Abstract
Background
Modular neck femoral stems are advantageous because they can accurately restore the ideal hip geometry using various options in terms of offset, length, and version. However, there are concerns regarding junctional problems. Despite several reports on such issues, there is a lack of study on mid- to long-term results of these stems. The current study evaluated the mid-term results of patients who underwent primary total hip arthroplasty using a titanium–titanium (Ti–Ti) modular neck femoral stem.
Methods
In total, data on 47 hips (42 patients) that could be followed-up for ≥ 5 years after primary total hip arthroplasty using the Ti–Ti modular neck femoral stem from 2011 to 2015 were reviewed. There were 22 male and 20 female patients, and their mean age was 56.3 (range: 31–76) years. The mean follow-up period was 8 (range: 5–12) years. Functional and radiological outcomes, complications, and reoperations were investigated. In addition, we conducted a comparative analysis of the outcomes between those who underwent surgery using the Ti–Ti modular neck femoral stem and 41 hips (35 patients, 19 males and 16 females) that underwent primary total hip arthroplasty using nonmodular femoral stems as a control.
Results
In all Ti–Ti cases, the mean Harris Hip Scores were 50.6 (range: 6–59) preoperatively and 92.7 (range: 78–99) at the last follow-up (P < 0.001). Regarding the neck component’s modularity, straight neck components were used in all Ti–Ti cases, and an anteverted or a retroverted neck was not used in any case. Stem revision was performed in one hip due to aseptic loosening. One hip underwent open reduction and internal fixation due to periprosthetic fracture without stem loosening. There were no cases of osteolysis and periprosthetic joint infection and clinically detectable junctional problems. The stem survival rate, with any stem revision as the endpoint, at 12 years was 96.6%. No significant difference was observed in the functional and radiological outcomes beween the Ti–Ti and nonmodular groups.
Conclusions
The Ti–Ti modular neck femoral stem had comparable results with broadly used nonmodular femoral stems; hence, it can be a reliable option in primary total hip arthroplasty. However, in terms of the modularity itself of the modular neck femoral stem, whether the modular neck femoral stem is useful in uncomplicated primary total hip arthroplasty is unclear.
Keywords: Modular neck femoral stem, Offset, Total hip arthroplasty, Junctional problem
Background
Hip offset is a factor that can affect joint reaction force, wear, stability, and longevity in total hip arthroplasty [1–3]. Modular neck femoral stems are advantageous as they can accurately restore the ideal hip geometry [4, 5]. Several authors have reported good clinical outcomes of primary total hip arthroplasty using these stems [6, 7]. In addition, these stems can be helpful in challenging cases such as dysplastic hips, due to various options in terms of offset, length, and version [8].
However, previous studies have reported junctional problems such as corrosion, adverse local tissue reaction, and modular neck fracture [9–12]. In addition, several implants are currently withdrawn from the market [13, 14]. Despite several case reports about junctional problems, studies assessing the mid- to long- term results of primary total hip arthroplasty using the modular neck femoral stem, as compared with broadly used cementless nonmodular fermoral stems, are lacking.
The current study investigated the mid-term (at least 5 years) results of a patient group who underwent primary total hip arthroplasty using the titanium–titanium (Ti–Ti) modular neck femoral stem that was used before withdrawal.
Materials and methods
The current study was approved by the Institutional Review Board of our institution. The electronic medical records and radiographic data of the patients who underwent primary total hip arthroplasty using a highly porous tantalum trabecular metal acetabular cup (Continuum Acetabular System; Zimmer, Warsaw, IN, the USA) and a Ti–Ti modular neck femoral stem (Kinectiv Technology; Zimmer, Warsaw, IN, the USA) from April 2011 to January 2015 were reviewed. Of 72 hips, 35 were lost to follow-up within 5 years. Finally, 47 hips (42 patients, 22 males and 20 females) who were followed-up for ≥ 5 years were included in this analysis. None of the patients presented with procedure-related complications and required stem reivision within 5 years.
Since a recall issue with the modular neck femoral stem in 2015, cementless nonmodular femoral stems have been primarily used in primary total hip arthroplasty at our institution. As a control, cases that underwent primary total hip arthroplasty using cementless nonmodular femoral stems (Ecofit; Implantcast GmbH, Germany and ML taper, Zimmer, Warsaw, IN, the USA) until 2018 were reviewed. Altogether, 41 hips (35 patients, 19 males and 16 females) who were followed-up for ≥ 5years were included as controls.
