Key Clinical Message
Acute aortic dissection in unusual/rare circumstances may become chronic and multi lumen. A high clinical acumen, examination and investigations in the acute setting, may help reduce late/misdiagnosis and complications in low resource settings.
Keywords: aortic, dissection, Ghanaian, triple‐barrel
1. INTRODUCTION
Aortic dissection is the most common of the acute aortic syndromes (70%–80% of cases). 1 The other two are intramural hematoma and penetrating aortic ulcers. It often occurs acutely and is usually catastrophic. 2 It occurs when there is a tear in the intimal lining of the aorta, creating an “intimal flap” and in effect, two or more lumen in the arterial wall (false lumen). Twenty percent of all cases die before reaching the hospital, and in those who survive, mortality rates increase by 1%–2% per hour without treatment. 3 Diagnosis requires a high index of suspicion as its presentation may mimic other conditions. A study by Kurabayashi et al determined the rate of misdiagnosis of aortic dissection on initial assessment in all patients presenting to the emergency room with chest pain as 16%. 4 While relatively uncommon (13 cases reported in the English literature), 5 a few cases may be asymptomatic.
Multiple barreled aortic dissections, with a new lumen being created in the false lumen, or an acute dissection occurring in the setting of a chronic dissection are very rare with a few cases described in the literature. We present a case of a delayed diagnosis of extensive triple‐barreled aortic dissection with limited peripheral arterial vascular involvement.
2. CASE REPORT
2.1. History and examination
A 63‐year‐old male was referred to the cardiology clinic with a 9‐month history of recurrent central chest pain that radiated to his back. He had been diagnosed with hypertension 3 years prior and was compliant with medication.
The chest pain that had occurred 9 months earlier was sharp and described as tearing and sometimes burning, radiating to his back (interscapular region), neck, and left flank. The initial episode was graded 10/10 and was associated with dyspnoea and lightheadedness leading to a 5‐day hospital admission. Thereafter, he sought medical care outpatient basis from various facilities on account of non‐specific chest pain and was eventually referred to our facility for further assessment and management.
In the initial review with our facility, he admitted to palpitations and visual disturbances but denied easy fatigue, syncope, unilateral weakness, nausea, diaphoresis, lower limb pain or paraesthesia, abdominal pain or discomfort or pedal swelling. There was no claudication.
He was of average height and reported both parents and siblings to be of average height and build. He had no history of hyper‐mobile joints or frequent joint dislocations, and neither did any of his siblings. There was no family history of cardiac illness or sudden cardiac death.
On assessment at the cardiac clinic, he was hemodynamically stable, not obese (BMI: 19.2 kg/m2) and in no acute distress. Vital signs were as follows: blood pressure 144/100 mmHg in the right arm and 147/94 mmHg in the left arm, pulse rate 70 beats/min, respiration rate 18/min, temperature 36.2°C, and oxygen saturation of 99% on room air. The cardiac exam showed radio‐radial synchrony, and all other pulses were equal and synchronous. The cardiac apex was in the sixth left intercostal space in the mid‐clavicular line with an apical heave and a thrill. There was a loud second heart sound best heard in the aortic area with a grade 2 ejection systolic murmur loudest at the aortic area which radiated to the back. Lung bases were clear on auscultation. There was no clinical evidence of limb ischaemia. All other systems were grossly normal.
2.2. Investigation and treatment
Initial laboratory investigations, which included a full blood count, renal function test and liver function test were unremarkable.
A chest x‐ray revealed a widened mediastinum with a left‐sided soft tissue mass that had displaced the trachea to the contralateral side, which heightened suspicion of an aortic dissection (Figure 1).
FIGURE 1.
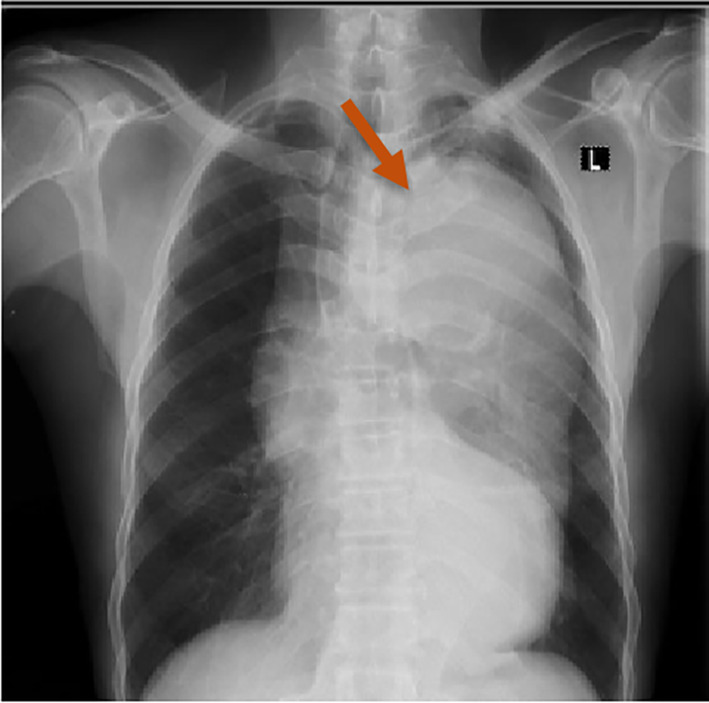
Chest radiograph showing widened mediastinum and prominent aortic shadowing.
