Abstract
Background
While multidimensional and interdisciplinary assessment of older adult patients improves their short-term outcomes after evaluation in the emergency department (ED), this assessment is time-consuming and ill-suited for the busy environment. Thus, identifying patients who will benefit from this strategy is challenging. Therefore, this study aimed to identify older adult patients suitable for a different ED approach as well as independent variables associated with poor short-term clinical outcomes.
Methods
We included all patients ≥65 years attending 52 EDs in Spain over 7 days. Sociodemographic, comorbidity, and baseline functional status data were collected. The outcomes were 30-day mortality, re-presentation, hospital readmission, and the composite of all outcomes.
Results
During the study among 96,014 patients evaluated in the ED, we included 23,338 patients ≥65 years—mean age, 78.4±8.1 years; 12,626 (54.1%) women. During follow-up, 5,776 patients (24.75%) had poor outcomes after evaluation in the ED: 1,140 (4.88%) died, 4,640 (20.51) returned to the ED, and 1,739 (7.69%) were readmitted 30 days after discharge following the index visit. A model including male sex, age ≥75 years, arrival by ambulance, Charlson Comorbidity Index ≥3, and functional impairment had a C-index of 0.81 (95% confidence interval, 0.80–0.82) for 30-day mortality.
Conclusion
Male sex, age ≥75 years, arrival by ambulance, functional impairment, or severe comorbidity are features of patients who could benefit from approaches in the ED different from the common triage to improve the poor short-term outcomes of this population.
Keywords: Emergencies, Geriatrics, Frail elderly, Triage
INTRODUCTION
Aging populations challenge health and social care systems worldwide.1) The percentage of people aged ≥65 years in European countries is predicted to increase from 16% in 2001 to 21% in 2020.2) Greece, Finland, Portugal, Germany, and Bulgaria (22%) had the highest forecast percentages, whereas Ireland (14%) and Luxembourg (15%) had the lowest. The group of individuals aged ≥80 years comprised nearly 6% of the population in 2020, a two-fold increase compared with 2001 (3.4%).2) Projections indicate that the percentage of people aged ≥80 years in Europe will multiply by 2.5-fold between 2020 and 2100, rising from 5.8% to 14.6%.
Over the past decade, increasing pressure on emergency care has led to crowding in emergency departments (EDs), which represents a major challenge. This has negative consequences for the efficiency, quality, and safety of emergency care.3,4) ED crowding is partially caused by a growing number of older adults.5) These individuals often have complex health problems and multimorbidities associated with high rates of health service utilization. This population accounts for an estimated 15%–25% of total ED visits.6)
Older adult patients experience age-related physiological changes in the immunological, cardiovascular, and respiratory systems, which may hinder the identification of disease severity.7) Older adult individuals also have a greater probability of atypical disease presentation, comorbidities, cognitive disorders, geriatric syndromes, and polypharmacy.8) In emergency care, these differences imply a more complex clinical evaluation requiring more staff time; a greater need for complementary tests and consultations with other specialists; longer stays in the ED; and a greater probability of misdiagnosis, hospitalization, and discharge with undetected or untreated problems, leading to a greater risk of medical complications, functional impairment, and poorer health following discharge.6,9,10) In addition, other factors such as pre-existing functional impairment, cognitive decline, and social issues hamper disposition planning.11-13)
Older patients also often experience poorer outcomes following ED visits. This is reflected in the hospitalization, return rates, and deaths in older adults compared with those in younger patients. Approximately 10%–23% of older patients return unexpectedly within the first month,14) and up to 25% of older adults return to the ED within 3 months.11) Within 3 months of discharge, 12.4% of the older patients die, 18.3% are hospitalized, and 2.6% subsequently enter a nursing home. Within 6 months of discharge after the index ED visit, 43.9% of older adults return to the ED at least once, and 7.5% return ≥3 times. Furthermore, approximately 80% of the older adults discharged from the ED have at least one unaddressed health issue.15) Such high rates of re-presentation and other adverse outcomes after initial ED admission support concerns regarding traditional ED models that do not meet the underlying needs of many older patients.16)
ED urgency triage aims to prioritize patients based on their clinical urgency, rapidly diagnose potentially lethal illnesses, and reduce the negative impact of treatment delays on prognosis.17) However, triage tools may allocate urgency less effectively in older populations,18-20) possibly due to different reference values for vital signs, atypical disease presentations, and the presence of cognitive impairment. Older patients are, therefore, at risk of “undertriage,” an assignment of an inappropriately low triage level, resulting in longer waiting times and the risk of adverse outcomes due to harm by delay in treatment.17) Triage performance is inferior in older patients compared to younger patients and is illustrated by a worse predictive ability for identifying in-hospital mortality risk in older patients.19,20)
Several geriatric screening tools have been developed to identify vulnerable geriatric patients in the ED.21-24) These tools are prognostic tools for long-term adverse outcomes, whereas urgent triage tools are primarily designed to assign short-term clinical priority and secondarily to predict short-term mortality. Multidimensional and interdisciplinary assessments of older patients have been shown to increase the likelihood of older people being alive and living in their own homes 12 months after admission. However, this process is time-consuming and ill-suited for busy ED environments.25)
Considering the above, determining which older patients are at risk of adverse effects related to their age or specific basal circumstances and for whom different or complementary triage models should be applied is critical. Therefore, this study aimed to identify in which older adult patients a different ED approach would be suitable, as well as variables independently associated with poor short-term clinical outcomes not included in common triage systems, based on sociodemographic characteristics, comorbidities, and baseline functional status characteristics in patients aged ≥65 years evaluated in the ED.
MATERIALS AND METHODS
Description of the emergency department and elders in need (EDEN) Challenge
The EDEN challenge emanates from the Spanish Investigators in Emergency Situations Team (SIESTA) network,26) which includes 52 EDs (approximately 20% of Spanish public EDs). These hospitals are representative both territorially (12 of the 17 Spanish regions) and in terms of typology (university, high technology, and regional hospitals). The results of this challenge have recently been presented.27) The primary objective is to increase knowledge about the sociodemographic, organizational, baseline, clinical, care, and evolutionary aspects of the population aged 65 years and older who consult Spanish EDs. To this end, we created a multipurpose registry that included all patients who consulted the ED regardless of the reason for consultation.
The inclusion period was April 1–7, 2019 (7 days). No exclusion criteria were applied and EDs wishing to participate were required to include all patients seen during the study period.
