Abstract
Purpose
To (1) perform a systematic review of level I randomized controlled trials (RCTs) detailing the incidence of anterior knee pain and kneeling pain following anterior cruciate ligament reconstruction (ACLR) with bone–patellar tendon–bone (BPTB) autograft and (2) investigate the effect of bone grafting the patellar harvest site on anterior knee and kneeling pain.
Methods
A systematic review of level I studies from 1980 to 2023 was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The primary outcome evaluated was the presence of donor site morbidity in the form of anterior knee pain or kneeling pain. A secondary subanalysis was performed to assess for differences in the incidence of postoperative pain between patient groups undergoing ACLR with BPTB receiving harvest site bone grafting and those in whom the defect was left untreated.
Results
Following full-text review, 15 studies reporting on a total of 696 patients met final inclusion criteria. Patients were followed for an average of 4.78 years (range, 2.0-15.3), and the mean age ranged from 21.7 to 38 years old. The incidence of anterior knee pain, calculated from 354 patients across 10 studies, ranged from 5.4% to 48.4%. The incidence of postoperative pain with kneeling was determined to range from 4.0% to 75.6% in 490 patients from 9 studies. Patients treated with bone grafting of the BPTB harvest site had no significant difference in incidence of any knee pain compared with those who were not grafted, with incidences of 43.3% and 40.2%, respectively.
Conclusions
Based on the current level I RCT data, the incidences of anterior knee pain and kneeling pain following ACLR with BPTB autograft range from 5.4% to 48.4% and 4.0% to 75.6%, respectively.
Level of Evidence
Level I, systematic review of RCTs.
Anterior cruciate ligament (ACL) injuries are debilitating and comprise a large portion of all traumatic knee pathologies. Injury to this ligament can occur in both noncontact and contact settings and is especially prevalent in athletic populations.1 For those who undergo surgical intervention via ACL reconstruction (ACLR), postsurgical rehabilitation and other factors (e.g., graft type, graft fixation, surgical technique, and adherence to postoperative rehabilitation) impact long-term outcomes and overall patient satisfaction.2 Graft type is a heavily debated topic, as many surgeons argue that different graft types come with specific advantages and disadvantages. Regardless of anatomic source, several studies have demonstrated superior outcomes and significantly lower re-rupture rates following ACLR with autograft compared with allograft, especially in young athletes.3, 4, 5 Although bone–patellar tendon–bone (BPTB) autograft has been considered the gold standard graft, disadvantages include donor site morbidity, including anterior knee pain and pain with kneeling.6 The inclination to decrease donor site morbidity associated with BPTB autograft has prompted some surgeons to utilize other graft types for ACLR, such as quadriceps tendon (QT) autograft.7 Several previous studies have demonstrated similar outcomes, stability, and graft survival with decreased donor site morbidity when using QT autograft compared with BPTB and hamstring tendon autografts.8, 9, 10
There is large variability in the incidence of anterior knee pain and kneeling pain following ACLR with BPTB autograft. As other graft options gain popularity, acquiring an accurate incidence of graft type morbidity will be essential to compare graft options. The purpose of this study was to (1) perform a systematic review of level I randomized controlled trials (RCTs) detailing the incidence of anterior knee pain and kneeling pain following ACLR with BPTB autograft and (2) investigate the effect of bone grafting the patellar harvest site on anterior knee and kneeling pain. It was hypothesized that low rates of postoperative anterior knee pain and pain with kneeling would be reported following ACLR with BPTB and that bone grafting of the donor site would not improve the incidence of patient-reported knee pain postoperatively.
Methods
Study Inclusion
A systematic review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The search query was performed in February 2023 using the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, PubMed (1980-2023), Ovid MEDLINE (1980-2023), and Embase (1980-2023). The search terms utilized were “Anterior Cruciate Ligament” AND “Patellar Tendon” AND “Pain” AND “Randomized.”
