Abstract
This article describes some of the key prevention services in the Leon Berard Comprehensive Cancer Center (CLB) Lyon, France, which are based on clinical prevention services, outreach activities, and collaboration with professional and territorial health communities. In addition, research is embedded at all stages of the prevention continuum, from understanding cancer causes through to the implementation of prevention interventions during and after cancer. Health promotion activities in the community and dedicated outpatient primary cancer prevention services for individuals at increased risk have been implemented. The CLB's experience illustrates how prevention can be integrated into the comprehensive mission of cancer centers, and how in turn, the cancer centers may contribute to bridging the current fragmentation between cancer care and the different components of primary, secondary, and tertiary prevention. With increasing cancer incidence, the shift toward integrated prevention-centered cancer care is not only key for improving population health, but this may also provide a response to the shortage of hospital staff and overcrowding in cancer services, as well as offer opportunities to reduce carbon emissions from cancer care.
Introduction
Despite advances in early detection and treatment, cancer has become the leading cause of death in France, with 467,965 new cancer cases and 185,621 cancer-related deaths in 2020 (1). The standardized cancer incidence rate in France (621 for 100,000 inhabitants) is slightly above the European Union (EU) average (569 for 100,000 inhabitants), while cancer mortality (239 cancer-related deaths for 100,000 inhabitants) is below EU average (247 cancer-related deaths for 100,000), with important social inequalities, as in other countries. The rising incidence due to changes in demographics, life expectancy, and cancer risks, as well as growing costs of new cancer therapies have dramatically increased cancer-related expenditures and the socio-economic burden of cancer. In France in 2017, over €18.3 billion was spent on cancer care (an increase of 48% since 2004), and the total economic burden, including productivity losses, was €28 billion. Despite advances, treatment alone will not be able to stem the growing cancer problem.
According to the International Agency of Research on Cancer (IARC), 41% of all new cancers diagnosed in France in 2015 were attributable to established lifestyle and environmental risk factors, targetable by cancer prevention (2). Improvements in cancer survival (63% at 5 years, overall) have further stressed the importance of preventive strategies for cancer survivors, as they have a 30% to 40% increased risk of second primary cancers (3). Healthy lifestyle in cancer survivors has been associated with reduced risk, in particular for tobacco- and alcohol-related second primary cancers, and lower risk of subsequent cardiometabolic diseases.
The significant burden that cancer places on the health care system, stresses the need to improve the integration between the different components of cancer prevention and care, and to strengthen the continuum from understanding cancer causes through to the implementation of effective prevention strategies and policies (4). The Leon Berard Comprehensive Cancer Center in Lyon, France, contributes to overcoming the complex and multifaceted challenges of cancer prevention through its comprehensive cancer prevention strategy, grounded in clinical prevention services, outreach activities, cross-disciplinary research, and collaboration with decision makers and professional and territorial health communities.
Context
The Leon Berard Comprehensive Cancer Center
The Leon Berard Comprehensive Cancer Center (CLB) is a comprehensive cancer center (private-nonprofit healthcare institution), that is 100% dedicated to cancer care and research. The CLB, located in Lyon in the French Auvergne-Rhône-Alpes (AURA) Region, is a member of the UNICANCER network of French Comprehensive Cancer Centers, and is the third largest cancer center in France (5). The CLB manages 13,000 new patients with cancer (including 250 childhood cancers) and follows 38,000 patients annually. More than 2,000 patients are recruited into clinical trials every year. About 45% of the patients managed at CLB, live in Metropolitan Lyon and the Rhône Department (1.9 million inhabitants), and 55% live in neighboring departments (4.5 million inhabitants) or farther away. The CLB conducts high-level research in the major cancer disciplines supported by national and international funding.