Ethical Considerations
The EDEN project was approved by the Clinical Research Ethics Committee of the Clínico San Carlos de Madrid Hospital (Protocol No. HCSC/22/005-E). Because of the characteristics of the study and the time periods for which data collection was planned, the requirement for written informed consent by the patients was waived. The database was used with coded patients to preserve their anonymity. The creation of the EDEN cohort and the work emanating from them followed the ethical principles of the Declaration of Helsinki.
This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.28)
EDEN-15 Study Design
The EDEN-15 study analyzed patients included in the EDEN cohort. We analyzed six sociodemographic characteristics (age, sex, how the patient arrived at the ED, how the patient was referred to the ED, home accompaniment status, and whether the patient had social support) and five characteristics related to the patient’s baseline functional status (dependence according to the Barthel Index, comorbidity according to the Charlson Comorbidity Index, falls in the previous 6 months, and previous diagnoses of dementia and depression). The outcome variables were 30-day mortality, re-presentation, and hospital readmission. For the calculation of re-presentation and hospital readmission, patients who died during hospitalization at the index visit were excluded. These outcomes were calculated based on hospital or ED discharge. Finally, we considered poor outcome as a composite variable, including all events (30-day mortality, re-presentation, and hospital readmission).
Statistical Analysis
The frequencies and percentages of qualitative variables and the median and interquartile range of continuous variables were recorded. Characteristics of alive and dead patients, readmitted patients, and represented after 1 month of follow-up were compared using the chi-square test for categorical variables. Cox proportional hazards regression analyses were performed to assess the accuracy of the different scores to predict 30-day mortality, readmission, and re-presentation. Univariate Cox regression models were used to assess the response variables. All variables with p<0.2 were considered in the multivariate Cox model. Hazard ratios (HRs), 95% confidence intervals (CIs), and p-values were calculated for each category. Differences between groups were considered statistically significant for p<0.05, or if the 95% CI of the HR excluded the value of 1. We also calculated the C-index to study the predictive accuracy of the model, where the null value of the C-statistic was 0.5. To create the scale score, we first assigned a weight to each category of each statistically significant variable, relative to the estimated beta parameter of each survival model. We added the total scores for each patient, with higher scores indicating a greater probability of each outcome.29) Once the risk score was developed, we divided the scores into three categories. Kaplan–Meier curves were generated for the four outcomes for the different scores. The optimal categorization of each continuous risk score was obtained using the CatPredi function of the R package CatPredi (https://cran.r-project.org/) using a genetic algorithm. Subsequently, the results were internally validated by bootstrapping with 500 resamples, and the C-index was calculated with 95% CI. All statistical processing was performed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA), SAS for Windows, version 9.4 (SAS Institute, Cary, NC, USA), and R version 4.1.1. The figures were produced using PowerPoint 2016 (Microsoft Corp., Redmond, WA, USA).
RESULTS
During the study period 96,014 patients were evaluated in the 52 EDs participating in the study; among these, 23,338 patients aged ≥65 years—mean age, 78.4±8.1 years; 12,626 (54.1%) women—were finally included (Fig. 1). During follow-up, 5,776 patients (24.75%) had a poor outcome after evaluation in the ED: 1,140 (4.88%) died, 4,640 (20.51%) returned to the ED, and 1,739 (7.69%) were readmitted within 30 days after discharge following the index visit. Table 1 shows the patient characteristics.
Fig. 1.
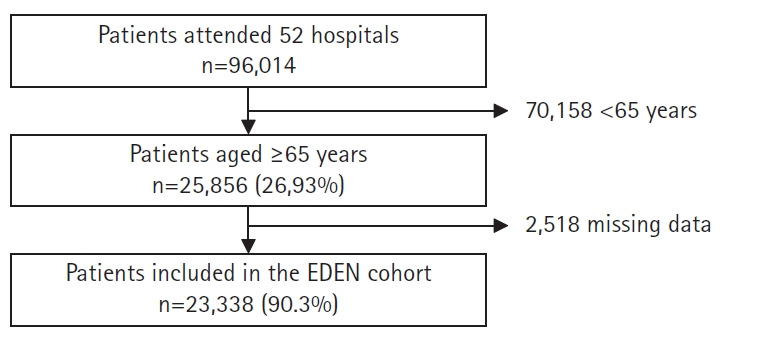
Flowchart for the inclusion of patients in the EDEN cohort.
Table 1.
Characteristics of the patients included (n=23,338)
| Characteristic | Value | |
|---|---|---|
| Sociodemographic | Age (y) | 78 (71–85) |
| Sex, female a) | 12,626 (54.1) | |
| Arrival to ED | ||
| Own transport | 17,291 (74.1) | |
| Non medicalised ambulance | 4,591 (19.7) | |
| Medicalised ambulance | 1,456 (6.2) | |
| Referral to the ED | ||
| Initiative of the patient or caregiver | 15,998 (68.6) | |
| From primary care | 4,747 (20.3) | |
| By medical specialist other than primary care | 635 (2.7) | |
| From another hospital | 512 (2.2) | |
| Situation at home a) | ||
| Lives alone, does not have professional caregivers | 1,685 (12.0) | |
| Lives with relatives | 10,373 (73.9) | |
| Live with professional caregiver 24 hours | 343 (2.4) | |
| Live with a professional caregiver for a few hours | 208 (1.5) | |
| Lives in residence | 1,412 (10.1) | |
| Has social assistance b) | 1,333 (17.1) | |
| Basal status | Barthel index | |
| Independent (100 points) | 15,615 (66.9) | |
| Mild-moderate dependence (60–95 points) | 5,480 (23.5) | |
| Severe dependency (<60 points) | 2,243 (9.6) | |
| Charlson Comorbidity Index | ||
| No comorbidity (0 points) | 6,114 (26.2) | |
| Mild comorbidity (1–2 points) | 9,505 (40) | |
| Moderate comorbidity (3–4 points) | 4,489 (19.2) | |
| Severe comorbidity (≥5 points) | 3,230 (14.6) | |
| Fall in the previous 6 months | 1,627 (7) | |
| Established diagnosis of cognitive impairment | 3,095 (13.3) | |
| Diagnosis of depression | 3,133 (13.4) | |
| Comorbidity | High blood pressure | 16,446 (70.5) |
| Dyslipidaemia | 11,752 (50.4) | |
| Diabetes mellitus | 6,762 (29) | |
| Chronic lung disease | 4,515 (19.3) | |
| Cancer | 3,935 (16.9) | |
| Heart failure | 3,477 (14.9) | |
| Ischaemic heart disease | 3,685 (15.8) | |
| Chronic kidney disease | 2,677 (11.5) | |
| Stroke | 2,850 (12.2) | |
| Dementia | 2,425 (10.4) | |
| Peripheral vascular disease | 2,294 (9.8) | |
| Connective tissue disease | 1,949 (8.4) | |
| Active smoking | 1,372 (5.9) | |
| Chronic liver disease | 890 (3.8) | |
| Ulcer disease | 973 (4.2) | |
| Alcoholism | 585 (2.5) | |
| HIV infection | 74 (0.3) |
Values are presented as median (interquartile range) or number (%).
