Abstract
Background
Internally displaced people (IDPs), uprooted by conflict, violence, or disaster, struggle with the trauma of violence, loss, and displacement, making them significantly more vulnerable to post-traumatic stress disorder (PTSD). Therefore, we conducted a systematic review and meta-analysis to assess the prevalence and associated factors of PTSD among IDPs in Africa.
Methods
A comprehensive search of electronic databases was conducted to identify relevant studies published between 2008 and 2023. The search included electronic databases such as PubMed, CABI, EMBASE, SCOPUS, CINHAL, and AJOL, as well as other search sources. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. Data were extracted using Microsoft Excel, and analysis was performed using STATA 17 software. The quality of the included studies was assessed using the JBI quality appraisal tool. A random-effects model was used to estimate the pooled prevalence of PTSD and its associated factors. The funnel plot and Egger’s regression test were used to assess publication bias, and I2 test statistics was used to assess heterogeneity. The protocol for this review has been registered with PROSPERO (ID: CRD42023428027).
Results
A total of 14 studies with a total of 7,590 participants met the inclusion criteria. The pooled prevalence of PTSD among IDPs in Africa was 51% (95% CI: 38.-64). Female gender (OR = 1.99, 95% CI: 1.65–2.32), no longer married (OR = 1.93, 95% CI: 1.43–2.43), unemployment (OR = 1.92, 95% CI: 1.17–2.67), being injured (OR = 1.94, 95% CI: 1.50–1.50), number of traumatic events experienced [4-7(OR = 2.09, 95% CI: 1.16–3.01), 8–11 (OR = 2.09, 95% CI: 2.18–4.12), 12–16 (OR = 5.37, 95% CI: 2.61–8.12)], illness without medical care (OR = 1.92, 95% CI: 1.41–2.29), being depressed (OR = 2.97, 95% CI: 2.07–3.86), and frequency of displacement more than once (OR = 2.13, 95% CI: 1.41–2.85) were significantly associated with an increased risk of PTSD.
Conclusions
The findings of this systematic review and meta-analysis highlight the alarming prevalence of PTSD among IDPs in Africa. Female gender, marital status, number of traumatic events, ill health without medical care, depression, and frequency of displacement were identified as significant risk factors for PTSD. Effective interventions and the development of tailored mental health programs are needed to prevent PTSD among IDPs, focusing on the identified risk factors.
Introduction
Internally displaced persons (IDPs) are individuals forced to flee their homes due to conflict, natural disasters, or other man-made or natural events [1]. These individuals face numerous challenges, including physical and psychological trauma, witnessing violence, loss of livelihoods, and separation from family and friends [2,3]. These challenges can contribute to the development of post-traumatic stress disorder (PTSD), a common mental health condition characterized by flashbacks, nightmares, hypervigilance, avoidance, and emotional numbness [4–6].
PTSD can have a profound and debilitating impact on the lives of IDPs, posing significant challenges to their recovery and reintegration into society [3]. The impact of PTSD on IDPs extends beyond the individual, affecting their families and communities as well. The emotional turmoil and behavioral changes associated with PTSD can strain relationships within families, leading to conflict, neglect, and further emotional distress [1,7]. PTSD can also lead to secondary problems such as substance abuse, self-harm, and suicide [8,9]. Moreover, the inability of IDPs with PTSD to contribute fully to their communities can hinder collective recovery efforts and exacerbate existing social and economic vulnerabilities [1,7,10]. The impact could have been highly significant in Africa because of several factors, including insufficient mental health services, the stigma associated with mental health problems, and the logistical challenges of providing mental health services to IDPs who are often living in remote areas [11–13].
Globally, more than 71 million people are internally displaced as of the end of 2022 across 120 countries because of conflict, violence, and disasters. This number shows an increase of 20% from the previous year [14]. Human and natural disasters that could potentially cause IDPs have been prominently reported in sub-Saharan Africa [15]. In 2020, Africa accounted for almost 40% of all new internal displacements globally, with natural disasters being the primary cause of displacement in 32 out of 54 African countries [16]. According to the United Nations Human Rights Commission (UNHCR), 42% of all IDP people globally have lived in Africa [17].
The prevalence of PTSD among IDPs varies widely, ranging from 3% to 88% depending on the specific country and population studied [18,19]. The prevalence of PTSD in East Africa ranges from 11% to 80.2% [20–22]. Similarly, a meta-analysis study conducted in sub-Saharan African countries reveals that the magnitude of PTSD ranges from 12.3% in Central Sudan to 85.5% in Nigeria, and the majority of them reported to have more than 50% of the magnitude of PTSD [23]. This suggests that PTSD is a significant public health problem among IDPs in Africa.
Several factors have been identified as being associated with an increased risk of PTSD among IDPs. These factors include: female gender, young age, trauma, experiencing or witnessing violence, depression, anxiety, stress, low level of educational status, lack of social support, and economic hardship [20,23,24]. Beyond the previously mentioned factors, a number of other factors may also increase the likelihood of PTSD in IDPs in Africa. These factors include political instability and ongoing conflict, which can prolong the trauma and displacement cycle and make it more challenging for IDPs to find stability and security. This ongoing exposure to stress and uncertainty can exacerbate PTSD symptoms and hinder recovery efforts. Poverty and food insecurity are also common among IDPs in Africa, creating additional stressors and challenges. These socio-economic factors can contribute to feelings of hopelessness, despair, and a sense of being trapped in a difficult situation, further exacerbating PTSD among these vulnerable groups [25–28].
Despite the high prevalence of PTSD among IDPs in different African countries, there is a lack of comprehensive studies that show the pooled impact of PTSD and the nature of risk factors. Thus, a comprehensive study that can address the overall public health impact of internal displacement in terms of causing PTSD could be important to provide mental health services for IDPs. Therefore, the purpose of this systematic review and meta-analysis is to synthesize existing evidence on the prevalence of PTSD and its associated factors among IDPs in Africa. This information will be used to inform the development of interventions to prevent and treat PTSD among IDPs in Africa.
Methods and materials
Study setting
The study provides a comprehensive synthesis of existing research on PTSD prevalence rates and examines risk factors contributing to the development of PTSD among IDPs in African countries. According to the African Development Bank, there are 54 countries in Africa today [29].
Protocol and registration
The protocol for this review was registered in the International Prospective Register of Systematic Reviews (PROSPERO), the University of York Centre for Reviews and Dissemination (Record ID: CRD42023428027, May 31st, 2023).
Data sources and search strategy
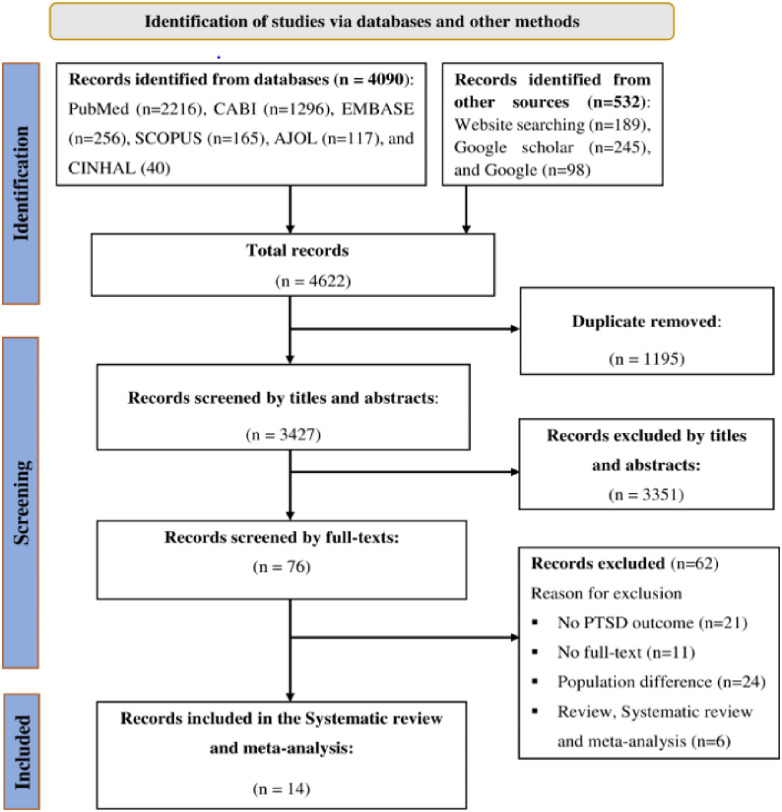
This review and meta-analysis were conducted according to the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The three phases drawn from the PRISMA flowchart were documented in the results to show the study selection process from identification to the included studies [30]. The PRISMA checklist was also used in the reporting of the systematic review and meta-analysis (S1 File).
