Abstract
Background
Poor mental health in medical students is a global concern. Effective interventions are required, which are tailored towards the training-related stressors medical students experience. The Reboot coaching programme is an online, tailored intervention based on cognitive-behavioural principles.
Aims
To evaluate whether the Reboot coaching programme tailored for medical students was feasible and associated with improvements in mental health outcome indicators.
Methods
Medical students participated in two group online workshops and a one-to-one coaching call with a Reboot-trained licensed psychological therapist. Participants provided data at: baseline (T1), post-workshops (T2), post-coaching call (T3) and 4-month follow-up (T4). Outcome measures included resilience, confidence, burnout and depression. Feedback was provided regarding the workshops at T2.
Results
115 participants (93/80.9% women; mage = 23.9; SD = 2.8) were recruited, 83 (72.2%) completed all intervention elements and 82 (71.3%) provided T4 data, surpassing recruitment and retention targets. There were significant improvements following baseline in resilience (ps < .001), confidence (ps < .001), burnout (ps < .001) and depression (ps ≤ .001). Most participants agreed the workshops imparted useful skills (n = 92; 99%) and would recommend Reboot to others (n = 89; 95.6%).
Conclusions
Existing interventions have produced mixed results regarding their effectiveness in improving medical students’ mental health. Reboot is a feasible intervention in this group which is associated with improvements in resilience, confidence, burnout and depression. Further controlled studies of Reboot are now needed.
Keywords: Medical education, medical students, burnout, depression, resilience
Poor mental health in medical students is a significant problem globally. 1 Burnout affects 50% of medical students, 2 one-third experience depression and 10% report suicidal ideation.3,4 Several factors contribute to poor mental health in this group, including a high academic workload and a tendency towards maladaptive perfectionism.5,6
Stressful clinical events on placement are also a key risk factor for poor mental health in medical students. 5 These events are those which are intrinsic to medical work, including experiencing death and working with dying patients7,8; involvement in medical errors 9 and unprofessional behaviour from colleagues. 7 However, there are no available evidence-based interventions to support medical students with placement-related stressors; the mental health interventions which have been tested in this group have been largely generic and ‘off-the-shelf’, including mindfulness, relaxation training and yoga. 10 These have been criticised for lacking relevance and failing to address those stressors intrinsic to medical training and practice.11,12 As such, there is an urgent need for tailored interventions which help students prepare and support them with the specific occupational stressors they will encounter during their placements, training and beyond.
To address this gap, we adapted and evaluated the feasibility of implementing the Reboot (Recovery-BOOsting Training) Coaching Programme for medical students, to enhance their preparedness for involvement in and recovery after stressful healthcare events. Reboot combines two online group workshops and a one-to-one follow-up coaching phone call, maximising the benefits of peer engagement in the group workshop and the opportunity for professional, confidential support in the call. In contrast to existing psychological interventions for medical students, Reboot has been designed specifically for healthcare professionals and students, drawing on a synergy of (1) research into the impacts of stressful healthcare events, (2) psychological resilience theory and (3) evidence-based cognitive-behavioural techniques. Importantly, Reboot addresses the stressful events which are inherent in healthcare professionals’ and students’ work, providing support for those events which cannot be targeted with organisational interventions.
We anticipated Reboot would be beneficial for medical students for four reasons. First, its pro-active, prevention-focused approach reduces stigma in participating; a key factor known to reduce participation in medical student groups.4,13,14 Second, it targets the reduction of maladaptive perfectionism, known to contribute to poor mental health in medical students. 6 Third, it uses materials and cases studies which are specific to the challenges medical students face on placement; it is experienced as engaging and relevant for students in a way which other interventions cannot be.15,16 Fourth, it is all delivered online, improving ease of access and opportunities to discuss experiences with medical students from different regions.
The overarching aim of the current study was to evaluate Reboot in medical students. Our primary objective was to assess whether it was feasible to deliver Reboot to medical students. Our secondary objective was to assess whether participating in Reboot was associated with increased self-reported psychological resilience, confidence in coping with adverse events, and decreased burnout and depression.
Methods
Design
A single-arm, before-after feasibility design, including a mixed-methods evaluation guided by the widely used Kirkpatrick model for assessing training interventions. 17 This recommends evaluating outcomes at four levels (reaction, learning, behaviour, results), and has been used in previous Reboot evaluations.15,16,18
Intervention
Reboot included two, 2-hour online group workshops and a one-to-one coaching call over 4 weeks. Group workshops involved exercises based around tailored case studies, which were adapted for the target sample. In this study, case studies were initially adapted by JJ and WL and then refined via feedback from focus groups (n = 4) with medical students (n = 7), junior doctors (n = 2) and medical educators (n = 3), and from one-to-one semi-structured interviews with medical students (n = 3), junior doctors (n = 2) and one medical educator (conducted by RT). The workshops introduced the intervention, involving individual and group-based exercises which were then personalised in the coaching video/phone call. Participants were allocated to workshop groups of 5–10 participants. For further intervention description, please see Appendix 1.
Participants, procedure and ethics
Participants were recruited UK-wide via medical schools and were from years involving clinical placements. Medical schools were contacted by email and via email cascade from the UK Medical Schools Council (MSC). We collected online questionnaire data at four-time points: Baseline (T1), on completion of the two group workshops (T2), on completion of an individual coaching call (T3), and 4 months post-baseline (T4). The study was approved by the School of Psychology, University of Leeds Ethics Committee (date: 19/01/2022; approval number: PSYC-542).