The ECG showed voltage criterion left ventricular hypertrophy with no evidence of coronary artery disease. On 2D echocardiography, the aortic root and ascending aorta appeared normal in size with no intimal flap noted. The suprasternal view was suboptimal and no evidence of a dissection was seen at that time. There was no associated aortic regurgitation however mild concentric hypertrophy of the left ventricle with normal systolic function and moderate dilatation of the left atrium were noted. The right ventricle appeared normal in size with no evidence of pulmonary hypertension seen (Figure 2).
FIGURE 2.

2D echocardiogram showing non‐involvement of the aortic root and part of the ascending aorta.
A contrast computerized tomography scan of the chest, obtained on the day he presented, showed a triple‐barreled aortic dissection involving the aortic arch and the descending thoracic aorta, throughout its course and down to the celiac trunk. There was one true lumen, two false lumens and two distinct intimal flaps. The true lumen was continuous with the aortic root superiorly and the celiac trunk inferiorly. The ascending aorta was normal. The true lumen had a diameter of 0.5 cm and the larger of the false lumens was 4.0 cm whilst the other was 0.8 cm. The ascending aorta was normal (Figure 3).
FIGURE 3.

Contrast CT scan of the chest showing triple lumen aortic dissection.
2.3. Outcome and follow‐up
The need for possible surgical correction was discussed with the patient and cardiac surgeons but declined with the patient opting for medical therapy as he was concerned about the cost of cardiac surgery. Medical therapy was initiated with beta‐blockers and an angiotensin receptor blocker. BP has been maintained at less than 120/70 mmHg and an average pulse rate of 60 beats/min. The patient has had no complaints and is stable on periodic follow‐up reviews.
3. DISCUSSION
The incidence of aortic dissection in the United States is reported to be 5–30 cases per 1 million people per year and out of every 1000 patients presenting to the emergency department with acute back, chest, or abdominal pain, three of them are found to have an acute aortic dissection. 6 Similar data in Africa is lacking as factors such as the availability of advanced imaging systems and high mortality rate influence the confirmation of diagnosis.
Risk factors for aortic dissection include advanced age, hypertension, connective tissue disorders, pre‐existing aortic aneurysms, bicuspid aortic valves, coarctation of the aorta, trauma and inflammatory diseases. 7
Most cases present with sudden onset severe tearing or ripping chest (ascending aorta) and/or back pain (descending aorta) with intensity usually worse on onset, and which radiates anywhere between the thorax and abdomen. There may be associated dyspnoea and hyper‐ or hypotension on presentation, and signs of end‐organ ischaemia (i.e., focal neurologic deficits from cerebral ischaemia, abdominal organ ischaemia, lower limb ischaemia, etc.). 8
Our patient had been managed for dyspepsia for months before his visit with us, due to the non‐specific nature of his symptoms, localization of pain to the left flank and lateral chest wall and apparent absence of signs of end‐organ damage or life‐threatening features. Aortic dissection is often missed as presentation, especially in females and in the elderly may be atypical and in rare cases asymptomatic. 9
The fundamentals of an accurate diagnosis rest on having a high index of suspicion, comprehensive history taking and a thorough physical exam. A history of sudden onset, severe chest pain which may be central and radiating to the back or flank in a patient with a history of hypertension, atherosclerotic disease, connective tissue disorders or other genetic predisposition should make a clinician suspect a possible aortic dissection. Patients with aortic dissection usually present with hemodynamic instability culminating in circulatory collapse (usually from proximal dissection), or with hypertension (which is also a risk factor for aortic dissection) especially with distal dissection. 10 , 11 These classical findings were absent in our patient. Pulse deficits or absences occur in 50% of patients with proximal aortic dissection, the brachiocephalic artery being more commonly affected. All pulses should be examined to pick up absent pulses or pulse deficits. 11
Risk scoring systems such as the Aortic dissection detection risk scoring (ADD‐RS) have been developed in conjunction with the d‐dimer to increase clinical suspicion and prompt further investigations in high‐risk patients who may present atypically. 10 Serum D‐dimer levels are elevated in acute aortic dissection, according to a study on biomarkers by the International Registry of Acute Aortic Dissection (IRAD) and have high negative predictive value (>90%), hence can be used as an effective clinical marker in ruling out aortic dissection. 12
There are two systems of classification of aortic dissection based on anatomical location: The Stanford and DeBakey classifications 12 (Figure 4).
