Abstract
Nurses experience poor sleep and high stress due to demanding work environments. Night shift work is common among nurses and may exacerbate stress-sleep associations. We examined bidirectional associations between daily stress and sleep, and moderation by recent shift worker status and daily work schedule among nurses. Participants were 392 nurses (92% female; 78% White, mean age = 39.54, SD = 11.15) who completed 14 days of electronic sleep diaries and actigraphy. They simultaneously completed assessments of daily stress and work schedule upon awakening (day shift vs. night shift [work between 9pm-6am] vs. off work). Participants were classified as recent night shift workers if they worked at least one night shift during the past 14 days (n = 101; 26%). In the entire sample, greater daily stress predicted shorter self-reported total sleep time and lower self-reported sleep efficiency that night. Shorter self-reported and actigraphy total sleep time and lower self-reported sleep efficiency predicted higher next-day stress. Compared to recent night shift workers, day workers reported higher stress after nights with shorter total sleep time. Stress-sleep associations mostly did not vary by nurses’ daily work schedule. Sleep disturbances and stress may unfold in a toxic cycle and are prime targets for tailored interventions among nurses. Night shift workers may be less susceptible to effects of short sleep on next-day stress. Research is needed to understand the short- and long-term effects of shift work and address the unique sleep challenges nurses face.
Keywords: shift work, actigraphy, sleep diaries, stress, multilevel modeling, health care workers
Nurses frequently experience disturbed sleep due to demanding work environments, exposure to workplace trauma, and frequently rotating work schedules (Lin et al., 2012). Approximately 53–76% of nurses work some form of night shift per month (Flo et al., 2012; Kim et al., 2013), 29–57% meet criteria for insomnia (Kageyama, Nishikido, Kobayashi, Oga, & Kawashima, 2001; Øyane, Pallesen, Moen, Akerstedt, & Bjorvatn, 2013), and 79% report chronic short sleep duration (< 6 hr sleep/24 hr) (Scott et al., 2007). Short and poor quality sleep among nurses may be compounded by worked-related stress, as approximately 42–92% of nurses report moderate to high levels of stress (Jordan, Khubchandani, & Wiblishauser, 2016; Sharma et al., 2014). Together, sleep disturbances and stress may impair nurses’ health, well-being, and ability to provide effective patient care, representing a critical public health challenge for the estimated 4.6 million nurses in the U.S. and their patients (Smiley et al., 2018).
Theoretical models provide support for the idea that daily stress and sleep may be bidirectionally associated among nurses. According to the hyperarousal model of insomnia, sleep loss or poor quality sleep may become a stressor for individuals. Following a night of poor sleep, individuals may experience emotional distress, rumination, and catastrophizing that can perpetuate insomnia symptoms and other sleep disturbances (Riemann et al., 2010). Increased exposure to stressful events (e.g., working overtime or irregular work schedules, role demand, dealing with a crisis at work) also may interfere with time for sufficient duration or quality of sleep among nurses (Geiger-Brown et al., 2012). Physiologically, perceived stress, sleep deprivation, and sleep fragmentation activate the sympatho-adreno-medullary system and hypothalamic pituitary adrenal axis, which release the stress hormones cortisol, norepinephrine, and epinephrine. These hormones can lead to cardiovascular, cognitive, and hormonal hyperactivity that makes the act of falling asleep, staying asleep, and obtaining restorative sleep more difficult (Riemann et al., 2010; Sladek, Doane, & Breitenstein, 2020).
Intensive longitudinal studies have confirmed that daily stress and sleep are reciprocally related. However, these studies have been conducted primarily in participants with normal timed sleep (i.e., not shift workers), including healthy young adults (Hanson & Chen, 2010), midlife adults specifically screened to not work night shifts (Lee, Crain, McHale, Almeida, & Buxton, 2017; Sin et al., 2017), and healthy adults screened to not have any sleep disorders (Åkerstedt et al., 2012). One study examined nurses and physicians specifically but only collected self-reported sleep quantity and quality and did not consider shift work (Rutledge et al., 2009). Across these studies, higher levels of daily stress have been associated with poorer self-reported sleep quality, lower sleep efficiency, and shorter total sleep time (Åkerstedt et al., 2012; Hanson & Chen, 2010; Yap, Slavish, Taylor, Bei, & Wiley, 2020). When examining reverse pathways from sleep to next-day stress, nights with shorter duration or poorer quality sleep are associated with greater odds of experiencing a stressor and greater stress severity the next day (Lee et al., 2017; Rutledge et al., 2009; Sin et al., 2017; Yap et al., 2020). A few studies using actigraphy-determined measures of sleep have shown similar results (Doane & Thurston, 2014; Hanson & Chen, 2010; Yap et al., 2020), although results are less consistent than with self-reported sleep.
Together, these studies suggest daily experiences of stress and sleep are tightly linked. However, the bidirectional daily stress-sleep association has not been tested among nurses or other shift workers using comprehensive measures of sleep. Further, several factors pertinent to nurses may modify these associations, explaining both when and for whom associations between sleep and stress may be strongest. It is possible these associations may vary as a function of an individual’s daily work schedule (i.e., day shift vs. night shift vs. off day) and their shift worker status (i.e., typical day worker vs. night shift worker). For example, night shift workers (individuals who regularly engage in work outside of the typical ~8am-6pm workday) report more sleep disturbances (Åkerstedt, Fredlund, Gillberg, & Jansson, 2002; Garde, Hansen, & Hansen, 2009; Gerber, Hartmann, Brand, Holsboer-Trachsler, & Pühse, 2010) and greater levels of stress compared to day workers (Gerber et al., 2010). Unfortunately, previous studies of sleep and stress in nurses did not examine typical work schedule as a moderator of this relationship. Thus, it is unclear whether the strength or direction of the sleep-to-stress or stress-to-sleep association varies by shift worker status in nurses.
Within night shift and daytime workers, associations between stress and sleep may also vary by an individual’s specific daily (or nightly) work schedule. For example, after working a night shift, night shift workers report shorter sleep duration, more sleepiness and fatigue (Garde et al., 2009; Khan, Conduit, Kennedy, & Jackson, 2019) and higher levels of stress (Khan et al., 2019) when compared to working a day shift or being off of work. Similarly, day workers may face greater levels of stress and more impaired sleep when they are working, compared to days they are off work. Supporting this idea, studies among day workers have shown that days with greater work stress are associated with lower sleep efficiency, shorter sleep duration, more insomnia symptoms, more sleep disturbances, and less restful sleep that night (Buxton et al., 2016; Vahle-Hinz, Bamberg, Dettmers, Friedrich, & Keller, 2014).
Overall, this research suggests an individual’s shift worker status (typical night shift vs. day worker) and daily work schedule (day shift vs. night shift vs. off work) may each modify associations between daily stress and sleep, although this remains to be tested empirically. These two fundamentally different questions — for whom and when are associations between stress and sleep strongest? — can each be answered using intensive longitudinal designs to capture within- and between-person fluctuations in work schedules, sleep, and stress. Understanding these questions may identify both at-risk nurses and under what conditions it may be most important to intervene to improve sleep and well-being.
The Current Study
To address these gaps in the literature, the current study had two aims: 1) examine the daily, bidirectional associations between daily stress severity with total sleep time and sleep efficiency assessed via sleep diary and actigraphy across 14 days; and 2) examine if the associations in Aim 1 differed by shift worker status (recent day worker vs. night shift worker) and daily work schedule (night shift vs. day shift vs. off work). We hypothesized that days with greater stress would be bidirectionally associated with shorter total sleep time and lower sleep efficiency. We also expected that night shift workers would have stronger negative associations between daily stress and sleep compared to day workers. Finally, we expected that among night shift workers, on days when they worked a night shift, they would have stronger associations between daily stress and poor sleep, compared to when they worked a day shift or were off work. Among day workers, we expected stronger associations between daily stress and poor sleep on work days compared to off work days.
Methods
Procedure
This study was part of a larger investigation on the effects of sleep on antibody response to the influenza vaccine (R01AI128359–01) that occurred between September 2018 to November 2018. Participants were recruited from two Dallas, Texas regional hospitals through nursing staff presentations, notification through employee email systems, and flyers that directed them to an initial online consent form. Nurses (N = 461) provided online consent and were asked to complete initial online Qualtrics surveys to collect demographic information as well as retrospective self-report estimates of recent health. Participants were then invited to enroll in the main portion of the study in the early fall (i.e., the start of the influenza season), which included completion of in-person informed consent approximately one month later. Of the 461 nurses, some chose not to enroll in the larger part of the study (N = 69). Remaining participants (N = 392) were given instructions on completing the stress surveys, sleep diaries, and wearing the actigraph, which they completed for the subsequent 14 days. All study procedures were approved by the Medical City Plano and University of North Texas Institutional Review Boards.
