Abstract
Purpose:
In 2013, age restrictions for adolescents on over-the-counter access were removed for “Plan B One-Step”, a single oral medication option for emergency contraception use. Restrictions on generic options of the emergency contraceptive pill (ECP) were removed in 2014.
Methods:
National Survey of Family Growth data were used to assess the prevalence of ever use of ECPs among sexually experienced female adolescents and young adults (AYA) aged 15–24 years (2015–2017 sample), and trends in indicators of ECP use and acquisition (2006–2017 samples). Prevalence estimates were obtained by age subgroups for 15–17, 18–19, and 20–24 years. Statistical significance was determined using an alpha of .05 and 95% confidence intervals calculated around the point estimates.
Results:
The weighted estimate of sexually experienced female AYA in the United States ranged from 13.3 million in 2006–2008 to 12.7 million in 2015–2017. The prevalence of ever ECP use was 18.2% (95% CI 15.7–21.1) and 31.8% (95% CI 26.9–37.1) in 2006–2008 and 2015–2017, respectively. Ever use in 2015–2017 varied by age group, number of lifetime opposite-sex partners and abortions, and experience of nonconsensual sex. In 2008–2010, 46.1% (95% CI 36.0–56.5) of respondents last obtained ECPs at community health or family planning clinics, and 31.8% (95% CI 22.9–42.2) last obtained ECPs at a pharmacy compared to 18.1% (95% CI 12.0–26.4) and 70.1% (95% CI 60.6–78.1) respectively in 2015–2017. Prevalence of provider counseling about emergency contraception in female AYA regardless of prior sexual experience in the past 12 months remained at or below 5% from 2006 to 2017.
Conclusion:
Increasing access to ECPs over-the-counter may have contributed to notable increases in reported ever use of ECPs and in the receipts from a pharmacy among AYA between 2006 and 2017. AYA may benefit if pharmacists and healthcare providers increase reproductive health counseling.
Keywords: Adolescent health, Young adult health, Emergency contraception, Hormonal contraception
The United States (U.S.) Food and Drug Administration approved the first oral emergency contraception (EC) method (“Plan B” in 1999 for use by prescription [1–3]. In the U.S., EC includes various forms of oral hormonal medications, including single medication pills containing only levonorgestrel or progestin (available as “Plan B One-Step,” “Take Action,” “Next Choice One Dose,” and “My Way”), combined medication pills (available by prescription as multiple doses of certain combined hormonal contraceptives) and ulipristal acetate pills (“Ella,” available by prescription), as well as the copper intrauterine device (IUD) (available with a medical procedure) [1,4,5].
EC can play a role in preventing unintended pregnancies when another contraceptive method is not used, or there is concern about method failure [1,4,5], and EC is included in the recommended treatments after a sexual assault [6]. However, the effectiveness of EC is related to the timing of use; single medication emergency contraceptive pill (ECP) options are levonorgestrel pills, labeled for use as soon as possible within 72 hours following unprotected intercourse, and ulipristal acetate within 120 hours; in addition, a copper IUD can be placed within 5 days of unprotected intercourse [1,4–6]. Efforts have been made to increase access to ECP [1–4,7]. In 2006, single medication options containing levonorgestrel were authorized for sale over-the-counter (OTC) for women ages 18 and older [1]. In 2009, the age at purchase for ECP was reduced to age 17, and in 2013, all age or point-of-sale restrictions for Plan B One-Step were removed, with the remaining age restrictions on generic options removed in 2014 [1–3].
Prior studies have examined the use of and counseling for EC among adolescent and young adults (AYA) (aged 15–24 years) [8–11], looked at trends in the urban-rural divide of EC use [12], and reported changes in EC use from 2008 to 2015 [13]. However, there does not seem to have been an examination of trends in ECP use among AYA with a particular focus on the location of purchase since age restrictions to OTC access were sequentially removed from 2006. The goal of this analysis is to explore population-based prevalence estimates in EC-related indicators from 2006 to 2017 among AYA and examine trends in ever use and location of acquisition of ECPs.
Methods
We used data from the National Survey of Family Growth (NSFG), a nationally representative continuous survey of noninstitutionalized women aged 15–44 years in U.S. households, with later additions, including a survey of men aged 15–44 years. Respondents complete face-to-face interviews, with some data collection utilizing computer-assisted personal interviewing. Data are released in 2-year periods. Further details on the survey design, operations, weighting, and variance estimation are available [14].
Using 2015–2017 survey data, we examined prevalence in 2015–2017 of reports of ever ECP use and characteristics of AYA who reported ECP use among sexually experienced (defined as ever having had sexual intercourse with a male partner) females aged 15–24 years. For our measure of ever use, we used the responses to the question: “Have you ever used emergency contraception, also known as ‘Plan B’, ‘Preven’, ‘Ella’, ‘Next Choice’, or ‘Morning after’ pills?” (From 2006 onward, this question added options as additional methods became available). Among sexually experienced AYA, we examined associations between ever use and demographic characteristics, sexual history and pregnancy history. We chose baseline demographic variables and additional variables closely related to sexual history, sexual activity and pregnancy history given our focus on EC. Demographic variables included respondent’s age (15–17,18–19, 20–24 years), race/ethnicity (Hispanic, non-Hispanic white single race, non-Hispanic black single race, and non-Hispanic Other or multiple race [includes American Indian or Alaska Native, Asian, or Pacific Islander]; classification based on 1997 OMB guidelines as collected and recoded by NSFG), percent of poverty level (≤200%, >200%), marital/living status (has ever married or cohabited vs. never married or cohabited), and current health insurance (private [includes Medigap], public [includes Medicaid, Medicare, CHIP, state-sponsored, military health, Indian Health Service, single-service plan or other government healthcare], and no insurance). Sexual history variables included age at first sexual intercourse (<15 years or 15 years and older), number of lifetime partners, any contraceptive method used at last sex in past 12 months, and infrequent sexual activity (respondents who reported “yes” to the question: were there “times when you were not having intercourse with a male at all for one month or more”). Nonconsensual sex was assessed among participants 18 and older using the question: “Have you ever been forced by a male to have vaginal intercourse against your will?” Pregnancy history questions assessed were the number of pregnancies, number of live births, and number of abortions.
