Abstract
Uganda is highly vulnerable to public health emergencies (PHEs) due to its geographic location next to the Congo Basin epidemic hot spot, placement within multiple epidemic belts, high population growth rates, and refugee influx. In view of this, Uganda’s Ministry of Health established the Public Health Emergency Operations Center (PHEOC) in September 2013, as a central coordination unit for all PHEs in the country. Uganda followed the World Health Organization’s framework to establish the PHEOC, including establishing a steering committee, acquiring legal authority, developing emergency response plans, and developing a concept of operations. The same framework governs the PHEOC’s daily activities. Between January 2014 and December 2021, Uganda’s PHEOC coordinated response to 271 PHEs, hosted 207 emergency coordination meetings, trained all core staff in public health emergency management principles, participated in 21 simulation exercises, coordinated Uganda’s Global Health Security Agenda activities, established 6 subnational PHEOCs, and strengthened the capacity of 7 countries in public health emergency management. In this article, we discuss the following lessons learned: PHEOCs are key in PHE coordination and thus mitigate the associated adverse impacts; although the functions of a PHEOC may be legalized by the existence of a National Institute of Public Health, their establishment may precede formally securing the legal framework; staff may learn public health emergency management principles on the job; involvement of leaders and health partners is crucial to the success of a public health emergency management program; subnational PHEOCs are resourceful in mounting regional responses to PHEs; and service on the PHE Strategic Committee may be voluntary.
Keywords: Public Health Emergency Operations Center, Uganda, Public Health Emergencies, Infectious Diseases Outbreaks, Epidemic Preparedness and Response
Introduction
The World Health Organization (WHO) established the Public Health Emergency Operations Center (PHEOC) Network in 2012, aiming to enhance global collaboration for prevention, early detection, and rapid response in public health emergencies (PHEs).1 PHEs present in the form of adverse health conditions caused by disease outbreaks, pandemics, bioterrorism, infectious agents, or biological toxins, which pose a substantial risk to human lives including death. The establishment of the PHEOC Network was in line with the requirements of the second edition of the International Health Regulations (2005).2 PHEOCs had existed earlier in some countries, although there was a need to harmonize their mode of operation in light of fast-spreading PHEs globally. Subsequently, WHO released a framework for PHEOCs as guidance for the harmonization process.3
Uganda is highly vulnerable to PHEs for several reasons, including its proximity to the ecologically biodiverse rich tropical Congo Basin—a known reservoir of infectious pathogens; location within mapped endemic areas of meningitis, flaviviruses (eg, yellow fever, Zika virus), filoviruses (eg, Marburg virus, Ebola virus); high population growth; and high refugee influx. These factors work in combination with other social and environmental factors to amplify Uganda’s vulnerability to PHEs.4
Before 2013, Uganda’s Ministry of Health (MOH) responded to several infectious disease outbreaks, including Ebola virus disease, yellow fever, meningitis, typhoid, anthrax, cholera, and Marburg virus disease.5–11 Although these outbreaks were eventually controlled, they were characterized by high morbidity and mortality due to late detection, slow response, and lack of central coordination, command, and control structures. Moreover, little attention was paid to the systematic documentation of response mechanisms and other vital aspects of these outbreaks, which are useful in informing future responses. In 2013, the MOH undertook a collaborative proof-of-concept demonstration project together with the US Centers for Diseases Control and Prevention (CDC), to assess effective approaches to PHEs. Detailed results of this project are documented elsewhere.12 Briefly, the project recommended the establishment of a national PHEOC; nationwide mechanisms for sample collection, transportation, and testing; and real-time sharing of information about outbreaks. In this article, we document how the Uganda PHEOC was established as well as its achievements, challenges encountered, and lessons learned between January 2014 and December 2021.
Establishing the PHEOC
The Uganda MOH established the national PHEOC in September 2013, following the WHO framework for PHEOCs.3 Under this framework, establishing and operating a PHEOC entails instituting a steering committee, establishing legal authority, developing emergency response plans, and developing a concept of operations. Core components of a PHEOC include plans and procedures, physical infrastructure, information systems, information and communication technology infrastructure, and human resources.
Scope of Operation
Uganda’s emergency management program is governed by the National Policy for Disaster Preparedness and Management (2011).13 Under this policy, whereas the Office of the Prime Minister is vested with the mandate to respond to every natural disaster, MOH responds to PHEs as a delegated function. Uganda thus established 2 national emergency operations centers: the National Emergency Coordination and Operations Center at the Office of the Prime Minister, and the PHEOC at the MOH. The PHEOC’s mandate is to serve as the MOH’s focal point for organizing, coordinating, conducting, and managing all aspects of PHE response efforts, while using resources in a coordinated, collective, and collaborative manner.
Steering Committee
The National Task Force (NTF) is a multidisciplinary and multisectoral body of policy and decisionmakers, vested with the authority to provide strategic directions for managing and controlling PHEs. The NTF is supported by a team of subject matter experts drawn from a wide spectrum of specialties including academic institutions, government ministries, health partners, United Nations organizations, and community-based organizations. Depending on their specialties, subject matter experts serve under 1 or more of 9 NTF subcommittees: Coordination, Surveillance, Laboratory, Risk Communication, Case Management, Logistics, Vaccination, Community Engagement, and Strategic Innovation. Service on the NTF is largely voluntary and attracts no financial gains. The NTF is chaired by the MOH Director General of Health Services or the Director of Animal Resources at the Ministry of Agriculture, Animal Industries and Fisheries.
During NTF coordination meetings, response updates from the affected district(s) are presented, which inform strategic decisions for response. All strategic, contingency, and response plans are reviewed, approved, and implemented at the NTF level. The NTF is also responsible for mobilizing both preparedness and response resources (financial and human) for all PHEs in the country and establishing or strengthening cross-border collaborations in PHE surveillance and response.
Structures that are similar to the NTF exist at subnational levels in the form of district task forces, whose technical arms are the district health teams. District task forces become activated whenever an outbreak is declared in their respective districts.
Physical and Structural Location
The PHEOC basic infrastructure was established between September 2013 and March 2014, including renting office space near the MOH, procuring equipment and furniture, setting up communication systems, and hiring and training staff in public health emergency management (PHEM) principles. The PHEOC offices comprise workstations for staff and the Incident Management Team, a PHEOC manager’s cubicle, and a boardroom.
Figure 1 shows the linkages between Uganda’s actors in PHE detection and response. Structurally, the PHEOC is placed within the MOH’s organogram as a unit under the Department of Integrated Epidemiology, Surveillance and Public Health Emergencies. Thus, the PHEOC is equally involved in the surveillance and epidemiology functions of MOH and conducts indicator- and event-based surveillance for epidemic-prone diseases. Furthermore, the PHEOC works with Uganda’s Public Health Fellowship Program14 and the One Health Coordination Office.
Figure 1.
