Abstract
Background:
The extensive use of various electronic games and communication devices, particularly among children and adolescents, has raised concerns, particularly during the COVID-19 pandemic. This study investigated the link between screen time and internalizing disorders, such as anxiety and depression, among individuals aged ≤18 during the global COVID-19 pandemic.
Methods:
This systematic review aims to summarize scientific publications from 2019 to early 2022 by searching databases, including the Cochrane Library, PubMed, Web of Science, Scopus, and PsycINFO, to identify suitable studies. In each paper, we searched the following keywords and their synonyms: screen, child, high school, middle school, and psychiatric disorders. The quality of the selected papers was evaluated using a checklist recommended by the National Institutes of Health (NIH) for observational cohort studies.
Results:
Out of 986 reports identified, we included 12 papers with 14,483 participants. The study revealed a negative correlation between screen time (TV, computer, video games, and mobile phones) and behavioral outcomes. Smartphones were the most frequently used devices, with video games being more prevalent among older participants for education, communication, and entertainment purposes. The prevalence of depression ranged between 10% and 25%. Furthermore, anxiety and depression were identified as predictors of increased screen usage. Some results displayed variation based on the type of screen exposure, the questionnaires used, and the age of the participants.
Conclusions:
The findings imply an indirect association between increased screen time and depression and anxiety. It is crucial to consider limitations on screen time exposure and parental supervision as measures to prevent certain mental disorders.
Keywords: Anxiety, children, COVID-19, depression
Introduction
While the policies such as travel controls, self-quarantine, lockdowns, and home confinement have produced positive outcomes regarding infection control. During COVID-19 pandemic, they have significantly impacted individuals across different age groups, resulting in notable lifestyle changes.[1,2]
The prioritization of mental health disorders as a public health concern during childhood has been attributed to the emergence of numerous internalized symptoms during adolescence.[3] These disorders are linked to disability and a diminished quality of life.[4] Internalizing disorders, encompassing conditions such as anxiety and depression, manifest through distress, fatigue, a sense of emptiness, and detachment.[5]
The show’s timing is one of the factors related to mental health. By World Health Organization recommendations, children aged 3–4 should not exceed 1–2 hours of screen time per day, while those aged 5–17 should adhere to the same guidelines.[6,7] Children, recognized as a vulnerable group undergoing critical developmental stages, tackle heightened physical and psychological challenges. The surge in online activities and screen usage following the closure of schools,[8,9,10] whether for educational purposes or entertainment, often occurs without adequate parental supervision,[11] posing threats to their well-being. Additionally, the practice of social distancing has led to an escalation of psychological consequences during the COVID-19 pandemic, including heightened fear,[12] insomnia,[13] anxiety,[14] depression,[10] and domestic violence.[15] Consequently, the prevalence of depression and anxiety among students during the initial period of home confinement ranges from 18.9% to 22.6%.[16]
Whether behavioral issues and psychological disorders result directly from increased screen time and online engagement or indirectly from concerns associated with the pandemic remains unclear. The rise in sedentary behaviors, reduced physical activity, and disrupted sleep patterns are closely linked to mental health issues even before the pandemic.[17,18]
Nevertheless, screen time and its effects on children’s mental health are contentious, primarily due to conflicting research findings and methodological limitations.[19,20,21] In the ongoing discourse, there exists a divide among experts regarding the advisability of limiting screen exposure in young children.[22,23] Conversely, an opposing viewpoint contends that restricted screen time and other activities like studying and physical exercise can yield certain advantages.[24,25,26] Conversely, children’s use of social networks has been associated with increased introversion and behavioral problems, including higher-than-normal levels of depression, attention deficits, and anxiety.[27]
As a result, the impact of screen use on some children’s mental health remains controversial to a certain extent.[28,29] Consequently, this review aims to inspect the connection between screen time and anxiety and depression amid the backdrop of the pandemic.
Methods
Study protocol
The study protocol for this investigation was officially registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the protocol number CRD42022334665.
Search strategy
This comprehensive systematic review conducted exhaustive searches across several reputable databases, including PubMed, Web of Sciences, Scopus, and PsycINFO. These searches encompassed articles published from 2019 to May 17, 2022, spanning the duration of the COVID-19 pandemic, within the confines of English-language peer-reviewed journals.
The Cochrane Library underwent thorough screening through multiple iterations of the research question. The search process included using a carefully crafted set of medical keywords (Medical Subject Headings or MeSH) and their synonyms.
The primary objective was to comprehensively investigate the intersection of child and adolescent populations with social networks, the Internet, cyberspace, smartphones, mobile applications, phones, cell phones, computers, Instagram, Telegram, WhatsApp, technology, electronic devices, video games, mobile phones, screens, psychology, mental disorders, psychiatric illnesses, psychiatric diseases, mental illnesses, psychiatric disorders, behavior disorders, psychiatric diagnoses, mental disorders, severe mental disorders, COVID-19, and SARS-CoV-2, all within the English-language context.
The process involved extracting key concepts concerning screen time, mental illnesses (including depression and anxiety), and children by carefully examining critical terms and thoroughly analyzing titles and abstracts within various databases. To guarantee a comprehensive scope, synonymous terms were consolidated using the “OR” operator, and subsequently, the results were further refined utilizing the “AND” operator to encompass all pertinent articles.
