Abstract
Background
The number of paediatric patients visiting the ED with non-urgent problems is increasing, leading to poor patient flow and ED crowding. Fast track aims to improve the efficiency of evaluation and discharge of low acuity patients. We aimed to identify which febrile children are suitable for a fast track based on presenting symptoms and management.
Methods
This study is part of the Management and Outcome of Fever in children in Europe study, which is an observational study including routine data of febrile children <18 years attending 12 European EDs. We included febrile, low urgent children (those assigned a triage acuity of either ‘standard’ or ‘non-urgent’ using the Manchester Triage System) and defined children as suitable for fast track when they have minimal resource use and are discharged home. Presenting symptoms consisted of neurological (n=237), respiratory (n=8476), gastrointestinal (n=1953) and others (n=3473, reference group). Multivariable logistic regression analyses regarding presenting symptoms and management (laboratory blood testing, imaging and admission) were performed with adjustment for covariates: patient characteristics, referral status, previous medical care, previous antibiotic use, visiting hours and ED setting.
Results
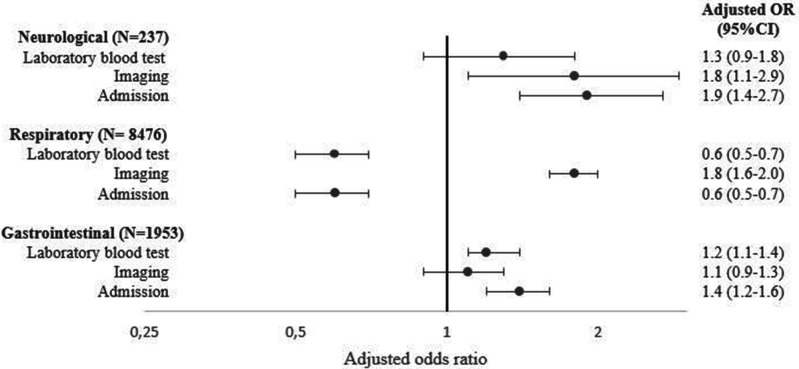
We included 14 139 children with a median age of 2.7 years (IQR 1.3–5.2). The majority had respiratory symptoms (60%), viral infections (50%) and consisted of self-referrals (69%). The neurological group received imaging more often (adjusted OR (aOR) 1.8, 95% CI 1.1 to 2.9) and were admitted more frequently (aOR 1.9, 95% CI 1.4 to 2.7). The respiratory group had fewer laboratory blood tests performed (aOR 0.6, 95% CI 0.5 to 0.7), were less frequently admitted (aOR 0.6, 95% CI 0.5 to 0.7), but received imaging more often (aOR 1.8, 95% CI 1.6 to 2.0). Lastly, the gastrointestinal group had more laboratory blood tests performed (aOR 1.2. 95% CI 1.1 to 1.4) and were admitted more frequently (aOR 1.4, 95% CI 1.2 to 1.6).
Conclusion
We determined that febrile children triaged as low urgent with respiratory symptoms were most suitable for a fast track. This study provides evidence for which children could be triaged to a fast track, potentially improving overall patient flow at the ED.
Keywords: triage, emergency department, pediatrics
WHAT IS ALREADY KNOWN ON THIS TOPIC
Poor patient flow and crowding are major issues at the ED.
A fast track intervention for patients with non-urgent problems improves patient flow at the ED and is a promising intervention to reduce length of stay and has been found to increase patient satisfaction.
WHAT THIS STUDY ADDS
In a multicentre observational study in Europe, we determined that among febrile children triaged as low urgent, those with respiratory symptoms were most suitable for a fast track.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This study provides evidence for which children could be triaged to a fast track, potentially improving overall patient flow at the ED.