Inclusion criteria were English language level I RCTs published between 1980 and 2023 reporting the incidence of anterior knee pain or kneeling pain in patients undergoing primary ACLR with BPTB autograft at minimum 2-year follow-up. The exclusion criteria were studies that included patients undergoing revision ACLR or those with multi-ligament knee injuries, cadaveric studies, diagnostic imaging studies, surgical technique studies, biomechanical studies, histological descriptions, case reports, and review articles. For studies reporting on double cohorts from the same senior author, only the most recent study with the longest available follow-up was included to increase the reliability of the aggregated data. Included articles were obtained following exclusion of duplicates, assessment of identified abstracts, and final review of full-text articles. Two investigators (L.A.P. and R.A.A.) independently reviewed abstracts from all identified articles. A third reviewer (Z.S.A.) was utilized to resolve any disagreements regarding inclusion criteria if needed. If necessary, full-text articles were obtained for review to allow for further application of inclusion and exclusion criteria. In addition, the reference lists from included studies were reviewed and reconciled to ensure that all eligible articles were included.
Data Collection
The primary outcome recorded was combined incidence of patient-reported anterior knee pain or kneeling pain following ACLR. The incidence of generalized, joint line, or hardware-related pain was not included in the primary outcome analysis. Secondary variables included bone grafting of the patellar harvest site, type of bone graft utilized, closure of the tendinous graft defect, and graft size. Patient demographics, graft harvesting and reconstruction technique, and rehabilitation protocols were also recorded and qualitatively reviewed.
Quality Assessment and Critical Appraisal
All included studies were reviewed by 2 authors (L.A.P. and R.A.A.) independently to evaluate for quality and risk of bias for controlled trials using the Grading of Recommendations Assessment, Development and Evaluation assessment methodology and the Jadad score.11, 12, 13 A Jadad score of 3 or higher is considered high-quality.
Statistical Analysis
Statistical analysis was performed using R software (R Foundation for Statistical Computing, Vienna, Austria). All studies were amenable to quantitative analysis. The total number of patients reporting anterior knee pain or kneeling pain was recorded for each study, and the incidence across the included studies was calculated as a proportion based on total patients reporting postoperative pain versus the total patient population. Statistical heterogeneity between trials was evaluated by the χ2 and I2 tests, with significance set at P < .01. Random effects and fixed effects models were used depending on the heterogeneity of the studies included. A subanalysis with χ2 and I2 tests was also performed to evaluate the pooled incidence of anterior knee pain or kneeling pain between patient groups undergoing ACLR with BPTB treated with harvest site bone grafting and those in whom the defect was left untreated. Incidence was reported as proportions with 95% confidence interval (CI).
Results
Study Demographics
The literature search identified 658 articles, and 15 studies met final inclusion criteria following full-text review (Fig 1). A total of 725 patients were included across the 15 studies, with 469 (64.6%) male patients, 206 (28.4%) female patients, and 50 (6.9%) patients for whom sex was not reported (Table 1). Patients were followed for an average of 4.78 years (range, 2.0-15.3), and the mean age across the included studies ranged from 21.7 to 38 years old. All included studies received a Jadad score of 3 or higher (range, 3-4); however, none of the studies were performed in a double-blinded fashion and thus were ineligible for a maximal score of 5 (Table 1). Because of the high degree of heterogeneity across studies (I2 > 75%), a formal meta-analysis was not performed to calculate pooled incidence of postoperative knee pain following ACLR with BPTB autograft.
Fig 1.
PRISMA flowchart based on study inclusion criteria. (PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.)
Table 1.