We extensively searched articles on PubMed/MEDLINE, CABI, EMBASE, SCOPUS, CINHAL, and African Journal Online (AJOL) up to June 11, 2023. According to the African Development Bank, there are 54 countries in Africa [29]. The search terms were selected to capture relevant articles on PTSD and IDPs in African countries. The search was conducted using a combination of keywords and controlled vocabulary (MeSH terms). The search strategy was adapted for each database as per their specific syntax and indexing terms. For the PubMed search, the following key terms were used in combination with the Boolean operators "AND" and "OR". ("Post-traumatic stress disorder" [All Fields] OR "Posttraumatic stress disorder" [All Fields] OR "PTSD" [All Fields]) AND ("Internally displaced persons" [All Fields] OR "Internally displaced people"[All Fields] OR "Internally displaced individuals" [All Fields] OR "IDP" [All Fields]) AND ("Associated factors" [All Fields] OR "Determinant factors" [All Fields] OR "Risk factors" [All Fields]) AND "Africa" [All Fields].
In addition to these electronic database searches, we searched the grey literature using website searches such as BioMed Central and National Institute of Mental Health, Behavioral and Brain Sciences—Cambridge University Press, etc., Google Search, and Google Scholar. We also searched the reference lists (bibliographies) of the included studies for additional relevant studies.
Eligibility criteria
Inclusion criteria
Articles that met the following criteria were considered for inclusion in this systematic review and meta-analysis.
Population: internally displaced persons (IDPs).
Outcomes: articles reported the quantitative outcome of the prevalence of PTSD and associated factors among IDPs in Africa.
Study design: a cross-sectional study.
Study setting: studies conducted in African countries.
Publication issue: peer-reviewed journal articles published before 11 June 2023.
Exclusion criteria
Systematic reviews, qualitative studies, letters to editors, short communications, and commentaries were excluded. In addition, articles that were not fully accessible after three personal email contacts with the corresponding author and articles that did not indicate the outcome interest of this study were all excluded.
Study selection process
The Endnote X9.2 (Thomson Reuters, Philadelphia, PA, USA) software reference manager was used to collect and organize search results and to remove duplicate articles. Three investigators (AHT, FMA, and GA) independently screened articles by their title, abstract, and full text to identify eligible articles using predetermined inclusion and exclusion criteria. The screened articles were then compiled together by three investigators (AHT, GSA, and AKS), and the disagreement between authors that arises during data abstraction and selection is solved based on evidence-based discussion and the involvement of other investigators (AKS, GTE, and AAA).
Data extraction and management
Data were extracted using the Joanna Briggs Institute (JBI) data extraction checklist. Four review authors (AHT, FMA, GGK, and BD) extracted the data independently using a Microsoft Excel spreadsheet. The data extraction format included (name of first author, publication year, study country, study design, sample size, response rate, prevalence of PTSD, total number of participants, factors associated with PTSD with their respective OR with 95% CI, and risk of bias). Disagreements between the review authors were resolved by a review by the other review authors based on an evidence-based discussion.
Quality assessment of the studies
The quality of the included articles was assessed using the Joanna Briggs Institute (JBI) quality appraisal tools for analytical cross-sectional studies [31]. Three investigators (AHT, AKS, and GA) independently assessed the quality of the included articles. The assessment tool contains eight criteria: (1) clear inclusion and exclusion criteria; (2) description of the study subject and study setting; (3) use of a valid and reliable method to measure the exposure; (4) standard criteria used for measurement of the condition; (5) identification of confounding factors; (6) development of strategies to deal with confounding factors; (7) use of a valid and reliable method to measure the outcomes; and (8) use of appropriate statistical analysis. The risks for biases were classified as low (total score, 6 to 8), moderate (total score, 3 or 5), or high (total score, 0 to 2) (S2 File). Finally, articles with low and moderate biases were considered in this review. Disagreements that arose during the full-text quality assessment were resolved through evidence-based discussion with the involvement of other review authors (GGK, GA, and BD).
Outcome of interest
The primary outcome of this review was the pooled prevalence of post-traumatic stress disorder (PTSD). It was reported as a percentage (%). The second outcome of this review was the pooled measure of the association between PTSD and associated factors among IDPs in Africa. It was determined using the pooled odds ratio (OR) with a 95% confidence interval.
Statistical methods and data analysis
The extracted data were exported from a Microsoft Excel spreadsheet to STATA version 17 for further analysis. Heterogeneity among the included studies was quantitatively measured by the index of heterogeneity (I2 statistics), in which 25%-51%, 50%-75%, and>75% represented low, moderate, and high heterogeneity, respectively [32]. The overall pooled estimate of PTSD among IDPs in Africa was computed using the metaprop STATA command. A subgroup analysis was conducted by a study country to see the difference in the pooled prevalence of PTSD between countries. The influence of a single study on the overall pooled estimate was assessed using a sensitivity analysis. Furthermore, the small-study effect was evaluated using the funnel plot test and Egger’s regression test, with a p-value <0.05 as a cutoff point to declare the presence of publication bias. A p-value <0.05 was used to declare factors associated with PTSD to be statistically significant with a pooled odds ratio (OR) at the 95% confidence level. The results were presented using graphs, tables, text, and a forest plot.
Results
Searching process
A total of 4622 articles were identified using electronic databases and manual searching. After removing duplicate records, 3427 records were screened for this review. Based on their titles and abstracts, 3351 articles were excluded. In addition, 62 articles were excluded based on the exclusion criteria. Finally, a total of 14 articles were included in this review. The PRISMA flow diagram was used to summarize the selection process (Fig 1).
Fig 1. PRISMA flow diagram for the systematic review and meta-analysis of PTSD and associated factors among IDPs in Africa.
Characteristics of the included studies
In this review, the publication year, country of study, study design, sample size, and prevalence of PTSD are summarized in Table 1. By design, all included studies were cross-sectional. This study included a total of 7,590 participants [2,10,20,21,24,26,33–40]. The included articles were published between 2008–2023. The included study sample sizes ranged from 93 to 1291. In this review, a study conducted in Sudan, South Darfur, at the Darfur Campaign study site, showed the lowest prevalence of PTSD (14.9%) [35], while a study conducted in IDP camps in Yobe State in northeastern Nigeria showed the highest prevalence of PTSD (94.2%) [2]. Three studies were from Ethiopia [20,26,33]; five studies were from Nigeria [2,24,38–40] and the remaining studies were from Kenya [34], Somalia [10], Sudan [35], South Sudan [36], Uganda [21] and the Democratic Republic of Congo (DRC) [37]. The included studies were categorized as having a low risk of bias (quality score 6 to 8). The description of the included studies is presented in Table 1.
Table 1. A description summary of the included articles for the systematic review and meta-analysis on the prevalence and associated factors of PTSD among IDPs in Africa, 2023.
| Author | Publication year | Country | Study design | Sample size | Response rate | Prevalence (%) | Quality status |
|---|---|---|---|---|---|---|---|
| Asnakew et al [33] | 2019 | Ethiopia | CS | 846 | 98.1 | 37.3 | Low risk |
| Madoro et al [20] | 2020 | Ethiopia | CS | 636 | 98.3 | 58.4 | Low risk |
| Makango et al [26] | 2023 | Ethiopia | CS | 410 | 99.0 | 67.5 | Low risk |
| Masau et al [34] | 2018 | Kenya | CS | 139 | 100.0 | 61.2 | Low risk |
| Ali et al [10] | 2023 | Somalia | CS | 422 | 95.0 | 32.2 | Low risk |
| Elhabiby et al [35] | 2014 | Sudan | CS | 90 | 82.2 | 14.9 | Low risk |
| Roberts et al [36] | 2009 | South Sudan | CS | 1291 | 96.2 | 36.2 | Low risk |
| Roberts et al [21] | 2008 | Uganda | CS | 1280 | 94.5 | 54.3 | Low risk |
| Veling et al [37] | 2013 | DRC | CS | 93 | 100.0 | 40 | Low risk |
| Sheikh et al [24] | 2014 | Nigeria | CS | 228 | 100.0 | 42.2 | Low risk |
| Aluh et al [38] | 2019 | Nigeria | CS | 1200 | 100.0 | 78 | Low risk |
| Ibrahim et al [2] | 2023 | Nigeria | CS | 450 | 100.0 | 94.2 | Low risk |
| Faronbi et al [39] | 2021 | Nigeria | CS | 240 | 100.0 | 56.7 | Low risk |
| Nwoga et al [40] | 2019 | Nigeria | CS | 450 | 93.8 | 37.7 | Low risk |
Note: CS: Cross-sectional, DRC: Democratic Republic of Congo.
