Abstract
Background
Syndesmotic injuries are frequently stabilized using syndesmotic screws. Traditionally, these screws were routinely removed during the postoperative period, however recent literature has brought into question the necessity of routine removal, citing no change in functional outcomes and the inherent risks of a second surgery. Our study aimed to compare outcomes of patients undergoing routine syndesmotic screw removal versus those undergoing an on-demand approach to removal.
Methods
A systematic search of studies comparing routine syndesmotic screw removal to on-demand screw removal following an acute ankle fracture, or an isolated syndesmotic injury was conducted across seven databases. Only Prospective randomized controlled trials were eligible for inclusion. Data reported on by at least 2 studies was pooled for analysis.
Results
Three studies were identified that met inclusion and exclusion criteria. No significant difference in Olerud-Molander Ankle Score (MD -2.36, 95% CI -6.50 to 1.78, p = 0.26), American Orthopedic Foot and Ankle Hindfoot Score (MD -0.45, 95% CI -1.59 to .69, p = 0.44), or dorsiflexion (MD 2.20, 95% CI -0.50 to 4.89, p = 0.11) was found between the routine removal group and on-demand removal group at 1-year postoperatively. Routine removal was associated with a significantly higher rate of complications than on-demand removal (RR 3.02, 95% CI 1.64 to 5.54, p = 0.0004). None of the included studies found significant differences in pain scores or range of motion by 1-year postoperatively.
Conclusion
Given the increased risk of complications with routine syndesmotic screw removal and the comparable outcomes when screws are retained, an as-needed approach to syndesmotic screw removal should be considered.
Keywords: Syndesmosis, Syndesmotic screw, Ankle fracture, Distal tibiofibular ligament, Routine removal, Syndesmotic screw removal, Syndesmotic injury
1. Introduction
With an incidence of 2.09 per 100,000 person-years, syndesmotic injuries affect an estimated 13% of all ankle sprains.1, 2, 3 Despite their prevalence, syndesmotic injuries can be difficult to diagnose and may often go missed.4 When left untreated they can lead to chronic instability and eventual degenerative arthritis.5 Thus, optimally repairing these injuries is crucial to prevent short and long-term issues.
Operative repair is often indicated for unstable syndesmotic injuries, with the treatment goal being maintenance of syndesmotic stability to facilitate healing of injured ligaments. Historically, screw fixation is utilized and is typically accomplished by using one 3.5 mm screw through three or four cortices.6 This exact methodology for screw fixation, with regard to the number and sizes of the screw used, as well as the number of cortices involved, remains a matter of debate. Yet the literature has consistently shown there is no difference in outcomes between using one or two screws, 3.5- or 4.5-mm screws, or 3 versus 4 cortices, respectively.7, 8, 9, 10
An additional point of discussion in clinical practice is whether patients should undergo routine syndesmotic screw removal. Despite previously being the standard of care and its continued widespread use, there has not been definitive evidence supporting the superiority of routine removal.10 Potential drawbacks that have been associated with the retention of syndesmotic screws include decreased ankle range of motion and discomfort.11 Yet prior meta-analyses have shown there to be no significant difference in patient outcomes after undergoing routine removal compared to those employing an on-demand approach, suggesting that routine removal may not be necessary for all patients.12, 13, 14, 15 This additional procedure is not inconsequential; studies have highlighted the inconvenience and potential for complications, such as wound infection, associated with the routine removal of syndesmotic screws.16, 17, 18
Previous systematic reviews on this topic did not limit their inclusion criteria to Randomized Controlled Trials (RCTs), thus weakening the strength of their results.12, 13, 14, 15 This was likely done because of the paucity of available RCTs on the topic. Notably, however, the “ROutine vs on DEmand removal Of the syndesmotic screw’ (RODEO)” trial, was recently completed in 2021.19 Being the largest multicenter RCT on this topic thus far, a new meta-analysis including their results is warranted.
Our study aims to compare the patient outcomes of those undergoing routine syndesmotic screw removal and those undergoing an on-demand approach to removal using data solely from RCTs. By critically examining level 1 evidence, we will provide stronger support for adopting an on-demand approach to syndesmotic screw removal and show that it has comparable outcomes to routine removal.