Beyond cancer care, the CLB has a longstanding commitment to cancer prevention. In 1945, when Charles de Gaulle established the French Comprehensive Cancer Centers, which was a major milestone in CLB's 100-year history, screening and cancer “prophylaxis” was defined as part of the Centers’ comprehensive cancer missions. In 1990, the CLB created a public health department responsible for implementing the first smoke-free hospital plan and an oncogenetics service. The cancer prevention and environment department, established in 2009, enlarged the CLB's cancer prevention scope to environmental and occupational exposures, nutrition, and physical activity. The CLB's comprehensive cancer prevention strategy, which is an integrated part of the center's medical-scientific program, addresses cancer prevention across all three stages of primary, secondary, and tertiary cancer prevention. Primary cancer prevention refers to interventions that limit cancer development, and includes healthy lifestyle, such as regular physical activity, healthy weight, and quitting smoking. Secondary cancer prevention refers to interventions that detect precancerous lesions, or cancers at early stages. Tertiary prevention refers to interventions that aim to reduce the detrimental impact of cancer and its treatment, and includes moderating complications, long-term sequelae and cancer recurrence, and prevention of second primary cancers.
The French Auvergne-Rhône-Alpes region
The French Auvergne-Rhône-Alpes (AURA) Region is as large as Ireland and has a population of 8.1 million (12.4% of the total French metropolitan population), which is similar to that in Switzerland. The region presents important disparities, with high-density urban areas and rural and mountainous zones of (very) low population density. The AURA Region has the second highest standard of living after Île-de-France, and is one of the regions least affected by poverty, with 12.7% of its population living below the poverty-line compared with 14.6% in metropolitan France (6). AURA is France's leading region for the industrial employment volume, structured around sectors associated with professional and environmental exposures, such as machinery and equipment, metallurgy, rubber-plastics, electrical-electronic products, textiles, and chemicals. The agricultural production is within the national average (accounting for 18% of the European production). Moreover, the AURA Region has among the highest national radon concentrations (classified as carcinogenic to humans by IARC (7) due to its granitic and volcanic soils.
The life expectancy at birth in AURA (80.2 and 85.8 years for men and women in 2022; 81.0 and 86.7 years for men and women in the Rhône Department) is marginally higher than for metropolitan France (79.3 and 85.2 years for men and women). The prevalence of most cancer lifestyle related cancer risk factors is similar to that reported at national levels. There were 42,400 new cancer cases in 2020 in AURA. Overall and premature (before the age of 65) cancer-related mortality was 4% and 10.7% lower in AURA than in metropolitan France. The density of general practitioners (GP) was higher than the national density in 2022 (91.4 vs. 87.4 per 100,000 inhabitants), and increased slightly between 2016 and 2020, compared to a 3% decrease nationally.
Rationale
In France, 20% of all cancers are estimated to be attributable to tobacco smoking, 8% to alcohol consumption and 12% to nutritional factors, including unhealthy diet, excess body weight and physical inactivity. The tobacco smoking rates in France remain among the highest in the EU, with marked social disparities; overall 26.9% of the population are daily smokers with 25.0% among the 17-year-olds. Tobacco control policies have been adopted to reduce smoking rates, with encouraging results. Alcohol consumption also remains higher than in the EU, with 28,000 cancers attributable to alcohol consumption annually. Alcohol consumption is seen as a risk factor for cancer increasingly by the French; 78.4% in 2015 compared with 92% in 2021 (8).
The prevalence of excess body weight (45% of the population) has tripled in the past 40 years, with over 17% being obese, although the prevalence of obesity remains low compared with other European countries (9). The burden of excess body weight-related cancers is expected to increase further, and even to exceed that of tobacco-related cancers (10). Over one-third of the French adult population accumulate a high-level of sedentary lifestyle and insufficient physical activity. More than 50% of cancer survivors declare having ceased or permanently reduced physical activity. The risk of cancer associated with lack of physical activity, unprotected sun exposure, or excess body weight is underestimated in the French population; less than 3% of respondents in a national survey spontaneously cited them as risk factors (8). Lower socioeconomic status and education, and migratory settings are associated with poorer health status and increased cancer risks, which is exacerbated by limited health literacy. While the human papillomavirus (HPV) vaccination coverage in metropolitan France has recently increased to 43% in girls following campaigns, it remains below the optimal coverage rate, despite national and regional implementation efforts.