Study Demographics
| Study | Jadad score | Follow-up, years | N (male, female) | Mean age, years |
|---|---|---|---|---|
| Aglietti et al., 200424 | 4 | 2.00 | 60 (46, 14) | 25.0 |
| Aune et al., 200118 | 3 | 2.00 | 35 (19, 16) | 25.0 |
| Barenius et al., 201025 | 3 | 8.40 | 78 (38, 14) | 33.0 |
| Brandsson et al., 199819 | 4 | 2.00 | 60 (40, 20) | 28.0 |
| Drogset et al., 201014 | 4 | 2.00 | 50 (NR, NR) | 26.0 |
| Guglielmetti et al., 202120 | 3 | 2.00 | 31 (23, 8) | 25.2 |
| Gupta et al., 202026 | 4 | 2.00 | 80 (79, 1) | 25.0 |
| Ibrahim et al., 200521 | 3 | 6.75 | 40 (40, 0) | 22.3 |
| Matsumoto et al., 200615 | 3 | 7.25 | 37 (21, 16) | 23.7 |
| Mohtadi et al., 201927 | 4 | 5.00 | 103 (60, 43) | 33.8 |
| Sajovic et al., 201122 | 3 | 11.00 | 25 (16, 9) | 38.0 |
| Shaieb et al., 200223 | 3 | 2.75 | 33 (26, 7) | 32.0 |
| Taylor et al., 200928 | 4 | 2.70 | 32 (25, 7) | 21.7 |
| Webster et al., 201616 | 3 | 15.30 | 22 (16, 6) | 26.6 |
| Zaffagnini et al., 201117 | 4 | 8.60 | 39 (20, 19) | 26.0 |
NR, not reported.
Incidence of Anterior Knee Pain and Kneeling Pain
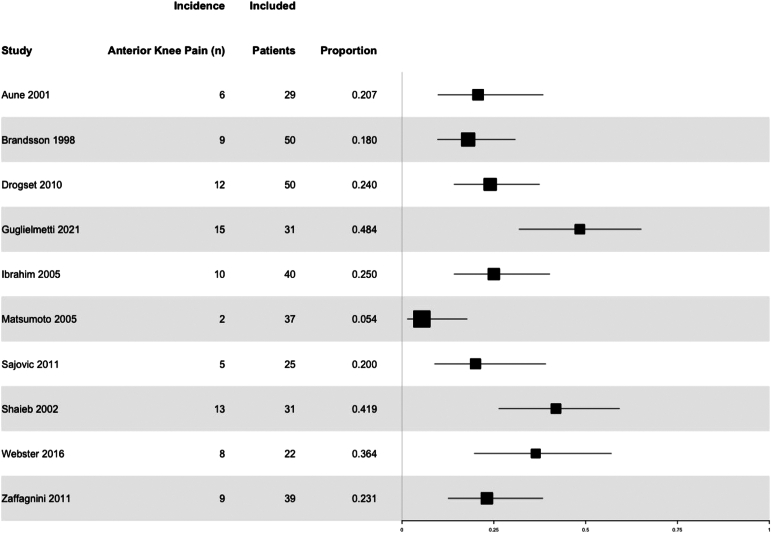
Four studies14, 15, 16, 17 reported both anterior knee pain and kneeling pain in patients undergoing ACLR with BPTB autograft, whereas 6 additional studies18, 19, 20, 21, 22, 23 reported only anterior knee pain and the remaining 5 studies24, 25, 26, 27, 28 reported only kneeling pain. The incidence of anterior knee pain, calculated from 354 patients across 10 studies,14, 15, 16, 17, 18, 19, 20, 21, 22, 23 ranged from 5.4% to 48.4% (Fig 2, Table 2). The incidence of postoperative pain with kneeling was determined to range from 4.0% to 75.6% in 490 patients from 9 studies (Fig 3, Table 2).14, 15, 16, 17,24, 25, 26, 27, 28 The incidence of patients reporting any knee pain, either anterior or kneeling pain, ranged from 9.7% to 86.4% across the 15 included studies (Fig 4).14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28
Fig 2.
Forest plot and 95% CIs for incidence of patients reporting anterior knee pain following ACLR with BPTB autograft. (ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone; CIs, confidence intervals.)
Table 2.
