Abstract
Background
Lower‐limb revascularization is a surgical procedure that is performed to restore an adequate blood supply to the limbs. Lower‐limb revascularization surgery is used to reduce pain and sometimes to improve lower‐limb function. Neuraxial anaesthesia is an anaesthetic technique that uses local anaesthetics next to the spinal cord to block nerve function. Neuraxial anaesthesia may lead to improved survival. This systematic review was originally published in 2010 and was first updated in 2011 and again in 2013.
Objectives
To determine the rates of death and major complications associated with spinal and epidural anaesthesia as compared with other types of anaesthesia for lower‐limb revascularization in patients aged 18 years or older who are affected by obstruction of lower‐limb vessels.
Search methods
The original review was published in 2010 and was based on a search until June 2008. In 2011 we reran the search until February 2011 and updated the review. For this second updated version of the review, we searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, LILACS, CINAHL and Web of Science from 2011 to April 2013.
Selection criteria
We included randomized controlled trials comparing neuraxial anaesthesia (spinal or epidural anaesthesia) versus other types of anaesthesia in adults (18 years or older) with arterial vascular obstruction undergoing lower‐limb revascularization surgery.
Data collection and analysis
Two review authors independently performed data extraction and assessed trial quality. We pooled the data on mortality, myocardial infarction, lower‐limb amputation and pneumonia. We summarized dichotomous data as odds ratio (OR) with 95% confidence interval (CI) using a random‐effects model.
Main results
In this updated version of the review, we found no new studies that met our inclusion criteria. We included in this review four studies that compared neuraxial anaesthesia with general anaesthesia. The total number of participants was 696, of whom 417 were allocated to neuraxial anaesthesia and 279 to general anaesthesia. Participants allocated to neuraxial anaesthesia had a mean age of 67 years, and 59% were men. Participants allocated to general anaesthesia had a mean age of 67 years, and 66% were men. Four studies had an unclear risk of bias. No difference was observed between participants allocated to neuraxial or general anaesthesia in mortality rate (OR 0.89, 95% CI 0.38 to 2.07; 696 participants; four trials), myocardial infarction (OR 1.23, 95% CI 0.56 to 2.70; 696 participants; four trials), and lower‐limb amputation (OR 0.84, 95% CI 0.38 to 1.84; 465 participants; three trials). Pneumonia was less common after neuraxial anaesthesia than after general anaesthesia (OR 0.37, 95% CI 0.15 to 0.89; 201 participants; two trials). Evidence was insufficient for cerebral stroke, duration of hospital stay, postoperative cognitive dysfunction, complications in the anaesthetic recovery room and transfusion requirements. No data described nerve dysfunction, postoperative wound infection, patient satisfaction, postoperative pain score, claudication distance and pain at rest.
Authors' conclusions
Available evidence from included trials that compared neuraxial anaesthesia with general anaesthesia was insufficient to rule out clinically important differences for most clinical outcomes. Neuraxial anaesthesia may reduce pneumonia. No conclusions can be drawn with regard to mortality, myocardial infarction and rate of lower‐limb amputation, or less common outcomes.
Keywords: Aged; Female; Humans; Male; Amputation, Surgical; Amputation, Surgical/statistics & numerical data; Anesthesia, Epidural; Anesthesia, Epidural/adverse effects; Anesthesia, Epidural/mortality; Anesthesia, General; Anesthesia, General/adverse effects; Anesthesia, General/mortality; Anesthesia, Spinal; Anesthesia, Spinal/adverse effects; Anesthesia, Spinal/mortality; Lower Extremity; Lower Extremity/blood supply; Lower Extremity/surgery; Myocardial Infarction; Myocardial Infarction/epidemiology; Pneumonia; Pneumonia/epidemiology; Randomized Controlled Trials as Topic; Vascular Surgical Procedures
Plain language summary
Neuraxial anaesthesia for surgical correction of arterial vascular obstruction in the lower limbs
Atherosclerosis is a chronic inflammatory process that is responsible for reduced blood flow to some parts of the body, including the lower limbs. People who do not receive adequate treatment can lose their lower limbs. Bypassing arterial vascular obstruction in the legs is a surgical procedure that improves blood flow to reduce leg pain and sometimes to improve function. The mortality rate can be 10.5% after acute occlusion of an arterial blood vessel. The surgical procedure can improve outcomes when performed up to 12 hours after symptoms are first noted. Usually the procedure is performed with the patient unconscious and under general anaesthesia or awake but with legs numbed by neuraxial anaesthesia. Neuraxial anaesthesia may be administered as an injection of local anaesthetic around the spinal cord either in the back (spinal anaesthetic) or in the area where the nerves from the legs come together (epidural anaesthesia). A combination of general and neuraxial anaesthesia can be used. Other types of anaesthesia are used less often. At present, no single guideline shows why one anaesthetic technique is better than another. This systematic review is important because review authors assessed the risk of important outcomes after lower‐limb revascularization with the participant under neuraxial or general anaesthesia. They performed this systematic review to answer a single research question: What are the rates of death and major complications with spinal and epidural anaesthesia as compared with other types of anaesthesia for lower‐limb revascularization? In this second update of the Cochrane review, we searched the databases until April 2013 but found no new studies. The total number of participants in the four included studies was 696, of whom 417 received neuraxial anaesthesia and 279 received general anaesthesia. No evidence revealed differences in postoperative risk of death, myocardial infarction or leg amputation between the two types of anaesthetic. The risk of pneumonia was 9% after neuraxial anaesthesia and 20% after general anaesthesia. Evidence was insufficient to show the effects of neuraxial anaesthesia compared with other types of anaesthesia on cerebral stroke, duration of hospital stay, postoperative cognitive dysfunction, complications in the anaesthetic recovery room and transfusion requirements. No data described nerve dysfunction, postoperative wound infection, patient satisfaction, postoperative pain score, claudication distance and pain at rest. One study recruited more than 50% of all reported cases.This systematic review shows that neuraxial anaesthesia may reduce the risk of pneumonia after lower‐limb revascularization, but evidence is insufficient to support other benefits or harms.
Summary of findings
Summary of findings for the main comparison. Neuraxial versus general anaesthesia for lower‐limb revascularization.
| Neuraxial versus general anaesthesia for lower‐limb revascularization | ||||||
| Patient or population: participants with lower‐limb revascularization Settings: Intervention: Neuraxial versus general anaesthesia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Neuraxial versus general anaesthesia | |||||
| Mortality-At any time | Study population | OR 0.89 (0.38 to 2.07) | 696 (4 studies) | ⊕⊕⊝⊝ low1 | ||
| 43 per 1000 | 38 per 1000 (17 to 85) | |||||
| Medium‐risk population | ||||||
| 55 per 1000 | 49 per 1000 (22 to 108) | |||||
| Myocardial infarction-Spinal anaesthesia | Study population | OR 1.89 (0.5 to 7.21) | 306 (2 studies) | ⊕⊕⊝⊝ low1,2 | ||
| 25 per 1000 | 46 per 1000 (13 to 156) | |||||
| Medium‐risk population | ||||||
| 24 per 1000 | 44 per 1000 (12 to 151) | |||||
| Myocardial infarction-Epidural anaesthesia | Study population | OR 0.98 (0.37 to 2.58) | 390 (3 studies) | ⊕⊕⊝⊝ low1,2 | ||
| 50 per 1000 | 49 per 1000 (19 to 120) | |||||
| Medium‐risk population | ||||||
| 44 per 1000 | 43 per 1000 (17 to 106) | |||||
| Amputation rate-Spinal anaesthesia | Study population | OR 1.04 (0.35 to 3.06) | 235 (2 studies) | ⊕⊕⊝⊝ low1,2 | ||
| 71 per 1000 | 74 per 1000 (26 to 190) | |||||
| Medium‐risk population | ||||||
| 69 per 1000 | 72 per 1000 (25 to 185) | |||||
| Amputation rate-Epidural anaesthesia | Study population | OR 0.66 (0.21 to 2.07) | 230 (2 studies) | ⊕⊕⊝⊝ low1,2 | ||
| 81 per 1000 | 55 per 1000 (18 to 154) | |||||
| Medium‐risk population | ||||||
| 79 per 1000 | 54 per 1000 (18 to 151) | |||||
| Pneumonia | Study population | OR 0.37 (0.15 to 0.89) | 201 (2 studies) | ⊕⊝⊝⊝ very low2,3,4 | ||
| 196 per 1000 | 83 per 1000 (35 to 178) | |||||
| Medium‐risk population | ||||||
| 196 per 1000 | 83 per 1000 (35 to 178) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
1 All trials recruited participants from elective surgery and did not define criteria for participants with high risk, moderate risk or low risk. Authors did not describe blinding. In Christopherson 1993, the cardiologists assessing cardiac outcomes were blinded to the group to which participants were allocated. Christopherson 1993, Cook 1986 and Dodds 2007 included few participants. 2 In Christopherson 1993, the rate of missing data was described as 3.1% in the intervention group and 1.9% in the control group. Cook 1986 reported that 11/50 intervention participants and 4/51 control participants were lost to follow‐up. Dodds 2007 did not report mortality during one‐year follow up. Bode 1996 reported complete data collection for non‐surgical outcomes during hospitalization in 423 participants. However, surgical outcomes over 30 postoperative days were reported for only 264 participants (159 missing). 3Cook 1986 described that more elderly participants and smokers were allocated to the general anaesthesia group and that this can influenced results 4 In Cook 1986, participants were analysed during hospital stay
Background
Description of the condition
Atherosclerosis is an inflammatory pathology that accumulates with age through an irreversible process (Tonner 2003). It causes endothelial dysfunction and is responsible for stiffness and loss of elasticity in the blood vessel wall, stenosis of the artery, plaque rupture and formation of aneurysms (vascular dilations of an artery) (Howard‐Alpe 2006). This systemic disease is responsible for reduced blood flow in many regional circulation systems, including those that supply the brain, kidneys, mesentery, myocardium and limbs (Smaka 2013).
The number of patients undergoing lower‐limb revascularization, a surgical procedure performed to restore adequate blood supply to the limbs, has increased as surgeons have attempted to improve functional status in elderly patients (Smaka 2013). Aging is associated with increasing prevalence of multiple diseases and disabilities (Fukuse 2005). Deteriorating respiratory function is associated with advancing age and, when combined with a variety of coexisting factors, predisposes a person to pulmonary complications (Zaugg 2000). Mortality rate can reach 10.5% after acute occlusion of arterial blood vessels; however, when surgical procedures are performed up to 12 hours after the start of symptoms, improved outcomes have been reported (Manojlović 2013).
Description of the intervention
Neuraxial anaesthesia refers to the injection of local anaesthetic drugs next to the spinal cord or the spinal nerves to block nerve input (Rodgers 2000). When these agents are injected into the subarachnoid space, the anaesthesia is termed spinal anaesthesia, and when they are injected into the epidural space, epidural anaesthesia (Rodgers 2000). Lower risk of respiratory complications such as myocardial infarction, deep vein thrombosis (formation of a blood clot within a vein) and pulmonary embolus (a blood clot that starts in a distant vein or artery and blocks blood supply to the lungs) has been reported after neuraxial blockade compared with general anaesthesia (Bonnet 2005). Neuraxial anaesthesia carries a risk of haematoma (a localized swelling filled with blood) in the vertebral canal, which is due to the frequent use of heparin during vascular surgery; the likelihood of this must always be considered preoperatively before any neuraxial anaesthesia is planned (Rasmussen 2000).
