Abstract
Background
The purpose of this study was to analyze myopic regression after corneal refractive surgery (CRS) in civilian pilots and to explore the factors that may cause long-term myopic regression.
Methods
We included civilian pilots who had undergone CRS to correct their myopia and who had at least 5 years of follow-up. We collected retrospective data and completed eye examinations and a questionnaire to assess their eye habits.
Results
A total of 236 eyes were evaluated in this study. 211 eyes had Intrastromal ablations (167 eyes had laser in situ keratomileusis, LASIK, 44 eyes had small incision lenticule extraction, SMILE) and 25 eyes had subepithelial ablations (15 eyes had laser epithelial keratomileusis, LASEK and 10 eyes had photorefractive keratectomy, PRK). The mean preoperative spherical equivalent (SE) was − 2.92 ± 1.11 D (range from − 1.00 to -5.00 D). A total of 56 eyes (23.6%) suffered from myopic regression after CRS. Comparisons of individual and eye characteristics between the regression and non-regression groups revealed statistically significant differences in age, cumulative flight time, postoperative SE (at 6 months and current), uncorrected visual acuity (UCVA), accommodative amplitude (AA), positive relative accommodation (PRA), postoperative period, types of CRS and eye habits. Generalized propensity score weighting (GPSW) was used to balance the distribution of covariates among different age levels, types of CRS, cumulative flying time, postoperative period and continuous near-work time. The results of GPS weighted logistic regression demonstrated that the associations between age and myopic regression, types of CRS and myopic regression, continuous near-work time and myopic regression were significant. Cumulative flying time and myopic regression, postoperative period and myopic regression were no significant. Specifically, the odds ratio (OR) for age was 1.151 (P = 0.022), and the OR for type of CRS was 2.769 (P < 0.001). The OR for continuous near-work time was 0.635 with a P value of 0.038.
Conclusions
This is the first report to analyze myopic regression after CRS in civilian pilots. Our study found that for each year increase in age, the risk of civilian pilots experiencing myopic regression was increased. Intrastromal ablations had a lower risk of long-term myopia regression than subepithelial ablations. There is a higher risk of myopic progression with continuous near-work time > 45 min and poor accommodative function may be related factors in this specific population.
Keywords: Myopic regression, Corneal refractive surgery, Civilian pilot, Accommodative, Eye habit
Background
Considerable experience with corneal refractive surgery (CRS) has been gained worldwide. The aim is generally to allow the patient to do away with spectacles or contact lenses. Previously reported limitations of glasses and contact lenses such as displacement, reduced field of view and poor contrast sensitivity required for flight duty can all be overcome with CRS [1, 2]. The success rate is high, and complications following refractive surgery are infrequent, but refractive regression has been noticed and reported. The maintenance of visual acuity is important to the safe operation of an aircraft and the most important risks, from an aviation standpoint, are loss of best-corrected visual acuity, under correction or overcorrection, fluctuation in vision at different times of the day, glare, “halo” or “starburst” effects due to corneal haze, loss of contrast sensitivity, loss of low-contrast visual acuity, and regression toward preoperative refraction levels [3]. Pilots provide the particular challenge of requiring clear vision at a range of distances and viewing positions, including optimal distance vision for taxiing and approach [1]. For flight safety reasons, when the distance vision loss caused by myopic regression is not fit for the standards (one eye is < 0.7 Landolt rings), there are some visual acuity test requirements that apply to aeromedical assessment, civilian pilots need to wear spectacles or contact lenses again when they return to flying duties [4, 5]. CRS was used to correct refractive errors of a degree that previously prevented applicants from obtaining medical certification needed to work in the aviation environment in China before 2006 [6]. To increase the recruitment pool of potential civilian pilots, moderate myopia and CRS were approved for civilian pilots at initial examination from 2017 [7]. There is, however, rarely any reason for an applicant to submit to refractive surgery in order to meet the visual requirement. One of the most important risks civilian pilots might contemplate is regression towards pre-operative refraction levels and wear glasses again. Pilots are required to use glasses during the exercise of the privileges of the licence or rating applied for or held. But most of them won’t keep using glasses in their daily lives. Uncorrected refractive errors may cause accommodative and binocular dysfunctions and asthenopia. These potential adverse effects that could be incompatible with flying duties [3]. Due to the limitations of identification standards [4–7] and no enough cognition about CRS, the number of myopic civilian pilots choosing CRS is still relatively small, but long-term follow-up myopic regression has been noticed. Therefore, this matter should be investigated, as myopic regression and refractive errors often bring safety problems to civilian pilots.
Refractive regression after any CRS refers to the tendency of the human eye to shift toward its original refraction after a period of desired refraction has been achieved postoperatively [8]. The definition of regression has varied between studies and has traditionally been defined as residual myopia or hyperopia of 0.25dioptres (D) or greater change occurring during follow-up [9]. Specifically, refractive regression is caused by changes at the level of the cornea, not any refractive changes due to lenticular processes or changes in axial length. Because different definitions of regression, methods, and follow-up periods often prevent meaningful comparisons between studies, the exact incidence of refractive regression is difficult to ascertain. Any degree of myopia results in reduced visual acuity, and the correlation between the amount of myopic regression and visual acuity is not clear [10]. Vision chart of Landolt rings projectors is adopted as the test equipment in Civil Aviation Administration of China (CAAC). It is more difficult than other vision tests. For example, it should contain ten symbols in each row with 8 random gaps, no error should be allowed per line of ten symbols. Examiners should not allow the applicant to squint during testing as using the eyelids as a stenopaeic slit may mask refractive errors. In many pilots there is a reluctance to wear spectacles so they may have “overachieved” on the subjective vision test. Aeromedical examiner (AME) found that a significant degree of myopia, i.e. -0.50D or more, will be detected difficult in finishing all symbols of 0.7 (Landolt rings) during the screening examination, provided the applicants is not allowed to squint. Therefore, we defined the regression group as pilots having myopia of more than 0.50D and uncorrected distant vision lower than 0.7 following CRS procedures based on the spherical equivalent (SE) of noncycloplegic refraction and uncorrected distant vision in our study. The definition criteria are less stringent than in other studies but can reflect the visual performance and needs of the airman more comprehensively from an aeromedical significance standpoint.
To date, the exact mechanism of refractive regression after CRS has not been elucidated. Many factors are postulated to be involved. Most observations are mainly related to corneal epithelial thickening and corneal biomechanical changes. The main risk factors are preoperative refractive [8], corneal thickness and the amount of correction [11], age [9], dry eye [12], surgical method [13], etc. Surgical method can be divided in two categories: Intrastromal ablations and subepithelial ablations. Different types and methods of CRS have the problem of refractive regression [14]. Currently, high myopia is considered a risk factor for myopic regression following laser refractive surgery. Our previous study has evaluated the safety of CRS in civilian pilots in China [15], however, the regression following CRS among this population has not been reported. So far, there is limited research on postoperative outcomes for moderate to low myopia and even fewer studies on the long-term myopic regression of patients without postoperative problems.