We examined the prevalence of indicators of ECP use and acquisition in 2006–2008, 2008–2010, 2011–2013, 2013–2015, and 2015–2017 using the NSFG survey data of 2006–2010, 2011–2013, and 2013–2017. Specific measures included ever ECP use, frequency of use, reasons for use, the last place ECP was obtained, whether a prescription was used, and counseling for ECP. Among those who reported use, we examined responses to questions about the frequency of lifetime use of any EC method (one, two, three, or more times), whether use occurred in the previous 12 months and the reason for use. To assess the latter, respondents who had used ECP were asked, “Did you use emergency contraception because you were worried your birth control method would not work, you did not use birth control that time, or for some other reason?”; up to three responses per respondent were allowed. Where ECP was most recently obtained from was first asked in 2007 and revised to its final version in 2008. Therefore, from 2008 onward, we examined where ECP was most recently obtained from, grouping responses into private care clinic (private doctor’s office, HMO facility, employer or company clinic), community health clinic (community health clinic, community clinic, public health clinic), family planning clinic (family planning or Planned Parenthood clinic), pharmacy or drug store, and other (consisting of school or school-based clinic, hospital or urgent care center, friend, partner or spouse, or mail order/internet). Whether ECP was most recently obtained by prescription was first asked in the 2008–2010 cycle, so from the 2008–2010 cycle onward we assessed whether the most recent ECP was obtained with or without a prescription.
To measure the receipt of recent ECP counseling, we examined responses to a question for all female AYA regardless of the report of sexual activity or report of ECP use or visit to a healthcare provider in the past 12 months.: “In the past 12 months, have you received counseling or information about emergency contraception, also known as ‘Plan B’, or the ‘Morning-after pill’?”. To measure receipt of ECP counseling in male AYA who had a visit to a doctor or healthcare provider in the past 12 months, we assessed responses to the following question: “During your visit in the past 12 months, did a doctor or healthcare provider talk with you about emergency contraception?” Counseling question to male AYA was included from 2011 to 2017.
To account for the multistage, probability-based complex survey design of NSFG, we used SAS and SAS-callable SUDAAN Version 9.3. NSFG-provided survey sampling weights were used to obtain estimates representative of AYA in U.S. households. For example, for the 2015–2017 survey data, we used the variable WGT2015_2017 as the weight. Chi-squared tests were performed to assess the homogeneity of distribution across each of the population characteristics, sexual history, and pregnancy history categories. We assessed linear and quadratic trends across time for two primary variables of interest related to the use and acquisition of ECPs: ever ECP use and location of most recent ECP acquisition, using the weighted least squares method. If the quadratic term was significant, then p values for both the linear and quadratic terms were reported. However, if the quadratic term was not significant, a reduced model, including only the linear term, was fit, and only the linear p value was reported. Statistical significance was determined using an alpha of .05. Since this analysis used deidentified data, the Centers for Disease Control and Prevention deemed this study to be research not involving human subjects and therefore did not need review by an institutional review board.
Results
The weighted estimate of the total number of sexually experienced female AYA in United States in the 2015–2017 sample was 12,711,422, and it represented 64.8% (95% confidence interval [CI] 60.7–68.6) of all female AYA in that sample (Table 1). Of these sexually experienced female AYA, 9.9% (95% CI 7.0–13.9) were aged 15–17 years, 21.3% (95% CI 16.7–26.7) were aged 18–19 years, and 68.8% (95% CI 62.3–74.6) were aged 20–24 years; 49.9 (95% CI 42.4–57.4) self-reported as non-Hispanic white, single race, 23.8% (95% CI 17.7–31.2) self-reported as Hispanic, 15.8% (95% CI 11.8–20.8) self-reported as non-Hispanic black, single race, and 10.5% (95% CI 7.5–14.5) self-reported as non-Hispanic other or multiple races; 51.9% (95% CI 46.2–57.6) had never married or co-habited; and 81.2% (95% CI 76.1–85.3) had used a contraceptive at last sex; additional characteristics are in Table 1.
Table 1.
Characteristics of sexually experienced females aged 15–24 years and ever use of emergency contraception from the National Survey of Family Growth, 2015–2017
| Characteristic | Unweighted n = 1029 | Ever used emergency contraception pills | ||
|---|---|---|---|---|
|
|
|
|||
| Weighted total | % Of total | Prevalence (95% CI) | p valuea | |
|
| ||||
| Total | 12,711,422 | 100 | 31.8 (26.9–37.1) | |
| Age group | <.001 | |||
| 15–17 years | 1,262,623 | 9.9 (7.0–13.9) | 14.0 (7.6–24.2) | |
| 18–19 years | 2,707,406 | 21.3 (16.7–26.7) | 21.2 (14.0–30.9) | |