2. Methods
2.1. Ethical statement
Our study utilized information from previously conducted studies, thus obviating the need for institutional review board approval. As all the data had been previously published, patient consent was deemed unnecessary for this study. This study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Our protocol details were registered in the PROSPERO database (CRD42023489342), National Institute for Health Research, University of York, Center for Reviews and Dissemination.
2.2. Search strategy and selection criteria
In December 2023, a systematic search for studies comparing routine versus on-demand syndesmotic screw removal was conducted on seven databases (MEDLINE, Embase, Cochrane CENTRAL, CINAHL, Web of Science, PubMed, and ClinicalTrials.gov). The full search syntax used is provided in the supplementary tables. No filters for publication years, language, age, or study design were used.
Only Prospective RCTs comparing routine removal and on-demand removal of syndesmotic screws following an acute ankle fracture or an isolated syndesmotic injury were eligible for inclusion. Literature such as case series, cadaveric studies, and prior reviews were excluded.
2.3. Study selection
Search results were uploaded to Covidence data extraction tool (Veritas Health Innovation, Melbourne, Australia) and automatically deduplicated. The Cochrane RCT Classifier developed by EPPI-Center, which has a sensitivity of 99.5% for detecting RCTs, was used to automatically screen out non-RCT (“ineligible”) studies.20 The first author reviewed the titles and abstracts of studies marked ineligible by the Cochrane RCT Classifier to ensure eligible studies were not erroneously excluded.
Two independent reviewers screened studies marked as eligible via title and abstract to determine project relevancy. Subsequent studies deemed relevant would undergo full-text review by two independent reviewers using predetermined inclusion and exclusion criteria. All screening was done independently, with voting concealed from other reviewers. If consensus between two reviewers could not be reached, the help of a third reviewer was enlisted to cast the deciding vote.
2.4. Data extraction
Data extraction was completed by two independent reviewers using predetermined templates within Covidence. The data collected with the use of the Covidence templates included general study information (author, year of publication, study identifiers), study methods (design, aim, unit of analysis, method of recruitment), baseline characteristics of the population (number randomized, age, sex, BMI), interventions (routine removal, on-demand removal), and outcomes (functional outcome scores, pain scores, and complications as defined by the authors of the respective article).
Certain complications such as screw breakage or loosening were excluded from data aggregation despite being reported as complications by some authors due to reports that loosened or broken screws may have superior functional outcomes and thus do not necessitate removal.21, 22, 23
2.5. Methodological quality assessment
The quality of included studies was assessed using the Cochrane Risk of Bias 2 (RoB2) tool and each study was assessed by two reviewers.24 Parameters for each study such as sequence generation, allocation concealment, blinding, etc. were rated as either ‘Low’, ‘High’, or ‘Some concern’.
2.6. Statistical analysis
The meta-analysis consisted of pooled data from outcomes that were reported on by at least 2 studies using Review Manager Software (RevMan 5.4.1). Studies that reported no events in either the routine removal or the on-demand removal group for a particular outcome were excluded from the analysis, in accordance with the Cochrane Handbook for Systematic Reviews.25 The mean difference (MD) was calculated for continuous outcomes and standard deviations were used to estimate the variance. When the mean was not reported, it was estimated using the reported median and range. Standard deviation was then estimated based on the reported range.26 The risk ratio (RR) was calculated when analyzing the total complications reported. Point estimates for all measures were calculated with their corresponding 95% confidence intervals (CIs) and two-tailed tests of significance were performed with a value of 0.05.
Heterogeneity was evaluated by calculating the I2 index; values > 51% represented moderate to high heterogeneity. The random-effect model was applied if I2 was ≥51%; the common-effect model was applied if the I2 value was less than ≤50%.
