Abstract
Purpose:
Fibular hemimelia has denoted a spectrum of postaxial longitudinal deficiency with fibular aplasia/hypoplasia; the term “terminal hemimelia” is reserved for patients with postaxial longitudinal deficiency having a normal fibula. We aimed to delineate the characteristics of terminal hemimelia.
Methods:
In total, 30 patients with postaxial longitudinal deficiency who had a normal or hypoplastic fibula and visited our institution between 1992 and 2022 were reviewed. Patients were divided into terminal hemimelia and classic fibular hemimelia groups, and their demographic characteristics and clinical and radiographic findings were compared.
Results:
Femoral shortening, knee valgus, and tibial spine hypoplasia were less common in terminal hemimelia (n = 13) than in classic fibular hemimelia (n = 17) (p = 0.03, p < 0.001, and p = 0.003, respectively). None of the patients in the terminal hemimelia group exhibited knee instability, whereas 12% of patients with classic fibular hemimelia did. Ball-and-socket ankle and absence of lateral rays were commonly observed in both groups. However, tarsal coalition was observed less frequently in terminal hemimelia (p = 0.004). All terminal hemimelia patients exhibited a painless plantigrade foot without ankle instability. Despite limb-length discrepancy at maturity averaging 40.4 mm for terminal hemimelia and 67.0 mm for classic fibular hemimelia (p < 0.001), patients with terminal hemimelia, except for one, exhibited > 20 mm of limb-length discrepancy. However, 46% of them underwent limb-length equalization procedures, mostly single-stage tibial lengthening, at a mean age of 11.2 years.
Conclusion:
Terminal hemimelia may present with a milder phenotype than classic fibular hemimelia. It mainly overlaps with the symptoms of fibular hemimelia below the ankle joint and manifests as limb-length discrepancy. However, a considerable number of patients with terminal hemimelia required limb-length equalization procedures, for example single-stage tibial lengthening.
Level of evidence:
level IV.
Keywords: Hemimelia, postaxial longitudinal deficiency, ball-and-socket ankle, absence of lateral foot ray, limb-length discrepancy
Introduction
Fibular hemimelia (FH) has been used to denote postaxial longitudinal deficiency (PALD) with a broad spectrum.1–5 FH presents as fibular aplasia or hypoplasia, and other associated anomalies of the lower extremity, such as limb-length discrepancy (LLD), lateral femoral condyle hypoplasia with knee valgus, tibial spine hypoplasia, anterior cruciate ligament (ACL) deficiency, tibial bowing, ball-and-socket ankle joint, tarsal coalition, and absence of lateral foot rays.1–6 The term “FH” derives from the notion that fibular aplasia/hypoplasia is a representative manifestation of PALD spectrum, although the degree of fibular deficiency varies markedly from complete absence of the fibula to fibular hypoplasia.1,6–9
However, two previous studies reported patients who may belong to the PALD category but have a normal fibula.2,5 Searle et al. 2 proposed to classify them as having type 0 FH. Baek et al. 5 suggested describing this entity as “terminal hemimelia” (TH) instead, highlighting that this pathology mainly affected the terminal regions of the lower extremity. We also focused on PALD with a normal fibula or TH, which can be the blind spot in the PALD spectrum, and conducted a comparative analysis to delineate the characteristics of it. In this study, we aimed to compare the clinical and radiographic manifestations of TH with classic FH, which is defined as PALD with a hypoplastic fibula, and further propose treatment options for TH.
Materials and methods
A retrospective analysis of the medical and radiographic records for children diagnosed with PALD between December 1992 and January 2022 at a single tertiary children’s hospital was performed. Ethical approval for the study was obtained from the Institutional Review Board (IRB No. H-2204-139-1319). Informed consent was waived because of the retrospective nature of the study and use of anonymous clinical data for analysis.