The purpose of this study was to analyze the myopic regression rate of civilian pilots after CRS for at least 5 years in southwest China and to explore the risk factors that may cause long-term myopia regression.
Methods
Subjects
This study is part of a large study to evaluate the safety of CRS in civilian pilots in China, aiming to analyze the long-term myopia regression rate after CRS and explore the risk factors causing myopia regression in civilian pilots. The study protocol was approved by the hospital’s institutional review board [No 2014(33), 1-6-2015] and conducted according to the Declaration of Helsinki. Written informed consent was obtained from all participants.
Civilian pilots who have had CRS and are being considered for medical certification or recertification should meet the following criteria in China [5, 7]: (a) The surgery is performing surface or flap corneal refractive surgery using an excimer laser or a femtosecond laser. (b) Vision is stable. (c) There is no corneal haze and no complaints of glare, halos or “ghosting”. (d) The result meets the visual requirements, and the assessment must be based on measurements made by a qualified vision care specialist acceptable to the Licensing Authority. (e) There should be follow-up examinations by a qualified vision care specialist six months after return to duty and yearly thereafter. The enrolled participants were grouped into a myopic regression group (uncorrected distant vision lower than 0.7 and with a degree of myopia of -0.5 D or more) and a non-regression group (uncorrected distant vision 0.7 or better and with a degree of myopia less than 0.5 D) based on the SE of noncycloplegic refraction and uncorrected distant vision. For those who applied to only one of the criteria were grouped by uncorrected distant vision only, but we don’t have this population in our sample.
The inclusion criteria were as follows: (1) aged 18–35 years; (2) unremarkable general and ocular health; (3) best-corrected visual acuity of at least 1.0 Landolt rings; (4) no myopic regression within 5 years after surgery: and (5) surgery including laser in situ keratomileusis, LASIK, small incision lenticule extraction, SMILE, photorefractive keratectomy, PRK, laser epithelial keratomileusis, and LASEK. The exclusion criteria included ocular pathology, retinal disorders, glaucoma and postoperative period of less than 5 years. We excluded those whose vision is not stable, those who had corneal haze or complications of glare, halos or “ghosting” and those who did not finish the follow-up examinations by a qualified vision care specialist after return to duty.
The two groups were asked to cooperate as retrospective data was collected, were asked to complete a questionnaire to assess their eye habits, and were requested to complete ocular examinations.
The procedures included the following:
Data collection and eye habits questionnaire
Retrospective data were collected from the treating hospital, including preoperative SE (D), age at surgery, types of surgery, and postoperative review records. 8 experienced surgeons performed all of the procedures. All pilots were examined by ophthalmologic tests preoperatively and at 6 months and every year after surgery by AME. 132 civilian pilots completed the eye habits questionnaire before the periodic ophthalmologic re-examinations by the AME which was conducted between October 2020 and April 2021. The collected data included gender, age, cumulative flying time, weekly outdoor activity time, daily screen time and continuous near-work time. Near-work includes activities done at a short working distance, such as reading books or writing, mobile phone or computer use/ playing video games, or watching TV /video, etc. [16, 17].
Ocular examinations
As an internationally uniform standard, we adopted Landolt rings as the distance vision test symbol, which is also needed to be used for civil aviation pilots in China. Uncorrected visual acuity (UCVA), best spectacle corrected visual acuity (BSCVA), manifest refraction, slit lamp and fundus examination, intraocular pressure (IOP), sodium fluorescein staining and corneal topography were examined [18]. The refractive examination was performed using static retinoscopy and subjective refraction (RT-600, Nidek Co. Ltd.). According to China’s 2013 expert consensus for the diagnosis and treatment of dry eyes, any one of the symptoms of dry eyes, including burning sensation and foreign body sensation, accompanied by a break-up time (BUT) ≤ 5 s, can be diagnosed as dry eye [19]. The IOP examination was performed using a CT-80 tonometer (Topcon, Japan).
Accommodative tests: accommodative amplitude (AA)was measured by the push-up method with a single 20/30 Snellen line target in free space. Positive and negative relative accommodation(PRA and NRA); were measured with plus and minus lenses, respectively, using an accommodative target of 20/30 visual acuity at 40 cm until a sustained blur was perceived. Monocular accommodative facility (MAF); was measured by the same method but without polarized glasses and with the nonviewing eye occluded. Binocular accommodative facility (BAF); was measured at 40 cm using ± 2.00 D flipper lenses and the 20/30 letter line on the Vectogram9 (Tianjin O put Visual Training Co. Ltd.), which included suppression control for the binocular measurement. Dynamic retinoscopy with the monocular estimate method at 40 cm was performed with the result of the subjective refraction placed in a trial frame while using trial lenses.
Data analysis
Statistical software R (Version 4.1.1; R Core Team, 2021) was used for data analysis and description. Descriptive statistics such as absolute and relative frequencies for discrete parameters as well as the mean and standard deviation for continuous parameters were computed. Independent sample t-test and  test were used to compare characteristics of included participants between the regression and non-regression groups. Generalized propensity score weighting (GPSW) was used to balance covariates that both related with exposure and outcome variables. Then GPS weighted logistic regression was applied to detect related factors and outcome variables. The significant level was set as α = 0.05. A P value less than and equal to 0.05 was considered statistically significant.
test were used to compare characteristics of included participants between the regression and non-regression groups. Generalized propensity score weighting (GPSW) was used to balance covariates that both related with exposure and outcome variables. Then GPS weighted logistic regression was applied to detect related factors and outcome variables. The significant level was set as α = 0.05. A P value less than and equal to 0.05 was considered statistically significant.
Results
Demographic data
A total of 132 civilian pilots had undergone CRS in Southwest China; 2 did not satisfy the inclusion criteria given that they were older than 35; 10 were excluded for a postoperative period of less than 5 years; and 1 was diagnosed with glaucoma. After these exclusions, 236 eyes were evaluated in this study (2 of 119 pilots had one eye CRS). A total of 211 eyes had Intrastromal ablations (167 eyes had LASIK, 44 eyes had SMILE) and 25 eyes had subepithelial ablations (15 eyes had LASEK and 10 eyes had PRK). The mean preoperative SE was − 2.92 ± 1.11 D (range from − 1.00 to −5.00 D). A total of 56 eyes (23.6%) suffered from myopic regression after CRS. The pilot’s preoperative data are shown in Table 1. Age at surgery and preoperative SE were similar in the two groups.
Table 1.