Participants
Interested individuals were first screened for inclusion/exclusion criteria, and eligible participants were invited to participate in the study. Inclusion criteria were: 1) not yet received the current season’s influenza vaccine, 2) between the ages of 18 and 65, and 3) registered nurses actively working at least part-time at one of two regional hospitals. Exclusion criteria were: 1) pregnant/nursing or planning to become pregnant or 2) having an egg allergy. Twenty-six percent of the sample reported working at least one night shift (work between 9pm and 6am) during the 14-day daily diary period and were classified as recent night shift workers. Table 1 reports demographic characteristics for the entire sample and split by recent night shift work status. The majority of participants were female (92%), White (78%), non-Hispanic/Latinx (89%), married (63%), and had children (65%).
Table 1.
Participant Characteristics for the Entire Sample and by Shift Worker Status
| Entire sample |
Day workers |
Night workers |
||||
|---|---|---|---|---|---|---|
| (n = 392) | (n = 291) | (n = 101) | ||||
| M (SD) | M (SD) | M (SD) | p |
Cohen’s
d |
ICC | |
| Age | 39.54 (11.15) | 40.74 (11.00) | 36.12 (10.89) | <0.001 | 0.42 | |
| Baseline perceived stress | 12.19 (6.20) | 11.98 (6.16) | 12.79 (6.29) | 0.263 | 0.17 | |
| Sleep | ||||||
| Actigraphy total sleep time (min.) | 402.10 (50.37) | 408.58 (46.84) | 383.47 (55.50) | <0.001 | 0.49 | 17% |
| Actigraphy sleep efficiency (%) | 86.97 (4.87) | 87.29 (4.73) | 86.05 (5.19) | 0.027 | 0.25 | 32% |
| Self-report total sleep time (min.) | 432.21 (49.20) | 439.51 (43.62) | 411.17 (57.82) | <0.001 | 0.55 | 13% |
| Self-report sleep efficiency (%) | 91.07 (5.10) | 91.77 (4.68) | 89.04 (5.70) | <0.001 | 0.52 | 25% |
| Daily stress | 0.79 (0.60) | 0.81 (0.63) | 0.72 (0.51) | 0.196 | 0.16 | 37% |
| Total night shifts | 1.21 (2.38) | 0.00 (0.00) | 4.71 (2.34) | <0.001 | 2.85 | |
| Total day shifts | 4.85 (3.33) | 6.12 (2.72) | 1.19 (1.96) | <0.001 | 2.08 | |
| Total work shifts (day or night) | 6.06 (2.56) | 6.12 (2.72) | 5.90 (2.06) | 0.466 | 0.09 | |
| Total off days | 6.18 (2.35) | 6.02 (2.39) | 6.64 (2.16) | 0.021 | 0.28 | |
| N (%) | N (%) | N (%) | p | OR | ||
| Gender (female) | 360 (91.8) | 270 (92.8) | 90 (89.1) | <0.001 | 0.96 | |
| Ethnicity (Hispanic/Latinx) | 42 (10.8) | 26 (9.0) | 16 (15.8) | <0.001 | 1.07 | |
| Race | ||||||
| White | 305 (77.8) | 232 (79.7) | 73 (72.3) | <0.001 | 0.93 | |
| African American/Black | 26 (6.6) | 15 (5.2) | 11 (10.9) | <0.001 | 1.06 | |
| American Indian/Alaska Native | 6 (1.5) | 3 (1.0) | 3 (3.0) | <0.001 | 1.02 | |
| Asian | 41 (10.5) | 30 (10.3) | 11 (10.9) | 0.510 | 1.01 | |
| Multiracial | 7 (1.8) | 6 (2.1) | 1 (1.0) | 0.005 | 0.99 | |
| Other | 7 (1.8) | 5 (1.7) | 2 (2.0) | 0.493 | 1.00 | |
| Marital Status | ||||||
| Married | 248 (63.3) | 194 (66.7) | 54 (53.5) | <0.001 | 0.88 | |
| Single | 101 (25.8) | 63 (21.6) | 38 (37.6) | <0.001 | 1.17 | |
| Divorced | 33 (8.4) | 25 (8.6) | 8 (7.9) | 0.403 | 0.99 | |
| Separated | 7 (1.8) | 7 (2.4) | 0 (0.0) | <0.001 | 0.98 | |
| Widowed | 3 (0.8) | 2 (0.7) | 1 (1.0) | 0.229 | 1.00 |
Note. M = mean, SD = standard deviation. Cohen’s d = standardized mean difference (measure of effect size). OR = odds ratio (measure of effect size). ICC = intraclass correlation coefficient (i.e., between-person variation divided by between-person + within-person variation). Day worker = did not work any shifts between 9pm and 6am in the past two weeks (reference group); Night worker = worked at least one shift between 9pm and 6am in the past two weeks. For demographic comparisons, the group that did not identify with that characteristic is the reference group. Baseline perceived stress was assessed using the Perceived Stress Severity scale (10-item version) (Cohen, Kamarck, & Mermelstein, 1994; Cohen & Williamson, 1988).
Measures
Actigraphy-determined sleep.
For 14 days, participants were instructed to continuously wear an Actiwatch Spectrum Pro (Philips Respironics, Bend, OR, USA) on their non-dominant wrist. The Actiwatch is a watch-like device used to infer objective sleep/wake patterns. Participants were asked to push an “event marker” button when they intended to go to sleep and when they got out of bed. Rest intervals were manually set in Actiware software (Version 6.0.8) by two trained individuals using a protocol that systematically relies a combination of event markers, sleep diary data, activity data, and light levels (Rijsketic, Dietch, Wardle-Pinkston, & Taylor, 2020). Briefly, if participants provided event markers that matched sleep diary bed and rise times within 30 minutes, event marker bed and rise times were used. If event markers and sleep diary times were >30 minutes discrepant, activity and light levels were used to confirm whether event markers corresponded to an approximate 50% reduction in light and activity levels. If event markers matched light and activity data within 30 minutes, event markers were used. If they did not match or if event markers were missing, but diaries matched activity and light level reductions within 30 minutes, diary bed and rise times were used. If diaries and activity and light level reductions were >30 minutes discrepant, light and activity levels were used. Discrepancies between the two scorers in setting the rest intervals were resolved by a third person. Data were exported using default settings (10 immobile minutes for sleep onset and offset, medium wake threshold [40 activity counts]). Exported actigraphy data were used to determine total sleep time (i.e., total number of minutes in a rest interval that are scored as sleep by the sleep interval detection algorithm) and sleep efficiency (total sleep time, divided by time elapsed between the start and end time of a given rest interval, multiplied by 100), which were used in the current analyses.
Self-reported sleep.
An electronic version of the Consensus Sleep Diary - Core (Carney et al., 2012) was completed by participants each morning upon awakening using REDCap (Harris et al., 2009). Diaries were used to determine total sleep time (time in bed [with the intention of sleeping] minus the sum of sleep onset latency, wake after sleep onset, and terminal wakefulness) and sleep efficiency (total sleep time divided by time in bed, multiplied by 100). Sleep diaries provide reliable and valid assessments of total sleep time and sleep efficiency, and correlate significantly with actigraphy (rs = .36 to .60), EEG (rs = .18 to .63), and polysomnography (rs = .36 to .59) measures (Dietch & Taylor, 2021; Lichstein et al., 2006; Williams et al., 2020).
Daily stress.
Upon awakening, participants reported on their stress severity levels during the previous day using the item “I felt stressed,” rated on a scale of 0 = not at all to 4 = extremely. Previous studies have used similar single-item approaches to capture daily stress (Petersen, Kecklund, D’Onofrio, Nilsson, & Åkerstedt, 2013).
Daily work schedule and shift worker status.
To classify daily work schedule, in the daily sleep diaries, participants reported whether they worked a night shift (“Did you have to be at work past 9pm OR before 6am?”), a day shift, or were off work during the previous 24-hour period. To classify shift worker status, participants who reported as least one night shift during the 14-day sleep diary collection were classified as a recent night shift worker. Most night workers (55%) worked at least 5 shifts across the 14 days (see Results for more descriptive information on work shifts). Nurses who did not report any night shifts across the 14 days were classified as a recent day worker.