General anaesthesia refers to temporary drug‐induced loss of consciousness (Afolabi 2007). Advantages of general anaesthesia include quick onset, reliability in providing adequate surgical anaesthesia, protection of the airway and avoidance of oversedation (Bode 1994). Complications include adverse reactions to the drugs used, difficulty in maintaining or establishing an airway, intraoperative hypotension and damage to the teeth or upper airways (Parker 2011).
How the intervention might work
Surgical and anaesthetic interventions lead to a great stress response that can be attributed to catecholamine levels and can bring changes in physiological functions (Smaka 2013). Potential advantages of neuraxial anaesthesia compared with general anaesthesia include attenuation of the neuroendocrine stress response, less impairment of cardiac function in patients with ischaemic (inadequate supply of oxygen) heart disease and fewer postoperative pulmonary complications (Bode 1994).
Minimally invasive surgical approaches combined with neuraxial anaesthetic techniques may be advantageous for the elderly, particularly when orthopaedic and vascular surgery of the lower extremities must be performed (Zaugg 2000). Neuraxial anaesthesia has been recommended (Borgeat 2003) because general anaesthesia is associated with greater risk of postoperative respiratory complications (Smaka 2013).
Why it is important to do this review
The importance of selecting the best anaesthesia for patients undergoing lower‐extremity revascularization has been debated for many years, and many clinicians have developed strong convictions that certain anaesthetic techniques are preferable for these patients (Tuman 1994). At the moment, no single guideline in clinical practice shows why one anaesthetic technique is better than another. Therefore it is relevant to assess the risk of important outcomes after lower‐limb revascularization under neuraxial or general anaesthesia. Several studies have compared the impact of general, spinal and epidural anaesthesia on postoperative complications in some clinical scenarios, but no systematic review to date has analysed the impact of the choice of anaesthetic technique on lower‐limb revascularization.
Objectives
The objective of this review was to determine the rates of death and major complications associated with spinal and epidural anaesthesia as compared with other types of anaesthesia for lower‐limb revascularization in patients aged 18 years or older who are affected by obstruction of lower‐limb vessels.
We defined lower‐limb revascularization as a surgical procedure that is performed to restore an adequate blood supply to the limbs.
Methods
Criteria for considering studies for this review
Types of studies
We included blinded or unblinded randomized controlled trials (RCTs) that evaluated the effects of neuraxial anaesthesia compared with other types of anaesthesia for elective or emergency lower‐limb revascularization surgery.
We excluded studies that were not randomized and studies of vascular surgery that did not consist of lower‐limb revascularization or limb revascularization above the iliac vessels. We also excluded studies that did not report the relevant outcomes.
Types of participants
We included studies with adult participants (aged 18 years and older) who were undergoing surgery for lower‐limb revascularization.
Types of interventions
Our experimental intervention was neuraxial anaesthesia, spinal or epidural.
Our control intervention was general anaesthesia.
Types of outcome measures
We included studies that analysed the effects of neuraxial anaesthesia compared with other types of anaesthesia on our primary and secondary outcomes.
Primary outcomes
Mortality (participants died during their hospital stay or during their follow‐up time).
Cerebral stroke (death of cerebral cells).
Myocardial infarction (death of heart cells).
Nerve dysfunction (loss of nerve function).
Rate of lower‐limb amputation, both in the operating room and during the postoperative period.
Secondary outcomes
Duration of hospital stay.
Postoperative cognitive dysfunction (a state of confusion after surgery).
Postoperative wound infection.
Pneumonia.
Complications in the anaesthetic recovery room (e.g. hypertension, hypotension, cardiac dysrhythmia, nausea, vomiting, tremor, need for supplementary oxygen).
Participant satisfaction.
Postoperative pain score (using a scale to quantify pain level after surgery).
Transfusion requirement (number of units transfused).
Urinary retention.
Claudication distance (pain‐free walking distance).
Pain at rest (pain in lower limb after surgery).
Search methods for identification of studies
Electronic searches
In our first published review, we searched the databases from inception until 2008 (Barbosa 2010). In 2011 we reran the searches from June 2008 until February 2011 and published the updated review.
In this second update of the review, we searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, 2013, Issue 4); MEDLINE (February 2011 to April 2013); EMBASE (February 2011 to April 2013); LILACS (February 2011 to April 2013); CINAHL (February 2011 to April 2013) and ISI Web of Science (February 2011 to April 2013) without language or publication restrictions.
We used the optimally sensitive strategies of The Cochrane Collaboration to identify randomized controlled trials in the MEDLINE and EMBASE searches (Castro 1999; Dickersin 1994; Lefebvre 1996).
We based each search strategy on the one developed for MEDLINE. Our search strategies can be found in the Appendices: CENTRAL (Appendix 1), MEDLINE (Appendix 2), EMBASE (Appendix 3), LILACS (Appendix 4), CINAHL (Appendix 5) and ISI Web of Science (Appendix 6).
Searching other resources
In our previous review, we checked the reference lists of included studies (Barbosa 2010).
We searched www.clinicaltrials.gov.
Data collection and analysis
Selection of studies
Two review authors, Fabiano Timbó Barbosa (FTB) and Mario Jorge Juca (MJJ), independently read the titles and abstracts of any reports identified by the search.
We retrieved and evaluated full‐text versions of potentially relevant studies that were chosen by at least one review author. We ensured that multiple publications of the same data set were used only once.
We resolved disagreements during a consensus meeting.
Data extraction and management
We followed the methods recommended by the Cochrane Anaesthesia Review Group.
Two review authors (FTB and MJJ) independently selected trials that met the inclusion criteria, using the information described in the section Criteria for considering studies for this review. We excluded studies that did not meet the inclusion criteria. The reasons for their exclusion are stated in the table Characteristics of excluded studies.
Two review authors (FTB and MJJ) independently extracted data using a standardized checklist.
We independently extracted and cross‐checked data. We summarized the results of each RCT on an intention‐to‐treat (ITT) basis for each outcome. We did not calculate continuous outcomes because the authors of the included studies did not describe any of the following information: mean, standard deviation (SD) or number of participants within each group.
We collected the following data (Appendix 7).
Methods: study question, hypothesis, objective, sequence randomization, allocation concealment, blinding (person responsible for participant care, participant, outcome assessor, researcher, data analysts and personnel who wrote the article), follow‐up time (duration, withdrawals and dropouts), how participant eligibility was defined, number of participants who received the intended treatment, number of participants who were analysed, time points at which measurements were taken during the study, time points reported in the study, the nature of trial design (parallel vs cross‐over), prognostic characteristics between groups, statistical methods (ITT analyses, per‐protocol analyses, subgroup analyses) and sample‐size calculations.
Participants: inclusion criteria, age, sex, number of participants, exclusion criteria, duration of the study and location of the study.
Interventions: anaesthetic technique and drugs used in both the intervention group and the control group.
Outcomes: mortality, cerebral stroke, myocardial infarction, nerve dysfunction, postoperative lower‐limb amputation rate, duration of hospital stay, postoperative cognitive dysfunction, postoperative wound infection, pneumonia, complications in the anaesthetic recovery room (e.g. hypertension, hypotension, cardiac dysrhythmia, nausea, vomiting, tremor, the need for supplementary oxygen), participant satisfaction, postoperative pain score, transfusion requirement, urinary retention, claudication distance and rest pain.
For studies with duplicate publications, we extracted data from both publications.
We resolved disagreements in a consensus meeting.
Assessment of risk of bias in included studies
Each included study was appraised according to the criteria described below and was designated as low risk, high risk or unclear risk of bias (Higgins 2011).
1. Random sequence generation Low risk: adequate sequence generation reported by referring to a random number table; using computer‐generated random numbers, codes or sealed envelopes; coin tossing; shuffling cards or envelopes; throwing dice; and drawing lots. High risk: sequence generated by odd or even date of birth; some rule based on date (or day) of admission; some rule based on hospital or clinic record number. Unclear risk: insufficient information about the sequence generation process to permit judgement of ‘low risk’ or ‘high risk’.
2. Allocation concealment Low risk: central allocation (including telephone, Web‐based and pharmacy‐controlled randomization); sequentially numbered drug containers of identical appearance and sequentially numbered, opaque, sealed envelopes. High risk: use of an open random allocation schedule (e.g. a list of random numbers); assignment envelopes without appropriate safeguards (e.g. if envelopes were unsealed, non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; and any other explicitly unconcealed procedure. Unclear risk: randomization mentioned in the trial report but no information provided on the method used; or method reported that was not clearly adequate.
3. Blinding of participants and personnel Low risk: no blinding or incomplete blinding but the review authors judged that the outcome is not likely to be influenced by lack of blinding; or blinding of participants and key study personnel ensured and unlikely that the blinding could have been broken. High risk: no blinding or incomplete blinding, and the outcome was likely to be influenced by lack of blinding; blinding of key study participants and personnel attempted, but likely that the blinding could have been broken and the outcome was likely to be influenced by lack of blinding. Unclear risk: insufficient information to permit judgement of ‘low risk’ or ‘high risk’, and the study did not address this outcome.
4. Blinding of outcome assessment Low risk: likely to be influenced by lack of blinding; blinding of outcome assessment ensured, and unlikely that the blinding could have been broken. High risk: no blinding of outcome assessment, and outcome measurement was likely to be influenced by lack of blinding; or blinding of outcome assessment but likely that the blinding could have been broken, and the outcome measurement was likely to be influenced by lack of blinding. Unclear risk: insufficient information to permit judgement of ‘low risk’ or ‘high risk’, and the study did not address this outcome.
5. Incomplete outcome data Low risk: no missing outcome data; reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size; missing data imputed using appropriate methods. High risk: reason for missing outcome data likely to be related to true outcome, with imbalance in numbers or reasons for missing data across intervention groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size; 'as‐treated’ analysis done with substantial departure of the intervention received from that assigned at randomization; potentially inappropriate application of simple imputation. Unclear risk: insufficient reporting of attrition and exclusions to permit judgement of ‘low risk’ or ‘high risk’ (e.g. number randomly assigned not stated, no reasons provided for missing data), and the study did not address this outcome.
6. Selective reporting Low risk: The study protocol is available, and all of the study’s prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way; the study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were prespecified (convincing text of this nature may be uncommon). High risk: Not all of the study’s prespecified primary outcomes have been reported; one or more primary outcomes are reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not prespecified; one or more of the reported primary outcomes were not prespecified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review were reported incompletely, so that they cannot be entered in a meta‐analysis; the study report failed to include results for a key outcome that would be expected to have been reported for such a study. Unclear risk: Reporting of attrition and exclusions were insufficient to permit judgement of ‘low risk’ or ‘high risk’.
7. Other bias Low risk: The study appears to be free of other sources of bias. High risk: The study had a potential source of bias related to the specific study design used, has been claimed to have been fraudulent, or had some other problem. Unclear risk: Information is insufficient for review authors to assess whether an important risk of bias exists, or rationale or evidence that an identified problem will introduce bias is insufficient.
Measures of treatment effect
We performed the meta‐analyses using Review Manager software (RevMan 5.1). We identified 22 possibly relevant studies and included four studies. We were not certain that there was no statistical heterogeneity, so we performed all analyses with the random‐effects model. We calculated dichotomous outcomes as odds ratios (ORs) with 95% confidence intervals (CIs).