Demographic, percentages and clinical findings of the subjects in both groups
| Regression group (N = 56) |
Non-regression (N = 180) |

|
P-value | |
|---|---|---|---|---|
| Gender (M/F) | 30/0 | 88/3 | 1.000 | |
| Age (years) | 32.03 ± 3.78 | 29.18 ± 3.32 | 3.895 | < 0.001 |
| Age at surgery (years) | 20.00 (19.00, 24.00) | 20.00 (18.00, 22.00) | 0.863 | 0.388 |
| Cumulative flying time (hours) |
5,000.00 (2,800.00, 8,200.00) |
3,200.00 (1,762.50, 5,500.00) |
2.323 | 0.020 |
| Types of CRS | 21.639 | < 0.001 | ||
| LASIK | 32(19.2) | 135(80.8) | ||
| SMILE | 10(22.7) | 34(77.3) | ||
| LASEK | 6(40.0) | 9(60.0) | ||
| PRK | 8(80.0) | 2(20.0) | ||
| Preoperative SE(D) | −3.12 ± 1.16 | −2.86 ± 1.09 | −1.541 | 0.125 |
| Postoperative data (at 6 months) | ||||
| SE(D) | + 0.80 ± 0.22 | 0.96 ± 0.26 | −4.1706 | 0.000 |
| CCT | 471.48 ± 27.39 | 478.90 ± 42.09 | −1.2393 | 0.216 |
| Postoperative SE | −1.11 ± 0.85 | 0.15 ± 0.44 | −10.694 | <0.001 |
| UCVA | 0.48 ± 0.19 | 0.98 ± 0.08 | −19.373 | <0.001 |
| IOP (mmHg) | 12.76 ± 3.00 | 12.60 ± 2.85 | 0.346 | 0.729 |
| Accommodative test | ||||
| AA (right eye only,D) | 9.07 ± 1.96 | 10.02 ± 1.94 | −3.186 | 0.002 |
| BAA | 8.91 ± 2.00 | 10.00 ± 1.97 | −2.566 | 0.012 |
| BAF (cpm) | 13.00 (8.75, 17.00) | 13.00 (9.00, 16.00) | 0.079 | 0.937 |
| MAF (right eye only,D) | 13.00 (8.00, 16.00) | 12.50 (8.00, 15.00) | 0.254 | 0.799 |
| NRA(D) | 1.92 ± 0.71 | 1.90 ± 0.56 | 0.187 | 0.851 |
| PRA(D) | 1.83 ± 1.82 | 2.76 ± 1.78 | −2.423 | 0.017 |
| MEM (right eye only,D) | 0.03 ± 0.37 | −0.09 ± 0.52 | 1.517 | 0.130 |
| MEM | 0.04 ± 0.33 | −0.11 ± 0.42 | 1.847 | 0.067 |
CRS Corneal refractive surgery, LASIK Laser in situ keratomileusis, SMILE Small incision lenticule extraction, PRK Photorefractive keratectomy, LASEK Laser epithelial keratomileusis, SE Spherical equivalent, UCVA uncorrected visual acuity, IOP Intraocular pressure. AA Accommodative amplitude, BAA Binocular Accommodative amplitude, BAF Binocular accommodative facility, MAF Monocular accommodative facility, MEM Monocular estimated method, PRA Positive relative accommodation, NRA Negative relative accommodation
Comparisons of individual and eye characteristics in regression and non-regression groups
When comparing individual and eye characteristics, there were statistically significant differences in age, cumulative flight time, types of CRS, postoperative SE (at 6 months and current), UCVA, AA and PRA between the regression and non-regression groups (Table 1). Differences in the postoperative period (which means 5–16 years postoperatively), types of CRS and eye habits were statistically significant (Table 2).
Table 2.
Demographics, percentages and clinical findings of the subjects in both groups
| Regression group (N = 56) |
Non-regression (N = 180) |

|
P-value | |
|---|---|---|---|---|
| Age at surgery, n(%) | <0.001 | 0.975 | ||
|
<20 ≥ 20 |
24(42.9) 32(57.1) |
78(43.3) 102(56.7) |
||
| Postoperative period (years), n(%); | 17.450 | < 0.001 | ||
| 5–10 | 26 (46.4) | 135 (75.0) | ||
| 11–16 | 30 (53.6) | 45 (25) | ||
| Types of CRS, n(%) | 16.090 | < 0.001 | ||
| Intrastromal ablations | 42 (75.0) | 169 (93.9) | ||
| subepithelial ablations | 14 (25.0) | 11 (6.1) | ||
| Preoperative SE(D), n(%); | 1.723 | 0.189 | ||
| −0.5D~−3.0D | 23(41.1) | 92(51.1) | ||
| −3.0D~−5.0D | 33(58.9) | 88(48.9) | ||
| Dry eye test, n(%) | 0.025 | 0.873 | ||
| Non-dry eye | 31 (55.4) | 98 (54.4) | ||
| Dry eye | 25 (44.6) | 82 (45.6) | ||
| Eye habits | ||||
| Weekly outdoor activity time, n(%) | 25.823 | < 0.001 | ||
| ≤ 5 h | 18(62.1) | 13(14.4) | ||
| >5 h | 11(37.9) | 77(85.6) | ||
| Daily screen time, n(%) | 18.631 | < 0.001 | ||
| ≤5 h | 4(13.8) | 20(22.2) | ||
| 5 to 8 h | 16(55.2) | 67(74.4) | ||
| >8 h | 9(31.0) | 3(3.4) | ||
| Continuous near-work time, n(%) | 13.910 | < 0.001 | ||
| >45 min | 18 (62.1) | 22 (24.4) | ||
| ≤ 45 min | 11(37.9) | 68(75.6) |
CRS Corneal refractive surgery, SE Spherical equivalent
Factors influencing refractive regression - based on generalized propensity score weighting (GPSW)
Age
Generalized propensity score weighting (GPSW) was used to balance the distribution of covariates among different age groups. After weighting, the mean absolute value of the correlation coefficient between age and covariates was 0.1 (≤ 0.1), indicating that the covariates were balanced, as shown in Table 3 and Fig. 1. The results of GPS weighted logistic regression demonstrated that the association between age and myopic regression was significant. Specifically, the odds ratio (OR) for age was 1.151 (P = 0.022), indicating that the OR for myopic regression was 1.151 with every one-year increase, Table 4.
Table 3.
Correlation coefficients between age and covariates before and after weighting with propensity scores– age
| Variables | Type | Uncorrected | Corrected | Status |
|---|---|---|---|---|
| Cumulative flying time | Binary | −0.693 | −0.242 | balanced |
| Continuous near-work time | Binary | −0.015 | −0.005 | balanced |
| AA | Continuous | −0.363 | −0.127 | balanced |
| PRA | Continuous | −0.170 | −0.059 | balanced |
| Types of CRS | Binary | 0.054 | 0.022 | balanced |
| Postoperative period | Binary | 0.547 | 0.190 | balanced |
| Spherical equivalent | Continuous | −0.294 | −0.104 | balanced |
| UCVA | Continuous | −0.306 | −0.108 | balanced |
| Age at surgery | Continuous | 0.415 | 0.143 | balanced |
| IOP | Binary | 0.181 | 0.063 | balanced |
Fig. 1.
