Abstract
BACKGROUND:
Tracheobronchial foreign body (FB) aspiration (FBA) is a life-threatening emergency mostly observed in childhood and advanced age. With early diagnosis, the FB can be removed using bronchoscopic methods without causing irreversible damage.
METHODS:
This was a single-center, retrospective observational study. Subjects diagnosed with FBA via either bronchoscopic methods and/or radiological findings, having no medical history of aspirated FB, and who were detected to have aspirated FB for longer than 30 days were included in the study. Medical records and radiological and bronchoscopic findings of the subjects were investigated from the hospital information database system.
RESULTS:
Of the 255 patients with FBA, 17.6% (N = 45) were diagnosed late. The mean age was 53 y; 28% were female, and 60% of the subjects had a history of ever smoking. The estimated residence time of the FB in the bronchial system was 22.8 months. The most common complaints were cough and shortness of breath. Forty-two percent of the aspirated FBs were organic material. FB artifact could be observed in 6.7% of posteroanterior chest radiographs and 65% of thorax computed tomography (CT) scans. Rigid bronchoscopy had been primarily preferred as therapeutic interventional procedure. It was also found that the artifact most frequently resided in the right bronchial system and was most commonly found in the right lower lobe, while granulation tissue was formed in 85% of the subjects.
CONCLUSIONS:
The findings of the present study demonstrate that subjects tended to forget the FBA, leading to insidious respiratory system symptoms, with recurrent infections. In cases with an endobronchial mass lesion image on thorax CT, clinicians should consider the possibility of FBA. Delayed diagnosis of both organic and inorganic FB may cause granulation tissue.
Keywords: bronchus, foreign body, foreign body aspiration, rigid bronchoscopy
Introduction
Tracheobronchial foreign body (FB) aspiration (FBA) is a life-threatening condition that is usually observed in childhood and advanced age, although it can be seen in all age groups.1,2 Whereas the aspirated material can be removed by bronchoscopic methods without causing irreversible damage to the respiratory system, diagnosis may be delayed in patients with few or atypical symptoms. Scar formation is another condition commonly detected in these cases.3,4 Late diagnosis of FBA is more common in patients with developmental disorders, behavioral-health disorders, Alzheimer’s disease, or alcohol use disorder.5 Limited data are available in the literature on late-diagnosed FBA in adults. The present study evaluated the clinical, radiological, and bronchoscopic findings of subjects with late-diagnosed FBA.
QUICK LOOK.
Current knowledge
Foreign body (FB) aspiration is one of the life-threatening chest disease emergencies. Generally, patients are admitted to the hospital within the first 48 h after aspiration, and the FB can be removed by bronchoscopic methods. In cases such as children, advanced age, Alzheimer’s, and alcohol use disorder, the aspirated material may remain in the bronchial system because they do not remember the aspiration history or cannot give adequate anamnesis.
What this paper contributes to our knowledge
Foreign bodies aspirated in the the respiratory tract can go unnoticed by the patient leading to delayed diagnosis and persistent symptoms. Subjects with late foreign body diagnosis often present with cough, shortness of breath and recurrent pulmonary infection. Imaging demonstrating an endobronchial mass on thoracic CT along with clinical symptoms should prompt a high index of suspicion for foreign body aspiration. In this series, foreign bodies were most commonly organic in origin (seeds, nuts, bones).
Methods
This retrospective, single-center, observational study was conducted at a reference center for chest diseases. All flexible fiberoptic bronchoscopy (FOB) and rigid bronchoscopy (RB) procedures performed in the bronchology unit of our hospital between January 2000–June 2021 were investigated via the hospital information database system. The medical files of subjects who had undergone FB removal during the procedure were evaluated. In sum, 255 FBs removed by bronchoscopic methods were recorded. Forty-five subjects either having no history of FBA before bronchoscopy or having a history of aspirated material longer than 30 d or subjects found to have an FB in the bronchial system for longer than 30 d along with previous radiological images were included in the study.
Subjects’ demographic data, symptoms at admission, physical examination findings, posteroanterior chest radiograph findings, computed tomography (CT) findings, FOB and RB findings, and characteristics of FB were recorded.