Incidence of Anterior Knee Pain and Pain With Kneeling by Study
| Study | Patients analyzed, N | Anterior knee pain, N | Anterior knee pain incidence, % | Kneeling pain, N | Kneeling pain incidence, % |
|---|---|---|---|---|---|
| Aglietti et al., 200424 | 60 | - | - | 37 | 61.7 |
| Aune et al., 200118 | 29 | 6 | 20.7 | - | - |
| Barenius et al., 201025 | 78 | - | - | 59 | 75.6 |
| Brandsson et al., 199819 | 50 | 9 | 18.0 | - | - |
| Drogset et al., 201014 | 50 | 12 | 24.0 | 2 | 4.0 |
| Guglielmetti et al., 202120 | 31 | 15 | 48.4 | - | - |
| Gupta et al., 202026 | 80 | - | - | 12 | 15.0 |
| Ibrahim et al., 200521 | 40 | 10 | 25.0 | - | - |
| Matsumoto et al., 200615 | 37 | 2 | 5.4 | 4 | 10.8 |
| Mohtadi et al., 201927 | 103 | - | - | 10 | 9.7 |
| Sajovic et al., 201122 | 25 | 5 | 20.0 | - | - |
| Shaieb et al., 200223 | 31 | 13 | 41.9 | - | - |
| Taylor et al., 200928 | 21 | - | - | 8 | 38.1 |
| Webster et al., 201616 | 22 | 8 | 36.4 | 11 | 50.0 |
| Zaffagnini et al., 201117 | 39 | 9 | 23.1 | 18 | 72.0 |
Fig 3.
Forest plot and 95% CIs for incidence of patients reporting kneeling pain following ACLR with BPTB autograft. (ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone; CIs, confidence intervals.)
Fig 4.
Forest plot and 95% CIs for incidence of patients reporting any knee pain, either anterior or kneeling pain, following ACLR with BPTB autograft. (ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone; CIs, confidence intervals.)
Effects of Bone Grafting at Patellar Harvest Site
With regard to the subgroup analysis assessing the impact of BPTB harvest site bone grafting on postoperative pain (anterior or kneeling) incidence, 9 studies15,16,19,23,24,27, 28, 29, 30 specified their approach to donor site management. Of these, 5 studies16,17,22,23,28 (138 patients) reported bone grafting of the BPTB harvest site and 4 studies15,19,24,27 (250 patients) elected to leave the defect unaddressed. Although none of the 5 studies performed formal bone grafting of the donor sites on the patella and tibial tubercle, all reported using bone fragments from BPTB graft preparation and tunnel drilling to fill the patellar and tibial tubercle defects.16,17,22,23,28 Patients who underwent donor site bone grafting had a similar incidence of postoperative pain (43.3%, 95% CI, 18.4% to 69.9%) as those who did not (40.2%, 95% CI, 11.6% to 72.9%) (Fig 5).
Fig 5.
Forest plot and 95% CIs for incidence of any reported knee pain in patients who received bone grafting of the harvest site versus those who did not following ACLR with BPTB autograft. (ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone; CIs, confidence intervals.)