Revised study inclusion and exclusion criteria
The research inquiry for this study adhered to the PEO (population, exposure, and outcomes) framework. The inclusion criteria encompassed studies that met the following conditions: (1) participants were children aged below 18 years, (2) measurement of screen time duration (in hours and/or minutes) was conducted, (3) assessment of internalizing disorders (such as depression and anxiety) was performed, and (4) the study design was either cross-sectional, observational, or longitudinal. Conversely, studies were excluded if they met any of the following criteria: (1) they were conducted before the onset of the COVID-19 pandemic, (2) there were instances of duplication across different databases, (3) the target demographic differed from the focus of the study, (4) the investigations centered on the family status of the child, and (5) externalizing problem behaviors (EXT), particularly those arising from interactions within the social environment (e.g. aggression, impulsivity, deviance, hyperactivity, attention-deficit/hyperactivity disorder symptoms, sleep disorders, and autism), were explicitly excluded. Furthermore, interventional studies, letters, review articles, case reports, and research exclusively involving adults 18 years and older were also excluded from consideration. The reference numbers remain unchanged.
Data extraction and quality assessment
To ensure impartiality and rigorous evaluation, two authors, SSD and M Kh, independently conducted the process of qualitative assessment and data extraction. Subsequently, the authors engaged in a collaborative discussion to reach a consensus on their findings.
The subsequent data points were gathered from the original reports:
Author’s name and year of publication.
The country where the study data were gathered.
The characteristics of the sample encompass various aspects, including study design, sample size, types of screen time, behavioral disorders under consideration, and the specific questionnaires employed.
To evaluate the quality of the chosen articles, we utilized a checklist recommended by the American National Institutes of Health (NIH), accessed at https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. This checklist, tailored to assess the quality of observational cohort and cross-sectional studies, comprises 14 questions, each requiring a binary response of “yes” or “no.” The final assessment is then categorized as either “good,” “fair,” or “poor” and is presented in Table 1.
Table 1.
Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies
| Hua Chen et al., 2021, Taiwan[11] | Lin Wang et al., 2021, China[30] | Chao Chen et al., 2022, China[15] | Rita Monteiro et al., 2020, Portugal[31] | Lisa S. Olive et al., 2022, Australi[10] | Xuedi Li et al., 2021, Canada[32] | Chika Ueno et al., 2022, Japan[33] | Brae McArthur et al., 2021, Canada[34] | Li Duan et al., 2020, China[35] | Michelle Drouin et al., 2020, USA[36] | Zhaojun Teng et al., 2021, China[37] | P S Tandon et al., 2021, USA[38] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was the research question or objective in this paper clearly stated? | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 2. Was the study population clearly specified and defined? | √ | √ | √ | No | √ | √ | CD | √ | CD | √ | √ | √ |
| 3. Was the participation rate of eligible persons at least 50%? | √ | √ | No | √ | √ | √ | √ | √ | NR | √ | √ | √ |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? | CD | √ | √ | √ | No | √ | √ | √ | NR | √ | √ | CD |
| 5. Was a sample size justification, power description, or variance and effect estimates provided? | √ | No | √ | No | √ | √ | No | No | NR | √ | √ | √ |
| 6. For the analyses in this paper, were the exposure(s) of interest measured before the outcome(s) being measured? | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? | √ | √ | √ | √ | √ | √ | No | √ | √ | √ | √ | √ |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 10. Was the exposure(s) assessed more than once over time? | NA | NA | √ | NA | NA | NA | NA | √ | NA | √ | √ | √ |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 12. Were the outcome assessors blinded to the exposure status of participants? | √ | √ | √ | √ | √ | √ | NR | NR | NR | √ | √ | √ |
| 13. Was loss to follow-up after baseline 20% or less? | √ | √ | √ | √ | √ | NR | No | √ | NR | √ | √ | √ |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? | No | √ | √ | No | No | √ | √ | √ | NR | √ | √ | √ |
| Quality Rating (Good, Fair, or Poor) SS D | Good | Good | Good | Fair | Good | Good | poor | Good | Poor | Good | Good | Good |
| Quality Rating (Good, Fair, or Poor) M Kh | Good | Good | Good | Good | Good | Good | poor | Good | Poor | Good | Good | Good |
NR: Not Reported, NA: not applicable, CD, cannot determine
Results
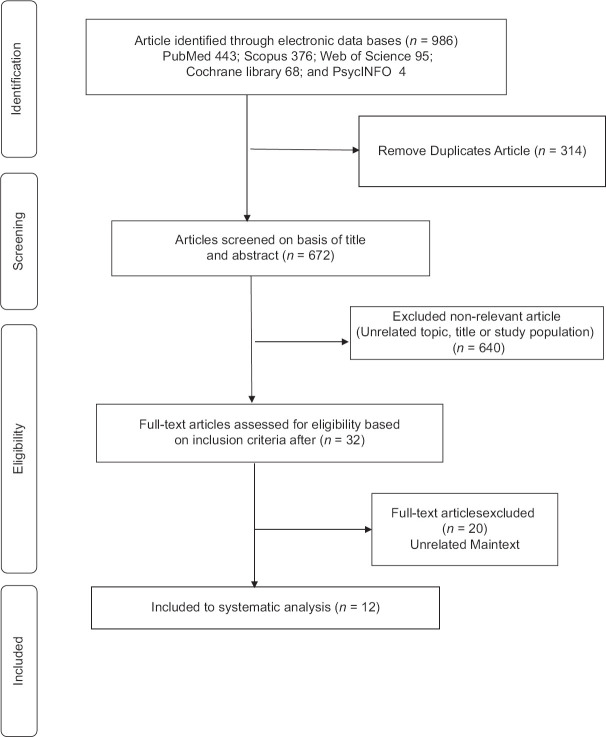
This research examined the correlation between the amount of time spent on electronic devices such as smartphones, video games, and social media and internalized disorders, specifically depression and anxiety, in children and adolescents during the COVID-19 pandemic. As illustrated in Figure 1, our initial search produced a total of 986 records from various sources, including PubMed (443), Scopus (376), Web of Science (95), the Cochrane Library (68), and PsycINFO (4). Subsequently, we identified and removed 314 duplicate records. Following this, we thoroughly assessed the abstracts of the remaining 672 articles.
Figure 1.