Study population
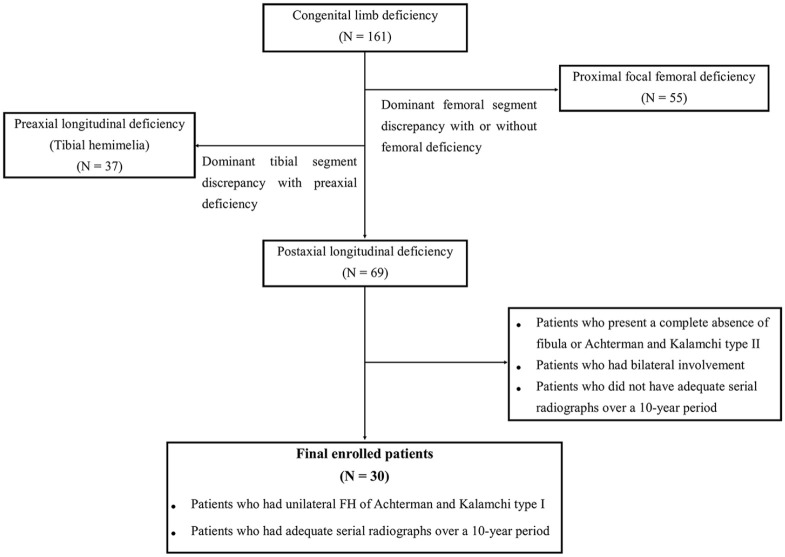
Among a total of 161 patients with congenital limb deficiency, 55 who had proximal femoral focal deficiency predominantly were excluded. Of these, 37 patients with preaxial longitudinal deficiency (tibial hemimelia) were also excluded. Among the remaining 69 patients with PALD, 30 patients who had unilateral FH of Achterman and Kalamchi type I and had adequate serial radiographs over a 10-year period were included in this study (Figure 1). Patients with a complete absence of the fibula or Achterman and Kalamchi type II were excluded because this study focused on the comparison of clinical and radiographic manifestations between PALD with a normal and a hypoplastic fibula.
Figure 1.
Patient selection and exclusion criteria.
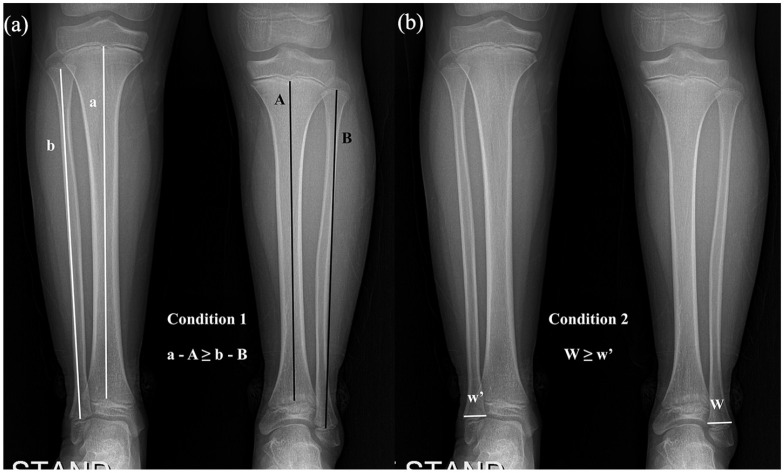
The 30 enrolled patients were divided into TH and classic FH groups based on their fibular status. This was defined as PALD with a normal fibula when the length discrepancy of the fibula to the unaffected side was not larger than that of the tibia (Figure 2(a)) and the distal metaphysis was not narrower than that of the unaffected side (Figure 2(b)).2,5,10 The lengths of the fibula and tibia were measured as the distance from the center of the proximal physis to the center of the distal physis of each bone, and the width of the fibula was measured at the juxta-physeal metaphysis of the distal fibula.
Figure 2.
(a) The length discrepancy of the fibula to the unaffected side was not larger than that of the tibia (a-A ≥ b-B) and (b) The width of the distal fibular metaphysis of the affected side was not narrower than that of the unaffected side (W ≥ w’).
Evaluations
Demographic characteristics and clinical and radiographic manifestations were compared between TH and classic FH groups. The demographics included age at diagnosis, sex, laterality, and follow-up period. The clinical and radiographic manifestations were divided into three categories as above-the-ankle, foot-and-ankle, and LLD.
Above-the-ankle manifestations included femoral shortening, lateral condylar hypoplasia with knee valgus, tibial spine hypoplasia, ACL deficiency, and tibial bowing. Femoral shortening included congenital short femur and proximal focal femoral deficiency.4,11,12 Lateral condyle hypoplasia was evaluated using the condylar height ratio as described by Boakes et al. 13 A condylar height ratio of < 0.75 was considered lateral condyle hypoplasia with knee valgus. 5 ACL deficiency was confirmed via magnetic resonance imaging (MRI) when it was suspected on physical examination.