| 20–24 years | 8,741,393 | 68.8 (62.3–74.6) | 37.6 (32.0–43.6) | |
| Race/ethnicity | 0.1 | |||
| Hispanic | 3,027,834 | 23.8 (17.7–31.2) | 44.0 (32.5–56.1) | |
| Non-Hispanic white, Single Race | 6,340,0612 | 49.9 (42.4–57.4) | 29.5 (23.9–35.9) | |
| Non-Hispanic black, Single Race | 010,097 | 15.8 (11.8–20.8) | 21.9 (14.6–31.3) | |
| Non-Hispanic Other or Multiple Raceb | 1,333,430 | 10.5 (7.5–14.5) | 29.6 (15.2–49.6) | |
| Percent of poverty level | 0.4 | |||
| ≤ 200 | 7,109,3375 | 55.9 (50.6–61.1) | 30.3 (23.7–37.8) | |
| >200 | 602,086 | 44.1 (38.9–49.4) | 33.7 (28.1–39.6) | |
| Marital status | .07 | |||
| Ever married or cohabited | 6,112,659 | 48.1 (42.4–53.9) | 35.7 (29.3–42.7) | |
| Never married or cohabited | 6,598,764 | 51.9 (46.2–57.6) | 28.09 (22.2–34.9) | |
| Current health insurancec | .17 | |||
| Private | 6,304,608 | 49.6 (43.5–55.7) | 32.1 (26.5–38.4) | |
| Public | 4,382,790 | 34.5 (28.7–40.7) | 26.7 (20.6–33.8) | |
| No insurance | 2,024,025 | 15.9 (12.4–20.2) | 41.7 (27.4–57.6) | |
| Age at first sexual intercourse | .81 | |||
| Less than 15 years old | 2,093,691 | 16.5 (13.2–20.4) | 33.1 (21.9–46.6) | |
| 15 years old or older | 10,617,731 | 83.5 (79.6–86.8) | 31.5 (26.6–36.9) | |
| Used contraception at last sex | .17 | |||
| Yes | 9,676,235 | 81.2 (76.1–85.3) | 34.4 (28.8–40.4) | |
| No | 2,247,003 | 18.9 (14.7–23.9) | 26.6 (17.8–37.7) | |
| Lifetime opposite-sex partners, n | <.001 | |||
| 1 | 3,160,366 | 24.9 (21.5–28.6) | 13.1 (8.4–19.9) | |
| 2 | 1,772,209 | 13.9 (11.0–17.5) | 25.8 (17.0–37.2) | |
| 3+ | 7,778,847 | 61.2 (57.0–65.3) | 40.7 (33.7–48.1) | |
| Number of pregnancies | .084 | |||
| 0 | 8,212,207 | 64.6 (59.8–69.2) | 30.7 (24.1–38.2) | |
| 1 | 2,539,814 | 20.0 (16.9–23.4) | 25.9 (17.9–35.9) | |
| 2+ | 1,959,402 | 15.4 (12.4–19.1) | 44.0 (33.1–55.5) | |
| Number of live births | .91 | |||
| 0 | 956,988 | 22.9 (16.6–30.6) | 35.9 (21.8–52.9) | |
| 1 | 2,224,915 | 53.1 (44.9–61.2) | 36.4 (26.3–47.9) | |
| 2+ | 1,007,081 | 24.0 (18.0–31.3) | 32.4 (19.0–49.3) | |
| Number of abortions | .04 | |||
| 0 | 3,474,020 | 82.9 (75.3–88.6) | 29.7 (21.9–38.9) | |
| 1 | 646,832 | 15.4 (9.8–23.5) | 61.8 (40.0–79.8) | |
| 2+ | 68,131 | 1.6 (.6–4.2) | 71.6 (27.1–94.5) | |
Chi-square.
Non-Hispanic Other includes American Indian or Alaska Native, Asian, or Pacific Islander.
Private includes Medigap; public includes Medicaid, Medicare, CHIP, state-sponsored, military health, Indian Health Service, single-service plan or other government healthcare.
In 2015–2017, 31.8% (95% CI 26.9–37.1) of sexually experienced AYA females reported ever using ECPs (Table 1). Prevalence of ever ECP use varied significantly by age, number of lifetime opposite-sex partners, number of abortions, and experience of nonconsensual sex. By age, 14.0% (95% CI 7.6–24.2), 21.2% (95% CI 14.0–30.9), and 37.6% (95% CI 32.0–43.6) of 15–17, 18–19, and 20–24-year-old sexually experienced females had ever used ECP, respectively (Table 1). Ever ECP use increased with the increasing number of lifetime opposite-sex partners (Table 1). The prevalence of ever ECP use was 29.7% (95% CI 21.9–38.9) for those reporting no abortions, 61.8% (95% CI 40.0–79.8) for those reporting one abortion, and 71.6% (95% CI 27.1–94.5) for those reporting more than one abortion. Among AYA females aged 18 years and older who had experienced nonconsensual sex, 52.5% (95% CI 38.5–66.1) had ever used ECP compared to 30.7% (95% CI 25.6–36.4) who had not. However, there were no differences in ever ECP use by frequency of sexual activity. Infrequent sexual activity was defined as times when an AYA female was not having intercourse with a male at all, for one month or more in the past 3 years, or since the date of first sex. One-third of female AYA with infrequent sexual activity reported ever ECP use (33.4%, 95% CI 27.3–40.1), similar to the prevalence of ECP use among those reporting frequent sexual activity (27.0%, 95% CI 20.1–35.1). There were no differences by the number of pregnancies or live births (Table 1).
The weighted estimate of sexually experienced female AYA in the United States ranged from 13.3 million in 2006–2008 to 12.7 million in 2015–2017 (Table 2). Percentage of sexually experienced female AYA among all female AYA was 64.4% (95% CI 60.5–68.2), 65.6% (95% CI 61.9–69.1), 65.9 (95% CI 62.0–69.6), 65.7 (95% CI 62.5–68.7), and 64.8% (95% CI 60.7–68.6) in 2006–2008, 2008–2010, 2011–2013, 2013–2015 and 2015e2017 respectively. Reported ever ECP use among sexually experienced female AYA increased from 18.2% (95% CI 15.7–21.1) in 2006–2008 to 31.8% (95% CI 26.9–37.1) in 2015–2017 (p value for linear trend<.001) (Table 2 and Figure 1). Trends stratified by age were also significant. The largest increase occurred in the 20–24 year age group (p < .001) (Figure 1), with an increase from 21.2% to 37.6%. Among 15–17-year-olds, ever use increased from 8.9% to 14.0% (p = .021), and among 18–19-year-olds ever use increased from 14.4% to 21.2% (p = .009). Prevalence of past year ECP use among ever EC users in 15–24-year-olds was 34.9% (95% CI 25.7–42.9) and 41.3% (95% CI 35.0–47.9) in 2008–2010 and 2015–2017, respectively (Table 2); estimates over time and by age in the frequency of use is shown in Table A1.
Table 2.
