 2011 | Overlay | n = 43 | 69 (80.3%) | 17 (19.7%) | 15–45 (range) | Not reported | Not reported | Not reported | General | Six months |
| Underlay | n = 43 | 15–45 (range) | Not reported | Not reported | Not reported | |||||
| Kawatra 2014 | Overlay | n = 30 | 16 (53.3%) | 14 (46.7%) | 29.43 ± 7 | Not reported | Not reported | Not reported | General | Four months |
| Underlay | n = 30 | 15 (50%) | 15 (50%) | 28.67 ± 9.72 | Not reported | Not reported | Not reported | |||
| Khawaja 2020 | Overlay | n = 40 | 22 (55%) | 22 (55%) | 29.68 ± 5.54 | 9 (22.5%) | 9 (22.5%) | 22 (55%) | Not reported | Three months |
| Underlay | n-40 | 18 (45%) | 18 (45%) | 29.48 ± 6.35 | 9 (22.5%) | 10 (25%) | 21 (52.5%) | |||
| Singh 2003 | Overlay | n = 28 | Not reported | Not reported | 16–40 (range) | Not reported | Not reported | Not reported | Not reported | One year |
| Underlay | n = 28 | Not reported | Not reported | 16–40 (range) | Not reported | Not reported | Not reported | |||
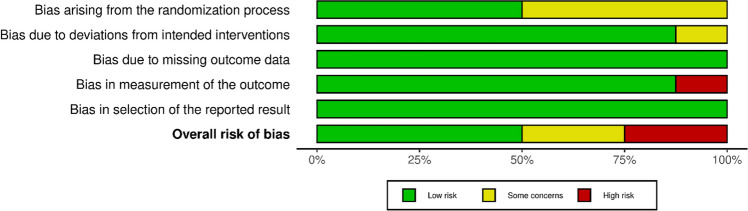
Quality Assessment
Four RCTs had a low risk of overall bias, two had some concerns, and two had a high risk of bias. Akhtar et al., 2022 [27]; Arif et al., [24]; Arumugam et al., 2016 [29]; Khawaja et al., 2020 [30], showed some concerns mainly attributed to the randomization process. Also, Akhtar et al., 2022 [27], showed some concerns mainly attributed to the deviation from the intended intervention. However, Arif et al., 2022 [24] showed a high risk of bias attributed to the measurement of the outcome, Figs. 2and 3.
Fig. 2.
Risk of bias graph of the included randomized controlled trials
Fig. 3.
Risk of bias summary of the included randomized controlled trials
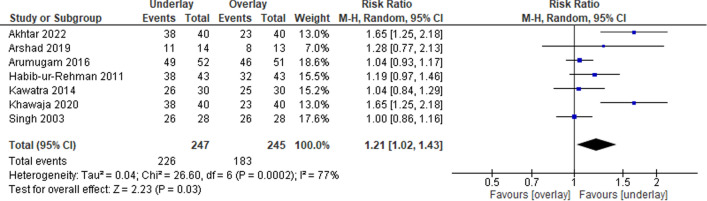
Surgical Success Rate (%)
Seven RCTs were included in this analysis with a total of 492 patients. The underlay technique was significantly associated with a higher surgical success rate, compared to the overlay technique (RR: 1.21 with 95% CI [1.02, 1.43], P = 0.03), Fig. 4. The pooled studies were heterogenous (P = 0.0002, I2 = 77%).
Fig. 4.
Meta-analysis of the surgical success rate (%)
Audiological Success Rate (%)
Four studies were included in this analysis with a total of 380 patients. The underlay technique was significantly associated with a higher audiological success rate, compared to the overlay technique (RR: 1.31 with 95% CI [1.18, 1.44], P < 0.001), Fig. 5. The pooled studies were homogenous (P = 0.68, I2 = 0%).
Fig. 5.
Meta-analysis of the audiological success rate (%)
Discussion
Significance of the Study and Summary of Findings
To the best of our knowledge, this is the first meta-analysis that compares the underlay and the overlay approaches of myringoplasty. The importance of our study is not limited to the field of otolaryngology but is disseminated to all surgical specialists that deal with grafts and reconstructive materials. Given that the majority of the included studies were conducted in Pakistan and India, the findings may also highlight regional differences in surgical outcomes, assisting in the development of tailored clinical strategies for these geographic locations.