The surgery was performed by one senior author using the modified Watson-Jones approach in the lateral position. After the procedure involving the acetabular cup, the procedure involving the femoral stem was performed. Stem size and neck offset were selected by evaluating leg length and stability intraoperatively, referred to planned stem size and neck offset using the preoperative template. The default version of the neck component was straight. However, anteverted or retroverted necks were considered if there were concerns about stability based on the examination after the trial insertion, intraoperatively.
Functional and radiological outcomes were investigated postoperatively. For functional evaluation, the Harris Hip Score (HHS) was examined and compared before and after surgery [15]. For radiological evaluation, the inclination and anteversion of the acetabular cup [16, 17], leg length discrepancy, stem subsidence, fixation of the stem and cup [18, 19], and osteolysis around the stem and cup according to the specific zones were evaluated on plain radiography [20, 21]. The inclination and anteversion of the cup and leg length discrepancy were measured on immediate postoperative hip anteroposterior radiography. Leg length discrepancy was defined as the difference in the distance between the level of the lower margin of the tear drop and the level of the apex of the lesser trochanter at both sides. Stem subsidence, fixation of the stem and cup, and osteolysis were evaluated in the last follow-up. To investigate the junctional problems, the symptoms and plain radiograpy and computed tomography (CT) scan were evaluated. Although CT was not routinely performed, in cases in which the CT scan of the abdominopelvic area or lower extremity was performed for medical evaluation at other departments in our institution during the follow-up period, abnormal findings associated with junctional problems such as fluid collection and cyst formation around the hip joint were evaluated [22]. If revision surgery was performed during the follow-up period, the cause of revision surgery was investigated.
Statistical analysis was performed using the Statistical Package for the Social Sciences software version 21.0 (SPSS Inc., Chicago, IL, the USA). For continous variables, t-test or nonparametric test was performed depending on whether the data have a normal distribution. Chi-square or Fisher’s exact test was used to examine for frequencies. P value of < 0.05 was considered statistically significant. In addition, the stem survival rate was investigated via Kaplan–Meier survival analysis.
Results
Regarding the demographic characteristics of the patients, no significant difference was observed between the Ti–Ti and the nonmodular groups (Table 1) [23–25]. The mean follow-up periods were 8 (range: 5–12) yeas and 6.4 (range: 5–8) years for the Ti-Ti and nonmodular groups, respectively.
Table 1.
Demographic data
| Ti–Ti modular neck femoral stem (n = 47) | Nonmodular femoral stem (n = 41) | P value | |
|---|---|---|---|
| Age (years) | 56.3 ± 11.4 | 60.6 ± 12.8 | 0.080 |
| Sex (M/F) | 22 (26 hips)/20 (21hips) | 19 (23 hips)/16 (18 hips) | 0.942 |
| Height (cm) | 163.7 ± 8.8 | 160.1 ± 9.0 | 0.062 |
| Weight (kg) | 62.7 ± 11.9 | 63.1 ± 11.3 | 0.795 |
| Body mass index (kg/m2) | 23.3 ± 2.8 | 24.6 ± 3.7 | 0.065 |
| American Society of Anesthesiologists classification | 1.6 ± 0.7 | 1.8 ± 0.7 | 0.084 |
| Charlson comorbidity index | 0.7 ± 1.2 | 0.5 ± 0.9 | 0.475 |
| Koval grade | 1.6 ± 1.3 | 1.6 ± 1.6 | 0.653 |
| Causes of total hip arthroplasty | 0.744 | ||
| Osteonecrosis | 31 | 27 | |
| Osteoarthritis | 12 | 10 | |
| Femoral neck fracture | 2 | 4 | |
| Rheumatoid arthritis | 1 | 0 | |
| Giant cell tumor | 1 | 0 |
Continuous variables are evaluated as the mean value ± standard deviation
Ti–Ti; titanium–titanium
In all Ti–Ti cases, straight neck components were used, and an anteverted or a retroverted neck was not used in any case. The neck offset was selected according to the patient’s own hip geometry (23 A, 16 B, 5 C, 1 E, 1 G, and 1 J). For the bearing surface, ceramic-on-ceramic was used in 36 cases and ceramic-on-highly cross-linked polyethylene in 11 cases, and the head sizes were 36, 32, and 28 mm in 23, 23, and 1 case, respectively. The mean inclination and anteversion of the cup were 43.5° (range: 32°–59°) and 23° (range: 10°–38°).