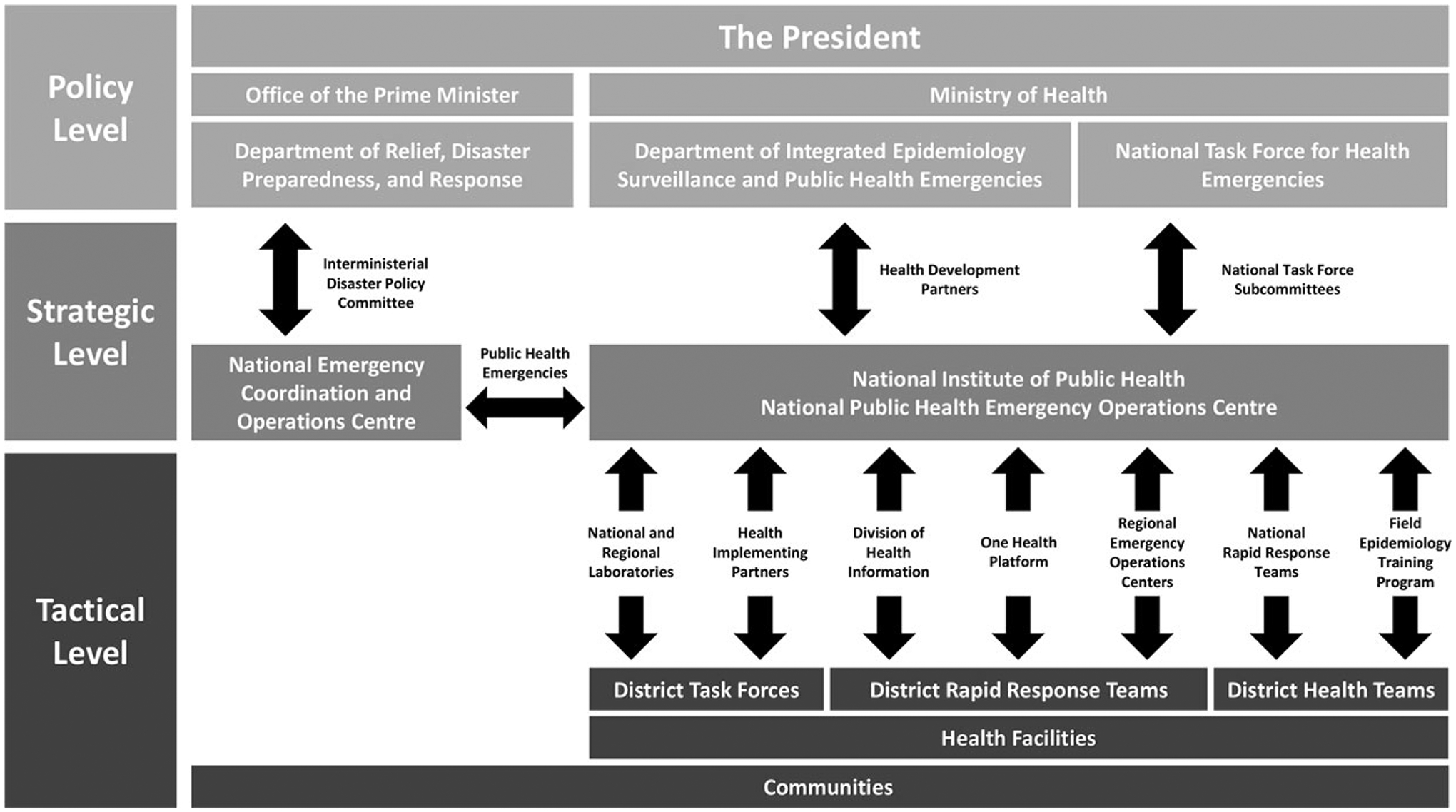
Linkages among public health emergency preparedness and response actors in Uganda.
Legal Framework
Although established in September 2013, the PHEOC’s legal framework was not secured until November 2019, following a presidential directive to establish Uganda’s National Institute of Public Health. The National Institute of Public Health brings together 4 actors in public health: Public Health Fellowship Program, PHEOC, National Health Laboratory Services, and Division of Health Information (Figure 1). Following recommendations of the 2017 Joint External Evaluation (JEE) of Uganda’s International Health Regulations Core Capacities,15 revisions of the current Public Health Act (1935)16 are being undertaken to incorporate sections that legalize National Institute of Public Health’s functions including the PHEOC.
Plans and Procedures
The PHEOC functions are governed by a set of plans, which are annexed to the country’s internal national multihazard emergency preparedness and response plan. Existing hazard-specific contingency plans include rabies, anthrax, plague, pandemic influenza, viral hemorrhagic fevers, cholera, brucellosis, meningitis, yellow fever, and antimicrobial resistance. All of these plans have been validated either in real-life PHE responses and/or through simulation exercises. Standard operating procedures and an internal handbook were developed to further govern the PHEOC’s daily operations. A concept of operations also exists, describing the roles and responsibilities of different stakeholders and how they should interact to achieve unity of purpose during PHE responses.
Both the National Multi-Hazard Emergency Preparedness and Response Plan and PHEOC handbooks have been validated in simulation exercises. Furthermore, the PHEOC organizes and coordinates after-action reviews following major activations to further test and improve the validity of these plans and procedures.
PHEOC Activations
The PHEOC is always in PHE “watch” mode. “alert” or “response” modes are activated by the director general of health services or the PHEOC director upon confirmation of any PHE. The processes leading to PHEOC activation are governed by the alert and response thresholds outlined in Uganda’s internal technical guidelines for Integrated Diseases Surveillance and Response (IDSR). Upon activation, each incident is given a unique identifier (eg, “Cholera Kampala Feb 2019”), whose nomenclature follows 4 parameters: causative agent, affected district, month, and year of detection.
Upon activation, the director general of health services signs a memo. The NTF then appoints an incident commander who selects an incident management team and dispatches national rapid response teams to support district rapid response teams in mounting appropriate responses. These teams then collect up-to-date information, which is provided to the NTF through the PHEOC for effective decisionmaking (Figure 1). The PHEOC further supports Uganda’s International Health Regulations focal point to notify WHO Regional Office for Africa of the PHE.
Information, Communication, and Technology Infrastructure and Systems
The PHEOC information and communication technology infrastructure includes wired and wireless internet connections, a firewall, virus-protected servers, toll-free telephone service, projectors, laptops, and TV monitors used to project up-to-date PHE information in the country, region, and world. This infrastructure has the capability of hosting both in-house and online coordination meetings, which proved helpful during the COVID-19 pandemic lockdowns and social distancing restrictions.
The PHEOC uses 2 major systems for information acquisition and sharing: the electronic IDSR17,18 and the virtual emergency operations center. The electronic IDSR collects and disseminates information on both immediate and notifiable conditions as guided by IDSR. Main applications of the virtual emergency operations center system include sharing outbreak situation updates, relaying laboratory results from central laboratories to requesting clinicians, managing the subject matter expert database, scheduling and coordinating NTF/Incident Management Team meetings, and tracking action points. Other systems used in conducting event-based surveillance include the WHO Epidemic Intelligence from Open Sources system, U-Report, mTrac, TweetDeck, Google alerts, ProMED, Global Public Health Intelligence Network for early outbreak detection, HealthMap, email exchanges, and a toll-free telephone line.
Human Resources
The PHEOC functions are coordinated by a team of 9 core staff, all trained in PHEM. A pool of surge staff is also available within the Integrated Epidemiology, Surveillance and Public Health Emergencies department; Public Health Fellowship Program; One Health platform; and health partners to support the incident management system functions and field deployments (Figure 1).
Achievements
Activations for Public Health Emergency Response
Between January 2014 and December 2021, the PHEOC was activated for 271 PHEs (Table), most of which were infectious diseases listed on Uganda’s IDSR priority list. Circumstances leading to PHEOC activations for conditions that are endemic in Uganda (eg, tuberculosis, malaria, typhoid) are defined by IDSR thresholds. The PHEOC was also activated for some landslide events because of the public health component associated with their occurrence, and preparedness to cross-border events such as Ebola and plague originating from the Democratic Republic of Congo. Additionally, the PHEOC has been activated for the elimination of mother-to-child transmission of HIV and annual mass gatherings that represent substantial risks of PHE importation and spread.19
Table.