3. Results
3.1. Search
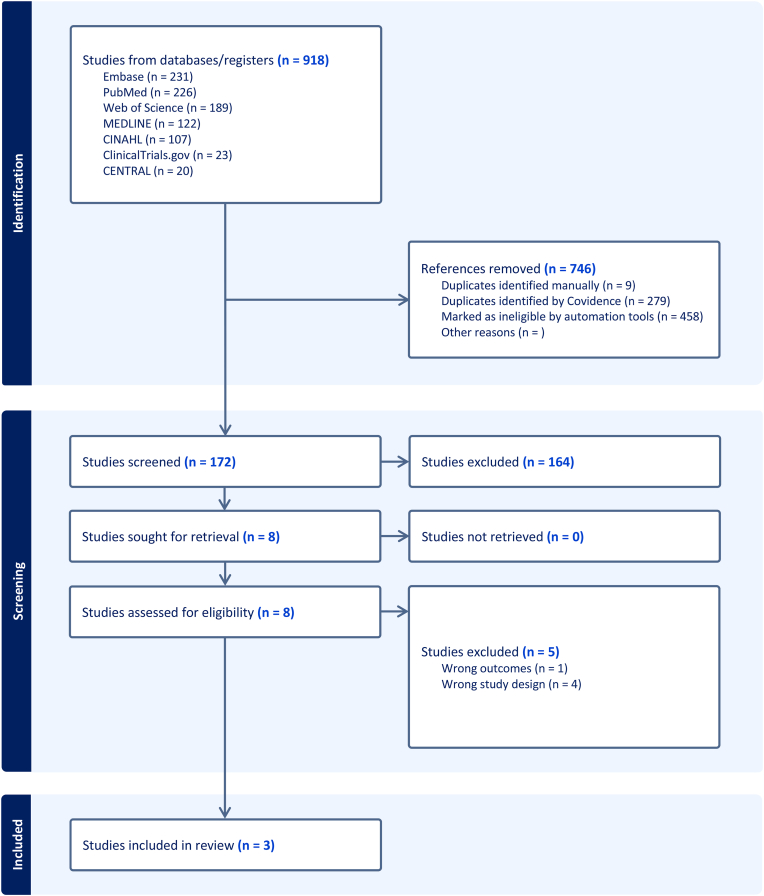
The systematic search, after the removal of duplicate studies, returned 630 articles. After title/abstract and full-text screening, only 3 RCTs were eligible for inclusion in this study (Fig. 1).7,16,17 An overview of the included studies is available in the supplementary tables.
Fig. 1.
PRISMA flow diagram showing study selection.
3.2. Included study characteristics
Of the included studies, only Boyle et al., 2014 controlled for fixation construct, using a singular 4.0 mm screw to engage 4 cortices (Table 1).16 Sanders et al., 2021 used 1 or 2 syndesmotic screws, with sizes ranging from 3.0 to 4.5 mm, to engage 3 or 4 cortices in both groups, with the most common choices, across both groups, being singular, 3.5 mm, and 3 cortices, respectively.17 Høiness and Strømsøe 2004 used either a singular 4.5 mm screw to engage 4 cortices or two 3.5 mm screws to engage 3 cortices, depending on which removal group the patient was in (Table 1).7 Of the included studies only Sanders et al., 2021 allowed for the inclusion of patients with an isolated syndesmotic injury, this ultimately accounted for 2 of the patients in our analysis.
Table 1.
Patient demographics & surgical characteristics.
| SandersFRK 2021 |
Boyle 2014 |
Høiness 2004 |
||||
|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Control | Intervention | |
| Female n (%) | 26 (46) | 36 (56) | 7 (26.9) | 9 (36) | 13 (43.3) | 19 (55.9) |
| Age (mean, SD) | 45.3, 15 | 48.3, 14 | 30.8, 12.8 | 36.2,14.1 | 41.8, 17.9 | 42.4, 14.7 |
| BMI (kg/m2) (mean, SD) | 27, 4 | 29, 6 | 30.6, 4.6 | 31.9, 5.5 | 27.1, 3.32 | 25.9, 3.27 |
| Nicotine Use n (%) | 17 (25) | 18 (24) | 9 (34.6) | 8 (32) | 4 (13.3) | 10 (29.4) |
| Diabetic n (%) | 3 (4) | 4 (5) | 0 (0) | 1 (4) | 1 (3.3) | 1 (2.9) |
| Number of Screws n (%) | ||||||
| 1 | 50 (69) | 51 (65) | 26 (100) | 25 (100) | 30 (100) | 0 (0) |
| 2 | 22 (31) | 28 (35) | 0 (0) | 0 (0) | 0 (0) | 34 (100) |
| Fixation through 3 Cortices n (%) | 57 (79) | 62 (78) | 0 (0) | 0 (0) | 0 (0) | 34 (100) |
| Fixation through 4 Cortices n (%) | 15 (21) | 17 (22) | 26 (100) | 25 (100) | 30 (100) | 0 (0) |
3.3. Outcomes
The three included studies respectively found there was no significant difference in functional outcome scores by the 1-year follow-up. Scoring methods differed among the included studies, with some using the American Orthopedic Foot and Ankle Hindfoot Score (AOFAS) and others using the American Academy of Orthopedic Surgeons (AAOS) foot and ankle scores. Only the Olerud-Molander Ankle Score (OMAS) was used by all three respective studies. OMAS is a patient-reported outcome measure (PROM) with a minimum score of 0 (completely impaired function) to 100 (complete function).27 It has an MCID of 7.5–10.5 at 12 months of follow-up.28 Pooled data analysis across 267 participants revealed patients in the routine removal group had a slightly lower OMAS compared to patients in the on-demand removal group at one-year follow-up, but this did not reach statistical significance MD -2.36, 95% CI -6.50 to 1.78, p = 0.26 (Fig. 2).