Unit of analysis issues
We did not have any unit of analysis issues.
Dealing with missing data
We tried to contact main authors to ask them for missing data.
Assessment of heterogeneity
We assessed statistical heterogeneity in the results of the trials both by inspecting a graphic representation of the study results with their 95% CI and by using a test of heterogeneity. The two tests used were the standard Chi2 test with N degrees of freedom, where N equals the number of trials contributing data minus one, and the I2 statistic, where I2 > 50% implies significant heterogeneity (Higgins 2002).
Agreement between the review authors during the review process was determined with the use of kappa statistics (Sim 2005). Possible interpretation included poor agreement (< 0.20), fair agreement (0.20 to 0.40), moderate agreement (0.4 to 0.6), good agreement (0.6 to 0.8) and very good agreement (0.8 to 1.0).
Assessment of reporting biases
We used the funnel plot to detect reporting bias. It is a scatter plot of the intervention effect estimate from included studies against each size of the study. If publication bias is absent, this plot has an inverted funnel shape.
Data synthesis
We pooled the results from included randomized controlled trials using a random‐effects model for I2 > 50%.
Subgroup analysis and investigation of heterogeneity
We did not plan a subgroup analysis. Three possible reasons for heterogeneity were prespecified: different responses based on differences in the quality of studies; sample sizes; and clinical heterogeneity (external validity).
Sensitivity analysis
We performed sensitivity analysis using values for dropouts and for participants lost in follow‐up testing of the best and the worst scenario. We tested our results using a fixed‐effect model.
Results
Description of studies
A description of the studies can be seen in Characteristics of included studies and Characteristics of excluded studies. Agreement between review authors regarding article selection was very good, with kappa statistics ranging from 0.8 to 1.
Results of the search
In this updated review, we reran our search until April 2013. Our search strategy identified 5885 publications in our previous work and 1192 in this updated review (Figure 1).
1.
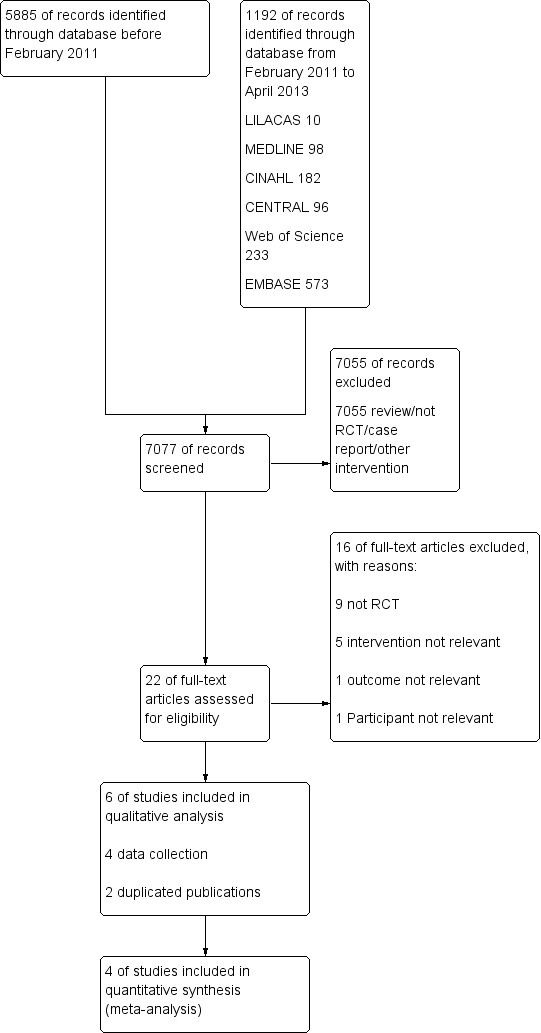
Flow diagram of the searching results (entire review).
Included studies
We did not find any new studies that fit our inclusion criteria. We included four studies in this review (Bode 1996; Christopherson 1993; Cook 1986; Dodds 2007). Participants were scheduled for elective surgery in three included studies (Bode 1996; Christopherson 1993; Dodds 2007). Cook 1986 did not report this datum. The included randomized controlled trials are superiority trials.
The number of participants in each included study was as follows: 100 participants in Christopherson 1993; 101 participants in Cook 1986; 77 participants in Dodds 2007 and 423 participants in Bode 1996. The total number of included participants in the meta‐analysis was 696, of whom 417 were allocated to neuraxial anaesthesia and 279 to general anaesthesia. Dodds 2007 reported that five participants underwent two operations, receiving two anaesthetic techniques.
The age limit for participation in Dodds 2007 was 50 years or older; no attempt at age limitation was reported by the other three included studies. Participants allocated to neuraxial anaesthesia had a mean age of 67 years, and 59% were men. Participants allocated to general anaesthesia had a mean age of 67 years, and 66% were men.
Christopherson 1993 recorded rehospitalization, cardiac morbidity and reoperation over six months. Two studies followed participants postoperatively for one year (Cook 1986; Dodds 2007), and Bode 1996 followed all participants until hospital discharge (for non‐surgical outcomes). Bode 1996 analysed graft patency 30 days after surgery in 264/423 of the recruited participants, and these data are provided in the Pierce 1997 publication, which used a per‐protocol analysis .
Grafting is a surgical procedure that takes tissue from one part of the body and moves it to another part of the body. This graft can be taken from the patient or from another person, or it can be artificially manufactured.
All studies compared neuraxial anaesthesia with general anaesthesia and were superiority trials. General anaesthesia was maintained with halogenated agents and nitrous oxide in all four studies (Bode 1996; Christopherson 1993; Cook 1986; Dodds 2007). Three studies compared general anaesthesia with one type of neuraxial blockade, whilst Bode 1996 compared general anaesthesia with both spinal and epidural techniques. We contacted the authors of the included studies. Unfortunately the information requested has not been made available.
Excluded studies
In our previous review (Barbosa 2010), we identified 22 potentially relevant publications. One of those studies was in Italian (Romano 1980) and another in Russian (Gallinger 1997), but the abstracts were in English and we analysed those. We excluded 16 of the initial 22 publications: nine studies were not randomized (Barkmeier 1997; Gallinger 1997; González‐Fajardo 1995; Hertzer 1981; Lurquin 1993; Rivers 1991; Romano 1980; Sabaté 1994; Singh 2006); and in five studies, the intervention was not relevant (Ballotta 2003; Ballotta 2004; Peduto 2003; Reuben 1994; Vascular Society 1995). One study did not have relevant outcomes (Breslow 1993), and in another the participants did not meet our inclusion criteria (Casati 1999).
Risk of bias in included studies
The included studies were RCTs.There was homogeneity between the participants included in the RCTs and their research questions were similar. All studies reached a moderate level of quality (Figure 2; Figure 3; Table 1). The data analysed in the included studies can be seen in the Characteristics of included studies.
2.
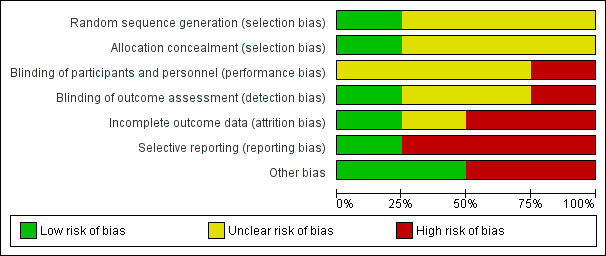
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
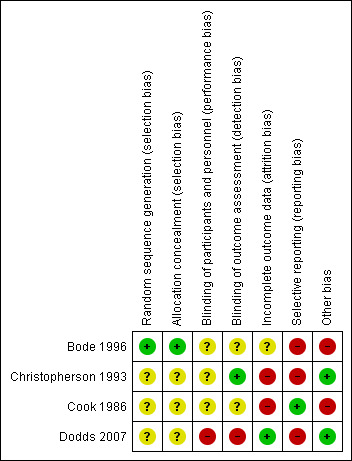
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Allocation
The method of random sequence generation was described and was adequate in Bode 1996. The authors of the other three studies reported that participants were randomly assigned without describing the sequence generation.
The method used to conceal the allocation sequence was clear in Bode 1996 but unclear in the other studies.
Blinding
In Christopherson 1993 the cardiologists assessing cardiac outcomes were blinded to the intervention group to which participants were allocated. No other attempts at blinding were reported by Christopherson 1993 or by the other three studies.
Incomplete outcome data
In Christopherson 1993 the rate of missing data was described as 3.1% in the intervention group and 1.9% in the control group.
Cook 1986 reported that 11/50 intervention participants and 4/51 control participants were lost to follow‐up.
Dodds 2007 did not report mortality during the one‐year follow‐up.
Bode 1996 reported complete data collection for non‐surgical outcomes during hospitalization in 423 participants. However, surgical outcomes over 30 postoperative days were reported for only 264 participants (159 missing).
Selective reporting
Christopherson 1993 incompletely reported duration of hospital stay; which we could not enter into the meta‐analysis.
One study reported all protocol outcomes (Cook 1986).
Dodds 2007 did not report mortality during the one‐year follow‐up.
Bode 1996 reported mortality and myocardial infarction. The outcome amputation was observed until 30 days.
Other potential sources of bias
In one study (Christopherson 1993), we could not find other sources of bias.
Recruitment bias may have affected the results of Cook 1986 because more elderly participants and smokers were included in the general anaesthesia group.
Dodds 2007 reported that 77 participants were allocated to groups: 72 participants had one operation and five participants had two operations, for a total of 77 participants having 82 operations. Five participants received both general and neuraxial anaesthesia.
Data in Bode 1996 and Christopherson 1993 were duplicated in two other publications.
Assessment of risk of bias in included studies can be found in the risk of bias graph in Figure 2 and the risk of bias summary in Figure 3.
Effects of interventions
See: Table 1
The authors of included studies were contacted to supply missing data. Unfortunately only Dodds 2007 was localized, but he did not give us the requested information. We used in our analysis the total number of 696 participants randomly assignedWe assumed that each event happened only once per participant. Included studies provided no data on nerve dysfunction, postoperative wound infection, participant satisfaction, postoperative pain score, claudication distance and pain at rest.
Bode 1996, Christopherson 1993 and Cook 1986 reported incorrect data for some measured outcomes.
The outcomes: nerve dysfunction, participant satisfaction, postoperative pain score, urinary retention, claudication distance and pain at rest were not measured by the RCTs.
Primary outcomes
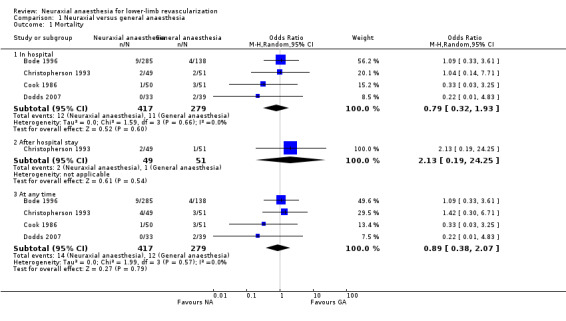
Mortality
All studies reported death (Figure 4). No statistically significant difference in mortality was noted between participants given neuraxial anaesthesia and those receiving general anaesthesia (OR 0.89, 95% CI 0.38 to 2.07).
4.