Uganda PHEOC Activations, January 2014 to December 2021
| Public Health Emergency | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Anthrax | Number of activations | 0 | 0 | 0 | 2 | 3 | 3 | 1 | 1 | 10 |
| Districts affected | – | – | – | 2 | 3 | 3 | 1 | 2 | 11 | |
| Suspected human cases | – | – | – | 62 | 160 | 22 | 9 | 29 | 282 | |
| Confirmed human cases | – | – | – | 6 | 8 | 9 | 0 | 0 | 23 | |
| Confirmed human fatalities | 1 | 0 | 0 | 0 | 1 | 2 | ||||
| Bilharzia/schistosomiasis | Number of activations | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Districts affected | – | – | – | 1 | – | – | – | – | 1 | |
| Confirmed human cases | – | – | – | 9 | – | – | – | – | 9 | |
| Confirmed human fatalities | – | – | – | 12 | – | – | – | – | 12 | |
| Cholera | Number of activations | 0 | 5 | 16 | 3 | 12 | 8 | 4 | 1 | 48 |
| Districts affected | – | 5 | 15 | 3 | 10 | 6 | 4 | 1 | 43 | |
| Suspected human cases | – | 583 | 1598 | 424 | 2800 | 323 | 1,269 | 173 | 6,997 | |
| Confirmed human cases | – | 131 | 225 | 54 | 424 | 86 | 34 | 7 | 954 | |
| Confirmed human fatalities | – | 15 | 38 | 5 | 59 | 4 | 7 | 0 | 128 | |
| Circulating vaccine-derived poliovirus 2 | Number of activations | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Districts affected | – | – | – | – | – | – | – | 1 | 1 | |
| Confirmed human cases | – | – | – | – | – | – | – | 3** | 3 | |
| Conjunctivitis | Number of activations | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| Districts affected | – | – | 1 | – | – | – | – | – | 1 | |
| Suspected human cases | – | – | 801 | – | – | – | – | – | 801 | |
| Confirmed human cases | – | – | 21 | – | – | – | – | – | 21 | |
| Confirmed human fatalities | – | – | 0 | – | – | – | – | – | 0 | |
| COVID-19 | Number of activations | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | |
| Districts affected | – | – | – | – | – | – | 136 | 136 | ||
| Suspected human cases | – | – | – | – | – | – | 2,166,777 | 2,166,777 | ||
| Confirmed human cases | – | – | – | – | – | – | 145,963 | 145,963 | ||
| Confirmed human fatalities | – | – | – | – | – | – | 3,306 | 3,306 | ||
| Crimean-Congo hemorrhagic fever | Number of activations | 0 | 1 | 0 | 2 | 6 | 7 | 1 | 1 | 18 |
| Districts affected | – | 1 | – | 2 | 6 | 6 | 1 | 1 | 17 | |
| Suspected human cases | – | 24 | – | 58 | 16 | 56 | 41 | 24 | 219 | |
| Confirmed human cases | – | 1 | – | 5 | 10 | 6 | 1 | 2 | 25 | |
| Confirmed human fatalities | – | 0 | – | 3 | 4 | 2 | 0 | 0 | 9 | |
| Dengue fever | Number of activations | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Districts affected | – | – | – | – | 1 | – | – | – | 1 | |
| Suspected human cases | – | – | – | – | 1 | – | – | – | 1 | |
| Confirmed human cases | – | – | – | – | 1 | – | – | – | 1 | |
| Confirmed human fatalities | – | – | – | – | 0 | – | – | – | 0 | |
| Ebola virus disease | Number of activations | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 2 |
| Districts affected | – | – | – | – | – | 1 | – | – | 1 | |
| Suspected human cases | – | – | – | – | – | 4 | – | – | 4 | |
| Confirmed human cases | – | – | – | – | – | 4 | – | – | 4 | |
| Confirmed human fatalities | – | – | – | – | – | 4 | – | – | 4 | |
| Ebola virus disease preparedness | Number of activations | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 2 | 2 |
| Districts affected | – | – | – | – | 30 | – | 30 | 30 | 60 | |
| Suspected human cases | – | – | – | – | 1072 | – | 1274 | 161 | 2,346 | |
| Influenza (H1N1, H5N8) | Number of activations | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 3 |
| Districts affected | – | 1 | – | 4 | – | – | – | – | 5 | |
| Suspected human cases | – | 37 | – | 3 | – | – | – | – | 40 | |
| Confirmed human cases | – | 24 | – | 2 | – | – | – | – | 26 | |
| Confirmed human fatalities | – | 0 | – | 1 | – | – | – | – | 1 | |
| Leptospirosis | Number of activations | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Districts affected | – | – | – | 4 | – | – | – | – | 4 | |
| Suspected human cases | – | – | – | 7 | – | – | – | – | 7 | |
| Confirmed human cases | – | – | – | 7 | – | – | – | – | 7 | |
| Confirmed human fatalities | – | – | – | 0 | – | – | – | – | 0 | |
| Marburg virus disease | Number of activations | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 |
| Districts affected | 1 | – | – | 2 | – | – | – | – | 3 | |
| Suspected human cases | 197 | – | – | 311 | – | – | – | – | 508 | |
| Confirmed human cases | 1 | – | – | 3 | – | – | – | – | 4 | |
| Confirmed human fatalities | 1 | – | – | 3 | – | – | – | – | 4 | |
| Measles | Number of activations | 0 | 8 | 5 | 11 | 50 | 25 | 8 | 0 | 107 |
| Districts affected | – | 47 | 43 | 36 | 86 | 98 | 42 | – | 352 | |
| Suspected human cases | – | 2,898 | 1,518 | 1,740 | 3,523 | 1,813 | 594 | – | 12,086 | |