Regarding the posopoperative leg length discrepancy, no significant difference was observed between the Ti–Ti and nonmodular groups [1.62 (range: 0–8) vs. 1.66 (range: 0–9), P = 0.834]. No significant difference in other radiological outcomes also noted between the two groups. (Table 2). All acetabular cups were obtained via stable fixation with bone ingrowth. There was no case of osteolysis in both groups.
Table 2.
Clinical outcomes
| Ti–Ti modular neck femoral stem (n = 47) | Nonmodular femoral stem (n = 41) | P value | |
|---|---|---|---|
| Stem fixation | 1.000 | ||
| Bony ingrowth | 45 | 39 | |
| Stable fibrous | 1 | 1 | |
| Unstable | 1 | 1 | |
| Stem subsidence (mm) | 3.5 (range: 2–9, n = 6) | 2.8 (range: 2–4, n = 4) | 1.000 |
| Leg length discrepancy (mm) | 1.62 (range: 0–8) | 1.66 (range: 0–9) | 0.834 |
| Postoperative HHS | 92.7 (range: 78–99) | 91.7 (range: 75–98) | 0.170 |
| Stem revision | 1 | 2 | 0.596 |
Ti–Ti; titanium–titanium, HHS; Harris Hip Score
In the Ti–Ti group, the mean preoperative and postoperative HHS were 50.6 (range: 6–59) and 92.7 (range: 78–99) (P < 0.001). There was no significant difference in postoperative HHS between the two groups (Table 2). In both groups, none of the patients developed dislocation and periprosthetic joint infection. In addition, there were no clinically detectable junctional problems based on symptoms and plain radiography and CT scan results in the Ti–Ti group. In 18 (19 hips) patients, CT scan of the abdominopelvic area or lower extremity was performed at other departments during the follow-up period. Further, there was no periarticular pathologic finding around the prosthesis indicating junctional problems.
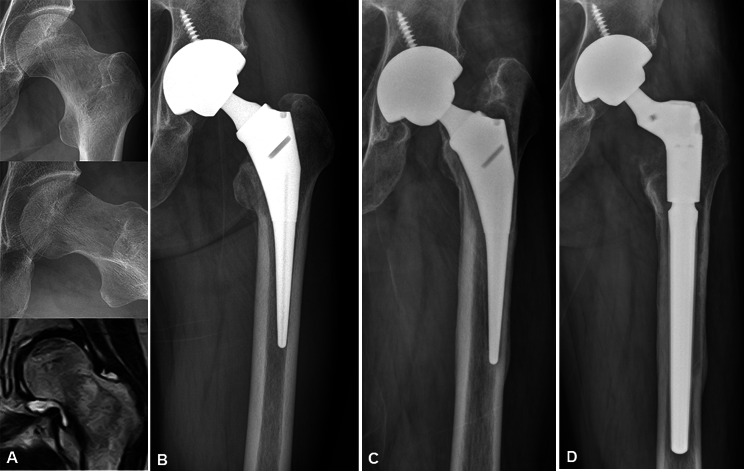
In one hip, stem revision was performed due to aseptic loosening at 8 years after surgery in the Ti–Ti group (Fig. 1). In addition, open reduction and internal fixation was conducted for proximal femoral periprosthetic fracture without stem loosening in one case. In the nonmodular group, stem revision was performed in two cases at 6 years after surgery due to aseptic loosening and proximal femoral periprostehtic fracture.
Fig. 1.
A 52-year-old male patient underwent total hip arthroplsty for osteonecrosis of the femoral head of left hip (A, B). At 8 years after the surgery, stem revision was performed due to aseptic loosening of the stem (C, D)
The stem survival rate of the Ti–Ti modular neck femoral stem, with any stem revision as the endpoint, at 12 years was 96.6% (Fig. 2). In the nonmodular femoral stems, the stem survival rate, with any stem revision as the endpoint, at 8 years was 93.8%.
Fig. 2.