Statistical Analysis Plan
All analyses were conducted in the open-source statistical program R (R Core Team, 2013). All R code and data used for analyses are available at: https://bit.ly/3ieOTD7. Multilevel models were conducted using the R package nlme (Pinheiro, Bates, DebRoy, Sarkar, & R Core Team, 2018). For all multilevel models, level 1 days were nested within level 2 people. Restricted maximum likelihood (REML) was used, which is a robust method for handling missing data using all available information to estimate the model. Intercepts were allowed to vary randomly across people, and slopes were fixed. All models in Aim 1 controlled for the following level 2 (between-person) variables: past 14-day shift worker status (0 = day worker; 1 = night worker); gender (0 = male, 1 = female) and age, given previous studies showing robust differences in sleep by these variables (Reyner, Horne, & Reyner, 1995). At level 1 (within-person level), all models controlled for work schedule during the previous wake period, which was dummy coded into two new variables: day shift and night shift (with days off as the reference group). For analyses examining sleep predicting subsequent stress, stress data were lagged back one day (as stress was reported in the morning, reflecting on stress experienced the previous day; Figure 1). For analyses examining stress predicting subsequent sleep, data were not lagged (as previous day’s stress and previous night’s sleep were reported simultaneously; Figure 1).
Figure 1.
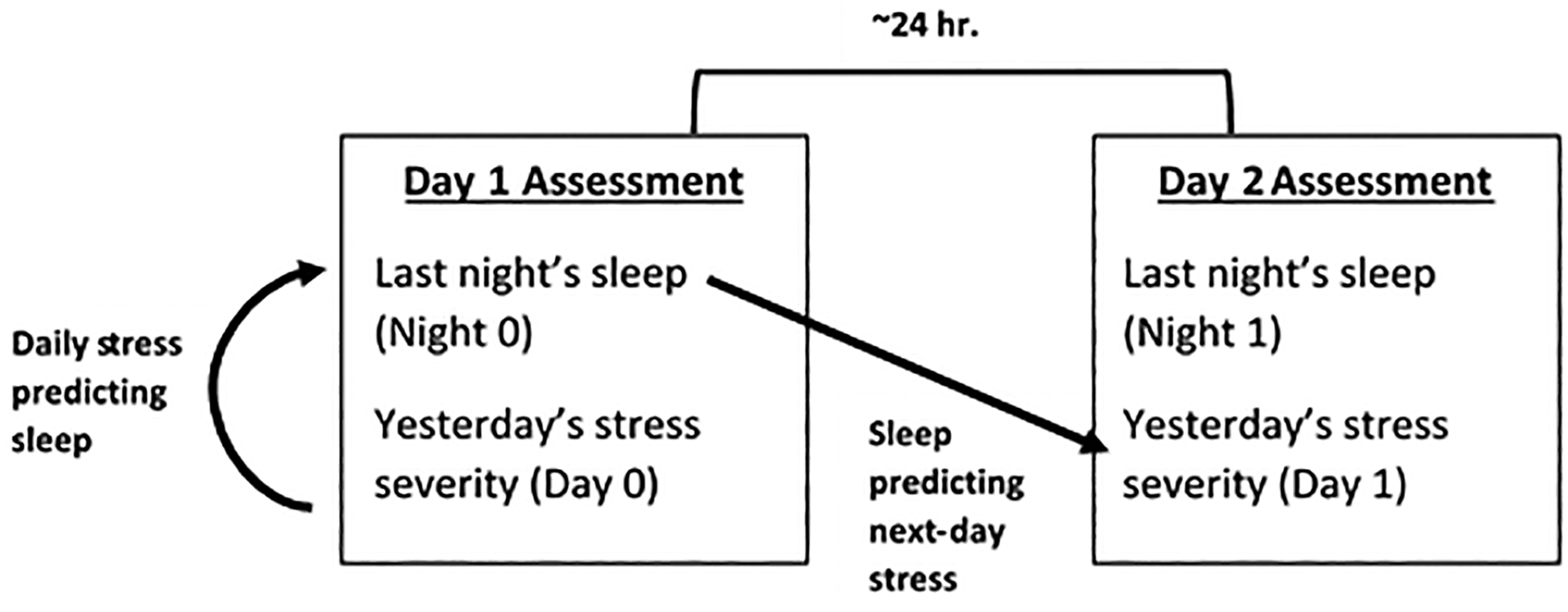
Timing of Daily Assessments and Lagged Analytic Plan
An example equation examining the moderating impact of between-person shift worker status (day vs. night shift worker) on the within-person association between daily stress on sleep (i.e., Aim 2) is shown below:
where: the within-person intercept β0j is modeled as a function of: γ00, the grand mean of sleep when all other predictors equal 0; γ01, the overall effect of shift worker status; γ02, the overall effect of age; γ03, the overall effect of gender; and μ0j, the random deviation of the jth person sleep from the grand mean; the within-person slope between daily stress and sleep β1j is modeled as a function of: γ10, the overall slope between stress and sleep, and γ11, the overall moderation effect of shift worker status on the slope between stress and sleep; and the within-person slope between daily work schedule and sleep β2j is modeled as a function of: γ20, the overall slope between daily work schedule and sleep.
Results
Descriptive results
Descriptive results and participant characteristics (for the entire sample and by shift worker status) are in Table 1. Between-person (i.e., 14-day average) correlations between key study variables are displayed in Table 2.
Table 2.
Between-Person (14-Day Average) Correlations Among Key Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Shift worker status | |||||||
| 2. Actigraphy total sleep time | −.22** | ||||||
| [−.31, −.12] | |||||||
| 3. Actigraphy sleep efficiency | −.11* | .41** | |||||
| [−.21, −.01] | [.32, .49] | ||||||
| 4. Self-report total sleep time | −.25** | .81** | .10* | ||||
| [−.34, −.16] | [.77, .84] | [.00, .20] | |||||
| 5. Self-report sleep efficiency | −.23** | .09 | .33** | .32** | |||
| [−.33, −.14] | [−.01, .19] | [.24, .42] | [.23, .41] | ||||
| 6. Daily stress | −.07 | .04 | .03 | −.07 | −.20** | ||
| [−.16, .03] | [−.06, .14] | [−.07, .13] | [−.17, .03] | [−.29, −.10] | |||
| 7. Gender | −.06 | .15** | .12* | .10 | −.01 | .07 | |
| [−.16, .04] | [.05, .25] | [.02, .22] | [−.00, .20] | [−.11, .09] | [−.03, .17] | ||
| 8. Age | −.18** | −.09 | .15** | −.20** | −.06 | .05 | .07 |
| [−.28, −.08] | [−.19, .01] | [.05, .24] | [−.29, −.10] | [−.16, .04] | [−.05, .15] | [−.03, .17] |
Note. Values in square brackets indicate the 95% confidence interval for each correlation. The confidence interval is a plausible range of population correlations that could have caused the sample correlation.
indicates p < .05.
indicates p < .01.
Gender is coded as 0 = male, 1 = female. Shift worker status is coded as 0 = day worker (did not work any shifts between 9pm and 6am in the past two weeks), 1 = night shift worker (worked at least one shift between 9pm and 6am in the past two weeks).
On average, participants completed 13.07 (SD = 1.6, median = 14, range = 4 to 14) out of 14 possible daily surveys, for an average compliance rate of 93.4%. In the entire sample, participants reported working 476 night shifts (10% of all observations), 1900 day shifts (40% of all observations), and 2422 days off work (50% of all observations). Day workers worked more total shifts (M = 6.12, SD = 2.72) than night shift workers across the 14 days (M = 5.90, SD = 2.06, p <.001, d = 0.47; Table 1). Night shift workers worked an average of 4.71 total night shifts (SD = 2.34, median = 5, range = 1 to 14; Table 1) and an average of 0.74 successive night shifts across the 14 days (SD = 1.16, median = 0, range = 0 to 5). Approximately 19% of night shift workers worked 1 or 2 night shifts across the two weeks; 26% worked 3 or 4 night shifts; 15% worked 5 night shifts; 19% worked 6 night shifts; 17% worked 7 night shifts; 2% worked 8 night shifts; and 3% worked 9+ night shifts. On average, in the entire sample, people reported daily stress scores of 0.79 (SD = 0.60), out of possible scores of 4.
Compared to recent day workers, recent night shift workers were younger, more likely to be Black/African American, American Indian/Alaskan Native, multiracial, Hispanic/Latinx, or single, and less likely to be White, married, or separated (Table 1). Night shift workers also had shorter average self-reported and actigraphy-determined total sleep time and sleep efficiency across the two weeks. Daily stress severity did not significantly differ by shift worker status.
For the repeated measures variables, the intraclass correlation coefficients (i.e., percentage of variation at the between-person level, compared to the within-person level) were 13% for self-reported total sleep time; 17% for actigraphy total sleep time; 25% for self-reported sleep efficiency; 32% for actigraphy sleep efficiency; and 37% for daily stress, suggesting that there was more variation at the within-person level (i.e., from day-to-day) than at the between-person level (i.e., from person-to-person) for each of these constructs.