Fig. 2.
Forest plot for Olerud-Molander Ankle Score at 12 months.
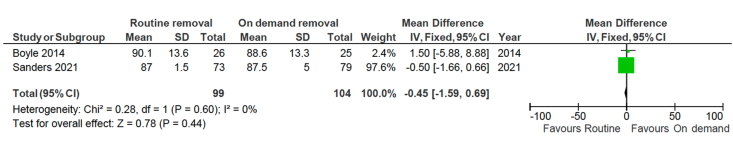
AOFAS was reported by 2 of the included studies.16,17 AOFAS is a PROM with a minimum score of 0 (completely impaired function) to 100 (complete function); the MCID for ankle fracture patients has not been determined.29 Pooled data analysis across 203 participants revealed patients in the routine removal group had a slightly lower AOFAS compared to patients in the on-demand removal group at one-year follow-up, but similarly to OMAS, this did not reach statistical significance MD -0.45, 95% CI -1.59 to 0.69, p = 0.44 (Fig. 3).
Fig. 3.
Forest plot for American Orthopedic Foot and Ankle Hindfoot Score at 12 months.
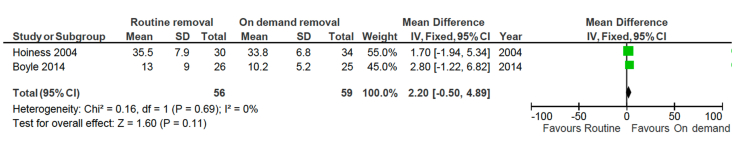
Ankle dorsiflexion at 1 year postoperatively was reported by 2 out of the 3 studies.7,16 Pooled data analysis across 115 participants revealed that patients in the routine removal group achieved slightly more dorsiflexion compared to patients in the on-demand removal group at one-year follow-up, but this did not reach statistical significance: MD 2.20, 95% CI -0.50 to 4.89, p = 0.11 (Fig. 4).
Fig. 4.
Forest plot for degrees of dorsiflexion in the affected ankle.
All 3 studies reported pain scores and range of motion (ROM), but the different reporting methods made data pooling for these respective measures impossible. Notably, none of the included studies found routine removal or on-demand removal to cause a significant difference in pain scores or ROM by the 1-year follow-up.
The total amount of complications was reported by all 3 of the included studies. Such complications included wound infection, diastasis, and synovitis (Table 2). Pooled data analysis across 267 participants revealed patients in the routine removal group had a significantly increased risk of experiencing a complication compared to patients in the on-demand removal group: RR 3.02, 95% CI 1.64 to 5.54, p = 0.0004 (Fig. 5).
Table 2.