Flowchart presenting the steps in the paper selection
Of the 672 articles, 640 did not align with our inclusion criteria as they either pertained to topics unrelated to our review or involved participants irrelevant to our study. Extensive discussions took place to ensure a consensus was reached at every stage of the review process. After carefully reviewing titles and abstracts, we incorporated 12 studies into our systematic review. Detailed information regarding these studies can be found in Table 2, including data on study authors, publication year, country of origin, study type, target population, sample size, electronic screens under examination, and the various types of behavioral disorders studied.
Table 2.
Summary of descriptive characteristics of the included studies according to main Data
| Author Year/country Type of study | Target population and sample size | Screen type used | Types of behavioral disorders | Questionnaire | Finding |
|---|---|---|---|---|---|
| HUA CHEN et al., 2021,[11] Taiwan A longitudinal study | primary school students’ mean age was 10.32 years (n=535; 265 boys) | 1. Smartphone 2. Social Media 3. Internet Gaming | Psychological distress (Depression, Anxiety, Stress) | DASS-21 | Schoolchildren who increased their by 15 or 30 min daily on internet-related activities showed an increased level of psychological distress |
| Lin Wang et al., 2020, China[30] A cross-sectional study | Children (6-11 years old) and adolescents (12-16 years old). n=12186 | Videogames | Psychosocial and behavioral problems | the Achenbach Child Behavior Checklist (CBCL). | The positive detection rate of psychological problems within Wuhan was greater than that outside Wuhan for schizoid, and depression in children, and for somatic complaints, immaturity, and delinquent behavior. |
| Chao Chen et al., 2019, China[15] A longitudinal study (Perspective) | Children (Mean [SD] age=10.83 [0.75] years) n=575 | 1. Smartphone Application 2. Internet Gaming | Psychological Distress | DASS 21, Smartphone Application-Based Addiction Scale | Cross-lagged models found that higher levels of problematic smartphone use were not significantly related prospectively to greater psychological distress before the COVID-19 outbreak, but this prospective relationship became significant during the COVID-19 outbreak. |
| Problematic gaming | (SABAS), Internet Gaming Disorder Scale-Short Form | Whereas problematic gaming was associated prospectively with psychological distress before the COVID-19 outbreak (between Waves 1 and 2), this association became nonsignificant during the COVID-19 lockdown (between Waves 2 and 3). | |||
| Rita Monteiro et al., 2020, Portugal[31] A Cross-Sectional Study | Children aged from 6 months to 6 years, n=193 | Exposure time (in hours) to television, cellphone, and Internet, | Behavioral and emotional symptoms on children | Baby Pediatric Symptom Checklist (BPSC), Preschool Pediatric Symptom Checklist (PPSC), Question about time use of screen time exposure | The findings revealed a modest relationship between children’s exposure time to screens and behavioral and emotional problems on children studied. It was also found that parents may play an important role in children’s behavioral and emotional adjustment during the confinement period. |
| Lisa S. Olive et al., 2020, Australi[10] A cross-sectional Study | n=2365, children aged ≤18 years, | Screen time | Mental health | DASS 21 | Children’s sleep problems were significantly associated with increased mental health problems after accounting for socioeconomic status, physical activity, and screen time and Children more using screen time on the weekend. |
| Xuedi Li et al., 2020, Canada[32] A Cohort Study | Aged 2–18 years, n=2026 | TV and digital media time, video games, electronic learning time, and video chatting time. | Depression-anxiety, conduct problems, Strengths and Weaknesses of Attention-Deficit/Hyperactivity Disorder (SWAN Symptoms and Normal Behavior Scale) | Strengths and Difficulties Questionnaire (SDQ), depression and anxiety), RCADS-P (Revised Children and Depression Scale–Parent Version) for older children, SCARED (Screen for Child Anxiety Related Disorders, TIDES (The Irritability and Dysregulation of Emotions questionnaire) was administered to measure. irritability | higher TV or digital media time was associated with higher levels of conduct problems and hyperactivity/inattention, higher levels of depression, anxiety, and inattention; higher levels of video game time were associated with higher levels of depression, irritability, inattention, and hyperactivity. Higher levels of electronic learning time were associated with higher levels of depression and anxiety. |
| Chika Ueno et al., 2020, Japan[33] A cross-sectional Study | 959 children in four public elementary schools. | screen time | Behavioral problems | Self-administrative questionnaire | Time of spending on TV and/or video and video games significantly longer during school closure than after school reopened. children’s behavioral problems during school closure were associated with longer total screen time (OR: 1.2, 95%, [CI]: 1.14–1.28, P<0.001). |
| Brae McArthur et al., 2021, Canada[34] A cross-sectional Study | n=846, (child age 9–11) | Screen time | Depression-anxiety | Depression Short Form (CES-D-10), 6-item Spielberger State Anxiety Inventory Short Form (SSAI-SF) | After controlling for child sex, age, and anxiety symptoms pre-COVID-19, connectedness to caregivers and child sleep were negative, and child screen time duration positively predicted anxiety. Depressive symptoms pre-COVID-19, connectedness to caregivers were negative, and child screen time duration was significantly predicting depressive symptoms. |
| Li Duan et al., 2020, China[35] A cross-sectional | 359 children and 3254 adolescents online | smartphone addiction, Internet Addiction | Depression | Spence Child Anxiety Scale, Child Depression Inventory, and Coping Style Scale | Seven significant factors associated with increased levels of anxiety, including female, resident in urban regions, and emotion-focused coping style. Nine factors are associated with increased levels of depression, such as smartphone addiction, Internet addiction, and residence in Hubei province. Two additional factors are associated with decreased levels of depressive symptoms: hours spent on Internet per day before the epidemic and the tendency to apply a problem-focused coping style. |
| Michelle Drouin et al., 2020, USA[36] A cross-sectional study | (n=260), children aged 0–19 years | social media, phone | Anxiety | Parent anxiety (PHQ-4) and other self-administrative questionnaire | On average, parents reported that both they and their children (especially teenagers aged 13–18) had increased technology and social media use since the beginning of social distancing. Moreover, even after controlling for demographic factors, structural equation models showed that parents and children with higher levels of anxiety (as reported by parents) were more likely to increase their technology use and use social media and phones to connect. |