Assessment methods of PTSD
This research review included studies with varying screening methods for PTSD. While standardized questionnaires were common, most lacked clinical confirmation, raising potential concerns about the accuracy of PTSD diagnoses. However, some studies employed both questionnaires and clinical confirmation, offering a more robust approach to assessing PTSD. Details of these assessment methods used in the original studies are summarized in Table 2.
Table 2. Sampling technique, data collection tool and data collection methods used in the original studies to assess PTSD.
| Authors, publication year | Sampling technique used to select study participants | Data collection tool used to assess PTSD | Methods of data collection |
|---|---|---|---|
| bAsnakew et al, 2019 [33] | Multistage sampling | PCL-C | IA |
| bMadoro et al, 2020 [20] | Simple random sampling | PCL-5 | IA |
| bMakango et al, 2023 [26] | Systematic random sampling | PCL-5 | IA |
| bMasau et al, 2018 [34] | Purposive sampling | NSESSS-PTSD | SA |
| bAli et al, 2023 [10] | Multistage sampling | HTQ | IA |
| aElhabiby et al, 2014 [35] | Purposive sampling | SCID-5-CV | SCI |
| bRoberts et al, 2009 [36] | Multistage sampling | HTQ | IA |
| bRoberts et al, 2008 [21] | Multistage sampling | HTQ | IA |
| aVeling et al, 2013 [37] | Purposive sampling | CIDI-PTSD | SCI |
| bSheikh et al, 2014 [24] | Systematic random sampling | HTQ | IA |
| bAluh et al, 2019 [38] | Purposive sampling | IES-6 questionnaire | IA |
| bIbrahim et al, 2023 [2] | Multistage sampling | HTQ | IA |
| bFaronbi et al, 2021 [39] | Multistage sampling | PCL-C | IA |
| baNwoga et al, 2019 [40] | Systematic random sampling | HTQ and CIDI-PTSD | IA and SCI |
Note: PCL-C = Post-Traumatic Stress Disorder Checklist for Civilians, PCL-5 = Post-Traumatic Stress Disorder Checklist for DSM-5, DSM = Diagnostic and Statistical Manual of Mental Disorder, NSESSS-PTSD = National Stressful Events Survey PTSD Short Scale, HTQ = Harvard Trauma Questionnaire, SCID-5-CV = Structured Clinical Interview for DSM-5 Disorders: Clinician Version, CIDI = Composite International Diagnostic Interview, IES = Impact of Event Scale-6, IA = Interviewer- administered, SA = Self-administered, SCI = Structured clinical interview.
a = Studies assess PTSD with clinical confirmation.
b = Studies assess PTSD without clinical confirmation.
ba = Studies assess PTSD using a mix of both assessments.
Meta-analysis
Pooled prevalence of PTSD among IDPs in Africa
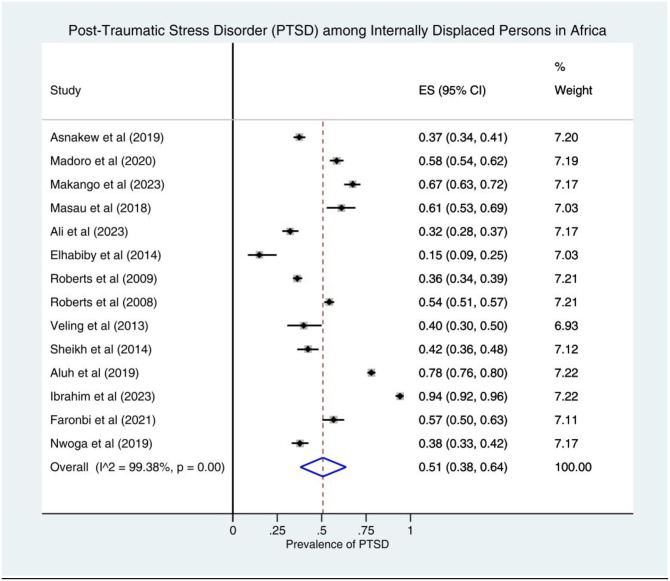
The pooled prevalence estimate of PTSD was found to be 51% (95% CI: 38–64; I2 = 99.38%). In this analysis, the lowest prevalence of PTSD was found in Sudan at 15% (95% CI: 9–25) [35] and the highest prevalence of PTSD was found in Nigeria at 94% (95% CI: 92–96) [2]. A forest plot shows the prevalence estimates of PTSD among IDPs in Africa (Fig 2).
Fig 2. Forest plot of prevalence of PTSD among IDPs in Africa, 2023.
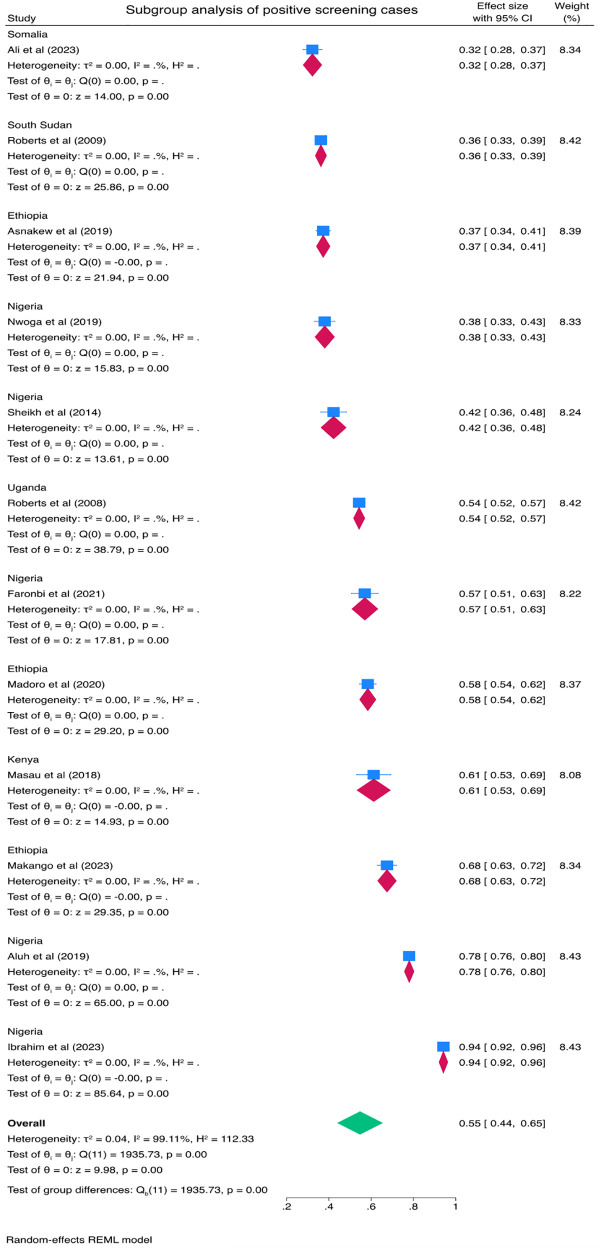
Subgroup analysis
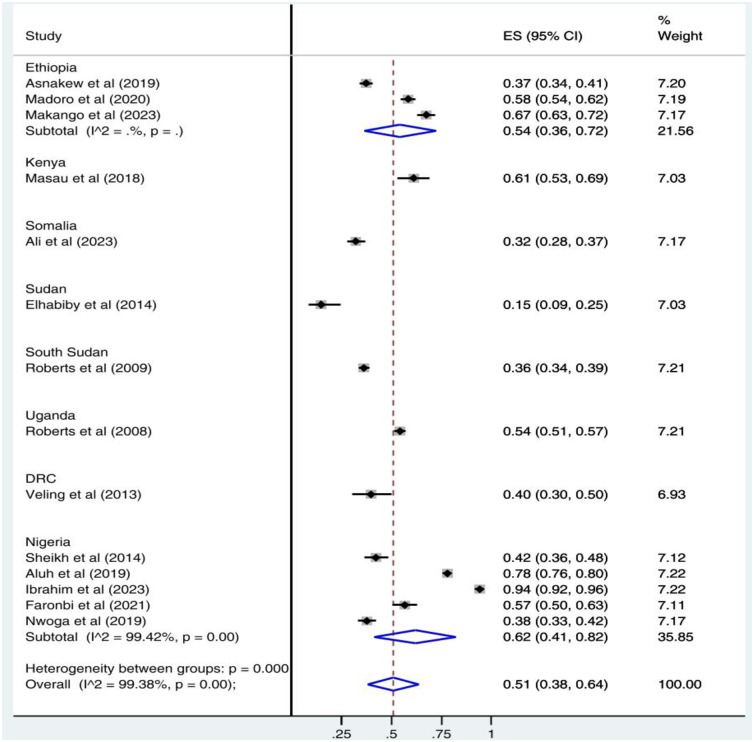
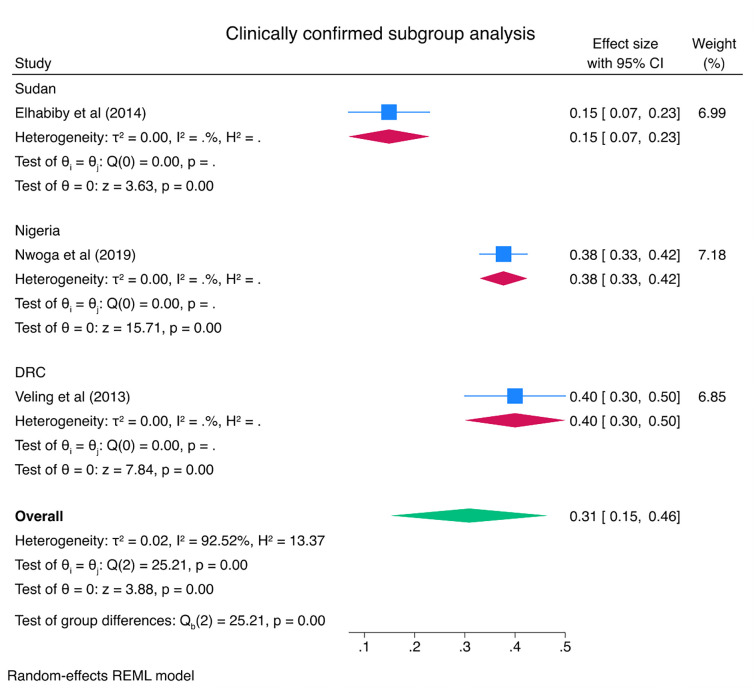
Subgroup analysis was done to see the pooled prevalence of PTSD by country. According to the result, of in-country subgroup analysis, the pooled prevalence of PTSD was 62% (95% CI: 41–82) in Nigeria and 54% (95% CI: 36–72) in Ethiopia. Subgroup analysis of the study showed that the highest and lowest prevalence of PTSD was in Nigeria, 62% (95% CI: 41–82), and Sudan, 15% (95% CI: 9–25), respectively (Fig 3). A subgroup analysis was also performed with clinically confirmed cases of PTSD and positive screening cases of PTSD as different subgroups. Accordingly, the pooled prevalence of clinically confirmed cases of PTSD was 31% (95% CI: 15–46) and positive screening cases of PTSD was 55% (95% CI: 44–65) (Figs 4 & 5).