France is recognized worldwide for its culinary tradition, and the Mediterranean diet is considered protective for several chronic diseases and all-cause mortality. However, the consumption of traditional foods is decreasing and that of industrial processed foods is increasing, with ultra-processed food representing 31.1% of the mean daily energy intake in the adult French population (2,111 kcal), with a higher percentage among younger individuals and in urban areas (11). About another 10% of the cancer burden is attributed to environmental and occupational exposures, that are believed to be underestimated. Air pollution is a major public health issue with 48,000 deaths attributable to ambient air pollution annually. In France, although the average annual NO2 and PM2.5 levels fell by 46% and 50%, respectively, between 2000 and 2019, 28% of the population were still exposed to values above the 2015 WHO annual PM2.5 limit value of10 μg/m3. In 2021 this threshold was reduced to 5 μg/m3 and, therefore, this exposure remains an important cause for concern.
In France, three organized screening programs have been established by successive cancer plans, that is, breast cancer (mammogram and clinical breast examination every two years for women aged 50 to 74 years); colorectal cancer (fecal immunochemical test every two years between 50 and 74 years) and cervical cancer screening (cytological screening in asymptomatic women aged 25 to 30 years followed by high-risk HPV test using cervical swab samples, in asymptomatic women aged 30 to 65 years). Organized cancer screening in France involves a variety of institutions at the national level (e.g., Directorate General for Health (strategic oversight), French National Health Authority (professional practices), French National Cancer Institute (operational oversight and screening promotion), French National Agency for Public Health (evaluation), (12). In addition, at the regional level, the Regional Cancer Screening Coordination Centers (CRCDC), overseen by regional health agencies and the Health Insurance, are responsible for implementation, coordination of health professionals, monitoring of the population, and quality assurance. Participation rates in organized colorectal and breast cancer screening are below the EU average, at 31% and 49%, respectively, while cervical cancer screening participation rates are close to the EU average, at 60%.
In France the importance of cancer prevention has recently grown with the 2021–2030 ten-year national cancer control strategy and the renaming of the Health Ministry as the Ministry of Health and Prevention in 2022. The Government has set ambitious targets for the 2021–2030 ten-year national cancer-control strategy, such as reducing the number of preventable cancers by 60,000 annually by 2040, increasing the number of screening procedures by one million by 2025 from the current approximate nine million procedures; and reducing from 2/3 to 1/3 the proportion of patients suffering from after-effects 5 years after cancer diagnosis. In 2022, it was decided to offer free medical prevention consultations at three important ages, that is, 25, 45 and 65 years, but this remains to be implemented.
The current fragmentation between primary, secondary and tertiary prevention, as well as between population-based approaches and targeted prevention interventions to individuals at increased risk, hinder the effective translation of current knowledge about cancer causes into cancer prevention strategies. This is thought to attenuate the benefits of existing cancer prevention efforts. The responsibility of health care providers in personalized cancer risk-assessment and prevention has been emphasized by the French High Council of Public Health (13). However, shortages of health care professionals and inadequate training, have been recognized as important barriers. Improved prevention outcomes have been documented when clinical services initiate prevention, and community-based prevention programs provide assistance and follow-up. The latter in turn, play an important role in promoting health literacy and behavioral change in the community, and in overcoming barriers of access to preventive services. These combined targeted and community-level approaches require enhanced multisectoral collaborations between service providers, policymakers, researchers, and stakeholders within and outside the domain of health. Unfortunately, the current funding model used in the French health care system is an obstacle to the development of preventive interventions and multisectoral collaboration.
