Abstract
Background:
Traction is used at our hospital before open reduction in infants with developmental dysplasia of the hip. Theoretically, it reduces soft-tissue tension, allowing an easier surgical reduction and therefore lower surgical complications. Owing to extended hospital stays, potential complications, and lack of evidence, the use of traction has decreased. This study aims to quantify whether traction is safe and whether it has any demonstrable effect.
Methods:
The perioperative course of 80 patients undergoing preoperative traction and hip open reduction were reviewed. The height of hip dislocation was classified using the International Hip Dysplasia Institute classification system on both radiographs taken before and after traction. Any complications related to traction were recorded, along with the requirement for femoral shortening osteotomies, incidence of re-dislocation, and longer-term rate of avascular necrosis.
Results:
Traction lowered the resting position of the majority of hips, with the median International Hip Dysplasia Institute grade before traction improving from 4 to 3, a statistically significant improvement (p < 0.00001). There were no neurovascular complications. Two babies were complicated with broken skin sores; however, surgery still progressed uneventfully. Zero hips in the cohort required femoral shortening osteotomies to achieve a tension-free reduction, and the re-dislocation rate was 0%. However, 96% of hips were Severin 1 or 2 at 6-year follow-up.
Conclusion:
Notably, 1 week of preoperative traction significantly improves the resting position of the hip in high dislocations. It is safe when used in infants weighing <12 kg, and subsequent surgical outcomes are excellent, thus supporting its use ahead of developmental dysplasia of the hip open reduction surgery.
Level of evidence:
Level IV.
Keywords: Developmental dysplasia of the hip, Gallows traction, preoperative traction, avascular necrosis
Introduction
Gallows traction, or Bryant’s traction, is a form of overhead skin traction that can be used in infants. It is indicated for femoral fractures in babies and in developmental dysplasia of the hip (DDH).1,2 In the context of DDH, it has been used as a definitive mode of reduction of dislocated hips, though over a course of approximately 6 months. 3 A further use in DDH is as an adjunct prior to surgical reduction of dislocated hips in infants.
Children of walking age with severe DDH may require surgical intervention under general anesthesia to reduce a dislocated hip. Re-dislocation and avascular necrosis (AVN) of the femoral head are complications that fill the pediatric orthopedic surgeon with dread, with implications for further surgery and poor longer-term outcomes for the child.4–6 Pre-reduction Gallows traction is theorized to reduce the incidence of re-dislocation and being protective against AVN by reducing the height of the hip dislocation prior to reduction, in turn reducing soft-tissue tension and allowing a more straightforward surgical reduction. The evidence base for a preoperative traction regime is limited. Previous studies have identified a protective effect; however, recent studies suggest traction does not protect against re-dislocation and AVN. In addition, the existing literature on Gallows traction regarding the protective effect of pre-reduction traction on AVN mainly focuses on it use before closed reduction.7–15 To date, there does not appear to be existing literature on Gallows traction related to whether traction over the course of 1 week is effective in reducing the soft-tissue tension or decreases the height of hip dislocation before surgery, which ultimately is the theorized benefit of traction.7–15
The use of traction is associated with subsequent complications, with complications of traction reported in the literature from the 1950s. These included significant neurovascular compromise and skin problems. 16 Therefore, a safe upper weight limit for Gallows traction is variably recommended as 12 and 16 kg to reduce the incidence of such complications, though this is based on historical Level 5 evidence.1,16–18 In addition, preoperative traction extends the stay of patients in hospital and requires expert nursing care. It undoubtedly adds further burden to the surgical journey for both families and medical teams alike.
Therefore, in combination with the current lack of clear evidence, many hospitals have stopped using preoperative traction in DDH. However, owing to the theorized protective effect against re-dislocation and AVN in the absence of a strong evidence to the contrary, coupled with excellent clinical outcomes following surgical reduction at our institution, Gallows traction has continued to be used at our institution for 1 week ahead of open reduction surgery in infants less than 12 kg in weight.