The analysis integrated data from eight RCTs with a total of 656 tympanic perforation membrane patients, primarily focusing on the success rates of the two surgical techniques utilized in treating tympanic membrane perforations. A critical finding of this study is the higher success rates, both surgically and audiologically, associated with the underlay technique compared to the overlay technique. The surgical success rate outcome showed significant heterogeneity across the analyzed studies, while the audiological success rate depicted homogeneity.
Explanation of Findings and Comparison with Previous Studies
The finding that the underlay technique has a higher surgical success rate, supported by a relative risk of 1.21, is clinically significant. It implies that patients who undergo this technique have a significantly better chance of achieving successful outcomes than those who undergo the overlay technique. However, it is important to note that the results are heterogeneous (I2 = 77%), implying that the outcomes of the individual studies analyzed vary significantly. This significant heterogeneity could be attributed to differences in study methodologies, population characteristics, or surgical expertise among the included studies. Furthermore, it could imply that there are underlying factors not addressed in the current study that have a significant impact on surgical outcomes. These could include the surgical setting, the surgeon’s skill, or the severity and location of the perforations. Additionally, the patient selection may possibly have played an important role in the high success rate, and it should be in mind that sometimes the success rate is not related to the operation itself, or the technique used.
The audiological success rate, on the other hand, demonstrated not only a higher success rate with the underlay technique, but also remarkable homogeneity across studies (I2 = 0%). This means that the underlay technique has a consistent and significant positive impact on patients’ audiological outcomes across multiple study contexts. A relative risk of 1.31 clearly shows that patients who undergo the underlay technique are more likely to have better hearing outcomes. This homogeneity suggests that the effect of the underlay technique on audiological outcomes is less influenced by other variables and that this finding may be more universally applicable.
In order to prevent infection and restore or improve hearing, the optimum reconstructive approach should result in a thin, conically shaped, vibrating membrane replacing the original eardrum. The properties of each underlay and overlay approach might be related to the surgical and audiological success rates. The underlay approach is considered to be technically easier [32]. The overlay approach, on the other hand, is more complex, and needs more expertise from the surgeon. Moreover, poorer hearing outcomes following the overlay approach could be due severe complications such as graft lateralization, epithelial pearls, acoustic trauma, delayed healing, and anterior angle blunting are conceivable [33]. Moreover, a recent prospective study found that the overlay group, four out of 24 patients had residual perforation (13.3%) whereas three out 25 patients had residual perforation (10%) in the underlay group [34].
The length of time required for surgery may have an impact on the outcome. According to a retrospective study, overlay myringoplasty took longer than underlay myringoplasty. This time disparity might be attributed to the difficulty of the overlay procedure, which requires the graft to be maintained lateral to the annulus and any residual fibrous layer of the tympanic membrane after carefully removing the squamous layer [34]. Additional factors that may influence the operation’s outcome include the size and location of the reported hole [35, 36]. As the overlay approach is often reserved for complete perforations and anterior perforations, the failure rate is expected to be greater.
A prospective study found that the graft uptake rate for the overlay group was 86.6% and the underlay technique was 90% [34]. These findings were close to the Guha et al. retrospective investigation. They observed that the overlay group had a 90% success rate while the underlay method had a 93.3% success rate [37]. The underlay technique’s high success rate is most likely due to less surgical manipulation of middle ear tissues and faster recovery, which reduces the bias associated with infrequent otologic surgeons whereas in the overlay group, the surgical treatment including the removal of the tympanic membrane remnant and the skin of the ear canal, which resulted in the formation of granulation tissue, resulted in a prolonged healing period.
Only the temporalis fascia has been used as a graft in our included studies. However, a study found that the graft material utilized in the overlay group was temporalis fascia in the majority of patients (96.6%), with tragal perichondrium used in only one patient (3.3%). Temporalis fascia was the graft material used in all patients (100%) in the underlay group. The difference in surgical graft material between the two groups was statistically insignificant [34]. Even the type of temporalis fascia (dry or wet) may have no effect on the outcome. A systematic review and meta‑analysis of eight RCTs including 989 patients found that the type of temporalis fascia graft (dry or wet) had no effect on the clinical results of type-I tympanoplasty [38].