CLB's comprehensive cancer prevention strategy
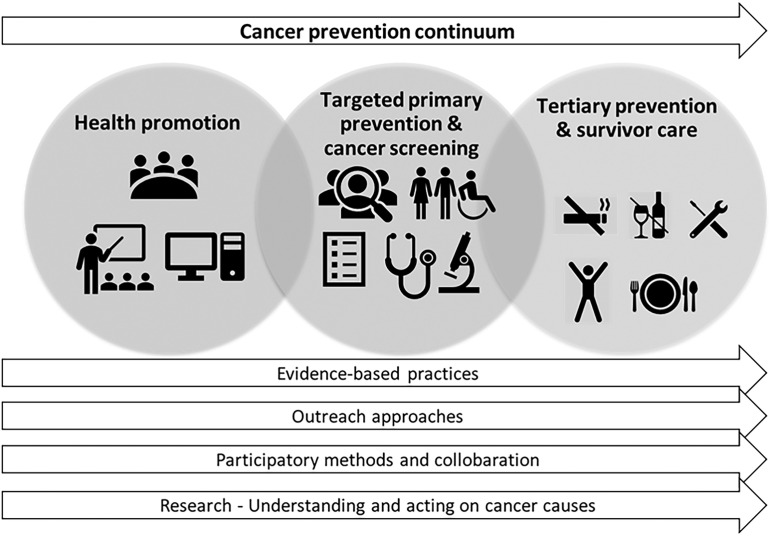
The CLB's comprehensive cancer prevention strategy encompasses the prevention continuum from understanding cancer causes through to the implementation of prevention interventions during and after cancer, as well as in primary prevention (Fig. 1). The strategy directly responds to the French national cancer control plan 2021–2030, the recommendations of the French High Council of Public Health, and the European Beating Cancer Plan.
Figure 1.
CLB's comprehensive cancer prevention strategy. The figure illustrates the CLB's comprehensive cancer prevention strategy encompassing health promotion, targeted primary prevention, cancer screening and tertiary prevention, grounded in evidence-based practices, outreach activities, clinical prevention services, participatory methods and collaboration, as well as cross-disciplinary research.
Research to improve our understanding of cancer causes and to evaluate innovative prevention interventions, is embedded in CLB's cancer prevention strategy and constitutes an important funding source for the activities developed. Moreover, CLB's teams contribute to the incorporation of cancer prevention into the curricula of medical and para-medical schools, as well as teaching programs and training for public health professions, researchers, and professionals from wider backgrounds. The expertise of CLB's leading-edge players contributes further to the development of national (14) and international prevention policies, such as the European Code against cancer and IARC initiatives. We describe here some of the key activities and cancer preventive services in place targeting: (i) cancer patients; (ii) healthy individuals at increased risk; (iii) the wider community population; and (iv) CLB's staff.
Prevention during and after cancer
As 64% of patients with cancer diagnosed since 2015 in France, survive more than 5 years after diagnosis, the focus of cancer management is increasingly being expanded to include the long-term health consequences of cancer and its treatments, and ensure prevention of second primary cancers. In this context, tertiary prevention measures have become an integrated part of CLB's cancer and survivor care pathways. This includes early detection, management, and follow up of risk factors, for example, tobacco smoking, alcohol consumption, overweight-obesity, physical inactivity, which can interfere with cancer treatment or can be associated with poor prognosis, increased risk of second primary cancers and subsequent comorbidities. For instance, the CLB offers a comprehensive range of support to patients to stop smoking, involving individual consultations and group sessions, as well as out- and inpatient addiction services. Proactive direct outreach strategies have been implemented to respond to patients’ needs and to attain hard-to-reach patient groups, taking advantage of shared electronic patient medical records to overcome issues of low referral rates via traditional routes. Teleconsultations, which developed during the COVID-19 pandemic, enhance access to services for patients living at-distance.