The aim of this study was twofold. First, we aimed to evaluate whether Gallows traction, as used at our institution preoperatively ahead of hip open reduction surgery, is safe within the 12 kg weight limit adopted. Second, for what appears to be the first time in the literature, we aimed to assess whether 1 week of preoperative traction has any noticeable effect on soft-tissue tension and height of hip dislocation. This was done by comparing the pre- and post-traction imaging for the resting position of the hip, the requirement of femoral shortening procedures, and the re-dislocation rate. The outcomes of this study would inform whether the existing practice of preoperative traction at our institution could be discontinued.
Materials and methods
This is a retrospective study of 80 infants who have undergone preoperative Gallows traction at our institution, ahead of hip open reduction surgery for DDH. Patients treated with Gallows traction were identified through the hospital database, having been granted ethical approval (Electronic Research and Governance Online (ERGO) Ref 60802). The most recent 80 infants, with complete medical and nursing notes, undergoing traction prior to surgical reduction between 2010 and 2020, were reviewed to explore the two aims of this study:
(a) The safety of Gallows traction;
(b) The effectiveness of Gallows traction in decreasing the height of the hip dislocation, with implication on soft-tissue tension and surgical outcomes.
Evaluating safety of traction
Overhead traction is performed by skilled staff and uses adhesives and a crepe bandage overwrap, as illustrated in Figure 1. Traction is used in all patients up to 12 kg, based on the historical evidence that weights > 12 kg are at increased risk of neurovascular complications.1,16–18 Patch testing for the adhesive used is done prior to the start of traction. During the traction regimen, patients are checked hourly for neurovascular complications. The bandages are also re-wrapped twice daily to allow the skin to be examined for cutaneous complications. This is the only time out of traction for the infant during the regime. Nappy/ diaper changing is not restricted by the infant being in traction. Feeding can occur with the child supine, though the traction arrangement allows the infant to spin around and lie on their front too.
Figure 1.

An infant happily undergoing Gallows traction ahead of hip open reduction surgery.
The duration of traction for each patient was noted and patient’s weight was recorded to support the identification of a safe weight range for traction. Complications following traction were identified by the review of all inpatient nursing and medical notes. Complications were categorized into neurological, vascular, and cutaneous.
Evaluating effectiveness of traction
All patients had a supine antero–posterior (AP) radiograph taken in the pediatric X-ray department on the day of admission, just before commencing their period of traction. A single AP image was repeated at the end of the period of traction, with traction removed. This was performed preoperatively in theater in the same supine position, under general anesthetic (GA) and before any surgery had commenced. The resting position of the hip on the plain AP radiographs was categorized using the International Hip Dysplasia Institute (IHDI) classification system (Figure 2). 19 The resting hip position was directly compared for each patient on the pre-traction radiograph to the post-traction (but preoperative) radiograph. A Wilcoxon signed-rank test was used to identify whether any change in resting hip position following traction was statistically different.
Figure 2.

(a) Radiological imaging outlining the IHDI classification system for hip position in DDH. The Right hip is normal and is IHDI I. The left hip is dislocated and is IHDI III. (b) A bar chart showing the resting position of each hip according to the IHDI classification system, both before and after traction. The red section shows the number of hips at IHDI grade IV, amber is for Grade III hips and green is for Grade II.
The intraoperative images and surgery notes were systematically reviewed to identify whether femoral shortening osteotomies were required intraoperatively to allow stable concentric reduction of the femoral head. Postoperative imaging and notes were then reviewed to identify hips which re-dislocated. All postoperative radiographs were reviewed for the measurement of AVN. Three classification systems were used, in order for this assessment to be as comprehensive as possible, namely Kalamchi and MacEwen, Salter, and Severin classifications.