Foot-and-ankle manifestations included ankle morphology, shortening of the fibula, presence of tarsal coalition, number of foot rays, and Paley 14 classification. Ankle morphology was categorized into three types: horizontal, valgus (triangular epiphysis of the distal tibia), and ball-and-socket. 1 The normal distal fibular physis was defined to locate the level with the distal tibial articular surface or distal extent of the tibial ossification center. 15 Shortening of the fibula was determined based on the level of fibular growth plate, in accordance with the study by Malhotra et al. 16 In addition, Paley 14 classification was determined based on the foot deformity, which was categorized into four types: stable ankle, dynamic valgus, fixed equinovalgus, and fixed equinovarus.
The following were investigated for LLD: LLD at maturity, Birch et al.’s 4 classification, and surgical history of LLD correction. In patients who underwent limb-length equalization procedures, LLD at maturity was estimated using the multiplier method before surgical intervention. 17 Birch et al.’s 4 classification was determined based on the amount of limb shortening: limb shortening < 6%, 6%−10%, 11%−30%, and > 30%. The LLD pattern was evaluated based on Shapiro’s 18 classification. In addition, in case of undergoing surgery for LLD correction, surgical complications and functional outcomes, at the latest follow-up, were assessed. Functional outcomes were evaluated in accordance with the American Orthopedic Foot and Ankle Society (AOFAS) ankle–hindfoot scale 19 and the Tegner and Lysholm 20 activity level scale.
Statistical analyses
We used independent t-test for continuous variables and Fisher’s exact test for categorical variables to compare the demographic characteristics and clinical and radiographic manifestations between TH and classic FH groups. All statistical analyses were performed using SPSS ver. 21.0 (SPSS, IBM Corp., Chicago, IL); p-values less than 0.05 were regarded as statistically significant.
Results
Demographic characteristics
Overall, 13 patients had TH, whereas 17 had classic FH (Table 1). There were no statistically significant differences in the demographic characteristics between the groups.
Table 1.
Comparison of demographics between terminal hemimelia and classic fibular hemimelia groups.
| Terminal hemimelia * (N = 13) | Classic fibular hemimelia ** (N = 17) | p value | |
|---|---|---|---|
| Age at diagnosis (month) † | 19.5 (0–71) | 13.1 (0–56) | 0.408 |
| Sex ‡ | 0.469 | ||
| Boys | 10 (77%) | 11 (65%) | |
| Girls | 3 (23%) | 6 (35%) | |
| Laterality ‡ | 0.177 | ||
| Right | 10 (77%) | 9 (53%) | |
| Left | 3 (23%) | 8 (47%) | |
| Follow-up period (year) † | 12.4 (10.0–19.0) | 14.4 (10.0–24.0) | 0.144 |
Terminal hemimelia was defined as a disease entity which belongs to a spectrum of postaxial longitudinal deficiency and has a normal fibula.
Classic fibular hemimelia was defined as a postaxial longitudinal deficiency with hypoplastic fibula.
Values are expressed as mean, with range in parentheses.
Values are expressed as number, with percentage in parentheses.
Clinical and radiographic manifestations
Both groups showed significantly different manifestations above the ankle joint. Femoral shortening, lateral condyle hypoplasia with knee valgus, and tibial spine hypoplasia were significantly less common in patients with TH than in those with classic FH (p = 0.03, p < 0.001, and p = 0.003, respectively) (Table 2). None of the patients with TH had ACL deficiency confirmed via MRI; however, the difference was not statistically significant. Tibial bowing was not observed frequently in either group.
Table 2.
Comparison of clinical and radiographic manifestations between terminal hemimelia and classic fibular hemimelia groups.