Nutrition and physical activity
Since 2009, a program of adapted physical activity and nutrition has been implemented for patients with cancer to prevent and manage sedentary lifestyles and excess body weight. In 2022, over 2,000 adult, adolescent and child patients were managed in a dedicated 300 m² facility during treatment for their localized or metastatic cancer, on an out-patient or day hospitalization basis, or during hospitalization, including sterile rooms. The services involve further online programming, use of connected devices, and dedicated patient education programs. The feasibility and efficacy of these physical activity interventions have been demonstrated in several trials, others are ongoing (e.g., ClinicalTrials.gov-NCT04354233; NCT03529383; NCT04052126; NCT0336905; refs. 15, 16). A multidisciplinary assessment is systematically proposed to patients with breast cancer with excess weight (BMI > 25 kg/m²) and obese patients with other cancers.
Prevention and early detection of sequalae and comorbidities
The CLB has implemented multidisciplinary assessments in adults (PASCA-program, NCT04671693) and children (SALT-program) to improve prevention, early detection and longer-term follow-up of risk factors, subclinical abnormalities, and complications after cancer treatment. Clinical algorithms, based on international and learned society recommendations, have been defined to manage risk factors and complications according to clinical and biological signs, Cancer survivors are referred further to professional and territorial health communities (PTHC) for management, if necessary.
Occupational exposure assessment
Occupational exposures and job-related cancers remain largely under-reported. The main barriers at the physician and patient levels include limited knowledge about the patient's job-related exposures, changes in exposure over time, and long latency between exposure and cancer appearance, as well as smoking-related stigma, and complex administrative procedures. To improve detection of occupational cancers and their compensation, a systematic screening of occupational exposures, combining a self-administered questionnaire and specialized occupational cancer consultation has been implemented since 2009, in collaboration with the Lyon University occupational health services. We have demonstrated that this systematic screening and outreach process can improve compensation for occupational lung cancer and that it can be used in other comprehensive cancer centers (17).
Cancer screening
Substantial gaps exist between age-appropriate screening for second primary cancers and observed screening practices for cancer survivors, despite the existence of tertiary prevention programs. Referral to cancer screening (onsite or elsewhere) is included in the tertiary prevention program. In addition, specific screening protocols, such as clinical and radiological breast cancer screening following thoracic or mediastinal irradiation in women 8 years after radiotherapy are also included. Moreover, specific clinical and radiologic screening is proposed to patients and their families with diagnoses of pathogenic variants of oncogenes predisposing to higher cancer risks.
Primary prevention
The CLB has progressively developed dedicated primary cancer prevention services for individuals at increased risk as well as health promotion activities in the community in line with national prevention programs and policies.
Personalized prevention for relatives and informal caregivers
Informal caregivers may adopt unhealthy behaviors and postpone or even abandon their own care when faced with high objective and subjective burden. Nonetheless, they often have an increased risk perception and motivation for change, particularly when they share hereditary or lifestyle risk factors with the patient. Moreover, prevention in caregiver relatives may help to maintain tertiary prevention in patients with cancer. In a survey among informal caregiver relatives by the CLB in 2020, 42% of respondents asked for a cancer prevention consultation and 44% asked for a dedicated consultation to support their caregiver activities. In response, a single-counter dedicated to caregivers has been implemented. This includes a personalized primary prevention intervention, codesigned with the caregivers themselves, that consists of an initial and a follow-up prevention consultation and evidence-based lifestyle advice, adapted to the expressed needs, identified cancer risk factors (tobacco, alcohol, diet, overweight/obesity, physical activity, ultraviolet radiations), and health literacy level. When required, individuals are referred to PTHC prevention services outside the CLB. The approach is currently being evaluated, PREV-AIDANT (NCT05310045) and another project assessing the transferability to other settings is underway, supported by national and European funding.
Personalized cancer prevention among individuals attending colorectal and breast cancer screening
Mammograms and colonoscopies are performed at CLB as part of the national breast and colorectal cancer screening programs. It has been suggested that screening attendance is a “teachable moment” during which individuals may be more receptive to advice on lifestyle and behavior change and is, therefore, an opportunity for personalized cancer prevention. Previous studies have reported that delivering prevention interventions at colorectal and mammography screening has shown promising results. At CLB, a dedicated prevention consultation comprising risk assessment and evidence-based lifestyle counselling is proposed to individuals attending primary or secondary colonoscopy in the setting of colorectal cancer screening (18). In collaboration with IARC, research teams at CLB are conducting a cluster randomized controlled trial to assess the effect of the intervention on adherence to the World Cancer Research Fund (WCRF) diet and lifestyle recommendations (ClinicalTrials.gov-PP201907–26).