Strengths and Limitations
To the best of our knowledge, this is the first systematic review and meta-analysis to show that the underlay technique has a greater surgical and audiological success rate than the overlay approach. Moreover, all of the included studies were RCTs. However, there are a few drawbacks associated with this study. First, our sample size is small, which limits generalizability of the results. Second, as the follow up periods were wide different in the studies (from 6 weeks to one year), We don’t know how successful this therapy will be in the long run. Third, post-surgical problems (e.g., tympanic membrane lateralization, anterior blunting, external ear canal stenosis, delayed healing, epithelial pearls, cholesteatoma development, etc.) were not reported. Fourth, some of the included studies utilized the temporal fascia as a graft, whereas others did not specify the type of grafting, limiting our results to the temporalis fascia graft. Fifth, we could not do subgroup analysis due to lack of data. Lastly, one of our outcomes had high heterogeneity and extremely low confidence of evidence; so, our findings should be interpreted with caution.
Recommendations for Future Research and Clinical Practice
Given the disparities in surgical success rates, future research should seek to identify the factors that contribute to these disparities. More in-depth research could be conducted to better understand the relationship between graft types and success rates. Furthermore, studies can focus on improving the randomization process to reduce bias, as seen in some of the included studies. Finally, Long-term monitoring study is needed and strongly recommended in the future.
Clinically, these findings support a preference for the underlay technique due to its higher success rates. It is critical for practitioners to receive training in order to perform this technique competently and potentially improve patient outcomes. Furthermore, developing guidelines that incorporate these findings could be a significant step forward.
Over-under tympanoplasty, a modified variant of the two the procedures described above, is a modern treatment in which the graft is put laterally to the malleus and beneath the remaining drum [39]. Also, in recent years, a new technique, the interlay, has evolved and is being used effectively with promising outcomes [40]. So, future meta-analyses comparing those new techniques with the traditional techniques (overlay and underlay) are required.
Conclusion
This meta-analysis underscores the potential superiority of the underlay technique in managing tympanic membrane perforations, with significant implications for surgical and audiological outcomes. However, the noticeable heterogeneity in surgical success rates necessitates further research to refine these findings. The study acts as a stepping stone towards enhancing the quality of care in patients with tympanic membrane perforations, directing practitioners towards potentially more successful surgical interventions and setting a foundation for future research in this domain.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank Omar Abdalwahab for his valuable assistant.
Author Contributions
EA contributed to study conception, study design, data collection, data analysis, write up of original draft of manuscript, and review of manuscript for editorial and intellectual contents. MS, and MA contributed to literature review, data collection, and review of manuscript for editorial and intellectual contents. AH contributed to supervision and review of manuscript for editorial and intellectual contents. All authors read and approved the final draft of manuscript.
Data Availability
All data are available within the manuscript and can be obtained from the corresponding author upon a reasonable request.