| Zhaojun Teng et al., 2020, China[37] A longitudinal study | n=1,778, children and adolescents (875 children, 903 adolescents) | videogame use, Internet Gaming | Depression-anxiety | The Internet Gaming Disorder Scale-Short Form (IGDS9-, impacts caused by the COVID-19 pandemic on different life domains (i.e., study activities, sleep quality, lifestyle habits [e.g., eating habits, physical exercise, and entertainment], social activities, and family relationships), The Chinese version of the Depression Scale (CES-D) and anxiety | The results indicated that both videogame use and Internet Gaming Disorder increased significantly for adolescents. The cross-lagged panel model results suggested that depressive and anxiety symptoms positively predicted Internet Gaming Disorder and video game use (especially for boys), but not inversely. |
| Pooja S Tandon et al., 2020, USA[38] A cross-sectional study | children aged 6 to 10 years and adolescents 11 to 17 years, n=547 | Screen time | Depression-anxiety | the Strengths and Difficulties Questionnaire (SDQ), and other questions related to mental health problems | Children reported a mean (SD) of 3.9 (2.2) d/wks. with at least 60 minutes of physical activity and 4.4 (2.5) h/d of recreational screen time. COVID-19 stressors were significantly associated with higher total difficulties for both younger and older groups. More screen time was correlated with higher total difficulties among younger and older children. There were no significant differences by sex. |
Due to the diversity of the studies, various reports on different behavioral disorders, and the insufficient quality of some studies and overlapping identities, a meta-analysis could not be conducted.
In total, this systematic review encompassed 14,483 children and adolescents. In a few studies,[10,36] the specific number of children was not clearly distinguished from adolescents. Furthermore, some studies examined screen time on different electronic devices,[10,33,34,38] while in three studies, video game usage was specifically evaluated.[30,37,39] However, certain studies did not distinguish between the types of electronic devices, such as smartphones, social media, and gaming.[38,39] In some instances, a minority of participants were children while others were adolescents; for instance, in Li Duan et al.’s study, only 10% of the 3254 participants were children, with the remainder being adolescents.[35]
Behavioral problems were assessed using a variety of questionnaires, ranging from locally validated Chinese instruments to the widely recognized DASS-21 questionnaire, the most commonly used tool. Most of the surveys were completed online by parents. For example, in the Duan et al. study,[35] the criteria examined were Internet and smartphone addiction. Most of these studies were conducted in Eastern countries, particularly China, while others were conducted in Western nations.
In general, electronic device usage time was increased across all studies during the disease outbreak, although the criteria and categorizations for electronic device time varied. Some studies mentioned specific durations, such as 4.4 (2.5) hours per day of screen time for enjoyable activities,[15] 4 (2.4) h/d,[38] or over 3-4 hours per day on weekdays, weekends, and weekends.[10] Additionally, another study indicated that access to smartphones and gaming devices for one hour or more was a significant benchmark[11].
The link between screen time and behavioral disorders was explored by considering various variables and confounding factors. For instance, in a study involving 535 children, the time spent on social media and smartphones increased by 0.14 and 1.02 hours per day, respectively, during the COVID-19 pandemic compared to the pre-pandemic period.[11] Notably, in this study, an increase of just 15-30 minutes in daily Internet-related activities was associated with higher levels of psychological distress, including stress, depression, and anxiety. This association was even more pronounced during school closures compared to before.[11] Conversely, a study by Ueno et al. involving 959 elementary school students found that an increase of 1.2 hours in screen usage resulted in the development of mental disorders.[33] Another study featuring 12,186 children and adolescents categorized online usage into two groups: less than 4 hours per day or more than 4 hours per day, without specifying the type of electronic devices. This study revealed that video games and online time, especially outside of Wuhan, were linked to depression in children.[30]
While smartphones were generally the primary media devices for most children, the specific type of screen has not been explicitly mentioned in previous research.[15] It appears that, during childhood, children spend more time watching TV or videos compared to playing video games.[31,33] Notably, during the critical period of the COVID-19 pandemic, when social interactions were limited, parents allowed their children to use screens for longer durations than usual, primarily for entertainment. Other reasons for increased screen time included communication with friends,[10,11] educational activities,[32] and watching TV for entertainment.[33] Interestingly, unlike smartphones, children’s time spent watching TV/videos and gaming decreased in some studies during the COVID-19 pandemic.[11,33]
There is significant interest in understanding the prevalence and identifying the risk factors for developing psychosocial and behavioral problems. The current study has reported varying degrees of psychological disorders. For instance, based on Ueno et al.,[33] involving 959 elementary school children, approximately half of the students experienced behavioral problems during school closures. In Duan et al.[35] study, nearly 25% of children and adolescents aged 7-18 displayed depressive symptoms. Tandon et al.[38] reported that depression and anxiety in children were15, and 10.4%, with depression being more common among adolescents.
Wang et al’s.[30] study indicated that the prevalence of depressive symptoms was higher in Wuhan children than those outside Wuhan. In a longitudinal study conducted by Chen et al. study[15] involving 1238 schoolchildren, spanning from before the pandemic to the third wave of COVID-19, the rates of psychological stress, depression, anxiety, and problematic smartphone (PSP) use were higher during the third wave (post-pandemic) in comparison to the first wave (pre-lockdown). This study reported moderate levels of depression, severe anxiety, and mild stress.[15]
Drouin et al.[36] found that 62.7% of children experienced anxiety symptoms for several days at the pandemic’s beginning in Li et al.’s longitudinal cohort study,[32] which involved 2026 children and youth; increased screen time spent watching TV and digital media among children aged 8 to 14.6 correlated with a higher prevalence of depression, anxiety, and inattention. A similar correlation was observed between video game usage and depression.