| Confirmed human cases | – | 219 | 133 | 203 | 621 | 626 | 141 | – | 1,943 | |
| Confirmed human fatalities | – | 0 | 3 | 3 | 1 | 0 | 0 | – | 7 | |
| Neisseria meningitidis | Number of activations | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 3 |
| Districts affected | – | – | 1 | 1 | 1 | – | – | – | 3 | |
| Suspected human cases | – | – | 186 | 1 | 18 | – | – | – | 205 | |
| Confirmed human cases | – | – | 16 | 1 | 2 | – | – | – | 19 | |
| Confirmed human fatalities | – | – | 2 | 0 | 7 | – | – | – | 9 | |
| Plague | Number of activations | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Districts affected | – | – | – | – | – | 1 | – | – | 1 | |
| Suspected human cases | – | – | – | – | – | 2 | – | – | 2 | |
| Confirmed human cases | – | – | – | – | – | 1 | – | – | 1 | |
| Confirmed human fatalities | – | – | – | – | – | 1 | – | – | 1 | |
| Rabies | Number of activations | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| Districts affected | – | – | – | – | – | – | – | 2 | 2 | |
| Suspected human cases | – | – | – | – | – | – | – | 57 | 57 | |
| Confirmed human cases | – | – | – | – | – | – | – | 30 | 30 | |
| Confirmed human fatalities | – | – | – | – | – | – | – | 0 | 0 | |
| Rift Valley fever | Number of activations | 0 | 0 | 1 | 4 | 13 | 5 | 6 | 3 | 32 |
| Districts affected | – | – | 1 | 4 | 13 | 4 | 5 | 3 | 30 | |
| Suspected human cases | – | – | 34 | 22 | 31 | 5 | 6 | 13 | 111 | |
| Confirmed human cases | – | – | 2 | 7 | 26 | 5 | 6 | 5 | 51 | |
| Confirmed human fatalities | – | – | 0 | 5 | 13 | 3 | 4 | 3 | 28 | |
| Tuberculosis upsurge | Number of activations | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| Districts affected | – | – | – | – | – | – | 27 | 52 | 79 | |
| Suspected human cases | – | – | – | – | – | – | 13,054 | 15,834 | 28,888 | |
| Confirmed human cases | – | – | – | – | – | – | 12,468 | 13,307 | 25,775 | |
| Typhoid upsurge | Number of activations | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 2 |
| Districts affected | – | 1 | – | – | – | – | 1 | – | 2 | |
| Suspected human cases | – | 10,230 | – | – | – | – | 11,919 | – | 22,149 | |
| Confirmed human cases | – | 51 | – | – | – | – | 217 | – | 268 | |
| Confirmed human fatalities | – | 17 | – | – | – | – | 54 | – | 71 | |
| West Nile virus | Number of activations | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Districts affected | – | – | – | – | – | – | 1 | – | 1 | |
| Suspected human cases | – | – | – | – | – | – | 1 | – | 1 | |
| Confirmed human cases | – | – | – | – | – | – | 1 | – | 1 | |
| Confirmed human fatalities | – | – | – | – | – | – | 0 | – | 0 | |
| Yellow fever | Number of activations | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 4 |
| Districts affected | – | – | 3 | – | – | 3 | 3 | 2 | 11 | |
| Suspected human cases | – | – | 65 | – | – | 9 | 34 | 3 | 111 | |
| confirmed human cases | – | – | 7 | – | – | 3 | 8 | 3 | 21 | |
| Confirmed human fatalities | – | – | 3 | – | – | 1 | 7 | 0 | 11 | |
| Food poisoning | Number of activations | 0 | 0 | 1 | 3 | 1 | 4 | 0 | 1 | 10 |
| Districts affected | – | – | 1 | 3 | 1 | 4 | – | 1 | 10 | |
| Suspected human cases | – | – | 10 | 18 | 40 | 328 | – | 22 | 418 | |
| Confirmed human cases | – | – | 8 | 14 | 15 | 6 | – | 1 | 44 | |
| Confirmed human fatalities | – | – | 3 | 4 | 0 | 6 | – | 0 | 13 | |
| Undiagnosed illness | Number of activations | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 4 |
| Districts affected | – | – | – | – | 1 | 2 | – | 2 | 5 | |
| Suspected human cases | – | – | – | – | 24 | 12 | – | 10 | 46 | |
| Confirmed human fatalities | – | – | – | – | 9 | 8 | – | 5 | 22 | |
| Landslides | Number of activations | 0 | 0 | 1 | 4 | 0 | 2 | 2 | 0 | 9 |
| Districts affected | – | – | 1 | 4 | – | 3 | 4 | – | 12 | |
| Confirmed human fatalities | – | – | 4 | 21 | – | 84 | 5 | – | 114 | |
Outbreak detected in environmental samples; no human detections made.
Exercises and Simulations
Within the observation period, PHEOC staff participated in 21 simulation exercises (Figure 2), all lasting between 1 and 3 days. Thirteen were tabletop exercises, 4 were drills, and 4 were functional exercises. Some exercises were specific to particular PHEs such as polio or Ebola virus disease preparedness, whereas others focused on validating existing plans and procedures, such as the PHEOC handbook and the National Multi-Hazard Emergency Preparedness and Response Plan.
Figure 2.
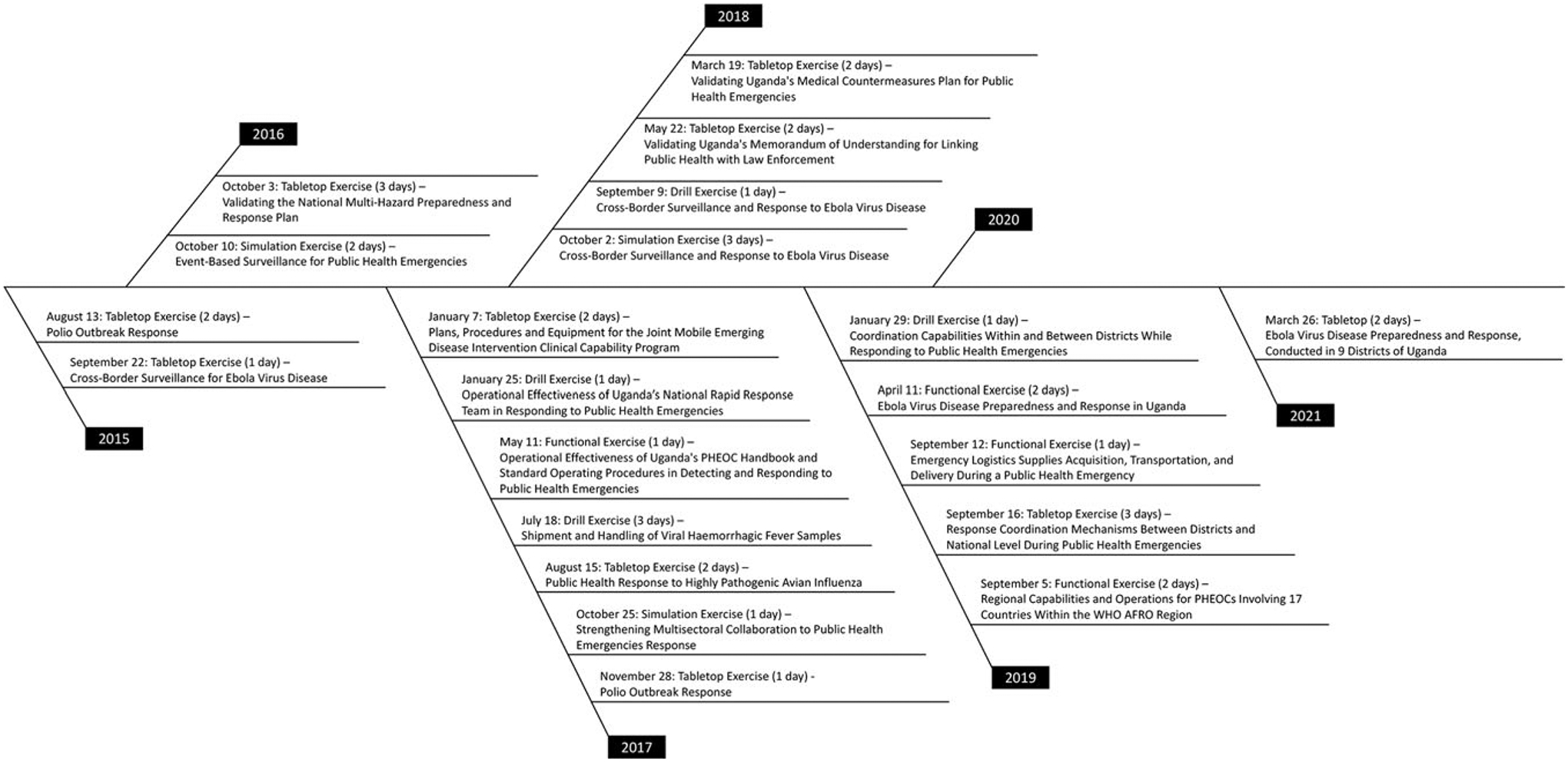
Simulation exercises in which Uganda’s PHEOC staff have participated between January 2014 and December 2021. Abbreviations: PHEOC, Public Health Emergency Operations Center; WHO AFRO, World Health Organization Regional Office for Africa.