Aim1: Daily, within-person associations between stress and sleep
At the within-person level, greater daily stress was associated with shorter self-reported but not actigraphy-determined sleep efficiency, covarying for gender, age, daily work schedule, and shift worker status (Table 3). Similarly, greater daily stress was also associated with lower self-reported but not actigraphy-determined total sleep time with the same covariates in the model (Table 4).
Table 3.
Main Effects of Daily Stress, Shift Worker Status, and Daily Work Schedule on Self-Report and Actigraphy Sleep Efficiency
| Self-Report Sleep Efficiency (%) | Actigraphy Sleep Efficiency (%) | |||||
|---|---|---|---|---|---|---|
| Predictors | Estimates | CI | p | Estimates | CI | p |
| (Intercept) | 93.858 | 91.491 – 96.225 | <0.001 | 82.992 | 80.605 – 85.379 | <0.001 |
| Daily stress | −0.636 | −0.943 – −0.329 | <0.001 | −0.127 | −0.396 – 0.141 | 0.352 |
| Age | −0.057 | −0.100 – −0.014 | 0.010 | 0.059 | 0.016 – 0.103 | 0.007 |
| Gender | 0.112 | −1.610 – 1.835 | 0.898 | 2.165 | 0.428 – 3.902 | 0.015 |
| Shift worker status | −2.338 | −3.486 – −1.190 | <0.001 | −0.729 | −1.867 – 0.409 | 0.209 |
| Daily work schedule (day shift) | 1.470 | 0.924 – 2.017 | <0.001 | 0.163 | −0.306 – 0.631 | 0.496 |
| Daily work schedule (night shift) | −0.778 | −1.743 – 0.188 | 0.114 | −0.832 | −1.679 – 0.015 | 0.054 |
| Random Effects | ||||||
| σ2 | 62.72 | 42.14 | ||||
| τ00 | 16.76 ID | 18.45 ID | ||||
| ICC | 0.22 | 0.30 | ||||
| N | 389 ID | 387 ID | ||||
| Observations | 4758 | 4428 | ||||
| Marginal R2 / Conditional R2 | 0.042 / NA | 0.028 / NA | ||||
Note. Bold values represent p <.05 estimates. Gender was coded as 0 = male, 1 = female. Shift worker status was coded as 0 = day worker (worked no night shifts in the past 14 days), 1= night shift worker (worked at least one night shift in the past 14 days). Daily work schedule was dummy coded, with days off as the reference group. Daily stress and daily work schedule are within-person (level 1) variables and all other predictors are between-person (level 2) variables. CI = 95% confidence intervals. p = p-value. For random effects: σ2 represents level 1 variance (within-person), τ00 represents level 2 variance (between-person), ICC represents the intraclass correlation coefficient, N is the total Level 2 sample size, and Observations are the number of Level 1 daily observations.
Table 4.
Main Effects of Daily Stress, Shift Worker Status, and Daily Work Schedule on Self-Report and Actigraphy Total Sleep Time
| Self-Report Total Sleep Time (min.) | Actigraphy Total Sleep Time (min.) | |||||
|---|---|---|---|---|---|---|
| Predictors | Estimates | CI | p | Estimates | CI | p |
| (Intercept) | 479.257 | 456.880 – 501.635 | <0.001 | 416.906 | 392.591 – 441.221 | <0.001 |
| Daily stress | −6.104 | −9.745 – −2.463 | 0.001 | −0.776 | −4.345 – 2.793 | 0.670 |
| Age | −1.185 | −1.588 – −0.782 | <0.001 | −0.618 | −1.055 – −0.180 | 0.006 |
| Gender | 14.385 | −1.829 – 30.598 | 0.082 | 22.437 | 4.811 – 40.062 | 0.013 |
| Shift worker status | 9.412 | −1.819 – 20.644 | 0.100 | 7.520 | −4.416 – 19.456 | 0.217 |
| Daily work schedule (day shift) | 3.024 | −3.709 – 9.758 | 0.379 | −3.560 | −10.006 – 2.887 | 0.279 |
| Daily work schedule (night shift) | −113.151 | −125.091 – −101.210 | <0.001 | −101.524 | −113.229 – −89.819 | <0.001 |
| Random Effects | ||||||
| σ2 | 9905.91 | 8276.16 | ||||
| τ00 | 1107.78 ID | 1513.31 ID | ||||
| ICC | 0.10 | 0.15 | ||||
| N | 389 ID | 387 ID | ||||
| Observations | 4759 | 4428 | ||||
| Marginal R2 / Conditional R2 | 0.107 / NA | 0.090 / NA | ||||
Note. Bold values represent p <.05 estimates. Gender was coded as 0 = male, 1 = female. Shift worker status was coded as 0 = day worker (worked no night shifts in the past 14 days), 1= night shift worker (worked at least one night shift in the past 14 days). Daily work schedule was dummy coded, with days off as the reference group. Daily stress and daily work schedule are within-person (level 1) variables and all other predictors are between-person (level 2) variables. CI = 95% confidence intervals. p = p-value. For random effects: σ2 represents level 1 variance (within-person), τ00 represents level 2 variance (between-person), ICC represents the intraclass correlation coefficient, N is the total Level 2 sample size, and Observations are the number of Level 1 daily observations.
When examining reverse associations at the within-person level, lower self-reported but not actigraphy-determined sleep efficiency was associated with greater next-day stress, covarying for gender, age, daily work schedule, and shift worker status (Table 5). Both longer sleep self-reported and actigraphy-determined total sleep time were associated with lower next-day stress with the same covariates in the model (Table 6).
Table 5.
Main Effects of Self-Report and Actigraphy Sleep Efficiency, Shift Worker Status, and Daily Work Schedule on Next-Day Stress
| Next-Day Stress | Next-Day Stress | |||||
|---|---|---|---|---|---|---|
| Predictors | Estimates | CI | p | Estimates | CI | p |
| (Intercept) | 0.833 | 0.429 – 1.237 | <0.001 | 0.777 | 0.346 – 1.208 | <0.001 |
| Age | 0.001 | −0.004 – 0.007 | 0.711 | 0.001 | −0.004 – 0.007 | 0.628 |
| Gender | 0.145 | −0.075 – 0.365 | 0.195 | 0.116 | −0.110 – 0.341 | 0.315 |
| Shift worker status | −0.057 | −0.110 – 0.086 | 0.436 | −0.051 | −0.197 – 0.096 | 0.498 |
| Daily work schedule (day shift) | 0.091 | 0.039 – 0.143 | 0.001 | 0.085 | 0.032 – 0.139 | 0.002 |
| Daily work schedule (night shift) | 0.042 | −0.053 – 0.137 | 0.384 | 0.061 | −0.039 – 0.160 | 0.232 |
| Self-report sleep efficiency (%) | −0.003 | −0.006 – <−0.001 | 0.041 | |||
| Actigraphy sleep efficiency (%) | −0.002 | −0.006 – 0.001 | 0.218 | |||
| Random Effects | ||||||
| σ2 | 0.52 | 0.52 | ||||
| τ00 | 0.31 ID | 0.32 ID | ||||
| ICC | 0.37 | 0.38 | ||||
| N | 389 ID | 386 ID | ||||
| Observations | 4228 | 3967 | ||||
| Marginal R2 / Conditional R2 | 0.006 / 0.375 | 0.004 / 0.382 | ||||
Note. Bold values represent p <.05 estimates. Gender was coded as 0 = male, 1 = female. Shift worker status was coded as 0 = day worker (worked no night shifts in the past 14 days), 1= night shift worker (worked at least one night shift in the past 14 days). Daily work schedule was dummy coded, with days off as the reference group. Daily stress and daily work schedule are within-person (level 1) variables and all other predictors are between-person (level 2) variables. CI = 95% confidence intervals. p = p-value. For random effects: σ2 represents level 1 variance (within-person), τ00 represents level 2 variance (between-person), ICC represents the intraclass correlation coefficient, N is the total Level 2 sample size, and Observations are the number of Level 1 daily observations.
Table 6.