FIGURE 4.
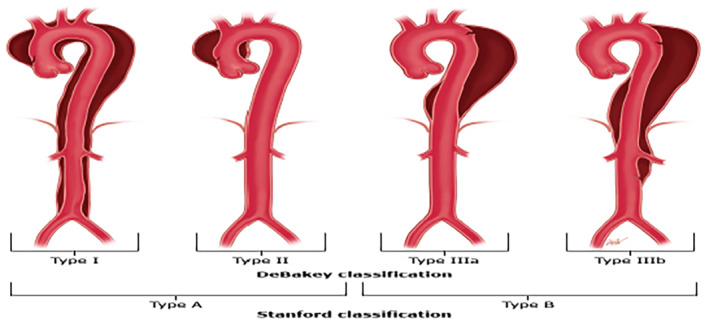
Stanford and Debakey classification of aortic dissection.
Multiple‐barrelled aortic dissections (Triple‐barreled, quadruple‐barrelled) however are uncommon with a few cases described in literature due to the poor outcomes. They are usually of the Stanford type B morphology and occur in patients with Marfan's disease and other connective tissue diseases. In triple‐barrelled dissections, the new dissection may occur within the old, (i.e., True‐False‐False), or as a new dissection, markedly narrowing the true lumen (False‐True‐False) and causing significant symptoms due to end‐organ damage/ hypoperfusion. New onset chest pain in a patient previously diagnosed with aortic dissection should raise suspicion for a new dissection that is, multi‐barreled dissection. 13
In a study done by Suyoeshi et al, multi‐barreled aortic dissection was found to be a powerful independent predictor of Aortic dissection‐related deaths. 14 75% of patients with multi‐barreled dissection (15/20) had AD‐related death over 140 months, as compared to 17.4% in the double‐barreled type. 15
In the evaluation of patients with recurrent chest pain which seems non‐specific, simple outpatient radiographic tests such as a chest x‐ray, electrocardiogram and echocardiogram should be performed early to rule out uncommon but sinister causes which tend to portend a poor prognosis. 16 The delay in diagnosis of this particular patient could be attributed to the fact that in our part of the world, such simple yet important investigative tools are not readily available in smaller healthcare facilities. Training and retraining of health workers and encouraging early referral to higher facilities and ensuring that these facilities have these basic infrastructure may help reduce late diagnosis.
Medical management is indicated as the modality of choice in uncomplicated descending aortic dissections (Stanford type B, DeBakey type III), estimated to be about 70% of all type B dissections. 17 It is also instituted preoperatively, intra‐ and post‐operatively in patients being prepared for surgical correction. In acute type A aortic dissection with an unfavorable prognosis, as determined by risk scoring, medical management alone may be instituted.
The goal of medical management in aortic dissection is to reduce aortic wall stress due to the rate and velocity of ventricular contraction and blood pressure. Initial targets are a heart rate of 60 beats/min and systolic blood pressure between 100 and 120 mmHg.
Emergency surgical management is indicated for type A aortic dissections and complicated type B aortic dissection. 17 The treatment approach traditionally involves open heart surgery. Endovascular surgery is increasingly used for descending thoracic aortic dissections (type B Aortic dissection). It is the recommended approach for complicated hyperacute or acute aortic dissections with favorable anatomy and prognosis. In multi‐lumen aortic dissection, optimal management involves open heart surgery with identification and resection of the initial intimal tear subsequently followed by grafting.
4. CONCLUSION
This case report has described chronic triple‐barreled aortic dissection with the main emphasis being to highlight the usefulness of good clinical acumen and basic investigations to diagnose this high‐risk condition in the acute setting. Though advanced diagnostics and surgical and or interventional modalities are largely inaccessible in Ghana, simple, accessible and useful tools such as a good history and physical exam, chest x‐ray, d dimer, ECG and echocardiography may prevent the catastrophic misdiagnosis of acute aortic dissection and hopefully, we will have more than luck on our side in reducing the high mortality in acute dissection and the debilitating morbidity of chronic dissection in our setting.