Reported complications within the first postoperative year.
| Sanders 2021 |
Boyle 2014 |
Høiness 2004 |
||||
|---|---|---|---|---|---|---|
| Control (n) | Intervention (n) | Control (n) | Intervention (n) | Control (n) | Intervention (n) | |
| Superficial Infection | 2 | 1 | 1 | 0 | 2 | 0 |
| Deep infection | 2 | 0 | 1 | 0 | 3 | 1 |
| Loss of reduction of the syndesmosis | — | — | — | — | 5 | 1 |
| Revision due to malreduction of the syndesmosis | — | — | — | — | 1 | 1 |
| Postoperative drop foot | — | — | — | — | 0 | 1 |
| Reduction of joint space less than 50% | — | — | — | — | 5 | 4 |
| Tricortical syndesmosis screws too long | — | — | — | — | – | 1 |
| Wound dehiscence | 5 | 0 | — | — | – | – |
| Diastasis after removal | 1 | 0 | — | — | – | – |
| Recurrent diastasis with a broken syndesmotic screw | — | — | 0 | 1 | – | – |
| Synovitis | 1 | 0 | — | — | – | – |
| Increase in stiffness after removal | 1 | 0 | — | — | – | – |
| Total | 12 | 1 | 2 | 1 | 16 | 9 |
—, data not reported.
Fig. 5.
Forest plot for total complications.
3.4. Risk of bias
Risk of bias assessment for the included studies can be seen in Supplemental Figs. S1 and S2. Similar to most RCTs investigating surgical treatments, the main sources of bias in our included studies stemmed from an inability to blind the research personnel and participants. Publication bias was not assessed due to insufficient studies.30
4. Discussion
Syndesmotic fixation is crucial in the healing process following a distal tibiofibular joint injury, yet the necessity of a second routine procedure to remove syndesmotic screws is debated. Our meta-analysis aimed to determine if patients undergoing routine syndesmotic screw removal and those undergoing an on-demand approach had similar functional outcomes and complication rates.
Our meta-analysis did not find any significant difference in OMAS, AOFAS, or degrees of dorsiflexion between routine removal and on-demand removal, but we did find routine removal to be associated with a significantly higher rate of complications. None of our included studies found a significant difference in pain scores, range of motion, or functional outcomes using different scoring methods. Our results support those of prior meta-analyses which included non-randomized studies.12, 13, 14, 15 Our increased complication rate was to be expected given prior literature showing 22% of removals experience some form of complication.31
Notably, a follow-up study of the RODEO trial patients also did not reveal significant differences in OMAS, AOFAS, Foot and Ankle Outcome Score (FAOS), and EuroQol five-dimension questionnaire (EQ-5D) score by the 4-year follow-up.32
Of the included studies, the RODEO trial had the highest rate of removal among the on-demand removal group; 23% by the 1-year follow-up. In the 4-year follow-up study, the removal rate among the on-demand group was 43% at 50 months. The increased costs, risk of complications, and non-superior outcomes associated with routine syndesmotic screw removal suggest that this should not be the standard of care.33
Alternative implants for syndesmotic fixation such as the suture button have been suggested as a solution that circumvents this debate, with many RCTs showing equal or superior outcomes compared to syndesmotic screws.34, 35, 36, 37 Despite this, their increased cost and concerns regarding their stability have likely contributed to their lack of widespread adoption.33,38, 39, 40
Our study, like other meta-analyses, is limited by the quality of our included studies. Firstly, Boyle et al., 2014 and Sanders et al., 2021 both had a high rate of patients lost to follow-up, 29% and 23% respectively, thus introducing a potential for selection bias.16,17 Additionally, post hoc power analyses conducted by other studies have criticized Boyle et al., 2014 as being underpowered for demonstrating non-inferiority between the two groups; however, the mathematics behind post hoc power analyses have been critiqued as a flawed.13,16,41 In the study by Høiness and Strømsøe the two groups did not receive the same initial treatment, with one group receiving two tricortical screws and the other receiving a singular quad-cortical screw, thus introducing the potential for confounding bias.7 While all included studies found comparable outcomes, it is worth noting that retained screws have the potential to eventually break and thus complicate any future procedures the patient may need. A notable example that comes to mind is the case of osteoarthritic patients needing a tibial nail or ankle replacement. Finally, data was not reported similarly across all studies, which limited our ability to pool data for meta-analysis. Given the wide range of patient-rated outcome measures and lack of consensus regarding a superior measure, future studies should continue to report their outcomes using multiple measures in order to allow results to be compared between studies.