Hosting National Task Force Coordination Meetings
The PHEOC hosted a total of 207 NTF coordination meetings between January 2014 and December 2021 (Figure 3). Two of these meetings were conducted at the Ministry of Agriculture, Animal Industries and Fisheries; 163 meetings were conducted at the MOH; and 42 meetings were hosted virtually. All meetings had an average attendance of 63 individuals, composed of human, animal, and environmental health specialists in the spirit of One Health. The PHEOC also hosts and supports all Incident Management Team and NTF subcommittee meetings and maintains their minutes for task tracking and archival purposes.
Figure 3.
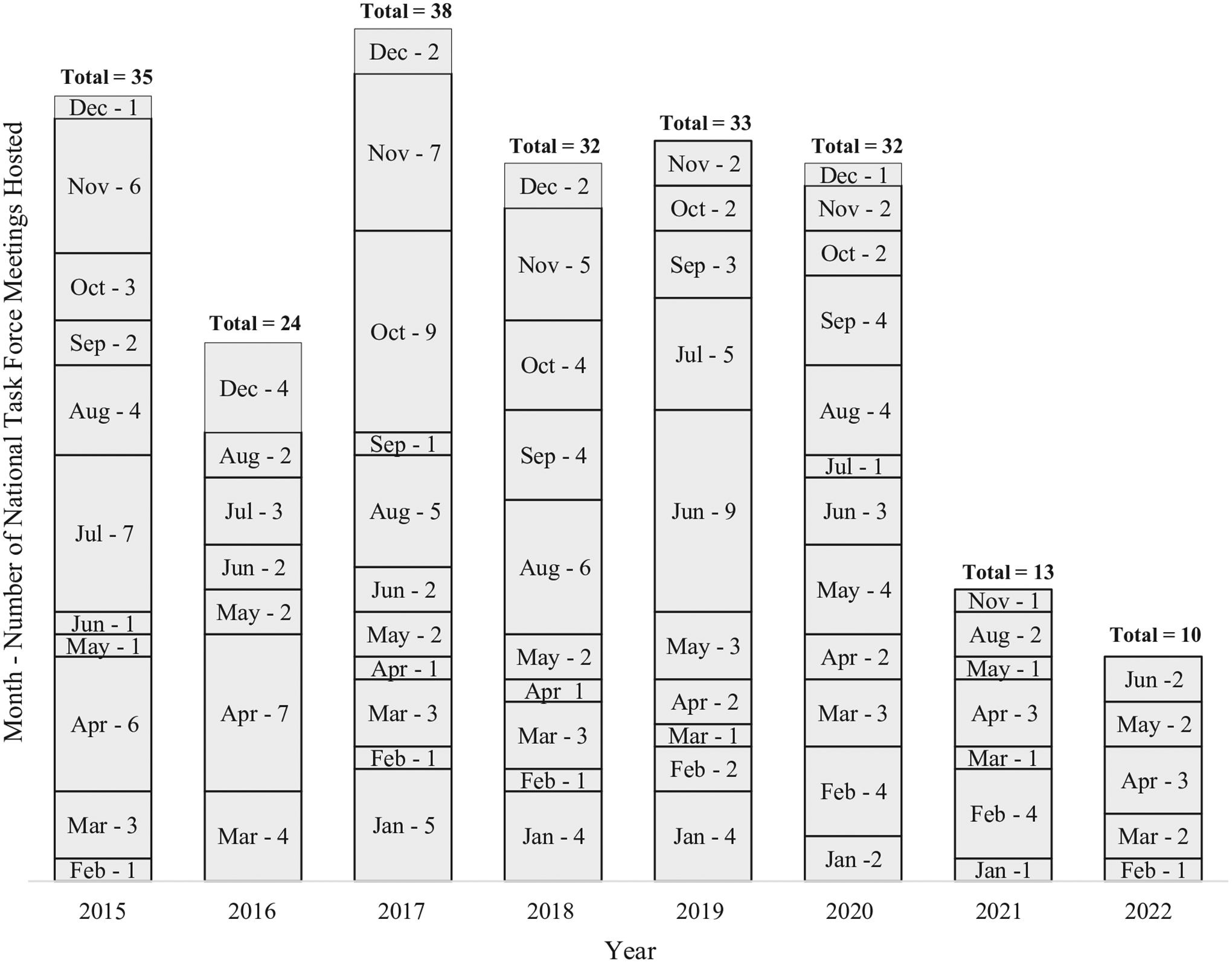
Number of National Task Force meetings convened at the PHEOC between January 2014 and December 2021. Abbreviation: PHEOC, Public Health Emergency Operations Center.
Staff Training and Continuous Learning
Five core staff members operated the PHEOC until December 2019, after which 4 additional staff joined the team. Three staff have undertaken the 4-month PHEM fellowship program offered by the US CDC in Atlanta, Georgia.20 All staff participated in a continuous, on-the-job, online training series in PHEM provided by the US Federal Emergency Management Agency, WHO, and the Africa CDC. These courses address topics including incident management system structures, PHEOC daily activities, planning and executing after action reviews and simulation exercises, PHEOC activation and deactivation, medical countermeasures in emergency situations, plans and procedures, and linkages with law enforcement authorities.
Planning, Coordinating, and Participating in After-Action Reviews
Within the observation period, the PHEOC planned, coordinated, and participated in 6 major after-action reviews including those for yellow fever (2016), Marburg virus (2017), Ebola virus (2019), anthrax and Rift Valley fever (2021), and the COVID-19 Intra-Action Review (2020). PHEOC staff also undertook internal reviews of response progress for each activation during routine weekly staff meetings.
Coordinating Global Health Security Agenda Activities in Uganda
During the observation period, the PHEOC has acted as Uganda’s coordination center for Global Health Security Agenda (GHSA) activities, including:
Coordinating the JEE assessment. Uganda undertook its first JEE assessment in June 2017 to evaluate the country’s International Health Regulations core capacities, whose process and scores are documented elsewhere.15,21 A follow-up, in-country JEE was conducted in May 2021. Throughout these processes, the PHEOC acted as the JEE Secretariat and tracked action points from all preparatory engagements.
Coordinating the development and implementation of the National Action Plan for Health Security. Following the recommendations from the JEE in 2017, Uganda developed the National Action Plan for Health Security,22 which was launched in 2019 and is being implemented until 2023. The PHEOC was responsible for arranging and coordinating all meeting and writing engagements that proceeded the drafting, editing, and launching of the National Action Plan for Health Security, and it is currently responsible for coordinating all plan implementation activities.
Coordinating activities for the International Food Safety Authorities Network. Under the GHSA, the International Food Safety Authorities Network (INFOSAN)23 aims to facilitate rapid information sharing concerning food safety events between WHO member states. In Uganda, network activities were launched in 2018 and are currently coordinated at the PHEOC.
Facilitating points of entry surveillance. By June 2021, Uganda had at least 76 points of entry located in 44 districts, of which 54 are designated and 4 are classified as seclusion points. Uganda also has numerous unofficial porous entry points that facilitate movement of both people and animals across borders. All points of entry surveillance activities are coordinated at the PHEOC, including tracking and notification of highly pathogenic and potential bioterrorism hazards.