In contrast to most studies, some research highlighted the predictive role of psychological disorders in screen usage. In Teng et al.’s study,[37] which involved 1,778 children and adolescents, depression and anxiety were identified as predictors and risk factors for video game use and Internet gaming disorder (IGD) during the COVID-19 pandemic. Furthermore, there was no significant difference in depression levels before and during the COVID-19 pandemic.
However, a history of depression and anxiety before the pandemic, the quality of the child’s relationship with their caregivers, and the child’s sleep patterns and screen usage were correlated with children’s mental health disorders.[34] The pandemic was associated with increased mental health issues and heightened engagement in video game activities. Additionally, in Drouin et al.[36] conducted in the USA involving 266 parents and their children aged 0-19, anxiety was identified as a predictor of social media use, with higher anxiety levels linked to excessive social media or smartphone use.
Discussion
This study presents a comprehensive research summary examining electronic devices’ impact on children’s behavioral disorders. The advent of the COVID-19 pandemic has significantly altered children’s lifestyles, adversely affecting their psychological well-being on a global scale. Current investigations have revealed that increased screen time during the pandemic may have exacerbated psychological challenges in a substantial cohort of schoolchildren. In this systematic review, we have synthesized data from 12 observational studies that explored the relationship between screen usage and behavioral disorders in children and adolescents.
The primary outcome of this study indicates that children and adolescents who spend more time on screens are at a higher risk of developing behavioral disorders, including depression and anxiety, compared to their peers, both before and during the pandemic.
Several factors contributed to this trend. Firstly, the closure of schools prompted a surge in children’s screen time, driven by educational needs and the desire for social interaction with friends.[33,35] Digital media consumption has increased compared to pre-pandemic levels.[3,10,30,32,33,35] Additionally, the transition to online learning-induced anxiety and depressive symptoms as students struggled to cope with the demands of excessive homework.[40] Moreover, the need to counteract the effects of lockdowns amplified Internet usage, especially among children and adolescents.[37] Heightened online activity facilitated access to misinformation and distressing news, leading to feelings of fear, loneliness, depression, anxiety, and other behavioral issues.[33] Importantly, it is worth noting that the psychological burden imposed by social distancing during the pandemic extended beyond screen usage alone. Passive screen time, devoid of social interaction, has had a more pronounced impact on psychological health than the mere closure of schools, as evidenced by the lack of significant increases in psychological disorders during summer vacations.[33] Furthermore, another study revealed higher levels of aggression in children who watched TV programs or played video games, particularly those with violent content.[41]
The detrimental effects of screen addiction on health have been explored in previous research. Consistent with these findings, excessive smartphone and Internet use was associated with mental and behavioral problems, impaired performance, reduced face-to-face social interaction, neglect of personal life, relationship difficulties, and mood disturbances.[42,43,44,45]
In alignment with the results of our current study, greater screen use correlated with heightened mental health issues in children and youth.[44,46] However, it is essential to note that the specific time thresholds for screen usage varied across studies. Nevertheless, it was observed that increased screen time from 1.2 hours per day to more than 4 hours per day was linked to higher rates of depression and anxiety. By established guidelines, preschool children and those aged 5 to 10 years should limit their daily screen time to one and two hours, respectively.[47]
Broadly, television viewing and smartphone usage were predominant media activities among younger children, as opposed to gaming.[11] Consequently, the prevalence and severity of anxiety, depression, and screen time were comparatively lower in this age group. This observation aligns with findings from other research studies.[48,49,50,51] However, certain studies indicated an increased prevalence of gaming during the pandemic,[30,37] possibly as a coping mechanism for dealing with negative emotions such as depression, anxiety, stress, and fear of missing out.[40] The allure of gaming, characterized by the anticipation of sequential rewards, played a significant role in this trend. It is noteworthy that problematic gaming (PG) was linked to psychological distress only before the COVID-19 outbreak and became non-significant during the pandemic lockdown, possibly due to increased parental supervision and a greater emphasis on the adverse effects of gaming on social connections before the pandemic.[15]
In contrast to most research findings[10,14,15,31,33,35,39] some studies have highlighted the predictive role of mental health in the prevalence of digital device usage and its correlation with depression and anxiety.[36,37] On one hand, mental disorders can lead children to fulfill their psychological needs through digital devices. It is important to note that due to the cross-sectional nature of these studies, we cannot definitively establish a causal relationship between these two aspects or provide a clear explanation of the association. On the other hand, research related to the pandemic has revealed that not only is screen time associated with mental health disorders, but other post-pandemic factors have also contributed to children’s concerns and behavioral issues during this critical period.
