Abstract
OBJECTIVES:
Recent studies document an association between mild traumatic brain injuries (mTBIs) in children and postinjury psychiatric disorders. However. these studies were subject to limitations in the design, lack of long-term follow-up, and poorly defined psychiatric outcomes. This study determines the incidence and relative risk of postinjury new affective and behavior disorders 4 years after mTBIs.
METHODS:
A cohort study of mTBI cases and matched comparisons within an integrated health care system. The mTBI group included patients ≤17 years of age, diagnosed with mTBI from 2000 to 2014 (N = 18 917). Comparisons included 2 unexposed patients (N = 37 834) per each mTBI-exposed patient, randomly selected and matched for age, sex, race/ethnicity, and date of medical visit (reference date to mTBI injury). Outcomes included a diagnosis of affective or behavioral disorders in the 4 years after mTBI or the reference date.
RESULTS:
Adjusted risks for affective disorders were significantly higher across the first 3 years after injury for the mTBI group, especially during the second year, with a 34% increase in risk. Adjusted risks for behavioral disorders were significant at years 2 and 4, with up to a 37% increase in risk. The age group with the highest risk for postinjury affective and behavioral disorders was 10- to 13-year-old patients.
CONCLUSIONS:
Sustaining an mTBI significantly increased the risks of having a new affective or behavioral disorder up to 4 years after injury. Initial and ongoing screening for affective and behavior disorders following an mTBI can identify persistent conditions that may pose barriers to recovery.
INTRODUCTION
Traumatic brain injury (TBI) in children has been associated with an increased risk of developing psychiatric disorders.1–7 Although most studies examined children with moderate to severe TBI, recent reports indicate increased risk of psychiatric symptoms after mild TBI (mTBI).3,4,6–9 These symptoms may persist up to 3 years after injury,3,4,8,9 and are more likely to occur in children with a history of a behavior problem or psychiatric disorder.3,4,8,9
Psychiatric effects of mTBI can include affective and behavior disorders. Affective disorders include depression, anxiety, posttraumatic stress disorder, acute stress, and adjustment disorders.8 Behavioral disorders include conduct disorder, oppositional defiant disorder (ODD), and attention deficit hyperactivity disorder (ADHD).6,9–11 The literature on behavioral diagnoses of non-ADHD after mTBI is limited, inconsistent, and the findings are not clinically significant. Although 1 study reported that children younger than age 10 years at the time of injury were more likely to have behavioral problems 1 year after mTBI,6 another study on conduct disorders 6 and 12 months after mild, moderate, and severe TBI found no conduct disorders at either point of follow-up.10,11 Although ADHD has been associated with TBI in children, this relationship is complex, lacks strong evidence for causality, and is complicated by those children diagnosed with ADHD preinjury as well as family and environmental circumstances.12,13 Although only 1 study reported that TBI was associated with an ADHD diagnosis 5 to 10 years after injury in young children,14 another found no significant risk for developing ADHD after mTBI.15
The incidence and impact of affective and behavior disorders in the pediatric mTBI population within an integrated health care system is unclear. Given that mTBI represents at least 75% of all TBIs annually, there is a high likelihood that the incidence of a cooccurring mental health condition is significant.16 We conducted a longitudinal cohort study comparing psychiatric outcomes (affective disorders [depressive, anxiety, and adjustment disorders] and behavioral disorders [conduct, ODD, and ADHD]) of pediatric patients who acquired an mTBI to a matched cohort without brain injuries within an integrated health care system. We predicted that children with an mTBI would have a significantly higher risk of developing a new psychiatric disorder 4 years after injury compared with children without mTBI. This follow-up period was selected based on the studies reviewed previously that indicate these disorders may emerge and persist up to 3 years after mTBI.
METHODS
Design and Setting
This study is an observational matched cohort design using electronic health records (EHRs) within an integrated health care system based in Northern California. The reference dates for the cohort entry were January 1, 2001, through December 31, 2014, with a 1-year lookback period and a 4-year follow-up period. The institutional review board of the integrated health care system approved this study with a waiver of consent.
Participants
mTBI Group
Eligible patients were aged 17 years and younger with a primary diagnosis of mTBI treated in the emergency department (ED), urgent care, or any outpatient clinic within the integrated health care system. The diagnoses codes for mTBI using the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) included: postconcussion syndrome, 310.2; concussion with no loss of consciousness, 850.0; concussion with brief loss of consciousness, 850.1; concussion with loss of consciousness of 30 minutes or less, 850.11; and concussion unspecified, 850.9.
We used the diagnostic criteria based on the Centers for Disease Control and Prevention Pediatric Mild TBI Guideline workgroup.17 A TBI was considered mild if ICD-9-CM codes indicated brief (<30 minutes) or no loss of consciousness and no documented traumatic intracranial lesions. The reference date in the mTBI group was the initial mTBI diagnosis date. Patients were excluded if they1: were aged 18 years or older at mTBI onset2; had a health plan membership (health insurance coverage) for less than 9 months in any 12-month period from lookback through follow-up3; died anytime during 4-year follow-up; and4 had postconcussion syndrome paired with any ICD-9-CM diagnoses more severe than an mTBI.
Comparison Group
Eligible patients were aged 17 years and younger who had medical visits in the ED, urgent care, or any outpatient clinic within the integrated health care system and1: did not have a TBI diagnosis between 2000 and 20182; had active health plan membership at least 9 months during each calendar year from 2000 to 2018; and were alive as of 2018.3 We used Mahalanobis distance function for each patient with mTBI to identify 2 within the comparison group who matched according to age, sex, and race/ethnicity.18,19 Patients in the comparison group eligible for the matching were those with eligible medical visits in the month of the reference date (corresponding to the mTBI date in the mTBI group). Because a patient could have medical visits in multiple months, matching was completed month by month from year 2001 to year 2014 to prevent duplication. Any patient selected as a comparison in a particular month was removed from the comparison eligibility pool for subsequent months.
Variables
Exposure
The independent variable is a binary variable indicating exposure to mTBI and was determined based on ICD-9-CM diagnosis codes, as specified previously.
Psychiatric Disorders
Primary outcomes were new affective and behavioral disorders (Table 1) diagnosed anytime during the 4-year follow-up. We used diagnoses from either the ICD-9-CM, the International Classification of Diseases, Tenth Revision, Clinical Modification, or the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, and Fifth Edition,20,21 whichever were assigned to a medical visit in the EHR during study observation.
TABLE 1.