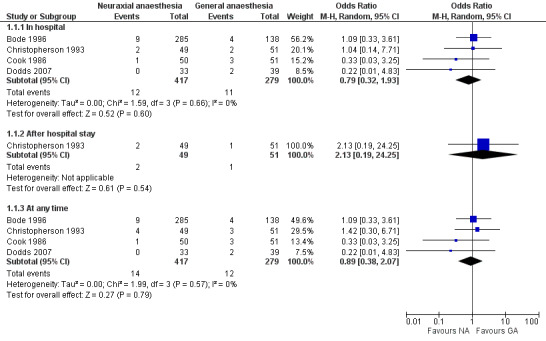
Forest plot of comparison: 1 Neuraxial versus general anaesthesia, outcome: 1.1 Mortality.
All studies reported mortality in hospital. In this analysis, 417 participants were allocated to neuraxial anaesthesia and 279 to general anaesthesia. No statistically significant difference in mortality whilst participants were hospitalized was noted (OR 0.79, 95% CI 0.32 to 1.93).
One study reported mortality after discharge from hospital (Christopherson 1993). In this analysis, 49 participants were allocated to neuraxial anaesthesia and 51 to general anaesthesia. No statistically significant difference in mortality was noted (OR 2.13, 95% CI 0.19 to 24.25).
Cerebral stroke
In one study (Cook 1986), a participant who received general anaesthesia had a cerebral stroke; statistically this did not represent a significant difference between groups. Bode 1996 reported that three participants (of 423) died because of cerebral stroke but did not report the overall rate of stroke in each group.
Myocardial infarction
This outcome was analysed in all studies (see Analysis 1.2). Two studies compared spinal anaesthesia with general anaesthesia (Bode 1996; Cook 1986), and three studies compared epidural anaesthesia with general anaesthesia (Bode 1996; Christopherson 1993; Dodds 2007). In this analysis, 417 participants were allocated to neuraxial anaesthesia and 279 to general anaesthesia. No statistically significant difference in risk of postoperative myocardial infarction was noted (OR 1.23, 95% CI 0.56 to 2.70). The results of these studies were statistically homogeneous (Tau2 = 0.00, Chi2 = 0.38 and I2 = 0%).
1.2. Analysis.
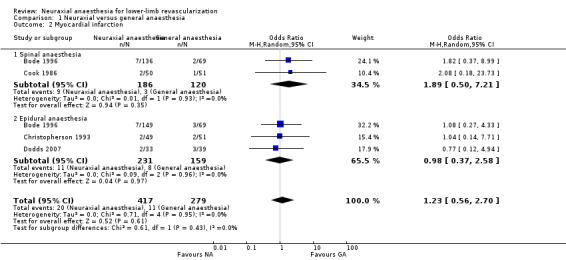
Comparison 1 Neuraxial versus general anaesthesia, Outcome 2 Myocardial infarction.
Postoperative rate of lower‐limb amputation
This outcome was analysed in three studies (Bode 1996; Christopherson 1993; Cook 1986) (see Analysis 1.3). In this analysis, 267 participants were allocated to neuraxial anaesthesia and 198 to general anaesthesia. No statistically significant difference in amputation risk was noted (OR 0.84, 95% CI 0.38 to 1.84). Results were statistically homogeneous.
1.3. Analysis.
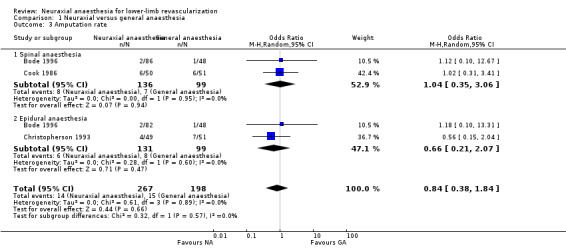
Comparison 1 Neuraxial versus general anaesthesia, Outcome 3 Amputation rate.
Authors of the included studies did not explicitly state whether they counted participants or amputations. We assumed that each participant experienced a maximum of one amputation.
Two studies (Bode 1996; Cook 1986) compared spinal anaesthesia with general anaesthesia. In this analysis, 136 participants were allocated to spinal anaesthesia and 99 to general anaesthesia. No statistically significant difference in amputation risk was noted (OR 1.02, 95% CI 0.35 to 3.06).
Two studies (Bode 1996; Christopherson 1993) compared epidural anaesthesia with general anaesthesia. In this analysis, 131 participants were allocated to epidural anaesthesia and 99 to general anaesthesia. No statistically significant difference in amputation risk was noted (OR 0.66, 95% CI 0.25 to 2.07).
Secondary outcomes
Duration of hospital stay
Two studies reported length of stay (Bode 1996; Christopherson 1993). Christopherson 1993 reported the median, not the mean. Bode 1996 reported no difference in mean length of stay: spinal anaesthesia 17 (SD 16) days, epidural anaesthesia 19 (SD 18) days and general anaesthesia 18 (SD 15) days.
Postoperative cognitive dysfunction
In one study, no difference in risk of postoperative delirium was noted between the general anaesthesia group (6/51) and the spinal anaesthesia group (9/50) (Cook 1986).
Pneumonia
This outcome was analysed in two studies (Christopherson 1993; Cook 1986) (see Analysis 1.4).
1.4. Analysis.
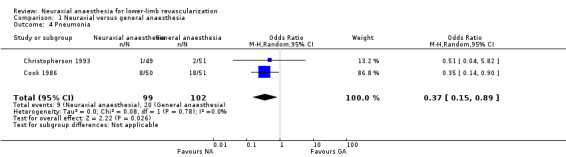
Comparison 1 Neuraxial versus general anaesthesia, Outcome 4 Pneumonia.
Christopherson 1993 defined major infection as pneumonia or sepsis. We assumed that participants experienced pneumonia.
The risk of pneumonia was less after neuraxial anaesthesia than after general anaesthesia (OR 0.37, 95% CI 0.15 to 0.89; 201 participants, two trials) (Analysis 1.4). Results of these studies were statistically homogeneous (Tau2 = 0.00, Chi2 = 0.08 and I2 = 0%).
Complications in the anaesthetic recovery room
One study (Cook 1986) provided data about this outcome. One participant in the general anaesthesia group experienced cardiac arrest (no statistically significant difference was noted between the groups).
Transfusion requirement
One study reported the volume of blood transfused (Christopherson 1993). No differences between neuraxial and general anaesthesia either during surgery (0.9 (SD 1.3) units vs 0.7 (SD 1.3) units, respectively) or in intensive care (0.15 (SD 0.41) units vs 0.33 (SD 0.71) units, respectively) were noted.
Subgroup analyses and investigation of heterogeneity
We did not perform subgroup analyses. We broke down our analysis by considering different neuraxial anaesthetic techniques. Different durations of follow‐up reported in each study for outcome assessment were considered in the mortality data analysis.
Differences in the quality of studies were not considered a reason for heterogeneity (Figure 3).
If we consider mortality frequency as 5% in one group and as 3% in the other, with 80% statistical power and a 5% significance level, the authors of the randomized controlled trials needed 1504 participants. Participants recruited in each study totalled 423 in Bode 1996, 100 in Christopherson 1993, 101 in Cook 1986 and 77 in Dodds 2007. We did not consider these different numbers of recruited participants as a cause of heterogeneity because the results observed in a particular included study were not different from those reported for other studies, except for pneumonia. A systematic review showed that mortality rate could be lower if neuraxial anaesthesia was used for orthopaedic surgical procedures, but this result was not the same for other clinical scenarios (Rodgers 2000). Cook 1986 showed different results for pneumonia, but the authors reported that more elderly people and smokers were included in the general anaesthesia group.
We did not identify clinical heterogeneity.
Publication bias
The shape of the funnel plot was not asymmetrical, and the overall effect of meta‐analysis was not affected by publication bias. The small number of included studies in this systematic review suggests the need for cautious interpretation.
Sensitivity analysis
We used participants lost during follow up time and tested the best and worst scenarios. The effects of the interventions did not change at the end of the analysis. We did not perform this assessment for pneumonia because data on this outcome were reported only for the time of hospital stay. Although Cook 1986 reported that more elderly people and smokers were included in the general anaesthesia group, we could not execute the meta‐analysis of pneumonia without including this trial. Use of a fixed‐effect model of analysis did not change the results.
Discussion
Neuraxial anaesthesia has been used in lower‐limb revascularization surgery for many years because some clinicians believe that this technique offers advantages over other types of anaesthesia. Although it was our intention to compare neuraxial anaesthesia with other types of anaesthesia, we found only studies that compared neuraxial with general anaesthesia for lower‐limb revascularization surgery.
The included studies in this systematic review explored spinal and epidural anaesthesia only when general anaesthesia was used and used different epidural drugs and levels of block. Studies that analysed spinal anaesthesia did not report the levels of block. In several analyses, spinal anaesthesia and epidural anaesthesia were combined as neuraxial anaesthesia, possibly hiding differences in outcome between techniques. Combining or separating these anaesthetic techniques did not change the results of the meta‐analysis.
Many outcomes have very wide confidence intervals that are almost meaningless and may obscure clinically important benefits or harms. This implies that currently available studies may be too small to generate a meaningful answer to the questions posed by this systematic review. A combined outcome of death and major complications (i.e. death, myocardial infarction, pneumonia, cerebral stroke and amputation) would serve as the basis for a potentially useful analysis; however among the included studies, the authors of randomized controlled trials did not present this outcome.
The quantitative summary estimate did not show lower rates of death and major complications in favour of neuraxial anaesthesia. The outcomes analysed included mortality, myocardial infarction, lower‐limb amputation rate and pneumonia. Evidence to date does not support a clinically meaningful benefit of neuraxial anaesthesia over general anaesthesia for lower‐limb revascularization surgery. The potential benefits of reduced postoperative pneumonia must be weighed carefully because in this review, this finding was based on the results of a single study (Cook 1986).
Summary of main results
In this updated review, we reran our search and did not find new studies. Our previous work did not show a statistically significant difference in the rate of death when spinal anaesthesia and epidural anaesthesia were compared with general anaesthesia.
Lower‐limb revascularization is performed predominantly in elderly participants, who may have multiple medical conditions. The high rate of mortality in this group of participants is often a result of other medical conditions rather than a direct consequence of the surgical procedure. The choice of anaesthetic technique may reduce mortality in elderly patients, but in this systematic review, we analysed four studies and found no statistically significant difference between intervention groups. The overview by Rodgers et al (Rodgers 2000) reported that postoperative mortality was significantly reduced (OR 0.70, 95% CI 0.54 to 0.90) with the use of neuraxial anaesthesia. This finding is inconsistent with the results described in this systematic review. Reasons for this may include the fact that we analysed participants undergoing lower‐limb revascularization whilst Rodgers et al analysed participants undergoing all types of surgery (general, orthopaedic, urological and vascular). Also, Rodgers et al included older studies than were included in this systematic review, and we included one study that had been realized in 2007. These differences may explain why Rodgers et al favoured neuraxial anaesthesia. The confidence intervals for the mortality data provided in this systematic review (OR 0.89, 95% CI 0.38 to 2.07) overlap with those of Rodgers et al.
Coronary artery disease is present in 50% to 70% of study participants undergoing vascular surgery (Venkataraman 2006). Parker et al (Parker 2011) analysed elderly participants who underwent orthopaedic surgery and found that the rate of myocardial infarction was 1% (5/502) in the neuraxial anaesthesia group, which was not significantly different from the rate after general anaesthesia. Our rate of myocardial infarction was 4% (32/696), and we noted no statistically significant difference between groups. Our sample size was small, and no individual study had numbers large enough to reveal whether differences could be attributed to sample size calculations described by the authors of the studies included in this meta‐analysis.