Main Effects of Self-Report and Actigraphy Total Sleep Time, Shift Worker Status, and Daily Work Schedule on Next-Day Stress
| Next-Day Stress | Next-Day Stress | |||||
|---|---|---|---|---|---|---|
| Predictors | Estimates | CI | p | Estimates | CI | p |
| (Intercept) | 0.919 | 0.600 – 1.238 | <0.001 | 0.879 | 0.552 – 1.206 | <0.001 |
| Age | <0.001 | −0.005 – 0.006 | 0.907 | 0.001 | −0.005 – 0.007 | 0.766 |
| Gender | 0.156 | −0.065 – 0.376 | 0.165 | 0.129 | −0.097 – 0.355 | 0.262 |
| Shift worker status | −0.040 | −0.183 – 0.103 | 0.580 | −0.043 | −0.190 – 0.104 | 0.567 |
| Daily work schedule (day shift) | 0.087 | 0.035 – 0.138 | 0.001 | 0.081 | 0.028 – 0.135 | 0.003 |
| Daily work schedule (night shift) | −0.042 | −0.140 – 0.056 | 0.401 | −0.012 | −0.115 – 0.091 | 0.814 |
| Self-report total sleep time (min.) | −0.001 | −0.001 – <−0.001 | <0.001 | |||
| Actigraphy total sleep time (min.) | −0.001 | −0.001 – <−0.001 | <0.001 | |||
| Random Effects | ||||||
| σ2 | 0.52 | 0.52 | ||||
| τ00 | 0.31 ID | 0.32 ID | ||||
| ICC | 0.37 | 0.38 | ||||
| N | 389 ID | 386 ID | ||||
| Observations | 4229 | 3967 | ||||
| Marginal R2 / Conditional R2 | 0.013 / 0.382 | 0.010 / 0.388 | ||||
Note. Bold values represent p <.05 estimates. Gender was coded as 0 = male, 1 = female. Shift worker status was coded as 0 = day worker (worked no night shifts in the past 14 days), 1= night shift worker (worked at least one night shift in the past 14 days). Daily work schedule was dummy coded, with days off as the reference group. Daily stress and daily work schedule are within-person (level 1) variables and all other predictors are between-person (level 2) variables. CI = 95% confidence intervals. p = p-value. For random effects: σ2 represents level 1 variance (within-person), τ00 represents level 2 variance (between-person), ICC represents the intraclass correlation coefficient, N is the total Level 2 sample size, and Observations are the number of Level 1 daily observations.
Aim 2: Moderation by between-person shift worker status
At the between-person level, shift worker status in the past 14 days (i.e., night worker vs. day worker) did not moderate the association between either self-reported or actigraphy-determined sleep efficiency with next-day stress, or stress with that night’s self-reported or actigraphy-determined sleep efficiency or total sleep time. However, shift worker status moderated associations between self-reported and actigraphy-determined total sleep time predicting next-day stress: Shorter self-reported total sleep time was associated with higher next-day stress for day workers (Figure 2, b = −0.0013, p < .0001), but not for night shift workers (Figure 2, b = −0.0001, p = .7578). Similarly, shorter actigraphy-determined total sleep time was associated with higher next-day stress for day workers (Figure 3, b = −0.0013, p < .0001), but not for night shift workers (Figure 3, b = 0.0001, p = .6045).
Figure 2. Between-Person Shift Worker Status as a Moderator of the Within-Person Association between Self-Reported Total Sleep Time and Next-Day Stress.
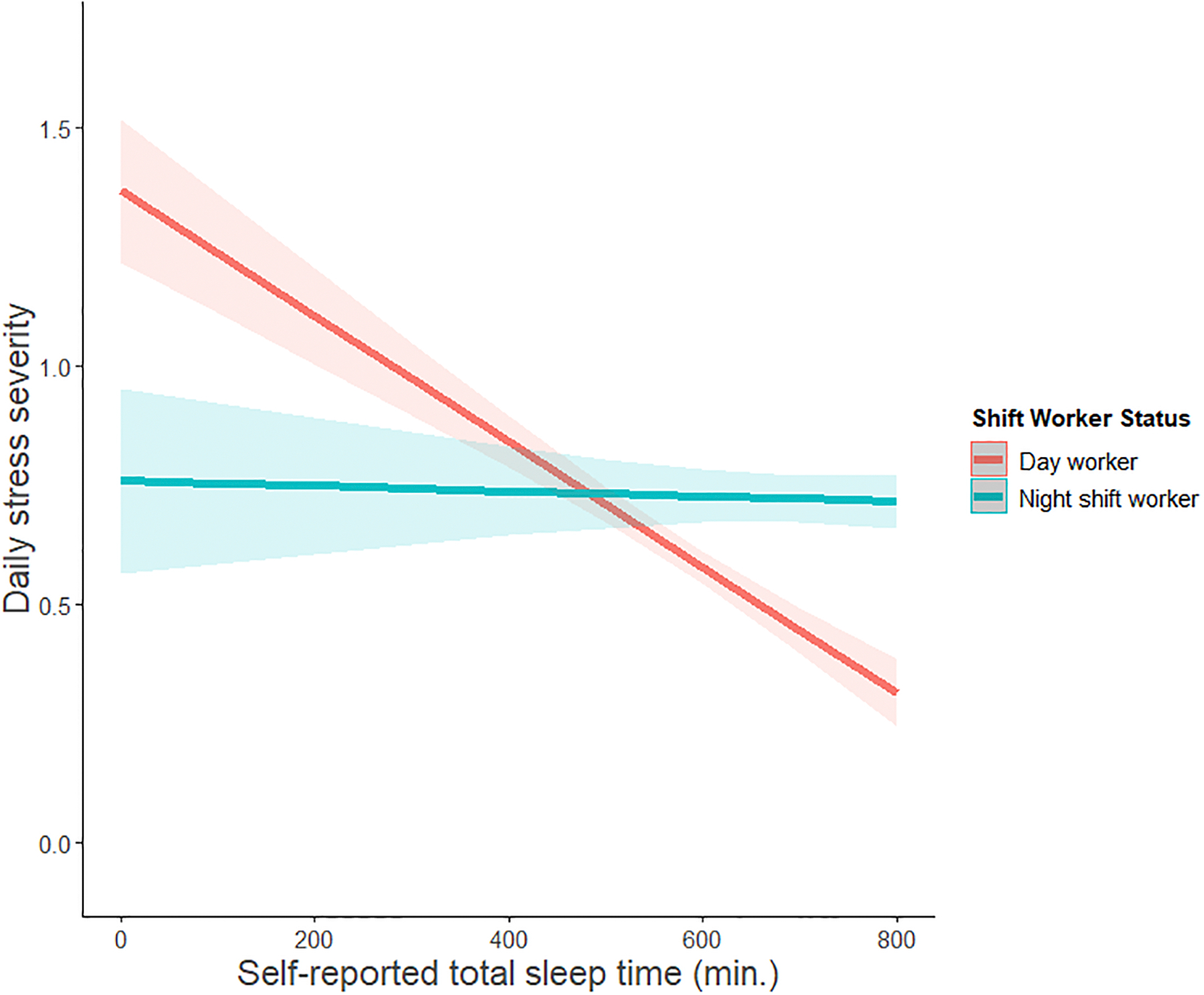
Shift worker status: Day worker = did not work any shifts between 9pm and 6am in the past two weeks; Night shift worker = worked at least one shift between 9pm and 6am in the past two weeks. Shorter self-reported total sleep time was associated with higher next-day stress for day workers (b = −0.0013, p < 0.0001), but not for night shift workers (b = −0.0001, p = 0.7578).
Figure 3. Between-Person Shift Worker Status as a Moderator of the Within-Person Association between Actigraphy-Determined Total Sleep Time and Next-Day Stress.