Emergency contraceptive (EC) use (ever use), recent use, receipt by prescription, and the reason for obtaining contraceptive services among sexually experienced females ages 15–24, from the National Survey of Family Growth (NSFG), 2006–2017
| NSFG cycle | 2006–2008 | 2008–2010 | 2011–2013 | 2013–2015 | 2015–2017 |
|---|---|---|---|---|---|
| Unweighted | n = 1386 | n = 1534 | n = 1334 | n = 1252 | n = 1029 |
| Weighted | N = 13,339,969 | N = 13,656,123 | N = 13,104,328 | N = 13,064,617 | N = 12,711,422 |
| Characteristic, prevalence (95% CI) | |||||
| Ever used ECa | |||||
| 15–24 yearsb | 18.2 (15.7–21.1) | 21.1 (17.5–25.3) | 29.4 (25.5–33.6) | 30.7 (26.8–34.9) | 31.8 (26.9–37.1) |
| 15–17 yearsb | 8.9 (5.6–13.7) | 6.5 (3.5–11.8) | 14.5 (8.2–24.4) | 20.6 (13.0–31.0) | 14.0 (7.6–24.3) |
| 18–19 yearsb | 14.4 (10.5–19.5) | 18.3 (12.6–25.7) | 26.2 (18.6–35.6) | 25.6 (18.6–34.2) | 21.2 (14.0–30.9) |
| 20–24 yearsb | 21.2 (18.1–24.7) | 24.6 (20.3–29.6) | 33.2 (28.4–38.3) | 33.6 (29.1–38.5) | 37.6 (32.0–43.6) |
| Among ever EC users, use in the previous 12 months | |||||
| 15–24 years | c | 34.9 (27.7–42.9) | 33.0 (26.9–39.7) | 39.8 (33.5–46.4) | 41.3 (35.0–47.9) |
| 15–17 years | 57.6 (26.9–83.3) | 65.6 (40.1–84.4) | 56.9 (28.4–81.5) | 63.2 (35.2–84.4) | |
| 18–19 years | 45.4 (25.9–66.4) | 39.1 (24.0–56.6) | 56.6 (37.9–73.5) | 53.6 (28.6–76.9) | |
| 20–24 years | 31.1 (22.9–40.5) | 28.7 (21.9–36.8) | 34.8 (27.5–42.9) | 37.9 (29.6–47.0) | |
| Reason for using ECd | |||||
| Was worried birth control method would not work | |||||
| 15–24 years | 45.8 (37.4–54.5) | 43.1 (35.1–51.5) | 38.9 (31.3–47.2) | 38.8 (31.6–46.5) | 36.8 (27.8–47.0) |
| 15–17 years | 14.1 (5.0–34.0) | 33.5 (10.6–68.1) | 17.3 (6.3–39.5) | 34.0 (15.4–59.5) | 20.0 (7.4–43.9) |
| 18–19 years | 30.5 (14.8–52.5) | 41.5 (27.2–57.4) | 35.0 (19.0–55.3) | 28.2 (16.8–43.3) | 44.5 (22.6–68.9) |
| 20–24 years | 51.6 (40.3–62.8) | 44.0 (35.2–53.1) | 41.6 (32.8–51.1) | 41.4 (33.2–50.0) | 36.4 (27.4–46.5) |
| You did not use birth control that time | |||||
| 15–24 years | 47.2 (38.9–55.6) | 50.9 (43.3–58.5) | 46.8 (38.7–55.1) | 45.9 (38.2–53.9) | 51.6 (40.9–62.0) |
| 15–17 years | 58.1 (38.4–75.5) | 51.2 (22.8–78.9) | 43.9 (17.4–74.4) | 44.0 (18.0–73.8) | 75.9 (53.3–89.7) |
| 18–19 years | 45.6 (26.6–66.1) | 46.9 (32.1–62.4) | 49.3 (30.6–68.3) | 42.3 (26.4–59.9) | 30.9 (17.2–48.9) |
| 20–24 years | 46.6 (36.4–57.1) | 52.0 (43.4–60.4) | 46.5 (37.1–56.1) | 46.9 (38.3–55.6) | 53.9 (42.3–65.0) |
| Other reason | |||||
| 15–24 years | 12.3 (7.8–19.0) | 12.9 (9.0–18.2) | 24.5 (18.1–32.4) | 19.5 (13.9–26.6) | 18.5 (10.8–29.9) |
| 15–17 years | 27.8 (11.8–52.6) | 27.3 (8.3–60.8) | 38.8 (16.9–66.4) | 22.0 (9.3–43.5) | 12.1 (3.5–34.4) |
| 18–19 years | 23.9 (10.7–45.1) | 23.9 (12.9–39.8) | 32.5 (15.9–55.2) | 30.7 (16.1–50.6) | 24.6 (9.7–49.8) |
| 20–24 years | 8.6 (4.4–16.2) | 9.4 (6.3–13.8) | 21.5 (14.8–30.1) | 17.0 (11.6–24.2) | 17.8 (10.2–29.1) |
| Got EC with prescriptiond | |||||
| 15–24 years | c | 20.5 (16.0–26.0) | 16.5 (10.6–24.7) | 13.3 (9.3–18.7) | 10.5 (5.8–18.1) |
| 15–17 years | 23.3 (8.2–50.8) | 18.5 (4.9–50.3) | 23.8 (5.6–62.2) | 9.6 (3.1–26.3) | |
| 18–19 years | 13.1 (6.1–25.9) | 12.5 (6.3–23.5) | 8.7 (3.8–18.5) | 19.5 (3.1–64.6) | |
| 20–24 years | 22.4 (16.6–29.5) | 17.2 (10.0–28.0) | 13.3 (9.3–18.7) | 8.9 (5.4–14.5) |
For Ever EC use, we used the weighted least squares method to assess linear and quadratic trends across time. If the quadratic term was significant, then p values for both the linear and quadratic terms were reported. However, if the quadratic term was not significant, a reduced model, including only the linear term, was fit, and only the linear p value was reported.
p (linear) < .01.
Data are missing for approximately half of the EC ever used observations during this cycle because this question was asked starting year two of the 2006–2008 data cycle.
The question asked of the respondent was: “Did you use emergency contraception because you were worried your birth control method would not work, you did not use birth control at that time, or for some other reason?” Up to three reasons could be chosen. This question was asked to respondents who had ever used EC.
Figure 1.