Fig 3. Subgroup analysis by country for the pooled proportion of PTSD among IDPs in Africa.
Fig 4. Subgroup analysis by clinically confirmed cases of PTSD among IDPs in Africa.
Fig 5. Subgroup analysis by positive screening cases of PTSD among IDPs in Africa.
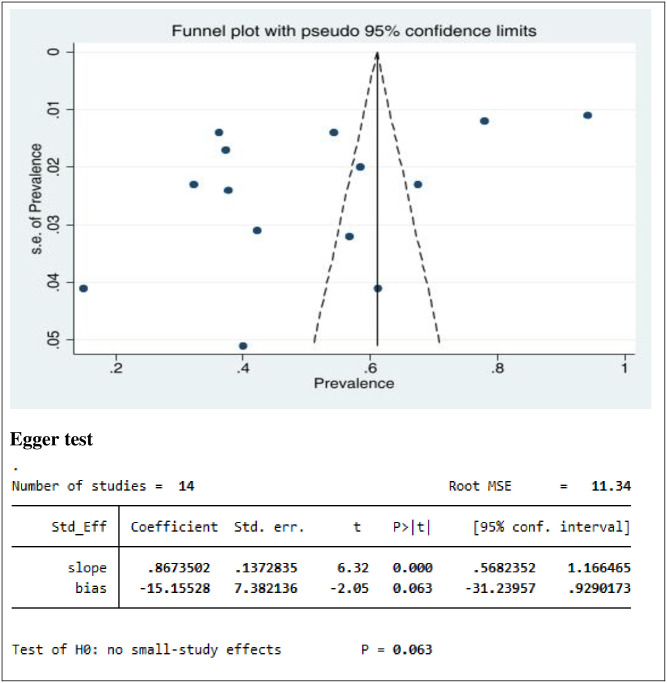
Heterogeneity and publication bias
The presence of heterogeneity and publication bias (small study effect) was assessed within the included studies. The included studies had a high degree of heterogeneity (I2 = 99.38%, p = 0.00). Publication bias was assessed using a funnel plot and Egger’s regression test at a p-value <0.05. The funnel plot showed that the distribution of studies was asymmetrical, whereas Egger’s test was found to be not statistically significant for the estimated prevalence of PTSD (p = 0.063), meaning that there was no evidence of publication bias (Fig 6).
Fig 6. Funnel plot and Egger’s test of studies reporting PTSD among IDPs in Africa.
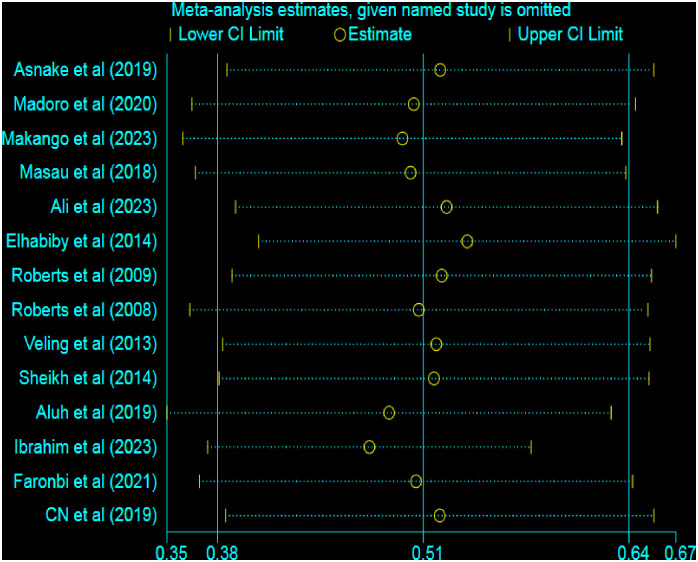
Sensitivity analysis test
A sensitivity analysis was performed to assess the effect of each study on the pooled estimate of PTSD. However, the results of the sensitivity analysis showed that there was no single study effect on the pooled prevalence of PTSD in the fitted meta-analytic model, as shown in Fig 7.
Fig 7. Sensitivity analysis graph to examine the effect of each study on the pooled result.
Factors associated with PTSD among IDPs in Africa
Factors associated with PTSD were identified based on the pooled effect of two or more studies. In this meta-analysis, factors associated with PTSD were assessed using 14 studies [2,10,20,21,24,26,33–40]. The analysis showed that in 4 of these studies [20,21,33,36], female IDPs were found to have a twofold higher risk of developing PTSD compared to male IDPs (OR = 1.99, 95% CI: 1.65–2.32). The pooled results of three studies [21,33,36] revealed that individuals who were no longer married (divorced, separated, widowed, or forcefully separated) had 1.93 times higher likelihood of PTSD compared to those who were married or single (OR = 1.93, 95% CI: 1.43–2.43). Similarly, the pooled findings of two studies [10,26] showed that the likelihood of PTSD was 1.92 times higher for unemployed IDPs compared to employed IDPs (OR = 1.92, 95% CI: 1.17–2.67). Furthermore, two studies’ combined results [33,36] revealed that the likelihood of PTSD was 1.94 times higher for injured IDPs than for uninjured ones (OR = 1.94, 95% CI: 1.50–2.37).
Moreover, the pooled results of two studies [20,21] of this meta-analysis revealed a positive correlation between the likelihood of developing PTSD and the commutative number of traumatic incidents encountered. The odds of PTSD were higher in IDPs who had experienced four or more of the sixteen traumatic events (OR = 2.09, 95% CI: 1.16–3.01), 3.15 times higher in those who had experienced eight to eleven traumatic events (OR = 2.09, 95% CI: 2.18–4.12), and 5.37 times higher in those who had experienced twelve or more traumatic events (OR = 5.37, 95% CI: 2.61–8.12) compared to those who had experienced zero to three traumatic events. The combined findings of two studies [21,36] revealed that the odds of having PTSD were 1.92 times higher for IDPs with poor health who did not receive medical care than for those who did receive medical care (OR = 1.92, 95% CI: 1.41–2.29). Furthermore, the pooled result from four studies [2,20,24,26] revealed that people with depression had a 2.97-fold increased risk of developing PTSD compared to people without depression (OR = 2.97, 95% CI: 2.07–3.86). Additionally, the current analysis discovered a substantial correlation between PTSD and a higher frequency of displacement. The meta-analysis’s combined findings showed that those who were internally relocated more than once had a 2.13-fold increased risk of developing PTSD (Table 3).