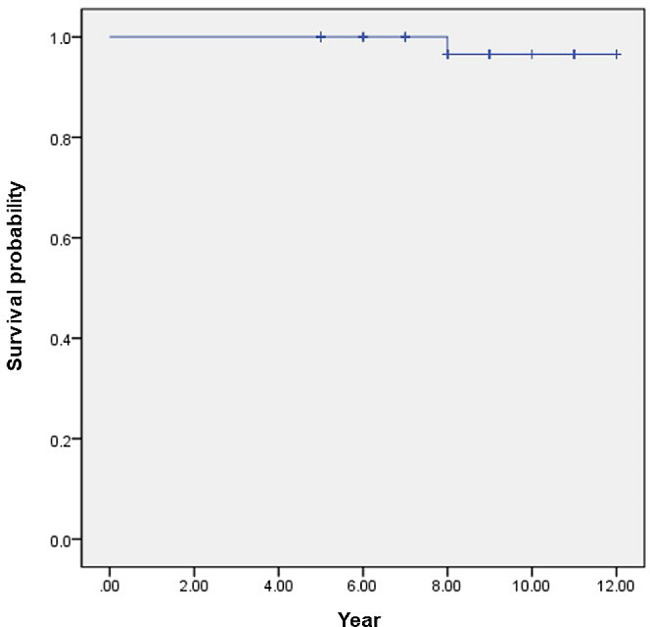
Kaplan–Meier survival curve of the Ti–Ti modular neck femoral stem with any stem revision as the end point
Discussion
Despite the theoretical advantages, there are concerns about junctional problems between the modular neck component and the stem body in the modular neck femoral stems [26]. However, mid- to long-term follow-up studies on the Ti–Ti modular neck femoral stem are lacking. The current study reported the results of our patients who underwent primary total hip arthroplasty using the modular neck femoral stem, with a mean follow-up of 8 years. The results were comparable, and there were no clinically detectable junctional problems.
In terms of the modularity of total hip arthroplasty, the research results on the head-neck taper were relatively greater than that on the modular neck [27]. Corrosion according to metal combination in the head-neck taper can occur over time. However, the parameters are different for similar and different metal combinations [28]. In addition, several studies have reported that mixed metal combinations in the head-neck taper are more susceptible to corrosion than similar metal combinations [29, 30]. Similarly, several authors have reported an increase in serum cobalt and chromium metal ions in cases that used a combination of titanium stem and cobalt–chromium neck, and based on these phenomenon, the limited use of this type of modular neck femoral stem was recommended [31–33]. According to existing literature, the combination of titanium stem and cobalt–chromium neck was commonly used in failed cases [10, 33]. There are only a few cases of junctional problems in the Ti–Ti modular neck [9, 11]. In addition, several clinical studies have shown that the Ti–Ti modular neck femoral stem has good clinical results [6, 7, 34]. This finding is in accordance with our findings. Although there are various factors influencing junctional problems [27], the results might have been influenced by the metal combination between the stem and modular neck. However, additional comparative studies should be conducted to validate this notion.
Considering the neck components used in this study group, the usefulness of the modularity itself of the modular neck femoral stem in cases of uncomplicated primary total hip arthroplasty has not been confirmed. The offset and length of the neck component were planned according to the preoperative template, and the neck component was finally determined with consideration of length, offset, and stability based on the intraoperative findings. In the current study, the version neck was not used. In all hips, the straight neck was utilized, and the A or B components were applied in 80% of the hips. In challenging cases such as patients with dysplastic hip accompanied by complex deformity, various modular neck femoral stems are more useful [35]. Sakai et al. conducted a comparative study on the modular neck and nonmodular neck in patients with developmental dysplasia of the hip who underwent total hip arthroplasty [8]. Results showed that the modular neck group had better clinical and radiological findings.
The current study had several limitations. First, it was a retrospective case series with a small number of cases. Second, all asymptomatic junctional problems at the modular neck junction were challenging to rule out, although a comprehensive clinical and radiological analysis including CT scan was performed. Additional metal ion studies and retrieval studies should be conducted to have a better understanding of these issues.
Conclusions
The Ti–Ti modular neck femoral stem had comparable results with broadly used nonmodular femoral stems; hence, it can be a reliable option in primary total hip arthroplasty. However, in terms of the modularity itself of the modular neck femoral stem, whether the modular neck femoral stem is useful in uncomplicated primary total hip arthroplasty is unclear.
Acknowledgements
Not applicable.