Psychiatric Diagnoses for Affective and Behavioral Disorders
| ICD-10 CM | ICD-9 CM | DSM-IV-TR/DSM-5 Diagnosis Description |
|---|---|---|
| Affective disorders | ||
| Depressive disorders | ||
| F06.30 | 293.83 | Depressive Disorder Due to Another Medical Conditiona,b |
| F06.31 | With depressive featuresa,b | |
| F06.32 | With major depressive-like episodea,b | |
| F06.34 | With mixed featuresa,b | |
| F32.9 | 296.20 | Major Depressive Disorder, Single Episode Unspecifieda,b |
| F32.0 | 296.21 | Major Depressive Disorder, Single Episode Milda,b |
| F32.1 | 296.22 | Major Depressive Disorder, Single Episode Moderatea,b |
| F32.2 | 296.23 | Major Depressive Disorder, Single Episode Severea,b |
| F32.3 | 296.24 | With psychotic featuresa,b |
| F32.4 | 296.25 | In partial remissiona,b |
| F32.5 | 296.26 | In full remissiona,b |
| F33.9 | 296.30 | Major Depressive Disorder, Recurrent Unspecifieda,b |
| F33.0 | 296.31 | Major Depressive Disorder, Recurrent Milda,b |
| F33.1 | 296.32 | Major Depressive Disorder, Recurrent Moderatea,b |
| F33.2 | 296.33 | Major Depressive Disorder, Recurrent Severea,b |
| F33.3 | 296.34 | With psychotic featuresa,b |
| F33.41 | 296.35 | In partial remissiona,b |
| F33.42 | 296.36 | In full remissiona,b |
| F32.89 | 296.82 | Atypical Depressive Disordera,b |
| F39 | 296.9 | Mood Disorder NOSa,b |
| F34.1 | 300.4 | Persistent Depressive Disorder (Dysthymia)a,b |
| F32.9 | 311 | Depressive Disorder NOS/Unspecifieda,b |
| F32.8 | 311 | Depressive Disorder Other Specifieda,b |
| F34.8 | 296.99 | Disruptive Mood Dysregulation Disordera,b |
| Anxiety disorders | ||
| F06.4 | 293.84 | Anxiety Disorder Due to Another Medical Conditiona,c |
| F41.9 | 300.00 | Anxiety Disorder Other Specifieda,c |
| F41.8 | 300.09 | Anxiety Disorder Unspecifieda,c |
| F41.0 | 300.01 | Panic Disorder Without Agoraphobiaa,c |
| F41.1 | 300.02 | Generalized Anxiety Disordera,c |
| 300.29 | Specific Phobiaa,c | |
| F40.218 | 300.29 | Animala,c |
| F40.228 | 300.29 | Natural Environmenta,c |
| F40.23× | 300.29 | Blood-injection-injurya,c |
| F40.248 | 300.29 | Situationala,c |
| F40.298 | 300.29 | Othera,c |
| F40.8 | 300.29 | Other Isolated or Simple Phobiaa,c |
| F40.9 | 300.2 | Phobic Disorder Unspecifieda,c |
| F40.01 | 300.21 | Agoraphobia With Panic Attacksa,c |
| F40.02 | 300.22 | Agoraphobia Without Panic Attacksa,c |
| F40.10 | 300.23 | Social Anxiety Disorder/Social Phobiaa,c |
| F42.9 | 300.3 | Obsessive Compulsive Disordera,c |
| F43.0 | 300.8 | Acute reaction to Stress/Acute Stress Disordera,c |
| F43.0 | 308.4 | Mixed Disorders as Reaction to Stressa,c |
| R45.7 | 308.9 | Unspecified Reaction to Stressa,c |
| F43.10 | 309.81 | Post-Traumatic Stress Disordera,c |
| F43.8 | 309.89 | Other Specified Trauma and Stressor Related Disordera,c |
| F43.20 | 309.9 | Other Unspecified Trauma and Stressor Related Disordera,c |
| F42 | 300.3 | Other Specified/Unspecified Obsessive-Compulsive and Related Disordera,c |
| F06.8 | 294.8 | Obsessive-Compulsive and Related Disorder Due to Another Medical Conditiona,c |
| F45.22 | 300.7 | Body Dysmorphic Disordera,c |
| Adjustment disorders | ||
| F43.21 | 309.0 | Adjustment Reaction/Disorder With Depressed Mood/Brief Depressive Reactiona,d |
| F43.22 | 309.24 | Adjustment Reaction/Disorder With Anxietya,d |
| F43.23 | 309.28 | Adjustment Reaction/Disorder With Mixed Anxiety and Depressed Mooda,d |
| F43.8 | 309.82 | Adjustment Reaction With Physical Symptomsa,d |
| F43.8 | 309.83 | Adjustment Reaction With Withdrawala,d |
| F43.20 | 309.9 | Adjustment Disorder Unspecifieda,d |
| F43.24 | 309.3 | Adjustment Disorder With Disturbance of Conducta,d |
| F43.25 | 309.4 | Adjustment Disorder With Mixed Disturbance of Emotions and Conducta,d |
| Behavior disorders | ||
| Conduct disorders | ||
| F91.0 | 312.89 | Conduct Disorder Confined to Family Contexte,f |
| F91.8 | 312.89 | Other Specified Disruptive, Impulse-Control, and Conduct Disordere,f |
| F91.2 | 312.82 | Conduct Disorder, Adolescent-Onset Typee,f |
| F91.2 | 312.20 | Socialized Conduct Disorder, Unspecifiede,f |
| F91.1 | 312.81 | Conduct Disorder, Childhood-Onset Typee,f |
| F91.1 | 312.00 | Undersocialized Conduct Disorder, Aggressive Type, Unspecifiede,f |
| F91.1 | 312.10 | Undersocialized Conduct Disorder, Unaggressive Type, Unspecifiede,f |
| F91.9 | 312.9 | Unspecified Disruptive, Impulse-Control, and Conduct Disordere,f |
| F91.3 | 313.81 | Oppositional Defiant Disordere,f |
| F63.81 | 312.34 | Intermittent Explosive Disordere,f |
| Attention-deficit/hyperactivity disorders | ||
| F90.2 | 314.01 | Attention Deficit/Hyperactivity Disorder, Combined Presentatione,g |
| F90.0 | 314.00 | Attention Deficit/Hyperactivity Disorder, Predominantly Inattentive Presentatione,g |
| F90.1 | 314.01 | Attention Deficit/Hyperactivity Disorder, Predominantly Hyperactive/Impulsive Presentatione,g |
| F90.8 | 314.2 | Attention-Deficit/Hyperactivity Disorder, Other Type/Hyperkinetic Conduct Disordere,g |
| F90.8 | 314.0 | Attention-Deficit/Hyperactivity Disordere,g |
| F90.8 | 314.01 | Other Specified Attention-Deficit/Hyperactivity Disordere,g |
| F90.9 | 314.01 | Unspecified Attention-Deficit/Hyperactivity Disordere,g |
| F90.9 | 314.9 | Attention-Deficit/Hyperactivity Disorder, Unspecified Type/Unspecified Hyperkinetic Syndromee,g |
| R41.840 | 799.51 | Attention and Concentration Deficite,g |
DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; ICD-9-CM, International Classification of Disease, Ninth Revision, Clinical Modification; ICD-10 CM, International Classification of Disease, Tenth Revision, Clinical Modification; NOS, not otherwise specified.
Diagnoses included in any affective disorder.
Diagnoses included in depressive disorders.
Diagnosis included in anxiety disorders.
Diagnoses included in adjustment disorders.
Diagnoses included in any behavioral disorder.
Diagnoses included in conduct disorder.
Diagnosis included in attention deficit hyperactivity disorder.
Demographics and Clinical History
Demographic data included age, race/ethnicity, sex, health plan benefit (eg, managed Medicare/Medicaid, commercial, self-pay), and low-income residence (residential address in a census block with ≥20% households below the federal poverty level). For clinical baseline data, we included affective and behavioral disorders diagnosed during the lookback period.
Mortality Status
We determined deaths using a mortality database of deaths recorded by the integrated health care system and California state death records. We also reviewed health care utilization records to confirm the mortality status.
Bias Mitigation
To ensure the accuracy of data extraction, study investigators (R.D. and B.R.T.) conducted structured EHR reviews on a random sample of 2% of patients from each study group. Electronic data extraction was adjusted as necessary before compiling the final study cohort (eg, cases were excluded when the primary mTBI diagnosis was documented outside the integrated health care system and without internal follow-up medical visit within 7 days). Additionally, the integrated health care system transitioned to an electronic documentation system (EHR implementation) about halfway through the cohort entry. We adjusted all regression analyses for pre versus post EHR implementation to control for pre- versus postimplementation variability in the standardization of diagnoses. In terms of demographics, there is evidence for higher risks of injury and adverse health outcomes after an mTBI among non-Hispanic Black children and Hispanic children.22,23 However, these risks may also be a proxy for, or correlated with, socioeconomic differences. Therefore, in our study, we controlled for both race/ethnicity in the matching model and with income levels in the regression model. Finally, we documented the proportion of psychiatric diagnoses made by mental health professionals versus other specialties to determine if most were made by clinicians trained to recognize, diagnose, and manage these disorders.
