Abstract
Ossifying fibroma (OF) is a slow-growing benign fibro-osseous neoplasm. It is mostly odontogenic in origin, and it arises in the jaws, particularly the mandible. OF is characterized by the production of bone and cementum-like calcifications in a fibrous stroma. OF reports of the bone of the maxilla are uncommon. Diagnosing OF can be challenging due to the considerable overlap of clinico-pathological characteristics with those of other neoplasms. Herein, the authors describe a case report OF in a 26-year-old male who presented with a huge fibro-osseous tumor of the maxilla. Histopathology established the diagnosis of maxillary OF. The tumor was surgically removed via a Weber–erguson approach with satisfactory functional and cosmetic results. No recurrence has been found after one year of follow-up. Clinical, radiological, and pathological characteristics, as well as surgical treatment approaches, are further discussed. This is one of a few documented cases of maxillary OF in our setting.
Keywords: benign, fibro-osseous neoplasm, maxilla, ossifying fibroma
Introduction
Ossifying fibroma (OF) is a well-demarcated fibro-osseous lesion composed of fibrocellular tissue and mineralized material of varying appearances [1]. Maxillary OF is a relatively uncommon tumor [2]. Typically, OF occurs in the 2nd to 4th decades and shows a predilection for females. Clinically, smaller OF lesions are asymptomatic, while larger lesions, as seen in our patient, present as painless swelling that causes jaw expansion, facial asymmetry, and tooth divergence [3]. OF lesions are circumscribed, grow slowly, but can reach a considerable size if left untreated. An extension to the nasal septum, orbital floor, and infraorbital foramen can be seen in larger lesions [3]. Rarely, OF is associated with the destruction of extraosseous soft tissue components [4]. The tumor rarely recurs after adequate surgical treatment. A case study of maxillary OF in a young adult male that was successfully treated at our institution is presented. A brief overview of the literature has been provided.
Case presentation
A 26-year-old male patient reported to the oral and maxillofacial unit of our institution with a chief complaint of a painless, slow-growing mass on the left side of his maxilla for three years. The lesion started as a small swelling that progressively increased in size with time, with no relieving or aggravating factors reported. There was no history of preceding trauma, loss of weight, or night sweat reported to be associated with the new growth. The patient was a non-smoker, with a healthy general condition. On examination, the patient did not have any systemic problems. There was a facial asymmetry due to the mass on his midface whose measurements were 6 by 7 cm, extending from the ala of the nose right side to the body of the zygoma bone on the same side, anterior posterior, zygomatic arch to the angle of the mouth right side, superior inferior direction (Fig. 1A). There was no enlargement of lymph nodes. Speech and swallowing remained undisturbed. On examination of the oral cavity, the mass on the maxilla, which was hard in consistency, non-tender, and measuring about 4 cm by 6 cm in its greatest dimensions, was appreciated (Fig. 1B). A clinical diagnosis of ossifying fibroma of the maxilla was considered, with a differential diagnosis of fibrous dysplasia. A CT scan of the head highlighted a well-defined expansile radiolulency mass with radiopaque features. The mass was causing bone erosion and opacification (Fig. 2A–D). Histopathology of an incisional biopsy demonstrated a benign fibro-osseous lesion composed of diffuse hyperchromatic stromal fibroblastic cell proliferation, without atypia or mitoses. The matrix was mineralized with woven and lamellar bone deposits, or cementum-like calcifications distributed throughout the lesion (Fig. 3). The diagnosis of maxillary OF was confirmed, and the treatment was scheduled.
Figure 1.

Photographs of the patient demonstrating facial asymmetry due to the maxillofacial mass extraorally (A), the mass protruding on the hard palate before surgery (B); an external appearance (C), the intraoral appearance of the patient 12 months after surgery, respectively.
Figure 2.
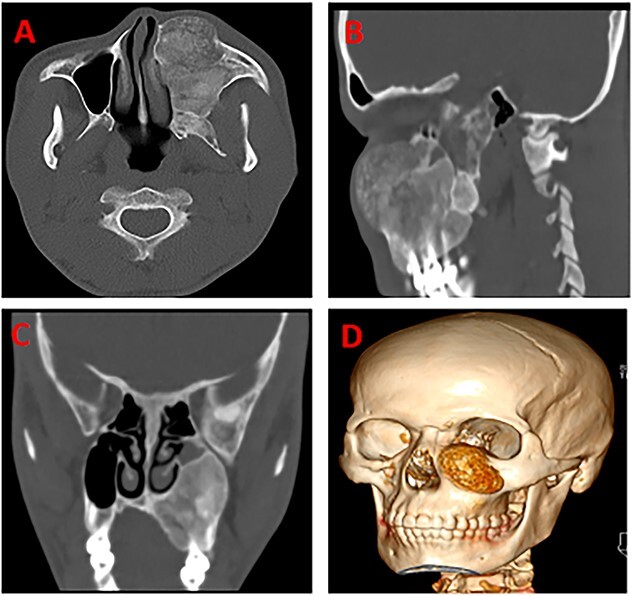
CT scans of the head highlighting a well-defined expansile radiolulency mass with radiopaque features (A), the mass is causing bone erosion (B), and opacification (C), a 3D of the tumor (D), respectively.