Discussion
The most important finding of this systematic review is that the expected incidences of anterior knee pain and kneeling pain following ACLR with BPTB autograft ranged from 5.4% to 48.4% and 4.0% to 75.6%, respectively. Second, patients treated with bone grafting of the BPTB harvest site had no significant difference in the incidence of any knee pain compared with those who were not grafted. Although the risk of knee pain following ACLR with BPTB autograft has been well documented in the literature, no prior studies have reported the incidence of this complication based on an in-depth analysis of pooled data from level I RCTs.31, 32, 33, 34, 35
Although BPTB autograft remains the gold standard graft choice for ACLR, the information from this study will allow surgeons to more accurately explain to patients what to expect in terms of postoperative knee and kneeling pain. It is thought that donor site morbidity associated with BPTB graft harvest is one of the primary factors contributing to anterior knee pain in patients following this procedure. When a patellar tendon defect is created with the removal of the central third of the tendon, complete closure of the defect may potentially cause inferior translation of the patella (patella baja) and may consequently lead to increased sensitivity or pain when kneeling or squatting. This may be avoided by avoiding complete closure of the tendon and closing the paratenon instead. Additionally, the central incision required for harvest of the patellar tendon graft can potentially injure the infrapatellar branch of the saphenous nerve. This is another factor that may contribute to a higher prevalence of anterior knee pain in patients treated with BPTB autograft compared with other graft options.36 Although BPTB allografts avoid the risk of donor site morbidity and are associated with lower rates of anterior knee pain postoperatively, autograft is still preferred for ACLR, particularly in younger patients, given its superior clinical outcomes and 3-fold lower re-rupture rates.5
When considering the expected incidence of postoperative knee pain associated with BPTB autograft, there is great variability across the current literature, and thus it is imperative to assess high-quality RCTs for the most reliable data and estimated rates of occurrence. Even within this review of 15 level I RCTs, reported rates of anterior knee pain and kneeling pain were heterogeneous across the included studies. Matsumoto et al.15 found only 5.4% (2 of 37) of patients experienced anterior pain over the graft harvest site at a mean follow-up of 7 years, whereas Guglielmetti et al.20 reported anterior pain in 48.4% (15 of 31) of patients at 2-year follow-up. It is possible that these discrepancies are attributable to the duration of follow-up in the selected studies, as patients may experience decreasing levels of anterior knee pain and sensitivity over the graft harvest site with time. Similarly, rates of kneeling pain varied considerably, as Drogset et al.14 reported an incidence of only 4.0% (2 of 50) at 2 years versus an incidence of 75.6% (59 of 78) at 8-year follow-up in a study by Barenius et al.25 The cause of these discrepancies in rates of postoperative pain is likely multifactorial, although they may be related to factors such as patient age and level of activity, concomitant soft tissue injuries, graft harvest approach, or bone grafting at the BPTB graft harvest site. The heterogeneous questioning methods used to assess for the presence and degree of postoperative pain (e.g., “do you have pain today?” vs “does the pain limit daily activities?”) likely confound these differences in incidences across the included studies.
As QT autografts have become an increasingly attractive option for ACLR, it is important to directly compare the associated complication rates with those of the current gold standard, BPTB autografts.10,32,37,38 Although there remains a paucity of literature reporting on pooled RCT data for complication rates observed with QT versus BPTB autografts, more recent reviews suggest that QT grafts are associated with a lower incidence of donor site morbidity and anterior knee pain postoperatively.32,39,40 These reduced rates of anterior knee pain support the hypothesis that QT autograft may be a more appropriate option for patients who have occupations requiring them to squat and kneel repetitively (e.g., carpenters, painters, plumbers) or patients who pray on their knees daily.5,41 It is important to note that the anterior knee pain experienced by patients following ACLR with BPTB is rarely debilitating and that this increased risk should not be the sole determinant of graft choice in most patient populations.42 Future studies should aim to directly compare the incidence of anterior knee pain and kneeling pain between QT and BPTB autografts.
Regarding management of patellar bone defects following BPTB graft harvest, there remains a lack of consensus on whether the donor site should be grafted or left untreated. Based on odds ratio calculations and χ2 analysis, patients included in this review treated with bone grafting of the BPTB harvest site reported no differences in the incidence of donor site pain at final follow-up compared with those left untreated. These results are in agreement with previous studies reporting no difference in outcomes or postoperative pain when grafting the patellar defect.19
Limitations
The limitations of this study should be noted. There was clinical heterogeneity in patient populations with respect to patient demographics, length of follow-up, and concomitant meniscal pathology. There were also differences across the included studies in questioning methods used to assess for the presence and degree of postoperative pain, which likely increased the variability of reported incidences included in the final analysis. Although patients were randomized in their respective level I studies, no randomization was performed for the present meta-analysis. Given the limited pool of level I RCT data reporting on knee pain following ACLR with BPTB and the heterogeneity in reported incidences, the present findings may be underpowered relative to larger national databases. Finally, there was considerable variability in the duration of follow-up across the included studies, which may limit the generalizability of the pooled quantitative analyses.