Coordinating the Private Sector Round Table forum in Uganda. The Private Sector Round Table is a global forum that mobilizes industries, philanthropies, and government agencies to invest in and promote the GHSA by preventing and mitigating PHE threats. In Uganda, the PHEOC acts as the secretariat for all Private Sector Round Table activities.
Coordinating preparatory activities for the 4th High Level GHSA Ministerial Meeting. Uganda hosted this meeting in October 2017, which attracted over 138 delegates from 41 countries. The PHEOC acted as the secretariat and coordination center for all preparatory activities, and implemented and documented the meeting discussions, declarations, and resolutions.
Tracking samples of highly pathogenic organisms. As part of the International Health Regulations (2005)2 requirement of controlling outbreaks at source, the PHEOC tracks samples of highly pathogenic nature transported from anywhere in the country through the hub system24 to selected national and regional laboratories, and relays results to requesting clinicians using the electronic IDSR and virtual emergency operations center systems.
Capacity Strengthening for Other PHEOCs and Individuals
Within the observation period, delegates from 7 countries have officially visited Uganda’s PHEOC to learn best practices in establishing and implementing a PHEM program. These included delegations from Botswana, Cameroon, The Gambia, Japan, Madagascar, Namibia, and Sierra Leone. Additionally, the PHEOC provided internship opportunities and acted as a mentorship and training center for numerous local and international professionals seeking to develop their careers in PHEM.
Establishment of Subnational PHEOCs
Uganda’s response to the COVID-19 pandemic was over-whelming, as it was the first outbreak to involve 136 districts of the country. Because of this, the MOH decentralized coordination of response activities to different regions of the country, to lessen the burden on the national PHEOC. This led to the establishment of 6 subnational PHEOCs, located in 6 of the 16 health regions of the country. Their establishment proceeded benchmarking and experience learning engagements with 4 countries that had already established regional mechanisms to PHEs: Ethiopia, Gambia, Nigeria, and Senegal. Even though the initial establishment was inspired by response to the COVID-19 pandemic, their scope of work currently extends to cover surveillance and response to all priority conditions listed in Uganda’s IDSR framework.
Discussion
Uganda’s MOH was able to mount successful responses to PHEs prior to the establishment of the PHEOC in 2013. This was made possible due to established surveillance and response structures under the IDSR framework and established partnerships. Responses to these PHEs, however, was associated with the lack of a central coordination facility to formally bring together partners and document response efforts to inform future responses. The initiative to establish the Ugandan PHEOC followed recommendations of a successful GHSA demonstration project in 2013.12 Formally established in September 2013, operationalization of the PHEOC has been gradual thereafter, as guided by the WHO PHEOC framework.3 Among the successes registered between January 2014 and December 2021 are: being activated to respond to 271 PHEs, hosting and tracking action tasks for 207 NTF coordination meetings, training all 9 staff in PHEM, participating in 21 simulation exercises, coordinating GHSA activities in the country, establishing 6 subnational PHEOCs, and providing PHEM capacity strengthening for 7 countries.
Several studies have been published on the PHEs for which the PHEOC has been activated for coordination, including outbreaks of Marburg virus,25–27 Ebola virus,28 cholera,29,30 measles,31–34 anthrax,35–38 plague,39 food poisoning,40–42 malaria,43,44 influenza,45,46 typhoid,47,48 and Ebola preparedness.28,49 Most of these outbreaks were controlled at the source, and morbidity and mortality per PHE have been low, with the exception of the COVID-19 pandemic (Table). The PHEOC sometimes becomes activated for selected natural disasters, such as landslides and mass gathering events, because of the public health component associated with their occurrence.
The success registered in coordinating PHE preparedness, detection, and response may be partly attributed to the strong surveillance linkages between national and community levels (Figure 1). The PHEOC maintains an updated database for all district health team contacts, who are trained in IDSR and can be called upon at any time to validate any signal in the community. While responding to the COVID-19 pandemic, MOH decentralized coordination mechanisms to outbreaks by establishing 6 subnational PHEOCs.
Strong collaborative mechanisms also exist between MOH and health partners at national and subnational levels. The placement of the PHEOC within the MOH Department of Integrated Epidemiology, Surveillance and Public Health Emergencies ensures collaboration and availability of trained workforce to validate potential threats and mount timely responses. Other sources for a trained and ready-to-deploy workforce include epidemiologists from the Public Health Fellowship Program,14 the One Health platform, and national and international health partners. All national rapid response team and district rapid response team members have been trained in outbreak preparedness and response under IDSR, and these skills are regularly rehearsed in real-life outbreaks or simulation exercises. This may explain the finding that, despite its high vulnerability to PHEs, Uganda has managed to control most outbreaks at the source and reduce the number of human lives affected (Table).
PHEOC staff have participated in several simulation exercises (Figure 2) as part of sharpening their skills. These exercises were undertaken in collaboration with partners including WHO, US CDC, Food and Agriculture Organization of the United Nations, and Africa CDC. PHEOC staff also undertake reviews of each activation during weekly staff meetings, to develop improvement plans. Additionally, after-action reviews are conducted following deactivation from major responses, with attendance from all actors involved in the responses. This helps reflect on what went well or wrong, and what can be improved for future responses.
The main challenge faced by Uganda’s PHEOC during the study period is that most of its activities have been funded by health partners, which is a threat to sustainability. The thin structure of the core PHEOC staff vis-à-vis its activities poses additional challenges, as staff are strained between the PHEOC’s core functions including routine surveillance, signal and alert monitoring, PHE activations and responses, coordination of GHSA activities, ensuring continuous learning through training, and simulation exercises. Similar challenges also exist within the already established 6 subnational PHEOCs.
Lessons Learned
Several lessons have been learned. First, any country can establish a PHEOC before securing its formal legal recognition. This can be done in “good faith,” with the aim of protecting citizens from PHEs, since legalization usually takes time. In Uganda’s experience, it took at least 6 years to secure this legal framework. If the MOH had waited that long before establishing an operational PHEOC and effective PHEM systems, effective coordination to PHEs would have been compromised. Additionally, and perhaps more strategically, the PHEOC’s legal framework may be secured as part of a National Institute of Public Health, especially if the latter already exists.
PHEM is a relatively new field, whose evolution may be traced back to the terrorist attacks of 9/11.50 Thus, countries establishing PHEOCs for the first time may not have staff sufficiently trained in PHEM principles, especially in low- and middle-income countries. Uganda’s PHEOC staff had to learn the basic PHEM principles on-the-job through available online material from Africa CDC, US CDC, US Federal Emergency Management Agency, and WHO. Another important training resource was the 4-month PHEM fellowship program conducted at the US CDC.20 Participating in simulation exercises is equally important while perfecting PHEM skills.51
Building strong support and connections with political leadership is important for optimizing the PHEOC’s roles and operational efficiency. Relevant PHEM skills could be passed on to the critical decisionmakers and key subject matter experts, including ministers and directors of the health, finance, and agriculture/animal ministries. This helps them appreciate the operational structures of the PHEOC and enables them to practically apply incident management system principles when needed. It is equally important that PHEOC staff develop close working relationships with decisionmakers during “moments of peace” (ie, before, and not during emergencies).