Results
Patient information
As planned, 80 babies were included in this cohort, comprising 48 females and 32 males. The median age at traction was 14 (range: 12–30) months. The mean weight of infants at the time of traction was 9.2 (5.2–12.5) kg. The mean follow-up was 6 years (range 24–144 months). All infants had standard hip open reduction surgery through an anterior approach after their preoperative traction.
Safety of traction
There were no neurological problems at any point in any infant. Regarding vascularity, there were three patients in whom transient sluggish capillary refill was reported. For each patient, this was for less than 2 h duration and warranted observation only, without discontinuation of the traction. These infants weighed 6.8, 7.0, and 9.5 kg, respectively. In a further nine patients, transient incidences of cool feet were reported. The weight of these patients ranged from 6.0 to 11.9 kg. There was no concern regarding limb perfusion throughout any of these events, and traction was continued uneventfully in all cases.
Small unbroken skin sores were reported in 20 infants (25%), but this did not stop the continued use of traction nor caused any longer-term effects or scars. All 20 of these babies weighed >8 kg. Broken skin sores were reported in two infants, weighing 8.8 and 12.2 kg. Traction was discontinued on Day 5 in both these cases and not restarted. Having completed most of the traction, these children progressed to their surgery as planned on the seventh day following initial traction.
There were two infants in whom traction had to be ceased earlier due to infection. The infections were one case of gastroenteritis that developed on Day 2 of traction and one case of chicken pox that developed on Day 4. In both cases, the traction was promptly discontinued, and their surgery was postponed. Neither of these infections can be linked to the traction but do highlight the importance of continued nursing care. Each infection would have led to surgery being postponed irrespective of traction. Each infant returned to complete a full week of preoperative traction uneventfully ahead of their postponed hip surgery.
Effectiveness of traction ahead of surgery
Before traction, according to IHDI classification, 49 hips were classified as Grade IV, 27 hips were Grade III, and 4 hips were Grade II. Following 1 week of preoperative Gallows traction, resting position was Grade IV in 24 hips, Grade III in 37 hips, and Grade II in 19 hips (Figure 2). An example of the resting hip position pre- and post-Gallows traction is illustrated in the radiographs in Figure 3.
Figure 3.

(a) Preoperative and pre-traction radiograph of a 13-month-old infant. The left hip is a high IHDI 4 hip. The right hip is also affected, to a lesser extent, and is IHDI 2. (b) Post-traction radiograph performed 7 days later, at rest with the traction removed, with the image intensifier before any surgery has commenced. Hilgenreiner’s line is plotted on both radiographs to illustrate the different resting positions of the hip. The left hip has improved from IHDI 4 to 3. The right hip is IHDI 2 on both radiographs, although can be seen to be nearer the anatomical level post-traction.
From the 49 hips which were Grade IV before traction, 24 remained Grade IV, though 23 became Grade III and 2 became Grade II. Of the initial 27 Grade III hips, 14 remained Grade III and 13 became Grade II. Four hips which were Grade II before traction did not change the position according to IHDI classification. A Wilcoxon signed-rank test indicated that the decrease in the height of the hip dislocation following traction was significant: pre-traction (Median = IHDI 4), post-traction (Median = IHDI 3), z = −5.51, p < 0.00001
Zero hips (0%) required femoral osteotomies to allow concentric reduction of the femoral head during open reduction. In addition, zero hips (0%) re-dislocated. AVN was measured by three classification methods, namely Kalamchi and MacEwen, Salter, and Severin. There were 77 of 80 hips (96%) that were Severin 1 or 2 (excellent/good) on the final radiograph at a mean follow-up of 6 years (Figure 4(a)). Of the three hips demonstrating unsatisfactory radiological appearance, two were Severin Grade 3 and one was Severin Grade 4. According to the Salter grading (Figure 4(b)), only 3 of 80 hips (4%) were Grade 4 (fragmentation of femoral head) or 5 (residual deformity after reossification). The remainder (96%) either showed no signs of AVN (61/80), some ossific nucleus delay (5/80), or some broadening of the femoral neck (9/80). According to the Kalamchi and MacEwen grading, there were 13 out of 80 hips (16%) that demonstrated Grade 3 or 4 AVN (Figure 4(c)). The follow-up of this cohort is longer than most papers on surgical outcomes of DDH, thus type 2 AVN (lateral growth arrest) is detected here (11/80 hips, 14%), whereas it has yet to become apparent in most papers that have shorter follow-up (20). Thus in all parameters, this cohort of hips that have undergone preoperative traction has a favorable rate of AVN compared to the existing literature.20–22
Figure 4.