Abbreviations
- Ti–Ti
Titanium–Titanium
- HHS
Harris Hip Score
- CT
Computed tomography
Author contributions
Conceptualization: Kye Young Han, Keong-Hwan Kim. Data curation: Jinwon Jang, Keong-Hwan Kim. Formal analysis: Jinwon Jang, Keong-Hwan Kim. Methodology: Keong-Hwan Kim. Supervision: Kye Young Han, Keong-Hwan Kim. Validation: Jinwon Jang, Keong-Hwan Kim. Writing – original draft: Kye Young Han. Writing – review & editing: Kye Young Han, Keong-Hwan Kim.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board in Kangwon National University Hospital (2023-03-004). Informed consent was waived due to a retrospective design from the Institutional Review Board in Kangwon National University Hospital (2023-03-004).
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sakalkale DP, Sharkey PF, Eng K, Hozack WJ, Rothman RH. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 2001 doi: 10.1097/00003086-200107000-00019.125-34. [DOI] [PubMed] [Google Scholar]
- 2.Forde B, Engeln K, Bedair H, Bene N, Talmo C, Nandi S. Restoring femoral offset is the most important technical factor in preventing total hip arthroplasty dislocation. J Orthop. 2018;15:131–3. doi: 10.1016/j.jor.2018.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lecerf G, Fessy MH, Philippot R, Massin P, Giraud F, Flecher X, et al. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res. 2009;95:210–9. doi: 10.1016/j.otsr.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 4.Duwelius PJ, Hartzband MA, Burkhart R, Carnahan C, Blair S, Wu Y, et al. Clinical results of a modular neck hip system: hitting the bull’s-eye more accurately. Am J Orthop (Belle Mead NJ) 2010;39:2–6. [PubMed] [Google Scholar]
- 5.Traina F, De Clerico M, Biondi F, Pilla F, Tassinari E, Toni A. Sex differences in hip morphology: is stem modularity effective for total hip replacement? J Bone Joint Surg Am. 2009;91(Suppl 6):121–8. doi: 10.2106/JBJS.I.00533. [DOI] [PubMed] [Google Scholar]
- 6.Collet T, Atanasiu JP, de Cussac JB, Oufroukhi K, Bothorel H, Saffarini M, et al. Midterm outcomes of titanium modular femoral necks in total hip arthroplasty. Ann Transl Med. 2017;5:395. doi: 10.21037/atm.2017.07.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ollivier M, Parratte S, Galland A, Lunebourg A, Flecher X, Argenson JN. Titanium-titanium modular neck for primary THA. Result of a prospective series of 170 cemented THA with a minimum follow-up of 5 years. Orthop Traumatol Surg Res. 2015;101:137–42. doi: 10.1016/j.otsr.2014.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Sakai T, Ohzono K, Nishii T, Miki H, Takao M, Sugano N. A modular femoral neck and head system works well in cementless total hip replacement for patients with developmental dysplasia of the hip. J Bone Joint Surg Br. 2010;92:770–6. doi: 10.1302/0301-620X.92B6.23001. [DOI] [PubMed] [Google Scholar]
- 9.Atwood SA, Patten EW, Bozic KJ, Pruitt LA, Ries MD. Corrosion-induced fracture of a double-modular hip prosthesis: a case report. J Bone Joint Surg Am. 2010;92:1522–5. doi: 10.2106/JBJS.I.00980. [DOI] [PubMed] [Google Scholar]
- 10.Cooper HJ, Urban RM, Wixson RL, Meneghini RM, Jacobs JJ. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am. 2013;95:865–72. doi: 10.2106/JBJS.L.01042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah R, Talmo C, Nandi S. Titanium neck-titanium stem taper corrosion in a modular neck stem. Arthroplast Today. 2019;5:145–7. doi: 10.1016/j.artd.2019.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dangles CJ, Altstetter CJ. Failure of the modular neck in a total hip arthroplasty. J Arthroplasty. 2010;25:e11695–7. doi: 10.1016/j.arth.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 13.United States Food and Drug Administration Class 1 Device Recall Zimmer M/L Taper Hip Prosthesis with Kinectiv Technology. 2015 June. Available from https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfRes/res.cfm?ID=137182.
- 14.United States Food and Drug Administration Class 2 Device Recall Rejuvenate Modular stems. 2012 July. Available from https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfres/res.cfm?id=110699.