Figure 3.
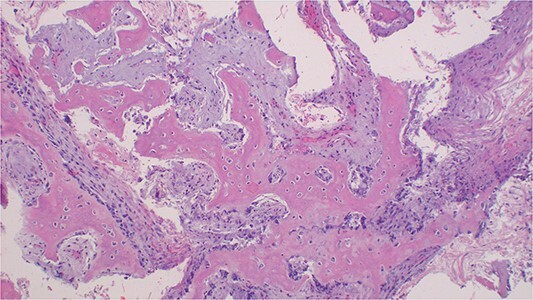
Photomicroscopy of ossifying fibroma demonstrating a benign fibro-osseous nature of the lesion composed of diffuse hyperchromatic stromal fibroblastic cell proliferation, without atypia, or mitoses. The matrix is mineralized with woven and lamellar bone deposits or cementum-like calcifications distributed throughout the lesion, H & E staining at 200 × original magnification.
Surgical procedure
The patient was planned for surgery under general anesthesia. The patient was intubated through an endotracheal tube via the nasal cavity (Fig. 4A). Under aseptic procedure, the tumor was exposed (Fig. 4B) and a complete excision was performed through a Weber– Ferguson approach (Fig. 4C). Complete tumor enucleation was done. The palatal bone, posterior and superior walls of the maxillary sinus remained intact after tumor enucleation. The surgical wound was primarily closed with the advancement of nearby muscles and skin in layers in a water tight fashion (Fig. 4D). The patient’s postoperative course was uneventful. Histopathology findings of the excised lesion were consistent with those from the previous incisional biopsy. No recurrence has been observed after a follow-up of 12 months (Fig. 1C and D).
Figure 4.
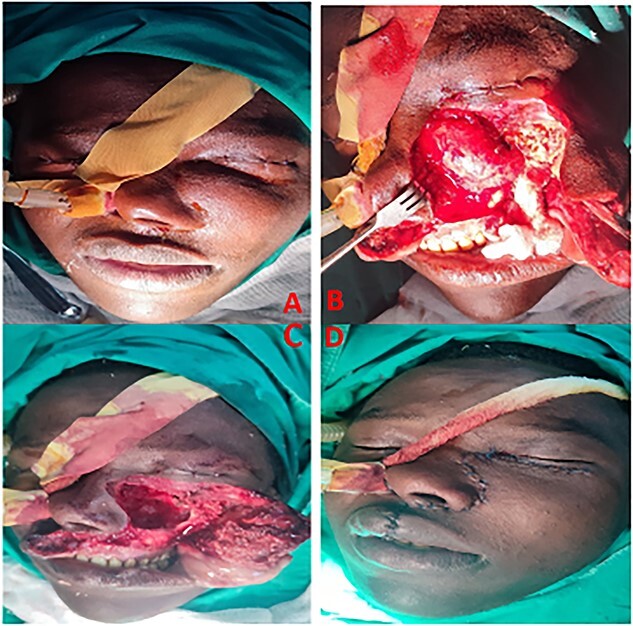
Photographs showing endotracheal intubation via the nasal cavity (A), surgical exposure of the tumor (B), and excision of the tumor through a Weber– Ferguson approach (C); the surgical wound primarily closed with the advancement of nearby muscles and skin in layers in a water tight fashion (D), respectively.
Discussion
OF case studies involving the maxilla of unusually large sizes are relatively uncommon. Several cases have been reported in English literature [3–7]. Jaw OF origin is believed to be odontogenic or from periodontal ligament progenitor cells [8]. The periodontal membrane has multipotent cells capable of forming cementum, lamellar bone, and fibrous tissue. Contrary to the index case, OF has a female predilection. Our case report showed an uncommon presentation in the anterior part of the maxilla of a 26 year old male patient. Due to the great fraction of cancellous bone and the sinus existing in the maxilla, OFs of the maxilla can enlarge and grow to huge sizes [4]. In our case, the lesion was occupying most of the anterior maxilla left side, and the patient presented with considerable clinical symptoms that included moderately facial distortion.
There are no specific laboratory tests that are available to confirm the OF diagnosis. The diagnosis is dependent on clinical, radiologic, and pathologic correlations [2]. OF is treated by enucleation and curettage, as it shells out easily and recurs rarely [3]. Untreated tumors may attain a massive size and rarely require en bloc resection [9]. To minimize the possibility of recurrence, for bigger or aggressive lesions, an enblock or partial resection of the jaw is ideal [10]. When the surgical resection is wide, added restoration using implants, obturators, or bone grafts should be considered because of functional and esthetic problems, mainly when teeth are removed from the part of the jaw bone.