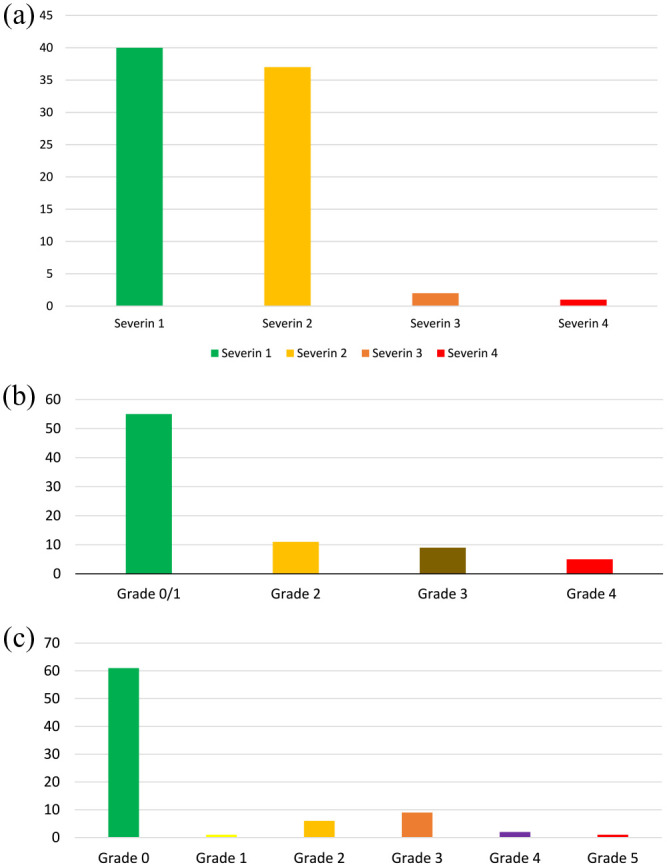
(a) Severin grade at mean of 6-year follow-up. Notably, 40 hips were Severin 1 (normal appearance), 37 hips were Severin 2 (mild deformity of the femoral head or neck or acetabulum), 2 hips were Severin 3 (dysplastic without subluxation), and 1 hip was Severin 4 (subluxed), (b) AVN grade using the Kalamchi and MacEwen classification system at mean of 6-year follow-up. Notably, 55 hips were Grade 0/1 (no AVN/delayed appearance or mild irregularity of ossific nucleus but with no long-standing change to development), 11 hips were Grade 2 (lateral growth arrest), 9 hips were Grade 3 (central necrosis), and 5 hips were Grade 4 (whole-head necrosis). (c) Avascular grade using the Salter classification system at mean of 6-year follow-up. Notably, 61 were Grade 0 (no evidence of AVN), 1 hip was Grade 1 (no ossific nucleus after 1 year post-reduction), 6 hips were Grade 2 (failure of growth in an existing ossifying nucleus for ≥ 1 year post-reduction), 9 hips were Grade 3 (broadening of the femoral neck), 2 hips were Grade 4 (fragmentation of the femoral head), and 1 hip was Grade 5 (residual deformity after reossification).