Introduction
The number of paediatric attendances to the ED with non-urgent problems is increasing in Europe, leading to poor patient flow and crowding.1 2 Non-urgent patients visiting the ED leads to more resource use, higher medical costs and higher work pressure for healthcare workers. A fast track intervention to improve patient flow at the ED is a promising intervention to reduce length of stay at the ED and has been found to increase patient satisfaction.3–9
A fast track is a separate healthcare pathway for the assessment and treatment of patients who need a lower level of care in a dedicated area near the ED,4 10 11 allowing more effective management of patients with non-urgent problems.12 In order to implement a fast track for non-urgent patients, an absolute requirement is having a reliable triage system. Triage at the ED is used to prioritise patients based on their clinical urgency and to ensure that patients are seen in order of clinical priority rather than in order of attendance.13 It can therefore be used to identify patients with less urgent problems who can safely wait longer until doctors’ assessment at the ED or who can be seen by another caregiver such as a general practitioner or nurse (practitioner).
The Manchester Triage System (MTS) is the most commonly used triage system in Europe; it categorises patients into one of five triage categories based on presenting symptoms.14 According to a prospective observational study in two paediatric emergency care settings, MTS can safely identify less urgent patients. Fever is one of the most common presenting symptoms in children visiting the ED, accounting for 20% of all paediatric ED visits.15 Therefore, implementing a fast track for febrile children may have large impact on patient flow by shortening the length of stay and waiting time at the ED.
The aim of our study is to determine which low urgent febrile children triaged by MTS as low urgency are suitable for assessment in a fast track. This approach is based on objective classification by the MTS and differs from forms of streaming where patients are directed to a healthcare provider after brief clinical assessment or telephone contact.16 Identifying febrile children suitable for a fast track may allow them to be treated in a lower resource setting, shortening their stay and potentially improving patient flow in the rest of the ED.
Methods
Study design
This is a secondary analysis of the Management and Outcome of Fever in children in Europe (MOFICHE) study, which is embedded in the Personalised Risk assessment in Febrile illness to Optimise Real-life Management across the European Union project.17 18 The MOFICHE study is an observational multicentre study assessing management and outcome of febrile children using routinely collected data of 12 EDs in 8 European countries (Austria, Germany, Greece, Latvia, the Netherlands n=3, Slovenia, Spain, the UK n=3). The hospital characteristics are described in previous studies.18 19
Study population and setting
Children up to 18 years with fever (temperature ≥38℃) measured at the ED or a history of fever within 3 days before the ED visit were included in the MOFICHE study. For this secondary analysis, we included the nine EDs who use the MTS for allocating triage urgency levels to patients, namely EDs in Austria, Germany, Latvia, the Netherlands (n=2), Spain, and the UK (n=3). Subsequently, from these EDs we included children who were triaged as low urgent (those assigned a triage acuity of either ‘standard’ or ‘non-urgent’ using the MTS) since we hypothesise that a proportion of these children are suitable for assessment in a fast track. Children with known comorbidities and with missing data on disposition were excluded.
Patient and public involvement
Patients and public were not involved in the design and conduct of the study.
Triage urgency level
The MTS consists of 52 flow charts based on the patients’ presenting problem such as abdominal pain.13 14 The most appropriate flow chart is chosen by triage nurses to prioritise patients on clinical urgency. Each flow chart consists of specific discriminators and categorises patients in one of the five triage categories, which are linked to a maximum waiting time for doctors’ assessment. The five MTS urgency categories are: immediate (maximum waiting time 0 min), very urgent (maximum waiting time 10 min), urgent (maximum waiting time 60 min), standard (maximum waiting time 120 min), non-urgent (maximum waiting time 240 min). For this study, we used predefined three-category triage levels consisting of the categories ‘high urgent’, ‘intermediate urgent’ and ‘low urgent’.20 The MTS categories very urgent and immediate were classified as high urgent, urgent was classified as intermediate urgent and patients allocated to standard or non-urgent were classified as low urgent.