Radiologic images and thorax CT findings of all subjects were reevaluated by 2 pulmonologists (KK, STO). Our study was approved by the University of Health Sciences Turkey, Yedikule Thoracic Diseases and Thoracic Surgery Training and Research Hospital Science Board (18.01.2021/2021-261). In accordance with the Helsinki Declaration and the general practice of our hospital, written and oral approval consent was obtained from the subjects.
Performance of Bronchoscopic Procedures in the Study Unit
In our hospital, FOB procedure is performed under conscious sedation. All patients are monitored with electrocardiography and oxygen saturation levels via saturation probe during the procedure. Intravenous midazolam 0.05–0.10 mg/kg and local lidocaine (maximum dose 8 mg/kg) are used, and dosages are adjusted to the patient’s condition. FOBs (Olympus, Medical, Tokyo, Japan; PENTAX Medical, Tokyo, Japan; Fujifilm, Tokyo, Japan) are inserted through the oral route.
RB procedures are performed under general anesthesia. All patients are monitored with electrocardiography and oxygen saturation levels via saturation probe during the procedure. General anesthesia induction is achieved with midazolam 0.05–0.10 mg/kg, propofol (maximum dose 1,000 mg), remifentanil (maximum dose 2 mg), and rocuronium (maximum dose 50 mg), with the dosage adjusted to the patient’s condition. The equipment used in the procedures included the Dumon Series II rigid bronchoscope (Efer Endoscopy, La Ciotat, France) with optical system. Argon plasma coagulation (40 W, blended mode/continuous flow) is applied using an instrument by Erbe Elektromedizin, (Tubigen, Germany). Endoluminal treatment is accomplished with a diode laser operating at a wavelength of 980 nm with 4–25 W in pulsed mode (Cerals D25, biolitec, Jena, Germany). Cryotherapy is performed with the ERBOKRYO system (Erbe Elektromedizin).
Statistics
All statistical analyses were carried out with SPSS 21.0 (IBM, Armonk, New York). Descriptive statistics were reported including mean (SD), median (interquartile range), and percentage. The Kolmogorov-Smirnov test was used to determine whether the continuous variables showed normal distribution or not. Pearson chi-square and Fisher exact test were used to determine differences between categorical variables. Values with a P values of ≤ .05 were considered statistically significant.
Results
When we retrospectively analyzed our hospital records, it was determined that there were 255 cases of FBA. We found that 17.6% (N = 45) of these cases were late-diagnosis FBA cases (Fig. 1). The mean age of the subjects with late diagnosis was 53.8 ± 18.0 (18–84) y, and 28.9% (n = 13) were female; 60% of the subjects were ever smokers. While 30 subjects had at least one comorbidity, the most common comorbidities were hypertension (n = 10), COPD (n = 8), and diabetes mellitus (n = 6). Five subjects were tracheostomized, while other comorbidities were bronchiectasis (n = 3), laryngeal cancer (n = 4), and lung cancer (n = 2).
Figure 1.
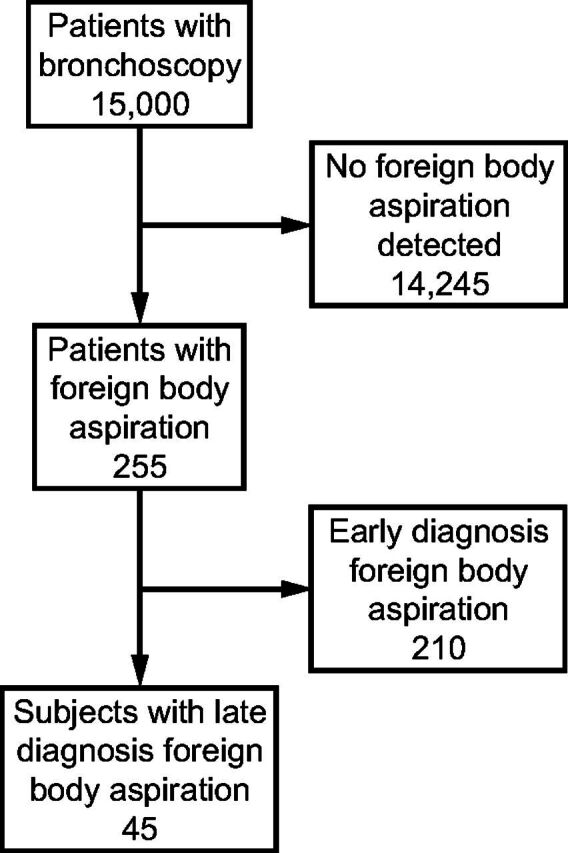
Flow chart.