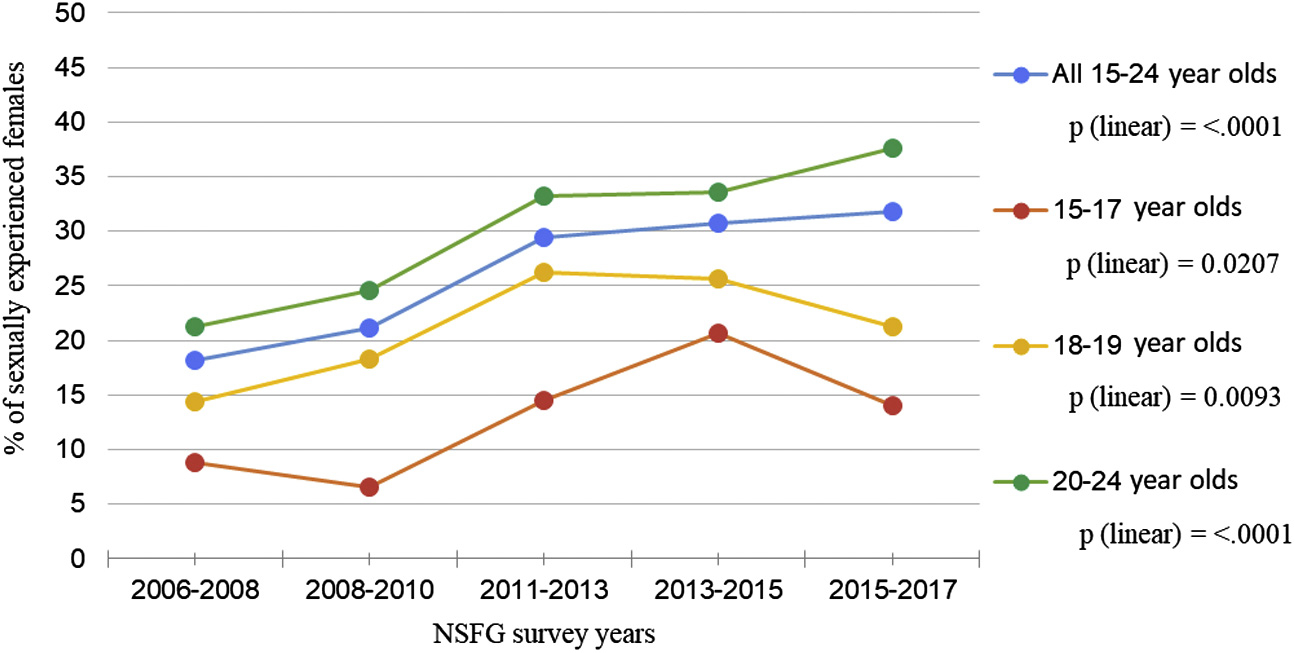
Prevalence of ever use of emergency contraceptive pills among sexually experienced adolescents (15–17-year-olds, 18–19-year-olds) and young adult females (20–24-year-olds) from the National Survey of Family Growth, by age group, 2006–2017.
In 2008–2010, 46.1% (95% CI 36.0–56.5) of AYA ECP users last obtained ECP at community health or family planning clinics, and in 2015–2017 that proportion was 18.1% (95% CI 12.0–26.4) (p value for linear trend <.001) (Figure 2, Table A2). Over the same time period, the proportion of AYA ECP users who last obtained ECP at a pharmacy or drug store increased from 31.8% (95% CI 22.9–42.2) to 70.1% (95% CI 60.6–78.1) (p value for linear trend<.0001). These trends were observed across all three age groups (Figure 2A–C). For example, the proportion of adolescent ECP users aged 15–17 years who most recently obtained ECP from a pharmacy or drug store increased from 8.8% (95% CI 1.5–37.6) in 2008–2010 to 53.0% (95% CI 28.0–76.5) in 2015–2017 (p value for linear trend = .0008) (Figure 2A, Table A2). In 2008–2010, the proportion of AYA ECP users who reported obtaining their most recent ECP by prescription was 20.5% (95% CI 16.0–26.0), and in 2015–2017 it was 10.5% (95% CI 5.8–18.1). In contrast to the changes over time for ever use and location of acquisition, no apparent changes were noted in the reasons for use over the same period (Table 2)
Figure 2.
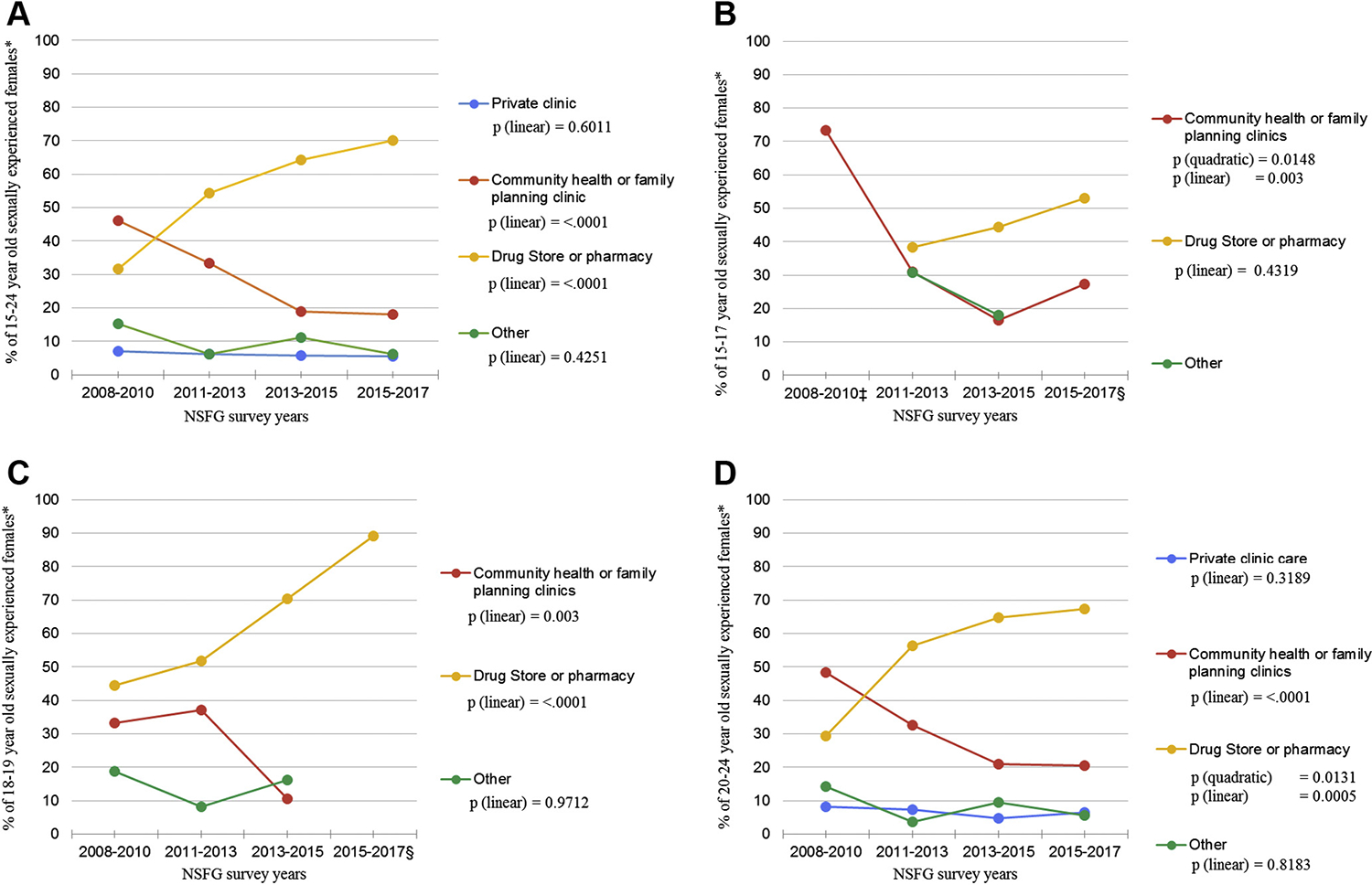
(A) Location of most recent emergency contraceptive pill (ECP) receipt among adolescent and young adult females aged 15–24 years who had used ECP from the National Survey of Family Growth, overall and by age group, 2008–2017. *who had used ECP. (B) Location of most recent ECP receipt among 15- to 17-year olds. *who had used ECP; ‡ Prevalence for Drug Store or pharmacy and Other for 2008–2010 do not meet National Center for Health Statistics standards of reliability as mentioned in the ‘2015–2017 NSFG User’s Guide, Appendix 6: Frequently Asked Questions (FAQ) about the NSFG’. § Prevalence for Other for 2015–2017 does not meet National Center for Health Statistics standards of reliability. (C) Location of most recent ECP receipt among 18- to 19-year olds. *who had used ECP; § Prevalence for Community health or family planning clinics and Other for 2015–2017 do not meet National Center for Health Statistics standards of reliability. (D) Location of most recent ECP receipt among 20- to 24-year olds. *who had used ECP.