Statistical Methods
Descriptive statistics (frequencies and percentages) describe the demographic and clinical characteristics of the cohort at baseline. χ-square tests were used to compare previous affective and behavioral disorders preceding mTBI or reference date. We calculated unadjusted incidence rates of psychiatric disorders (affective/behavioral disorders and by subtypes) over the 4-year follow-up and by the end of each follow-up year for each cohort group overall and by age groups (0–5, 6–9, 10–13, and 14–17 years). Adjusted relative risk estimates of psychiatric disorders comparing the mTBI group with the comparison group were computed using generalized linear models with logit link function for fixed-interval, interval-censored data, controlled for age, sex, race, low-income residence, and EHR implementation period. These models were repeated for each age group. Patients with preexisting affective and behavioral disorders were excluded from the analyses on outcomes.
All analyses were performed using SAS software version 9.4 (SAS, Cary, North Carolina) and conducted to test for significance at α = .05. Bonferroni error correction was used when multiple comparisons were conducted within each omnibus test to mitigate for inflation of type I error. The study outcomes had 8 multiple comparisons that may be correlated because of comorbid psychiatric disorders; therefore, our threshold for reporting a significant finding was P < .00625.
RESULTS
Cohort Characteristics
A total of 2139984 pediatric patients received care at EDs, urgent care, and outpatient clinics in the integrated health care system between 2001 and 2014. Figure 1 summarizes the cohort selection criteria for both the mTBI group and the comparison group. The final mTBI group consisted of 18917 patients who received their mTBI diagnosis at EDs (38%), urgent care (14%), and outpatient clinics (44%; predominantly at a pediatric visit), and unspecified (4%). These mTBI patients were matched to 37834 non–brain-injured pediatric patients in a 2:1 matching ratio.
FIGURE 1.
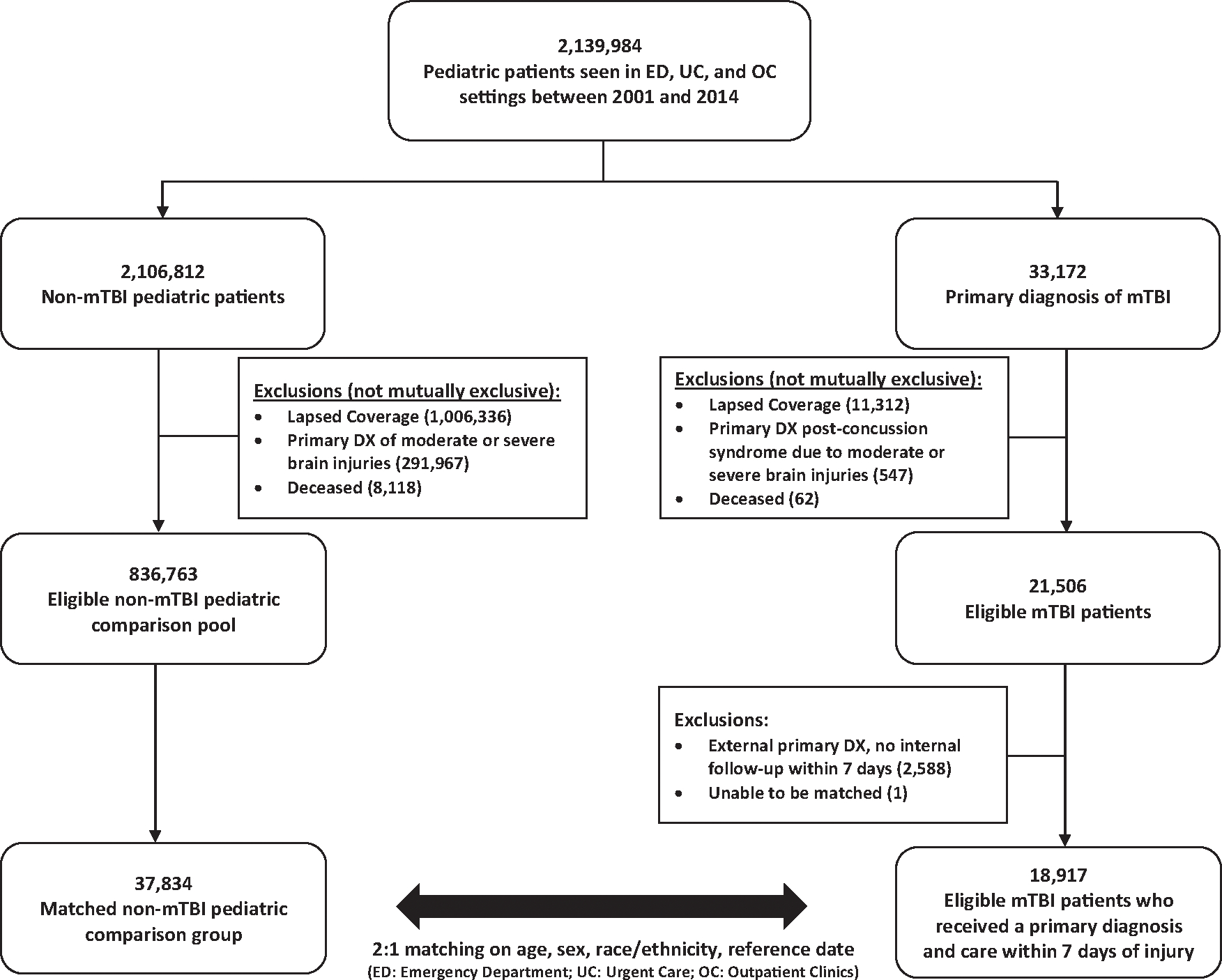
Summary of the cohort selection criteria for the mTBI and noninjured comparison groups. DX, diagnosis; mTBI, mild traumatic brain injury.
Table 2 describes the characteristics of the study cohort. Patients were predominantly 14 to 17 years old (48%), followed by the age 10–13 (28%), 6–9 (13%), and 0–5 (11%) age groups. Patients were also predominantly male (64%) and had racial/ethnic group distributions that were reflective of the population in Northern California. Less than 10% of the cohort qualified as being from low-income households. Twelve percent of the noninjured comparisons and 8% of the mTBI patients had a previous affective disorder (P < .001). Similarly, 10% of the noninjured comparisons and 7% of the mTBI patients had a previous behavioral disorder (P < .001).
TABLE 2.
Demographic Characteristics of the Study Cohort
| Variable | Comparisona N = 37 834 | mTBI N = 18 917 | P | Odds Ratio (95% CI) |
|---|---|---|---|---|
| Age groups, y (n) | 1.000 | N/A | ||
| 0–5 | 11 (4338) | 11 (2169) | ||
| 6–9 | 13 (4792) | 13 (2396) | ||
| 10–13 | 28 (10476) | 28 (5238) | ||
| 14–17 | 48 (18 228) | 48 (9144) | ||
| Sex (n) | 1.000 | N/A | ||
| Female | 36 (13 530) | 36 (6756) | ||
| Male | 64 (24 304) | 64 (12 152) | ||
| Race/ethnicity (n) | 1.000 | N/A | ||
| White (non-Hispanic) | 49 (18 678) | 49 (9339) | ||
| Hispanic/Latino | 24 (8949) | 24 (4476) | ||
| Asian/Pacific Islander | 10 (3608) | 10 (1807) | ||
| Black/African American | 9 (3493) | 9 (1746) | ||
| Other race/ethnicity | 8 (3106) | 8 (1549) | ||
| Low-income households - % (n) | 9 (3574) | 8 (1552) | <.0001b | 0.86 (0.81–0.91)b |
| Previous diagnoses (n) | ||||
| Affective disorders | 12 (4449) | 8 (1489) | <.0001b | 0.64 (0.60–0.68)b |
| Behavioral disorders | 10 (3643) | 7 (1273) | <.0001b | 0.68 (0.63–0.72)b |
mTBI, mild traumatic brain injury; N/A, not available.