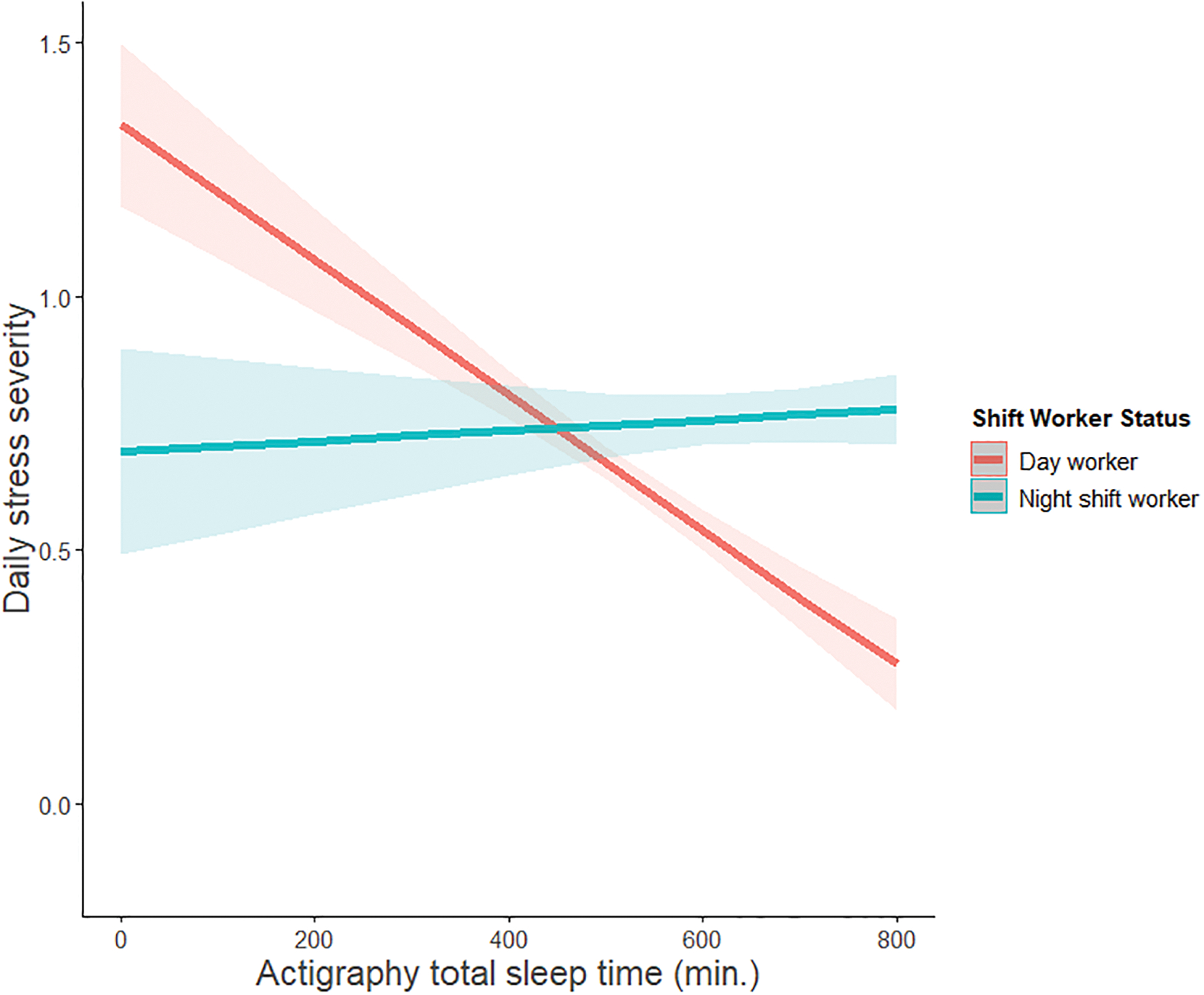
Shift worker status: Day worker = did not work any shifts between 9pm and 6am in the past two weeks; Night shift worker = worked at least one shift between 9pm and 6am in the past two weeks. Shorter actigraphy-determined total sleep time was associated with higher next-day stress for day workers (b = −0.0013, p < 0.0001), but not for night shift workers (b = 0.0001, p = 0.6045).
Aim 2: Moderation by within-person, daily work schedule
Next, we examined the within-person associations between daily stress and sleep in Aim 1 separately in day workers and night workers, and how these varied as a function of an individual’s daily work schedule (day shift vs. day off among day workers, and day shift vs. night shift vs. day off among night workers; Supplementary Materials). Among recent night shift workers, all daily stress-sleep associations were null. However, among day workers, greater daily stress was associated with shorter self-reported total sleep time (b = −5.88, p < .01) and lower self-reported sleep efficiency (b = −0.74, p < .001). Shorter self-reported total sleep time (b = −.001, p < .001), shorter actigraphy total sleep time (b = −.001, p < .001), and lower self-reported sleep efficiency (b = −.004, p < .05) were associated with greater next-day stress among day workers. Only one significant moderation effect of daily work schedule emerged: Among day workers, lower self-reported sleep efficiency was associated with greater next-day stress on work days (b = −0.0087, p = .0019), but not off days (b = −0.0003, p = .9124; Supplementary Table S5 and Supplementary Figure S1).
Discussion
This was the first study to examine how daily associations between stress and sleep may vary as a function of nurses’ typical and daily work schedules. In the entire sample, daily stress and sleep were associated in a bidirectional fashion. Specifically, days with greater stress were associated with lower self-reported sleep efficiency and shorter sleep duration. Shorter self-reported and actigraphy sleep duration, as well as lower self-reported sleep efficiency were associated with greater next-day stress. Our between-person moderation findings also revealed that compared to recent night shift workers, day workers had greater increases in next-day stress following nights with shorter self-reported sleep duration. This finding suggests night shift workers may be less susceptible to the detrimental effects of short sleep on next-day psychological stress. At the within-person level, an individual’s daily work schedule largely did not impact stress and sleep associations. Together, our findings suggest the importance of examining both stable and dynamic facets of an individuals’ work schedule on daily stress and sleep.
Our findings extend previous research on daily stress and sleep conducted in young or midlife working adults by examining these associations among a unique sample of day and night shift working nurses (Doane & Thurston, 2014; Lee et al., 2017; Yap et al., 2020). Daily stress may increase negative emotions and rumination which heighten and sustain sympathetic nervous system activity and cognitive arousal that interfere with sleep. Indeed, stressor-related rumination appears to explain subsequent impairments in sleep (Zoccola, Dickerson, & Lam, 2009), and being bothered or upset at work is associated with poorer subjective sleep quality (Burgard & Ailshire, 2009). Future studies should examine how emotion and rumination may mediate associations between daily stressful events and sleep among nurses and other populations.
Interestingly, stress was only a predictor of self-reported but not actigraphy-derived sleep parameters. In contrast to actigraphy, which captures activity levels, sleep diaries capture an individual’s perceptual awareness and interpretation of sleep/wake, and thus, may be influenced by one’s current emotional state or arousal level (Slavish et al., 2021; Williams et al., 2020). Further, previous day’s stress and previous night’s sleep were reported simultaneously in the sleep diaries upon awakening, which may have confounded our results. Despite these potential reporting biases, sleep diaries are the primary means by which insomnia is diagnosed and may have important clinical utility not offered by actigraphy, EEG, or polysomnography measures of sleep (Carney et al., 2012; Williams et al., 2020).
Looking at reverse pathways from sleep to next-day stress, we found that shorter sleep duration (both self-reported and actigraphy) and lower self-reported sleep efficiency were associated with greater next-day stress. Nights characterized by shorter and more fragmented sleep may increase cortisol (Jackowska, Ronaldson, Brown, & Steptoe, 2016; Wright et al., 2015) and cardiovascular activity (Jackowska et al., 2016), which heighten subjective arousal the next day. Individuals who experience a bad night of sleep may also worry how sleep loss will affect their daytime performance (Thielsch et al., 2015). Sleep loss and poor sleep quality can also deplete coping resources and impair emotion regulation, rendering individuals more reactive to next-day stressors. For example, among medical residents, sleep loss amplifies negative emotions in response to disruptive work events, and it is possible similar results may extend to nurses (Zohar, Tzischinsky, Epstein, & Lavie, 2005). These daytime impairments may have particularly dire consequences among nurses, impairing their ability to concentrate and provide effective patient care in high stakes medical situations.
Extending previous research, we also examined the unique impact of work schedule on daily stress and sleep associations. On average, being a recent (past two week) night shift worker had an impact on daily stress and sleep, but an individual’s day-to-day fluctuations in work schedule largely did not. Nights with shorter self-reported and actigraphy sleep duration were associated with greater next-day stress among recent day workers but not night workers. It may be that night shift nurses are more accustomed to disturbances in sleep or have developed more effective coping strategies or compensatory behaviors for dealing with lost sleep (e.g., caffeine use, bright light exposure, changes in meal timing). It is also possible that night shift workers have fewer work tasks and thus less stress. We found night shift workers reported poorer sleep, but also somewhat lower levels of daily stress than day workers (although this was not a statistically significant difference). Future studies should examine stressor frequency, severity, and type by work schedule. For example, night and day shift workers may face similar levels of work stress, but different levels of home stress. When night shift workers do experience short sleep duration, it may make less of an impact on their next-day perceptions of stress. Partially supporting this idea, several studies have shown that there are substantial trait-like individual differences in susceptibility to cognitive and mood deficits and following sleep loss (Van Dongen, Baynard, Maislin, & Dinges, 2004).
Those individuals who are less affected by sleep disturbances may also self-select into night shift work. Greater “sleep reactivity” (i.e., trait‐like vulnerability to stress-related disturbances in sleep) is a strong predictor of whether shift-working individuals will go on to develop shift work disorder (Kalmbach, Pillai, Cheng, Arnedt, & Drake, 2015). In fact, the odds of developing shift work disorder after transitioning from day to rotating night shifts is over five times greater among individuals with high levels of premorbid sleep reactivity (Kalmbach et al., 2015). Finally, it is also possible there is a common cause of both increased tolerance to shift work and lower stress levels. For example, some personality characteristics linked to lower perceived stress (e.g., low neuroticism, high extraversion) are also associated with greater shift work tolerance (Saksvik, Bjorvatn, Hetland, Sandal, & Pallesen, 2011). Together, these results suggest that night and day shift workers may exhibit different pre-existing characteristics or behaviors that differentially impact their daily patterns of stress and sleep.