Three studies analysed the rate of lower‐limb amputation (Bode 1996; Christopherson 1993; Cook 1986). No statistically significant difference was noted between groups. We had expected that the amputation rate would be lower in the neuraxial anaesthesia group than in the general anaesthesia group because of vasodilatation of the lower limbs resulting from adrenergic blockade, but this result was not confirmed in this systematic review, probably because the vasodilatation was of short duration and did not occur in all participants during the postoperative period. Thromboprophylactic agents have been used during lower‐limb revascularization to reduce the risk of graft reocclusion (Smaka 2013). No individual study reported details on the use of warfarin, heparin or low molecular weight heparins for thromboprophylaxis (preventative treatment for blood clotting), nor did they report epidural haematoma (blood outside the blood vessels) as an outcome.
The outcomes of pneumonia were analysed in only two studies (Christopherson 1993; Cook 1986). A statistically significant difference between groups favoured neuraxial anaesthesia. One study (Christopherson 1993) contributed only two events and the other (Cook 1986) contributed 18 events in the general anaesthesia group. The rate of pneumonia in the general anaesthesia group as reported by Cook et al was 35%. These investigators attributed their results in part to the numbers of smokers and elderly participants included in the general anaesthesia group and in part to the use of dry inspired gases and endotracheal intubation (placement of a tube into the trachea to keep it open) (Cook 1986). Randomization serves to eliminate any influence on allocation of treatment that may be exerted by the investigator, and characteristics that can influence study results are distributed equally between groups (Altman 1991). Cook did not discuss why more elderly people and smokers were included in the general anaesthesia group of that study (Cook 1986). Use of dry inspired gases may not explain the high rate of pneumonia reported in the Cook 1986publication. Parker 2011 included studies published at the same time as the studies included in this systematic review, and these studies also used dry inspired gases. The rate of pneumonia after general anaesthesia was 4.7%, and no differences between the neuraxial and general anaesthesia groups were noted.
Overall completeness and applicability of evidence
We identified four studies that analysed rates of death and major complications. An overall view of these studies reveals no differences between neuraxial anaesthesia and general anaesthesia as used in lower‐limb revascularization, and data that could be used to combine their results were available only for mortality, myocardial infarction, lower‐limb amputation rate and pneumonia. Applicability of these study results to clinical practice may be limited because the most recent study was published in 2007, and the anaesthetic agents used in the other three studies cannot be used frequently today. Our results show that pneumonia was less common in the neuraxial anaesthesia group, but this result was based on the findings reported by a single study.
Quality of the evidence
Avoidance of selection bias depends mainly on two experimental design choices: generation of the random sequence and confidentiality of the allocation (Schulz 2002). Random allocation is one sequence generation method for assigning participants to different intervention groups in a randomized trial. Use of this method implies that each individual or unit that is entered into a trial has the same chance of receiving each of the possible interventions (Green 2005). Concealment of allocation is the process used to ensure that the person who decides to enter a participant into a randomized controlled trial does not know the comparison group into which that individual will be allocated (Green 2005). Three included studies used terms such as randomized study or random distribution to describe their processes, but these terms were not sufficient to describe how sequence generation and allocation concealment were done. Blinding protects the sequence of randomization after allocation, and correct description of this item is extremely important (Schulz 2002). Only one study reported blinding. It would be more useful if authors of future randomized controlled trials describe blinding of the participant, the person responsible for participant care, the outcome assessor, the researcher, data analysts and the personnel who write the article. Cumulative information, individual study data and quality of evidence for the most important outcomes can be seen in Table 1.
Potential biases in the review process
This meta‐analysis is based on four studies. One study (Bode 1996) recruited more than 50% of all cases. We think that this study did not influence the results of the meta‐analysis excessively for the following reasons. First, this study was not used in all analyses; second, the results of the systematic review did not show statistically significant differences with or without the results of the Bode 1996 study; third, only pneumonia showed a statistically significant difference in risk, and the study was not included in this analysis; and fourth, the results were statistically homogeneous.
Two of the four included studies are more than 10 years old and one is more than 20 years old. Some pharmacological agents used today, such as alpha blockers (pharmacological agents that act as antagonists of α‐adrenergic receptors) and opioids (substances that are like opium), were not used in the included studies. Nitrous oxide (a volatile anaesthetic agent) was used in all included studies but today is used less in patients at high cardiac risk. Anaesthetic techniques reported in the older studies included in this systematic review may not represent modern anaesthetic practice. With this point in mind, Bode 1996 used pulmonary artery catheters for all participants.
Agreements and disagreements with other studies or reviews
A similar review published in 2007 reported that the use of local anaesthetics to perform neuraxial anaesthesia compared with general anaesthesia can reduce postoperative pulmonary complications, such as pneumonia, after major vascular surgery or in high‐risk participants (Liu 2007). The authors concluded that their evidences were too limited to confirm or deny this benefit (Liu 2007). We report here a similar result.
Authors' conclusions
Implications for practice.
Evidence available from randomized trials comparing neuraxial anaesthesia with general anaesthesia for lower‐limb revascularization surgery was insufficient to confirm or rule out clinically significant differences for most clinical outcomes. Evidence suggests that neuraxial anaesthesia may reduce the occurrence of pneumonia, but no definitive conclusions regarding mortality, myocardial infarction and rate of lower‐limb amputation can be drawn.
Implications for research.
Additional randomized controlled trials are needed to answer questions on the effects of neuraxial anaesthesia compared with other types of anaesthesia on clinical outcomes in patients undergoing lower‐limb revascularization surgery. If mortality is to be reduced from 5% to 3%, with 80% statistical power using two‐tail tests and at the 5% significance level, 1504 participants would be required. Outcomes must be assessed by intention‐to‐treat analyses, and follow‐up should be continued for five years.
What's new
| Date | Event | Description |
|---|---|---|
| 10 June 2014 | Amended | Contact details updated |
History
Protocol first published: Issue 2, 2008 Review first published: Issue 1, 2010
| Date | Event | Description |
|---|---|---|
| 2 July 2013 | New search has been performed | We reran the searches until 28 April 2013. We updated the Methods section. We extended our search for ClinicalTrials.gov. |
| 2 July 2013 | New citation required but conclusions have not changed | We found no new studies that could answer our research question. |
| 10 February 2011 | New search has been performed | We previously searched the databases until June 2008. In this updated version, we reran the searches until 1st February 2011. We found no new studies which fulfilled our inclusion criteria. We have included risk of bias and summary of finding tables. |
Acknowledgements
We would like to thank John Carlisle (content editor), Nathan Pace (statistical editor), Tim Cook and Pierre Foëx (external peers) and Janet Wale (Cochrane Consumer Network) for their help and editorial advice during the preparation of this review.
We would also like to thank Dr John Carlisle (content editor), Professor Pierre Foëx, Dr ASM Hopson (peer reviewers) and Hoda Javaheri (Cochrane Consumer Network) for their help and editorial advice during the preparation of the protocol for this systematic review.
Appendices
Appendix 1. Search strategy for CENTRAL, The Cochrane Library
#1 MeSH descriptor Lower Extremity explode all trees #2 lower near Limb* #3 limb*:ti,ab #4 limb* near revasculari?at* #5 limb* and revascular* #6 (#1 OR #2 OR #3 OR #4 OR #5) #7 an?esth*:ti,ab #8 MeSH descriptor Anesthesia explode all trees #9 MeSH descriptor Anesthesia, General explode all trees #10 MeSH descriptor Anesthetics, General explode all trees #11 MeSH descriptor Anesthesia, Conduction explode all trees #12 (#7 OR #8 OR #9 OR #10) #13 (( #6 AND #11 ) OR #5)
Appendix 2. Search strategy for MEDLINE (Ovid SP)
#1 exp Lower‐Extremity/ #2 (lower adj5 Limb*).mp. #3 limb*.ti,ab. #4 (limb* adj5 revasculari?at*).mp. #5 (limb* and revascular*).mp. #6 1 or 2 or 3 or 4 or 5 #7 an?esth*.ti,ab. #8 exp Anesthesia/ #9 exp Anesthetics General/ or exp Anesthesia‐General/ #10 exp Anesthesia Conduction/ #11 7 or 8 or 9 or 10 #12 (6 and 11) or 5 #13 (randomized controlled trial.pt. or controlled clinical trial.pt.or randomized.ab. or placebo.ab. or clinical trials as topic.sh. or randomly.ab. or trial.ti.) and humans.sh. #14 12 and 13
Appendix 3. Search strategy for EMBASE (Ovid SP)
#1 exp limb/ #2 lower leg/ #3 (lower adj5 Limb*).mp. #4 limb* .ti,ab. #5 (limb* adj5 revasculari?at*).mp. #6 (limb* and revascular*).mp. #7 1 or 2 or 3 or 4 or 5 or 6 #8 an?esth* .ti,ab. #9 exp anesthesia/ or exp anesthesiainduction/ #10 exp anesthesia/ or exp anesthesiainduction/ #11 general anesthesia/ or anesthetic agent/ #12 8 or 9 or 10 or 11 #13 7 and 12 #14 RANDOMIZEDCONTROLLEDTRIAL/ or RANDOMIZATION/ or CONTROLLEDSTUDY/ or MULTICENTERSTUDY/ or PHASE3CLINICALTRIAL/ or PHASE4CLINICALTRIAL/ or DOUBLEBLINDPROCEDURE/ or SINGLEBLINDPROCEDURE/) or RANDOM* or CROSS?OVER* or FACTORIAL* or PLACEBO* or VOLUNTEER*) or SINGL* or DOUBL* or TREBL* or TRIPL*) adj3 BLIND* or MASK*))).ti,ab) and human*.ec,hw,fs. #15 13 and 14
Appendix 4. Search strategy for LILACS (via BIREME)
"revascular$" or "REVASCULARIZATION" or "REVASCULARIZATIONS" or "REVASCULARIZAUAO" or "REVASCULARIZED" or "REVASCULARIZING" or "REVASCULARIZO" or "REVASCULARIZOU" or "REVASCULARYZATION" or "REVASCULATIZACOES" or "REVASCULATIZATION" or "REVASCULIZADORA" or "REVASCULIZAR" or "REVASCULIZARLO" or "REVASCULRIZACAO" [Words] or "limb$" or "LIMB" or "LIMBALES" or "LIMBAR" or "LIMBATA" or "LIMBE" [Words] and "anaesth$" or "anesth$" or "ANESTHESIA" or "ANESTHESIA ADJUVANTS/" or "ANESTHESIA AND ANALGESIA" or "ANESTHESIA, CAUDAL/" or "ANESTHESIA, CLOSED‐CIRCUIT/" or "ANESTHESIA, CONDUCTION/" or "ANESTHESIA, ELECTRIC/" or "ANESTHESIA, EPIDURAL/AE" or "ANESTHESIA, GENERAL/" or "ANESTHESIA, INFILTRATION/" or "ANESTHESIA, INHALATION/" or "ANESTHESIA, LOCAL/" or "ANESTHESIA, RECTAL/" or "ANESTHESIA, REGIONAL/" or "ANESTHESIAS" or "ANESTHESICAL" or "ANESTHESICS" or "ANESTHESIE" or "ANESTHESIIA" or "ANESTHESTETIC" or "ANESTHESYA" or "ANESTHETIC" [Words]
Appendix 5. Search strategy for CINAHL (EBSCOhost)
S1 MW Lower Extremity S2 TX (lower and Limb*) S3 TX limb* S4 TX (limb* and revascular*) S5 S1 or S2 or S3 or S4 S6 TX an?esth* S7 MW Anesthesia or MW Anesthesia Conduction S8 MW Anesthetics General or MW Anesthesia General S9 S6 or S7 or S8 S10 S5 and S9
Appendix 6. Search strategy for ISI Web of Science
#1 TS=(lower SAME Limb*) #2 TS=(limb* SAME revascular*) #3 TS=(limb* AND revascular*) #4 TI=limb* #5 #4 OR #3 OR #2 OR #1 #6 TS=anaesth* or TS=anesth* #7 #6 AND #5
Appendix 7. Data extraction form
References to trial
Study ID: ____________________________________________Date: ___/___/______
Title: _________________________________________________________________
Authors:_______________________________________________________________
MEDLINE Journal ID: _______________________________ Language: _____________
Study eligibility
Relevant study
The anaesthetic technique was adequately allocated?