Two comparison patients were selected for each mTBI patient. Comparisons have the same “reference date” (ie, corresponding to the injury date of the paired mTBI patient). mTBI patients were matched to their respective comparisons using Mahalanobis distance function based on sex, age, and race/ethnicity.
Statistically significant risk ratios (P < .05).
Incidence and Risk for Postinjury Affective Disorders
Psychiatry and behavioral health clinicians diagnosed most affective disorders (84%). Table 3 summarizes the individual 4-year and overall incidence and adjusted risk of affective disorders. The mTBI group was 25% more likely to be diagnosed with an affective disorder during the overall 4-year study follow-up period; the adjusted risk was significant across the first 3 years. Specifically, these diagnoses were only significant in the 10 to 13 and 14 to 17 year age groups, with the former being 48% more likely to be diagnosed with any affective disorders at year 2.
TABLE 3.
Incidence and Adjusted Riska of Affective Disorders During 4 Years After mTBI Versus Comparisons
| Psychiatric Diagnoses % (n) | Study Groups | Overall | 0–12 mo | 13–24 mo | 25–36 mo | 37–48 mo |
|---|---|---|---|---|---|---|
| Any affective disorder | Comparisons | 16.9% (5656) | 5.3% (1780) | 4.3% (1370) | 4.2% (1281) | 4.2% (1225) |
| mTBI | 20.1% (3553) | 6.6% (1141) | 5.8% (936) | 5.1% (783) | 4.8% (693) | |
| P | <.0001b | <.0001b | <.0001b | <.0001b | .0098 | |
| RR (95% CI) | 1.25 (1.19–1.31) | 1.23 (1.14–1.33) | 1.34 (1.23–1.46) | 1.22 (1.11–1.33)b | 1.13 (1.03–1.25) | |
| 0–5 y old | Comparisons | 4.3% (187) | 0.6% (27) | 0.9% (38) | 1.6% (67) | 1.3% (55) |
| mTBI | 5.5% (118) | 0.8% (18) | 1.4% (29) | 1.2% (26) | 2.2% (45) | |
| P | .0393 | .3167 | .1075 | .2999 | .0093 | |
| RR (95% CI) | 1.28 (1.01–1.63) | 1.36 (0.74–2.47) | 1.50 (0.92–2.45) | 0.78 (0.50–1.24) | 1.70 (1.14–2.53) | |
| 6–9 y old | Comparisons | 12.6% (563) | 3.6% (162) | 3.3% (143) | 3.0% (125) | 3.3% (133) |
| mTBI | 14.0% (321) | 4.3% (99) | 3.3% (73) | 4.1% (86) | 3.1% (63) | |
| P | .1116 | .1722 | .9983 | .0309 | .7051 | |
| RR (95% CI) | 1.13 (0.97–1.31) | 1.19 (0.92–1.54) | 1.00 (0.75–1.33) | 1.36 (1.03–1.80) | 0.94 (0.69–1.28) | |
| 10–13 y old | Comparisons | 18.8% (1746) | 5.2% (485) | 4.7% (410) | 5.0% (421) | 5.4% (430) |
| mTBI | 23.6% (1137) | 6.7% (325) | 6.7% (300) | 6.5% (274) | 6.1% (238) | |
| P | <.0001b | .0002b | <.0001b | .0003b | .1017 | |
| RR (95% CI) | 1.34 (1.23–1.46) | 1.31 (1.14–1.52) | 1.48 (1.27–1.72) | 1.34 (1.14–1.57b | 1.15 (0.97–1.35) | |
| 14–17 y old | Comparisons | 20.7% (3160) | 7.2% (1106) | 5.5% (779) | 5.0% (668) | 4.8% (607) |
| mTBI | 24.3% (1977) | 8.6% (699) | 7.2% (534) | 5.7% (397) | 5.3% (347) | |
| P | <.0001b | .0004b | <.0001b | .0253 | .1052 | |
| RR (95% CI) | 1.23 (1.15–1.31b | 1.20 (1.08–1.32) | 1.32 (1.18–1.48) | 1.16 (1.02–1.32) | 1.12 (0.98–1.28) | |
| Depressive disorders | Comparisons | 9.7% (3450) | 2.9% (1031) | 2.5% (851) | 2.3% (781) | 2.4% (787) |
| mTBI | 11.3% (2053) | 3.4% (624) | 3.0% (533) | 2.7% (459) | 2.6% (437) | |
| P | <.0001b | .0027b | .0004b | .0145 | .1349 | |
| RR (95% CI) | 1.17 (1.10–1.24) | 1.17 (1.06–1.29) | 1.22 (1.09–1.36) | 1.16 (1.03–1.30) | 1.09 (0.97–1.23) | |
| 0–5 y old | Comparisons | 4.3% (187) | 0.6% (27) | 0.9% (38) | 1.6% (67) | 1.3% (55) |
| mTBI | 5.5% (118) | 0.8% (18) | 1.4% (29) | 1.2% (26) | 2.2% (45) | |
| P | .6936 | .3933 | .8237 | .3200 | .0835 | |
| RR (95% CI) | 1.15 (0.57–2.35) | 0.39 (0.05–3.36) | 0.83 (0.16–4.29) | 1.60 (0.63–4.07) | 1.25 (0.97–1.60) | |
| 6–9 y old | Comparisons | 12.6% (563) | 3.6% (162) | 3.3% (143) | 3.0% (125) | 3.3% (133) |
| mTBI | 14.0% (321) | 4.3% (99) | 3.3% (73) | 4.1% (86) | 3.1% (63) | |
| P | .0835 | .6015 | .7480 | .0937 | .3760 | |
| RR (95% CI) | 1.25 (0.97–1.60) | 1.16 (0.66–2.02) | 1.09 (0.64–1.86) | 1.51 (0.93–2.46) | 1.21 (0.79–1.85) | |
| 10–13 y old | Comparisons | 18.8% (1746) | 5.2% (485) | 4.7% (410) | 5.0% (421) | 5.4% (430) |
| mTBI | 23.6% (1137) | 6.7% (325) | 6.7% (300) | 6.5% (274) | 6.1% (238) | |
| P | <.0001b | .0004b | .0002b | .0353 | .2466 | |
| RR (95% CI) | 1.30 (1.18–1.44) | 1.43 (1.17–1.74) | 1.44 (1.19–1.75) | 1.22 (1.01–1.48) | 1.12 (0.93–1.35) | |
| 14–17 y old | Comparisons | 20.7% (3160) | 7.2% (1106) | 5.5% (779) | 5.0% (668) | 4.8% (607) |
| mTBI | 24.3% (1977) | 8.6% (699) | 7.2% (534) | 5.7% (397) | 5.3% (347) | |
| P | .0182 | .2007 | .0750 | .3071 | .5823 | |
| RR (95% CI) | 1.10 (1.01–1.18) | 0.108 (0.96–1.22) | 1.13 (0.99–1.30) | 1.09 (0.93–1.27) | 1.05 (0.88–1.24) | |
| Anxiety disorders | Comparisons | 11.8% (4182) | 3.4% (1216) | 2.9% (981) | 3.0% (990) | 3.1% (995) |
| mTBI | 13.2% (2392) | 3.8% (681) | 3.5% (601) | 3.3% (555) | 3.4% (555) | |
| P | <.0001b | .0589 | .0003b | .0430 | .0450 | |
| RR (95% CI) | 1.14 (1.08–1.20 | 1.10 (1.00–1.21) | 1.21 (1.09–1.34)b | 1.11 (1.00–1.24) | 1.11 (1.00–1.24) | |
| 0–5 y old | Comparisons | 2.8% (119) | 0.4% (19) | 0.7% (28) | 0.8% (35) | 0.9% (37) |
| mTBI | 3.3% (72) | 0.5% (10) | 0.8% (18) | 1.0% (21) | 1.1% (23) | |
| P | .2033 | .8584 | .5169 | .4797 | .3703 | |
| RR (95% CI) | 1.21 (0.90–1.64) | 1.07 (0.50–2.31) | 1.22 (0.67–2.24) | 1.22 (0.71–2.10) | 1.27 (0.75–2.14) | |
| 6–9 y old | Comparisons | 8.0% (371) | 2.2% (102) | 2.4% (107) | 1.9% (86) | 1.8% (76) |
| mTBI | 9.1% (213) | 2.9% (69) | 2.0% (45) | 2.5% (55) | 2.0% (44) | |