Discussion
There is remarkably little evidence to support or refute the use of preoperative Gallows traction prior to open reduction surgery of dislocated hips in infants. This study has confirmed it to be safe in infants up to 12 kg. We have also identified, for the first time in the literature, a significant improvement in the resting position of the hip following 1 week of traction. Alongside this, there was no requirement for femoral shortening osteotomies to enable tension-free reduction, which is a sign of the low soft-tissue tension. This is further validated by the fact that none of these hips re-dislocated and the AVN rates are extremely favorable to all published literature.20–22
Whether the period of traction and reduction in soft-tissue tension has any translatable impact onto AVN and long-term outcomes is harder to establish, as the causes of AVN are complex and multifactorial. It can be difficult to tease out any protective effect of individual factors, which undoubtedly reflects conflicting views in the literature.7–15 Previous studies have advocated the effectiveness of traction at preventing complications following closed reduction, particularly AVN.7–9 However, recent literature suggests traction does not affect the stability of reduction nor protect against AVN of the femoral head following closed reduction.13–15 The unproven protective effect of traction, combined with the added burden on nursing, resources, and family units, has resulted in a growing consensus that traction has limited clinical utility.10–15
At a mean of 6-year follow-up in this study, 96% of this cohort were Severin 1 or 2 (excellent or good radiological appearance) on final follow-up. The Severin classification assesses both deformity of the femoral head and acetabulum and evaluates the position of the femoral head in relation to the acetabulum, in doing so allowing accurate interpretation of the proximal femoral growth disturbance in this cohort of hips. The Severin rate in this cohort of operated hips concurs with the value from a cohort of 100 hips from our center at 12-year follow-up, treated by the same surgeons with this identical perioperative regime, whereby 95% of hips are Severin 1 or 2 (excellent or good). 23 Due to the changes in the Picture Archiving Computer System (PACS), many of the post-traction images were unavailable for analysis on this earlier cohort, otherwise, this group would have been used for this study.
Three classification systems for AVN were used to provide the most comprehensive assessment. All measure slightly different factors, thus numbers vary. The clinically significant rate of AVN reported here following surgery and the preoperative traction regime, by whichever classification chosen, is extremely favorable to the existing literature.20–22 This supports the theoretical protective use of preoperative Gallows traction, though clearly this study cannot conclude that it is a direct cause–effect phenomenon. These favorable outcomes are undoubtedly multifactorial, perhaps contributed by the relatively high volume of open reduction cases performed at our institution, double consultant operating, and the familiarity of the theater teams with these cases. However even with a well-designed randomized controlled trial, these multiple influencing factors would be hard to account for. Nonetheless, these findings do support the case that preoperative Gallows traction can decrease the rate of AVN.
There were no permanent neurovascular complications in this cohort. Small unbroken skin sores (25% of patients) were common in our cohort. However, only two patients progressed to broken sores requiring cessation of traction, which were both on Day 5. These complications affecting the skin were not significant to the patient’s operative management and did not affect the final outcomes. Therefore, pre-reduction traction, as used at our institution, appears safe with up to 12 kg infant weight. It may be that a heavier weight limit is also safe, but as our institutional policy is up to 12 kg, then further comment cannot be made on weights above this. What is imperative is that there is appropriate nursing staff expertise to manage babies in traction. While almost all perceived complications were minor and temporary, with no action required, the monitoring of these requires a certain level of expertise, making it essential to have appropriately trained staff. The pediatric orthopedic nursing teams provide constant support to families while their baby is on traction. This undoubtedly explains why there was no infant for whom the traction had to be stopped prematurely due to the family not coping with it.
This study, for the first time, provided evidence of a reduction in soft-tissue tension around the hip, following traction. However soft-tissue tension cannot be directly measured, and “ease of reduction” would be entirely subjective and hard to quantify. Therefore, this study evaluated what could be measured in a reproducible and meaningful way, namely whether traction altered the height of hip displacement. Whether femoral shortening osteotomies were required to allow tension-free reduction, and the re-dislocation rate, are also outcomes that are theoretically related to preoperative traction. The incidence of re-dislocation following open reduction is reported usually around 8% in the literature.20,24–26 Our rate of 0% re-dislocations therefore compares favorably, especially considering the majority of children in this study are high-grade dislocations and over a one-fourth of the cohort are late presentations after 18 months of age. In addition, zero femoral shortening procedures were required to allow tension-free concentric reductions without subsequent re-dislocation. Like “ease of reduction,” the avoidance of need for femoral osteotomy is subjective and a surgeon-dependent consideration, which is therefore a softer sign. However, in combination with the low re-dislocation rate, low AVN rate, and objective improvement in the resting position of the hip found in this study, the evidence for preoperative traction reducing soft-tissue tension is compelling.