ED, emergency department; HIV, human immunodeficiency virus.
a)Calculated from 14,021 patients, b)calculated from 7,773 patients.
Supplementary Table S1 presents the comparative analysis of poor outcomes (mortality, readmission, and re-presentation within 1 month) and the composite poor outcome, including all variables analyzed. The results of the univariate analysis of poor outcomes are shown in Supplementary Table S2. The factors associated with a higher risk for 30-day mortality included age >84 years (HR=4.510; 95% CI, 3.822–5.321), living in a geriatric residence (HR=4.329; 95% CI, 3.257–5.754), ED arrival by ambulance (HR=5.792; 95% CI, 5.106–6.569), having moderate or severe comorbidities (HR=4.237; 95% CI, 3.216–5.582 and HR=10.025; 95% CI, 7.714–13.029, respectively), having moderate or severe impairment (HR=3.735; 95% CI, 3.225–4.326 and HR=8.234; 95% CI, 7.078–9.579, respectively), dementia (HR=3.159; 95% CI, 2.750–3.606), and delirium (HR=3.035; 95% CI, 2.417–3.877). The factors associated with a higher risk of 30-day readmission were age >84 years (HR=1.784; 95% CI, 1.584–2.009), living in a geriatric residence (HR=1.674; 95% CI, 1.321–2.120), ED arrival by ambulance (HR=1.711; 95% CI, 1.551–1.888), and having moderate or severe functional impairment (HR=1.906; 95% CI, 1.716–2.117 and HR=2.305; 95% CI, 2.009–2.645, respectively). Thirty-day re-presentation was mainly related to male sex (HR=1.204; 95% CI, 1.136–1.277) and moderate or severe functional impairment (HR=1.335; 95% CI, 1.250–1.426 and HR=1.309; 95% CI, 1.188–1.442, respectively).
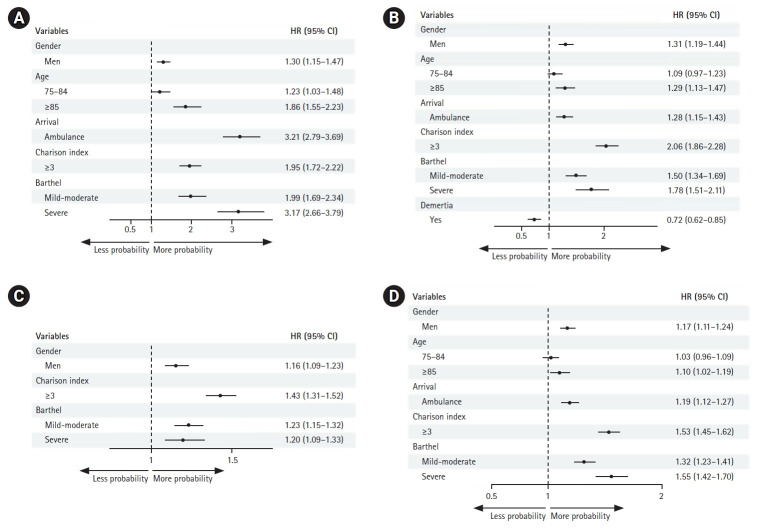
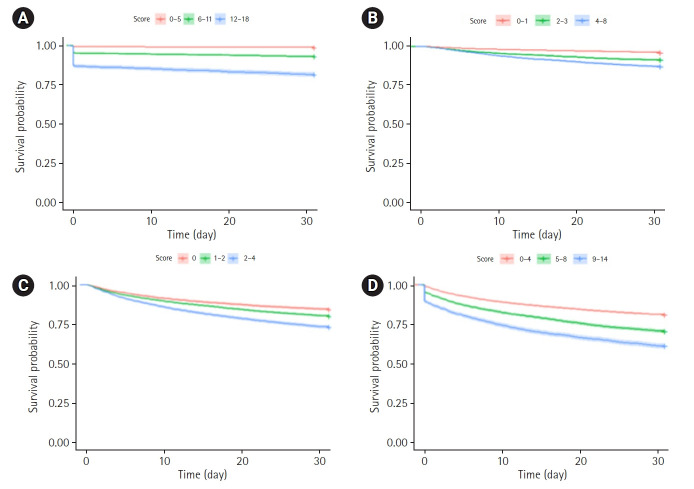
Table 2 shows the results of the multivariate analysis using univariate survival models for poor outcomes, as well as the models obtained, and the points assigned to each variable. A model including sex (male), age ≥75 years, arrival by ambulance, Charlson Comorbidity Index ≥3, and having functional impairment, even mild, had a C-index of 0.81 (95% CI, 0.80–0.82) for 30-day mortality. The C-index for the 30-day readmission was 0.66 (95% CI, 0.64–0.67). The model for 30-day re-presentation had a C-index of 0.57 (95% CI, 0.56–0.58) and included male sex, Charlson Comorbidity Index ≥3, and functional impairment. A model for the composite outcome had a C-index of 0.61 (95% CI, 0.60–0.62) and included male sex, age >84 years, arrival by ambulance, Charlson Comorbidity Index ≥3, and the presence of functional impairment. A forest plot of the HRs is shown in Fig. 2. Table 3 shows the functioning of risk groups derived from the developed models. In Fig. 3, the Kaplan–Meier curves for the models are presented for each dependent variable for the three patient groups: 0–5, 6–11, and 12–18–case for 30-day mortality; 0–1, 2–3, and 4–8 for 30-day readmission; 0, 1–2, and 2–4 for 30-day re-presentation; and 0–4, 5–8, and 9–14 for poor outcome within 30 days.
Table 2.