Table 3. Factors associated with PTSD among IDPs in Africa, 2023.
| Factors (Reference) | Authors (year) and I2 with p-value | Odds ratio with 95% CI | % Weight |
|---|---|---|---|
| Sex (Male) | Asnakew et al (2019) [33] | 1.70 (1.20, 2.50) | 26.79 |
| Madoro et al (2020) [20] | 2.35 (1.61, 3.44) | 13.52 | |
| Roberts et al (2009) [36] | 2.01 (1.52, 2.66) | 34.84 | |
| Roberts et al (2008) [21] | 2.06 (1.49, 2.84) | 24.84 | |
| Overall, IV (I2 = 0.0%, p = 0.704) | 1.99 (1.65, 2.32) | 100.00 | |
| No longer married* | Asnakew et al (2019) [33] | 2.10 (1.30, 3.40) | 22.72 |
| Roberts et al (2009) [36] | 2.10 (1.28, 3.44) | 21.48 | |
| Roberts et al (2008) [21] | 1.80 (1.25, 2.59) | 55.80 | |
| Overall, IV (I2 = 0.0%, p = 0.843) | 1.93 (1.43, 2.43) | 100.00 | |
| Employment status (Employed) | Makango et al (2021) [26] | 2.09 (1.24, 3.54) | 42.56 |
| Ali et al (2021) [10] | 1.79 (1.06, 3.04) | 57.44 | |
| Overall, IV (I2 = 0.0%, p = 0.698) | 1.92 (1.17, 2.67) | 100.00 | |
| Being injured (No) | Asnakew et al (2019) [33] | 8.30 (5.00, 13.60) | 1.01 |
| Roberts et al (2009) [36] | 1.87 (1.49, 2.36) | 98.99 | |
| Overall, IV (I2 = 88.2%, p = 0.004) | 1.94 (1.50, 2.37) | 100.00 | |
| Number of cumulative trauma events (0–3 trauma) | |||
| 4–7 trauma events | Madoro et al (2020) [20] | 1.90 (1.10, 3.40) | 64.50 |
| Roberts et al (2008) [21] | 2.43 (1.30, 4.40) | 35.50 | |
| Overall, IV (I2 = 0.0%, p = 0.590) | 2.09 (1.16, 3.01) | 100.00 | |
| 8–11 trauma events | Madoro et al (2020) [20] | 2.90 (2.00, 4.10) | 85.50 |
| Roberts et al (2008) [21] | 4.62 (2.70, 7.80) | 14.50 | |
| Overall, IV (I2 = 33.1%, p = 0.222) | 3.15 (2.18, 4.12) | 100.00 | |
| 12–16 trauma events | Madoro et al (2020) [20] | 4.10 (1.70, 9.70) | 47.44 |
| Roberts et al (2008) [21] | 6.51 (3.70, 11.30) | 52.56 | |
| Overall, IV (I2 = 0.0%, p = 0.392) | 5.37 (2.61, 8.12) | 100.00 | |
| Ill health without medical care (No) | Roberts et al (2009) [36] | 1.89 (1.41, 2.53) | 43.86 |
| Roberts et al (2008) [21] | 1.95 (1.52, 2.51) | 56.14 | |
| Overall, IV (I2 = 0.0%, p = 0.875) | 1.92 (1.55, 2.29) | 100.00 | |
| Depression (No) | Madoro et al (2020) [20] | 2.60 (1.79, 3.78) | 80.80 |
| Makango et al (2023) [26] | 5.42 (3.20, 8.31) | 9.51 | |
| Sheikh et al (2014) [24] | 3.53 (1.66, 7.48) | 9.47 | |
| Ibrahim et al (2023) [2] | 7.00 (1.30, 37.90) | 0.22 | |
| Overall, IV (I2 = 21.7%, p = 0.280) | 2.97 (2.07, 3.86) | 100.00 | |
| Frequency of the displacement (Once) | Madoro et al (2020) [20] | 3.69 (2.35, 5.82) | 17.17 |
| Roberts et al (2009) [36] | 1.81 (1.18, 2.76) | 82.83 | |
| Overall, IV (I2 = 73.2%, p = 0.053) | 2.13 (1.41, 2.85) | 100.00 | |
Key:
* No longer married (divorced/separated, widowed, forcefully separated) compared to married and never married.
Discussion
Internally displaced persons (IDPs) are particularly vulnerable to PTSD because they have often experienced traumatic events such as violence, loss of loved ones, and destruction of their homes [41,42]. They may also have difficulty accessing mental health care, which can make it harder to recover from PTSD. Investigating the overall impact and risk factors might be important to the development of interventions to prevent and treat PTSD among IDPs in Africa. The current review presents comprehensive findings on the pooled magnitude of PTSD and its associated factors among IDPs in Africa.
This systematic review and meta-analysis found that the pooled prevalence of PTSD among IDPs in Africa was 51% (95% CI: 38–64%). The prevalence of PTSD in this review was aligned with the studies carried out in the Kurdistan region of Iraq (60%) [43], and Sri Lanka (56%) [44]. Moreover, this finding is in concordance with a systematic review and meta-analysis study in Syria which reported a pooled estimate of 36% PTSD [45]. On the other hand, the prevalence of PTSD in this review was lower than that of the study done in Medellin, Colombia (88%) [46]. There are several possible explanations for these disparities. One possibility could be a difference in methodological approaches. Another possibility is that the studies were conducted with different populations in different cultural and social contexts to manage problems related to displacements [47]. Antithetically, the estimated prevalence of PTSD in the current review was higher than the studies carried out in another study in Sri Lanka (2.3%) [48], Georgia (23.3%) [49], Iraq (20.8%) [50], and India (9%) [51]. Furthermore, the prevalence of PTSD in the current study is higher than in a systematic review and meta-analysis of an epidemiological study done by Nexhmedin M. et al which reported a 26% pooled prevalence of PTSD among survivors living in war-afflicted regions [52].
The subgroup meta-analysis of this review showed that the pooled prevalence of clinically confirmed cases of PTSD was 31% (95% CI: 15–46) and positive screening cases of PTSD was 55% (95% CI: 44–65). One possible explanation for the higher prevalence rate among positive screening cases (55%) compared to clinically confirmed cases (31%) could be related to the sensitivity of the screening tool used. Screening tools are designed to identify individuals who may be at risk or likely to have the condition, but they may also capture individuals with false positives those who screen positive but may not meet the diagnostic criteria upon further clinical assessment. These false positives could inflate the prevalence rate among positive screening cases. On the other hand, clinically confirmed cases undergo a more comprehensive diagnostic evaluation, which includes clinical interviews, symptom assessment, and adherence to specific diagnostic criteria. This process is typically conducted by trained professionals such as qualified mental health professional and aims to ensure a more accurate diagnosis of PTSD. By applying stricter criteria, the diagnostic process may exclude individuals who had initially screened positive but do not meet the clinical diagnostic threshold. Consequently, the prevalence rate among clinically confirmed cases may be lower compared to positive screening cases [53–55].
Several factors may also contribute to the differences. The first possible reason could be due to the impact of conflict, mass displacement, and the level of property destruction repeatedly encountered in the African region where this review was conducted. This may include a combination of war and political and ethnic conflict [22]. In addition, this difference may be related to the differences in the accessibility and affordability of mental health care services in those different settings [23]. Furthermore, it is also possible that the studies were conducted at different times, and that the prevalence of PTSD has changed over time.
A meta-analysis of this review found that females were at higher risk of PTSD than men. Several factors could contribute to the higher prevalence of PTSD among females compared to males. Numerous studies across different countries have documented the higher prevalence of PTSD among females compared to males [13,23,56–60]. These factors can broadly be related to biological, psychological, and social factors. Hormonal differences between females and males that estrogen may enhance emotional reactivity and memory consolidation, potentially increasing the risk of PTSD [61]. Social factors could also contribute to increased PTSD in females because females are more likely to experience interpersonal trauma, such as sexual assault or domestic violence compared with males [23,62,63], which are associated with a higher risk of PTSD compared to other types of traumas. Gender roles and expectations of females may also emphasize emotional expressiveness and vulnerability, which could make them more susceptible to developing PTSD symptoms. Furthermore, psychological factors like coping strategies and social support might be among the factors contributing to the occurrence of PTSD among female IDPs. Females may be more likely to use emotion-focused coping strategies, such as rumination and suppression, which may exacerbate PTSD symptoms. Males, on the other hand, may favor problem-focused coping, which may be more effective at managing stress. In addition, females often have stronger social networks, which can provide emotional support and buffer against stress. However, these networks may also expose females to more trauma-related discussions, potentially increasing the risk of PTSD. Therefore, understanding these factors is crucial for developing effective prevention and treatment strategies for PTSD in this population. This finding may also suggest that it could be important to give more attention to females to provide psychological and general support to minimize the impact on their daily lives.