Contrary to our expected hypotheses, when we examined the impact of daily work schedule separately in recent night vs. day shift workers, we did not find it moderated most associations between stress and sleep. In other words, associations between daily stress and sleep were relatively similar regardless of whether one was working a night shift, day shift, or was off work on any given day. These findings are in contrast with some studies, which have shown differential levels of stress and sleep on days after having worked a night shift vs. a day shift (Garde et al., 2009; Khan et al., 2019). Instead, our results suggest that one’s typical or recent cumulative (i.e., past two week) work schedule may influence stress and sleep more than day-to-day fluctuations in work schedules. When we examined stress-sleep associations separately by shift work status, it appears most significant results in the overall sample were driven by the day workers. However, these results should be interpreted cautiously, as the day worker group was nearly three times the size of the night worker group. From an intervention standpoint, our findings tentatively suggest a need to differentially target day and night shift workers, or possibly equip them with different tools to cope with stress and lost or poor quality sleep.
Limitations and Future Directions
Although this study has several notable strengths (e.g., large sample of day- and night shift-working nurses; 5488 possible measurement occasions; self-report and actigraphy repeated measures of sleep), there are some limitations warranting future research. First, our sample was relatively healthy, with nurses reporting low stress and relatively good sleep on average. These results are consistent with other nurse samples (Rutledge et al., 2009). However, we observed substantial within-person variability in stress and sleep, suggesting some days were characterized by high stress and severely disturbed sleep. These within-person fluctuations may accumulate over time to predict impaired health outcomes. Additionally, the measurement scale for total sleep time and sleep efficiency (i.e., in minutes and percentage from 0 to 100) may have contributed to seemingly small effect sizes. Further work is needed to determine if our within-person effects translate to meaningful clinical changes. Building on prior work, we measured stress across 14 days, as opposed to a more traditional single time point retrospective questionnaire with multiple items. Daily measures have greater ecological validity and reduced recall bias (Almeida, 2005).
We also measured retrospective self-reported stress and sleep concurrently and only once daily. Ideally, multiple assessments of stress would be taken daily in real-time (e.g., via ecological momentary assessment) to capture real-time experiences and dynamics across a day. However, additional assessments should always be weighed against potential participant burden, particularly in high-burden populations such as essential health care workers. More nuanced and objective assessments of physiological stress responses (e.g., blood pressure, cortisol, heart rate), are also needed, as well as investigations of the effects of specific types of stressors on sleep (e.g., interpersonal stressors vs. work stressors vs. home stressors).
We also did not exclude individuals based on sleep disorders (e.g., obstructive sleep apnea, insomnia), mental health, or chronic health conditions, which will be important to assess in future studies. We considered controlling for baseline levels of these variables, but that is generally discouraged when there are known group differences in the dependent variable (Miller & Chapman, 2001), as is the case for sleep patterns among those with vs. without chronic health conditions (e.g., Taylor, Lichstein, Durrence, Reidel, & Bush, 2005; Taylor et al., 2007). Future studies should assess other moderators of the associations we observed, including chronotype, gender, age, and race/ethnicity and discrimination. Evening chronotypes, women, older adults, and racial/ethnic minorities typically report worse sleep on average (Lichstein, Durrence, Riedel, Taylor, & Bush, 2004; Ong, Huang, Kuo, & Manber, 2007). Finally, it will also be important to examine how our results generalize to nurses across different countries or cultures, although research suggests a high prevalence of burnout, stress, and sleep disturbances among nurses worldwide (An et al., 2016; Cénat et al., 2021; Woo, Ho, Tang, & Tam, 2020).
Conclusion
Work experiences can have a strong impact on daily experiences of stress and sleep. Our findings suggest daily stress and sleep are bidirectionally associated among nurses. However, day shift working nurses were less resilient to the effects of short sleep on next-day stress compared to night shift workers. Particular attention must be paid to supporting nurses to mitigate potential negative effects on downstream health outcomes. Given the nursing profession is expected to grow over the next decade, this represents a particularly timely issue to address. We urge future sleep researchers to consider the important role that both daily and typical work schedules may play in shaping individuals’ everyday experiences of stress and sleep.
Supplementary Material
Acknowledgements:
This research supported by National Institute of Allergy and Infectious Diseases grant R01AI128359-01 (PIs: Kelly & Taylor). We wish to thank the participants, research assistants, and nurse principal investigators who helped contribute to this research.
Footnotes
Conflict of interests: DCS, JRD, HSK, BAM, OG, JFW, YY, KK, CR, and DJT report no conflicts of interest.
References
- Åkerstedt T, Fredlund P, Gillberg M, & Jansson B (2002). Work load and work hours in relation to disturbed sleep and fatigue in a large representative sample. Journal of Psychosomatic Research, 53(1), 585–588. [DOI] [PubMed] [Google Scholar]
- Åkerstedt T, Orsini N, Petersen H, Axelsson J, Lekander M, & Kecklund G (2012). Predicting sleep quality from stress and prior sleep – A study of day-to-day covariation across sixweeks. Sleep Medicine, 13(6), 674–679. [DOI] [PubMed] [Google Scholar]
- Almeida DM (2005). Resilience and vulnerability to daily stressors assessed via diary methods. Current Directions in Psychological Science, 14, 64–68. [Google Scholar]
- An FR, Qi YK, Zeng JY, Ding YM, Chiu HF, Ungvari GS, … Xiang YT (2016). The Prevalence of Insomnia, Its Demographic Correlates, and Treatment in Nurses Working in Chinese Psychiatric and General Hospitals. Perspect Psychiatr Care, 52(2), 88–94. [DOI] [PubMed] [Google Scholar]
- Burgard SA, & Ailshire JA (2009). Putting work to bed: stressful experiences on the job and sleep quality. Journal of Health and Social Behavior, 50(4), 476–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton OM, Lee S, Beverly C, Berkman LF, Moen P, Kelly EL, … Almeida DM (2016). Work-Family Conflict and Employee Sleep: Evidence from IT Workers in the Work, Family and Health Study. Sleep, 39(10), 1871–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, & Morin CM (2012). The consensus sleep diary: Standardizing prospective sleep self-monitoring. Sleep, 35(2), 287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat JM, Blais-Rochette C, Kokou-Kpolou CK, Noorishad PG, Mukunzi JN, McIntee SE, … Labelle PR (2021). Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Research, 295, 113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1994). Perceived stress scale. Measuring stress: A guide for health and social scientists, 235–283. [Google Scholar]
- Cohen S, & Williamson GM (1988). Perceived stress in a probability sample of the United States. In Spacapan S & Oskamp S (Eds.), The social psychology of health (pp. 31–67). Newbury Park, CA: Sage. [Google Scholar]
- Dietch JR, & Taylor DJ (2021). Evaluation of the Consensus Sleep Diary in a community sample: comparison with single-channel EEG, actigraphy, and retrospective questionnaire. J Clin Sleep Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doane LD, & Thurston EC (2014). Associations among sleep, daily experiences, and loneliness in adolescence: evidence of moderating and bidirectional pathways. Journal of Adolescence, 37(2), 145–154. [DOI] [PubMed] [Google Scholar]
- Flo E, Pallesen S, Magerøy N, Moen BE, Grønli J, Nordhus IH, & Bjorvatn B (2012). Shift work disorder in nurses–assessment, prevalence and related health problems. PLoS ONE, 7(4), e33981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garde AH, Hansen AM, & Hansen J (2009). Sleep length and quality, sleepiness and urinary melatonin among healthy Danish nurses with shift work during work and leisure time. International Archives of Occupational and Environmental Health, 82(10), 1219–1228. [DOI] [PubMed] [Google Scholar]