| Yes No Indeterminate |
Relevant participants
The participants were appropriated to answer the study question?
| Yes No Indeterminate |
| Participants | Diagnostic |
| |
Relevant interventions
The intervention is clearly defined?
| Yes No Indeterminate |
Which were the comparison groups?
| Intervention group | Control group |
Information about included studies
Study ID: ______________________________________________Date: ___/___/____
Title: _________________________________________________________________
MEDLINE Journal ID: _____________________________________________________
What is the category of the methods of concealment allocation?
| RevMan title | Information to collect |
| 1. Methods | 1.1) Study question: 1.2) Hypothesis: 1.3) Objective: 1.4) Randomization: 1.4.1 Generation of allocation sequence: 1.4.2 Allocation concealment: 1.5) Blinding: 1.5.1 Person responsible for participant care: 1.5.2 Participant: 1.5.3 Outcome assessor: 1.5.4 Researcher: 1.5.5 Data analysts: 1.5.6 Personnel who write the article: 1.6) Lost to follow‐up: 1.6.1 Withdrawals: 1.6.2 Dropouts: 1.7) Duration of follow‐up: 1.8) How was participant eligibility defined? 1.9) Number of participants who received intended treatment (enrolled in study): 1.10) Number of participants who were analysed: 1.11) Time points when measurements were taken during the study: 1.12) Time points reported in the study: 1.13) Time points that will be used in meta‐view: 1.14) Trial design (e.g. parallel/cross‐over): 1.15) The groups were comparable in relation to the most important prognostic characteristic? 1.16) Intention‐to‐treat analyses: 1.17) Sample size calculation: 1.18) Representativeness: 1.19) Risk of bias assessment in included studies: 1.19.1 Random sequence generation: ( ) Low risk ( ) High risk ( ) Unclear risk 1.19.2 Allocation concealment: ( ) Low risk ( ) High risk ( ) Unclear risk 1.19.3 Blinding of participants and personnel: ( ) Low risk ( ) High risk ( ) Unclear risk 1.19.4 Blinding of outcome assessment: ( ) Low risk ( ) High risk ( ) Unclear risk 1.19.5 Incomplete outcome data: ( ) Low risk ( ) High risk ( ) Unclear risk 1.19.6 Selective reporting: ( ) Low risk ( ) High risk ( ) Unclear risk 1.19.7 Other bias: ( ) Low risk ( ) High risk ( ) Unclear risk |
| 2. Participants | 2.1) Inclusion criteria: 2.2) Age: 2.3) Sex: 2.4) Number of participants: 2.5) Exclusion criteria: 2.6) Duration of the study: 2.7) Location of the study: |
| 3. Interventions | 3.1) Intervention group: 3.1.1 Anaesthetic technique: 3.1.2 Drugs used: 3.2) Control group: 3.2.1 Anaesthetic technique: 3.2.2 Drugs used: |
| 4. Outcomes | 4.1) Primary outcomes: 4.1.1 Mortality: 4.1.2 Myocardial infarction: 4.1.3 Cardiac stroke: 4.1.4 Nerve dysfunction: 4.1.5 Postoperative lower‐limb amputation rate: 4.2) Secondary outcomes: 4.2.1 Duration of hospital stay: 4.2.2 Postoperative cognitive dysfunction: 4.2.3 Postoperative wound infection: 4.2.4 Pneumonia: 4.2.5 Complications in the anaesthetic recovery room (e.g. hypertension, hypotension, cardiac dysrhythmia, nausea, vomiting, tremor, need for supplementary oxygen): 4.2.6 Participant satisfaction: 4.2.7 Postoperative pain score: 4.2.8 Transfusion requirement: 4.2.9 Urinary retention: 4.2.10 Claudication distance: 4.2.11 Rest pain: |
| 5. Notes |
References to other trials
| Did this report include any references to published reports of potentially eligible trials not already identified for this review? | ||
| First author | Journal/Conference | Year of publication |
| Did this report include any references to unpublished reports of potentially eligible trials not already identified for this review? | ||
| First author | Journal/Conference | Year of publication |
Data extraction
Study ID: ______________________________________________Date: ___/___/____
Title: _________________________________________________________________
MEDLINE Journal ID: _____________________________________________________
Continuous data
| Outcomes | Unit measurement | Intervention group | Control group | ||||
| N* | Mean | SD | N* | Mean | SD | ||
* N: number of participants.
Dichotomous data
| Outcomes | Unit measurement | Intervention group | Control group | ||
| Event | N* | Event | N* | ||
· N: number of participants.
Data and analyses
Comparison 1. Neuraxial versus general anaesthesia.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality | 4 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 In hospital | 4 | 696 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.32, 1.93] |
| 1.2 After hospital stay | 1 | 100 | Odds Ratio (M‐H, Random, 95% CI) | 2.13 [0.19, 24.25] |
| 1.3 At any time | 4 | 696 | Odds Ratio (M‐H, Random, 95% CI) | 0.89 [0.38, 2.07] |
| 2 Myocardial infarction | 4 | 696 | Odds Ratio (M‐H, Random, 95% CI) | 1.23 [0.56, 2.70] |
| 2.1 Spinal anaesthesia | 2 | 306 | Odds Ratio (M‐H, Random, 95% CI) | 1.89 [0.50, 7.21] |
| 2.2 Epidural anaesthesia | 3 | 390 | Odds Ratio (M‐H, Random, 95% CI) | 0.98 [0.37, 2.58] |
| 3 Amputation rate | 3 | 465 | Odds Ratio (M‐H, Random, 95% CI) | 0.84 [0.38, 1.84] |
| 3.1 Spinal anaesthesia | 2 | 235 | Odds Ratio (M‐H, Random, 95% CI) | 1.04 [0.35, 3.06] |
| 3.2 Epidural anaesthesia | 2 | 230 | Odds Ratio (M‐H, Random, 95% CI) | 0.66 [0.21, 2.07] |
| 4 Pneumonia | 2 | 201 | Odds Ratio (M‐H, Random, 95% CI) | 0.37 [0.15, 0.89] |
1.1. Analysis.
Comparison 1 Neuraxial versus general anaesthesia, Outcome 1 Mortality.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bode 1996.
| Methods | Randomized controlled trial. Randomization was done by computer program and results were placed in sealed envelopes. The envelopes were not opened until after eligible patients consented to participate in the study Duration: four years, from 1988 to 1991 |
|
| Participants | Number: 423 patients scheduled for elective peripheral vascular surgery Inclusion criteria: elective peripheral vascular surgery (femoral to distal artery) Exclusion criteria: patients who refused to participate and those with pre‐existing coagulopathy, operations requiring arm veins and prior lower‐back surgery |
|
| Interventions | Spinal anaesthesia was performed with hyperbaric tetracaine 1% (16 to 20 mg) with phenylephrine (3 to 5 mg) using a 22G spinal needle at L3‐L4 or L4‐L5 in the lateral decubitus position Epidural anaesthesia was performed with lidocaine 2% and was maintained with bupivacaine (0.5%) titrated to maintain a dermatome level between T8 and T10 General anaesthesia with thiopental (2 to 4 mg/kg), fentanyl (1 to 5 μg/kg), succinylcholine (1 to 1.5 mg/kg), vecuronium (0.1 mg/kg), nitrous oxide and isoflurane and enflurane |
|
| Outcomes |
Cardiac morbidity, operating room time, maximum pulmonary artery and central venous pressures and operative fluids were not assessed in the review |
|
| Notes | Location: New England Settings: operating room and general hospital Source of funding: not described This study was identified as a duplicated publication and was included in the meta‐analysis Bode 1996reported on primary, non‐surgical (primarily cardiac) endpoints during hospital stay Pierce 1997 was a post hoc analysis of 264/423 participants for whom graft patency data were available 30 days after surgery. It is was a per‐protocol analysis, not an intention‐to‐treat analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patients were randomly allocated" Comment: randomization was generated by computer program |
| Allocation concealment (selection bias) | Low risk | Comment: envelopes were used and were opened only when patients had consented to participate in the study |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: insufficient information to permit judgement. Blinding of participants and personnel probably was not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: insufficient information to permit judgement. Blinding for participants and person responsible for outcome assessment probably was not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no missing outcome data reported in Bode 1996 (for 423 participants until hospital discharge or death). Pierce 1997 reported surgical outcomes during 30 postoperative days for only 264/423 participants |
| Selective reporting (reporting bias) | High risk | Comment: amputation over 30 days was described in the Pierce 1997 publication |
| Other bias | High risk | Pierce 1997 was a post hoc analysis of the population recruited in Bode 1996. Pierce presented graft function at 30 days in 264 of the 423 participants recruited into the original study |
Christopherson 1993.
| Methods | Randomized controlled trial. Randomization was stratified within blocks of variable sizes arranged in random order. Participants were randomly assigned in the operating room immediately before surgery Duration: four years, from October 1988 to June 1991 |
|
| Participants | Number: 100 participants scheduled for elective extremity revascularization Inclusion criteria: elective lower extremity revascularization for atherosclerotic peripheral vascular disease Exclusion criteria: procedures in iliac arteries or aorta, coagulopathy, significant upper airway abnormality and electrocardiographic abnormalities that made ambulatory cardiac ischaemia monitoring unreliable |
|
| Interventions | Epidural anaesthesia was performed with bupivacaine (0.75%) at L2‐L3 or L3‐L4 lumbar space. Doses were given incrementally after test dose with 3.0 ml of the same drug General anaesthesia with thiamylal (50 mg), fentanyl (25 to 50 μg), succinylcholine (1 to 1.5 mg/kg), nitrous oxide, enflurane and pancuronium was performed |
|
| Outcomes |
Major cardiac morbidity, respiratory failure, renal failure and readmission to the intensive care unit were not assessed in the review |
|
| Notes | Location: United States of America Settings: operating room, intensive care unit and general hospital Source of funding: not described This study was identified as a duplicated publication (Christopherson 1996) and was included in the meta‐analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (from report): "blocks of variable sizes arranged in random order" Comment: randomization was described using blocks arranged in random order, but authors did not report how these blocks were chosen |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation was done immediately before the procedure but it is unclear how sequence was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (from report): "the anaesthesiologist cannot be blinded" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Comment: the participants and staff caring for the participants were not blinded, the cardiologists assessing cardiac outcomes were blinded to the group to which participants were allocated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | From report: "The overall rate [of] missing data was 1.9% in patients assigned to the general anaesthesia regimen and 3.1% in patients assigned to epidural anaesthesia and analgesia" |
| Selective reporting (reporting bias) | High risk | One outcome (hospital stay) was reported incompletely and cannot be entered into a meta‐analysis |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Cook 1986.