In our case, the lesion was treated by enucleasion and curettage to preserve the posterior and superior walls of the maxillary sinus and palatal bone. Conservative treatment is the therapy of choice as it results in slight morbidity, no loss of sensation, no need for a bone graft, good consolidation, and faster bone formation. Radiotherapy should be considered in patients for whom reexcision after a recurrence would result in unacceptable morbidity [11]. The prognosis is favorable with no recurrence in majority of cases.
Conclusion
Maxillary ossifying fibromas with large sizes, as presented in our case, are uncommon and may pose treatment challenges. It may complicate surgical procedures, postoperative complaints, or prosthetic needs. Postoperative follow-up is essential, especially in cases where incomplete removal was performed. Patients should be instructed not only about the importance of early detection of the lesion but also about the necessity of routine, periodic check-ups for the avoidance of recurrence or future complications after treatment.
Acknowledgements
The authors would like to thank Dr Rwakatema, Dr Jackson Mariki and Dr Calvin Baraka, department of dentistry of KCMC.
Contributor Information
Kanankira A Nnko, Department of Dental Surgery, Kilimanjaro Christian Medical Centre, Box 3010, Moshi, Tanzania; Faculty of Medicine, Kilimanjaro Christian Medical University College, Box 2240, Moshi, Tanzania.
Raphael T Pima, Department of Dental Surgery, Kilimanjaro Christian Medical Centre, Box 3010, Moshi, Tanzania.
Sosthenes Damas, Department of Dental Surgery, Kilimanjaro Christian Medical Centre, Box 3010, Moshi, Tanzania.
Alex Mremi, Faculty of Medicine, Kilimanjaro Christian Medical University College, Box 2240, Moshi, Tanzania; Department of Pathology, Kilimanjaro Christian Medical Centre, Box 3010, Moshi, Tanzania.
Author contributions
Kanankira A Nnko (Conceptualization; data curation; writing –original draft), Raphael T Pima (Data curation; writing –original draft), Sosthenes Damas (Data curation; writing –review and editing), Alex Mremi (Conceptualization; investigation; writing –original draft; writing—review and editing).
Conflict of interest statement
All authors have declared that no competing interests exist.
Funding
This work did not receive any fund from any source.
Data availability
There is no data generated from this study.
Ethics statement
The patient provided written informed consent to allow for his de-identified medical information to be used in this publication. A waiver for ethical approval was obtained from the authors’ institutional review board committee.
Consent
Written informed consent for publication of clinical details and images was obtained from the patient.
References
- 1. Jih MK, Kim JS. Three types of ossifying fibroma: a report of 4 cases with an analysis of CBCT features. Imaging Sci Dent 2020;50:65–71. https://doi.org/doi: 10.5624/isd.2020.50.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Phattarataratip E, Pholjaroen C, Tiranon P. A clinicopathologic analysis of 207 cases of benign fibro-osseous lesions of the jaws. Int J Surg Pathol 2014;22:326–33. https://doi.org/doi: 10.1177/1066896913511985. [DOI] [PubMed] [Google Scholar]
- 3. Agarwal SP, Kumar S, Singh HP, et al. Huge ossifying fibroma maxilla. Natl J Maxillofac Surg 2015;6:241–3. https://doi.org/doi: 10.4103/0975-5950.183862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bhat SV, Kumar SP, Periasamy S, et al. An uncommon presentation of ossifying fibroma in the maxilla. Cureus 2022;14:e23638. https://doi.org/doi: 10.7759/cureus.23638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Liu JJ, Thompson LD, Janisiewicz AM, et al. Ossifying fibroma of the maxilla and sinonasal tract: case series. Allergy Rhinol (Providence) 2017;8:32–6. https://doi.org/doi: 10.2500/ar.2017.8.0190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vura NG, Gaddipati R, Ramisetti S, et al. Surgical management of ossifying fibroma in maxilla: report of two cases. J Int Oral Health 2015;7:115–8. [PMC free article] [PubMed] [Google Scholar]
- 7. Shetty SK, Dasukil S, Arora G. Aggressive ossifying fibroma of the maxilla. Ann Maxillofac Surg 2020;10:262–6. https://doi.org/doi: 10.4103/ams.ams_121_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Collins LHC, Zegalie NFT, Sassoon I, et al. A clinical, radiological and histopathological review of 74 ossifying fibromas. Head Neck Pathol 2023;17:433–46. https://doi.org/doi: 10.1007/s12105-022-01522-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. MacDonald-Jankowski DS. Ossifying fibroma: a systematic review. Dentomaxillofac Radiol 2009;38:495–513. 10.1259/dmfr/70933621. [DOI] [PubMed] [Google Scholar]
- 10. Nnko KA, Rwakatema DS, Mariki JM, et al. Massive ossifying fibroma of mandible: a case report and review of the literature. Clin Case Rep 2023;11:e7950. https://doi.org/doi: 10.1002/ccr3.7950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Strickler S, Hitchcock KE, Dziegielewski PT, et al. Radiotherapy for juvenile ossifying fibroma of the maxillary sinus: case report and literature review. Head Neck 2017;39:E81–4. 10.1002/hed.24811. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
There is no data generated from this study.