| P | .1432 | .0607 | .3025 | .1907 | .4667 | |
| RR (95% CI) | 1.14 (0.96–1.36) | 1.35 (0.99–1.84) | 0.83 (0.58–1.18) | 1.26 (0.89–1.77) | 1.15 (0.79–1.67) | |
| 10–13 y old | Comparisons | 12.2% (1202) | 3.3% (325) | 2.8% (267) | 3.2% (295) | 3.5% (315) |
| mTBI | 13.8% (689) | 3.4% (169) | 3.9% (190) | 3.5% (163) | 3.7% (167) | |
| P | .0062b | .8192 | .0003b | .2753 | .4809 | |
| RR (95% CI) | 1.15 (1.04–1.28) | 1.02 (0.84–1.23) | 1.42 (1.18–1.72) | 1.11 (0.92–1.36) | 1.07 (0.88–1.30) | |
| 14–17 y old | Comparisons | 14.9% (2490) | 4.6% (770) | 3.6% (579) | 3.7% (574) | 3.8% (567) |
| mTBI | 16.5% (1418) | 5.0% (433) | 4.3% (348) | 4.0% (316) | 4.3% (321) | |
| P | .0009b | .1357 | .0137 | .2397 | .1026 | |
| RR (95% CI) | 1.13 (1.05–1.22) | 1.10 (0.97–1.24) | 1.19 (1.03–1.36) | 1.09 (0.94–1.25) | 1.12 (0.98–1.29) | |
| Adjustment disorders | Comparisons | 6.2% (2275) | 1.9% (695) | 1.6% (555) | 1.5% (521) | 1.5% (504) |
| mTBI | 7.8% (1431) | 2.5% (469) | 2.0% (361) | 1.7% (305) | 1.7% (296) | |
| P | <.0001b | <.0001b | .0001b | .0255 | .0209 | |
| RR (95% CI) | 1.27 (1.19–1.36) | 1.35 (1.20–1.52) | 1.30 (1.14–1.49) | 1.18 (1.02–1.36) | 1.19 (1.03–1.37) | |
| 0–5 y old | Comparisons | 1.8% (79) | 0.2% (8) | 0.4% (16) | 0.8% (34) | 0.5% (21) |
| mTBI | 2.4% (52) | 0.3% (7) | 0.6% (12) | 0.4% (9) | 1.1% (24) | |
| P | .1034 | .2662 | .2702 | .0919 | .0044b | |
| RR (95% CI) | 1.34 (0.94–1.91) | 1.78 (0.64–4.92) | 1.52 (0.72–3.23) | 0.53 (0.25–1.11) | 2.35 (1.31–4.24) | |
| 6–9 y old | Comparisons | 5.8% (268) | 1.8% (82) | 1.3% (61) | 1.2% (54) | 1.6% (71) |
| mTBI | 7.4% (173) | 2.1% (49) | 1.6% (37) | 2.0% (45) | 1.9% (42) | |
| P | .0079 | .3417 | .3339 | .0109 | .3467 | |
| RR (95% CI) | 1.31 (1.07, 1.59) | 1.19 (0.83, 1.70) | 1.22 (0.81, 1.85) | 1.68 (1.13, 2.50) | 1.20 (0.82, 1.77) | |
| 10–13 y old | Comparisons | 7.2% (722) | 2.0% (204) | 1.8% (179) | 1.8% (170) | 1.8% (169) |
| mTBI | 9.6% (491) | 2.9% (147) | 2.4% (118) | 2.3% (112) | 2.4% (114) | |
| P | <.0001b | .0007b | .0177 | .0188 | .0099 | |
| RR (95% CI) | 1.39 (1.23–1.57) | 1.45 (1.17–1.80) | 1.33 (1.05–1.68) | 1.33 (1.05–1.70) | 1.37 (1.08–1.74) | |
| 14–17 y old | Comparisons | 6.9% (1206) | 2.3% (401) | 1.8% (299) | 1.6% (263) | 1.5% (243) |
| mTBI | 8.1% (715) | 3.0% (266) | 2.3% (194) | 1.7% (139) | 1.4% (116) | |
| P | .0005b | .0005b | .0060b | .6045 | .6710 | |
| RR (95% CI) | 1.19 (1.08–1.31) | 1.32 (1.13–1.55) | 1.29 (1.08–1.55) | 1.06 (0.86–1.30) | 0.95 (0.76–1.19) |
mTBI, mild traumatic brain injury; RR, relative risk.
Adjusted relative risk estimates were generated using generalized linear models with logit link function for fixed-interval, interval-censored data, controlled for age, sex, race/ethnicity, low-income residence, and electronic health record transition period. Bonferroni correction resulted in a significance threshold of 2-sided P < .00625.
Statistically significant risk ratios.
The overall adjusted risk for post mTBI depressive disorders was 17% more likely in the mTBI group and was sustained over the first 2 years after injury. However, this increased risk was only significant in the 10 to 13 year age group, which was approximately 40% more likely to be diagnosed with a depressive disorder during the first 2 years after mTBI. For anxiety disorders, the mTBI group was 14% more likely to be diagnosed across all 4 years in aggregate, and this adjusted risk was only sustained during the second year after mTBI. The 10 to 13 year age group was most at risk, being 42% more likely to receive a diagnosis for anxiety disorders 2 years after mTBI. The mTBI patients in the 14 to 17 year age group were 13% more likely to be diagnosed with anxiety disorders when aggregated over 4 years, but effect sizes were not significant when analyzed for each of these years individually. Adjustment disorders were 27% more likely in the mTBI group, and this effect was sustained over the first 2 years after mTBI. Although mTBI patients in the 10 to 13 year age group were 39% more likely to have an adjustment disorder, this risk was only sustained during the first year after mTBI. The 14 to 17 year age group was approximately 30% more likely to be diagnosed with adjustment disorders over the first 2 years after mTBI. Finally, the 0 to 5 year olds with mTBI had a significantly increased risk for adjustment disorders at year 4. However, the differences between the small sample sizes in this age group resulted in a dramatically high relative risk, although absolute numbers of cases were low.
Incidence and Risk for Postinjury Behavioral Disorders
Psychiatry and behavioral health clinicians predominantly (70%) diagnosed behavioral disorders. Table 4 summarizes the individual 4-year and overall incidence and adjusted risk of behavioral disorders. Overall, the mTBI group was 18% more likely to be diagnosed with any behavioral disorders during the 4-year follow-up. An increase in risk during the second and fourth year was also observed, with the mTBI group being 21% and 37% more likely to be diagnosed with any behavioral disorders, during the second and fourth years, respectively. However, that trend was not observed when examined within age groups. Only the 10 to 13 year age group had significant risk and was up to 50% more likely to be diagnosed with any behavioral disorders during the first 2 years after mTBI.
TABLE 4.