Conclusions
Based on the current level I RCT data, the incidences of anterior knee pain and kneeling pain following ACLR with BPTB autograft range from 5.4% to 48.4% and 4.0% to 75.6%, respectively.
Disclosures
The authors report the following potential conflicts of interest or sources of funding: A.J.S. declares he is a paid consultant for Mitek and owns stock or stock options in Zimmer Biomet, ConMed Linvatec, Johnson & Johnson, Pfizer, Smith & Nephew, and Stryker. M.K.M. declares she is a board or committee member of the American Academy of Orthopaedic Surgeons, American Orthopaedic Association, American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America, Ruth Jackson Orthopaedic Society, and The Forum; is on the editorial or governing board of Journal of Bone & Joint Surgery, American Journal of Sports Medicine Electronic Media, Arthroscopy, and OrthoInfo; and is a paid presenter or speaker for Arthrex.
Supplementary Data
References
- 1.Hootman J.M., Dick R., Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42:311–319. [PMC free article] [PubMed] [Google Scholar]
- 2.Dodwell E.R., Lamont L.E., Green D.W., et al. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42:675–680. doi: 10.1177/0363546513518412. [DOI] [PubMed] [Google Scholar]
- 3.Kaeding C.C., Aros B., Pedroza A., et al. Allograft versus autograft anterior cruciate ligament reconstruction: Predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kane P.W., Wascher J., Dodson C.C., et al. Anterior cruciate ligament reconstruction with bone–patellar tendon–bone autograft versus allograft in skeletally mature patients aged 25 years or younger. Knee Surg Sports Traumatol Arthrosc. 2016;24:3627–3633. doi: 10.1007/s00167-016-4213-z. [DOI] [PubMed] [Google Scholar]
- 5.Kraeutler M.J., Bravman J.T., McCarty E.C. Bone–patellar tendon–bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: A meta-analysis of 5182 patients. Am J Sports Med. 2013;41:2439–2448. doi: 10.1177/0363546513484127. [DOI] [PubMed] [Google Scholar]
- 6.Kraeutler M.J., Wolsky R.M., Vidal A.F., Bravman J.T. Anatomy and biomechanics of the native and reconstructed anterior cruciate ligament: Surgical implications. J Bone Joint Surg Am. 2017;99:438–445. doi: 10.2106/JBJS.16.00754. [DOI] [PubMed] [Google Scholar]
- 7.Freedman K.B., D’Amato M.J., Nedeff D.D., Kaz A., Bach B.R., Jr. Arthroscopic anterior cruciate ligament reconstruction: A metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2–11. doi: 10.1177/03635465030310011501. [DOI] [PubMed] [Google Scholar]
- 8.Dai W., Leng X., Wang J., et al. Quadriceps tendon autograft versus bone–patellar tendon–bone and hamstring tendon autografts for anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Am J Sports Med. 2022;50:3425–3439. doi: 10.1177/03635465211030259. [DOI] [PubMed] [Google Scholar]
- 9.Mulford J.S., Hutchinson S.E., Hang J.R. Outcomes for primary anterior cruciate reconstruction with the quadriceps autograft: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:1882–1888. doi: 10.1007/s00167-012-2212-2. [DOI] [PubMed] [Google Scholar]
- 10.Belk J.W., Kraeutler M.J., Marshall H.A., Goodrich J.A., McCarty E.C. Quadriceps tendon autograft for primary anterior cruciate ligament reconstruction: A systematic review of comparative studies with minimum 2-year follow-up. Arthroscopy. 2018;34:1699–1707. doi: 10.1016/j.arthro.2018.01.047. [DOI] [PubMed] [Google Scholar]
- 11.Jadad A.R., Moore R.A., Carroll D., et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 12.Phi L., Ajaj R., Ramchandani M.H., et al. Expanding the grading of recommendations assessment, development, and evaluation (Ex-GRADE) for evidence-based clinical recommendations: Validation study. Open Dent J. 2012;6:31–40. doi: 10.2174/1874210601206010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atkins D., Best D., Briss P.A., et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drogset J.O., Strand T., Uppheim G., et al. Autologous patellar tendon and quadrupled hamstring grafts in anterior cruciate ligament reconstruction: A prospective randomized multicenter review of different fixation methods. Knee Surg Sports Traumatol Arthrosc. 2010;18:1085–1093. doi: 10.1007/s00167-009-0996-5. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto A., Yoshiya S., Muratsu H., et al. A comparison of bone–patellar tendon–bone and bone–hamstring tendon–bone autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:213–219. doi: 10.1177/0363546505279919. [DOI] [PubMed] [Google Scholar]