Firstly, the intensity of the COVID-19 pandemic, as an unprecedented and unknown viral disease, has contributed to psychiatric disorders. For example, Wang et al.,[30] in their study involving 12,186 children aged 6-16 from five regions in China, found that parent-child conflicts, sleep disturbances, reduced physical activity, fewer close friends, and eating disorders were all linked to behavioral problems. Moreover, children and adolescents living in Wuhan faced additional distress [30,37] due to the severe conditions of the epidemic, especially during the quarantine period. Secondly, other worries, such as concerns about the infection of family members or friends, the high prevalence of the disease, and its mortality,[14,35,38,49] as well as anxiety,[36] have threatened children’s physical well-being. Furthermore, factors such as misinformation,[15,35] fear of COVID-19,[52] reduced physical activity, altered sleep patterns,[10] attachment to caregivers, and a history of depression and anxiety[34] all play a crucial role in exacerbating mental health issues and depressive symptoms. For instance, Chen et al.[15] underscored the role of disease outbreak alongside screen time, showing a significant positive association between problematic smartphone (PSP) usage and psychological distress during the COVID-19 outbreak but not before. Conversely, some studies have found that these issues existed before COVID-19, with excessive electronic device use negatively affecting a child’s sleep-wake cycle, resulting in further behavioral problems and occasional stereotypical motor behaviors.[53,54]
The present study has pointed to increased anxiety associated with increased screen time usage during the pandemic.[10,32] Feelings of isolation, a reduced sense of social support, and the physical demands brought on by the fear of missing out on interactions with friends following school closures have driven children to spend more time on Internet-related activities, leading to heightened anxiety symptoms. Various theories, including the compensatory Internet use theory,[55] have emphasized the interactive relationship between problematic smartphone usage, video games, and anxiety.[55,56,57] Despite the notion that spending time on social media during the pandemic was considered a strategy to alleviate negative emotions,[58] our findings did not align with this. The high reported rates of COVID-19 transmission and mortality have led to psychological distress.[12] Parents’ anxiety and sleep disturbances during the pandemic have also been linked to children’s stress.[10] Previous studies have documented various symptoms of mental health disorders, including stress, depression, anxiety, and post-traumatic symptoms during the pandemic.[59]
Conclusion
In this systematic review, we have illuminated a notable inverse correlation between screen and digital media exposure and the psychological well-being of children. Our investigation reveals that schoolchildren significantly increased their smartphone and social media usage during the pandemic, coinciding with a heightened prevalence of depression and anxiety. However, it is imperative to contemplate the implementation and refinement of strategies for monitoring children’s mental health and regulating their access to the Internet and smartphones. However, this situation presents an opportune moment for healthcare professionals to design psychological interventions utilizing screen-based and online platforms, replacing conventional in-person assessments.
Limitations
This study is not without its limitations, which merit discussion. Firstly, heterogeneity exists in mental health measures, screen time assessment methodologies, and self-reported data collection across the studies, which restricts our analysis. Secondly, the studies included a mixed population of children and adolescents, making it impossible to differentiate results based on age groups. Furthermore, various covariates have been considered potential confounders in the relationship between screen time and mental disorders. The predominantly descriptive nature of the study designs inhibits us from definitively establishing causality in the associations observed.
Despite these limitations, the study’s principal strength lies in including several high-quality research endeavors. Additionally, our research team conducted a meticulous and comprehensive literature search, scrutinizing articles from various regions across the globe. Moreover, a rigorous checklist was employed to assess the quality of the included articles.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
Ethical Consideration
No ethical barrier or limitation has been determined. This research is approved by Research Ethics Committee of Isfahan University of Medical sciences.
Code of Ethics
IR.ARI.MUI.REC.1401.243.
Authors’ Contribution
SS D. and M Kh, independently conducted the process of qualitative assessment and data extraction. H J. Performed the analysis. primary search and writing has done by MA. RK designed the study and revised the manuscript. Revision has done by SS D. and M Kh.
Acknowledgments
The authors extend their gratitude for the support received from the Isfahan University of Medical Science.
References
- 1.WHO. Coronavirus disease (COVID-19):Situation report, 206. Geneva: World Health Organization; 2020. [[Last accessed on 2020 Aug 13]]. [Google Scholar]
- 2.Zhang X, Luo W, Zhu J. Top-down and bottom-up lockdown:Evidence from COVID-19 prevention and control in China. J Chin Polit Sci. 2021;26:189–211. doi: 10.1007/s11366-020-09711-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doering S, Larsson H, Halldner L, Gillberg C, Kuja-Halkola R, Lundström S. Internalizing symptoms in adolescence are modestly affected by symptoms of anxiety, depression, and neurodevelopmental disorders in childhood. BMC Psychiatry. 2022;22:233. doi: 10.1186/s12888-022-03875-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen H, Cohen P, Kasen S, Johnson JG, Berenson K, Gordon K. Impact of adolescent mental disorders and physical illnesses on quality of life 17 years later. Arch Pediatr Adolesc Med. 2006;160:93–9. doi: 10.1001/archpedi.160.1.93. [DOI] [PubMed] [Google Scholar]
- 5.Zahn–Waxler C, Klimes–Dougan B, Slattery MJ. Internalizing problems of childhood and adolescence:Prospects, pitfalls, and progress in understanding the development of anxiety and depression. Dev Psychopathol. 2000;12:443–66. [PubMed] [Google Scholar]