Data collection
Data were routinely collected from electronic health records for at least 1 year during the MOFICHE study period from January 2017 to April 2018. Period of active data collection per month differed in the participating hospitals ranging from 1 week per month to the entire month. Characteristics of the participating hospitals are shown in online supplemental appendix A. Data collected included patient characteristics (age, gender, presenting symptoms, comorbidity (chronic condition expected to last at least 1 year21), referral status, triage urgency, visiting hours, previous medical care, previous antibiotic use, vital signs (HR, RR, oxygen saturation, temperature), diagnostic tests performed in the ED (laboratory blood testing, imaging), antibiotic prescription (at the ED or first day of admission) and disposition. Presenting symptoms were categorised into four groups: neurological (febrile convulsions, meningeal signs or focal neurological signs), respiratory (runny nose, sore throat or coughing), gastrointestinal (diarrhoea or vomiting) and other (eg, rash, urogenital symptoms) presenting symptoms. Referral status was dichotomised into self-referred and referred (referral by general practitioner or other hospital or emergency medical services). Previous medical care was defined as a visit to a healthcare setting (general practitioner or ED) in the previous 5 days, and previous antibiotic use was defined as therapeutic antibiotic use in the last 7 days. Visiting hours were categorised as office hours and out-of-office hours, with out-of-office hours defined as ED attendances in weekends or between 17:00 hours and 08:00 hours on weekdays. Tachypnoea and tachycardia were defined according to age-specific cut-off values as described in APLS guidelines.22 The focus of infection and cause of infection were retrospectively assigned by the local research teams. The focus of infection was categorised into respiratory tract, gastrointestinal tract, urinary tract, childhood exanthema/flu-like illness, soft tissue/skin/musculoskeletal, sepsis/meningitis and other (eg, undifferentiated fever). The cause of infection was determined using a previously published phenotyping algorithm, which combines clinical symptoms and diagnostic results.18 Patients were categorised as presumed bacterial, presumed viral, unknown bacterial/viral or other (eg, inflammatory illness). Children with a mixed bacterial and viral infection were classified as bacterial (online supplemental appendix B).
emermed-2023-213375supp001.pdf (408.1KB, pdf)
Outcome measures
We defined children suitable for a fast track when resource use at the ED is minimal and when there is no need for admission. This definition was based on previous literature and on expert opinions of the research group including paediatricians.5 11 Resource use included laboratory blood testing and imaging performed at the ED. Laboratory blood tests included markers of infection; C reactive protein (CRP), procalcitonin and white blood cell (WBC) count. Imaging included X-ray, ultrasound, MRI scan and CT scan. We defined children with laboratory blood testing, any kind of imaging or being admitted as not suitable for a fast track.
Data analysis
Descriptive statistics were used for patient characteristics and management. We performed univariable and multivariable logistic regression analyses for the association between presenting symptoms and laboratory blood testing, imaging and admission. We adjusted the analyses for the confounders of age, sex, referral status, previous medical care, previous antibiotic use, visiting hours and ED setting. Additionally, we stratified the analysis for ED settings with low (22%–57%) and high (65%–89%) prevalence of low urgent triaged children during the study period. Subgroup analysis describing frequency of patient management stratified by age groups were performed when relevant for a fast track. We used multiple imputation with the MICE package in R for missing data on clinical covariates. Data were analysed using SPSS software V.25.0 and a p value <0.05 was considered statistically significant.
Results
Patient population and characteristics
A total of 29 588 febrile children attended the 9 European EDs, of which 16 683 (56%) were triaged as low urgent. The proportion of low urgent triaged children ranged from 22% to 73% across the EDs, and the three triage urgency categories per ED setting are shown in online supplemental appendix C. After excluding children with comorbidity (14%) and missing data on disposition (0.1%), the population for analyses consisted of 14 139 children. Table 1 describes the patient characteristics of the study population with a median age of 2.7 years (IQR 1.3–5.2) and 54% being boys. Most of the ED attendances were during out-of-office hours (70%) and the majority consisted of self-referrals (68%). Respiratory symptoms were the most common presenting symptom (60%), whereas neurological symptoms were least common (2%). Abnormal vital signs varied from 0.6% to 14% and the median duration of fever was 1.5 days. Patient characteristics per presenting symptom group are shown in online supplemental appendix D. The percentage of self-referrals was the lowest in the neurological group and all other characteristics were comparable between the presenting symptom groups.