Health promotion in the local and regional community
In addition to preventive clinical services, CLB undertakes outreach health promotion activities in the local and regional communities, guided by three principles:
(i) All information and messages are evidence-based and sourced, and any uncertainties are clearly presented as such.
(ii) Contents are adapted to the target audience, including development of dedicated support for professionals (e.g., teachers, health promotion operators, policy makers), based on a strong collaboration culture and participatory approaches involving actors within and outside the domain of health at the local and regional level.
(iii) Activities involve face-to-face and virtual interventions and presence on social media platforms (Twitter, LinkedIn), and an interactive traveling exhibition on cancer risk factors (specifically for middle schools) to reach large audiences. A dedicated evidence-based web-portal that was set up in 2011, has 1.9 million visits annually (19). French translations of the synthesis of the IARC monographs are disseminated via this portal (20).
Health promoting comprehensive cancer center and environmental management
CLB's longstanding commitment to cancer prevention has led to the development of a grounded health promotion organizational culture. CLB has been a “smoke-free hospital” since 1990 and was the first “health promoting hospital” in the AURA Region in 2020. CLB's environmental management has been certified ISO 14001 since 2011. In addition to the mandatory occupational health and safety requirements, different programs encourage employees to take care of their health, including smoking cessation support, and on-site physical activity sessions. Employees can obtain financial aid for the purchase of a bicycle and its maintenance with the aim of promoting active transport and reducing the environmental impact. In 2019, 50% of CLB's employees used active transport to go to work.
Implementation of the “Reduce, Reuse, Recycle” initiative has successfully prevented increased waste despite significant activity growth, and the effective recycling of recyclable materials has increased from 10% to 50% since 2015. CLB's policy to limit the impact of CLB's cancer care and hospital emissions on the environment, includes a local purchasing policy and connection to the urban heating network. Teleconsultations has led to savings of 5 million vehicle-kilometers since 2020, and a patient hotel has led to savings of 1.2 million vehicle-kilometers annually.
Research
Interdisciplinary research is an essential component of the CLB's prevention strategy, comprising interventional studies, molecular research, as well as an important interdisciplinary research program on environmental exposures (21) and nutritional factors combining epidemiologic and spatial approaches. Infrastructures are in place to facilitate the collection and analyses of clinical and biological data. Moreover, the CLB coordinates the French National Cancer Primary Prevention Transdisciplinary Research Network, CANCEPT, funded by the French National Cancer Institute in 2022. The CANCEPT Network aims to overcome fragmentation in cancer prevention and transform actionable knowledge on nutritional and environmental cancer causes into innovative cancer prevention based on transdisciplinary research, field expertise, and stakeholder knowledge. The CANCEPT network gathers a key group of internationally recognized institutions and researchers with complementary high-level expertise in cancer prevention research. Participatory approaches, the exposome paradigm and a planetary health perspective serve as a backbone to guide the research program. Close and sustained collaboration with IARC has been a catalyst for developing international collaborations in epidemiology and prevention research through the unique network of IARC partners across the world, providing access to data from population cohorts, as well as field access to IARC scientists.
Conclusions and perspectives
The CLB's experience illustrates how prevention can be integrated into the comprehensive mission of cancer centers, as well as how the cancer centers may contribute to bridging the current fragmentation between the different components of primary, secondary and tertiary prevention. The CLB's unique program substantially contributes to the prevention strategy of the Unicancer comprehensive cancer center network that has gradually become increasingly involved in primary, secondary and tertiary prevention. To date only few cancer centers have a similar long-standing expertise as the CLB. Collaborative projects and formal assessment of transferability of interventions allows to mutualize expertise within the Unicancer network. Given the shortage of medical personal and the absence of a clearly established economic model for valuing prevention activities in the hospital context, the activities described here remain experimental and difficult to generalize to other hospitals. Advances in the understanding of the biology that regulates premalignancy as well as of the pathways that control the occurrence of second primary cancers, provide important opportunities for research on cancer interception and tertiary prevention (4, 22).