| Terminal hemimelia * (N = 13) | Classic fibular hemimelia ** (N = 17) | p value | |
|---|---|---|---|
| Femoral shortening ‡ | 4 (31%) | 12 (71%) | 0.03 |
| Lateral condyle hypoplasia | |||
| Condyle height ratio † | 0.86 (0.69–0.95) | 0.73(0.61–0.91) | <0.001 |
| Knee valgus ‡ | 2 (15%) | 13 (76%) | <0.001 |
| Tibial spine hypoplasia ‡ | 2 (15%) | 12 (71%) | 0.003 |
| ACL deficiency ‡ | 0 | 2 (12%) | 0.238 |
| Tibial bowing ‡ | 2 (15%) | 3 (18%) | 1.000 |
| Ankle morphology ‡ | |||
| Horizontal | 4 (31%) | 2 (12%) | 0.286 |
| Valgus | 0 | 1 (6%) | |
| Ball-and-socket | 9 (69%) | 14 (82%) | |
| Shortening of the fibula ‡ | |||
| Grade 0 | 10 (77%) | 6 (35%) | 0.006 |
| Grade 1 | 3 (23%) | 3 (18%) | |
| Grade 2 | 0 | 5 (29%) | |
| Grade 3 | 0 | 3 (18%) | |
| Tarsal coalition ‡ | 5 (38%) | 15 (88%) | 0.004 |
| Number of rays ‡ | |||
| 3 | 3 (23%) | 4 (24%) | 0.514 |
| 4 | 9 (69%) | 9 (53%) | |
| 5 | 1 (8%) | 4 (24%) | |
| Paley classification ‡ | |||
| Stable ankle | 13 (100%) | 6 (35%) | 0.002 |
| Dynamic ankle valgus | 0 | 6 (35%) | |
| Fixed equinovalgus | 0 | 3 (18%) | |
| Fixed equinovarus | 0 | 2 (12%) | |
| LLD prior to operation (mm) † | 33.3 (17.0–46.0) | 47.3 (25.0–74.0) | 0.002 |
| Age at first operation (year) † | 11.2 (9.1–12.7) | 8.5 (5.3–13.7) | <0.001 |
| LLD at maturity (mm) † | 40.4 (19.7–52.0) | 67.0 (28.6–88.0) | <0.001 |
| Birch classification ‡ | |||
| 1A (limb shortening < 6%) | 10 (77%) | 5 (29.4%) | 0.006 |
| 1B (limb shortening 6%–10%) | 3 (23%) | 7 (41.2%) | |
| 1C (limb shortening 11%–30%) | 0 | 5 (29.4%) | |
| 1D (limb shortening > 30%) | 0 | 0 | |
ACL: anterior cruciate ligament; LLD: limb-length discrepancy.
Terminal hemimelia was defined as a disease entity which belongs to a spectrum of postaxial longitudinal deficiency and has a normal fibula.
Classic fibular hemimelia was defined as a postaxial longitudinal deficiency with hypoplastic fibula.
Values are expressed as mean, with range in parentheses.
Values are expressed as number, with percentage in parentheses.
Foot-and-ankle manifestations of TH were similar to those of classic FH in terms that the ball-and-socket ankle (Figure 3(a) and (d)) and the absence of lateral rays (Figure 3(b) and (e)) were commonly observed. Tarsal coalition was more frequently observed in classic FH (p = 0.004), but it was also not uncommon (38%, 5/13) in TH (Figure 3(c) and (e)). However, shortening of the fibula at the ankle joint, compared to the opposite side, was almost insignificant in TH, whereas significant shortening was presented in 47% (8/17) of classic FH cases (p = 0.006). In addition, all patients with TH exhibited a painless plantigrade foot without ankle instability, whereas 30% of patients with classic FH had fixed equinovalgus or equinovarus deformity (p = 0.002).
Figure 3.
Foot-and-ankle manifestations in patients with TH. (a)−(c) Radiographs of an 11-year-old girl and (d)−(f) an 11-year-old boy with TH showing absent lateral rays, ball-and-socket ankle, and tarsal coalition.