- 15.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–55. doi: 10.2106/00004623-196951040-00012. [DOI] [PubMed] [Google Scholar]
- 16.Engh CA, Griffin WL, Marx CL. Cementless acetabular components. J Bone Joint Surg Br. 1990;72:53–9. doi: 10.1302/0301-620X.72B1.2298795. [DOI] [PubMed] [Google Scholar]
- 17.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–306. doi: 10.2106/00004623-198264090-00004. [DOI] [PubMed] [Google Scholar]
- 18.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990.107–28. [PubMed]
- 19.Latimer HA, Lachiewicz PF. Porous-coated acetabular components with screw fixation. Five to ten-year results. J Bone Joint Surg Am. 1996;78:975–81. doi: 10.2106/00004623-199607000-00001. [DOI] [PubMed] [Google Scholar]
- 20.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976.20–32. [PubMed]
- 21.Gruen TA, McNeice GM, Amstutz HC. Modes of failure of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979.17–27. [PubMed]
- 22.Mulcahy H, Chew FS. Current concepts of hip arthroplasty for radiologists: part 2, revisions and complications. AJR Am J Roentgenol. 2012;199:570–80. doi: 10.2214/AJR.12.8844. [DOI] [PubMed] [Google Scholar]
- 23.ASA House of Delegates. ASA Physical Status Classification system. 2014. https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system.
- 24.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 25.Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995.150–9. [PubMed]
- 26.Solarino G, Vicenti G, Carrozzo M, Ottaviani G, Moretti B, Zagra L. Modular neck stems in total hip arthroplasty: current concepts. EFORT Open Rev. 2021;6:751–8. doi: 10.1302/2058-5241.6.200064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weiser MC, Lavernia CJ. Trunnionosis in total hip arthroplasty. J Bone Joint Surg Am. 2017;99:1489–501. doi: 10.2106/JBJS.17.00345. [DOI] [PubMed] [Google Scholar]
- 28.Gilbert JL, Buckley CA, Jacobs JJ. In vivo corrosion of modular hip prosthesis components in mixed and similar metal combinations. The effect of crevice, stress, motion, and alloy coupling. J Biomed Mater Res. 1993;27:1533–44. doi: 10.1002/jbm.820271210. [DOI] [PubMed] [Google Scholar]
- 29.Collier JP, Mayor MB, Williams IR, Surprenant VA, Surprenant HP, Currier BH. The tradeoffs associated with modular hip prostheses. Clin Orthop Relat Res. 1995.91–101. [PubMed]
- 30.Goldberg JR, Gilbert JL, Jacobs JJ, Bauer TW, Paprosky W, Leurgans S. A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin Orthop Relat Res. 2002 doi: 10.1097/00003086-200208000-00018.149-61. [DOI] [PubMed] [Google Scholar]
- 31.Laurencon J, Augsburger M, Faouzi M, Becce F, Hassani H, Rudiger HA. Systemic Metal Ion Levels in patients with Modular-Neck stems: a prospective cohort study. J Arthroplasty. 2016;31:1750–5. doi: 10.1016/j.arth.2016.01.030. [DOI] [PubMed] [Google Scholar]
- 32.Lopez RE, Pelayo de Tomas JM, Morales Suarez Varela M, Rodrigo Perez JL. Evolution of chromium and cobalt serum levels after the use of a modular neck stem in primary total hip arthroplasty. Rev Esp Cir Ortop Traumatol. 2024;68:26–34. doi: 10.1016/j.recot.2023.11.010. [DOI] [PubMed] [Google Scholar]
- 33.Bernstein DT, Meftah M, Paranilam J, Incavo SJ. 86% failure rate of a modular-Neck femoral stem design at 3 to 5 years: lessons learned. J Bone Joint Surg Am. 2016;98:e49. doi: 10.2106/JBJS.15.01082. [DOI] [PubMed] [Google Scholar]
- 34.Yi J, Han KY, Nam YJ, Kim KW. Result of modular necks in primary total hip arthroplasty with a average follow-up of four years. Hip Pelvis. 2016;28:142–7. doi: 10.5371/hp.2016.28.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Montalti M, Castagnini F, Giardina F, Tassinari E, Biondi F, Toni A. Cementless Total Hip Arthroplasty in Crowe III and IV Dysplasia: high hip Center and Modular necks. J Arthroplasty. 2018;33:1813–9. doi: 10.1016/j.arth.2018.01.041. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.