Multivariate analysis in people over 65 years of age for 30-day mortality, readmission, and re-presentation using univariate survival models
| 30-day mortality | 30-day readmission | 30-day re-presentation | 30-day poor outcome | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR (95% IC) | p-value | Coeff | Weight | HR (95% IC) | p-value | Coeff | Weight | HR (95% IC) | p-value | Coeff | Weight | HR (95% IC) | p-value | Coeff | Weight | |
| Sex, male | 1.302 (1.151–1.473) | <0.0001 | 0.264 | 1 | 1.31 (1.189–1.444) | <0.0001 | 0.160 | 1 | 1.157 | 0.0005 | 0.146 | 1 | 1.173 (1.112–1.238) | <0.0001 | 0.16 | 2 |
| Age (y) | ||||||||||||||||
| 65–74 | Ref. | Ref. | Ref. | 0 | Ref. | Ref. | Ref. | 0 | - | - | - | - | Ref. | Ref. | Ref. | 0 |
| 75–84 | 1.232 (1.026–1.480) | 0.0258 | 0.209 | 1 | 1.092 (0.969–1.230) | 0.4171 | 0.027 | 1 | - | - | - | - | 1.027 (0.963–1.095) | 0.4171 | 0.027 | - |
| ≥85 | 1.862 (1.552–2.233) | <0.0001 | 0.622 | 2 | 1.291 (1.131–1.474) | 0.0093 | 0.097 | 2 | - | - | - | - | 1.102 (1.024–1.186) | 0.0093 | 0.097 | 1 |
| Arrival (ambulance) | 3.209 (2.794–3.686) | <0.0001 | 1.166 | 6 | 1.285 (1.154–1.432) | <0.0001 | 0.176 | 6 | - | - | - | - | 1.192 (1.122–1.267) | <0.0001 | 0.176 | 2 |
| Charlson Comorbidity Index (≥3) | 1.952 (1.716–2.220) | <0.0001 | 0.669 | 3 | 2.06 (1.863–2.278) | <0.0001 | 0.428 | 3 | 1.43 (1.344–1.522) | <0.0001 | 0.358 | 2 | 1.535 (1.452–1.622) | <0.0001 | 0.428 | 4 |
| Barthel index | ||||||||||||||||
| Independent | Ref. | Ref. | Ref. | 0 | Ref. | Ref. | Ref. | 0 | Ref. | Ref. | Ref. | 0 | Ref. | Ref. | Ref. | 0 |
| Mild-moderate dependence | 1.989 (1.693–2.338) | <0.0001 | 0.688 | 3 | 1.504 (1.338–1.691) | <0.0001 | 0.276 | 3 | 1.233 (1.151–1.321) | <0.0001 | 0.210 | 1 | 1.317 (1.234–1.407) | <0.0001 | 0.276 | 3 |
| Severe dependence | 3.174 (2.660–3.787) | <0.0001 | 1.155 | 6 | 1.785 (1.509–2.112) | <0.0001 | 0.441 | 6 | 1.201 (1.087–1.327) | 0.0003 | 0.183 | 1 | 1.555 (1.423–1.699) | <0.0001 | 0.441 | 5 |
| Dementia (yes) | - | - | - | - | 0.724 (0.616–0.851) | <0.0001 | -0.322 | 1 | - | - | - | - | - | - | - | - |
| C-index (95% IC) | 0.81 (0.80–0.82) | 0.66 (0.64–0.67) | 0.57 (0.56–0.58) | 0.61 (0.60–0.62) | ||||||||||||
| Score c-index (95% IC) | 0.81 (0.80–0.82) | 0.65 (0.64–0.66) | 0.56 (0.55–0.57) | 0.60 (0.59–0.51) | ||||||||||||
| Bootstrap validation c-index (95% IC) | 0.81 (0.80–0.82) | 0.66 (0.65–0.67) | 0.57 (0.56–0.58) | 0.60 (0.59–0.61) | ||||||||||||
| Bootstrap validation score c-index (95% IC) | 0.81 (0.80–0.82) | 0.65 (0.64–0.66) | 0.56 (0.55–0.57) | 0.60 (0.59–0.61) | ||||||||||||
Multivariate analysis in people over 65 years of age for 30-day mortality, readmission, and re-presentation using univariate survival models.
Fig. 2.
Forest plot results for the four outcomes: (A) 30-day mortality, (B) 30-day readmission, (C) 30-day re-presentation, and (D) 30-day poor outcome.
Table 3.
Risk groups of the four outcomes
| Total | n (%) | HR (95% CI) | p-value | |||
|---|---|---|---|---|---|---|
| 30-day mortality | Score <6 | 14,123 | 181 (0.79) | Ref | Ref | |
| 6≤ Score <12 | 5,922 | 418 (1.82) | 5.681 (4.772–6.762) | <0.0001 | ||
| Score ≥12 | 2,804 | 517 (2.26) | 15.831 (13.366–18.752) | <0.0001 | ||
| C-index (95% CI) | 0.78 (0.76–0.79) | |||||
| Bootstrap C-index (95% CI) | 0.77 (0.76–0.79) | |||||
| 30-day readmission | Score <2 | 10,012 | 390 (1.76) | Ref | Ref | |
| 2≤ Score <4 | 6,123 | 530 (2.39) | 2.282 (2.002–2.601) | <0.0001 | ||
| Score ≥4 | 6,013 | 775 (3.50) | 3.461 (3.064–2.909) | <0.0001 | ||
| C-index (95% CI) | 0.64 (0.62–0.65) | |||||
| Bootstrap C-index (95% CI) | 0.64 (0.62–0.65) | |||||
| 30-day re-presentation | Score <1 | 6,661 | 248 (1.11) | Ref | Ref | |
| 1≤ Score <3 | 9,814 | 682 (3.08) | 1.901 (1.644–2.198) | <0.0001 | ||
| Score ≥3 | 5,673 | 765 (3.45) | 3.812 (3.303–4.388) | <0.0001 | ||
| C-index (95% CI) | 0.56 (0.55–0.57) | |||||
| Bootstrap C-index (95% CI) | 0.56 (0.55–0.57) | |||||
| 30-day poor outcome | Score <5 | 13,471 | 2,564 (11.22) | Ref | Ref | |
| 5≤ Score <9 | 6,100 | 1,801 (7.88) | 1.665 (1.568–1.769) | <0.0001 | ||
| Score ≥9 | 3,278 | 1,278 (5.59) | 2.406 (2.249–2.573) | <0.0001 | ||
| C-index (95% CI) | 0.56 (0.55–0.57) | |||||
| Bootstrap C-index (95% CI) | 0.56 (0.55–0.57) | |||||
HR, hazard ratio; CI, confidence interval.
Fig. 3.
Kaplan-Meier curves for the variables studied: (A) 30-day mortality, (B) 30-day readmission, (C) 30-day re-presentation, and (D) 30-day poor outcome.