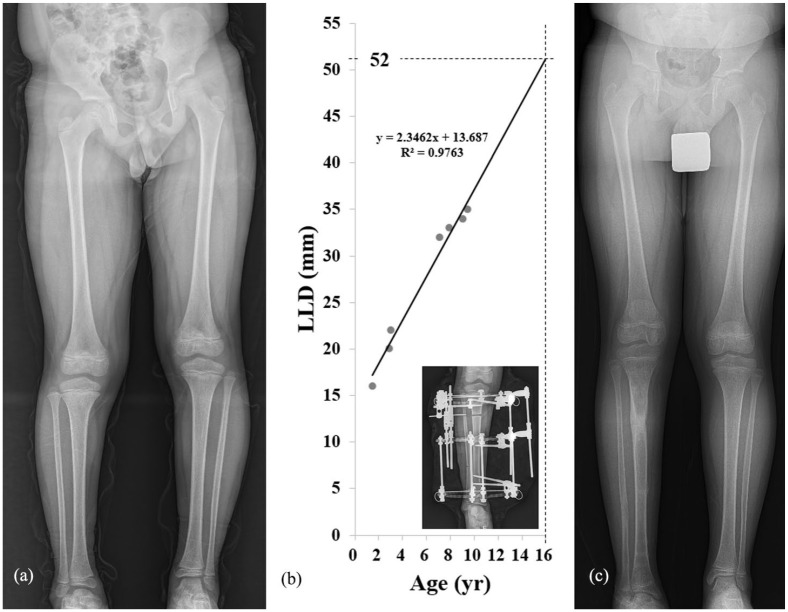
The two groups showed significant differences in terms of LLD. LLD at maturity averaged 40.4 (19.7–52.0) mm in TH and 67.0 (28.6–88.0) mm in classic FH (p < 0.001). In addition, limb shortening was significantly lower in the TH group than in the classic FH group according to the Birch classification (p = 0.006). However, except for one patient with TH (19.7 mm), the LLD of patients with TH and classic FH was either measured or estimated to be > 20 mm. The LLD in TH progressed in a linear pattern, similar to that in classic FH (Shapiro type I, Figure 4).
Figure 4.
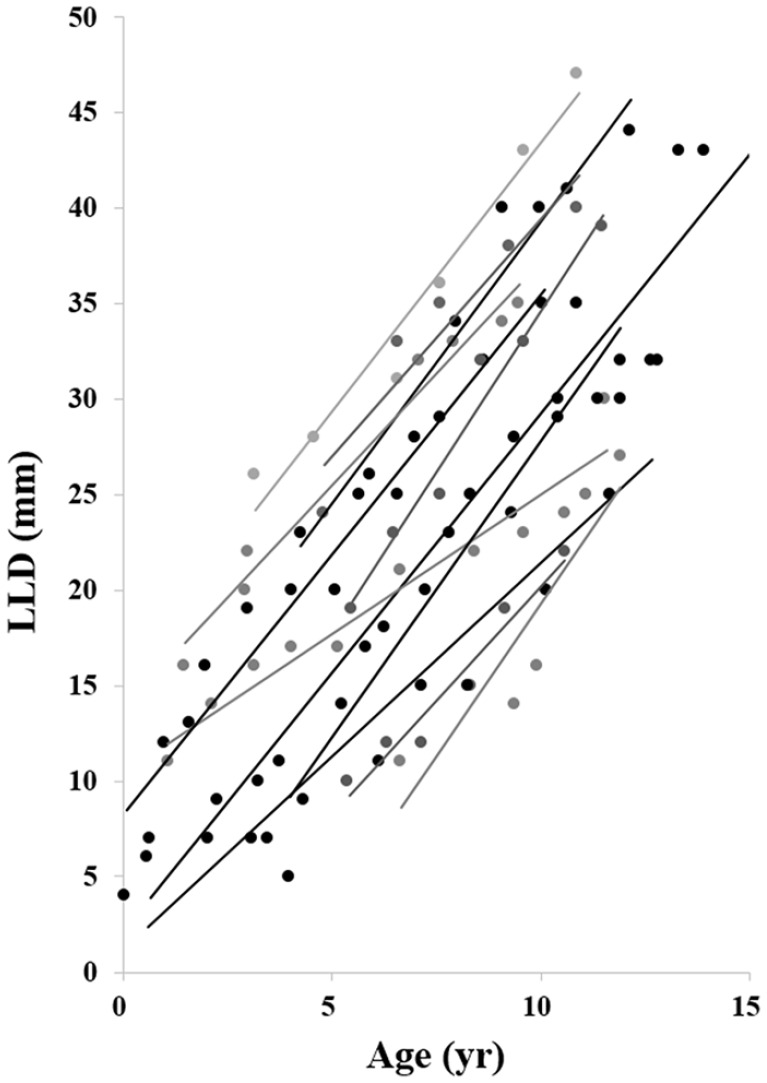
Progression pattern of limb-length discrepancy in patients with terminal hemimelia.