Table 1.
Patient characteristics (n=14 139)
| Low triaged febrile children N=14 139 |
Missing (%) | |
| Age* (years) | 2.7 (1.3–5.2) | |
| Gender (boys) | 7613 (54) | |
| Visit hours (out of office) | 9852 (70) | |
| Referral (self-referred) | 9630 (68) | 556 (4) |
| Previous medical care | 3381 (24) | 671 (5) |
| Previous antibiotic treatment | 1486 (11) | 294 (2) |
| Presenting symptoms | ||
| Neurological | 237 (2)† | |
| Respiratory | 8476 (60) | |
| Gastrointestinal | 1953 (14) | |
| Other | 3473 (25) | |
| Ill appearance | 1653 (12) | 514 (4) |
| Vital signs | ||
| Tachycardia | 2019 (14) | 1317 (9) |
| Tachypnoea | 1346 (10) | 2465 (17) |
| Hypoxia | 78 (0.6) | 2788 (20) |
| Duration of fever (days)* | 1.5 (0.5–3) | 1067 (8) |
Absolute numbers and percentages (%) are given.
*Median and (IQR 25–75).
†87% status after febrile convulsion.
Management and diagnosis
Table 2 depicts the management, focus of infection and the presumed cause of infection of our study population. Laboratory blood tests were performed in 34% of the visits, of which CRP and WBC count were most frequently performed (33%). Thirteen per cent received any kind of imaging, 13% were admitted and 31% received antibiotic treatment. The majority had a respiratory focus of infection (69%) and a presumed viral infection (50%).
Table 2.
Management and working diagnosis
| Low triaged febrile children N=14 139 |
|
| Laboratory blood tests | 4740 (34) |
| CRP | 4659 (33) |
| PCT | 252 (2) |
| WBC | 4665 (33) |
| Imaging | 1864 (13) |
| X-ray | 1603 (11) |
| Ultrasound | 338 (2) |
| CT scan | 40 (0.3) |
| MRI scan | 18 (0.1) |
| Admission | 1840 (13) |
| Left without being seen | 70 (0.5) |
| Antibiotic treatment | 4395 (31) |
| Focus of infection | |
| Respiratory | 9702 (69) |
| Gastrointestinal | 1317 (9) |
| Urinary | 374 (3) |
| Childhood exanthema/flu-like illness | 746 (5) |
| Soft tissue/Skin/Musculoskeletal | 382 (3) |
| Sepsis/Meningitis | 21 (0.1) |
| Other | 1596 (11) |
| Cause of infection | |
| Presumed bacterial | 3375 (24) |
| Unknown bacterial/viral | 2348 (17) |
| Presumed viral | 7034 (50) |
| Other | 1194 (8) |
Absolute numbers and percentages (%) are given.
CRP, C reactive protein; PCT, procalcitonin; WBC, white blood cell.