- 16.Webster K.E., Feller J.A., Hartnett N., Leigh W.B., Richmond A.K. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: A 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44:83–90. doi: 10.1177/0363546515611886. [DOI] [PubMed] [Google Scholar]
- 17.Zaffagnini S., Bruni D., Marcheggiani Muccioli G.M., et al. Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: A prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc. 2011;19:390–397. doi: 10.1007/s00167-010-1225-y. [DOI] [PubMed] [Google Scholar]
- 18.Aune A.K., Holm I., Risberg M.A., Jensen H.K., Steen H. Four-strand hamstring tendon autograft compared with patellar tendon–bone autograft for anterior cruciate ligament reconstruction. A randomized study with two-year follow-up. Am J Sports Med. 2001;29:722–728. doi: 10.1177/03635465010290060901. [DOI] [PubMed] [Google Scholar]
- 19.Brandsson S., Faxen E., Eriksson B.I., et al. Closing patellar tendon defects after anterior cruciate ligament reconstruction: Absence of any benefit. Knee Surg Sports Traumatol Arthrosc. 1998;6:82–87. doi: 10.1007/s001670050077. [DOI] [PubMed] [Google Scholar]
- 20.Guglielmetti L.G.B., Salas V.E.R., Jorge P.B., et al. Prospective and randomized clinical evaluation of hamstring versus patellar tendon autograft for anterior cruciate ligament reconstruction in soccer players. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211028168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ibrahim S.A., Al-Kussary I.M., Al-Misfer A.R., et al. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: Patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy. 2005;21:412–417. doi: 10.1016/j.arthro.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Sajovic M., Strahovnik A., Dernovsek M.Z., Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: An 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39:2161–2169. doi: 10.1177/0363546511411702. [DOI] [PubMed] [Google Scholar]
- 23.Shaieb M.D., Kan D.M., Chang S.K., Marumoto J.M., Richardson A.B. A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:214–220. doi: 10.1177/03635465020300021201. [DOI] [PubMed] [Google Scholar]
- 24.Aglietti P., Giron F., Buzzi R., Biddau F., Sasso F. Anterior cruciate ligament reconstruction: Bone–patellar tendon–bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86:2143–2155. [PubMed] [Google Scholar]
- 25.Barenius B., Nordlander M., Ponzer S., Tidermark J., Eriksson K. Quality of life and clinical outcome after anterior cruciate ligament reconstruction using patellar tendon graft or quadrupled semitendinosus graft: An 8-year follow-up of a randomized controlled trial. Am J Sports Med. 2010;38:1533–1541. doi: 10.1177/0363546510369549. [DOI] [PubMed] [Google Scholar]
- 26.Gupta R., Kapoor A., Soni A., et al. No difference in outcome of anterior cruciate ligament reconstruction with “bone–patellar tendon–bone versus semitendinosus–gracilis graft with preserved insertion”: A randomized clinical trial. Indian J Orthop. 2020;54:665–671. doi: 10.1007/s43465-020-00073-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mohtadi N.G., Chan D.S. A randomized clinical trial comparing patellar tendon, hamstring tendon, and double-bundle ACL reconstructions: Patient-reported and clinical outcomes at 5-year follow-up. J Bone Joint Surg Am. 2019;101:949–960. doi: 10.2106/JBJS.18.01322. [DOI] [PubMed] [Google Scholar]