Overall, 46% of TH patients (6/13) underwent limb-length equalization procedures at a mean age of 11.2 (9.1–12.7) years, whereas 94% of classic FH patients (16/17) underwent surgeries at 8.5 (5.3–13.7) years (p < 0.001). Single-stage tibial lengthening was most commonly performed in patients with TH (4/6), and either contralateral epiphysiodesis or lengthening combined with contralateral epiphysiodesis was performed in one patient each. Two of four patients required percutaneous Achilles tendon lengthening by triple hemisection after single-stage tibial lengthening, and one patient presented superficial pin-tract infection that responded to oral antibiotics. Five of six patients had excellent results and one patient had a good result on the AOFAS ankle–hindfoot scale. At the latest follow-up, all of them were able to participate in competitive sports, including soccer, tennis, and badminton more actively, as compared to recreational level. However, two-stage tibial and femoral lengthening or lengthening combined with contralateral epiphysiodesis was required in patients with classic FH (14/16). In addition, 5 of those 14 patients required percutaneous Achilles tendon lengthening by triple hemisection, and 1 patient underwent brisement procedure for knee stiffness. Patellar instability and ankle pain associated with valgus instability were observed in one and three patients, respectively. The remaining two patients underwent contralateral permanent epiphysiodesis for LLD correction. Scoring the patients on the AOFAS ankle–hindfoot scale, excellent results were observed in five patients, good in four, fair in four, and poor in three patients. However, 31% of patients (5/16) were not able to participate in competitive sports even at a recreational level at the latest follow-up.
Illustrative case
A boy first visited the outpatient clinic and was diagnosed with TH at the age of 1 year. He was otherwise normal, except for the absence of lateral rays, ball-and-socket ankle, and tarsal coalition, and had a plantigrade mobile foot (Figure 3(d)−(f)). Despite these symptoms, he maintained normal daily activities while wearing a shoe lift until the age of 9 years. At that time, the patient had a 35-mm LLD without angular deformity or knee instability (Figure 5(a)). The LLD in this patient progressed linearly, and the predicted LLD at maturity was 52 mm (Figure 5(b)). The patient subsequently underwent a 52-mm tibial lengthening (Figure 5(c)). No perioperative complications were observed during 2 years of follow-up. The patient recovered and had a normal gait. The patient had excellent results based on the AOFAS ankle–hindfoot scale (100 points) and was able to participate in competitive sports, including soccer and tennis (activity level of 7).
Figure 5.
An 11-year-old patient with terminal hemimelia and a history of single-stage tibial lengthening. (a) The patient had 35 mm of limb-length discrepancy (LLD) at the age of 9 years. (b) The LLD, following linear progression, was calculated as 52 mm at maturity. (c) The patient subsequently underwent a 52-mm tibial lengthening according to growth calculation.
Discussion
Through this study, we aimed to delineate the characteristics of PALD with a normal fibula or TH rather than to propose a new classification system among the spectrum of PALD. Our study findings mostly align with the two previous studies in introducing PALD with a normal fibula or TH.2,5 As the previous studies mentioned, these patients mainly presented with the symptoms of FH at the terminal regions of the lower extremity (e.g. absence of lateral rays, ball-and-socket ankle, and tarsal coalition) and LLD, whereas other symptoms of FH were present in a reduced proportion.2,5
However, several differentiating points were observed between TH and classic FH. First, although the observation frequency of ball-and-socket ankle in TH was similar to that in classic FH, all patients with TH had a painless plantigrade foot without ankle instability. Thus, all patients categorized to Paley type I (stable ankle). The postulated reason for this was that the length of the fibula at the ankle joint, compared to that in the opposite side, was relatively well maintained in TH, whereas 47% of patients with classic FH presented significant shortening of the fibula. Second, the amount of LLD at maturity was significantly lower in TH than in classic FH. However, the LLD of TH was expected to be at an average of 40.6 mm, and a considerable number of patients with TH (46%) underwent limb-length equalization procedures. In addition, all patients, except one, required surgeries for > 20 mm of LLD correction. Hence, LLD seems to be the most important feature of TH that may lead to surgical treatment. LLD in the TH group progressed in a linear pattern similar to that in classic FH.4,21,22
Therefore, single-stage tibial lengthening using distraction osteogenesis can be a good treatment option compared to various surgical strategies for LLD correction among patients with TH. This is because these patients have a stable knee joint with a functional plantigrade foot without ankle instability, and the LLD is relatively mild compared with that in classic FH. Neither the ball-and-socket ankle nor the tarsal coalition affected the outcomes of tibial lengthening, similar to that reported in a previous study by Birch et al. 4 However, it would be mandatory to check the foot and ankle instability based on a clinical examination before deciding for a lengthening procedure, as mentioned by Paley. 14 Considering that our patients achieved satisfactory outcomes after a lengthening procedure at an average age of 11 years, it is recommended to perform tibial lengthening in early adolescence. Furthermore, we agree that the amount of tibial lengthening should be determined by referring to the accompanying reduction in foot height or femoral shortening since LLD is not caused solely by tibial shortening. 4 In patients with minor LLD, shoe lift or contralateral epiphysiodesis may be an alternative option for LLD management.