It was found that there was no record of FBA in the medical history taken before the FB was detected by interventional procedures of the 45 subjects. In the medical history taken again after FBA was detected, 24.4% (n = 11) of subjects stated that they forgot about the event because it had been a long time, and thus they did not mention it in the history. The other 34 cases did not remember the aspiration event. In subjects with late diagnosis, the estimated mean residence time of the FB in the bronchial system was 22.8 ± 63.4 months (1–365 d), with a median duration of 3 months.
At presentation, one subject was asymptomatic. The most common complaints were cough (n = 28, 62%), shortness of breath (n = 21, 47%), fever (n = 11, 24%), sputum (n = 11, 24%), chest pain (n = 8, 18%), hemoptysis, and fatigue (n = 1, for each). Respiratory examination was normal in 16 subjects. The examination findings were decreased breath sounds in 28.9% (n = 13), localized crackles in 24.4% (n = 11), bronchiectasis in 13.3% (n = 6), and prolonged expiration in 6.7% (n = 3). Neither stridor nor wheezing was detected. FBs removed from the bronchial system consisted of organic (42%, n = 19) and inorganic material (29%, n = 13), while 29% (n = 13) of substances could not be differentiated pathologically. Organic substances included fish bones, chickpeas, cinnamon sticks, pits, olive seeds (n = 2), chestnuts, bones (n = 2), and hazelnut shells. Inorganic ones were plastic stopper (n = 2), tooth and dental prosthesis (n = 5), tracheostomy cannula (n = 1), and speech apparatus (n = 3) (Table 1).
Table 1.
List of Aspirated Foreign Bodies
It was determined that RB (n = 26) was used as the first choice method for the removal of the FB from the bronchial system, and flexible bronchoscopy (n = 17) was the second choice. The FB was removed with cryotherapy in 7 cases and biopsy forceps in 19 cases in which RB was performed. Whereas it was determined that biopsy forceps were used in 10 of the cases who underwent flexible bronchoscopy, sufficient data could not be found in 7 cases. The cryotherapy extraction method was most commonly used for organic (57%) materials. There was no statistically significant difference between the interventional methods used and the presence of granulation tissue (P = .13), age (P = .65), additional disease (P = .09), or organic or inorganic material (P = .13). Consolidation (55%) and atelectasis (42.2%) were found most commonly in lung radiographs of 39 cases (86.6%). FB artifact could be observed in 6.7% of posteroanterior chest radiographs. Consolidation (81%), atelectasis (65%), and endobronchial FB artifact (65%) were detected in thorax CT images of 32 cases accessible from hospital records. Although the thorax CT reports of 6 (19%) cases were reported as normal, after detailed reevaluation of the images it was found that there was FB artifact, and the thorax CT report was written as normal. FB artifact was detected in 10 (55.5%) cases when thorax CT images of 18 subjects who were reported as normal, and no FB artifact was detected on chest radiographs that were evaluated. Radiologic findings on posteroanterior chest radiograph were evaluated by age (P = .74), comorbid disease (P = .06), sex (P = .94), respiratory symptoms (P = .68), and respiratory system examination findings (P = .16). No associations were found between smoking history (P = .44), organic/inorganic material (P = .67), presence of granulation tissue (P = .25), and FB location in the left/right main bronchus system (P = .41), with no statistically significant result detected. There was no significant difference between the presence of organic or inorganic FB and the radiologic findings of either consolidation or atelectasis on the thoracic CT (P = .76). Table 2 shows the distribution of foreign thorax CT and chest radiograph findings. Both organic and inorganic materials were mostly detected in the right bronchial system and most frequently in the right lower lobe (Fig. 2). The distribution and granulation rates of the FB in the bronchial system are given in Table 3.