In this review, being divorced, separated, and widowed was found to be more associated with PTSD compared with being married and/or single. The finding is also consistent with previous studies [23,64]. Marital status can influence an individual’s vulnerability to PTSD in several ways: social support and emotional buffer, joint problem-solving and resource sharing, and sociocultural factors that marriage can provide a strong source of social support and emotional buffering, which can help individuals cope with stress and trauma. These findings suggest that marital status can play a significant role in influencing the risk of PTSD among IDPs. The supportive and protective aspects of marriage can help individuals cope with the challenges of displacement and trauma, reducing their vulnerability to PTSD. However, it is important to note that the relationship between marital status and PTSD may not always be straightforward. In some cases, some studies showed that marital strain or conflict can increase the risk of PTSD among married individuals [65,66]. Therefore, the impact of marital status on PTSD may vary depending on individual circumstances, cultural factors, and the specific nature of the traumatic event.
Consistent with earlier findings [10], employment status was also found to have a significant association with PTSD among IDPs. Several factors contribute to this association: loss of routine and structure that unemployment disrupts an individual’s daily routine and structure, which can be particularly destabilizing for IDPs who have already experienced the upheaval of displacement; financial strain, and economic hardship, adding to the stress and anxiety of displacement; limited access to mental health care that can hinder an individual’s ability to access mental health care, either due to financial constraints or the lack of employer-sponsored health insurance. These findings underscore the importance of employment in promoting mental health and well-being among IDPs. Supporting employment opportunities and providing vocational training can help IDPs regain a sense of normalcy, purpose, and control, reducing their risk of developing PTSD and improving their overall quality of life.
This review revealed that being injured is significantly associated with the existence of PTSD among IDPs, which is in line with other studies [23,42,67]. Experiencing physical injury during displacement can significantly increase an individual’s risk of developing PTSD because of direct trauma and physical pain, psychological impact of injury, impact on daily living and functioning, limited access to healthcare and support, trauma reactivation, and reminders of injury. These findings highlight the importance of addressing physical injuries and providing comprehensive support services for IDPs to mitigate the risk of developing PTSD. Timely and effective medical care, rehabilitation services, and psychological support can significantly improve the physical and mental health outcomes of IDPs who have experienced injuries.
The current finding has shown, consistent with earlier evidence [23,45,68,69], that the number of trauma events experienced was positively associated with the risk of PTSD. There is a well-established relationship between the number of trauma events experienced and the risk of PTSD among IDPs. Research suggests that each additional trauma event increases the likelihood of developing PTSD. This association can be attributed to several factors, such as accumulation of stress and emotional overload. Each trauma event exposes an individual to significant stress and emotional overload, taxing their coping mechanisms and increasing their vulnerability to developing PTSD. The cumulative effect of multiple trauma events can overwhelm an individual’s ability to process and integrate these experiences, leading to the development of PTSD symptoms. In addition, repeated exposure to traumatic events can heighten an individual’s sensitivity to trauma cues, making them more likely to experience flashbacks, nightmares, and intrusive thoughts related to the traumatic experiences. This sensitization can maintain the state of hypervigilance and emotional arousal characteristic of PTSD. These findings may underscore the importance of preventing and addressing trauma exposure among IDPs to reduce the risk of developing PTSD. Providing early intervention and mental health support services can help IDPs cope with the effects of trauma and prevent the development of PTSD.
Illness in the absence of medical care was found to be significantly associated with the presence of PTSD among IDPs and this is in line with other findings [21]. The absence of medical care significantly elevates the risk of developing PTSD among IDPs. This association stems from several interconnected factors including unmet physical and psychological needs. Lack of access to medical care can lead to the neglect of both physical and psychological needs following a traumatic event. These findings highlight the importance of providing comprehensive healthcare services to IDPs, including both physical and mental healthcare. Addressing their medical needs can significantly reduce the risk of developing PTSD and promote their overall well-being.
In the current review, the presence of depression is found to have a significant association with PTSD among IDPs, which is in line with earlier studies [10,21,23]. The co-occurrence of depression and post-traumatic stress disorder (PTSD) is prevalent among internally displaced persons (IDPs). This could be because of shared etiological factors that both depression and PTSD share common risk factors, such as exposure to trauma, genetic predisposition, and neurobiological alterations. Both depression and PTSD involve dysregulation of stress hormones, such as cortisol and norepinephrine. These hormonal imbalances can contribute to the development and maintenance of both conditions. In addition, IDPs face a range of social and environmental stressors, such as displacement, loss of social support, and economic hardship. These stressors can contribute to both depression and PTSD by exacerbating emotional distress and reducing resilience. These findings implicate the importance of addressing both depression and PTSD simultaneously in IDPs. Integrated treatment approaches that target both conditions can significantly improve the mental health outcomes of IDPs.
The current review also revealed that an increased frequency of displacement was also found to be significantly associated with PTSD. The finding is consistent with previous studies [21,23,42,67,68]. The number of times an individual had been displaced was positively associated with the risk of PTSD. Multiple factors contribute to the increased risk of PTSD among IDPs who experience repeated displacements. This could be because each displacement experience exposes an individual to significant stress and emotional overload, taxing their coping mechanisms and increasing their vulnerability to developing PTSD. Repeated displacements lead to an accumulation of traumatic experiences, making it increasingly difficult to process and integrate these experiences, ultimately increasing the risk of PTSD. Frequent displacements can heighten an individual’s sensitivity to trauma cues, making them more likely to experience flashbacks, nightmares, and intrusive thoughts related to the traumatic experiences. This sensitization perpetuates the state of hypervigilance and emotional arousal characteristic of PTSD. These findings suggest the importance of preventing and addressing repeated displacements to reduce the risk of PTSD among IDPs. Providing stable housing, livelihood support, and mental health services can help IDPs cope with the effects of displacement and prevent the development of PTSD.
Strengths and limitations of the study
This study was a first-of-its-kind systematic review and meta-analysis that estimated the pooled prevalence and associated risk factors of PTSD among IDPs in Africa. The study identified several significant risk factors for PTSD among IDPs. This information can be used to develop targeted interventions to prevent PTSD. This study has its limitations. Firstly, it was a cross-sectional study, so it could not establish cause-effect relationships. In addition, the lack of studies from countries other than those included may limit the continental representativeness of the study. Overall, the study is a valuable contribution to our understanding of PTSD among IDPs in Africa. The findings can be used to inform the development of targeted interventions to prevent PTSD among this vulnerable population.
Conclusions
The findings of this systematic review and meta-analysis highlight the alarming prevalence of PTSD among IDPs in Africa. The estimated pooled prevalence of 51% is significantly higher than the general population prevalence of PTSD, demonstrating the unique challenges faced by IDPs in coping with trauma and displacement. The study’s identification of significant risk factors, including female gender, marital status, traumatic events, ill health without medical care, depression, and frequency of displacement, provides valuable insights for targeted interventions. Effective interventions and the development of tailored mental health programs are needed to prevent and treat PTSD among IDPs, with focusing on the identified risk factors. Future studies focusing on the determinant factors of PTSD and their impacts on IDPs need to be welcomed.
Supporting information
(DOCX)
(DOCX)
(DTA)
Acknowledgments
The authors would like to thank the University of Gondar, Ethiopia, for providing an office and free internet service. Moreover, the authors thanked and recognized the articles included in this study and used them as a basis for this systematic review and meta-analysis.
Data Availability
All relevant data are within the manuscript and its Supporting information files (S3 File).
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Yigzaw GS, Abitew EB: Causes and impacts of internal displacement in Ethiopia. African Journal of Social Work 2019, 9(2):32–41. [Google Scholar]
- 2.Ibrahim UU, Aliyu AA, Abdulhakeem OA, Abdulaziz M, Asiya M, Sabitu K, et al. : Prevalence of Boko Haram crisis related depression and post-traumatic stress disorder symptomatology among internally displaced persons in Yobe state, North East, Nigeria. Journal of Affective Disorders Reports 2023, 13:100590. [Google Scholar]
- 3.Chukwuorji JBC, Ifeagwazi CM, Eze JE: Event centrality influences posttraumatic stress disorder symptoms via core beliefs in internally displaced older adults. Aging & mental health 2019, 23(1):113–121. doi: 10.1080/13607863.2017.1396580 [DOI] [PubMed] [Google Scholar]
- 4.Edition F: Diagnostic and statistical manual of mental disorders. Am Psychiatric Assoc 21, 591–643. In.; 2013. [Google Scholar]
- 5.Perrin M, Vandeleur CL, Castelao E, Rothen S, Glaus J, Vollenweider P, et al. : Determinants of the development of post-traumatic stress disorder, in the general population. Social psychiatry and psychiatric epidemiology 2014, 49:447–457. doi: 10.1007/s00127-013-0762-3 [DOI] [PubMed] [Google Scholar]
- 6.Ehlers A, Clark DM: A cognitive model of posttraumatic stress disorder. Behaviour research and therapy 2000, 38(4):319–345. doi: 10.1016/s0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- 7.Kagee A, Del Soto AG: INTERNAL DISPLACEMENT AND TRAUMA. ACTA GEOGRAPHICA–TRONDHEIM:229.