The etiology of either classic FH or TH remains unclear.3,5,7,23 It has been assumed that a failure of limb patterning of the anterior–posterior axis, caused by a deficiency of sonic hedgehog in the zone of polarizing activity, plays a key role in the development of PALD.5,23 Baek et al. 5 speculated that sonic hedgehog expression might be deficient during the later phase in TH compared to that in classic FH. Besides, vascular deficiency during early limb bud formation was also suggested as an etiologic factor for PALD. 24 Hootnick et al. 25 reported vascular abnormalities, such as the absence of the anterior tibial artery or the absence of the trifurcation of the popliteal artery, or the presence of atypically large posterior artery in patients with PALD.
The current study has several limitations. As this was a retrospective study, the follow-up interval among patients was not constant. However, the follow-up period was > 10 years for all patients. For that reason, we were only able to evaluate categories already investigated. Furthermore, as torsional study was conducted only in few patients, although preferred, we were unable to evaluate the differences in femoral retroversion between TH and FH. In addition, owing to the rarity of this entity (PALD), the number of study participants was insufficient. Accordingly, the variable (ACL deficiency) was expected to be statistically significant but could not be verified for statistical significance. Nonetheless, we conducted a comparative analysis on a larger case series than in previously conducted studies.2,5
Our study findings indicate that TH manifests as a milder phenotype than classic FH. It mainly overlaps with the symptoms of FH below the ankle joint and manifests as LLD. Single-stage tibial lengthening can be a good option for limb-length equalization in patients with TH than in those with classic FH because most patients with TH have moderate LLD and a painless plantigrade foot without knee and ankle instability.
Supplemental Material
Supplemental material, sj-pdf-1-cho-10.1177_18632521241227830 for Characteristics of terminal hemimelia: What is the difference between terminal hemimelia and classic fibular hemimelia? by Mi Hyun Song, Chang-Ho Shin, In Ho Choi and Tae-Joon Cho in Journal of Children’s Orthopaedics
Footnotes
Author contributions: M.H.S., I.H.C., and T.-J.C. contributed to study design. M.H.S. involved in data interpretation, and writing and revising the article. C.-H.S. and I.H.C. provided critical review. C.-H.S. and T.-J.C. participated in revising the article. M.H.S., I.H.C., and T.-J.C. provided final approval of the article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: This retrospective study was approved by the Seoul National University College of Medicine/Seoul National University Hospital Institutional Review Board (IRB no. H-2204-139-1319).
Informed consent: Informed consent was waived because of the retrospective nature of the study, and the analysis used anonymous clinical data.