CLB has started the construction of a local Prevention Center with financial support from regional and local governments, national and charity funds, complemented by a regional virtual Cancer Prevention Center, to bring together in one place all prevention activities, and to strengthen clinical primary prevention services targeted to people at increased risk.
Given the increasing cancer incidence, prevention is not only crucial to improving the population health, but may also represent a potential response to hospital staff shortage and overcrowding of cancer services, which are currently affecting the cancer care system. A prevention rebalancing has become imperative in the setting of an increasing ageing population who present with multiple comorbidities.
While cancer care and follow up of cancer survivors is based on a multidisciplinary approach, cancer prevention requires an even stronger interprofessional, if not intersectoral, collaboration between service providers, policy makers, and stakeholders within and outside the domain of health, as well as researchers. Developing health care professionals’ abilities for this is essential to foster greater collaboration among all sectors relevant to prevention and population health. This is all the more important so that the substantial current fragmentation can be overcome to ensure that the current challenges in cancer prevention can be successfully addressed.
The shift toward integrated prevention centered cancer care may result in addition benefits through the protection of the environment by mitigating emissions from the healthcare sector, estimated at 8% of greenhouse gas emissions in France, and which, in turn, may contribute to improving population health. Research and rigorous evaluation of prevention strategy and innovative practices to assess whether they fulfil their objectives and to guide decision-makers and inform the development of economic models of cancer prevention is a scientific and ethical responsibility.
Acknowledgments
The French National Cancer Primary Prevention Transdisciplinary Research Network, CANCEPT is supported by the French National Cancer Institute (ResPP22–002). The construction of the Prevention Center is financially supported by the Région Auvergne-Rhône-Alpes, the Fonds National d'Aménagement et de Développement du Territoire (FNADT), and the Métropole de Lyon. The funding bodies had no role in the conception, planning, or conduction of the prevention strategy. The authors thank Margaret Haugh, MediCom Consult (Villeurbanne, France) for editorial services.
Authors' Disclosures
B. Fervers reports grants from French National Cancer Institute, grants from Région Auvergne-Rhöne-Alpes, grants from Fonds National d'Aménagement et de Développement du Territoire (FNADT), and grants from Métropole de Lyon during the conduct of the study. C. Rousset-Jablonski reports other support from Organon, Theramex, Novartis, other support from Roche, and other support from Gedeon RIchter outside the submitted work. T. Philip reports grants from French National Cancer Institute, grants from Région Rhöne-Alpes, grants from Fond National d'Aménagement et Développement du Territoire, and grants from Métropole de Lyon during the conduct of the study. No disclosures were reported by the other authors.
References
- 1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021;71:209–49. [DOI] [PubMed] [Google Scholar]
- 2. Soerjomataram I, Shield K, Marant-Micallef C, Vignat J, Hill C, Rogel A, et al. Cancers related to lifestyle and environmental factors in France in 2015. Eur J Cancer 2018;105:103–13. [DOI] [PubMed] [Google Scholar]
- 3. Jégu J, Colonna M, Daubisse-Marliac L, Trétarre B, Ganry O, Guizard AV, et al. The effect of patient characteristics on second primary cancer risk in France. BMC Cancer 2014;14:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lippman SM, Abate-Shen C, Colbert Maresso KL, Colditz GA, Dannenberg AJ, et al. AACR white paper: shaping the future of cancer prevention - a roadmap for advancing science and public health. Cancer Prev Res (Phila) 2018;11:735–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centre Leon Berard. Available from:https://www.centreleonberard.fr/en.
- 6. National Institute of Statistics and Economic Studies. Available from:https://www.insee.fr/fr/statistiques/.