Declarations
Conflict of interest
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Brar S, Watters C, Winters R. Tympanoplasty. Indian J Otolaryngol Head Neck Surg. 2023;46:63–66. doi: 10.1007/BF03048873. [DOI] [Google Scholar]
- 2.Xing C, Liu H, Li G, et al. Type 1 tympanoplasty in patients with large perforations: comparison of temporalis fascia, partial-thickness cartilage, and full-thickness cartilage. J Int Med Res. 2020;48:030006052094514. doi: 10.1177/0300060520945140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chavan RP, Ingole SM, Birajdar SN. Overview of tympanoplasty techniques and results. Int J Otorhinolaryngol Head Neck Surg. 2017 doi: 10.18203/issn.2454-5929.ijohns20170360. [DOI] [Google Scholar]
- 4.Karunaratne D, Violaris N. Myringoplasty outcomes from a 5-Year single surgeon’s experience and important Surgical Technical Aspects. J Audiol Otol. 2021;25:224. doi: 10.7874/jao.2021.00311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bayram A, Bayar Muluk N, Cingi C, Bafaqeeh SA. Success rates for various graft materials in tympanoplasty–a review. J Otol. 2020;15:107–111. doi: 10.1016/j.joto.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh BJ, Sengupta A, Das SK, et al. A comparative study of different graft materials used in myringoplasty. Indian J Otolaryngol Head Neck Surg. 2009;61:131. doi: 10.1007/s12070-009-0051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aggarwal R, Saeed SR, Green KJM. Myringoplasty. J Laryngol Otol. 2006;120:429–432. doi: 10.1017/S0022215106000697. [DOI] [PubMed] [Google Scholar]
- 8.Miller KA, Fina M, Lee DJ. Principles of Pediatric endoscopic ear Surgery. Otolaryngol Clin North Am. 2019;52:825–845. doi: 10.1016/j.otc.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Anzola JF, Nogueira JF. Endoscopic techniques in Tympanoplasty. Otolaryngol Clin North Am. 2016;49:1253–1264. doi: 10.1016/J.OTC.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 10.Maran RK, Jain AK, Haripriya GR, Jain S. Microscopic Versus Endoscopic Myringoplasty: a comparative study. Indian J Otolaryngol Head Neck Surg. 2019;71:1287. doi: 10.1007/S12070-018-1341-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Albazee E, Abu-Zaid A, Alshammari B, et al. Efficacy of gelfoam middle ear packing in type-1 tympanoplasty: systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2023;280:3503–3514. doi: 10.1007/s00405-023-07975-1. [DOI] [PubMed] [Google Scholar]
- 12.Sergi B, Galli J, De Corso E, et al. Overlay versus underlay myringoplasty: report of outcomes considering closure of perforation and hearing function. Acta Otorhinolaryngol Ital. 2011;31:366. [PMC free article] [PubMed] [Google Scholar]
- 13.Kim TK, Kang BC, Kim J, II, et al. Clinical usefulness of simple underlay myringoplasty. Korean J Otorhinolaryngol Head Neck Surg. 2022 doi: 10.3342/kjorl-hns.2021.00794. [DOI] [Google Scholar]
- 14.Anand S, Danti S, Moroni L, Mota C. Regenerative therapies for tympanic membrane. Prog Mater Sci. 2022;127:100842. doi: 10.1016/j.pmatsci.2022.100942. [DOI] [Google Scholar]
- 15.Plodpai Y, Paje N. The outcomes of overlay myringoplasty: endoscopic versus microscopic approach. Am J Otolaryngol Head Neck Med Surg. 2017 doi: 10.1016/j.amjoto.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Kartush JM, Michaelides EM, Becvarovski Z, LaRouere MJ. Over-under tympanoplasty. Laryngoscope. 2002 doi: 10.1097/00005537-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Gulia JS, Yadav SPS, Khaowas AK. Medio-lateral myringoplasty versus medial myringoplasty: a comparative study. Otolaryngol Head Neck Surg. 2013 doi: 10.1177/0194599813496044a270. [DOI] [Google Scholar]
- 18.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/BMJ.N71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins JPT, Thomas J, Chandler J et al (2019) Cochrane handbook for systematic reviews of interventions. Cochrane Handbook Syst Rev Intervent 1–694. 10.1002/9781119536604
- 20.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/BMJ.L4898. [DOI] [PubMed] [Google Scholar]
- 22.Twells LK. Evidence-based decision-making 1: critical appraisal. Methods Mol Biol. 2015;1281:385–396. doi: 10.1007/978-1-4939-2428-8_23. [DOI] [PubMed] [Google Scholar]