Incidence and Adjusted Riska of Behavioral Disorders During 4 Years After mTBI Versus Comparisons
| Psychiatric Diagnoses % (n) | Study Groups | Overall | 0–12 mo | 13–24 mo | 25–36 mo | 37–48 mo |
|---|---|---|---|---|---|---|
| Any behavioral disorders | Comparisons | 6.7% (2277) | 2.7% (921) | 1.7% (551) | 1.3% (440) | 1.1% (365) |
| mTBI | 7.8% (1377) | 2.9% (512) | 2.0% (345) | 1.6% (265) | 1.5% (255) | |
| P | <.0001b | .2405 | .0057b | .0456 | .0001b | |
| RR (95% CI) | 1.18 (1.10–1.26) | 1.07 (0.96–1.19) | 1.21 (1.06–1.39) | 1.17 (1.00–1.36) | 1.37 (1.17–1.61) | |
| 0–5 y old | Comparisons | 4.5% (192) | 0.7% (30) | 0.8% (35) | 1.3% (56) | 1.7% (71) |
| mTBI | 5.5% (119) | 0.8% (18) | 1.1% (24) | 1.5% (32) | 2.2% (45) | |
| P | .0436 | .5092 | .2088 | .4814 | .1657 | |
| RR (95% CI) | 1.28 (1.01–1.62) | 1.22 (0.68–2.19) | 1.40 (0.83–2.36) | 1.17 (0.75–1.81) | 1.31 (0.89–1.91) | |
| 6–9 y old | Comparisons | 9.1% (394) | 3.8% (164) | 2.7% (111) | 1.7% (67) | 1.3% (52) |
| mTBI | 10.1% (228) | 4.0% (89) | 2.0% (44) | 2.6% (56) | 1.9% (39) | |
| P | .2385 | .8994 | .1186 | .0124 | .0849 | |
| RR (95% CI) | 1.11 (0.93–1.32) | 1.02 (0.78–1.32) | 0.75 (0.53–1.07) | 1.58 (1.10–2.27) | 1.45 (0.95–2.20) | |
| 10–13 y old | Comparisons | 7.7% (703) | 2.8% (258) | 2.0% (173) | 1.7% (151) | 1.4% (121) |
| mTBI | 10.0% (480) | 3.7% (179) | 2.9% (136) | 1.8% (80) | 1.9% (85) | |
| P | <.0001b | 0058b | .0004b | .8811 | .0302 | |
| RR (95% CI) | 1.32 (1.17–1.49) | 1.31 (1.08–1.60) | 1.50 (1.20–1.89) | 1.02 (0.78–1.34) | 1.36 (1.03–1.80) | |
| 14–17 y old | Comparisons | 6.0% (988) | 2.9% (469) | 1.4% (232) | 1.1% (166) | 0.8% (121) |
| mTBI | 6.5% (550) | 2.7% (226) | 1.7% (141) | 1.2% (97) | 1.1% (86) | |
| P | .1124 | .4361 | .1126 | .3088 | .0204 | |
| RR (95% CI) | 1.09 (0.98–1.22) | 0.94 (0.80–1.10) | 1.19 (0.96–1.46) | 1.14 (0.88–1.47) | 1.39 (1.05–1.83) | |
| Conduct disorder | Comparisons | 1.7% (644) | 0.6% (233) | 0.5% (172) | 0.4% (133) | 0.3% (106) |
| mTBI | 2.2% (418) | 0.8% (155) | 0.6% (107) | 0.5% (84) | 0.4% (72) | |
| P | <.0001b | 0060b | .0773 | .0775 | .0419 | |
| RR (95% CI) | 1.31 (1.15–1.48) | 1.33 (1.09–1.63) | 1.24 (0.98–1.58) | 1.28 (0.97–1.68) | 1.37 (1.01–1.84) | |
| 0–5 y old | Comparisons | 1.3% (57) | 0.3% (14) | 0.4% (15) | 0.3% (12) | 0.4% (16) |
| mTBI | 1.5% (33) | 0.5% (10) | 0.3% (7) | 0.5% (11) | 0.2% (5) | |
| P | .4471 | .3608 | .9191 | .1359 | .3871 | |
| RR (95% CI) | 1.18 (0.77–1.82) | 1.46 (0.65–3.30) | 0.95 (0.39–2.35) | 1.87 (0.82–4.24) | 0.64 (0.23–1.75) | |
| 6–9 y old | Comparisons | 2.4% (113) | 0.7% (32) | 0.7% (34) | 0.6% (26) | 0.5% (21) |
| mTBI | 2.4% (58) | 1.1% (26) | 0.4% (9) | 0.4% (9) | 0.6% (14) | |
| P | .8784 | .0679 | .0963 | .3304 | .4011 | |
| RR (95% CI) | 1.02 (0.74–1.41) | 1.62 (0.96–2.74) | 0.53 (0.26–1.12) | 0.68 (0.32–1.47) | 1.34 (0.68–2.64) | |
| 10–13 y old | Comparisons | 2.1% (216) | 0.7% (69) | 0.6% (57) | 0.4% (44) | 0.5% (46) |
| mTBI | 3.4% (175) | 1.0% (50) | 1.0% (50) | 0.9% (46) | 0.6% (29) | |
| P | <.0001b | .0495 | .0040b | .0003b | .3232 | |
| RR (95% CI) | 1.64 (1.34–2.01) | 1.44 (1.00–2.08) | 1.75 (1.20–2.57) | 2.17 (1.43–3.29) | 1.26 (0.79–2.02) | |
| 14–17 y old | Comparisons | 1.4% (258) | 0.7% (118) | 0.4% (66) | 0.3% (51) | 0.1% (23) |
| mTBI | 1.7% (152) | 0.8% (69) | 0.5% (41) | 0.2% (18) | 0.3% (24) | |
| P | .1112 | .3032 | .2889 | .2081 | .0116 | |
| RR (95% CI) | 1.18 (0.96–1.44) | 1.17 (0.87–1.58) | 1.23 (0.83–1.83) | 0.71 (0.41–1.21) | 2.09 (1.18–3.71) | |
| Oppositional defiant disorder | Comparisons | 1.8% (668) | 0.8% (283) | 0.4% (163) | 0.4% (131) | 0.3% (91) |
| mTBI | 2.0% (373) | 0.7% (123) | 0.6% (107) | 0.4% (82) | 0.3% (61) | |
| P | .0923 | .1818 | .0320 | .1172 | .0630 | |
| RR (95% CI) | 1.11 (0.98–1.27) | 0.86 (0.70–1.07) | 1.31 (1.02–1.67) | 1.25 (0.95–1.65) | 1.36 (0.98–1.89) | |
| 0–5 y old | Comparisons | 0.8% (34) | 0.2% (7) | 0.2% (7) | 0.2% (7) | 0.3% (13) |
| mTBI | 0.7% (16) | 0.1% (2) | 0.1% (3) | 0.2% (4) | 0.3% (7) | |
| P | .8824 | .4905 | .8133 | .7953 | .8286 | |
| RR (95% CI) | 0.95 (0.52–1.74) | 0.57 (0.11–2.77) | 0.85 (0.22–3.29) | 1.18 (0.34–4.03) | 1.11 (0.44–2.78) | |
| 6–9 y old | Comparisons | 2.6% (122) | 0.9% (44) | 0.6% (30) | 0.5% (25) | 0.5% (23) |
| mTBI | 3.0% (71) | 0.8% (19) | 0.6% (14) | 0.9% (22) | 0.7% (16) | |
| P | .3044 | .5603 | .8377 | .0525 | .2902 | |
| RR (95% CI) | 1.17 (0.87–1.57) | 0.85 (0.49–1.46) | 0.93 (0.49–1.77) | 1.77 (0.99–3.15) | 1.41 (0.74–2.69) | |
| 10–13 y old | Comparisons | 2.6% (269) | 0.9% (91) | 0.7% (69) | 0.6% (63) | 0.5% (46) |
| mTBI | 3.5% (179) | 1.0% (51) | 1.1% (57) | 0.8% (38) | 0.7% (33) | |
| P | .0030b | .5358 | .0053b | .3738 | .0947 | |
| RR (95% CI) | 1.34 (1.10–1.62) | 1.11 (0.79–1.57) | 1.65 (1.16–2.35) | 1.20 (0.80–1.80) | 1.47 (0.93–2.30) | |
| 14–17 y old | Comparisons | 1.4% (243) | 0.8% (141) | 0.3% (57) | 0.2% (36) | 0.1% (9) |
| mTBI | 1.2% (107) | 0.6% (51) | 0.4% (33) | 0.2% (18) | 0.1% (5) | |
| P | .2524 | .0463 | .5379 | .9668 | .8645 | |
| RR (95% CI) | 0.87 (0.69–1.10) | 0.72 (0.52–0.99) | 1.14 (0.74–1.76) | 0.99 (0.56–1.74) | 1.10 (0.37–3.28) | |
| Attention-deficit/hyperactivity disorder | Comparisons | 5.2% (1812) | 2.0% (705) | 1.3% (456) | 1.1% (350) | 0.9% (301) |
| mTBI | 6.1% (1089) | 2.2% (394) | 1.6% (275) | 1.2% (206) | 1.3% (214) | |
| P | <.0001b | .2524 | .0451 | .1421 | 0002b | |
| RR (95% CI) | 1.17 (1.08–1.27) | 1.07 (0.95–1.22) | 1.17 (1.00–1.36) | 1.14 (0.96–1.35) | 1.40 (1.17–1.66) | |
| 0–5 y old | Comparisons | 3.6% (154) | 0.4% (17) | 0.6% (24) | 1.2% (50) | 1.5% (63) |
| mTBI | 4.7% (101) | 0.5% (10) | 1.0% (21) | 1.0% (22) | 2.3% (48) | |
| P | .0222 | .6656 | .0553 | .6775 | .0195 | |
| RR (95% CI) | 1.35 (1.04–1.75) | 1.19 (0.54–2.60) | 1.78 (0.99–3.21) | 0.90 (0.54–1.49) | 1.57 (1.07–2.30) | |
| 6–9 y old | Comparisons | 7.8% (340) | 3.2% (139) | 2.4% (101) | 1.4% (58) | 1.0% (42) |
| mTBI | 8.3% (188) | 3.1% (71) | 2.0% (43) | 2.0% (43) | 1.5% (31) | |
| P | .5737 | .8018 | .2487 | .1049 | .1521 | |
| RR (95% CI) | 1.05 (0.87–1.27) | 0.96 (0.72–1.29) | 0.81 (0.56–1.16) | 1.39 (0.93–2.07) | 1.41 (0.88–2.25) | |
| 10–13 y old | Comparisons | 5.9% (547) | 2.2% (207) | 1.6% (142) | 1.2% (109) | 1.0% (89) |
| mTBI | 7.5% (363) | 2.9% (142) | 2.1% (99) | 1.2% (56) | 1.5% (66) | |
| P | .0006b | .0174 | .0308 | .9073 | .0284 | |
| RR (95% CI) | 1.27 (1.11–1.46) | 1.30 (1.05–1.62) | 1.33 (1.03–1.72) | 0.98 (0.71–1.36) | 1.43 (1.04–1.97) | |