In 2006–2008 and 2015–2017, the percentage of all AYA females (those with and without sexual experience) reporting counseling or information about EC in the past 12 months was 5.0% (95% CI 3.9–6.5) and 3.7% (95% CI 2.3–5.7), respectively (Table 3). Percentage of AYA males reporting discussion about EC during a visit to a healthcare provider in the past 12 months (Table 3) was 7.7% (95% CI 5.8–10.2) in 2011%–2013% and 10.1% (95% CI 7.9–13.0) in 2015–2017.
Table 3.
Reports of counseling or information about emergency contraception (EC) in the past 12 months from females aged 15–24 years in 2006–2008, 2008–2010, 2011–2013, 2013–2015, and 2015–2017 and reports of talk of EC during a visit to a healthcare provider in the past 12 months from males aged 15–24 years in 2011–2013, 2013–2015, and 2015–2017
| Percentage of adolescent or young adult femalesa reporting counseling or information about EC in the past 12 months | |||||
|---|---|---|---|---|---|
|
| |||||
| Prevalence (95% CI) | |||||
|
|
|||||
| 2006–2008 N = 20,702,261 |
2008–2010 N = 20,823,440 |
2011–2013 N = 19,885,434 |
2013–2015 N = 19,898,507 |
2015–2017 N = 19,630,924 |
|
|
| |||||
| 15–24 years | 5.0 (3.9–6.5) | 5.3 (3.6–7.7) | 4.5 (3.3–6.1) | 5.3 (4.1–6.8) | 3.7 (2.3–5.7) |
| 15–17 years | 2.9 (1.8–4.6) | 3.5 (2.0–6.0) | 2.6 (1.5–4.8) | 3.4 (2.0–5.6) | 3.4 (.9–12.4) |
| 18–19 years | 6.0 (4.0–9.1) | 5.3 (3.4–8.1) | 6.8 (4.3–10.7) | 3.4 (2.1–5.4) | 2.5 (1.3–4.9) |
| 20–24 years | 5.8 (4.1–8.1) | 6.4 (4.0–10.1) | 4.6 (3.0–7.2) | 7.0 (4.9–10.0) | 4.3 (2.9–6.2) |
|
| |||||
| Percentage of adolescent or young adult malesb reporting talk of EC during a visit to a healthcare provider in the past 12 months | |||||
|
| |||||
| NA | NA | 2011–2013 N = 15,025,899 |
2013–2015 N = 15,466,588 |
2015–2017 N = 15,112,821 |
|
|
| |||||
| 15–24 years | 7.7 (5.8–10.2) | 7.1 (5.2–9.6) | 10.1 (7.9–13.0) | ||
| 15–17 years | 4.74 (2.9–7.6) | 5.3 (3.7–7.6) | 6.9 (4.4–10.7) | ||
| 18–19 years | 11.8 (7.7–17.6) | 8.0 (4.8–13.1) | 12.5 (8.2–18.7) | ||
| 20–24 years | 7.9 (5.3–11.8) | 8.1 (5.0–12.9) | 11.4 (7.8–16.3) | ||
Among all 15–24-year-old female respondents, regardless of prior sexual experience or visit to a healthcare provider in the past 12 months.
Among all 15–24-year-old male respondents who visited a healthcare provider in the past 12 months, regardless of prior sexual experience.
In 2013–2015, the proportion of female AYA aged 18–24 years who had experienced nonconsensual sex was 19.5% (95% CI 16.3–23.0), and in the 2015–2017 sample, it was 19.4% (95% CI 15.3–24.2). Among these AYA, the proportion who had ever used ECP in 2013–2015 was 43.9% (95% CI 36.6–51.4), and in 2015–2017 was 49.4% (95% CI 36.8–62.1).