- 23.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/BMJ.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arif M, Mudassar M, Noor A. Efficacy of underlay versus overlay technique for myringoplasty in terms of hearing improvement. J Med Sci. 2022;30:114–116. doi: 10.52764/JMS.22.30.2.2. [DOI] [Google Scholar]
- 25.Arshad M, Shahnaz A, Bashir M, Zaman A. Comparison of graft uptake in patients undergoing myringoplasty/ tympanoplasty by overlay and underlay procedure. Prof Med J. 2019;26:1861–1865. doi: 10.29309/TPMJ/2019.26.11.2913. [DOI] [Google Scholar]
- 26.Khawaja M, Sajid T, Aziz T, et al. Comparison of graft uptake by underlay and overlay technique in myringoplasty. J Ayub Med Coll Abbottabad. 2020;32(Suppl 1):S640–S643. doi: 10.53350/pjmhs22163793. [DOI] [PubMed] [Google Scholar]
- 27.Akhtar A, Ikram A, Akaash H, et al. Comparison of graft Uptake by Underlay and overlay technique in myringoplasty. Pak J Med Health Sci. 2022;16:793–795. [Google Scholar]
- 28.Javaid H-U-RF-I-W M, et al. Otitis media: comparison of outcome of underlay versus overlay myringoplasty. Pak J Med Sci. 2011;27:1076–1078. [Google Scholar]
- 29.Arumugam I, Kannappan AL, Rizwan RM. A comparative study of overlay and underlay myringoplasty considering closure of perforation and hearing results: our experience. J Evol Med Dent Sci. 2016;5:1635–1638. doi: 10.14260/jemds/2016/385. [DOI] [Google Scholar]
- 30.Kawatra DR, Maheshwari DP, Kumar DG. A comparative study of the techniques of myringoplasty—Overlay underlay and interlay. IOSR J Dent Med Sci. 2014;13:12–16. doi: 10.9790/0853-131251216. [DOI] [Google Scholar]
- 31.Singh M, Rai A, Bandyopadhyay S, Gupta SC. Comparative study of the underlay and overlay techniques of myringoplasty in large and subtotal perforations of the tympanic membrane. J Laryngol Otol. 2003;117:444–448. doi: 10.1258/002221503321892262. [DOI] [PubMed] [Google Scholar]
- 32.Pai GMS, Pavithran VK. Myringoplasty: underlay versus overlay techniques—A comparative study. Int J Otorhinolaryngol Head Neck Surg. 2018;4:381–386. doi: 10.18203/ISSN.2454-5929.IJOHNS20180697. [DOI] [Google Scholar]
- 33.Faramarzi A, Hashemi SB, Rajaee A. Mucosal pocket myringoplasty: a modification of underlay technique for anterior or subtotal perforations. Am J Otolaryngol. 2012;33:708–713. doi: 10.1016/J.AMJOTO.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 34.Saraf A, Manhas M, Jamwal PS, et al. Comparative study of overlay and underlay techniques of myringoplasty-our experience. Indian J Otolaryngol Head Neck Surg. 2022;74:426–432. doi: 10.1007/S12070-020-02197-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karabulut B, Mutlu F, Sahin S, Cirik AA. Anatomical and functional long-term results of endoscopic butterfly inlay myringoplasty. Eur Arch Otorhinolaryngol. 2018;275:2653–2658. doi: 10.1007/S00405-018-5120-3. [DOI] [PubMed] [Google Scholar]
- 36.Das A, Sen B, Ghosh D, Sengupta A. Myringoplasty: impact of size and site of perforation on the Success Rate. Indian J Otolaryngol Head Neck Surg. 2015;67:185–189. doi: 10.1007/S12070-014-0810-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.T1 G, B2 C, B3 D Onlay versus inlay myringoplasty with tragal perichondrium—A hospital-based retrospective study. J Evid Based Med Healthc. 2016;3:1–3. [Google Scholar]
- 38.Albazee E, Abdelaziz A, Magzoub H, et al. Dry versus wet temporalis fascia graft in type-I tympanoplasty: a systematic review and meta-analysis of randomized controlled trials. Eur Arch Otorhinolaryngol. 2023;280:1005–1015. doi: 10.1007/S00405-022-07725-9. [DOI] [PubMed] [Google Scholar]
- 39.Erbele ID, Fink MR, Mankekar G, et al. Over-under cartilage tympanoplasty: technique, results and a call for improved reporting. J Laryngol Otol. 2020;134:875–881. doi: 10.1017/S0022215120001978. [DOI] [PubMed] [Google Scholar]
- 40.Sharma N, Sharma P, Goyal VP, Sharma KG. Interlay versus underlay type 1 tympanoplasty: a comparative study of the techniques in 100 cases. Int J Otorhinolaryngol Head Neck Surg. 2019;5:64–68. doi: 10.18203/ISSN.2454-5929.IJOHNS20185071. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are available within the manuscript and can be obtained from the corresponding author upon a reasonable request.