| 14–17 y old | Comparisons | 4.6% (771) | 2.1% (342) | 1.2% (189) | 0.8% (133) | 0.7% (107) |
| mTBI | 5.1% (437) | 2.0% (171) | 1.3% (112) | 1.0% (85) | 0.9% (69) | |
| P | .0764 | .8120 | .2099 | .1104 | .1281 | |
| RR (95% CI) | 1.11 (0.99–1.23) | 0.98 (0.81–1.18) | 1.16 (0.92–1.47) | 1.25 (0.95–1.64) | 1.27 (0.93–1.72) |
mTBI, mild traumatic brain injury; RR, relative risk.
Adjusted relative risk estimates were generated using generalized linear models with logit link function for fixed-interval, interval-censored data, controlled for age, sex, race/ethnicity, low-income residence, and EHR transition period. Bonferroni correction resulted in a significance threshold of 2-sided P < .00625.
Statistically significant risk ratios.
The risk for a post-mTBI conduct disorder was overall 31% more likely in the mTBI group with a sustained risk only during 1-year after injury. The 10 to 13 year age group was the only group with a significant risk for conduct disorders, being overall 64% more likely to be diagnosed, with increases in risk at years 2 and 3 after mTBI (at 75% and 117% increase in risk, respectively). Although these risk ratios were large in magnitude, the sample sizes in these groups were very small. A similar trend was observed with small sample sizes with ODD, with the 10 to 13 year age group being 34% more likely to receive this diagnosis after mTBI, with only a significant elevated risk at year 2 after injury. Finally, the mTBI group was 17% overall more likely to be diagnosed with ADHD, with the risk only significantly emerging in year 4. The 10 to 13 year age group was the only one with a significant risk (27% more likely) for being diagnosed with ADHD after mTBI.
DISCUSSION
The current study examined new mental health sequelae of mTBI in pediatric patients in an integrated health system in Northern California. In general, sustaining an mTBI significantly increased the risk of being diagnosed with a new affective disorder 4 years after injury. These findings clarify and expand on previous studies of the post-mTBI development of psychiatric disorders in children and adolescents.8 Our results show an elevated risk of developing an affective disorder diagnosis after an mTBI in children as age increases and is especially pronounced in the 10- to 13-year-old age group. This age group had the highest risk of developing depressive, anxiety, and adjustment disorders. These findings are consistent with Massagli et al,4 with the exception of adjustment disorders in the 0 to 5 year age group. We did not find any significant differences in new psychiatric diagnoses in children younger than age 10 years. This is most likely because of a reluctance among clinicians for establishing an affective disorder diagnosis in younger children. In our post hoc chart reviews of the 0 to 5 year olds who had a significant risk for adjustment disorders, we did indeed find that the latency between injury and a psychiatric diagnosis was on average 3.5 years later, and the majority of these diagnoses were made when they were older than 5 years of age.
Our study showed that sustaining an mTBI also significantly increased the likelihood of a new behavioral disorder diagnosis during the 4 years after injury. The risk for developing any behavioral disorder was highest during the first 2 years after injury, and specifically for the 10 to 13 year old age group only. However, except for ADHD, which was a significant risk only during the fourth year, the absolute numbers of cases for all other disorders were low and therefore consistent with previous findings that diagnosed behavioral disorders were rare and not likely to emerge as a new diagnosis after an mTBI.10,11
Considering recent findings documenting an increasing rate of mTBI in the pediatric population,24 our study demonstrates that children who have sustained an mTBI can benefit from initial and ongoing assessment for affective and behavioral disorders. Specifically, these assessments should be prioritized for 10- to 17-year-old children during the first 2 years after injury. Regarding behavioral disorders, these assessments should ideally be conducted up to 4 years after injury and be focused on the 10- to 13-year-old subgroup. Our findings replicate a previous study on affective disorders after mTBI in adults.25 Across the age span from infants to older adults, the risk of having affective disorders after mTBI is greatest during the first 2 years postinjury. In children, behavioral disorders are an additional risk. Identifying and treating these mental health disorders could reduce the impact and burden associated with the multifactorial challenges of mTBI. These findings show that mTBI may have a pronounced mental health impact on middle- and high school–aged children. This may be due to increased social and academic demands compared with elementary school–aged children. In addition, other unexplored social factors may further explain these findings, especially underlying factors of socioeconomic vulnerability,10,11,26,27 such as lower levels of parental education, lower household income, and health insurance coverage.28,29
Despite the study’s design, several potential limitations exist. First, 43% of our initial sample of children with mTBIs was excluded for various factors (eg, lapses in health plan coverage and/or the child was initially seen outside the integrated health care system). This may have biased our findings by potentially underestimating how affective and behavioral disorders may be reflected in uninsured children. Second, our requirement to have a diagnosis of mTBI documented in the EHR did not include children who did not seek care for their mTBI, who might have sought care outside our health care system, or who had symptomatology not reaching a threshold for diagnosis of a disorder. Those patients’ diagnostic profiles, outcomes, and other injury-related characteristics may be different than our sample because of variations in clinical practice and limited access to mental health services. Third, we did not investigate the additional impact of multiple mTBIs30 because preliminary review of our database indicated that this subset was too small relative to the index mTBI cohort. Finally, funding limitations did not permit further exploration of treatment, medication use, and other factors of interest that may have added explanatory variables to our study.