| Methods | Randomized controlled trial. Methods of randomization and blinding were not described Duration: not described |
|
| Participants | Number: 101 participants scheduled for lower‐limb vascular surgery. Participants were randomly assigned to receive general or spinal anaesthesia Inclusion criteria: lower‐limb vascular surgery Exclusion criteria: not described |
|
| Interventions | Spinal anaesthesia was performed with hyperbaric cinchocaine 0.5% (7 to 8 mg) with adrenaline (0.1 to 0.2 ml) 1:1000 using a 22G spinal needle in the mid‐lumbar region and in the lateral position General anaesthesia with thiopental, fentanyl (1.5 to 2.0 ug/kg), pancuronium or alcuronium, nitrous oxide and halothane was performed |
|
| Outcomes |
Blood loss was not assessed in the review. |
|
| Notes | Location: United States of America Settings: operating room and general hospital Source of funding: not described We contacted the author to clarify the methods of randomization and concealment allocation but did not receive an answer |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no information provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: The method of concealment was not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: insufficient information to permit the judgement. Blinding for participants and personnel probably was not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: insufficient information to permit the judgement. Blinding for outcome assessor probably was not done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | One year: 11/50 missing from intervention group; 4/51 missing from control group. Participants were lost during the follow‐up time |
| Selective reporting (reporting bias) | Low risk | The outcome data were reported adequately |
| Other bias | High risk | The authors reported that more elderly people and smokers were included in the general anaesthesia group |
Dodds 2007.
| Methods | Randomized non‐blinded clinical trial. Methods of randomization and blinding were not described Duration: not described |
|
| Participants | Number: 77 participants scheduled for femoral‐popliteal or femoral‐distal revascularization surgery, older than 49 years of age. Participants were randomly assigned to receive epidural or general anaesthesia. However, 5 participants had a second operation on the other leg, for which they received the type of anaesthetic that they had not had received for the first operation (a total of 82 operations). The authors report the number of outcomes for 82 operations, not for 77 participants. This had led to some 'unit of analysis' problems Inclusion criteria: patients scheduled for femoral‐popliteal or femoral‐distal revascularization procedure and 50 years of age or older Exclusion criteria: patients who had previously had a vascular surgical procedure on the same leg and those with pre‐existing neurological deficit, infection at catheter insertion site and coagulopathy. |
|
| Interventions | Epidural anaesthesia was performed with lidocaine 1.5% with adrenaline 1:200 000 to establish an upper sensory level at approximately the sixth thoracic dermatome. Supplemental doses were used in the epidural catheter during surgery General anaesthesia with benzodiazepine as premedication, fentanyl (2 to 5 µg/kg), nitrous oxide and inhalational agent |
|
| Outcomes |
Length of surgery, blood loss and graft failure were not assessed in the review |
|
| Notes | Location: United States of America Settings: operating room and general hospital Source of funding: not described It is unclear from the study how long the 5 participants who received general anaesthesia for one operation and neuraxial anaesthesia for another operation were followed up We contacted the author to clarify the methods of randomization and concealment allocation and to ask for additional information about other outcomes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no information provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: The method of concealment was not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (from report): "using a prospective, randomized, non‐blinded clinical trial design" Comment: No blinding was used |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (from report): "using a prospective, randomized, non‐blinded clinical trial design" Comment: No blinding was used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | This study addressed two outcomes of interest for this review: mortality and myocardial infarction. No missing outcome data |
| Selective reporting (reporting bias) | High risk | Mortality was not reported during one year of follow‐up |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ballotta 2003 | Intervention not relevant. The authors randomly assigned participants to surgery technique |
| Ballotta 2004 | Intervention not relevant. The authors randomly assigned participants to surgery technique |
| Barkmeier 1997 | Non‐randomized study. The authors used only one anaesthetic technique |
| Breslow 1993 | Outcomes not relevant. The catecholamine levels were measured |
| Casati 1999 | Patients did not meet our inclusion criteria. The patients were ASA I‐II for elective orthopaedic surgery |
| Gallinger 1997 | Non‐randomized study. The authors used only combined spinal‐epidural anaesthesia |
| González‐Fajardo 1995 | Non‐randomized study. The authors divided participants according to surgery technique |
| Hertzer 1981 | Non‐randomized study. The authors reported a series of 273 consecutive participants |
| Lurquin 1993 | Non‐randomized study |
| Peduto 2003 | Intervention not relevant. The authors used only epidural anaesthesia |
| Reuben 1994 | Intervention not relevant. The study started after the conclusion of the surgery |
| Rivers 1991 | Non‐randomized study |
| Romano 1980 | Non‐randomized study. The metabolic basis was measured |
| Sabaté 1994 | Non‐randomized study. The authors divided participants according to duration of surgery |
| Singh 2006 | Non‐randomized study. This study was an analysis of a prospectively collected database |
| Vascular Society 1995 | Intervention not relevant. The surgeons were randomly assigned |
ASA: American Society of Anesthesiology.
Differences between protocol and review
We planned to analyse studies that compared neuraxial anaesthesia with all other types of anaesthesia, but all of the studies included in this review compared neuraxial anaesthesia with general anaesthesia for lower‐limb revascularization surgery.
We planned, at the protocol stage, to extract data for nerve dysfunction, postoperative wound infection, patient satisfaction, postoperative pain score, urinary retention, claudication distance and pain at rest, but the trial authors of the included studies did not analyse these outcomes.
In the primary version of the protocol, we grade trial quality as A: low risk of bias or B: intermediate risk of bias, but instead of judging study quality in this way, we included the risk of bias table. This table has domains that can identify more precisely more types of bias. This table addresses six specific domains: sequence generation; allocation concealment; blinding of participants, personnel, and outcome assessors; incomplete outcome data; selective outcome reporting; and other sources of bias.
In our last updated review, we included the summary of findings table. This table can summarize the quality of the evidence.
We extended our search to include ClinicalTrials.gov. We looked for studies that could be considered in our inclusion criteria.
Contributions of authors
Conceiving the review: Fabiano Timbó Barbosa (FTB) Co‐ordinating the review: FTB Undertaking manual searches: FTB, Mário J Jucá (MJJ) Screening search results: FTB, MJJ Organizing retrieval of papers: FTB, MJJ Screening retrieved papers against inclusion criteria: FTB, MJJ Appraising quality of papers: FTB, MJJ Abstracting data from papers: FTB, MJJ Writing to authors of papers for additional information: FTB Providing additional data about papers: FTB, MJJ Obtaining and screening data from unpublished studies: FTB, MJJ Providing data management for the review: FTB Entering data into Review Manager (RevMan 5.1): FTB Managing RevMan statistical data: FTB Performing other statistical analyses without using RevMan: Jairo C Cavalcante (JCC) Performing double entry of data: (data entered by person one: FTB; data entered by person two: MJJ) Interpreting data: FTB, MJJ, Aldemar A Castro (AAC) Making statistical inferences: JCC Writing the review: FTB Securing funding for the review: FTB Performing previous work that served as the foundation of the present study: FTB Serving as guarantor for the review (one author): FTB Taking responsibility for reading and checking the review before submission: FTB
Sources of support
Internal sources
Federal University of Alagoas, Brazil.
External sources
No sources of support supplied
Declarations of interest
Fabiano T Barbosa: none known.
Mário J Jucá: none known.
Aldemar A Castro: none known.
Jairo C Cavalcante: none known.
Edited (no change to conclusions)
References
References to studies included in this review
Bode 1996 {published data only}
- Bode Jr RH, Lewis KP, Zarich SW, Pierce ET, Roberts M, Kowalchuk GJ, et al. Cardiac outcome after peripheral vascular surgery: comparison of general and regional anaesthesia. Anesthesiology 1996;84(1):3‐13. [PUBMED: 8572352] [DOI] [PubMed] [Google Scholar]
- Pierce ET, Pomposelli Jr FB, Stanley GD, Lewis KP, Cass JL, LoGerfo FW, et al. Anesthesia type does not influence early graft patency or limb salvage rates of lower extremity arterial bypass. Journal of Vascular Surgery 1997;25(2):226‐32. [PUBMED: 9052557] [DOI] [PubMed] [Google Scholar]
Christopherson 1993 {published data only}
- Christopherson R, Beattie C, Frank SM, Norris EJ, Meinert CL, Gottlieb SO, et al. Perioperative morbidity in patients randomized to epidural or general anaesthesia for lower extremity vascular surgery. Anesthesiology 1993;79(3):422‐34. [PUBMED: 8363066] [DOI] [PubMed] [Google Scholar]
- Christopherson R, Glavan NJ, Norris EJ, Beattie C, Rock P, Frank SM, et al. Control of blood pressure and heart rate in patients randomized to epidural or general anaesthesia for lower extremity vascular surgery. Journal of Clinical Anesthesia 1996;8(7):578‐84. [PUBMED: 8910181] [DOI] [PubMed] [Google Scholar]
Cook 1986 {published data only}
- Cook PT, Davies MJ, Cronin KD, Moran P. A prospective randomised trial comparing spinal anaesthesia using hyperbaric cinchocaine with general anaesthesia for lower limb vascular surgery. Anaesthesia and Intensive Care 1986;14(4):373‐80. [PUBMED: 3551674] [DOI] [PubMed] [Google Scholar]
Dodds 2007 {published data only}
- Dodds TM, Fillinger MP, Walsh DB, Surgenor SD, Mandel D, Yeager MP. Clinical outcomes after lower extremity revascularization: a comparison of epidural and general anaesthesia. The Journal of Applied Research 2007;7(3):238‐49. [NLM UID: 101132979] [Google Scholar]
References to studies excluded from this review
Ballotta 2003 {published data only}