DISCUSSION
In the present study, one in four patients had a poor short-term outcome after being evaluated in the ED, 5% died, one in five patients returned to the ED, and 7% were readmitted within the first month of discharge. To improve these results, new strategies are required during the index visit to identify high-risk patients. A model including male sex, age ≥75 years, ED arrival by ambulance, functional impairment, and Charlson Comorbidity Index ≥3 could be useful for identifying short-term mortality. In patients meeting these criteria, geriatric screening tools should be used to improve outcomes. The other three risk-scoring models (30-day readmission, 30-day re-presentation, and composite poor outcome) presented relatively low C-index values (0.55–0.65), suggesting their limited predictive accuracy.
Kuriyama et al.30) evaluated the accuracy of common triage systems used in the ED and showed that accuracy diminishes with increasing patient age. While underestimation of severity in these patients did not significantly increase, misclassification significantly increased with patient age. Gasperini et al.31) measured the proportion of patients >65 years of age who were assigned a lower triage level than the real level of care needed, showing undertriage in 7.6% of the patients evaluated, which occurred more frequently in patients aged >85 years (9.2%) than in those aged 75–84 years (7.5%) and 65–74 years (6.4%). Different reference values for vital signs and atypical presentations of diseases in older adult patients could contribute to undertriage.32)
Several geriatric screening tools have been developed to identify vulnerable geriatric patients in the ED, including the Identification of Seniors at Risk,22) Triage Risk Screening Tool,23) and Acute Presentation of Older Patients.33) These screening tools could add value, as they improve knowledge and approaches to geriatric patients in the ED.32) The American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Medicine developed the Geriatric Emergency Department Accreditation (GEDA) program to provide a standardized set of guidelines to effectively improve the care of the geriatric population.34) These guidelines create a template for staffing, equipment, education, policies, procedures, follow-up care, and performance improvements.
Geriatric education programs based on content and teaching methods, learning outcome effects, and factors promoting or hindering program implementation can improve ED professionals’ geriatric knowledge and positively impact their clinical practice.35) A systematic review15) including interventions in EDs targeted at reducing ED revisits, hospitalizations, nursing home admissions, and deaths in older patients after initial ED discharge showed that studies varied in their design and outcome measurements, but suggested that the use of a validated risk prediction tool to stratify patients into high- and low-risk groups could lead to improved patient outcomes. Furthermore, interventions that extend beyond simple referral might reduce the rates of adverse outcomes after ED discharge and should be considered. More intensive interventions that followed patients beyond referral and the use of a clinical risk prediction tool were associated with improved outcomes. Our study results could help define which patients could benefit from such specific approaches.
Nevertheless, these strategies are not widely implemented, partly because of their complexity in environments such as the ED, where time is limited.36) The term geriatric has different definitions over time. Fries et al.37) defined three groups by dividing the older adult population into young old (65–74 years), middle old (75–85 years), and oldest (>85 years). The World Health Organization defines the older population starting at 60 years of age.38) The GEDA guidelines use 65 years as the cutoff for the geriatric population. Nevertheless, hospitals may find that using the age of ≥65 years does not match the aim of identifying a high-risk population.
One challenge in the ED is recognizing which patients will benefit from this strategy; therefore, it is crucial to identify patients at risk of poor outcomes, independent of the reason for consultation, using variables available at presentation in the ED. Common triage uses vital signs for classification; however, older adult patients experience age-related physiological changes, leading to a lower heart rate or temperature, and increased stiffness of the arterial wall, which leads to increased blood pressure.7) Considering these changes, we did not include vital signs in the analysis and used only variables related to the basal status of older adult patients to identify those at risk for poor outcomes that could benefit from the application of multidimensional and interdisciplinary assessments to improve clinical results.
Our study has some limitations. First, the 52 participating EDs were not chosen at random but rather expressed their interest in participating. However, the broad representation both territorially (12 of the 17 autonomous communities were represented) and in terms of typology (universities, high technology, and regional hospitals) means that bias in this regard is probably small. Second, the analysis was not conducted by nosology groups but rather globally. This may indicate that the findings are conditioned by certain processes that may be more prevalent according to the patient’s sex or age. Nonetheless, our design captured the entire spectrum of attended patients and was not limited to a single disease or a group of diseases, thus providing an overall picture. Third, this was a secondary analysis of a multi-purpose cohort, and the associations may have been influenced by factors not covered in the cohort design. Therefore, the findings should be considered hypothesis-generating and confirmed by studies specifically designed for this purpose. Fourth, patients in the EDEN cohort were included by episode rather than by patient, and some episodes may have corresponded to the same patient. However, as the inclusion period was very short (7 days), the chance of a repeat visit for a particular patient was low. Finally, the inclusion period was limited to a single week of the year. Pathologies affecting older adult patients may differ depending on the season of the year, especially related to infectious diseases. However, the large number of included patients may have limited the impact of this consideration.
In conclusion, male sex, age ≥75 years, ED arrival by ambulance, the presence of functional impairment, or severe comorbidity are features of patients in whom the application of a specific approach different from common triage may be useful in the ED to improve the poor short-term outcomes of this population. While it may be difficult to integrate these variables into the structured triage systems already established in EDs, alerts could be included in the electronic medical histories of EDs to make attending physicians aware of the possible need for a specialized taxonomic approach.