Association between presenting symptoms and management
Management stratified by presenting symptom group is shown in table 3. Imaging was most frequently performed in the respiratory group (15%), while laboratory blood tests were most often performed in the other presenting symptoms groups (41%), and children with neurological symptoms were most often admitted (27%). The association between presenting symptoms and management after adjustment for confounders is shown in the forest plot (figure 1). The neurological group received imaging more often (aOR 1.8, 95% CI 1.1 to 2.9) and were admitted more frequently (aOR 1.9, 95% CI 1.4 to 2.7). The respiratory group had fewer laboratory blood tests performed (aOR 0.6, 95% CI 0.5 to 0.7), were less frequently admitted (aOR 0.6, 95% CI 0.5 to 0.7), but received imaging more often (aOR 1.8, 95% CI 1.6 to 2.0). Lastly, the gastrointestinal group had more laboratory test performed (aOR 1.2. 95% CI 1.1 to 1.4) and were admitted more frequently (aOR 1.4, 95% CI 1.2 to 1.6). Unadjusted ORs are shown in online supplemental appendix E. Stratifying ED settings by low (4 EDs) and high (5 EDs) prevalence of low urgent triaged children showed the same trend, which is shown in online supplemental appendix F.
Table 3.
Management per presenting symptom group
| Neurological N=237 |
Respiratory N=8476 |
Gastrointestinal N=1953 |
Other N=3473 |
|
| Laboratory blood test | 65 (28) | 2473 (29) | 777 (40) | 1425 (41) |
| Imaging | 24 (10) | 1269 (15) | 196 (10) | 375 (11) |
| Admission | 65 (27) | 808 (10) | 390 (20) | 577 (17) |
Absolute numbers and percentages (%) are given.
Figure 1.
Association between presenting symptoms and management. Other presenting symptoms group as reference group. Adjusted for age, gender, referral status, previous medical care, previous antibiotic use, visiting hours, ED setting.
Additionally, we performed a subgroup analysis stratified for age groups in the respiratory group since they had less laboratory blood testing and were less frequently admitted, and therefore might be suitable for a fast track. Four age groups were created: <2 years, 2<5 years, 5<12 years, 12<18 years. The oldest children had most extensive management with 43% receiving laboratory blood testing, 24% receiving imaging and 15% being admitted (table 4).
Table 4.
Management in the respiratory subgroup stratified by age groups (n=8476)
| <2 years (n=3263) | 2<5 years (n=3130) | 5<12 years (n=1648) | 12<18 years (n=435) | |
| Laboratory blood testing | 878 (27) | 923 (30) | 485 (29) | 187 (43) |
| Imaging | 412 (13) | 525 (17) | 228 (14) | 104 (24) |
| Admission | 369 (11) | 266 (9) | 106 (6) | 67 (15) |
Absolute numbers and percentages (%) are given.
Discussion
More than half (56%) of febrile children attending European EDs are triaged as low urgent, with the majority of this group presenting with respiratory symptoms (60%). Most of the children had the respiratory tract as focus of infection and half of them a presumed viral infection, which is usually self-limiting.23 Children with respiratory symptoms had less laboratory blood testing and were less frequently admitted than children in the other presenting symptoms group, although children with respiratory symptoms received more imaging. Most of the imaging performed in this respiratory group were chest X-rays (93%). However, routine chest X-rays are no longer recommended to distinguish between bacterial and viral cases, and treatment decisions are according to the guidelines based on clinical findings.24 Moreover, we found that older children with respiratory symptoms had a higher rate of diagnostic tests and 15% required admission. Therefore, we suggest that febrile children with respiratory symptoms are most suitable for a fast track with older children (>12 years) being less suitable since they receive more extensive management than younger children. We deemed children in the neurological group and gastrointestinal group unsuitable for a fast track since they received more laboratory blood testing or imaging and were admitted more frequently compared with the other presenting symptoms group. Previous studies examining the implementation of a fast track at paediatric EDs showed reduced arrival-to-triage times and decreased length of stay of lower acuity patients treated in these units.5 25 However, these studies involved broad paediatric ED populations and did not examine subgroups such as children presenting with fever separately.