- Geiger-Brown J, Rogers VE, Trinkoff AM, Kane RL, Bausell RB, & Scharf SM (2012). Sleep, Sleepiness, Fatigue, and Performance of 12-Hour-Shift Nurses. Chronobiology International, 29(2), 211–219. [DOI] [PubMed] [Google Scholar]
- Gerber M, Hartmann T, Brand S, Holsboer-Trachsler E, & Pühse U (2010). The relationship between shift work, perceived stress, sleep and health in Swiss police officers. Journal of Criminal Justice, 38(6), 1167–1175. [Google Scholar]
- Hanson MD, & Chen E (2010). Daily stress, cortisol, and sleep: the moderating role of childhood psychosocial environments. Health Psychology, 29(4), 394–402. [DOI] [PubMed] [Google Scholar]
- Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde J (2009). Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackowska M, Ronaldson A, Brown J, & Steptoe A (2016). Biological and psychological correlates of self-reported and objective sleep measures. J. Psychosom. Res, 84, 52–55. [DOI] [PubMed] [Google Scholar]
- Jordan TR, Khubchandani J, & Wiblishauser M (2016). The Impact of Perceived Stress and Coping Adequacy on the Health of Nurses: A Pilot Investigation. Nursing Research and Practice, 2016, 5843256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kageyama T, Nishikido N, Kobayashi T, Oga J, & Kawashima M (2001). Cross-sectional survey on risk factors for insomnia in Japanese female hospital nurses working rapidly rotating shift systems. Journal of Human Ergology, 30(1–2), 149–154. [PubMed] [Google Scholar]
- Kalmbach DA, Pillai V, Cheng P, Arnedt JT, & Drake CL (2015). Shift work disorder, depression, and anxiety in the transition to rotating shifts: the role of sleep reactivity. Sleep Medicine, 16(12), 1532–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan W, Conduit R, Kennedy G, & Jackson ML (2019). The effect of rotating shift on sleep, mood, and stress of Australian paramedics: A field study. Journal of Sleep Research, 28(S1), e133_12913. [Google Scholar]
- Kim M-J, Son K-H, Park H-Y, Choi D-J, Yoon C-H, Lee H-Y, … Cho M-C (2013). Association between shift work and obesity among female nurses: Korean Nurses’ Survey. BMC Public Health, 13(1), 1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Crain TL, McHale SM, Almeida DM, & Buxton OM (2017). Daily antecedents and consequences of nightly sleep. Journal of Sleep Research, 26(4), 498–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichstein KL, Durrence HH, Riedel BW, Taylor DJ, & Bush AJ (2004). Epidemiology of sleep: Age, gender, and ethnicity: Psychology Press. [Google Scholar]
- Lichstein KL, Stone KC, Donaldson J, Nau SD, Soeffing JP, Murray D, … Aguillard RN (2006). Actigraphy validation with insomnia. Sleep, 29(2), 232–239. [PubMed] [Google Scholar]
- Lin P-C, Chen C-H, Pan S-M, Pan C-H, Chen C-J, Chen Y-M, … Wu M-T (2012). Atypical work schedules are associated with poor sleep quality and mental health in Taiwan female nurses. International Archives of Occupational and Environmental Health, 85(8), 877–884. [DOI] [PubMed] [Google Scholar]
- Miller GA, & Chapman JP (2001). Misunderstanding analysis of covariance. Journal of Abnormal Psychology, 110(1), 40–48. [DOI] [PubMed] [Google Scholar]
- Ong JC, Huang JS, Kuo TF, & Manber R (2007). Characteristics of insomniacs with self-reported morning and evening chronotypes. J Clin Sleep Med, 3(3), 289–294. [PMC free article] [PubMed] [Google Scholar]
- Øyane NMF, Pallesen S, Moen BE, Akerstedt T, & Bjorvatn B (2013). Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS ONE, 8(8), e70228–e70228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen H, Kecklund G, D’Onofrio P, Nilsson J, & Åkerstedt T (2013). Stress vulnerability and the effects of moderate daily stress on sleep polysomnography and subjective sleepiness. Journal of Sleep Research, 22(1), 50–57. [DOI] [PubMed] [Google Scholar]
- Pinheiro J, Bates D, DebRoy S, Sarkar D, & R Core Team. (2018). nlme: Linear and Nonlinear Mixed Effects Models (Version 3.1–137). Retrieved from https://CRAN.R-project.org/package=nlme
- R Core Team. (2013). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. Retrieved from http://www.R-project.org/ [Google Scholar]
- Reyner LA, Horne JA, & Reyner A (1995). Gender- and age-related differences in sleep determined by home-recorded sleep logs and actimetry from 400 adults. Sleep, 18(2), 127–134. [PubMed] [Google Scholar]
- Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, & Nissen C (2010). The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Medicine Reviews, 14(1), 19–31. [DOI] [PubMed] [Google Scholar]
- Rijsketic JM, Dietch JR, Wardle-Pinkston S, & Taylor DJ (2020). Actigraphy (Actiware) Scoring Hierarchy Manual. Retrieved from insomnia.arizona.edu/actigraphy
- Rutledge T, Stucky E, Dollarhide A, Shively M, Jain S, Wolfson T, … Dresselhaus T (2009). A real-time assessment of work stress in physicians and nurses. Health Psychology, 28(2), 194–200. [DOI] [PubMed] [Google Scholar]
- Saksvik IB, Bjorvatn B, Hetland H, Sandal GM, & Pallesen S (2011). Individual differences in tolerance to shift work--a systematic review. Sleep Medicine Reviews, 15(4), 221–235. [DOI] [PubMed] [Google Scholar]
- Scott LD, Hwang W-T, Rogers AE, Nysse T, Dean GE, & Dinges DF (2007). The relationship between nurse work schedules, sleep duration, and drowsy driving. Sleep, 30(12), 1801–1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma P, Davey A, Davey S, Shukla A, Shrivastava K, & Bansal R (2014). Occupational stress among staff nurses: Controlling the risk to health. Indian Journal of Occupational and Environmental Medicine, 18(2), 52–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin NL, Almeida DM, Crain TL, Kossek EE, Berkman LF, & Buxton OM (2017). Bidirectional, temporal associations of sleep with positive events, affect, and stressors in daily life across a week. Annals of Behavioral Medicine, 51, 402–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sladek MR, Doane LD, & Breitenstein RS (2020). Daily rumination about stress, sleep, and diurnal cortisol activity. Cognition and Emotion, 34(2), 188–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavish DC, Dietch JR, Messman B, Asbee J, Veeramachaneni K, Scott B, & Taylor DJ (2021). The cycle of daily stress and sleep: Sleep measurement matters. Annals of Behavioral Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smiley RA, Lauer P, Bienemy C, Berg JG, Shireman E, Reneau KA, & Alexander M (2018). The 2017 National Nursing Workforce Survey. Journal of Nursing Regulation, 9(3), S1–S88. [Google Scholar]
- Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, & Bush AJ (2005). Epidemiology of insomnia, depression, and anxiety. Sleep, 28(11), 1457–1464. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, & Bush AJ (2007). Comorbidity of chronic insomnia with medical problems. Sleep, 30(2), 213–218. [DOI] [PubMed] [Google Scholar]
- Thielsch C, Ehring T, Nestler S, Wolters J, Kopei I, Rist F, … Andor T (2015). Metacognitions, worry and sleep in everyday life: Studying bidirectional pathways using Ecological Momentary Assessment in GAD patients. J. Anxiety Disord, 33, 53–61. [DOI] [PubMed] [Google Scholar]
- Vahle-Hinz T, Bamberg E, Dettmers J, Friedrich N, & Keller M (2014). Effects of work stress on work-related rumination, restful sleep, and nocturnal heart rate variability experienced on workdays and weekends. Journal of Occupational Health Psychology, 19(2), 217–230. [DOI] [PubMed] [Google Scholar]
- Van Dongen HP, Baynard MD, Maislin G, & Dinges DF (2004). Systematic interindividual differences in neurobehavioral impairment from sleep loss: evidence of trait-like differential vulnerability. Sleep, 27(3), 423–433. [PubMed] [Google Scholar]
- Williams JM, Taylor DJ, Slavish DC, Gardner CE, Zimmerman MR, Patel K, … Estevez R (2020). Validity of actigraphy in young adults with insomnia. Behavioral Sleep Medicine, 18, 91–106. [DOI] [PubMed] [Google Scholar]
- Woo T, Ho R, Tang A, & Tam W (2020). Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J Psychiatr Res, 123, 9–20. [DOI] [PubMed] [Google Scholar]
- Wright KP, Drake AL, Frey DJ, Fleshner M, Desouza CA, Gronfier C, & Czeisler CA (2015). Influence of sleep deprivation and circadian misalignment on cortisol, inflammatory markers, and cytokine balance. Brain, Behavior, and Immunity, 47, 24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yap Y, Slavish DC, Taylor DJ, Bei B, & Wiley JF (2020). Bi-directional relations between stress and self-reported and actigraphy-assessed sleep: A daily intensive longitudinal study. Sleep, 43(3), zsz250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoccola PM, Dickerson SS, & Lam S (2009). Rumination predicts longer sleep onset latency after an acute psychosocial stressor. Psychosomatic Medicine, 71(7), 771–775. [DOI] [PubMed] [Google Scholar]
- Zohar D, Tzischinsky O, Epstein R, & Lavie P (2005). The effects of sleep loss on medical residents’ emotional reactions to work events: a cognitive-energy model. Sleep, 28, 47–54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