It is equally important for the PHEOC to build and maintain good relations with development and implementing partners for health emergencies. This is particularly true for low- and middle-income countries, where financial and technical resources for prevention and early detection of PHEs, and rapid response to PHEs, are scarce and/or hard to access. In the case of Uganda, most PHEOC activities have been supported over the years by partners including WHO and the US CDC. Partner support has played a key role in ensuring the relatively strong surveillance and response systems to PHEs that exist in Uganda and has enabled the country to mitigate impacts of the numerous outbreaks registered.
Countries establishing PHEOCs will benefit from assembling a steering committee whose members’ participation is voluntary. In the case of Uganda, NTF members expect no financial gains from their service and actually engage in actively garnering national and international support (financial and technical) for PHE detection and response.
Forming ties with law enforcement, cross-border authorities, and the private sector are important components of operating a country’s PHEOC. Because this entails working with external bodies, such ties may be established through developing memoranda of understanding. In the case of Uganda, memoranda of understanding exist between public health and law enforcement, the Private Sector Round Table, medical countermeasures in emergency situations, laboratories handling forensic investigations, and neighboring countries for cross-border surveillance.
Wherever possible, countries are encouraged to establish subnational PHEOCs. Their establishment in Uganda substantially eased the COVID-19 pandemic response that was initially entirely borne by the national PHEOC. Subnational PHEOCs can align their operations and staffing within existing regional structures to ensure sustainability. Certainly, their establishment comes with additional operational costs, which might be a limitation for low-and middle-income countries. In such cases, the national PHEOC could consider developing strong coordination mechanisms with subnational surveillance and response teams or consider operating virtual subnational PHEOCs.
Acknowledgments
The PHEOC staff would like to acknowledge the strong working relationship that has been exhibited by the leadership at the MOH; Ministry of Agriculture, Animal Industries and Fisheries; and the Office of the Prime Minister. Specific thanks are directed to the current Minister of Health, who is a champion of GHSA in Uganda and the world, due to her active involvement in its conceptualization and Uganda’s 2013 pilot project, which contributed to the birth of the GHSA worldwide, and the establishment of the PHEOC in Uganda.
Additionally, the PHEOC would never have existed and registered such achievements had it not been for the good relationships existing with both development and implementing health partners. These include WHO, the US CDC, the US Agency for International Development, Médecins Sans Frontières, the United Nations Children’s Fund, the European Civil Protection and Humanitarian Aid Operations, Uganda Red Cross Society, UK Department for International Development (now renamed the Foreign, Commonwealth & Development Office), World Vision Uganda, the Infectious Diseases Institute, the African Field Epidemiology Network, Africa CDC, China CDC, Makerere University Walter Reed Project, Makerere University School of Public Health, World Food Programme, International Organization for Migration, the UN Resident Coordinator Office in Uganda, UN Women, United Nations Population Fund, United Nations High Commissioner for Refugees, United Nations Department of Safety and Security, United Nations Clinic, Baylor College of Medicine Children’s Foundation-Uganda, the Lutheran World Federation, International Rescue Committee, CARE International, Irish Aid, Resolve to Save Lives, Oxfam International, Uganda Police Force, Uganda People’s Defence Forces, Walimu Uganda, FHI 360, Humanitarian OpenStreetMap Team, GOAL Uganda, and the media.
Establishment of Uganda’s PHEOC and its daily operations are supported by health partners including the US CDC. The process of documenting its achievements in this manuscript received no funding from any source. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US CDC.
References
- 1.World Health Organization (WHO). Public Health Emergency Operations Centre Network [EOC-NET]. Consultation Meeting 19–20 November 2012. Geneva: WHO; 2013. Accessed December 17, 2021. https://apps.who.int/iris/bitstream/10665/85378/1/WHO_HSE_GCR_2013.4_eng.pdf%3E [Google Scholar]
- 2.World Health Organization (WHO). International Health Regulations (2005). 2nd ed. Geneva: WHO; 2005. Accessed June 28, 2022. http://www.who.int/ihr/publications/9789241596664/en/ [Google Scholar]
- 3.World Health Organization (WHO). Framework for a Public Health Emergency Operations Centre. Geneva: WHO; 2015. Accessed December 17, 2021. https://apps.who.int/iris/rest/bitstreams/874073/retrieve [Google Scholar]
- 4.Ario AR, Makumbi I, Bulage L, et al. The logic model for Uganda’s health sector preparedness for public health threats and emergencies. Glob Health Action. 2019;12(1): 1664103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wamala JF, Malimbo M, Okot CL, et al. Epidemiological and laboratory characterization of a yellow fever outbreak in northern Uganda, October 2010-January 2011. Int J Infect Dis. 2012;16(7):e536–e542. [DOI] [PubMed] [Google Scholar]
- 6.Mbonye A, Wamala J, Winyi-Kaboyo R, Tugumizemo V, Aceng J, Makumbi I. Repeated outbreaks of viral hemorrhagic fevers in Uganda. Afr Health Sci. 2012;12(4):579–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Okware SI, Omaswa FG, Zaramba S, et al. An outbreak of Ebola in Uganda. Trop Med Int Heal. 2002;7(12):1068–1075. [DOI] [PubMed] [Google Scholar]
- 8.Borchert M, Mutyaba I, Van Kerkhove MD, et al. Ebola haemorrhagic fever outbreak in Masindi District, Uganda: outbreak description and lessons learned. BMC Infect Dis. 2011;11(1):357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Towner JS, Sealy TK, Khristova ML, et al. Newly discovered Ebola virus associated with hemorrhagic fever outbreak in Uganda. PLoS Pathog. 2008;4(11):e1000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neil KP, Sodha SV, Lukwago L, et al. A large outbreak of typhoid fever associated with a high rate of intestinal perforation in Kasese District, Uganda, 2008–2009. Clin Infect Dis. 2012;54(8):1091–1099. [DOI] [PubMed] [Google Scholar]
- 11.Adjemian J, Farnon EC, Tschioko F, et al. Outbreak of Marburg hemorrhagic fever among miners in Kamwenge and Ibanda districts, Uganda, 2007. J Infect Dis. 2011; 204(suppl 3):S796–S799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borchert JN, Tappero JW, Downing R, et al. Rapidly building global health security capacity–Uganda demonstration project, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(4):73–76. [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Disaster Preparedness and Management, Office of the Prime Minister. The National Policy for Disaster Preparedness and Management. Kampala, Uganda: Office of the Prime Minister; 2011. Accessed June 28, 2022. https://reliefweb.int/report/uganda/national-policy-disaster-preparedness-and-management [Google Scholar]
- 14.Ario AR, Wanyenze RK, Opio A, et al. Strengthening global health security through Africa’s first absolute post-master’s fellowship program in field epidemiology in Uganda. Health Secur. 2018;16(suppl 1):S87–S97. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization (WHO). Joint External Evaluation of IHR Core Capacities of the Republic of Uganda. Mission Report: June 26–30, 2017. Geneva: WHO; 2017. Accessed December 20, 2021. http://apps.who.int/iris/bitstream/handle/10665/259164/WHO-WHE-CPI-REP-2017.49-eng.pdf?sequence=1 [Google Scholar]