- 7. El Ghissassi F, Baan R, Straif K, Grosse Y, Secretan B, Bouvard V, et al. WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens–part D: radiation. Lancet Oncol 2009;10:751–2. [DOI] [PubMed] [Google Scholar]
- 8. Foucaud J, Soler M, Bauquier C, Pannard M, Préau M. Baromètre Cancer 2015. Cancer et facteurs de risque. Opinions et perceptions de la population française. Institut national du cancer. Santé publique France; 2018. Availablr from: https://www.santepubliquefrance.fr/. [Google Scholar]
- 9. Fontbonne A, Currie A, Tounian P, Picot MC, Foulatier O, Nedelcu M, et al. Prevalence of overweight and obesity in France: The 2020 Obepi-Roche Study by the « Ligue Contre l'Obésité ». J Clin Med 2023;12:925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. GBD 2019Cancer Risk Factors Collaborators. The global burden of cancer attributable to risk factors, 2010–19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2022;400:563–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Calixto Andrade G, Julia C, Deschamps V, Srour B, Hercberg S, Kesse-Guyot E, et al. Consumption of ultra-processed food and its association with sociodemographic characteristics and diet quality in a representative sample of French adults. Nutrients 2021;13:682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dupays S, Leost H, Le Guen Y. Organized cancer screening in France. General Inspectorate for Social Affairs; 2021. Available from: https://www.igas.gouv.fr/Organized-cancer-screening-in-France.html.
- 13. French High Council of Public Health. La place des offreurs de soins dans la prévention; 2024. Available from:https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=689.
- 14. Salas S, Cottet V, Dossus L, Fassier P, Ginhac J, Latino-Martel P, et al. Nutritional factors during and after cancer: impacts on survival and quality of life. Nutrients 2022;14:2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Touillaud M, Fournier B, Pérol O, Delrieu L, Maire A, Belladame E, et al. Connected device and therapeutic patient education to promote physical activity among women with localised breast cancer (DISCO trial): protocol for a multicentre 2×2 factorial randomised controlled trial. BMJ Open 2021;11:e045448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Marec-Bérard P, Delrieu L, Febvey-Combes O, Mongondry R, Pérol O, Moumjid-Ferdjaoui N, et al. Implementation of a prevention program based on adapted physical activity and recommendations for adolescents and young adults with cancer: PREVAPAJA Study. J Adolesc Young Adult Oncol 2022;11:189–201. [DOI] [PubMed] [Google Scholar]
- 17. Pérol O, Lepage N, Noelle H, Lebailly P, de Labrusse B, Clin B, et al. A multicenter study to assess a systematic screening of occupational exposures in lung cancer patients. Int J Environ Res Public Health 2023;20:5068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huybrechts I, Kliemann N, Perol O, Cattey-Javouhey A, Benech N, Maire A, et al. Feasibility study to assess the impact of a lifestyle intervention during colorectal cancer screening in France. Nutrients 2021;13:3685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Centre Leon Berard. Portail cancer environnement;2024. Available from:https://www.cancer-environnement.fr/.
- 20. International Agency for Research on Cancer. IARC Monographs on the identification of carcinogenic hazards to humans. Agents Classified by the IARC Monographs; 2024. Available from:https://monographs.iarc.who.int/agents-classified-by-the-iarc/.
- 21. Amadou A, Praud D, Coudon T, Deygas F, Grassot L, Dubuis M, et al. Long-term exposure to nitrogen dioxide air pollution and breast cancer risk: A nested case-control within the French E3N cohort study. Environ Pollut 2023;317:120719. [DOI] [PubMed] [Google Scholar]
- 22. Heudel PE, de Montfort A, Debieuvre D, Chouaid C, Carton M, Audigier-Valette C, et al. Reduced risk of secondary primary extra pulmonary cancer in advanced/metastatic lung cancer patients treated with immune checkpoint inhibitors. Lung Cancer 2023;182:107280. [DOI] [PubMed] [Google Scholar]