Strengths and limitations
The main strength of this study is the use of data from a large cohort of febrile children visiting European EDs increasing generalisability of findings. Additionally, data collection in MOFICHE was extensive, which made it possible to assess management performed in four presenting symptom subgroups to determine which children are most suitable for a fast track. However, several limitations should be mentioned as well. Information on revisits of children was not available in our database. However, revisits do not correspond with inadequate use of a fast track and a previous study showed that low urgent triaged children did not have many revisits with serious illness.26 Additionally, our results might not be generalisable to all ED settings, since we included large tertiary hospitals. However, we excluded children with comorbidity in order to make our population more comparable to the paediatric population visiting general hospitals. Furthermore, the large range of 22%–73% of children with low triage urgency attending the participating EDs shows that there is variety in our study population. Finally, our study did not test whether, in practice, these children would have been managed the same way in a fast track or if they would have had shorter stays.
Implications for clinical practice
Although different streaming approaches might already be in place at ED settings mostly in the UK, this large study across different European EDs show that EDs can direct low urgent triaged febrile children with respiratory symptoms to a fast track based on objective and standardised triage. Implementation of a fast track in emergency care settings might lead to lower medical costs, shorter waiting time and length of stay at the ED for these patients, while improving better patient flow in the rest of the ED.3 4 10 For the assessment of children in a fast track, a separate assigned area and the availability of healthcare professionals are required. Having junior doctors or nurse practitioners to clinically assess these children in a fast track and discharge them would be ideal.27 28 In general, laboratory blood testing is discouraged in a fast track to ensure a short turnaround time. However, in our study laboratory blood testing in children with respiratory symptoms mostly entailed CRP (99%), which can be performed as point-of-care in a fast track. Most of the European EDs have point-of-care CRP testing available, which can be used in a fast track setting.29
Future research is needed in the form of a before/after study or cluster randomised design to compare length of stay, waiting times and revisits before and after implementation of a fast track intervention for low urgent triaged children with respiratory symptoms at paediatric emergency care settings. The effectiveness of implementing a fast track also depends on the patient volume at the ED and the availability of healthcare professionals. Lastly, a fast track should be implemented in routine care as part of the triage process at the ED.
Conclusion
In this study, we determined that low urgent triaged febrile children with respiratory symptoms were the most suitable for assessment in a fast track. Implementing a fast track for these children presenting to EDs with non-urgent problems could potentially improve patient flow in the ED.
emermed-2023-213375supp002.pdf (108.9KB, pdf)
Footnotes
Handling editor: Gene Yong-Kwang Ong
Twitter: @ejlim8, @rgnijman
Presented at: This paper was presented as abstract at the ESPID 2021 Annual Meeting.
Collaborators: PERFORM consortium author names are presented in online supplemental appendix G.
Contributors: CT, CLV, JMZ, UvB, EDC, IE, ME, MvdF, JH, BK, ML, EL, IM, FM-T, RGN, MP, IR-C, AR, MT, WZ, DZ and HAM contributed to the study conceptualisation and design of the study, and the interpretation of the findings. CT performed the analyses and drafted the initial and final manuscript. CT, CLV, JMZ, UvB, EDC, IE, ME, MvdF, JH, BK, ML, EL, IM, FM-T, RGN, MP, IR-C, AR, MT, WZ, DZ and HAM critically reviewed the manuscript, read and approved the final manuscript and agreed to be accountable for all aspects of the work. HAM acts as guarantor.
Funding: This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement no. 848196. The research was supported by the National Institute for Health Research Biomedical Research Centres at Imperial College London, Newcastle Hospitals NHS Foundation Trust and Newcastle University.
Disclaimer: The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Data are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Approval by the ethics committees of all participating hospitals was obtained: Austria (Ethikkommission Medizinische Universität Graz, ID: 28-518 ex 15/16), Germany (Ethikkommission der LMU München, ID: 699-16), Greece (Ethics committee, ID: 9683/18.07.2016), Latvia (Centrala medicinas etikas komiteja, ID: 14.07.201 6. No. Il 16-07-14), Slovenia (Republic of Slovenia National Medical Ethics Committee, ID: 0120-483/2016-3), Spain (Comité Autonómico de Ética de la Investigación de Galicia, ID: 2016/331), The Netherlands (Commissie Mensgebonden onderzoek, ID: NL58103.091.16), the UK (Ethics Committee, ID: 16/LO/1684, IRAS application no. 209035, Confidentiality advisory group reference: 16/CAG/0136). The need for informed consent was waived and an additional opt-out mechanism was in place in the UK settings.