These results have changed clinical practice at our center, with traction now only used for high-grade dislocations (IHDI III and IV). This is based on the rationale that the low-grade dislocations (IHDI II) lacked the marked response from traction seen in the higher dislocations. The authors were surprised by the dramatic improvement in resting hip position of the high dislocations. We had expected there to be no notable change and that we would be able to dispense with the traditional preoperative traction regime. We surprised ourselves as to the effectiveness of preoperative traction, thus its use has been validated and continues in our practice, now with scientific justification. This study has also supported our preoperative consent process and justification to families.
A limitation of this study is that the pre-traction radiographs were obtained in a preoperative clinic, whereas the post-traction images were taken under GA with traction removed before surgical reduction had started. Although both images are taken supine by experienced radiographers in identical positions, the key difference is the GA. Although there is no muscle relaxant used, the sedation effect of GA could still have an effect. Furthermore, a crying baby when awake in the X-ray room may add to muscle tension. To address this potential major confounding factor, the senior author measured the position of the hip on preoperative images and intraoperative images on 10 hips which were not eligible for traction, either because of being the second hip of bilateral disease to undergo reduction or over 12 kg at the time of surgery. In these 10 hips, there was no change in the resting position of the hip between preoperative radiograph and intraoperative image prior to surgery (Figure 5). This validates that the change in the position of the hip seen in this study post-traction is truly secondary to the use of traction and not an effect of the GA.
Figure 5.
(a) Bar chart showing the preoperative resting position of 10 hips that did not undergo preoperative traction. The first column is the standard departmental radiograph and the second column is the comparative film under GA but before any surgery. The red section is IHDI Grade IV hips and amber is for the Grade III hip. There is no change in the position on any hip, thus excluding the effect of GA on the cohort of hips that had preoperative traction in this study, (b) this is illustrated, and (c) with no difference seen. This should be compared to Figure 3, where the difference in resting hip position after traction is clear.
Since traction requires increased hospital stays and nursing involvement, in a landscape where there is increasing financial restraints and resource shortages, a cost-effective analysis would be invaluable. However, any health economic analysis is fraught with difficulties and requires, at least, consideration of later total hip replacement, along with the ensuing time off work, reduction in tax contributions, and decreased economic contribution. That was not a part of this study. The favorable radiographic outcomes would infer that total hip replacement would likely be later in adult life or less frequently required in our cohort than in other post-surgical cases. 27 Thus, this would heavily offset any increased costs associated with extra days in hospital on preoperative traction. It would also be important to evaluate the psychological effect of traction on family units, an aspect of care which is incredibly important and often overlooked. Engagement of our families is, however, excellent and the time enables further consent and discussion.
This study has now provided the clearest evidence to date of the beneficial effect of preoperative tract. By demonstrating a true difference in resting hip position following preoperative traction, this study supports the rationale that it decreases soft-tissue tension, allowing a stable tension-free surgical reduction while avoiding the additional complexity and surgical insult of femoral osteotomies. In combination with excellent clinical outcomes, including low re-dislocation and AVN rates, plus the excellent safety profile, this study supports the use of traction before open reduction surgery in high-grade dislocations.
Supplemental Material
Supplemental material, sj-pdf-1-cho-10.1177_18632521241229620 for Preoperative Gallows traction as an adjunct to hip open reduction surgery: Is it safe and is it effective? by Nicholas C Uren, Julia Judd, Edward A Lindisfarne, Kirsten G Elliott and Alexander Aarvold in Journal of Children’s Orthopaedics
Footnotes
Authors’ Note: The APC is provided by the Southampton Hospitals Charity.