Table 2.
Thorax Computed Tomography Findings and Posteroanterior Chest Radiograph Findings
Figure 2.
Distribution of the foreign bodies in the bronchial system.
Table 3.
Distribution of the Foreign Body in the Bronchial System, Distribution According to the Material, and Granulation Tissue Ratios
Histopathologically, 38 (85%) of 45 subjects had granulation tissue around the FB. When the formation of granulation tissue was evaluated, no statistically significant difference was found for type of material (organic vs inorganic, P = .46), FB location (right or last main bronchus, P = .10), sex (P = .98), comorbidities (P = .77), smoking history (P = .96), or age (P = .39).
Discussion
As FBA generally causes acute, life-threatening partial or complete obstruction of the airways, especially in childhood, it causes admission to the emergency department. However, it progresses rather differently in adult patients. In particular, late-diagnosed FBA cases are seen more frequently in childhood due to insufficient anamnesis but are not very common in adults due to the presentation to health institutions after aspiration.1,3 In healthy adult individuals, especially when the anamnesis was deepened, it was found that some of these cases had a history of aspiration in childhood. Late diagnosis of FBA is more common in patients with developmental disorders, behavioral-health disorders, Alzheimer’s disease, and a history of alcohol abuse.5 Though, in our study, there were no cases related to ethyl alcohol or behavioral health issues. On the other hand, there were 5 tracheostomized subjects. In our study, the mean age of late-diagnosed FBA subjects was 53 y, and it was found to be similar to early-diagnosed FBA cases. Therefore, we infer that advanced age alone is not a risk factor by itself for FBA.6
The symptoms of FBA depend on the degree of obstruction, the duration, and location of the FB in the airway. FBA in children is a potentially life-threatening event with airway obstruction followed by shortness of breath. In contrast, the clinical presentation of FBA in adults is often subtle. Therefore, symptoms seen in other diseases such as chronic cough, fever, chest pain, and hemoptysis due to distal obstruction of the lower airways are observed. Rarely, adults experience acute suffocation from FBA followed by upper-airway obstruction. Acute or chronic cough occurs in 80% of all cases.7 When FBA is suspected in the lower respiratory tract, the first imaging to be performed is direct chest radiograph. If negative, thoracic CT may be performed for further evaluation. Clinical experience shows that the sensitivity of chest radiograph in adults is low.8 Because of its better resolution, CT is more sensitive than chest radiography in detecting FBs. However, it cannot easily distinguish FB from inflammation or malignancy. Although unproven or not routine, 3-dimensional imaging (called virtual bronchoscopy) in multi-detector, multi-slice CT has been used to enhance the detection of FBs in the airway.9 Long-standing FBs may present with signs and symptoms that mimic both benign and malignant diseases (for example, unexplained dyspnea or unilateral wheezing mimicking atypical asthma). Generally, laryngoscopy (direct or oropharyngeal) or bronchoscopy is used to see an FB in the upper airway (above the vocal cords), and bronchoscopy (flexible or rigid) is used for FBs in the lower airway. In non–life-threatening FBAs, early diagnostic flexible bronchoscopy is indicated in patients without signs or symptoms of acute asphyxia. Even in patients with stable breathing, it is recommended to have advanced airway devices and RB for resuscitation and airway management during bronchoscopy due to accidental dislocation of the FB. In adults, the success of flexible bronchoscopic extraction ranges from 60–90%. The oral approach is preferred because the FB is more easily removed than the nasal passage. Depending on the size, shape, weight, and nature of the FB, many retraction equipment, including forceps, fishing-net baskets, magnet-tipped probes, basket baskets, and cryoprobes, are used with flexible bronchoscopy. If a granulation tissue surrounds the FB, which firmly attaches to the airway wall and makes extraction difficult, laser, argon plasma, or electrocautery to release the FB is applicable. However, precautions should be taken to prevent these applications from coming into contact with the normal airway mucosa or the FB itself. The rigid bronchoscope provides excellent access to the central airways. Forceps, vacuum catheters, and even the flexible bronchoscope can pass through RB. Because the FB removal procedure is usually short lived, it can be performed under general anesthesia with short-acting intravenous agents such as propofol. Rigid forceps are used to grasp large, central FBs during RB.