Footnotes
This article was prepared on behalf of the local investigators of the SIESTA network by Hospital Clínico San Carlos, Madrid: Jorge García Lamberechts, Paula Queizán García, Andrea B Bravo Periago, Blanca Andrea Gallardo Sánchez, Alejandro Melcon Villalibre, Sara Vargas Lobé, Laura Fernández García; Hospital Universitario Infanta Cristina, Parla: Ángel Iván Diaz Salado, Alicia Fuente Gaforio, Cristina Güemes de la Iglesia, Beatriz Honrado Galán; Hospital Santa Tecla, Tarragona: Enrique Martín Mojarro, Sílvia Flores Quesada; Hospital Universitario de Canarias, Tenerife: Aarati Vaswani-Bulchand, Patricia Eiroa-Hernández; Hospital Norte Tenerife: Patricia Parra-Esquivel; Hospital General Universitario Reina Sofia, Murcia: Pascual Piñera Salmerón, José Andrés Sánchez Nicolás, Manuel E. Castillo Vargas, María del Carmen Molina Morazo, Elena Sánchez García, Eduardo Alarcón Capel; Hospital Universitario del Henares, Madrid: Elena Cavero Porrero, Irene Iglesias Campos, Eloisa Delgado Torres: Hospital Clinic, Barcelona: Sonia Jiménez, Francesc Xavier Alemany González, María Florencia Poblete Palacios, Claudia Lorena Amarilla Molinas, Ivet Gina Osorio Quispe, Sandra Cuerpo Cardeñosa; Hospital General Universitario de Elche: Matilde González Tejera, Ana Puche Alcaraz, Cristina Chacón García; Hospital Universitario y Politécnico La Fe, Valencia: Leticia Serrano Lázaro, Javier Millán Soria, Jésica Mansilla Collado, María Bóveda García; Hospital. General Universitario Dr. Balmis, Alicante: Adriana Gil Rodrigo, Begoña Espinosa Fernández, Mónica Veguillas Benito, Sergio Guzmán Martínez, Gema Jara Torres, María Caballero Martínez; Hospital Universitario de Bellvitge, L'Hospitalet de Llobregat, Barcelona: Ferran Llopis, Elena Fuentes, Lidia Fuentes, Francisco Chamorro, Lara Guillen, Nieves López; Hospital de la Axiarquia de Velez-Malaga: Lucía Zambrano Serrano, Rocío Muñoz Martos, Rocío Lorenzo Álvarez; Hospital Regional Universitario de Málaga: Manuel Salido Mota, Valle Toro Gallardo, Antonio Real López, Lucía Ocaña Martínez, Esther Muñoz Soler, Mario Lozano Sánchez, Eva Fraguero Blesa; Hospital Santa Barbara, Soria: Fahd Beddar Chaib, Rodrigo Javier Gil Hernández; Hospital Valle Pedroches, Pozoblanco, Cordoba: Jorge Pedraza García, Paula Pedraza Ramírez; Hospital Reina Sofia, Córdoba: F. Javier Montero-Pérez, Carmen Lucena Aguilera, F. de Borja Quero Espinosa, Angela Cobos Requena, Esperanza Muñoz Triano, Inmaculada Bajo Fernández, María Calderón Caro, Sierra Bretones Baena; Hospital Universitario Gregorio Marañon, Madrid: Esther Gargallo Garcia, Juan Antonio Andueza Lillo, Iria Miguens Blanco, Ioana Muñoz Betegón, Dariela Edith Micheloud Giménez, Jorge Sánchez-Tembleque Sánchez, Belén Macías Bou, Paloma Díez Romero; Hospital Universitario de Burgos: Maria Pilar López Diez, Karla López López, Ricardo Hernández Cardona, Leopoldo Sánchez Santos, Monika D’ Oliveira Millán; Complejo Asistencial Universitario de León: Marta Iglesias Vela, Mónica Santos Orús, Rudiger Carlos Chávez Flores, Alberto Álvarez Madrigal, Albert Carbó Jordá, Enrique González Revuelta, Héctor Lago Gancedo; Hospital Universitario Morales Meseguer, Murcia: Rafael Antonio Pérez-Costa, María Rodríguez Romero, Esperanza Marín Arranz, Ana Barnes Parra; Hospital Francecs de Borja de Gandía: María José Fortuny Bayarri, José Sananton López, Sonia Losada Figarella, Silvia Mainero Mendoza; Hospital Universitario Severo Ochoa, Leganés: María José Hernández Martínez, Ana Benito Blanco, Vanesa Abad Cuñado, Julia Martínez-Ibarreta Zorita, Irene Cabrera Rodrigo; Hospital Universitario Virgen Arrixaca, Murcia: Eva Quero Motto, Nuria Tomas Garcia, Laura Bernal Martínez, Miguel Parra Morata; Hospital Universitario Lorenzo Guirao, Cieza: Carmen Escudero Sánchez, José Joaquín Giménez Belló; Hospital Josep Trueta, Girona: Maria Adroher Muñoz, Ester Soy Ferrer, Eduard Anton Poch Ferrer; Hospital de Mendaro, Gipuzkoa: Jeong-Uh Hong Cho; Hospital Miguel Servet, Zaragoza: Patricia Trenc Español, Fernando López López, Jorge Navarro Calzada, Belén Gros Bañeres, Cristina Martín Durán, María Teresa Escolar Martínez-Berganza, Iciar González Salvatierra, Hospital Comarcal El Escorial, Madrid: Sara Gayoso Martín; Hospital Do Salnes, Villagarcía de Arosa: Goretti Sánchez Sindín; Hospital de Barbanza. Ribeira, A Coruña: Azucena Prieto Zapico, Jésica Pazos González; Hospital del Mar, Barcelona: Isabel Cirera Lorenzo, Patricia Gallardo Vizcaíno, Margarita Puiggali Ballard, M Carmen Petrus Rivas; Hospital Santa Creu y Sant Pau, Barcelona: Adriana Laura Doi Grande, Sergio Herrera Mateo, OlgaTrejo Gutiérrez, Paola Ponte Márquez, Carlos Romero Carrete, Sergio Pérez Baena; Hospital de Vic: Lluís Llauger; Hospital del Nalón, Langreo, Asturias: Ana Murcia Olagüenaga, Sayoa Francesena González, Cesar Roza Alonso; Hospital Altagracia, Manzanares: Ivana Tavasci Lopez, Edmundo Ramon Figuera Castro; Hospital Nuestra Señora del Prado de Talavera de la Reina: Ricardo Juárez González, Mar Sousa, Laura Molina, Mónica Cañete; Hospital Universitario Vinalopó, Elche: Esther Ruescas, María Martínez Juan, María José Blanco Hoffman, Pedro Ruiz Asensio; Hospital de Móstoles: Fátima Fernández Salgado, Eva de las Nieves Rodríguez, Gema Gómez García, Beatriz Paderne Díaz; Hospital Virgen del Rocio: Amparo Fernández-Simón Almela, Esther Pérez García, Pedro Rivas Del Valle, María Sánchez Moreno, Rafaela Rios Gallardo, Teresa Pablos Pizarro, Mariano Herranz García, Laura Redondo Lora; Hospital General Universitario Dr. Peset, Valencia: María Amparo Berenguer Diez, María Ángeles De Juan Gómez, María Luisa López Grima; Hospital Universitario Son Espases: Bernardino Comas Diaz, Sandra Guiu Martí, Juan Domínguez Casasola, Pere Rull Bertrán, Núria Perelló Viola; Clinica Universitaria Navarra Madrid: Nieves López-Laguna, Lourdes Hernández-Castells, Clinico Universitario De Valencia, José J. Noceda Bermejo, María Teresa Sánchez Moreno, Raquel Benavent Campos, Jacinto García Acosta, Alejandro Cortés Soler; Hospital Alvaro Cunqueiro, Vigo: María Teresa Maza Vera, Raquel Rodríguez Calveiro, Paz Balado Dacosta, Violeta Delgado Sardina, Emma González Nespereira, Carmen Fernández Domato, Elena Sánchez Fernández-Linares; Hospital Universitario de Salamanca: Ángel García García, Francisco Javier Diego Robledo, Manuel Ángel Palomero Martín, Jesús Ángel Sánchez Serrano; Hospital de Zumarraga, Guipuzcoa: Patxi Ezponda; Hospital Virxe da Xunqueira, A Coruña: Andrea Martínez Lorenzo; Hospital Universitario Los Arcos del Mar Menor, San Javier, Murcia: Juan Vicente Ortega Liarte; Hospital Universitario Río Ortega Valladolid: Susana Sánchez Ramón, Inmaculada García Rupérez, Pablo González Garcinuño, Raquel Hernando Fernández, José Ramón Oliva Ramos, Virginia Carbajosa Rodríguez; Hospital Juan Ramón Jiménez, Huelva: Jose Maria Santos Martin, Setefilla Borne Jerez, Asumpta Ruiz Aranda, Maria José Marchena; Hospital Central de Asturias, Oviedo: Eugenia Prieto Piquero, Hugo Mendes Moreira, Isabel Lobo Cortizo, Jennifer Turcios Torres, Lucia Hinojosa Diaz, Jesús Santianes Patiño, Octavio Gutiérrez Alcalá.