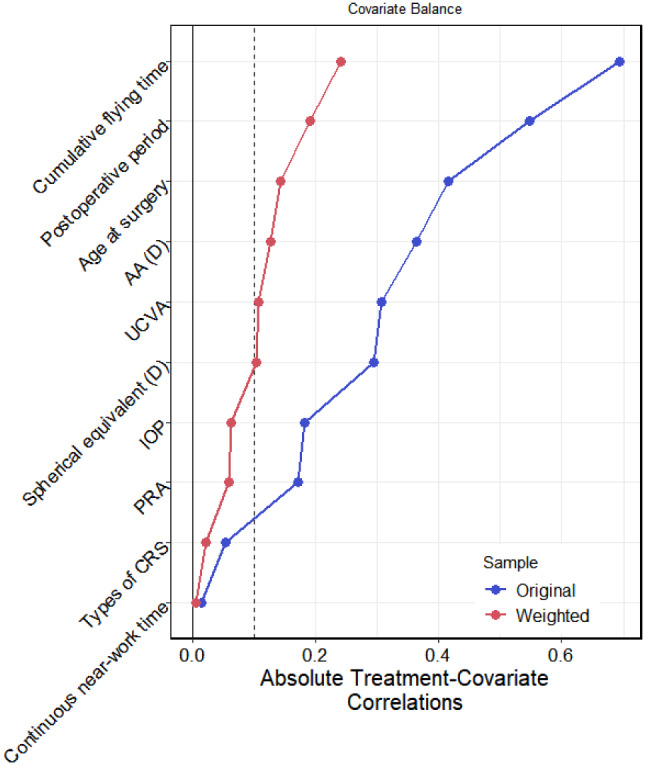
Correlation coefficients between age and covariates before and after weighting with propensity scores
Table 4.
Logistic regression model of the association between age weighted with propensity scores and myopic Regression
| Variables | B | SE | Z | P value | OR | LCI | HCI |
|---|---|---|---|---|---|---|---|
| Intercept | −5.474 | 1.864 | −2.936 | 0.003 | 0.004 | < 0.001 | 0.162 |
| Age | 0.141 | 0.061 | 2.296 | 0.022 | 1.151 | 1.021 | 1.298 |
Types of CRS
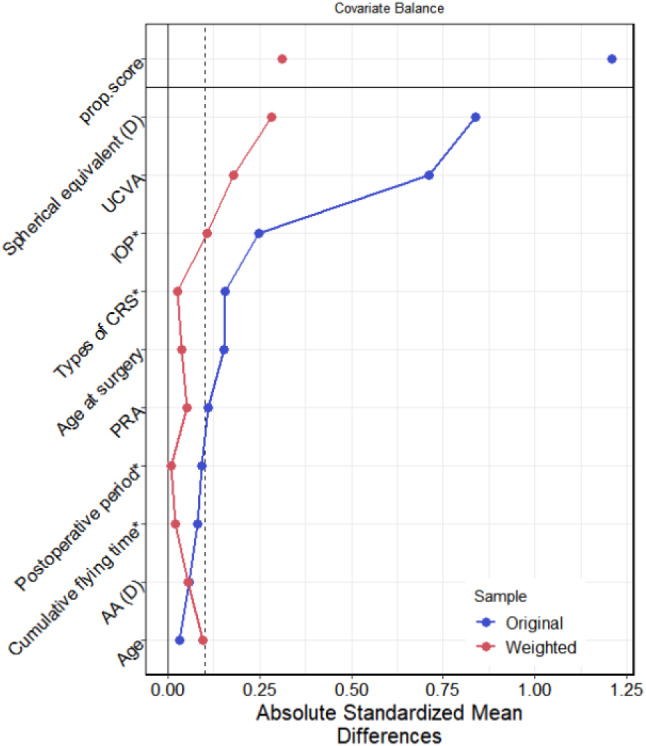
Propensity score weighting (PSW) was used to balance the distribution of covariates between the intrastromal ablations and subepithelial ablations groups. The mean absolute difference after PSW was 0.196 (> 0.1), indicating that the covariates were not balanced (Table 5; Fig. 2). Therefore, the conclusion based on the following propensity score weighted logistic regression might still be affected by confounding effects. The results of the PS weighted logistic regression demonstrated that the association between the types of CRS with myopic regression was significant, where the OR for types of CRS = 2.769 (P < 0.001). This indicated that the risk of refractive regression in the subepithelial ablations group was 2.769 times that in the intrastromal ablations group (Table 6).
Table 5.
Correlation coefficients between types of surgery and covariates before and after weighting with propensity scores– types of surgery
| Variables | Type | Uncorrected | Corrected | Status |
|---|---|---|---|---|
| Age | Continuous | 0.161 | −0.043 | balanced |
| Cumulative flying time | Binary | −0.270 | −0.240 | balanced |
| Continuous near-work time | Binary | −0.372 | −0.266 | unbalanced |
| AA | Continuous | −0.453 | −0.285 | unbalanced |
| PRA | Continuous | −0.061 | −0.045 | balanced |
| Postoperative period | Binary | 0.002 | −0.127 | balanced |
| Spherical equivalent | Continuous | −0.632 | −0.425 | unbalanced |
| UCVA | Continuous | −0.623 | −0.360 | unbalanced |
| Age at surgery | Continuous | −0.129 | −0.150 | balanced |
| IOP | Binary | 0.010 | 0.025 | balanced |
Fig. 2.

Correlation coefficients between types of surgery and covariates before and after weighting with propensity scores
Table 6.
Logistic regression model of the association between type of surgery weighted with propensity scores and myopic regression
| Variables | B | SE | Z | P value | OR | LCI | HCI |
|---|---|---|---|---|---|---|---|
| Intercept | −2.344 | 0.372 | −6.304 | < 0.001 | 0.096 | 0.046 | 0.199 |
| Types of CRS | 1.019 | 0.246 | 4.147 | < 0.001 | 2.769 | 1.711 | 4.481 |
Continuous near-work time
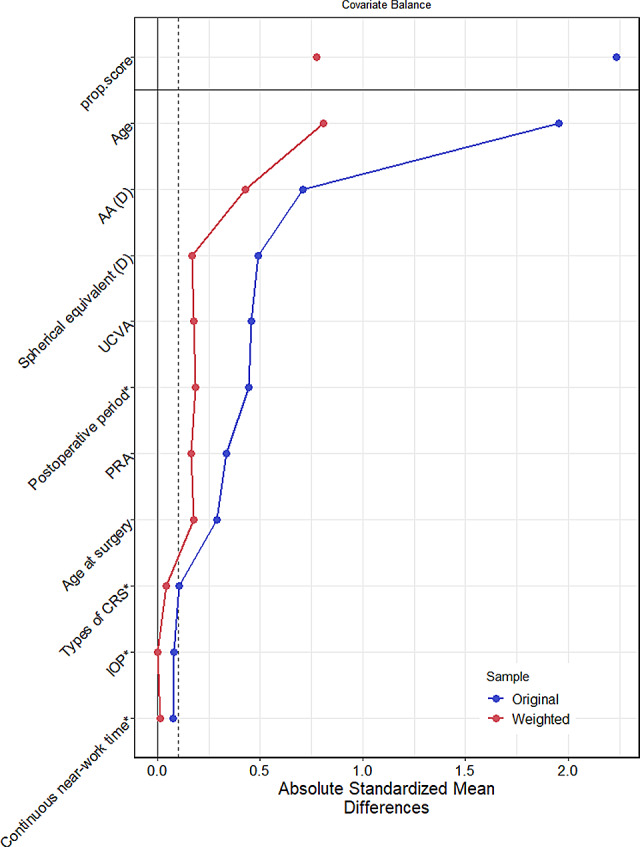
PSW was used to balance the covariates between different times of continuous near-work. The weighted standardized mean difference of the absolute values between groups is 0.086 (≤ 0.1), indicating that the covariate levels were balanced. Please refer to Table 7; Fig. 3 for more details.