In our study, in accordance with the literature, 71% of the subjects were male.7,10-12 Although there is no sex difference is anonymized data shared from the United States,6 it was reported that it is more common in females in another study.13 Similar to studies conducted in children and adults, the most common symptom in our subjects was cough (62%) followed by shortness of breath (42%).6,10,14 Whereas factors such as alcohol and sedative substance use, neurodegenerative diseases, and trauma, which are risk factors for FBA in adult subjects, were not detected, the most common comorbid disease was hypertension; 5 subjects had tracheostomy, and 5 subjects had dental prosthesis.15 In a study that included 23 subjects, the rate of late diagnosis was reported as 58%,5 but we found this in less than 20% of our subjects. We think that this variance is due to the higher number of cases and the inclusion of only postoperative cases in the aforementioned study. In a pediatric study, the rate of subjects with a diagnosis delayed for > 1 month was found to be 27%.10 We believe that the difference is due to the inability to obtain aspiration history in pediatric subjects. In addition, 24% of our subjects were found to have a history of aspiration in the anamnesis retaken after bronchoscopy, and that shows that the history of aspiration should be questioned in the anamnesis in the adult subject group.
Similar to the study of Duan et al,5 in our study the estimated duration of the FB in the bronchial system was found to be 22 months on average in subjects with late diagnosis. The subjects had similar symptoms for many years and comorbid conditions with similar symptoms such as COPD and bronchiectasis. It may indicate that the accurate history has been overlooked since aspiration tends to have been experienced by these adults years ago. When questioned retrospectively, it found that there is an actual history of aspiration in 24% of the subjects. It should be pointed out that when thoracic CT reports and images of 6 subjects were evaluated it was observed that although there was endobronchial FB artifact in radiological images FB artifact failed to be noticed and was thus reported as normal. We believe that this is again caused by long duration of between the 2 occurrences.
In a study performed in the emergency department, the rate of FB detection in posteroanterior chest radiograph was 22%, whereas in our study 86% of posteroanterior chest radiograph had pathological findings, and 6.7% of them had FB artifacts.16 We think that the difference may be related to another study conducted in the emergency department where the subject group applied immediately after aspiration. The type, amount and nature of the aspirated material, and the location of the FB in the tracheobronchial system were also important for the aforementioned variance between results. In another study, it was reported that FB could not be detected between 8–80% in posteroanterior chest radiograph.17 In a 2014 study, FB artifact was found in 6.4% on posteroanterior chest radiograph.5 There were pathological findings in thorax CT scans, and FB artifact was present in 75% of them. All of the FB artifacts observed in the posteroanterior chest radiograph were found to be caused by inorganic (radiopaque) material, and 13 (52%) of the subjects with FBs on thorax CT were found to be inorganic and 12 (48%) organic material. In our study, consolidation and atelectasis were found most frequently in posteroanterior chest radiograph; and FB artifact, consolidation, and atelectasis in thorax CT, in line with the literature.16,18,19 Although thoracic CT is more sensitive than chest radiography, it is still not specific. In our study, similar findings were found with radiological findings of early-diagnosis FBA; and unlike early-diagnosis FBA, air trapping was not observed. In addition, we observed that endobronchial lung cancer image was formed in thorax CT findings originating from granulation tissue, which developed differently from early-diagnosis FBA; these expressions were included in one of the reports, and an FB was detected while the subjects were being examined especially for lung cancer. We propose that in subjects with a history or suspected FBA subjects should be evaluated with thorax CT even if the posteroanterior chest radiograph findings seem normal. In addition, since 18% of the cases have FB artifact on thorax CT images, but they are reported as normal in thorax CT reports, we suggest that clinicians should not make a decision based on thorax CT reports alone, should definitely evaluate thorax CT radiological images.