References
- 1. Stanitski DF, Stanitski CL. Fibular hemimelia: a new classification system. J Pediatr Orthop 2003; 23: 30–34. [PubMed] [Google Scholar]
- 2. Searle CP, Hildebrand RK, Lester EL, et al. Findings of fibular hemimelia syndrome with radiographically normal fibulae. J Pediatr Orthop B 2004; 13(3): 184–188. [DOI] [PubMed] [Google Scholar]
- 3. Hamdy RC, Makhdom AM, Saran N, et al. Congenital fibular deficiency. J Am Acad Orthop Surg 2014; 22: 246–255. [DOI] [PubMed] [Google Scholar]
- 4. Birch JG, Lincoln TL, Mack PW, et al. Congenital fibular deficiency: a review of thirty years’ experience at one institution and a proposed classification system based on clinical deformity. J Bone Joint Surg Am 2011; 93: 1144–1151. [DOI] [PubMed] [Google Scholar]
- 5. Baek GH, Kim JK, Chung MS, et al. Terminal hemimelia of the lower extremity: absent lateral ray and a normal fibula. Int Orthop 2008; 32: 263–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Achterman C, Kalamchi A. Congenital deficiency of the fibula. J Bone Joint Surg Br 1979; 61: 133–137. [DOI] [PubMed] [Google Scholar]
- 7. Lewin SO, Opitz JM. Fibular a/hypoplasia: review and documentation of the fibular developmental field. Am J Med Genet Suppl 1986; 2: 215–238. [DOI] [PubMed] [Google Scholar]
- 8. Letts M, Vincent N. Congenital longitudinal deficiency of the fibula (fibular hemimelia). Parental refusal of amputation. Clin Orthop Relat Res 1993; 287: 160–166. [PubMed] [Google Scholar]
- 9. Coventry MB, Johnson EW., Jr. Congenital absence of the fibula. J Bone Joint Surg Am 1952; 34: 941–955. [PubMed] [Google Scholar]
- 10. Bohne WH, Root L. Hypoplasia of the fibula. Clin Orthop Relat Res 1977; 125: 107–112. [PubMed] [Google Scholar]
- 11. Stevens PM, Arms D. Postaxial hypoplasia of the lower extremity. J Pediatr Orthop 2000; 20: 166–172. [PubMed] [Google Scholar]
- 12. Rodriguez-Ramirez A, Thacker MM, Becerra LC, et al. Limb length discrepancy and congenital limb anomalies in fibular hemimelia. J Pediatr Orthop B 2010; 19(5): 436–440. [DOI] [PubMed] [Google Scholar]
- 13. Boakes JL, Stevens PM, Moseley RF. Treatment of genu valgus deformity in congenital absence of the fibula. J Pediatr Orthop 1991; 11(6): 721–724. [DOI] [PubMed] [Google Scholar]
- 14. Paley D. Surgical reconstruction for fibular hemimelia. J Child Orthop 2016; 10(6): 557–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ogden JA, McCarthy SM. Radiology of postnatal skeletal development. VIII. Distal tibia and fibula. Skeletal Radiol 1983; 10(4): 209–220. [DOI] [PubMed] [Google Scholar]
- 16. Malhotra D, Puri R, Owen R. Valgus deformity of the ankle in children with spina bifida aperta. J Bone Joint Surg Br 1984; 66(3): 381–385. [DOI] [PubMed] [Google Scholar]
- 17. Paley D, Bhave A, Herzenberg JE, et al. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg Am 2000; 82: 1432–1446. [DOI] [PubMed] [Google Scholar]
- 18. Shapiro F. Developmental patterns in lower-extremity length discrepancies. J Bone Joint Surg Am 1982; 64(5): 639–651. [PubMed] [Google Scholar]
- 19. Schneider W, Jurenitsch S. Normative data for the American Orthopedic Foot and Ankle Society ankle-hindfoot, midfoot, hallux and lesser toes clinical rating system. Int Orthop 2016; 40(2): 301–306. [DOI] [PubMed] [Google Scholar]
- 20. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 1985; 198: 43–49. [PubMed] [Google Scholar]
- 21. Hootnick D, Boyd NA, Fixsen JA, et al. The natural history and management of congenital short tibia with dysplasia or absence of the fibula. J Bone Joint Surg Br 1977; 59: 267–271. [DOI] [PubMed] [Google Scholar]
- 22. Tsai A, Kleinman PK, Laor T, et al. Lower-extremity growth patterns and skeletal maturation in children with unilateral fibular hemimelia. Pediatr Radiol 2019; 49(1): 122–127. [DOI] [PubMed] [Google Scholar]
- 23. Zhang Z, Yi D, Xie R, et al. Postaxial limb hypoplasia (PALH): the classification, clinical features, and related developmental biology. Ann N Y Acad Sci 2017; 1409(1): 67–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Graham JM., Jr. Limb anomalies as a consequence of spatially-restricting uterine environments. Prog Clin Biol Res 1983; 110: 413–422. [PubMed] [Google Scholar]
- 25. Hootnick DR, Levinsohn EM, Randall PA, et al. Vascular dysgenesis associated with skeletal dysplasia of the lower limb. J Bone Joint Surg Am 1980; 62(7): 1123–1129. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cho-10.1177_18632521241227830 for Characteristics of terminal hemimelia: What is the difference between terminal hemimelia and classic fibular hemimelia? by Mi Hyun Song, Chang-Ho Shin, In Ho Choi and Tae-Joon Cho in Journal of Children’s Orthopaedics