Table 7.
Correlation coefficients between eye habits and covariates before and after weighting with propensity scores– continuous near-work time
| Variables | Type | Uncorrected | Corrected | Status |
|---|---|---|---|---|
| Age | Continuous | −0.033 | 0.094 | balanced |
| Cumulative flying time | Binary | 0.081 | −0.021 | balanced |
| AA | Continuous | −0.059 | −0.053 | balanced |
| PRA | Continuous | 0.110 | 0.051 | balanced |
| Types of CRS | Binary | −0.155 | −0.027 | balanced |
| Postoperative period | Binary | −0.092 | 0.009 | balanced |
| Spherical equivalent | Continuous | 0.838 | 0.281 | unbalanced |
| UCVA | Continuous | 0.712 | 0.177 | balanced |
| Age at surgery | Continuous | 0.153 | 0.038 | balanced |
| IOP | Binary | 0.247 | 0.106 | balanced |
Fig. 3.
Correlation coefficients between eye habits and covariates before and after weighting with propensity scores– continuous near-work time
The analysis results of the logistic regression model after propensity score weighting show that there is a statistically significant association between continuous near-work time and myopic progression. Specifically, the OR for continuous near-work time was 0.635, with a p value of 0.038, indicating that there was a higher risk of myopic progression in the pilots with continuous near-work time > 45 min than in the pilots with continuous near-work time < 45 min. Please see Table 8 for more information.
Table 8.
Logistic regression model of the association between eye habits weighted with propensity scores and myopic regression
| Variables | B | SE | Z | P value | OR | LCI | HCI |
|---|---|---|---|---|---|---|---|
| Intercept | −0.825 | 0.15 | −5.509 | < 0.001 | 0.438 | 0.327 | 0.588 |
| Continuous near-work time | −0.454 | 0.219 | −2.070 | 0.038 | 0.635 | 0.413 | 0.976 |
Cumulative flying time
GPSW was used to balance the distribution of covariates among different cumulative flying time. After weighting, the mean absolute value of the correlation coefficient between cumulative flying time and covariates was 0.21 (>0.1), indicating that the covariates were unbalanced, as shown in Table 9 and Fig. 4. Therefore, the conclusion based on the following propensity score weighted logistic regression might still be affected by confounding effects. The results of GPS weighted logistic regression demonstrated that the association between cumulative flying time and myopic regression was no significant (OR = 0.649, P = 0.073) (Table 10).
Table 9.
Correlation coefficients between cumulative flying time and covariates before and after weighting with propensity scores– Cumulative flying time
| Variables | Type | Uncorrected | Corrected | Status |
|---|---|---|---|---|
| Age | Continuous | −1.955 | −0.807 | unbalanced |
| Continuous near-work time | Binary | 0.077 | −0.014 | balanced |
| AA (D) | Continuous | 0.706 | 0.426 | unbalanced |
| PRA | Continuous | 0.334 | 0.164 | balanced |
| Types of CRS | Binary | −0.107 | −0.041 | balanced |
| Postoperative period | Binary | −0.444 | −0.185 | balanced |
| Spherical equivalent (D) | Continuous | 0.490 | 0.168 | balanced |
| UCVA | Continuous | 0.457 | 0.178 | balanced |
| Age at surgery | Continuous | −0.290 | −0.176 | balanced |
| IOP | Binary | −0.080 | 0.002 | balanced |
Fig. 4.
Correlation coefficients between cumulative flying time and covariates before and after weighting with propensity scores
Table 10.
Logistic regression model of the association between cumulative flying time weighted with propensity scores and myopic regression
| Variables | B | SE | Z | P value | OR | LCI | HCI |
|---|---|---|---|---|---|---|---|
| Intercept | −0.984 | 0.165 | −5.97 | < 0.001 | 0.374 | 0.271 | 0.516 |
| Cumulative flying time | −0.432 | 0.241 | −1.792 | 0.073 | 0.649 | 0.405 | 1.041 |
Postoperative period
PSW was used to balance the distribution of covariates between the postoperative period 5–10 years and 11–16 years groups. The mean absolute difference after PSW was 0.087 (<0.1), indicating that the covariates were balanced (Table 11; Fig. 5). The results of the PS weighted logistic regression demonstrated that the association between the postoperative period with myopic regression was no significant, where the OR for postoperative period = 1.117 (P = 0.611) (Table 12).
Table 11.
Correlation coefficients between postoperative period and covariates before and after weighting with propensity scores– Postoperative period
| Variables | Type | Uncorrected | Corrected | Status |
|---|---|---|---|---|
| Age | Continuous | 1.405 | 0.186 | balanced |
| Cumulative flying time | Binary | −0.491 | 0.013 | balanced |
| Continuous near-work time | Binary | −0.097 | 0.065 | balanced |
| AA (D) | Continuous | −0.244 | −0.017 | balanced |
| PRA | Continuous | −0.157 | 0.312 | unbalanced |
| Types of CRS | Binary | 0.001 | −0.033 | balanced |
| Spherical equivalent (D) | Continuous | −0.467 | −0.016 | balanced |
| UCVA | Continuous | −0.461 | 0.082 | balanced |
| Age at surgery | Continuous | −0.392 | −0.118 | balanced |
| IOP | Binary | 0.111 | 0.028 | balanced |
Fig. 5.

Correlation coefficients between postoperative period and covariates before and after weighting with propensity scores
Table 12.