Author contributions: N.C.U. (BMBS) is the primary author and involved throughout with ethics, design of the study, data collection, data analysis, and creation of the article. J.J. (BSc) is involved with study design, data collection, and creation of the article. E.A.L. (FRCS) and K.G.E. (FRCS) are the senior authors and involved throughout with the primary design of the study, data collection and analysis, and creation of the article. A.A. (FRCS) is the senior author and involved throughout with ethics, design of the study, data collection and analysis, and creation of the article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The APC is provided by the Southampton Hospitals Charity. The author(s) received no other financial support for the research, authorship, and/or publication of this article.
Ethical statement: Integrated Research Application system (IRAS) approval had been granted to Mr Alex Aarvold to analyze data from the cohort of DDH patients treated at Southampton Children’s Hospital (CHI 0509, REC 09/H0502/88—A Prospective, International Hip Dysplasia Registry with Follow-up to Skeletal Maturity: An Analysis of Risk Factors, Screening Practices and Treatment Outcomes). Ethical approval was subsequently granted by Ethics and Research Governance Online II (ERGO II)—Reference: 60802
References
- 1. Hunter JB. Femoral shaft fractures in children. Injury 2005; 36(Suppl. 1): A86–A93. [DOI] [PubMed] [Google Scholar]
- 2. Holmes SJ, Sedgwick DM, Scobie WG. Domiciliary gallows traction for femoral shaft fractures in young children. Feasibility, safety and advantages. J Bone Joint Surg Br 1983; 65(3): 288–290. [DOI] [PubMed] [Google Scholar]
- 3. Rampal V, Sabourin M, Erdeneshoo E, et al. Closed reduction with traction for developmental dysplasia of the hip in children aged between one and five years. J Bone Joint Surg Br 2008; 90(7): 858–863. [DOI] [PubMed] [Google Scholar]
- 4. Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: a clinical and experimental investigation. Can J Surg 1969; 12(1): 44–61. [PubMed] [Google Scholar]
- 5. Fogarty EE, Accardo NJ., Jr. Incidence of avascular necrosis of the femoral head in congenital hip dislocation related to the degree of abduction during preliminary traction. J Pediatr Orthop 1981; 1(3): 307–311. [DOI] [PubMed] [Google Scholar]
- 6. Weinstein SL, Dolan LA. Proximal femoral growth disturbance in developmental dysplasia of the hip: what do we know? J Child Orthop 2018; 12(4): 331–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Langenskiöld A, Paavilainen T. The effect of prereduction traction on the results of closed reduction of developmental dislocation of the hip. J Pediatr Orthop 2000; 20(4): 471–474. [PubMed] [Google Scholar]
- 8. Ishii Y, Ponseti IV. Long-term results of closed reduction of complete congenital dislocation of the hip in children under one year of age. Clin Orthop Relat Res 1978(137): 167–174. [PubMed] [Google Scholar]
- 9. Sibiński M, Murnaghan C, Synder M. The value of preliminary overhead traction in the closed management of DDH. Int Orthop 2006; 30(4): 268–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kutlu A, Ayata C, Ogün TC, et al. Preliminary traction as a single determinant of avascular necrosis in developmental dislocation of the hip. J Pediatr Orthop 2000; 20(5): 579–584. [DOI] [PubMed] [Google Scholar]
- 11. Segal LS, Boal DK, Borthwick L, et al. Avascular necrosis after treatment of DDH: the protective influence of the ossific nucleus. J Pediatr Orthop 1999; 19(2): 177–184. [DOI] [PubMed] [Google Scholar]
- 12. Sucato DJ, De La Rocha A, Lau K, et al. Overhead Bryant’s traction does not improve the success of closed reduction or limit AVN in developmental dysplasia of the hip. J Pediatr Orthop 2017; 37(2): e108–e113. [DOI] [PubMed] [Google Scholar]