- 16.The Public Health Act. Ch 281 (1969) (Ug). http://library.health.go.ug/download/file/fid/1810
- 17.Lamorde M, Mpimbaza A, Walwema R, et al. A cross-cutting approach to surveillance and laboratory capacity as a platform to improve health security in Uganda. Health Secur. 2018;16(suppl 1):S76–S86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Behumbiize P, Lule J, Magoba B, et al. Evaluation of the implementation and utilisation of a case based diseases surveillance (electronic Integrated Disease Surveillance and Reporting (eIDSR-CBS)) in the West Nile region: August 2018 to February 2019. Texila Int J Pub Health. 2019;7(4): 34–48. [Google Scholar]
- 19.Mwebaza S, Jjuuko J, Kesande P. Religious tourism and pilgrimage: conflicts and challenges, a case of the Namugongo Martyrs Shrines in Uganda. Tur Kult. 2018; 7(7):117–131. [Google Scholar]
- 20.Brencic DJ, Pinto M, Gill A, Kinzer MH, Hernandez L, Pasi OG. CDC support for global public health emergency management. Emerg Infect Dis. 2017;23(suppl 1):S183–S189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kayiwa J, Kasule J-N, Ario A-R, et al. Conducting the Joint External Evaluation in Uganda: the process and lessons learned. Health Secur. 2019;17(3):174–180. [DOI] [PubMed] [Google Scholar]
- 22.Ministry of Health. National Action Plan for Health Security 2019 – 2023. Kampala: MOH; 2019. Accessed July 15, 2022. http://library.health.go.ug/publications/work-plans/national-action-plan-health-security-2019-2023-0 [Google Scholar]
- 23.World Health Organization (WHO). FAO/WHO International Food Safety Authorities Network (INFOSAN). Geneva: WHO; 2019. Accessed July 20, 2022. https://www.who.int/groups/international-food-safety-authorities-network-infosan [Google Scholar]
- 24.Kiyaga C, Sendagire H, Joseph E, et al. Uganda’s new national laboratory transport system: a successful model for improving access to diagnostic services for early infant HIV diagnosis and other programs. PLoS One. 2013;8(11):e78609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wasswa H. Uganda grapples with new Marburg disease outbreak. BMJ. 2017;359:j5252. [DOI] [PubMed] [Google Scholar]
- 26.Siya A, Bazeyo W, Tuhebwe D, et al. Lowland grazing and Marburg virus disease (MVD) outbreak in Kween district, Eastern Uganda. BMC Public Health. 2019;19:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nyakarahuka L, Shoemaker TR, Balinandi S, et al. Marburg virus disease outbreak in Kween District Uganda, 2017: epidemiological and laboratory findings. PLoS Negl Trop Dis. 2019;13(3):e0007257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aceng JR, Ario AR, Muruta AN, et al. Uganda’s experience in Ebola virus disease outbreak preparedness, 2018–2019. Global Health. 2020;16:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Monje F, Ario AR, Musewa A, et al. A prolonged cholera outbreak caused by drinking contaminated stream water, Kyangwali refugee settlement, Hoima District, Western Uganda: 2018. Infect Dis Poverty. 2020;9:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhu B-P, Pande G, Kwesiga B, Ario AR. Cholera outbreak in a fishing village in Uganda: a case study. Pan Afr Med J. 2018;30(suppl 1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walekhwa AW, Ntaro M, Kawungezi PC, et al. Measles outbreak in Western Uganda: a case-control study. BMC Infect Dis. 2021;21:596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mafigiri R, Nsubuga F, Ario AR. Risk factors for measles death: Kyegegwa District, western Uganda, February-September, 2015. BMC Infect Dis. 2017;17:462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Biribawa C, Atuhairwe JA, Bulage L, et al. Measles outbreak amplified in a pediatric ward: Lyantonde District, Uganda, August 2017. BMC Infect Dis. 2020;20:398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ario AR, Nsubuga F, Bulage L, Zhu B-P. Investigating an outbreak of measles in Kamwenge District, Uganda, July 2015. Pan Afr Med J. 2018;30(suppl 1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nakanwagi M, Ario AR, Kwagonza L, et al. Outbreak of gastrointestinal anthrax following eating beef of suspicious origin: Isingiro District, Uganda, 2017. PLoS Negl Trop Dis. 2020;14(2):e0008026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kungu JM, Nsamba P, Wejuli A, Kabasa JD, Bazeyo W. Perceptions and practices towards anthrax in selected agricultural communities in Arua District, Uganda. J Trop Med. 2020;2020:9083615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kisaakye E, Ario AR, Bainomugisha K, et al. Outbreak of anthrax associated with handling and eating meat from a cow, Uganda, 2018. Emerg Infect Dis. 2020;26(12):2799–2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coffin JL, Monje F, Asiimwe-Karimu G, Amuguni HJ, Odoch T. A One Health, participatory epidemiology assessment of anthrax (Bacillus anthracis) management in Western Uganda. Soc Sci Med. 2015;129:44–50. [DOI] [PubMed] [Google Scholar]
- 39.Apangu T, Acayo S, Atiku LA, et al. Intervention to stop transmission of imported pneumonic plague–Uganda, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(9):241–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doreen B, Eyu P, Okethwangu D, et al. Fatal methanol poisoning caused by drinking adulterated locally distilled alcohol: Wakiso District, Uganda, June 2017. J Environ Public Health. 2020;2020:5816162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alitubeera PH, Eyu P, Kwesiga B, Ario AR, Zhu B-P. Outbreak of cyanide poisoning caused by consumption of cassava flour — Kasese District, Uganda, September 2017. MMWR Morb Mortal Wkly Rep. 2019;68(13):308–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abia WA, Montgomery H, Nugent AP, Elliott CT. Tropane alkaloid contamination of agricultural commodities and food products in relation to consumer health: learnings from the 2019 Uganda food aid outbreak. Compr Rev Food Sci Food Saf. 2021;20(1):501–525. [DOI] [PubMed] [Google Scholar]
- 43.Kigozi SP, Kigozi RN, Sebuguzi CM, et al. Spatial-temporal patterns of malaria incidence in Uganda using HMIS data from 2015 to 2019. BMC Public Health. 2020;20:1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Epstein A, Namuganga JF, Kamya EV, et al. Estimating malaria incidence from routine health facility-based surveillance data in Uganda. Malar J. 2020;19:445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ndumu D, Zecchin B, Fusaro A, et al. Highly pathogenic avian influenza H5N8 Clade 2.3.4.4B virus in Uganda, 2017. Infect Genet Evol. 2018;66:269–271. [DOI] [PubMed] [Google Scholar]
- 46.Nantima N, Ademun ARO, Sentumbwe J, et al. Managing the challenges of a highly pathogenic avian influenza H5N8 outbreak in Uganda: a case study. Rev Sci Tech. 2019;38(1):225–237. [DOI] [PubMed] [Google Scholar]
- 47.Mirembe BB, Mazeri S, Callaby R, Nyakarahuka L, Kankya C, Muwonge A. Temporal, spatial and household dynamics of Typhoid fever in Kasese district, Uganda. PLoS One. 2019;14(4):e0214650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bulage L, Masiira B, Ario AR, et al. Modifiable risk factors for typhoid intestinal perforations during a large outbreak of typhoid fever, Kampala Uganda, 2015. BMC Infect Dis. 2017;17:641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nanziri C, Ario AR, Ntono V, et al. Ebola virus disease preparedness assessment and risk mapping in Uganda, August-September 2018. Health Secur. 2020;18(2):105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rose DA, Murthy S, Brooks J, Bryant J. The evolution of public health emergency management as a field of practice. Am J Public Health. 2017;107(suppl 2):S126–S133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gebbie KM, Valas J, Merrill J, Morse S. Role of exercises and drills in the evaluation of public health in emergency response. Prehosp Disaster Med. 2006;21(3):173–182. [DOI] [PubMed] [Google Scholar]