Logistic regression model of the association between postoperative period weighted with propensity scores and myopic regression
| Variables | B | SE | Z | P value | OR | LCI | HCI |
|---|---|---|---|---|---|---|---|
| Intercept | −1.283 | 0.344 | −3.725 | < 0.001 | 0.277 | 0.141 | 0.544 |
| Postoperative period | 0.111 | 0.218 | 0.508 | 0.611 | 1.117 | 0.729 | 1.713 |
Discussion
Research has found that older patients with high myopia are more prone to experience myopic regression than younger patients, suggesting a correlation with the surgeon’s tendency toward under-correction to compensate for the progressive loss of accommodation by age [20, 21].The age range for pilots opting for CRS is usually concentrated between high school graduation and college, so the time of surgery among the pilots in our study is relatively centered at 18 to 23, with an average age of 20. Analysis of postoperative data (at 6 months) indicates that surgeons choose slight overcorrection during the surgical design phase to prevent myopic regression, hence, no cases of myopic regression were observed in the early postoperative period. However, there was statistically significant differences in postoperative period (5–16 years) and cumulative flight time between the two groups. Civilian pilots start their cumulative flying time in their third year of university, around at age of 20, studying flight practical training. Further comparison was made divided by age and no statistically significant difference was found in terms of myopic regression. This indicates that choosing CRS around at age of 20 might not have a general impact on myopic regression. GPSW was used in our data analysis and the results of the PS weighted logistic regression demonstrated that the association between postoperative period with myopic regression and cumulative flight time with myopic regression was no significant (P = 0.611 and P = 0.073). This indicates that different postoperative period and cumulative flight time might not have a general impact on myopic regression in pilots. Current research suggests that cellular proliferation events play a significant role in myopic regression [13]. It has been noted that epithelial compensation and corneal stroma undergoing longitudinal morphological changes can lead to refractive regression over time [22, 23]. Our study found that for each year increase in age, the risk of pilots experiencing refractive regression increased by a factor of 1.151. A study by Lim et al. [18] also found progressive myopic regression and corneal thickening in moderate myopic eyes during a 10-year follow-up after CRS, which is consistent with our results. After ruling out noncorneal factors, the reason for myopic regression in pilots, related to age, is more inclined toward biomechanical changes in the cornea after corneal ablation or environmental risk factors. Further studies are needed in this area.
CRS have potential adverse effects that could be incompatible with flying duties, including corneal scarring or opacities, worsening or variability of vision, and night glare [3]. Only 22 pilots in the Chinese Air Force chose CRS by 2023, all of which were LASEK or PRK, intrastromal ablations have not been implemented [2]. The advantages of subepithelial ablations include no residual corneal flap, thick postoperative corneal stromal thickness, and fewer surgically induced higher-order aberrations. The proportion of choosing CRS is only 5.50% in civilian pilots with refractive errors in southwest China [24]. We found that the long-term myopic regression rates for pilots who chose intrastromal ablations group and subepithelial ablations group were 19.9% and 56%, respectively. The results of the propensity score (PS)-weighted logistic regression demonstrated that the association between the two groups with myopic regression was significant, which indicated that the risk of refractive regression in the subepithelial ablations group was 2.769 times that in the intrastromal ablations group. However, the conclusion based on the following propensity score weighted logistic regression might still be affected by confounding effects for the mean absolute difference after PSW was 0.196 (> 0.1). Further comparison was made divided by types of surgery and we found that the long-term myopic regression rates for pilots who chose LASIK, SMILE, LASEK, PRK were 19.2%, 22.7%, 40% and 80%, respectively. However, the small number of participants in the subepithelial ablations group was a limitation. Song et al. [2] found that subepithelial ablations can significantly improve the visual acuity and refractive error of military pilots in the early stage, and ensure effectiveness, stability and safety. However, a follow-up is needed to understand the natural course of LASEK and PRK. Lim et al. [18] found that the myopic regression rates after 10 years of LASIK and LASEK for moderate myopia were 66.7% and 73.0%, respectively, with average myopia changes of −1.09 D and − 1.34 D, respectively, indicating progressive myopic regression. Chen et al. [25] suggested that the myopic regression rate for LASIK is approximately 21% (5.5–22.7%). Naderi et al. [26] estimated that the myopic regression rate after PRK is approximately 19%. Different research results may be attributed to variations in study subjects and observation periods. Kuryan et al. [27] in a randomized controlled trial, found uncertainty regarding better refractive and visual outcomes between LASEK and LASIK in patients with low to moderate myopia.
Myopia results from complex genetic and environmental causes. Environmental risk factors that have been determined to be associated with myopia include continuous near-work time and little outdoor exposure [16, 28]. Previous studies have shown that increased near-work time can cause asthenopia, affect myopia development [29], and increase the incidence of myopia [16]. In our study, there was a statistically significant association between eye habits and myopic progression. Specifically, the OR for continuous near-work time is 0.635 with a p value of 0.038, indicating that there is a higher risk of myopic progression in the pilots with continuous near-work time > 45 min. Several studies in adults have demonstrated gene‒environment interactions for refractive error, particularly with accumulated near-work activity [30–32]. Since myopia genes are common in the population, adjustment of lifestyle should be a major focus in the prevention of myopia. For myopic patients, consciously limiting the time of continuous near work can not only delay the progression of myopia but also reduce asthenopia [17]. Myopic pilots receiving CRS should be aware of the prevention of myopia regression by lifestyle factors.
Accommodative dysfunctions (ADs) are significant potential risk factors for the progression of myopia [33], so we analyzed accommodative parameters, including AA, PRA/NRA, AF, and MEM, in this study. There were statistically significant differences in AA and PRA between the two groups. The accommodative function in the myopic regression group was poorer. This may be attributed to the fact that pilots in the postoperative period experienced myopic regression but did not consistently wear glasses. It is also possible that eyes with lower amplitudes of accommodation must use more of their accommodative reserve for near work. Myopia may be an adaptation that develops in eyes with reduced accommodative amplitudes [34]. Many findings may explain that the poor performance and limited accommodative function are associated with age [35, 36]. The result is consistent with the progressive loss of accommodation by age in this study, though our study did not have data for people over 35 years old. The relationship between accommodation and myopia has long been a subject of interest, as myopia usually accompanies ADs [37]. From the current research, most studies on postoperative accommodative function after CRS have been positive [38], but there is no literature on the study of accommodative function in postoperative myopic regression. While the causal relationship between accommodation and myopia is still debated, the involvement of accommodative function in the emmetropization process of the eye is widely accepted. Therefore, we speculate that if we can improve the accommodative function of postoperative myopic regression pilots by visual training [39], it may effectively alleviate or even prevent further regression.
CRS is a cause of iatrogenic dry eye syndrome [40], and chronic dry eye may lead to a higher regression rate in CRS patients after surgery [40, 41] Treatment with drugs to lower intraocular tension can effectively reduce the incidence of corneal ectasia and early myopic regression [42]. In this study, the 236 eyes included had a preoperative refraction of less than − 5.0 D, with an average of −2.92 ± 1.11 D and an average intraocular pressure of 12.74 ± 2.97 mmHg. Myopic regression occurred in 23.1% of pilots with dry eyes and 24% of pilots with non-dry eyes(p>0.05). Negative results may be related to the selection of the subjects, as civilian pilots have strict aeromedical restrictions when they choose CRS and resume airman duties [5]. Overall, impotent observations that would help us in the daily clinic.