- 8.Auxéméry Y: Post-traumatic psychiatric disorders: PTSD is not the only diagnosis. La Presse Médicale 2018, 47(5):423–430. doi: 10.1016/j.lpm.2017.12.006 [DOI] [PubMed] [Google Scholar]
- 9.Panagioti M, Gooding P, Tarrier N: Post-traumatic stress disorder and suicidal behavior: A narrative review. Clinical psychology review 2009, 29(6):471–482. doi: 10.1016/j.cpr.2009.05.001 [DOI] [PubMed] [Google Scholar]
- 10.Ali M, Mutavi T, Mburu JM, Mathai M: Prevalence of Posttraumatic Stress Disorder and Depression Among Internally Displaced Persons in Mogadishu-Somalia. Neuropsychiatric disease and treatment 2023:469–478. doi: 10.2147/NDT.S398423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nicholas A, Joshua O, Elizabeth O: Accessing mental health Services in Africa: current state, efforts, challenges and recommendation. Annals of Medicine and Surgery 2022, 81:104421. doi: 10.1016/j.amsu.2022.104421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanhori Z, Hauff E, Eide AH, Mdala I, Abdelrahman A, Brunborg C, et al. : Changes in prevalence of mental disorders among internally displaced persons in central Sudan: a 1-year follow-up study. Global Mental Health 2020, 7:e24. doi: 10.1017/gmh.2020.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Djatche JM, Herrington OD, Nzebou D, Galusha D, Boum Y, Hassan S: A cross-sectional analysis of mental health disorders in a mental health services-seeking population of children, adolescents, and young adults in the context of ongoing violence and displacement in northern Cameroon. Comprehensive psychiatry 2022, 113:152293. doi: 10.1016/j.comppsych.2021.152293 [DOI] [PubMed] [Google Scholar]
- 14.Umenweke MN, Orabueze AI: PROTECTION OF INTERNALLY DISPLACED PERSONS IN NIGERIA: WHOSE LEGAL RESPONSIBILITY? NIGERIAN JOURNAL OF AFRICAN STUDIES (NJAS) 2023, 5(2). [Google Scholar]
- 15.Siriwardhana C, Adikari A, Pannala G, Siribaddana S, Abas M, Sumathipala A, et al. : Prolonged internal displacement and common mental disorders in Sri Lanka: the COMRAID study. PloS one 2013, 8(5):e64742. doi: 10.1371/journal.pone.0064742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Speidel JJ, O’Sullivan JN: Advancing the Welfare of People and the Planet with a Common Agenda for Reproductive Justice, Population, and the Environment. World 2023, 4(2):259–287. [Google Scholar]
- 17.UNHCR-UNHCR’S INITIATIVE ON INTERNAL DISPLACEMENT 2020–2021: https://reporting.unhcr.org/sites/default/files/UNHCR%20Initiative%20on%20Internal%20Displacement%202020-2021.pdf.
- 18.Morina N, Akhtar A, Barth J, Schnyder U: Psychiatric disorders in refugees and internally displaced persons after forced displacement: a systematic review. Frontiers in psychiatry 2018, 9:433. doi: 10.3389/fpsyt.2018.00433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bogic M, Njoku A, Priebe S: Long-term mental health of war-refugees: a systematic literature review. BMC international health and human rights 2015, 15(1):1–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Madoro D, Kerebih H, Habtamu Y, G/tsadik M, Mokona H, Molla A, et al. : Post-traumatic stress disorder and associated factors among internally displaced people in South Ethiopia: a cross-sectional study. Neuropsychiatric disease and treatment 2020:2317–2326. doi: 10.2147/NDT.S267307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E: Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC psychiatry 2008, 8(1):1–9. doi: 10.1186/1471-244X-8-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Njau JW: Posttraumatic stress disorder among the heads of households of ethnic clashes survivors in the Rift Valley Province, Kenya: a comparative study. University of Nairobi; 2005. [Google Scholar]
- 23.Koshe T, Jarso MH, Walde MT, Ebrahim J, Mamo A, Esmael A, et al. : A post-traumatic stress disorder among internally displaced people in sub-Saharan Africa: a systematic review. Frontiers in Psychiatry 2023, 14. doi: 10.3389/fpsyt.2023.1261230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheikh TL, Mohammed A, Agunbiade S, Ike J, Ebiti WN, Adekeye O: Psycho-trauma, psychosocial adjustment, and symptomatic post-traumatic stress disorder among internally displaced persons in Kaduna, Northwestern Nigeria. Frontiers in psychiatry 2014, 5:127. doi: 10.3389/fpsyt.2014.00127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taru MY, Bamidele LI, Makput DM, Audu MD, Philip TF, John DF, et al. : Posttraumatic stress disorder among internally displaced victims of Boko Haram terrorism in north-eastern Nigeria. Jos Journal of Medicine 2018, 12(1):8–15. [Google Scholar]
- 26.Makango B, Alemu ZA, Solomon T, Lemma N, Girma T, Mohammednur T, et al. : Prevalence and factors associated with post-traumatic stress disorder among internally displaced people in camps at Debre Berhan, Amhara Region, Ethiopia: a cross-sectional study. BMC psychiatry 2023, 23(1):81. doi: 10.1186/s12888-023-04570-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Owoaje ET, Uchendu OC, Ajayi TO, Cadmus EO: A review of the health problems of the internally displaced persons in Africa. Nigerian postgraduate medical journal 2016, 23(4):161–171. doi: 10.4103/1117-1936.196242 [DOI] [PubMed] [Google Scholar]
- 28.Abidde SO: The Challenges of Refugees and Internally Displaced Persons in Africa: Springer; 2021. [Google Scholar]
- 29.Group ADB: Tracking Africa’s progress in figures. In.: African Development Bank Tunis; 2014.