- Ballotta E, Renon L, Tofano M, Giau G. Prospective randomized study on bilateral above‐knee femoropopliteal revascularization: polytetrafluoroethylene graft versus reversed saphenous vein. Journal of Vascular Surgery 2003;38(5):1051‐5. [PUBMED: 14603216] [DOI] [PubMed] [Google Scholar]
Ballotta 2004 {published data only}
- Ballota E, Renon L, Rossi A, Barbon B, Terranova O, Giau G. Prospective randomized study on reversed saphenous vein infrapopliteal bypass to treat limb‐threatening ischemia: common femoral artery versus superficial femoral or popliteal and tibial arteries as inflow. Journal of Vascular Surgery 2004;40(4):732‐40. [PUBMED: 15472602] [DOI] [PubMed] [Google Scholar]
Barkmeier 1997 {published data only}
- Barkmeier LD, Hood DB, Sumner DS, Mansour MA, Hodgson KJ, Mattos MA, et al. Local anaesthesia for infrainguinal arterial reconstruction. The American Journal of Surgery 1997;174(2):202‐4. [PUBMED: 9293845] [DOI] [PubMed] [Google Scholar]
Breslow 1993 {published data only}
- Breslow MJ, Parker SD, Frank SM, Norris EJ, Yates H, Raff H, et al. Determinants of catecholamine and cortisol responses to lower extremity revascularization. Anesthesiology 1993;79(6):1202‐9. [PUBMED: 8267195] [DOI] [PubMed] [Google Scholar]
Casati 1999 {published data only}
- Casati A, Fanelli G, Aldegheri G, Colnaghi E, Casaletti E, Cedrati V, et al. Frequency of hypotension during conventional or asymmetric hyperbaric spinal block. Regional Anesthesia and Pain Medicine 1999;24(3):214‐9. [PUBMED: 10338170] [DOI] [PubMed] [Google Scholar]
Gallinger 1997 {published data only}
- Gallinger Elu, Seleznev MN, Babalyan GV. Use of combined lidocaine and bupivacaine spinal‐epidural anaesthesia in peripheral vascular surgery of the lower limbs. Anesteziologiia I Reanimatologiia 1997;5(2):60‐2. [PUBMED: 9432896] [PubMed] [Google Scholar]
González‐Fajardo 1995 {published data only}
- González‐Fajardo JA, Pérez‐Burkhardt JL, Mateo AM. Intraoperative fibrinolytic therapy for salvage of limbs with acute arterial ischaemia: an adjunct to thromboembolectomy. Annals of Vascular Surgery 1995;9(2):179‐86. [PUBMED: 7786704] [DOI] [PubMed] [Google Scholar]
Hertzer 1981 {published data only}
- Hertzer NR. Fatal myocardial infarction following lower extremity revascularization: two hundred seventy‐three patients followed six to eleven postoperative years. Annals of Surgery 1981;193(4):492‐8. [PUBMED: 7212811] [PMC free article] [PubMed] [Google Scholar]
Lurquin 1993 {published data only}
- Lurquin P, Mendes da Costa PR. Surgical pathology of aorta and arteries of the lower limbs in the elderly. Acta Chirurgica Belgica 1993;93(3):131‐4. [PUBMED: 8372587] [PubMed] [Google Scholar]
Peduto 2003 {published data only}
- Peduto VA, Baroncini S, Montanini S, Proietti R, Rosignoli L, Tufano R, et al. A prospective, randomized, double‐blind comparison of epidural levobupivacaine 0.5% with epidural ropivacaine 0.75% for lower limb procedures. European Journal of Anesthesiology 2003;20(12):979‐83. [PUBMED: 14690101] [DOI] [PubMed] [Google Scholar]
Reuben 1994 {published data only}
- Reuben SS, Dunn SM, Duprat KM, O´Sullivan P. An intrathecal fentanyl dose‐response study in lower extremity revascularization procedures. Anesthesiology 1994;81(6):1371‐5. [PUBMED: 7992905] [DOI] [PubMed] [Google Scholar]
Rivers 1991 {published data only}
- Rivers SP, Scher LA, Sheehan E, Veith FJ. Epidural versus general anesthesia for infrainguinal arterial reconstruction. Journal of Vascular Surgery 1991;14(6):764‐8. [PUBMED: 1960806] [DOI] [PubMed] [Google Scholar]
Romano 1980 {published data only}
- Romano E, Gullo A, Alagni G, Mocavero G. Anesthesia problems in reconstructive vascular surgery problems in reconstructive vascular surgery of the lower extremities [Problemi di anestesia nella chiruria vascolare ricostruttiva degli arti inferiori]. Minerva Cardioangiologica 1980;28(7‐8):525‐38. [PUBMED: 7453972] [PubMed] [Google Scholar]
Sabaté 1994 {published data only}
- Sabaté A, Asbert R, Gracia T, Camprubi I, Sopena R, Udina E. Regional anaesthesia and elderly patients: continuous subarachnoid anaesthesia versus single dose in peripheral vascular surgery. Regional Anesthesia 1994;19(2):79‐84. [Google Scholar]
Singh 2006 {published data only}
- Singh N, Sidawy AN, Dezee K, Neville RF, Weiswasser J, Arora S, et al. The effects of the type of anaesthesia on outcomes of lower extremity infrainguinal bypass. Journal of Vascular Surgery 2006;44(5):964‐8. [PUBMED: 17000075] [DOI] [PubMed] [Google Scholar]
Vascular Society 1995 {published data only}
- No authors listed. Critical limb ischaemia: management and outcome. Report of a national survey. The Vascular Surgical Society of Great Britain and Ireland. European Journal Vascular Endovascular Surgery 1995;10(1):108‐3. [PUBMED: 7633958] [DOI] [PubMed] [Google Scholar]
Additional references
Afolabi 2007
- Afolabi BB, Lesi FEA, Merah NA. Regional versus general anaesthesia for caesarean section. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI: 10.1002/14651858.CD004350.pub2] [DOI] [PubMed] [Google Scholar]
Altman 1991
- Altman DG. Randomisation. BMJ 1991;302(22):1481‐2. [PUBMED: 1855013] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bode 1994
- Bode Jr RH, Lewis KP. Con: regional anaesthesia is not better than general anaesthesia for lower extremity revascularization. Journal of Cardiothoracic and Vascular Anesthesia 1994;8(1):118‐21. [PUBMED: 8167271] [DOI] [PubMed] [Google Scholar]
Bonnet 2005
- Bonnet F, Marret E. Influence of anaesthetic and analgesic techniques on outcome after surgery. British Journal of Anaesthesia 2005;95:52‐8. [PUBMED: 15579487] [DOI] [PubMed] [Google Scholar]
Borgeat 2003
- Borgeat A, Ekatodramis G. Orthopaedic surgery in the elderly. Best Practice & Research. Clinical Anaesthesiology 2003;17(2):235‐44. [PUBMED: 12817917] [DOI] [PubMed] [Google Scholar]
Castro 1999
- Castro AA, Clark OA, Atallah AN. Optimal search strategy for clinical trials in the Latin American and Caribbean Health Science Literature database (LILACS database: update). Sao Paulo Medical Journal 1999;117(3):138‐9. [PUBMED: 10511734] [DOI] [PubMed] [Google Scholar]
Christopherson 1996
- Christopherson R, Glavan NJ, Norris EJ, Beattie C, Rock P, Frank SM, et al. Control of blood pressure and heart rate in patients randomized to epidural or general anaesthesia for lower extremity vascular surgery. Journal of Clinical Anesthesia 1996;8(7):578‐84. [PUBMED: 8910181] [DOI] [PubMed] [Google Scholar]
Dickersin 1994
- Dickersin K, Scherer R, Lefebvre C. Identifying relevant studies for systematic reviews. BMJ 1994;309(6964):1286‐91. [PUBMED: 7718048] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fukuse 2005
- Fukuse T, Satoda N, Hijiya K, Fujinaga T. Importance of a comprehensive geriatric assessment in prediction of complications following thoracic surgery in elderly patients. Chest 2005;127(3):886‐91. [PUBMED: 15764772] [DOI] [PubMed] [Google Scholar]
Green 2005
- Green S, Higgins J, editors. Glossary. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]. The Cochrane Collaboration, August 1, 2009. http://www.cochrane.org/resources/handbook/.
Higgins 2002
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;15(21):1539‐58. [PUBMED: 12111919] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Howard‐Alpe 2006
- Howard‐Alpe GM, Sear JW, Foex P. Methods of detecting atherosclerosis in non‐cardiac surgical patients: the role of biochemical markers. British Journal of Anaesthesia 2006;97(6):758‐69. [PUBMED: 17074779] [DOI] [PubMed] [Google Scholar]
Lefebvre 1996
- Lefebvre C, McDonald S. Development of a sensitive search strategy for reports of randomized controlled trials in EMBASE. Fourth International Cochrane Colloquium, October 20‐24, 1996, Adelaide, Australia. 1996.
Liu 2007
- Liu SS, Wu CL. Effect of postoperative analgesia on major postoperative complications: a systematic update of the evidence. Anesthesia Analgesia 2007;104(3):689‐02. [PUBMED: 17312231] [DOI] [PubMed] [Google Scholar]
Manojlović 2013
- Manojlović V, Popović V, Nikolić D, Milosević D, Pasternak J, Kaćanski M. Analysis of associated diseases in patients with acute critical lower limb ischemia. Medicinski Pregled 2013;66(1‐2):41‐5. [PUBMED: 23534299] [DOI] [PubMed] [Google Scholar]
Parker 2011
- Parker MJ, Handoll HHG, Griffiths R. Anaesthesia for hip fracture surgery in adults. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD000521.pub2] [DOI] [PubMed] [Google Scholar]
Pierce 1997
- Pierce ET, Pomposelli Jr FB, Stanley GD, Lewis KP, Cass JL, LoGerfo FW, et al. Anesthesia type does not influence early graft patency or limb salvage rates of lower extremity arterial bypass. Journal of Vascular Surgery 1997;25(2):226‐32. [PUBMED: 9052557] [DOI] [PubMed] [Google Scholar]
Rasmussen 2000
- Rasmussen LS, Moller JT. Central nervous system dysfunction after anaesthesia in the geriatric patient. Anesthesiology Clinics of North America 2000;18(1):59‐70. [PUBMED: 10935000] [DOI] [PubMed] [Google Scholar]
RevMan 5.1 [Computer program]
- Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. RevMan 5.1 (Review Manager) (RevMan) [Computer program]. Version 5.1.. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Rodgers 2000
- Rodgers A, Walker N, Schug S, McKee A, Kehlet H, Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. British Medical Journal 2000;321:1493‐7. [PUBMED: 11118174] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schulz 2002
- Schulz KF, Chalmers I, Altman DG. The landscape and lexicon of blinding in randomized trials. Annals of Internal Medicine 2002;136(5):254‐9. [PUBMED: 11827510] [DOI] [PubMed] [Google Scholar]
Sim 2005
- Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Physical Therapy 2005;85(3):257‐68. [PUBMED: 15733050] [PubMed] [Google Scholar]
Smaka 2013
- Smaka TJ, Miller TE, Hutchens MP, Schenning K, Fleisher LA, Gan TJ, et al. Anesthesia for vascular surgery. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega R editor(s). Clinical Anesthesia. 7th Edition. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins, 2013:1112‐43. [Google Scholar]
Tonner 2003
- Tonner PH, Kampen J, Scholz J. Pathophysiological changes in the elderly. Best Practice & Research. Clinical Anaesthesiology 2003;17(2):163‐77. [PUBMED: 12817912] [DOI] [PubMed] [Google Scholar]
Tuman 1994
- Tuman KJ, Ivankovich AD. Pro: regional anaesthesia is better than general anaesthesia for lower extremity revascularization. Journal of Cardiothoracic and Vascular Anesthesia 1994;8(1):114‐7. [PUBMED: 8167270] [DOI] [PubMed] [Google Scholar]
Venkataraman 2006
- Venkataraman R. Vascular surgery critical care: perioperative cardiac optimization to improve survival. Critical Care Medicine 2006;34 Suppl(9):200‐7. [PUBMED: 16917424] [DOI] [PubMed] [Google Scholar]
Zaugg 2000
- Zaugg M, Lucchinetti E. Respiratory function in the elderly. Anesthesiology Clinics of North America 2000;18(1):47‐57. [PUBMED: 10934999] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Barbosa 2010
- Barbosa FT, Jucá MJ, Castro AA, Cavalcante JC. Neuraxial anaesthesia for lower‐limb revascularization. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD007083.pub2] [DOI] [PubMed] [Google Scholar]