To date, factors affecting myopic regression after CRS for civilian pilots have never been reported. There is little knowledge about the long-term myopia regression of patients with low to moderate myopia after surgery. There are some limitations in this study. The number of participants in our study was small and observation in different follow-up years is needed to understand the course of myopic regression after CRS. We did not check current epithelial maps. The surgical technique was not effectively controlled because the surgeon that performed the surgery and the equipment used were not the same between groups. A total of 75 eyes (31.8%) after CRS more than 10 years. These data were based on the currently outdated broad beam laser rather than contemporary techniques, such as femtosecond laser technology. Nevertheless, preoperative and early postoperative data were well controlled between the regression and non-regression pilots. The interference caused by early postoperative myopia regression was eliminated.
Conclusions
Our study found that significant differences in age, cumulative flight time, postoperative SE (at 6 months and current), UCVA, AA, PRA, postoperative period, types of CRS and eye habits between the regression and non-regression groups. For each year increase in age, the risk of civilian pilots experiencing myopic regression was increased. Intrastromal ablations had a lower risk of long-term myopia regression than subepithelial ablations. There is a higher risk of myopic progression with continuous near-work time > 45 min and poor accommodative function may be related factors in this specific population.
Acknowledgements
This work was performed with financial support from the Safety Capacity Building Project of Civil Aviation. The authors are grateful to all the subjects for their participation in this research.
Abbreviations
- CRS
Corneal refractive surgery
- LASIK
Laser in situ keratomileusis
- SMILE
Small incision lenticule extraction
- PRK
Photorefractive keratectomy
- LASEK
Laser epithelial keratomileusis
- SE
Spherical equivalent
- UCVA
Uncorrected visual acuity
- IOP
Intraocular pressure
- AA
Accommodative amplitude
- BAF
Binocular accommodative facility
- MAF
Monocular accommodative facility
- MEM
Monocular estimated method
- PRA
Positive relative accommodation
- NRA
Negative relative accommodation
- ADs
Accommodative dysfunctions
- GPSW
Generalized propensity score weighting
Author contributions
ZZ: the idea and concept of the study, shared in writing the manuscript, collection of data. LXX: writing the manuscript, analysis of the data. YW: revised and edited the manuscript. QL: reviewing article, collecting data. SHK: revised the manuscript, collecting data. LQL: revised and edited the manuscript, revised the statistical analysis, shared in idea of the study. All authors read and approved the final manuscript.
Funding
This study was supported by Safety Capacity Building Project of Civil Aviation (2015DFS0457).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of West China Hospital of Sichuan University [No 2014 (33), 1-6-2015] and conducted according to the Declaration of Helsinki. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Reinstein DZ, Ivory E, Chorley A, Archer TJ, Vida RS, Gupta R, Lewis T, Carp GI, Fonseca A, Parbhoo M. PRESBYOND Laser blended Vision LASIK in Commercial and Military pilots requiring Class 1 Medical Certification. J Refract Surg. 2023;39(1):6–14. doi: 10.3928/1081597X-20221129-02. [DOI] [PubMed] [Google Scholar]
- 2.Qi Lin song . Zhang Qyue, Yao L, et al. Visual outcomes after PRK and LASEK in military pilots. Military Med Sci. 2022;46(4):258–62. [Google Scholar]
- 3.International Civil Aviation Organization. Doc 8984, Manual of Civil Aviation Medicine, International Civil Aviation Organization.2012, III-11-34.
- 4.China Civil Administrative Regulation. Flying standards 67, revised Version 2. Beijing. Civil Aviation Administration of China; 2012.
- 5.China Civil Administrative Regulation . Flying standards 67, revised Version 3. Beijing (China): Civil Aviation Administration of China; 2017. [Google Scholar]
- 6.Civil Aviation Administration of China . Appraisal standard od physical examination for recruitment of civil aviation airman trainees. Beijing: Civil Aviation Administration of China; 2006. pp. 2–3. [Google Scholar]
- 7.Civil Aviation Administration of China . Appraisal standard od physical examination for recruitment of civil aviation airman trainees. Beijing: Civil Aviation Administration of China; 2017. pp. 3–4. [Google Scholar]
- 8.Chayet AS, Assil KK, Montes M, Espinosa Lagana M, Castellanos A, Tsioulias G. Regression and its mechanisms after laser in situ keratomileusis in moderate and high myopia. Ophthalmology. 1998;105:1194–9. doi: 10.1016/S0161-6420(98)97020-8. [DOI] [PubMed] [Google Scholar]
- 9.Yan MK, Chang JS, Chan TC. Refractive regression after laser in situ keratomileusis. Clin Exp Ophthalmol. 2018;46(8):934–44. doi: 10.1111/ceo.13315. [DOI] [PubMed] [Google Scholar]
- 10.Zhou J, Gu W, Li S, Wu L, Gao Y, Guo X. Predictors affecting myopic regression in– 6.0D to– 10.0D myopia after laser-assisted subepithelial keratomileusis and laser in situ keratomileusis flap creation with femtosecond laser-assisted or mechanical microkeratome-assisted. Int Ophthalmol. 2020;40(1):213–25. doi: 10.1007/s10792-019-01179-5. [DOI] [PubMed] [Google Scholar]
- 11.Pang G, Zhan S, Li Y, et al. Myopic regression after photorefractive keratectomy. Zhong Hua Yan Ke Za Zhi. 1998;34:451–3. [PubMed] [Google Scholar]
- 12.Nair S, Kaur M, Sharma N, Titiyal JS. Refractive surgery and dry eye - an update. Indian J Ophthalmol. 2023;71(4):1105–14. doi: 10.4103/IJO.IJO_3406_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moshirfar M, Desautels JD, Walker BD, Murri MS, Birdsong OC, Hoopes PCS. Mechanisms of Optical Regression following corneal laser refractive surgery: epithelial and stromal responses. Med Hypothesis Discov Innov Ophthalmol 2018 Spring;7(1):1–9. [PMC free article] [PubMed]
- 14.Kim J, Ryu IH, Kim JK, Lee IS, Kim HK, Han E, Yoo TK. Machine learning predicting myopic regression after corneal refractive surgery using preoperative data and fundus photography. Graefes Arch Clin Exp Ophthalmol. 2022;260(11):3701–10. doi: 10.1007/s00417-022-05738-y. [DOI] [PubMed] [Google Scholar]
- 15.Wu Ye, Zhang Zhen, Tang Xue lin. Evaluation of distant visual functions in the civil aviation pilots after corneal refractive surgery. Chin J Aerospace Med.2017 Dec 28(4):277–281.