CONCLUSIONS
Sustaining mTBI significantly increased the risk of having a new affective or behavioral disorder up to 4 years after injury, especially among those who sustained mTBI when aged 10 to 13 years. Initial and ongoing screening for affective and behavior disorders after mTBI in children and adolescents can identify persistent conditions that may pose barriers to recovery.17
WHAT’S KNOWN ON THIS SUBJECT:
Recent studies document an association between mild traumatic brain injuries in children and the development of postinjury psychiatric disorders. However, these studies were subject to limitations in the design, lack of long-term follow-up, and poorly defined psychiatric outcomes.
WHAT THIS STUDY ADDS:
Sustaining an mTBI increased the risk of new affective or behavioral disorders up to 4 years postinjury, especially in children aged 10–13 years old. Early screening after an mTBI can identify persistent conditions that may pose barriers to recovery.
FUNDING:
This study was funded by the Kaiser Permanente Northern California Community Health Grant Award.
ABBREVIATIONS
- ADHD
attention deficit hyperactivity disorder
- ED
emergency department
- EHR
electronic health record
- ICD-9-CM
International Classification of Disease, Ninth Revision, Clinical Modification
- mTBI
mild traumatic brain injury
- ODD
oppositional defiant disorder
- TBI
traumatic brain injury
Footnotes
CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no potential conflicts of interest to disclose. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Data Sharing Statement:
Deidentified individual participant data will not be made available.
REFERENCES
- 1.Babikian T, Merkley T, Savage RC, Giza CC, Levin H. Chronic aspects of pediatric traumatic brain injury: review of the literature. J Neurotrauma. 2015;32(23):1849–1860 [DOI] [PubMed] [Google Scholar]
- 2.Barlow KM, Crawford S, Stevenson A, Sandhu SS, Belanger F, Dewey D. Epidemiology of postconcussion syndrome in pediatric mild traumatic brain injury. Pediatrics. 2010;126(2):e374–e381 [DOI] [PubMed] [Google Scholar]
- 3.Gornall A, Takagi M, Morawakage T, Liu X, Anderson V. Mental health after paediatric concussion: a systematic review and meta-analysis. Br J Sports Med. 2021;55(18):1048–1058 [DOI] [PubMed] [Google Scholar]
- 4.Massagli TL, Fann JR, Burington BE, Jaffe KM, Katon WJ, Thompson RS. Psychiatric illness after mild traumatic brain injury in children. Arch Phys Med Rehabil. 2004;85(9):1428–1434 [DOI] [PubMed] [Google Scholar]
- 5.Sariaslan A, Sharp DJ, D’Onofrio BM, Larsson H, Fazel S. Long-term outcomes associated with traumatic brain injury in childhood and adolescence: a nationwide Swedish cohort study of a wide range of medical and social outcomes. PLoS Med. 2016;13(8):e1002103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor HG, Orchinik LJ, Minich N, et al. Symptoms of persistent behavior problems in children with mild traumatic brain injury. J Head Trauma Rehabil. 2015;30(5):302–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Report to Congress: The Management of Traumatic Brain Injury in Children Atlanta, GA: National Center for Injury Prevention and Control; 2018 [Google Scholar]
- 8.Ledoux AA, Webster RJ, Clarke AE, et al. Risk of mental health problems in children and youths following concussion. JAMA Netw Open. 2022;5(3):e221235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ellis MJ, Ritchie LJ, Koltek M, et al. Psychiatric outcomes after pediatric sports-related concussion. J Neurosurg Pediatr. 2015;16(6):709–718 [DOI] [PubMed] [Google Scholar]
- 10.Lowet DS, Kolan A, Vaida F, et al. Novel oppositional defiant disorder 6 months after traumatic brain injury in children and adolescents. J Neuropsychiatry Clin Neurosci. 2022;34(1):68–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lowet DS, Vaida F, Hesselink JR, et al. Novel oppositional defiant disorder 12 months after traumatic brain injury in children and adolescents. J Neuropsychiatry Clin Neurosci. 2022;34(2):149–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yeates KO, Max JE, Narad ME. Advances in understanding the association between pediatric traumatic brain injury and attention-deficit/hyperactivity disorder. JAMA Pediatr. 2021;175(10):1001–1003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adeyemo BO, Biederman J, Zafonte R, et al. Mild traumatic brain injury and ADHD: a systematic review of the literature and meta-analysis. J Atten Disord. 2014;18(7):576–584 [DOI] [PubMed] [Google Scholar]
- 14.Narad ME, Kennelly M, Zhang N, et al. Secondary attention-deficit/hyperactivity disorder in children and adolescents 5 to 10 years after traumatic brain injury. JAMA Pediatr. 2018;172(5):437–443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asarnow RF, Newman N, Weiss RE, Su E. Association of attention-deficit/hyperactivity disorder diagnoses with pediatric traumatic brain injury: a meta-analysis. JAMA Pediatr. 2021;175(10):1009–1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Heads Up: Facts for Physicians About Mild Traumatic Brain Injury (MTBI). Atlanta, GA; 2002 [Google Scholar]
- 17.Lumba-Brown A, Yeates KO, Sarmiento K, et al. Diagnosis and Management of Mild Traumatic Brain Injury in Children: A Systematic Review. JAMA Pediatr. 2018;172(11):e182847. [DOI] [PubMed] [Google Scholar]
- 18.Hansen BB, Klopfer SO. Optimal full matching and related designs via network flows. J Comput Graph Stat. 2006;15(3):609–627 [Google Scholar]
- 19.Feng W, Jun Y, Xu R. Paper PR05 - a method/macro based on propensity score and Mahalanobis distance to reduce bias in treatment comparison in observational study. The Pharmaceutical Industry SAS Users Group Conference; May 21–24, 2006; Bonita Springs, Florida, USA [Google Scholar]
- 20.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. 2013 [Google Scholar]
- 21.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed text revision. 2000 [Google Scholar]
- 22.Wallace JS, Mannix RC. Racial disparities in diagnosis of concussion and minor head trauma and mechanism of injury in pediatric patients visiting the emergency department. J Pediatr. 2021;233:249–254.e1 [DOI] [PubMed] [Google Scholar]
- 23.Jimenez N, Ebel BE, Wang J, et al. Disparities in disability after traumatic brain injury among Hispanic children and adolescents. Pediatrics. 2013;131(6):e1850–e1856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen C, Peng J, Sribnick EA, Zhu M, Xiang H. Trend of age-adjusted rates of pediatric traumatic brain injury in U.S. emergency departments from 2006 to 2013. Int J Environ Res Public Health. 2018;15(6):1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Delmonico RL, Theodore BR, Sandel ME, Armstrong MA, Camicia M. Prevalence of depression and anxiety disorders following mild traumatic brain injury. PM R. 2022;14(7):753–763 [DOI] [PubMed] [Google Scholar]
- 26.Max JE, Judd N, Bigler ED, et al. Three-month psychiatric outcome of pediatric mild traumatic brain injury: a controlled study. J Neurotrauma. 2021;38(23):3341–3351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fineblit S, Selci E, Loewen H, Ellis M, Russell K. Health-related quality of life after pediatric mild traumatic brain injury/concussion: a systematic review. J Neurotrauma. 2016;33(17):1561–1568 [DOI] [PubMed] [Google Scholar]
- 28.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800–812 [DOI] [PubMed] [Google Scholar]
- 29.Zonfrillo MR, Durbin DR, Koepsell TD, et al. Prevalence of and risk factors for poor functioning after isolated mild traumatic brain injury in children. J Neurotrauma. 2014;31(8):722–727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eisenberg MA, Andrea J, Meehan W, Mannix R. Time interval between concussions and symptom duration. Pediatrics. 2013;132(1):8–17 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Deidentified individual participant data will not be made available.