AUTHOR CONTRIBUTIONS
Nana Adjoa M. Coleman: Conceptualization; data curation; investigation; writing – original draft. Aba Folson: Conceptualization; supervision; writing – review and editing. Mawufemor A. Bekui: Conceptualization; supervision; writing – review and editing. Bennett Owusu: Conceptualization; investigation; writing – review and editing.
FUNDING INFORMATION
There was no funding for this work.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy. A copy of the written consent is available for review by the Editor‐in‐Chief of this journal.
ACKNOWLEDGMENTS
The authors would like to thank the patient for his cooperation during the assessment and writing of this report.
Coleman NAM, Folson AA, Bekui MA, Owusu B. A rare presentation of triple‐barrel aortic dissection in a Ghanaian male. Clin Case Rep. 2024;12:e8708. doi: 10.1002/ccr3.8708
DATA AVAILABILITY STATEMENT
All data generated or analyzed during this study are included in this published article (and its additional information files).
REFERENCES
- 1. Vignaraja V, Thapar A, Dindyal S. Acute Aortic Syndrome. StatPearls Publishing; 2022. [Google Scholar]
- 2. Criado FJ. Aortic dissection: a 250‐year perspective. Tex Heart Inst J. 2011;38(6):694‐700. [PMC free article] [PubMed] [Google Scholar]
- 3. Harris KM, Nienaber CA, Peterson MD, et al. Early mortality in type a acute aortic dissection: insights from the international registry of acute aortic dissection. JAMA Cardiol. 2022;7(10):1009‐1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kurabayashi M, Miwa N, Ueshima D, et al. Factors leading to failure to diagnose acute aortic dissection in the emergency room. J Cardiol. 2011;58(3):287‐293. [DOI] [PubMed] [Google Scholar]
- 5. Kamalakannan D, Rosman HS, Eagle KA. Acute aortic dissection. Crit Care Clin. 2007;23(4):779‐800. vi. [DOI] [PubMed] [Google Scholar]
- 6. A, Zhou Z, Cecchi AC, Prakash SK, Milewicz DM. Risk factors for thoracic aortic dissection. Genes (Basel). 2022;13(10):1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Levy D, Goyal A, Grigorova Y, Farci F, Le JK. Aortic Dissection. StatPearls Publishing; 2023. [Google Scholar]
- 8. Imoto K, Uchida K, Karube N, et al. Risk analysis and improvement of strategies in patients who have acute type A aortic dissection with coronary artery dissection. Eur J Cardiothorac Surg. 2013;44(3):419‐424. [DOI] [PubMed] [Google Scholar]
- 9. Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17‐year trends from the international registry of acute aortic dissection. J Am Coll Cardiol. 2015;66(4):350‐358. [DOI] [PubMed] [Google Scholar]
- 10. Hirata K, Wake M, Takahashi T, et al. Clinical predictors for delayed or inappropriate initial diagnosis of type A acute aortic dissection in the emergency room. PLoS One. 2015;10(11):e0141929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nordon IM, Hinchliffe RJ, Loftus IM, Morgan RA, Thompson MM. Management of acute aortic syndrome and chronic aortic dissection. Cardiovasc Intervent Radiol. 2011;34:890‐902. [DOI] [PubMed] [Google Scholar]
- 12. Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897‐903. [DOI] [PubMed] [Google Scholar]
- 13. Sherk WM, Khaja MS, Williams DM. Anatomy, pathology, and classification of aortic dissection. Tech Vasc Interv Radiol. 2021;24(2):100746. [DOI] [PubMed] [Google Scholar]
- 14. Sueyoshi E, Sakamoto I, Hayashi K, Yamaguchi T, Imada T. Growth rate of aortic diameter in patients with type B aortic dissection during the chronic phase. Circulation. 2004;110:II256‐II261. [DOI] [PubMed] [Google Scholar]
- 15. Sueyoshi E, Nagayama H, Hayashida T, Sakamoto I, Uetani M. Comparison of outcome in aortic dissection with single false lumen versus multiple false lumens: CT assessment. Radiology. 2013;267(2):368‐375. [DOI] [PubMed] [Google Scholar]
- 16. von Kodolitsch Y, Schwartz AG, Nienaber CA. Clinical prediction of acute aortic dissection. Arch Intern Med. 2000;160(19):2977‐2982. [DOI] [PubMed] [Google Scholar]
- 17. MacGillivray TE, Gleason TG, Patel HJ, et al. The Society of Thoracic Surgeons/American Association for Thoracic Surgery clinical practice guidelines on the management of type B aortic dissection. Ann Thorac Surg. 2022;113(4):1073‐1092. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its additional information files).