- 6.Tremblay MS, Carson V, Chaput J-P, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth:An integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41:S311–27. doi: 10.1139/apnm-2016-0151. [DOI] [PubMed] [Google Scholar]
- 7.McWilliams C, Ball SC, Benjamin SE, Hales D, Vaughn A, Ward DSJP. Best-practice guidelines for physical activity at child care. Pediatrics. 2009;124:1650–9. doi: 10.1542/peds.2009-0952. [DOI] [PubMed] [Google Scholar]
- 8.Mustafa N. Impact of the 2019–20 coronavirus pandemic on education. Int J Health Prefer Res. 2020;4:25–30. [Google Scholar]
- 9.Sun Y, Li Y, Bao Y, Meng S, Sun Y, Schumann G, et al. Brief report:Increased addictive internet and substance use behavior during the COVID-19 pandemic in China. Am J Addict. 2020;29:268–70. doi: 10.1111/ajad.13066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olive LS, Sciberras E, Berkowitz TS, Hoare E, Telford RM, O'Neil A, et al. Child and parent physical activity, sleep, and screen time during COVID-19 and associations with mental health:Implications for future psycho-cardiological disease? Front Psychiatry. 2022;12:774858. doi: 10.3389/fpsyt.2021.774858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen IH, Chen C-Y, Pakpour AH, Griffiths MD, Lin C-Y, Li X-D, et al. Problematic internet-related behaviors mediate the associations between levels of internet engagement and distress among schoolchildren during COVID-19 lockdown:A longitudinal structural equation modeling study. J Behav Addict. 2021;10:135–48. doi: 10.1556/2006.2021.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale:Development and initial validation. Int J Ment Health Addict. 2022;20:1537–45. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the Coronavirus Disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921. doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen CY, Chen IH, Hou WL, Potenza MN, O'Brien KS, Lin CY, et al. The relationship between children's problematic internet-related behaviors and psychological distress during the onset of the COVID-19 pandemic:A longitudinal study. J Addict Med. 2022;16:e73–80. doi: 10.1097/ADM.0000000000000845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;174:898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lewis R, Roden LC, Scheuermaier K, Gomez-Olive FX, Rae DE, Iacovides S, et al. The impact of sleep, physical activity and sedentary behaviour on symptoms of depression and anxiety before and during the COVID-19 pandemic in a sample of South African participants. Sci Rep. 2021;11:1–11. doi: 10.1038/s41598-021-02021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merrill RM. Mental health conditions according to stress and sleep disorders. Int J Environ Res Public Health. 2022;19:7957. doi: 10.3390/ijerph19137957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elson M, Ferguson CJ, Gregerson M, Hogg JL, Ivory J, Klisanin D, et al. Do policy statements on media effects faithfully represent the science? Adv Methods Pract Psychol Sci. 2019;2:12–25. [Google Scholar]
- 20.Kaye LK, Orben A, Ellis DA, Hunter SC, Houghton S. The conceptual and methodological mayhem of “Screen Time”. Int J Environ Res Public Health. 2020;17:3661. doi: 10.3390/ijerph17103661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vickers NJ. Animal communication:When I'm calling you, will you answer too? Curr Biol. 2017;27:R713–5. doi: 10.1016/j.cub.2017.05.064. [DOI] [PubMed] [Google Scholar]
- 22.Jeffery CP. Parenting in the digital age:Between socio-biological and socio-technological development. New Media Soc. 2020;23:1045–62. [Google Scholar]
- 23.Gür D, Türel YK. Parenting in the digital age:Attitudes, controls and limitations regarding children's use of ICT. Comput Educ. 2022;183:104504. [Google Scholar]
- 24.Omar SZ, Daud A, Hassan MS, Bolong J, Teimmouri M. Children internet usage:Opportunities for self development. Procedia Soc Behav Sci. 2014;155:75–80. [Google Scholar]
- 25.Shen C-X, Liu R-D, Wang D. Why are children attracted to the Internet?The role of need satisfaction perceived online and perceived in daily real life. Comput Human Behav. 2013;29:185–92. [Google Scholar]
- 26.Genevieve Marie J. Internet use and child development:Validation of the ecological techno-subsystem. J Biochem Technol. 2010;13:176–85. [Google Scholar]
- 27.Kamaşak T, Topbaş M, Ozen N, Esenülkü G, Yıldız N, Şahin S, et al. An investigation of changing attitudes and behaviors and problematic internet use in children aged 8 to 17 years during the COVID-19 pandemic. Clin Pediatr (Phila) 2021;61:194–205. doi: 10.1177/00099228211065842. [DOI] [PubMed] [Google Scholar]
- 28.Odgers CL, Jensen MR. Annual research review:Adolescent mental health in the digital age:Facts, fears, and future directions. J Child Psychol Psychiatry. 2020;61:336–48. doi: 10.1111/jcpp.13190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Browne D, Thompson DA, Madigan S. Digital media use in children:Clinical vs Scientific responsibilities. JAMA Pediatr. 2020;174:111–2. doi: 10.1001/jamapediatrics.2019.4559. [DOI] [PubMed] [Google Scholar]
- 30.Wang L, Chen L, Jia F, Shi X, Zhang Y, Li F, et al. Risk factors and prediction nomogram model for psychosocial and behavioural problems among children and adolescents during the COVID-19 pandemic:A national multicentre study:Risk Factors of Childhood Psychosocial Problems. J Affect Disord. 2021;294:128–36. doi: 10.1016/j.jad.2021.06.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Monteiro R, Rocha NB, Fernandes S. Are emotional and behavioral problems of infants and children aged younger than 7 years related to screen time exposure during the coronavirus disease 2019 confinement?an exploratory study in Portugal. Front Psychol. 2021;12:590279. doi: 10.3389/fpsyg.2021.590279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li X, Vanderloo LM, Keown-Stoneman CD, Cost KT, Charach A, Maguire JL, et al. Screen use and mental health symptoms in Canadian children and youth during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e2140875. doi: 10.1001/jamanetworkopen.2021.40875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ueno C, Yamamoto S. The relationship between behavioral problems and screen time in children during COVID-19 school closures in Japan. Scand J Child Adolesc Psychiatr Psychol. 2022;10:1–8. doi: 10.21307/sjcapp-2022-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McArthur BA, Racine N, McDonald S, Tough S, Madigan S. Child and family factors associated with child mental health and well-being during COVID-19. Eur Child Adolesc Psychiatry. 2023;32:223–33. doi: 10.1007/s00787-021-01849-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Duan L, Shao XJ, Wang Y, Huang YL, Miao JX, Yang XP, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020;275:112–8. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Drouin M, McDaniel BT, Pater J, Toscos T. How parents and their children used social media and technology at the beginning of the COVID-19 pandemic and associations with anxiety. Cyberpsychol Behav Soc Netw. 2020;23:727–36. doi: 10.1089/cyber.2020.0284. [DOI] [PubMed] [Google Scholar]