References
- 1. Sartini M, Carbone A, Demartini A, et al. Overcrowding in emergency department: causes, consequences, and solutions-a narrative review. Healthcare (Basel) 2022;10:1625. 10.3390/healthcare10091625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Timm NL, Ho ML, Luria JW. Pediatric emergency department overcrowding and impact on patient flow outcomes. Acad Emerg Med 2008;15:832–7. 10.1111/j.1553-2712.2008.00224.x [DOI] [PubMed] [Google Scholar]
- 3. Barata I, Brown KM, Fitzmaurice L, et al. Best practices for improving flow and care of pediatric patients in the emergency department. Pediatrics 2015;135:e273–83. 10.1542/peds.2014-3425 [DOI] [PubMed] [Google Scholar]
- 4. Bond K, Blitz S, Friesen C, et al. Interventions to reduce overcrowding in emergency departments. 2006.
- 5. Martin HA, Noble M, Wilmarth J. Improving patient flow and decreasing patient length of stay in the pediatric emergency department through implementation of a fast track. Adv Emerg Nurs J 2021;43:162–9. 10.1097/TME.0000000000000351 [DOI] [PubMed] [Google Scholar]
- 6. Hampers LC, Cha S, Gutglass DJ, et al. Fast track and the pediatric emergency department: resource utilization and patients outcomes. Acad Emerg Med 1999;6:1153–9. 10.1111/j.1553-2712.1999.tb00119.x [DOI] [PubMed] [Google Scholar]
- 7. Simon HK, McLario D, Daily R, et al. "Fast tracking" patients in an urban pediatric emergency department. Am J Emerg Med 1996;14:242–4. 10.1016/S0735-6757(96)90166-7 [DOI] [PubMed] [Google Scholar]
- 8. Considine J, Kropman M, Kelly E, et al. Effect of emergency department fast track on emergency department length of stay: a case-control study. Emerg Med J 2008;25:815–9. 10.1136/emj.2008.057919 [DOI] [PubMed] [Google Scholar]
- 9. Dinh MM, Enright N, Walker A, et al. Determinants of patient satisfaction in an Australian emergency department fast-track setting. Emerg Med J 2013;30:824–7. 10.1136/emermed-2012-201711 [DOI] [PubMed] [Google Scholar]
- 10. De Freitas L, Goodacre S, O’Hara R, et al. Interventions to improve patient flow in emergency departments: an umbrella review. Emerg Med J 2018;35:626–37. 10.1136/emermed-2017-207263 [DOI] [PubMed] [Google Scholar]
- 11. Oredsson S, Jonsson H, Rognes J, et al. A systematic review of triage-related interventions to improve patient flow in emergency departments. Scand J Trauma Resusc Emerg Med 2011;19:43. 10.1186/1757-7241-19-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Karpiel M, Williams M. Developing a FAST TRACK program. J Ambul Care Mark 1988;2:35–48. 10.1300/j273v02n02_05 [DOI] [PubMed] [Google Scholar]
- 13. Mackway‐Jones K, Marsden J, Windle J. Emergency triage: Manchester Triage Group. Third Edition: John Wiley & Sons, Ltd, 2013. 10.1002/9781118299029 [DOI] [Google Scholar]
- 14. Amthauer C, Cunha MLC da. Manchester triage system: main flowcharts, discriminators and outcomes of a pediatric emergency care. Rev Lat Am Enfermagem 2016;24:e2779. 10.1590/1518-8345.1078.2779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sands R, Shanmugavadivel D, Stephenson T, et al. Medical problems presenting to paediatric emergency departments: 10 years on. Emerg Med J 2012;29:379–82. 10.1136/emj.2010.106229 [DOI] [PubMed] [Google Scholar]
- 16. The Royal College of Emergency Medicine . Initial assessment of emergency Department patients February. 2017. Available: https://rcem.ac.uk/wpcontent/uploads/2021/10/SDDC_Intial_Assessment_Feb2017.pdf