- 28.Taylor D.C., DeBerardino T.M., Nelson B.J., et al. Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction: A randomized controlled trial using similar femoral and tibial fixation methods. Am J Sports Med. 2009;37:1946–1957. doi: 10.1177/0363546509339577. [DOI] [PubMed] [Google Scholar]
- 29.Feller J.A., Webster K.E. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:564–573. doi: 10.1177/03635465030310041501. [DOI] [PubMed] [Google Scholar]
- 30.Sajovic M., Vengust V., Komadina R., Tavcar R., Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: Five-year follow-up. Am J Sports Med. 2006;34:1933–1940. doi: 10.1177/0363546506290726. [DOI] [PubMed] [Google Scholar]
- 31.Slone H.S., Romine S.E., Premkumar A., Xerogeanes J.W. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: A comprehensive review of current literature and systematic review of clinical results. Arthroscopy. 2015;31:541–554. doi: 10.1016/j.arthro.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 32.Mouarbes D., Menetrey J., Marot V., et al. Anterior cruciate ligament reconstruction: A systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone–patellar tendon–bone and hamstring–tendon autografts. Am J Sports Med. 2019;47:3531–3540. doi: 10.1177/0363546518825340. [DOI] [PubMed] [Google Scholar]
- 33.Poehling-Monaghan K.L., Salem H., Ross K.E., et al. Long-term outcomes in anterior cruciate ligament reconstruction: A systematic review of patellar tendon versus hamstring autografts. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117709735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spindler K.P., Kuhn J.E., Freedman K.B., et al. Anterior cruciate ligament reconstruction autograft choice: Bone–tendon–bone versus hamstring: Does it really matter? A systematic review. Am J Sports Med. 2004;32:1986–1995. doi: 10.1177/0363546504271211. [DOI] [PubMed] [Google Scholar]
- 35.Li S., Su W., Zhao J., et al. A meta-analysis of hamstring autografts versus bone–patellar tendon–bone autografts for reconstruction of the anterior cruciate ligament. Knee. 2011;18:287–293. doi: 10.1016/j.knee.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 36.Kartus J., Ejerhed L., Sernert N., Brandsson S., Karlsson J. Comparison of traditional and subcutaneous patellar tendon harvest. A prospective study of donor site-related problems after anterior cruciate ligament reconstruction using different graft harvesting techniques. Am J Sports Med. 2000;28:328–335. doi: 10.1177/03635465000280030801. [DOI] [PubMed] [Google Scholar]
- 37.Lubowitz J.H. Editorial commentary: Quadriceps tendon autograft use for anterior cruciate ligament reconstruction predicted to increase. Arthroscopy. 2016;32:76–77. doi: 10.1016/j.arthro.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 38.Middleton K.K., Hamilton T., Irrgang J.J., et al. Anatomic anterior cruciate ligament (ACL) reconstruction: A global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc. 2014;22:1467–1482. doi: 10.1007/s00167-014-2846-3. [DOI] [PubMed] [Google Scholar]
- 39.Mouarbes D., Dagneaux L., Olivier M., et al. Lower donor-site morbidity using QT autografts for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28:2558–2566. doi: 10.1007/s00167-020-05873-1. [DOI] [PubMed] [Google Scholar]
- 40.Cohen D., Slawaska-Eng D., Almasri M., Sheean A., de Sa D. Quadricep ACL reconstruction techniques and outcomes: An updated scoping review of the quadricep tendon. Curr Rev Musculoskelet Med. 2021;14:462–474. doi: 10.1007/s12178-021-09726-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hurley E.T., Calvo-Gurry M., Withers D., et al. Quadriceps tendon autograft in anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2018;34:1690–1698. doi: 10.1016/j.arthro.2018.01.046. [DOI] [PubMed] [Google Scholar]
- 42.Brown D.W., Curry C.M., Ruterbories L.M., Avery F.L., Anson P.S. Evaluation of pain after arthroscopically assisted anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25:182–186. doi: 10.1177/036354659702500207. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.