FOB has a 90% success rate in early-diagnosis FBAs. It is primarily preferred because it is easily accessible in the early period; does not require general anesthesia; can be performed on an out-patient basis; is common and accessible; has a low cost; and has lower cost, mortality, and morbidity compared to RB.20-22 In our study, it was determined that the rigid bronchoscopic method (58%) was preferred primarily in late-diagnosis FBA. In our hospital, which is a reference center, subjects are evaluated primarily with FOB. It was observed that 80% of our subjects included in our study who underwent RB were previously performed FOB, the FB could not be removed from the bronchial system, and subjects with obstruction or bleeding due to granulation tissue were switched to RB. It has been determined that the extraction process by cryobiopsy is preferred in organic materials. Although FOB is a method used to detect the presence and location of FBs in the bronchial tree in the early period, it is more appropriate to perform the procedure by securing the airway with RB in subjects with respiratory distress due to airway obstruction. The place of use of the FOB should be mainly for the confirmation of this suspicion in the presence of a suspicion of FB aspiration that cannot be detected radiologically. In Figure 3, radiological and bronchoscopic images of the cinnamon stick (an organic substance) that has been in the bronchial system for 7 y are given. Figure 3A and 3B show an endobronchial FB arterial visible within the left main bronchial system. Figure 3C shows a bronchoscopic view of the FB in the left main bronchial system, and Figure 3D shows a 7-cm cinnamon stick removed.
Figure 3.
Radiological and bronchoscopic images of the cinnamon stick. A and B: Endobronchial foreign body (FB) arterial visible within the left main bronchial system; C: bronchoscopic view of the FB in the left main bronchial system; and D: a 7-cm cinnamon stick that was removed.
When the FB stays in the bronchial system for a long time, granulation tissue may develop due to mucosal hyperplasia, and sometimes the endobronchial mass may be confused with the lesion. Duan et al5 in his study it was found that granulation tissue developed in 30% of late-diagnosed cases, whereas granulation tissue developed in 85% of the cases in our study.5,15,23 There was no statistically significant difference between the FB being organic or inorganic, localized in the main bronchus or segmental areas, being in the right or left bronchial system, the stay in the bronchial system, the age of the subject, and the development of granulation.
FBA is mostly seen in the right bronchial system, since the right main bronchus is in the midline and vertical anatomically. In the study by Duan et al,5 late-diagnosis FBA was mostly found in the right bronchus (64%); and similarly in our study, it was found in the right bronchial system, especially in the right lower lobe, in 69%.
Since it was a retrospective study, our main limitation was being limited to the information accessible on the patient electronic information system. Nevertheless, although the number of subjects who could be included in the study was limited.
Conclusions
It was determined that most of the late-diagnosed FBAs were composed of organic material and were most commonly localized in the right lower lobe. Due to the limited number of subjects, no significant difference was found between the groups regarding the location of the FB, the type of material, and the formation of granulation tissue in the statistical evaluation. We think that FBA should be kept in mind in patients who are admitted to the hospital frequently due to recurrent infections and have an endobronchial mass lesion image on thorax CT. Larger series and prospective studies should be planned to investigate the underlying causes of granulation tissue formation and late diagnosis.
Footnotes
The authors have disclosed no conflicts of interest.
REFERENCES
- 1. Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest 1999;115(5):1357–1362. [DOI] [PubMed] [Google Scholar]
- 2. Hussain M, Naqvi SMA. Experience of foreign body removal by flexible bronchoscopy in tertiary care hospital. J Post Grad Med Inst 2019;33:237–241. [Google Scholar]
- 3. Oğuzkaya F, Akçali Y, Kahraman C, Bilgin M, Sahin A. Tracheobronchial foreign body aspirations in childhood: a 10-year experience. Eur J Cardiothorac Surg 1998;14(4):388–392. [DOI] [PubMed] [Google Scholar]
- 4. Hewlett JC, Rickman OB, Lentz RJ, Prakash UB, Maldonado F. Foreign body aspiration in adult airways: therapeutic approach. J Thorac Dis 2017;9(9):3398–3409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Duan L, Chen X, Wang H, Hu X, Jiang G. Surgical treatment of late-diagnosed bronchial foreign body aspiration: a report of 23 cases. Clin Respir J 2014;8(3):269–273. [DOI] [PubMed] [Google Scholar]
- 6. National Safety Council (Itasca-IL, USA) [Internet]. 2020. Available from: https://injuryfacts.nsc.org.