5. Conclusion
In conclusion, this systematic review and meta-analysis did not reveal a significant difference in functional outcomes between routine removal and on-demand removal of syndesmotic screws at 1-year postoperatively. Both OMAS and AOFAS, as well as dorsiflexion measurements, showed no significant findings, suggesting that the choice of removal strategy does not significantly impact functional recovery. However, the significantly higher incidence of complications in the routine removal group raises important considerations about the risks and potential disadvantages of this approach. Thus, we support the recommendations by Walley et al., 2017.15 An as-needed approach to syndesmotic screw removal could be considered, with removal being performed in cases where implant failure leads to symptoms or malreduction of the syndesmosis.
Guardian/patient's consent
This item is not applicable because this study was a review of anonymized data.
Author contributions, CRediT
Conceptualization, DA; Methodology, DA, AM, EV, AAA; Investigation, DA, AS, KK, TC, PJ; Writing – Original Draft, DA, AS, KK, TC, PJ; Writing – Review & Editing, DA, KK, AM, EV, AAA; Resources, DA; Supervision, DA, KK, AM, EV, AAA.
Ethical statement
This study was not subject to institutional review board approval because it was a review of anonymized data.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Daniel Acevedo reports was provided by Nova Southeastern University. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2024.03.012.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Search syntax used for each respective database and number of results.
Overview of Included Studies.
Supplemental Fig. 1.
Risk of bias analysis.
Supplemental Fig. 2.
Risk of bias summary.
References
- 1.Langner I., Frank M., Kuehn J.P., et al. Acute inversion injury of the ankle without radiological abnormalities: assessment with high-field MR imaging and correlation of findings with clinical outcome. Skeletal Radiol. Apr 2011;40(4):423–430. doi: 10.1007/s00256-010-1017-y. [DOI] [PubMed] [Google Scholar]
- 2.Schoennagel B.P., Karul M., Avanesov M., et al. Isolated syndesmotic injury in acute ankle trauma: comparison of plain film radiography with 3T MRI. Eur J Radiol. Oct 2014;83(10):1856–1861. doi: 10.1016/j.ejrad.2014.06.034. [DOI] [PubMed] [Google Scholar]
- 3.Vosseller J.T., Karl J.W., Greisberg J.K. Incidence of syndesmotic injury. Orthopedics. Mar 2014;37(3):e226–e229. doi: 10.3928/01477447-20140225-53. [DOI] [PubMed] [Google Scholar]
- 4.Lin C.F., Gross M.L., Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. Jun 2006;36(6):372–384. doi: 10.2519/jospt.2006.2195. [DOI] [PubMed] [Google Scholar]
- 5.Jelinek J.A., Porter D.A. Management of unstable ankle fractures and syndesmosis injuries in athletes. Foot Ankle Clin. Jun 2009;14(2):277–298. doi: 10.1016/j.fcl.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Shafiq H., Iqbal Z., Khan M.N.H., et al. Ankle syndesmotic injury: tightrope vs screw fixation, A clinical academic survey. Ann Med Surg. 2021/09/01/2021;69 doi: 10.1016/j.amsu.2021.102680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Høiness P., Strømsøe K. Tricortical versus quadricortical syndesmosis fixation in ankle fractures: a prospective, randomized study comparing two methods of syndesmosis fixation. J Orthop Trauma. 2004;18(6):331–337. doi: 10.1097/00005131-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Moore J.A., Jr., Shank J.R., Morgan S.J., Smith W.R. Syndesmosis fixation: a comparison of three and four cortices of screw fixation without hardware removal. Foot Ankle Int. 2006;27(8):567–572. doi: 10.1177/107110070602700801. [DOI] [PubMed] [Google Scholar]
- 9.Thompson M.C., Gesink D.S. Biomechanical comparison of syndesmosis fixation with 3.5-and 4.5-millimeter stainless steel screws. Foot Ankle Int. 2000;21(9):736–741. doi: 10.1177/107110070002100904. [DOI] [PubMed] [Google Scholar]