- 17. PERFORM . Personalised risk assessment in febrile illness to Optimise real-life management 2020. n.d. Available: https://www.perform2020.org/
- 18. Hagedoorn NN, Borensztajn DM, Nijman R, et al. Variation in antibiotic prescription rates in febrile children presenting to emergency departments across Europe (MOFICHE): a multicentre observational study. PLoS Med 2020;17:e1003208. 10.1371/journal.pmed.1003208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Borensztajn D, Yeung S, Hagedoorn NN, et al. Diversity in the emergency care for febrile children in Europe: a questionnaire study. BMJ Paediatr Open 2019;3:e000456. 10.1136/bmjpo-2019-000456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zachariasse JM, Seiger N, Rood PPM, et al. Validity of the Manchester triage system in emergency care: a prospective observational study. PLoS One 2017;12:e0170811. 10.1371/journal.pone.0170811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Simon TD, Haaland W, Hawley K, et al. Development and validation of the pediatric medical complexity algorithm (PMCA) version 3.0. Acad Pediatr 2018;18:577–80. 10.1016/j.acap.2018.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Turner NM. Advanced paediatric life support de nederlandse editie. Houten: Bohn Stafleu Van Loghum, 2017. [Google Scholar]
- 23. Tan CD, Hagedoorn NN, Dewez JE, et al. Rapid viral testing and antibiotic prescription in febrile children with respiratory symptoms visiting emergency departments in Europe. Pediatr Infect Dis J 2022;41:39–44. 10.1097/INF.0000000000003326 [DOI] [PubMed] [Google Scholar]
- 24. van de Maat JS, Garcia Perez D, Driessen GJA, et al. The influence of chest X-ray results on antibiotic prescription for childhood pneumonia in the emergency department. Eur J Pediatr 2021;180:2765–72. 10.1007/s00431-021-03996-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Doyle SL, Kingsnorth J, Guzzetta CE, et al. Outcomes of implementing rapid triage in the pediatric emergency department. J Emerg Nurs 2012;38:30–5. 10.1016/j.jen.2010.08.013 [DOI] [PubMed] [Google Scholar]
- 26. Nijman RG, Borensztajn DH, Zachariasse JM, et al. A clinical prediction model to identify children at risk for revisits with serious illness to the emergency department: a prospective multicentre observational study. PLoS One 2021;16:e0254366. 10.1371/journal.pone.0254366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wood C, Wettlaufer J, Shaha SH, et al. Nurse practitioner roles in pediatric emergency departments: a national survey. Pediatr Emerg Care 2010;26:406–7. 10.1097/PEC.0b013e3181e057b8 [DOI] [PubMed] [Google Scholar]
- 28. Doetzel CM, Rankin JA, Then KL. Nurse practitioners in the emergency department: barriers and facilitators for role implementation. Adv Emerg Nurs J 2016;38:43–55. 10.1097/TME.0000000000000090 [DOI] [PubMed] [Google Scholar]
- 29. Dewez JE, Pembrey L, Nijman RG, et al. Availability and use of rapid diagnostic tests for the management of acute childhood infections in Europe: a cross-sectional survey of paediatricians. PLoS One 2022;17:e0275336. 10.1371/journal.pone.0275336 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
emermed-2023-213375supp001.pdf (408.1KB, pdf)
emermed-2023-213375supp002.pdf (108.9KB, pdf)
Data Availability Statement
Data are available on reasonable request. Data are available from the corresponding author on reasonable request.