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization, JGC, OM; Data curation, NLA, SGG; Investigation, JGC; Methodology, NLA, SGG; Supervision, JGC; Writing-original draft, NLA, JGC; Writing-review & editing, NLA, JGC.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4235/agmr.23.0121.
Comparative analysis of risk factors for poor outcome in people over 65 years of age with respect to 30-day mortality, readmission, and re-presentation
Univariate analysis for poor outcomes in people over 65 years of age for 30-day mortality, readmission, and re-presentation using univariate survival models
REFERENCES
- 1.King AII, Boyd ML, Raphael DL, Jull A. The effect of a gerontology nurse specialist for high needs older people in the community on healthcare utilisation: a controlled before-after study. BMC Geriatr. 2018;18:22. doi: 10.1186/s12877-018-0717-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Instituto Nacional de Estadistica . Madrid, Spain: Instituto Nacional de Estadistica; 2021. [Demographics in Europe] [Internet] [cited 2023 Nov 30]. Available from: https://www.ine.es/prodyser/demografia_UE/bloc-1c.html?lang=es. [Google Scholar]
- 3.Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS One. 2018;13:e0203316. doi: 10.1371/journal.pone.0203316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pines JM, Griffey RT. What we have learned from a decade of ED crowding research. Acad Emerg Med. 2015;22:985–7. doi: 10.1111/acem.12716. [DOI] [PubMed] [Google Scholar]
- 5.Schouten B, Driesen BE, Merten H, Burger BH, Hartjes MG, Nanayakkara PW, et al. Experiences and perspectives of older patients with a return visit to the emergency department within 30 days: patient journey mapping. Eur Geriatr Med. 2022;13:339–50. doi: 10.1007/s41999-021-00581-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin-Sanchez FJ, Fernandez Alonso C, Gil Gregorio P. Key points in healthcare of frail elders in the emergency department. Med Clin (Barc) 2013;140:24–9. doi: 10.1016/j.medcli.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez Del Castillo J, Escobar-Curbelo L, Martinez-Ortiz de Zarate M, Llopis-Roca F, Garcia-Lamberechts J, Moreno-Cuervo A, et al. GYM score: 30-day mortality predictive model in elderly patients attended in the emergency department with infection. Eur J Emerg Med. 2017;24:183–8. doi: 10.1097/MEJ.0000000000000321. [DOI] [PubMed] [Google Scholar]
- 8.Puig-Campmany M, Ris-Romeu J. Frail older patients in the emergency department: main challenges. Emergencias. 2022;34:415–7. [PubMed] [Google Scholar]
- 9.Blomaard LC, de Groot B, Lucke JA, de Gelder J, Booijen AM, Gussekloo J, et al. Implementation of the acutely presenting older patient (APOP) screening program in routine emergency department care : a before-after study. Z Gerontol Geriatr. 2021;54:113–21. doi: 10.1007/s00391-020-01837-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wallis M, Marsden E, Taylor A, Craswell A, Broadbent M, Barnett A, et al. The Geriatric Emergency Department Intervention model of care: a pragmatic trial. BMC Geriatr. 2018;18:297. doi: 10.1186/s12877-018-0992-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heeren P, Devriendt E, Fieuws S, Wellens NI, Deschodt M, Flamaing J, et al. Unplanned readmission prevention by a geriatric emergency network for transitional care (URGENT): a prospective before-after study. BMC Geriatr. 2019;19:215. doi: 10.1186/s12877-019-1233-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garcia-Martinez A, Gil-Rodrigo A, Placer A, Alemany X, Aguilo S, Torres-Machado V, et al. Probability of new falls and factors associated with them in aged patients treated in emergency departments after falling: data from the FALL-ER registry. Emergencias. 2022;34:444–51. [PubMed] [Google Scholar]
- 13.Afonso-Argiles FJ, Comas Serrano M, Blazquez-Andion M, Castells Oliveres X, Cirera Lorenzo I, Garcia Perez D, et al. Factors associated with short-term mortality after emergency department care of residents living in aged care homes: findings from the multicenter Caregency study. Emergencias. 2022;34:437–43. [PubMed] [Google Scholar]
- 14.Kolk D, Kruiswijk AF, MacNeil-Vroomen JL, Ridderikhof ML, Buurman BM. Older patients’ perspectives on factors contributing to frequent visits to the emergency department: a qualitative interview study. BMC Public Health. 2021;21:1709. doi: 10.1186/s12889-021-11755-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karam G, Radden Z, Berall LE, Cheng C, Gruneir A. Efficacy of emergency department-based interventions designed to reduce repeat visits and other adverse outcomes for older patients after discharge: a systematic review. Geriatr Gerontol Int. 2015;15:1107–17. doi: 10.1111/ggi.12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim H, Han SJ, Lee JH, Lim J, Moon SD, Moon H, et al. A descriptive study of emergency department visits within 30 days of discharge. Ann Geriatr Med Res. 2021;25:245–51. doi: 10.4235/agmr.21.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Montero-Perez J. Emergency triage: separating the wheat from the chaff. Emergencias. 2022;34:161–2. [PubMed] [Google Scholar]
- 18.Platts-Mills TF, Travers D, Biese K, McCall B, Kizer S, LaMantia M, et al. Accuracy of the Emergency Severity Index triage instrument for identifying elder emergency department patients receiving an immediate life-saving intervention. Acad Emerg Med. 2010;17:238–43. doi: 10.1111/j.1553-2712.2010.00670.x. [DOI] [PubMed] [Google Scholar]