- 30.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. : Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews 2015, 4(1):1–9. doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Institute JB: Critical appraisal tools for use in JBI systematic reviews. Checklist for analytical cross-sectional studies. Australia: The Joanna Briggs Institute; 2017. [Google Scholar]
- 32.Higgins JP, Thompson SG: Quantifying heterogeneity in a meta‐analysis. Statistics in medicine 2002, 21(11):1539–1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 33.Asnakew S, Shumet S, Ginbare W, Legas G, Haile K: Prevalence of post-traumatic stress disorder and associated factors among Koshe landslide survivors, Addis Ababa, Ethiopia: a community-based, cross-sectional study. BMJ open 2019, 9(6):e028550. doi: 10.1136/bmjopen-2018-028550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Musau JN, Omondi M, Khasakhala L: The prevalence of post-traumatic stress disorder (PTSD) among internally displaced persons (IDPs) in Maai Mahiu Camp in Nakuru County, Kenya. Journal of Internal Displacement 2018, 8(1):20–33. [Google Scholar]
- 35.Elhabiby MM, Radwan DN, Okasha TA, El-Desouky ED: Psychiatric disorders among a sample of internally displaced persons in South Darfur. International journal of social Psychiatry 2015, 61(4):358–362. doi: 10.1177/0020764014547061 [DOI] [PubMed] [Google Scholar]
- 36.Roberts B, Damundu EY, Lomoro O, Sondorp E: Post-conflict mental health needs: a cross-sectional survey of trauma, depression and associated factors in Juba, Southern Sudan. BMC psychiatry 2009, 9(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Veling W, Hall BJ, Joosse P: The association between posttraumatic stress symptoms and functional impairment during ongoing conflict in the Democratic Republic of Congo. Journal of anxiety disorders 2013, 27(2):225–230. doi: 10.1016/j.janxdis.2013.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aluh DO, Okoro RN, Zimboh A: The prevalence of depression and post-traumatic stress disorder among internally displaced persons in Maiduguri, Nigeria. Journal of public mental health 2019, 19(2):159–168. [Google Scholar]
- 39.Faronbi JO, Adegbola GA, Bello CB, Akinyoola OD, Oginni MO: Posttraumatic stress disorder and suicidal ideation among the internally displaced persons in Nigeria. Egyptian Nursing Journal 2020, 17(3):154. [Google Scholar]
- 40.Nwoga C, Dakwak S, Audu M, Goar S, Agbir T, Armiya’u A, et al. : Post-traumatic Stress Disorder and Functional Disability among Internally Displaced Persons in North-East Nigeria. Journal of BioMedical Research and Clinical Practice 2019, 2(2):132–137. [Google Scholar]
- 41.Anbesaw T, Zenebe Y, Asmamaw A, Shegaw M, Birru N: Post-traumatic stress disorder and associated factors among people who experienced traumatic events in dessie town, Ethiopia, 2022: a community based study. Frontiers in psychiatry 2022, 13:1026878. doi: 10.3389/fpsyt.2022.1026878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rofo S, Gelyana L, Moramarco S, Alhanabadi LH, Basa FB, Dellagiulia A, et al. : Prevalence and risk factors of posttraumatic stress symptoms among Internally Displaced Christian couples in Erbil, Iraq. Frontiers in Public Health 2023, 11:1129031. doi: 10.3389/fpubh.2023.1129031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mahmood HN, Ibrahim H, Goessmann K, Ismail AA, Neuner F: Post-traumatic stress disorder and depression among Syrian refugees residing in the Kurdistan region of Iraq. Conflict and Health 2019, 13(1):1–11. doi: 10.1186/s13031-019-0238-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ranasinghe PD, Levy BR: Prevalence of and sex disparities in posttraumatic stress disorder in an internally displaced Sri Lankan population 6 months after the 2004 Tsunami. Disaster Medicine and Public Health Preparedness 2007, 1(1):34–41. doi: 10.1097/DMP.0b013e318068fbb7 [DOI] [PubMed] [Google Scholar]
- 45.Kanan J, Leão T: Post-traumatic stress disorder in youth exposed to the Syrian conflict: A systematic review and meta-analysis of prevalence and determinants. Journal of health psychology 2022:13591053221123141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Richards A, Ospina-Duque J, Barrera-Valencia M, Escobar-Rincón J, Ardila-Gutiérrez M, Metzler T, et al. : Posttraumatic stress disorder, anxiety and depression symptoms, and psychosocial treatment needs in Colombians internally displaced by armed conflict: A mixed-method evaluation. Psychological Trauma: Theory, Research, Practice, and Policy 2011, 3(4):384. [Google Scholar]
- 47.Tesfaw TA: Internal displacement in ethiopia: a scoping review of its causes, trends and consequences. Journal of Internal Displacement 2022, 12(1):2–31. [Google Scholar]
- 48.Husain F, Anderson M, Cardozo BL, Becknell K, Blanton C, Araki D, et al. : Prevalence of war-related mental health conditions and association with displacement status in postwar Jaffna District, Sri Lanka. Jama 2011, 306(5):522–531. doi: 10.1001/jama.2011.1052 [DOI] [PubMed] [Google Scholar]
- 49.Makhashvili N, Chikovani I, McKee M, Bisson J, Patel V, Roberts B: Mental disorders and their association with disability among internally displaced persons and returnees in Georgia. Journal of traumatic stress 2014, 27(5):509–518. doi: 10.1002/jts.21949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.AlShawi AF: Prevalence of posttraumatic stress disorders among sample of internally displaced persons in Iraq, a preliminary study. J Community Med Health Educ 2018, 8(599):2161–0711. doi: 10.1007/BF00220824 . [DOI] [PubMed] [Google Scholar]
- 51.WHO: Psychological Effects among Internally Displaced Persons (IDPS) Residing in two Districts of Sindh. In.; 2013.
- 52.Morina N, Stam K, Pollet TV, Priebe S: Prevalence of depression and posttraumatic stress disorder in adult civilian survivors of war who stay in war-afflicted regions. A systematic review and meta-analysis of epidemiological studies. Journal of affective disorders 2018, 239:328–338. doi: 10.1016/j.jad.2018.07.027 [DOI] [PubMed] [Google Scholar]
- 53.Shah A, Banner N, Heginbotham C, Fulford B: 7. American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th edn. American Psychiatric Publishing, Arlington, VA. 8. Bechara, A., Dolan, S. and Hindes, A.(2002) Decision-making and addiction (Part II): myopia for the future or hypersensitivity to reward? Neuropsychologia, 40, 1690–1705. 9. Office of Public Sector Information (2005) The Mental Capacity Act 2005. http://www Substance Use and Older People 2014, 21(5):9. [DOI] [PubMed]
- 54.Creamer M, Bell R, Failla S: Psychometric properties of the impact of event scale—revised. Behaviour research and therapy 2003, 41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010 [DOI] [PubMed] [Google Scholar]
- 55.Prins A, Kimerling R, Cameron R, Oumiette P, Shaw J, Thrailkill A, et al: The primary care PTSD screen (PC-PTSD). In: 15th annual meeting of the International Society for Traumatic Stress Studies Miami, FL: 1999; 1999.
- 56.Aysazci-Cakar F, Schroder T, Hunt N: A systematic review of prevalence and correlates of post-traumatic stress disorder, depression and anxiety in displaced Syrian population. Journal of Affective Disorders Reports 2022:100397. [Google Scholar]
- 57.Farhood L, Fares S, Hamady C: PTSD and gender: could gender differences in war trauma types, symptom clusters and risk factors predict gender differences in PTSD prevalence? Archives of women’s mental health 2018, 21:725–733. doi: 10.1007/s00737-018-0849-7 [DOI] [PubMed] [Google Scholar]
- 58.Murad ZK: Assessment of Post-Traumatic Stress Disorder Among Shengalian Internally Displaced Persons Journal of Archives of Nursing and Care 2019, 2(4). [Google Scholar]
- 59.Irish LA, Fischer B, Fallon W, Spoonster E, Sledjeski EM, Delahanty DL: Gender differences in PTSD symptoms: An exploration of peritraumatic mechanisms. Journal of anxiety disorders 2011, 25(2):209–216. doi: 10.1016/j.janxdis.2010.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Elklit A, Lasgaard M, Palic S: Social support, coping and posttraumatic stress symptoms in young refugees. Torture: quarterly journal on rehabilitation of torture victims and prevention of torture 2012, 22(1):11–23. [PubMed] [Google Scholar]
- 61.Ney LJ, Gogos A, Hsu C-MK, Felmingham KL: An alternative theory for hormone effects on sex differences in PTSD: The role of heightened sex hormones during trauma. Psychoneuroendocrinology 2019, 109:104416. doi: 10.1016/j.psyneuen.2019.104416 [DOI] [PubMed] [Google Scholar]
- 62.Basheti IA, Ayasrah SM, Al-Qudah RA: Post-traumatic stress disorders among Syrian refugees residing in non-camp settings in Jordan. Saudi medical journal 2023, 44(1):91. doi: 10.15537/smj.2023.44.1.20220701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kong BS, Gezimu W, Demeke A, Duguma A: Prevalence of Rape and Its Predictors among Female Students Attending Elementary Schools: In the Case of Kule Refugee Camp, Gambella, Southwest Ethiopia—A Cross-Sectional Study. International journal of reproductive medicine 2023, 2023. doi: 10.1155/2023/5559246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Roberts B, Browne J: A systematic review of factors influencing the psychological health of conflict-affected populations in low-and middle-income countries. Global public health 2011, 6(8):814–829. doi: 10.1080/17441692.2010.511625 [DOI] [PubMed] [Google Scholar]
- 65.Hamid AA, Musa SA: Mental health problems among internally displaced persons in Darfur. International Journal of Psychology 2010, 45(4):278–285. doi: 10.1080/00207591003692620 [DOI] [PubMed] [Google Scholar]
- 66.Essizoglu A, Keser I: Post-traumatic stress disorder in internally displaced people subjected to displacement by armed forces. J Trauma Stress Disor Treat 2014, 3(2):2–6. [Google Scholar]
- 67.Kim GU, Jung E, Shim MS, Kim GS: Association between post‐traumatic stress symptoms and functional health among internally displaced people in Myanmar. Journal of psychiatric and mental health nursing 2022, 29(4):555–567. doi: 10.1111/jpm.12837 [DOI] [PubMed] [Google Scholar]
- 68.Abu Suhaiban H, Grasser LR, Javanbakht A: Mental health of refugees and torture survivors: a critical review of prevalence, predictors, and integrated care. International journal of environmental research and public health 2019, 16(13):2309. doi: 10.3390/ijerph16132309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Scholte WF, Olff M, Ventevogel P, de Vries G-J, Jansveld E, Cardozo BL, et al. : Mental health symptoms following war and repression in eastern Afghanistan. Jama 2004, 292(5):585–593. doi: 10.1001/jama.292.5.585 [DOI] [PubMed] [Google Scholar]