Discussion
From 2006–2008 to 2015–2017, reported ever use of ECPs increased by 74.7% among AYA aged 15–24 years. These increases were not accompanied by the increased receipt of EC counseling, which might occur during routine health visits, or by increases in nonconsensual sex, an indication for EC use. The use of other contraceptive methods among this age group also increased around this same period, but not as markedly, with the exception of long-acting emergency contraceptive (LARC) methods [15,16]. During this same period, AYA increasingly reported obtaining ECP from pharmacies or drug stores (from 31.8% in 2008–2010 to 70.1% in 2015–2017). Concomitantly, since 2008, fewer AYA reported having last obtained ECPs from a community health or family planning clinic (from 46.1% in 2008–2010 to 31.8% (2015–2017). These findings may reflect the elimination of FDA age and point-of-sale restrictions to OTC access to some ECP while also allowing for a decreased burden of stigma and embarrassment associated with its acquisition [13].
A potential unintended consequence of the shift from clinics to pharmacies as the primary location of acquiring ECP may be fewer opportunities for contraceptive counseling from providers [1,13]. Reported past year receipt of counseling on ECPs among female AYA during the study period appeared to remain stable albeit low (ranging from 4% to 5%). Prior studies have found AYA females rely on a mix of Ob-Gyn, family physicians, and pediatricians as their main healthcare providers, and that in some estimates, only about half of the pediatricians regularly provide reproductive health services to patients [17]. These findings underscore the need for counseling about the full range of contraceptive options by healthcare providers, particularly pediatricians, during routine healthcare visits for adolescent females and males [5,18–20]. This is in line with American College of Obstetricians and Gynecologists (ACOG) guidelines recommending that contraceptive counseling, including routine discussion of ECP and provision of advance prescriptions for ECPs, should not be based on patients’ prior sexual activity [21]. Expansion of provider knowledge through training to increase comfort discussing contraceptive topics with AYA, including current OTC status of ECP and other options, if available, may facilitate increased counseling [22]. Training and comfort on contraceptive topics could also enhance clinical providers’ ability to assess sensitive social topics and respond to patients’ sexual and reproductive health questions.
Retail settings may also offer additional venues to increase contraceptive counseling for ECP methods. In states that are providing direct access to hormonal contraception via pharmacists, the infrastructure needed to provide contraception counseling for EC is likely in place, although reimbursement for counseling may be a challenge [23,24]. In states with and without these provisions, additional efforts may be required to implement EC counseling services for OTC ECP products but could include counseling and referral for continuous contraception with increased efficacy. Some states that have initiated access to oral contraceptive pills through pharmacies have included requirements for information and materials to accompany the provision of ECP [23,24].
Despite promising findings regarding increasing use of ECPs, which may be related to increasing acquisition in retail settings, challenges with access persist [25–29]. Pharmacies may misunderstand the FDA changes to age restrictions and vary in the level of in-store accessibility and counseling provided, found to be particularly harmful to low-income and minority communities [30–33]. Many young people may not be aware that these methods are available without a prescription, and awareness and access vary by age, race/ethnicity, socioeconomic status, foreign-born status, and urbanicity [25,27]. Cost may also be a barrier since OTC ECP coverage by Medicaid varies by state, and higher income levels have been found to be associated with higher rates of EC use [13,31]. While prescribed ECPs may be covered by private insurance, provision of reproductive health services may be reported to parent(s) or guardian(s) if they are the source of the insurance, potentially presenting confidentiality concerns for AYA ([34]).
Limitations of the current study include that significance testing for trends was conducted only for two indicators (time and age) related to ECP use and acquisition. This approach minimizes concerns about multiple comparisons but limits conclusions we can draw about changes over time for other variables. We did not evaluate the use of the copper IUD since the question about ECP does not address the use of the copper IUD for EC. Bivariate analysis between ever ECP use and characteristics of AYA who reported ECP use may be biased due to potential confounding. Also, for bivariate analyses, limited sample sizes reduced power to detect differences and interactions between ECP use, age, sexual behavior, and pregnancy-related characteristics. Additionally, biases exist from self-reporting to NSFG across all survey years. Because NSFG is a national sample, we were unable to evaluate state differences in ECP use, which may be affected by local laws and regulations.
In summary, findings suggest increased use of ever ECP use among sexually experienced adolescents and young adults and changes in where they obtain ECP from 2006–2008 to 2015–2017. Fewer report having last obtained ECP from community health or family planning clinics, and more purchased ECP at pharmacies or drug stores. Research on the implications of changes in receipt of ECP, and how to increase EC counseling among AYA are needed. Additional efforts, using existing tools that support youth-friendly, quality, confidential care (34), may be beneficial for training various healthcare providers that serve adolescents and young adults to provide information to their patients. Finally, ongoing analysis of ECP use may improve our understanding of its relationship to unintended pregnancy and birth rates among AYA.
Supplementary Material
IMPLICATIONS AND CONTRIBUTIONS.
From 2006 to 2017, sexually experienced adolescents and young adults reported increased use of emergency contraception, from 18.2% to 31.8%, and most reported last purchase from pharmacies and without a prescription; possibly reflecting the elimination of FDA age restrictions for adolescents on over-the-counter access to emergency contraception starting in 2013.
Acknowledgements
This work was completed as part of routine work conducted by government employees and a student fellow.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
Disclaimer: The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
Supplementary Data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jadohealth.2022.01.229.
References
- [1].Trussell J, Raymond EG, Cleland K. Emergency contraception: A last chance to prevent unintended pregnancy. Princeton University Office of Population Research. Princeton University. 2019. Available at: http://ec.princeton.edu/questions/ec-review.pdf. Accessed October 1, 2019. [Google Scholar]
- [2].“The Fight for emergency contraception: Every Second counts.” Center for Reproductive Rights. 2018. Available at: www.reproductiverights.org/emergency-contraception-timeline. Accessed October 1, 2019.
- [3].FDA’s Decision regarding plan B: Questions and Answers. Available at: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/fdas-decision-regarding-plan-b-questions-and-answers#:~:text=Emergency%20contraceptives%20contain%20the%20hormones%20estrogen%20and%20progestin,in%201998%29%20and%20Plan%20B%20%28approved%20in%201999%29. Accessed February 1, 2020.