- 10.Peek A.C., Fitzgerald C.E., Charalambides C. Syndesmosis screws: how many, what diameter, where and should they be removed? A literature review. Injury. Aug 2014;45(8):1262–1267. doi: 10.1016/j.injury.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Needleman R.L., Skrade D.A., Stiehl J.B. Effect of the syndesmotic screw on ankle motion. Foot Ankle. Aug 1989;10(1):17–24. doi: 10.1177/107110078901000104. [DOI] [PubMed] [Google Scholar]
- 12.Desouky O., Elseby A., Ghalab A.H. Removal of syndesmotic screw after fixation in ankle fractures: a systematic review. Cureus. Jun 4 2021;13(6) doi: 10.7759/cureus.15435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dingemans S.A., Rammelt S., White T.O., Goslings J.C., Schepers T. Should syndesmotic screws be removed after surgical fixation of unstable ankle fractures? a systematic review. Bone Joint Lett J. Nov 2016;98-b(11):1497–1504. doi: 10.1302/0301-620x.98b11.Bjj-2016-0202.R1. [DOI] [PubMed] [Google Scholar]
- 14.Khurana A., Kumar A., Katekar S., et al. Is routine removal of syndesmotic screw justified? A meta-analysis. Foot. Dec 2021;49 doi: 10.1016/j.foot.2021.101776. [DOI] [PubMed] [Google Scholar]
- 15.Walley K.C., Hofmann K.J., Velasco B.T., Kwon J.Y. Removal of hardware after syndesmotic screw fixation: a systematic literature review. Foot Ankle Spec. Jun 2017;10(3):252–257. doi: 10.1177/1938640016685153. [DOI] [PubMed] [Google Scholar]
- 16.Boyle M.J., Gao R., Frampton C.M.A., Coleman B. Removal of the syndesmotic screw after the surgical treatment of a fracture of the ankle in adult patients does not affect one-year outcomes A RANDOMISED CONTROLLED TRIAL. Bone Joint J. 2014;96B(12):1699–1705. doi: 10.1302/0301-620X.96B12.34258. [DOI] [PubMed] [Google Scholar]
- 17.Sanders F.R.K., Birnie M.F., Dingemans S.A., et al. 103-B. 2021. p. 1709. (Functional Outcome of Routine versus On-Demand Removal of the Syndesmotic Screw: A Multicentre Randomized Controlled Trial). 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andersen M.R., Frihagen F., Madsen J.E., Figved W. High complication rate after syndesmotic screw removal. Injury. 2015;46(11):2283–2287. doi: 10.1016/j.injury.2015.08.021. [DOI] [PubMed] [Google Scholar]
- 19.Sanders F.R.K., Birnie M.F., Dingemans S.A., et al. Functional outcome of routine versus on-demand removal of the syndesmotic screw: a multicentre randomized controlled trial. Bone Joint J. 2021;103(11):1709–1716. doi: 10.1302/0301-620X.103B11.BJJ-2021-0348.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas J., McDonald S., Noel-Storr A., et al. Machine learning reduced workload with minimal risk of missing studies: development and evaluation of a randomized controlled trial classifier for Cochrane Reviews. J Clin Epidemiol. May 2021;133:140–151. doi: 10.1016/j.jclinepi.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamid N., Loeffler B.J., Braddy W., Kellam J.F., Cohen B.E., Bosse M.J. Outcome after fixation of ankle fractures with an injury to the syndesmosis. J Bone Jt Surg Br. 2009;91-B(8):1069–1073. doi: 10.1302/0301-620x.91b8.22430. [DOI] [PubMed] [Google Scholar]
- 22.Kaftandziev I., Spasov M., Trpeski S., Zafirova-Ivanovska B., Bakota B. Fate of the syndesmotic screw—search for a prudent solution. Injury. 2015;46:S125–S129. doi: 10.1016/j.injury.2015.10.062. [DOI] [PubMed] [Google Scholar]
- 23.Manjoo A., Sanders D.W., Tieszer C., MacLeod M.D. Functional and radiographic results of patients with syndesmotic screw fixation: implications for screw removal. J Orthop Trauma. 2010;24(1) doi: 10.1097/BOT.0b013e3181a9f7a5. [DOI] [PubMed] [Google Scholar]
- 24.Sterne J.A.C., Savović J., Page M.J., et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. Aug 28 2019;366 doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 25.Higgins J.P., Green S. 2008. Cochrane handbook for systematic reviews of interventions. [Google Scholar]
- 26.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. Dec 19 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olerud C., Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103(3):190–194. doi: 10.1007/bf00435553. [DOI] [PubMed] [Google Scholar]