- 13. Gangaram-Panday S, de Vos-Jakobs S, Reijman M. The effect of traction before closed reduction in patients with developmental dysplasia of the hip. Children 2022; 9(9): 1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Elerson EE, Martin BD, Muchow RD, et al. Outpatient Bryant’s overhead traction does not affect the rate of open reduction or a vascular necrosis in developmental dislocation of the hip. J Pediatr Orthop 2022; 42(3): e266–e270. [DOI] [PubMed] [Google Scholar]
- 15. Li YQ, Li M, Guo YM, et al. Chinese paediatric orthopaedics multicentre clinical study group. Traction Does not decrease failure of reduction and femoral head a vascular necrosis in patients aged 6–24 months with developmental dysplasia of the hip treated by closed reduction: a review of 385 patients and meta-analysis. J Pediatr Orthop B 2019; 28(5): 436–441. [DOI] [PubMed] [Google Scholar]
- 16. Nicholson JT, Foster RM, Heath RD. Bryant’s traction; a provocative cause of circulatory complications. J Am Med Assoc 1955; 157: 415–418. [DOI] [PubMed] [Google Scholar]
- 17. Taylor I. Ward manual of orthopaedic traction. Edinburgh: Churchill Livingstone, 1987. [Google Scholar]
- 18. Judd J, Aarvold A. What is the safe upper weight limit for Gallows traction? Pediatric orthopaedic practitioners society. In: Annual conference, Austin, TX, May 2018. [Google Scholar]
- 19. Narayanan U, Mulpuri K, Sankar WN, et al. Reliability of a new radiographic classification for developmental dysplasia of the hip. J Pediatr Orthop 2015; 35(5): 478–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kiani SN, Gornitzky AL, Matheney TH, et al. A prospective, multicenter study of developmental dysplasia of the hip: what can patients expect after open reduction? J Pediatr Orthop 2023; 43(5): 279–285. [DOI] [PubMed] [Google Scholar]
- 21. Castaneda P, Masrouha KZ, Ruiz CV, et al. Outcomes following open reduction for late-presenting developmental dysplasia of the hip. J Child Orthop 2018; 12(4): 323–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kothari A, Grammatopoulos G, Hopewell S, et al. How does bony surgery affect results of anterior open reduction in walking-age children with developmental hip dysplasia. Clin Orthop Relat Res 2016; 474(5): 1199–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aarvold A, Uren N, Lindisfarne EA, et al. Open Reduction, Capsulorrhaphy & Acetabuloplasty (ORCA): a one stop surgical treatment for infant DDH. In: British society of children’s orthopaedic surgeons (BSCOS), 2022, https://www.orthomedia.org.uk/Title/45aa0879-0342-477d-9623-60634b6c54e5
- 24. Ning B, Yuan Y, Yao J, et al. Analyses of outcomes of one- stage operation for treatment of late-diagnosed developmental dislocation of the hip: 864 hips followed for 3.2 to 8.9 years. BMC Musculoskelet Disord 2014; 15: 401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kershaw CJ, Ware HE, Pattinson R, et al. Revision of failed open reduction of congenital dislocation of the hip. J Bone Joint Surg Br 1993; 75(5): 744–749. [DOI] [PubMed] [Google Scholar]
- 26. Kamath SU, Bennet GC. Re-dislocation following open reduction for developmental dysplasia of the hip. Int Orthop 2005; 29(3): 191–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thomas SR, Wedge JH, Salter RB. Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. J Bone Joint Surg Am 2007; 89(11): 2341–2350. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cho-10.1177_18632521241229620 for Preoperative Gallows traction as an adjunct to hip open reduction surgery: Is it safe and is it effective? by Nicholas C Uren, Julia Judd, Edward A Lindisfarne, Kirsten G Elliott and Alexander Aarvold in Journal of Children’s Orthopaedics