- [4].Emergency contraception. Practice Bulletin No. 152. American College of Obstetricians and Gynecologists. Obstet Gynecol; 2015;126:e1–11. [DOI] [PubMed] [Google Scholar]
- [5].Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for contraceptive Use, 2016. MMWR Recomm Rep 2016;65:1–66. [DOI] [PubMed] [Google Scholar]
- [6].Centers for Disease Control and Prevention. Sexual assault and abuse and STDs. 2015 sexually Transmitted Diseases treatment guidelines. Atlanta (GA): CDC; 2015. [Google Scholar]
- [7].Upadhya KK AAP Committee on adolescence. Emergency contraception. Pediatrics 2019;144:e20193149. [DOI] [PubMed] [Google Scholar]
- [8].Abma JC, Martinez GM. In: Sexual activity and contraceptive use among teenagers in the United States, 2011–2015. National health statistics reports 2017; no 104. Hyattsville, MD: National Center for Health Statistics; 2018. [PubMed] [Google Scholar]
- [9].Liddon N, Steiner RJ, Martinez GM. Provider communication with adolescent and young females during sexual and reproductive health visits: Findings from the 2011–2015 national survey of family Growth. Contraception 2018;97:22–8. [DOI] [PubMed] [Google Scholar]
- [10].Kavanaugh ML, Williams SL, Schwarz EB. Emergency contraception use and counseling after changes in United States prescription status. Fertil Steril 2011;95:2578–81. [DOI] [PubMed] [Google Scholar]
- [11].Daniels K, Jones J, Abma J. Use of emergency contraception among women aged 15–44: United States, 2006–2010. NCHS data brief, no 112. Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- [12].Milkowski CM, Ziller EC, Ahrens KA. “Rural-urban Residence and emergency contraception Use, access, and counseling in the United States, 2006–2017”. Contraception 2021;X:100061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hussain R, Kavanaugh ML. Changes in use of emergency contraceptive pills in the United States from 2008 to 2015. Contracept X 2021;3:100065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Centers for Disease Control and Prevention 2011–2013 National Survey of Family Growth (NSFG): Summary of Design and Data Collection Methods. 2011–2013 NSFG: Public Use data Files, Codebooks, and Documentation. Available at: https://www.cdc.gov/nchs/data/nsfg/NSFG_2011_2013_DesignandDataCollectionMethods.pdf. Accessed June 1, 2019.
- [15].Branum AM, Jones J. Trends in long-acting reversible contraception use among U.S. women aged 15–44. NCHS data Brief 2015, no 188. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- [16].Daniels K, Daugherty J, Jones J, Mosher W. Current contraceptive use and variation by selected characteristics among women aged 15–44: United States, 2011–2013. National Health statistics reports 2015; no 86. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- [17].Jaccard J, Levitz N. Counseling adolescents about contraception: Towards the development of an evidence-based protocol for contraceptive counselors. J Adolesc Health 2013;52:S6–13. [DOI] [PubMed] [Google Scholar]
- [18].Health Care Providers and Teen Pregnancy Prevention. Available at: https://www.cdc.gov/teenpregnancy/health-care-providers/index.htm. Accessed January 28, 2020.
- [19].Gavin L, Moskosky S, Carter M, et al. Providing quality family planning services: Recommendations of CDC and the U.S. Office of population Affairs. Recommendations Rep 2014;63:1–29. [PubMed] [Google Scholar]
- [20].Potter J, Santelli JS. Contraceptive counseling for adolescents. Womens Health (Lond Engl) 2015;11:737–41. [DOI] [PubMed] [Google Scholar]
- [21].Committee Opinion No. 710: Counseling adolescents about contraception. Obstet Gynecol 2017;130:e74–80. [DOI] [PubMed] [Google Scholar]
- [22].Brittain AW, Loyola Briceno AC, Pazol K, et al. Youth-friendly family planning services for young people: A Systematic review update. Am J Prev Med 2018;55:725–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kooner M, Joseph H, Griffin B, et al. Hormonal contraception prescribing by pharmacists: 2019 update. J Am Pharm Assoc 2020:1544–3191. [DOI] [PubMed] [Google Scholar]
- [24].Emergency Contraception Protocol. Section 1746. California state board of pharmacy. Amended Eff 7–1-2013. Available at: https://www.pharmacy.ca.gov/publications/ec_protocol.pdf. Accessed October 1, 2019.
- [25].Wilkinson TA, Clark P, Rafie S, et al. Access to emergency contraception after removal of age restrictions. Pediatrics 2017;140:e20164262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Yen S, Parmar DD, Lin EL, Ammerman S. Emergency contraception pill awareness and knowledge in Uninsured adolescents: High rates of Misconceptions concerning indications for Use, Side Effects, and access. J Pediatr Adolesc Gynecol 2015;28:337–42. [DOI] [PubMed] [Google Scholar]
- [27].Moore A, Ryan S, Stamm C. Seeking emergency contraception in the United States: A review of access and barriers. Women Health 2019;59:364–74. [DOI] [PubMed] [Google Scholar]
- [28].Baldwin SB, Solorio R, Washington DL, et al. Who is using emergency contraception? Awareness and use of emergency contraception among California women and teens. Womens Health Issues 2008;18:360–8. [DOI] [PubMed] [Google Scholar]
- [29].Cleland K, Bass J, Doci F, Foster AM. Access to emergency contraception in the over-the-counter Era. Womens Health Issues 2016;26:622–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Rafie S, Stone RH, Wilkinson TA, et al. Role of the community pharmacist in emergency contraception counseling and delivery in the United States: Current trends and future prospects. Integr Pharm Res Pract 2017;6:99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Medicaid coverage of emergency contraceptives. 2015. Available at: https://www.kff.org/womens-health-policy/state-indicator/medicaid-coverage-of-emergency-contraceptives/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed December 7, 2020.
- [32].Qato DM, Alexander GC, Guadamuz JS, et al. Pharmacist-prescribed and over-the-counter hormonal contraception in Los Angeles county retail pharmacies. Health Aff (Millwood) 2020;39:1219–28. [DOI] [PubMed] [Google Scholar]
- [33].Stone RH, Rafie S, Ernest D, Scutt B. “Emergency contraception access and counseling in urban pharmacies: A comparison between states with and without pharmacist prescribing”. Pharmacy (Basel, Switzerland) 2020;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Brittain A, Williams JR, Zapata LB, et al. Confidentiality in family planning services for young people: A Systematic review. Am J Prev Med 2015;49:S85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