- 37.Teng Z, Pontes HM, Nie Q, Griffiths MD, Guo C. Depression and anxiety symptoms associated with internet gaming disorder before and during the COVID-19 pandemic:A longitudinal study. J Behav Addict. 2021;10:169–80. doi: 10.1556/2006.2021.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tandon PS, Zhou C, Johnson AM, Gonzalez ES, Kroshus E. Association of children's physical activity and screen time with mental health during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e2127892. doi: 10.1001/jamanetworkopen.2021.27892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li XD, Vanderloo LM, Keown-Stoneman CDG, Cost KT, Charach A, Maguire JL, et al. Screen use and mental health symptoms in Canadian children and youth during the COVID-19 pandemic. JAMA Network Open. 2021;4:e2140875. doi: 10.1001/jamanetworkopen.2021.40875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fawaz M, Samaha A. E-learning:Depression, anxiety and stress symptomatology among Lebanese university students during COVID-19 quarantine. Nurs Forum. 2021;56:52–7. doi: 10.1111/nuf.12521. [DOI] [PubMed] [Google Scholar]
- 41.Yousef S, Eapen V, Zoubeidi T, Mabrouk A. Behavioral correlation with television watching and videogame playing among children in the United Arab Emirates. Int J Psychiatry Clin Pract. 2014;18:203–7. doi: 10.3109/13651501.2013.874442. [DOI] [PubMed] [Google Scholar]
- 42.Cash H, Rae CD, Steel AH, Winkler A. Internet addiction:A brief summary of research and practice. Curr Psychiatry Rev. 2012;8:292–8. doi: 10.2174/157340012803520513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pantic I. Online social networking and mental health. Cyberpsychol Behav Soc Netw. 2014;17:652–7. doi: 10.1089/cyber.2014.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suchert V, Hanewinkel R, Isensee B. Sedentary behavior and indicators of mental health in school-aged children and adolescents:A systematic review. Prev Med. 2015;76:48–57. doi: 10.1016/j.ypmed.2015.03.026. [DOI] [PubMed] [Google Scholar]
- 45.Liu Q, Zhou Y, Xie XY, Xue Q, Zhu KH, Wan ZH, et al. The prevalence of behavioral problems among school-aged children in home quarantine during the COVID-19 pandemic in China. J Affect Disord. 2021;279:412–6. doi: 10.1016/j.jad.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Babic MJ, Smith JJ, Morgan PJ, Eather N, Plotnikoff RC, Lubans DR. Longitudinal associations between changes in screen-time and mental health outcomes in adolescents. Ment Health Phys Act. 2017;12:124–31. [Google Scholar]
- 47.Gupta P, Shah D, Bedi N, Galagali P, Dalwai S, Agrawal S, et al. Indian Academy of Pediatrics Guidelines on screen time and digital wellness in infants, children and adolescents. Indian Pediatr. 2022;59:235–44. [PubMed] [Google Scholar]
- 48.Elhai JD, McKay D, Yang H, Minaya C, Montag C, Asmundson GJ. Health anxiety related to problematic smartphone use and gaming disorder severity during COVID-19:Fear of missing out as a mediator. Hum Behav Emerg Technol. 2021;3:137–46. doi: 10.1002/hbe2.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yuan G, Elhai JD, Hall B. The influence of depressive symptoms and fear of missing out on severity of problematic smartphone use and Internet gaming disorder among Chinese young adults:A three-wave mediation model. Addict Behav. 2021;112:106648. doi: 10.1016/j.addbeh.2020.106648. [DOI] [PubMed] [Google Scholar]
- 50.Wang C-Y, Wu Y-C, Su C-H, Lin P-C, Ko C-H, Yen J-Y. Association between Internet gaming disorder and generalized anxiety disorder. J Behav Addict. 2017;6:564–71. doi: 10.1556/2006.6.2017.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.King DL, Delfabbro PH, Billieux J, Potenza MN. Problematic online gaming and the COVID-19 pandemic. J Behav Addict. 2020;9:184–6. doi: 10.1556/2006.2020.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fitzpatrick KM, Harris C, Drawve G. Living in the midst of fear:Depressive symptomatology among US adults during the COVID-19 pandemic. Depress Anxiety. 2020;37:957–64. doi: 10.1002/da.23080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kondo Y, Tanabe T, Kobayashi-Miura M, Amano H, Yamaguchi N, Kamura M, et al. Association between feeling upon awakening and use of information technology devices in Japanese children. J Epidemiol. 2012;22:12–20. doi: 10.2188/jea.JE20110019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Subki AH, Alsallum MS, Alnefaie MN, Alkahtani AM, Almagamsi SA, Alshehri ZS, et al. Pediatric motor stereotypies:An updated review. J Pediatr Neuroradiol. 2017;15:151–6. [Google Scholar]
- 55.Elhai JD, Levine JC, Hall BJ. The relationship between anxiety symptom severity and problematic smartphone use:A review of the literature and conceptual frameworks. J Anxiety Disord. 2019;62:45–52. doi: 10.1016/j.janxdis.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 56.Lee Y-S, Joo JH, Shin J, Nam CM, Park E-C. Association between smartphone overdependence and generalized anxiety disorder among Korean adolescents. J Affect Disord. 2023;321:108–13. doi: 10.1016/j.jad.2022.10.018. [DOI] [PubMed] [Google Scholar]
- 57.Sanders T, Parker PD, del Pozo-Cruz B, Noetel M, Lonsdale C. Type of screen time moderates effects on outcomes in 4013 children:Evidence from the longitudinal study of Australian children. Int J Behav Nutr Phys Act. 2019;16:1–10. doi: 10.1186/s12966-019-0881-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.KWB. Using social media to our advantage:Alleviating anxiety during a pandemic. Cyberpsychol Behav Soc Netw. 2020;23:197–8. doi: 10.1089/cyber.2020.29180.bkw. [DOI] [PubMed] [Google Scholar]
- 59.Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, Simoes-e-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct. 2020;51:101845. doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]