- 7. Boyd M, Chatterjee A, Chiles C, Chin R., Jr. Tracheobronchial foreign body aspiration in adults. South Med J 2009;102(2):171–174. [DOI] [PubMed] [Google Scholar]
- 8. Martinot A, Closset M, Marquette CH, Hue V, Deschildre A, Ramon P, et al. Indications for flexible versus rigid bronchoscopy in children with suspected foreign body aspiration. Am J Respir Crit Care Med 1997;155(5):1676–1679. [DOI] [PubMed] [Google Scholar]
- 9. Tong B, Zhang L, Fang R, Sha Y, Chi F. 3D images based on MDCT in evaluation of patients with suspected foreign body aspiration. Eur Arch Otorhinolaryngol 2013;270(3):1001–1007. [DOI] [PubMed] [Google Scholar]
- 10. Goyal S, Jain S, Rai G, Vishnu R, Kamath GS, Bishnoi AK, et al. Clinical variables responsible for early and late diagnosis of foreign body aspiration in pediatrics age group. J Cardiothorac Surg 2020;15(1):271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chousein EGU, Tanrıverdi E, Turan D, Yıldırım BZ, Yılmaz S, Chousein I, et al. Management of adults with suspected foreign body aspiration. Dicle Med J 2021;48(1):99–107. [Google Scholar]
- 12. Sehgal IS, Dhooria S, Ram B, Singh N, Aggarwal AN, Gupta D, et al. Foreign body inhalation in the adult population: experience of 25,998 bronchoscopies and systematic review of the literature. Respir Care 2015;60(10):1438–1448. [DOI] [PubMed] [Google Scholar]
- 13. Özdemir C, Sökücü SN, Karasulu L, Büyükkale S, Dalar L. Eriskinde yabancı cisim aspirasyonu 28 olgunun analizi. Eurasian J Pulmonol 2015. [Google Scholar]
- 14. Bittencourt PF, Camargos PA, Scheinmann P, de Blic J. Foreign body aspiration: clinical, radiological findings, and factors associated with its late removal. Int J Pediatr Otorhinolaryngol 2006;70(5):879–884. [DOI] [PubMed] [Google Scholar]
- 15. Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med 1990;112(8):604–609. [DOI] [PubMed] [Google Scholar]
- 16. Pinto A, Scaglione M, Pinto F, Guidi G, Pepe M, Del Prato M, et al. Tracheobronchial aspiration of foreign bodies: current indications for emergency plain chest radiography. Radiol Med 2006;111(4):497–506. [DOI] [PubMed] [Google Scholar]
- 17. Zissin R, Shapiro-Feinberg M, Rozenman J, Apter S, Smorjik J, Hertz M. CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol 2001;11(4):606–611. [DOI] [PubMed] [Google Scholar]
- 18. Bai W, Zhou X, Gao X, Shao C, Califano JA, Ha PK. Value of chest CT in the diagnosis and management of tracheobronchial foreign bodies. Pediatr Int 2011;53(4):515–518. [DOI] [PubMed] [Google Scholar]
- 19. Gibbons AT, Casar Berazaluce AM, Hanke RE, McNinch NL, Person A, Mehlman T, et al. Avoiding unnecessary bronchoscopy in children with suspected foreign body aspiration using computed tomography. J Pediatr Surg 2020;55(1):176–181. [DOI] [PubMed] [Google Scholar]
- 20. Swanson KL, Prakash UBS, McDougall JC, Midthun DE, Edell ES, Brutinel MW, et al. Airway foreign bodies in adults. J Bronchology Interv Pulmonol 2003;10(2):107–111. [Google Scholar]
- 21. Debeljak A, Sorli J, Music E, Kecelj P. Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974–1998. Eur Respir J 1999;14(4):792–795. [DOI] [PubMed] [Google Scholar]
- 22. Surka A, Chin R, Conforti J. Bronchoscopic myths and legends: airway foreign bodies. Clin Pulm Med 2006;13(3):209–211. [Google Scholar]
- 23. Nakhosteen JA. Tracheobronchial foreign bodies. Eur Respir J 1994;7(3):429–430. [DOI] [PubMed] [Google Scholar]