- 16.Huang HM, Chang DS, Wu PC. The Association between Near Work activities and Myopia in Children-A systematic review and Meta-analysis. PLoS ONE. 2015;10(10):e0140419. doi: 10.1371/journal.pone.0140419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang J, Zeng P, Deng XW, Liang JQ, Liao YR, Fan SX, Xiao JH. Eye Habits Affect the Prevalence of Asthenopia in Patients with Myopia. J Ophthalmol.2022; 2022:8669217. [DOI] [PMC free article] [PubMed]
- 18.Lim SA, Park Y, Cheong YJ, Na KS, Joo CK. Factors affecting long-term myopic regression after laser in situ keratomileusis and laser-assisted Subepithelial Keratectomy for Moderate Myopia. Korean J Ophthalmol. 2016;30(2):92–100. doi: 10.3341/kjo.2016.30.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ping Z, Kan xing Z, Lihua L, et al. Clinical analysis of accommodation dysfunction and convergence dysfunction in asthenopia. Chin J Practical Ophthalmol. 2014;32(4):424–7. [Google Scholar]
- 20.Wang Y, Zhang fengju, Chen yueguo et al. Chinese expert consensus on laser corneal refractive surgery for correction of refractive errors with age-related accommodation deficiency (2021)Chinese Journal of Ophthalmology. 2021 Sep; 57:651–7. [DOI] [PubMed]
- 21.Morgan IG, French AN, Ashby RS, Guo X, Ding X, He M, Rose KA. The epidemics of myopia: Aetiology and prevention. Prog Retin Eye Res. 2018;62:134–49. doi: 10.1016/j.preteyeres.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 22.Kanellopoulos AJ, Asimellis G. Longitudinal postoperative lasik epithelial thickness profile changes in correlation with degree of myopia correction. J Refract Surg. 2014;30(3):166–71. doi: 10.3928/1081597X-20140219-01. [DOI] [PubMed] [Google Scholar]
- 23.Rocha KM, Krueger RR. Spectral-domain optical coherence tomography epithelial and flap thickness mapping in femtosecond laser-assisted in situ keratomileusis. Am J Ophthalmol. 2014;158(2):293–301. doi: 10.1016/j.ajo.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 24.Zhang Zhen, Xiang Lanxi, Yao Hua. Prevalence of refractive error and the status analysis of corneal refractive surgery in civil pilots. Chin J Aerosp Med. 2021 Apr;32(02):106–9.
- 25.Chen YI, Chien KL, Wang IJ, Yen AM, Chen LS, Lin PJ, Chen TH. An interval-censored model for predicting myopic regression after laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2007;48(8):3516–23. doi: 10.1167/iovs.06-1044. [DOI] [PubMed] [Google Scholar]
- 26.Naderi M, Sabour S, Khodakarim S, Daneshgar F. Studying the factors related to refractive error regression after PRK surgery. BMC Ophthalmol. 2018;18(1):198. doi: 10.1186/s12886-018-0879-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuryan J, Cheema A, Chuck RS. Laser-assisted subepithelial keratectomy (LASEK) versus laser-assisted in-situ keratomileusis (LASIK) for correcting myopia. Cochrane Database Syst Rev. 2017;2(2):CD011080. doi: 10.1002/14651858.CD011080.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tideman JWL, Polling JR, Hofman A, Jaddoe VW, Mackenbach JP, Klaver CC. Environmental factors explain socioeconomic prevalence differences in myopia in 6-year-old children. Br J Ophthalmol. 2018;102(2):243–7. doi: 10.1136/bjophthalmol-2017-310292. [DOI] [PubMed] [Google Scholar]
- 29.Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ, Mitchell P. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008;49(7):2903–10. doi: 10.1167/iovs.07-0804. [DOI] [PubMed] [Google Scholar]
- 30.Wojciechowski R, Yee SS, Simpson CL, Bailey-Wilson JE, Stambolian D. Matrix metalloproteinases and educational attainment in refractive error: evidence of gene-environment interactions in the Age-Related Eye Disease Study. Ophthalmology. 2013;120(2):298–305. doi: 10.1016/j.ophtha.2012.07.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fan Q, Verhoeven VJ, Wojciechowski R, Barathi VA, Hysi PG, Guggenheim JA, et al. Meta-analysis of gene-environment-wide association scans accounting for education level identifies additional loci for refractive error. Nat Commun. 2016;7:11008. doi: 10.1038/ncomms11008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morgan IG, Ohno-Matsui K, Saw SM. Myopia Lancet. 2012;379(9827):1739–48. doi: 10.1016/S0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 33.Allen PM, Radhakrishnan H, Rae S, Calver RI, Theagarayan BP, Nelson P, Osuobeni E, Sailoganathan A, Price H, O’Leary DJ. Aberration control and vision training as an effective means of improving accommodation in individuals with myopia. Invest Ophthalmol Vis Sci. 2009;50(11):5120–9. doi: 10.1167/iovs.08-2865. [DOI] [PubMed] [Google Scholar]
- 34.Fong DS. Is myopia related to amplitude of accommodation? Am J Ophthalmol. 1997;123(3):416–8. doi: 10.1016/S0002-9394(14)70148-5. [DOI] [PubMed] [Google Scholar]
- 35.Erdinest N, London N, Lavy I, Morad Y, Levinger N. Vision through healthy aging eyes. Vis (Basel) 2021;5(4):46. doi: 10.3390/vision5040046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Croft MA, Lütjen-Drecoll E, Kaufman PL. Age-related posterior ciliary muscle restriction - A link between trabecular meshwork and optic nerve head pathophysiology. Exp Eye Res. 2017;158:187–9. doi: 10.1016/j.exer.2016.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Allen PM, O’Leary DJ. Accommodation functions: co-dependency and relationship to refractive error. Vis Res. 2006;46(4):491–505. doi: 10.1016/j.visres.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 38.Zheng K, Han T, Zhou X. Accommodative changes after SMILE for moderate to high myopia correction. BMC Ophthalmol. 2016;16(1):173. doi: 10.1186/s12886-016-0352-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Takada M, Miyao M, Satoh M, et al. Effect of accommodation training on visual function of visual inspection workers and middle-aged people[J] J Sports Med Doping Stud. 2012;2(112):2161–0673. [Google Scholar]
- 40.Albietz JM, Lenton LM, McLennan SG. Chronic dry eye and regression after laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2004;30(3):675–84. doi: 10.1016/j.jcrs.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 41.Turu L, Alexandrescu C, Stana D, Tudosescu R. Dry eye disease after LASIK. J Med Life. 2012;5(1):82–4. [PMC free article] [PubMed] [Google Scholar]
- 42.Gao J, Sun Y, Wen C, et al. Clinical analysis of refractive regression after LASIK in moderate and high myopic eyes. Guo Ji Yanke Za Zhi (Int Eye Sci) 2019;19(4):614–8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.