- 28.Penning D., Kleipool S., van Dieren S., Dingemans S.M., Schepers T. The minimal clinically important difference (MCID) of the Olerud Molander Ankle Score (OMAS) in patients with unstable ankle fracture. Arch Orthop Trauma Surg. Jun 2023;143(6):3103–3110. doi: 10.1007/s00402-022-04533-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kitaoka H.B., Alexander I.J., Adelaar R.S., Nunley J.A., Myerson M.S., Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994/07/01 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 30.Dalton J.E., Bolen S.D., Mascha E.J. Publication bias: the elephant in the review. Anesth Analg. Oct 2016;123(4):812–813. doi: 10.1213/ane.0000000000001596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schepers T., Van Lieshout E.M.M., de Vries M.R., Van der Elst M. Complications of syndesmotic screw removal. Foot Ankle Int. 2011/11/01 2011;32(11):1040–1044. doi: 10.3113/FAI.2011.1040. [DOI] [PubMed] [Google Scholar]
- 32.Svd Heuvel, Penning D., Sanders F., et al. Functional outcome of routine versus on-demand removal of the syndesmotic screw. Bone Joint Open. 2023;4(12):957–963. doi: 10.1302/2633-1462.412.Bjo-2023-0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Penning D., Sanders F.R.K., van Dieren S., et al. Cost-effectiveness of on-demand removal of syndesmotic screws. Eur J Trauma Emerg Surg. Apr 2023;49(2):921–928. doi: 10.1007/s00068-022-02158-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andersen M.R., Frihagen F., Hellund J.C., Madsen J.E., Figved W. Randomized trial comparing suture button with single syndesmotic screw for syndesmosis injury. J Bone Joint Surg Am. Jan 3 2018;100(1):2–12. doi: 10.2106/jbjs.16.01011. [DOI] [PubMed] [Google Scholar]
- 35.Lehtola R., Leskelä H.V., Flinkkilä T., et al. Suture button versus syndesmosis screw fixation in pronation-external rotation ankle fractures: a minimum 6-year follow-up of a randomised controlled trial. Injury. Oct 2021;52(10):3143–3149. doi: 10.1016/j.injury.2021.06.025. [DOI] [PubMed] [Google Scholar]
- 36.Ræder B.W., Figved W., Madsen J.E., Frihagen F., Jacobsen S.B., Andersen M.R. Better outcome for suture button compared with single syndesmotic screw for syndesmosis injury: five-year results of a randomized controlled trial. Bone Joint Lett J. Feb 2020;102-b(2):212–219. doi: 10.1302/0301-620x.102b2.Bjj-2019-0692.R2. [DOI] [PubMed] [Google Scholar]
- 37.Ræder B.W., Stake I.K., Madsen J.E., et al. Randomized trial comparing suture button with single 3.5 mm syndesmotic screw for ankle syndesmosis injury: similar results at 2 years. Acta Orthop. Dec 2020;91(6):770–775. doi: 10.1080/17453674.2020.1818175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee J.S., Curnutte B., Pan K., Liu J., Ebraheim N.A. Biomechanical comparison of suture-button, bioabsorbable screw, and metal screw for ankle syndesmotic repair: a meta-analysis. Foot Ankle Surg. Feb 2021;27(2):117–122. doi: 10.1016/j.fas.2020.03.008. [DOI] [PubMed] [Google Scholar]
- 39.Lubberts B., Vopat B.G., Wolf J.C., Longo U.G., DiGiovanni C.W., Guss D. Arthroscopically measured syndesmotic stability after screw vs. suture button fixation in a cadaveric model. Injury. Nov 2017;48(11):2433–2437. doi: 10.1016/j.injury.2017.08.066. [DOI] [PubMed] [Google Scholar]
- 40.Meekaew P., Paholpak P., Wisanuyotin T., et al. Biomechanics comparison between endobutton fixation and syndesmotic screw fixation for syndesmotic injury ankle fracture; a finite element analysis and cadaveric validation study. J Orthop. Nov-Dec 2022;34:207–214. doi: 10.1016/j.jor.2022.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dziak J.J., Dierker L.C., Abar B. The interpretation of statistical power after the data have been gathered. Curr Psychol. Jun 2020;39(3):870–877. doi: 10.1007/s12144-018-0018-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search syntax used for each respective database and number of results.
Overview of Included Studies.