- 19.Brouns SH, Mignot-Evers L, Derkx F, Lambooij SL, Dieleman JP, Haak HR. Performance of the Manchester triage system in older emergency department patients: a retrospective cohort study. BMC Emerg Med. 2019;19:3. doi: 10.1186/s12873-018-0217-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zachariasse JM, Seiger N, Rood PP, Alves CF, Freitas P, Smit FJ, et al. Validity of the Manchester Triage System in emergency care: a prospective observational study. PLoS One. 2017;12:e0170811. doi: 10.1371/journal.pone.0170811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carpenter CR, Shelton E, Fowler S, Suffoletto B, Platts-Mills TF, Rothman RE, et al. Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta-analysis. Acad Emerg Med. 2015;22:1–21. doi: 10.1111/acem.12569. [DOI] [PubMed] [Google Scholar]
- 22.McCusker J, Bellavance F, Cardin S, Trepanier S, Verdon J, Ardman O. Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc. 1999;47:1229–37. doi: 10.1111/j.1532-5415.1999.tb05204.x. [DOI] [PubMed] [Google Scholar]
- 23.Cousins G, Bennett Z, Dillon G, Smith SM, Galvin R. Adverse outcomes in older adults attending emergency department: systematic review and meta-analysis of the Triage Risk Stratification Tool. Eur J Emerg Med. 2013;20:230–9. doi: 10.1097/MEJ.0b013e3283606ba6. [DOI] [PubMed] [Google Scholar]
- 24.de Gelder J, Lucke JA, de Groot B, Fogteloo AJ, Anten S, Mesri K, et al. Predicting adverse health outcomes in older emergency department patients: the APOP study. Neth J Med. 2016;74:342–52. [PubMed] [Google Scholar]
- 25.Jay S, Whittaker P, Mcintosh J, Hadden N. Can consultant geriatrician led comprehensive geriatric assessment in the emergency department reduce hospital admission rate? A systematic review. Age Ageing. 2017;46:366–72. doi: 10.1093/ageing/afw231. [DOI] [PubMed] [Google Scholar]
- 26.Miro O, Gonzalez Del Castillo J. Collaboration among Spanish emergency departments to promote research: on the creation of the SIESTA (Spanish Investigators in Emergency Situations TeAm) network and the coordination of the UMC-19 (Unusual Manifestations of COVID-19) macroproject. Emergencias. 2020;32:269–77. [PubMed] [Google Scholar]
- 27.Miro O, Gonzalez Del Castillo J. SIESTA: the Spanish Investigators in Emergency Situations TeAm - during the COVID-19 pandemic: a summary of results of the network’s first challenge. Emergencias. 2022;34:225–7. [PubMed] [Google Scholar]
- 28.Noh JH, Jung HW, Ga H, Lim JY. Ethical guidelines for publishing in the Annals of Geriatric Medicine and Research. Ann Geriatr Med Res. 2022;26:1–3. doi: 10.4235/agmr.22.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sullivan LM, Massaro JM, D’Agostino RB Sr. Presentation of multivariate data for clinical use: the Framingham Study risk score functions. Stat Med. 2004;23:1631–60. doi: 10.1002/sim.1742. [DOI] [PubMed] [Google Scholar]
- 30.Kuriyama A, Ikegami T, Nakayama T. Impact of age on the discriminative ability of an emergency triage system: a cohort study. Acta Anaesthesiol Scand. 2019;63:781–8. doi: 10.1111/aas.13342. [DOI] [PubMed] [Google Scholar]
- 31.Gasperini B, Cherubini A, Fazi A, Maracchini G, Prospero E. Older adults in emergency departments: the challenge of undertriage. Intern Emerg Med. 2016;11:1145–7. doi: 10.1007/s11739-016-1503-x. [DOI] [PubMed] [Google Scholar]
- 32.Blomaard LC, Speksnijder C, Lucke JA, de Gelder J, Anten S, Schuit SC, et al. Geriatric screening, triage urgency, and 30-day mortality in older emergency department patients. J Am Geriatr Soc. 2020;68:1755–62. doi: 10.1111/jgs.16427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kabell Nissen S, Rueegg M, Carpenter CR, Kaeppeli T, Busch JM, Fournaise A, et al. Prognosis for older people at presentation to emergency department based on frailty and aggregated vital signs. J Am Geriatr Soc. 2023;71:1250–8. doi: 10.1111/jgs.18170. [DOI] [PubMed] [Google Scholar]
- 34.American College of Emergency Physicians . Irving, TX: American College of Emergency Physicians; c2023. Geriatric emergency department accreditation program [Internet] [cited 2023 Nov 30]. Available from: https://www.acep.org/geda/ [Google Scholar]
- 35.Hesselink G, Demirbas M, Rikkert MO, Schoon Y. Geriatric education programs for emergency department professionals: a systematic review. J Am Geriatr Soc. 2019;67:2402–9. doi: 10.1111/jgs.16067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Gelder J, Lucke JA, Blomaard LC, Booijen AM, Fogteloo AJ, Anten S, et al. Optimization of the APOP screener to predict functional decline or mortality in older emergency department patients: cross-validation in four prospective cohorts. Exp Gerontol. 2018;110:253–9. doi: 10.1016/j.exger.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 37.Fries BE, Morris JN, Skarupski KA, Blaum CS, Galecki A, Bookstein F, et al. Accelerated dysfunction among the very oldest-old in nursing homes. J Gerontol A Biol Sci Med Sci. 2000;55:M336–41. doi: 10.1093/gerona/55.6.m336. [DOI] [PubMed] [Google Scholar]
- 38.World Health Organization . Geneva, Switzerland: World Health Organization; 2022. Ageing and health [Internet] [cited 2023 Nov 30]. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparative analysis of risk factors for poor outcome in people over 65 years of age with respect to 30-day mortality, readmission, and re-presentation
Univariate analysis for poor outcomes in people over 65 years of age for 30-day mortality, readmission, and re-presentation using univariate survival models