Sample size
We aimed to recruit ≥81 participants, based on a power analysis for a one-group repeated measures ANOVA main effect, assuming a correlation between pre- and post-intervention scores of r = 0.5; a power of 1 − b = 0.9 and a small effect size of f = 0.15. This calculation accounted for potential participant drop-out. Anticipating medium-large effect sizes 15 ; with 81 participants we could still detect a medium effect (f = 0.25) with a power of 1 − b = 0.9 with around 50% dropout at T4.
Primary feasibility outcomes
Our primary feasibility outcomes included demand (number of expressions of interest), recruitment (number consenting, completing baseline measures and attending the first workshop) and retention (defined as the number: (1) participating in all intervention elements and (2) completing T4 outcome indicators). Consistent with previous evaluations,15,18 feasibility was established if the following criteria were met:
- ≥ 80 expressions of interest
- ≥ 80 recruited
- ≥ 70% completing all intervention elements
- ≥ 50% completing all T4 measures.
Secondary outcomes
Resilience. The six-item Brief Resilience Scale (BRS) measures perceptions of personal resilience, including ‘I tend to bounce back quickly after hard times’. It has good concurrent validity with other resilience questionnaires 19 detects learning changes15,16 and had good internal reliability in the present study (Cronbach's alphas = 0.85–0.87). Resilience was measured at T1, T3 and T4. Items are scored from 1 to 5 and cut-offs for the BRS are based on mean scores:1.00–2.99 = low resilience; 3.00–4.300 = normal resilience and 4.31–5.00 = high resilience.
Confidence. The three-item Confidence in Coping with Adverse Events scale (CAE) includes items such as ‘If I was involved in an adverse event for which I thought I held some responsibility I know the things I would do to help manage my stress levels’.15,16 It has acceptable internal reliability (Cronbach's alphas = 0.47–0.69) and detects learning changes.15,16 Confidence was measured at all time points.
Burnout. We included six items from the Oldenburg Burnout Inventory (OLBI), the three highest loading items on each subscale of ‘exhaustion’ and ‘disengagement’. Items included ‘After my work, I usually feel worn out and weary’. The present version has been used in previous evaluations to detect change.15,16 It had acceptable internal reliability in the present study (Cronbach's alphas = 0.63–0.74). Burnout was measured at T1, T3 and T4.
Depression. The 9-item Patient-Health Questionnaire-9 (PHQ-9) is widely used to measure depression.20–22 It captures change 21 and had good internal reliability in the present study (Cronbach's alphas = 0.84–0.88). Depression was measured at T1, T3 and T4. Total scores of 0–4 suggest no depression, 5–9 suggest mild depression, 10–14 suggest moderate depression, 15–19 suggest moderate-severe depression and >20 suggest severe depression.
Reactions to the training questionnaire. This contained eight items exploring how relevant, useful and engaging the training was (see Table 3) which have been used in previous evaluations.15,16,18,23 This was administered at T2.
Table 3.
Feedback following the training.
| Item | Strongly disagree (%) | Disagree (%) | Neither agree/disagree (%) | Agree (%) | Strongly agree (%) | Missing (%) |
|---|---|---|---|---|---|---|
| 1. The workshops were relevant for medical students | 0 (0) | 0 (0) | 3 (3.2) | 31 (33.3) | 59 (63.4) | 0 (0) |
| 2. I learned skills in the workshops which will be useful in future | 0 (0) | 0 (0) | 1 (1.1) | 30 (32.3) | 62 (66.7) | 0 (0) |
| 3. There was adequate time to cover the material | 0 (0) | 1 (1.1) | 1 (1.1) | 33 (35.5) | 58 (62.4) | 0 (0) |
| 4. I found the workshops engaging | 0 (0) | 0 (0) | 10 (10.8) | 36 (38.7) | 47 (50.5) | 0 (0) |
| Yes | No | Prefer not to say | Missing | |||
| 5. Were there any aspects of the workshops you did not find useful? | 12 (12.9) | 78 (83.9) | 1 (1.1) | 2 (2.2) | ||
| 6. Is there anything else you would have liked to see in the workshops which were not included? | 19 (20.4) | 72 (77.4) | 1 (1.1) | 1 (1.1) | ||
| 7. If you were involved in a stressful placement event, would you do anything differently as a result of attending these workshops? | 85 (91.4) | 4 (4.3) | 0 (0) | 4 (4.3) | ||
| 8. Would you recommend the workshops to other medical students | 89 (95.6) | 2 (2.2) | 2 (2.2) | 0 (0) | ||
Analysis plan
Descriptive analyses were calculated and reported. To assess for changes over time, we employed simple random intercepts linear mixed models (restricted maximum likelihood estimation) through the R lme4 package. 24 Each outcome was modeled separately, and timepoint as a categorical variable was our main predictor (baseline, T1 and post-intervention time-points: T2, T3 and T4). Analyses were conducted both unadjusted for any demographic variables, and subsequently adjusted for key variables (age, gender). Analyses were conducted using participants with complete data (‘CC’) only, or as a conservative sensitivity analysis, carrying participants’ last recorded outcome score forward to subsequent time points (‘LPCF’). Model-implied marginal means were compared for all outcomes in Holm-adjusted post hoc t-tests for all types of models. Estimates of standardised mean differences (Cohen's ds) are outlined and were calculated as the average difference in outcomes between two comparator time points (e.g., CAE mean T1 minus T3), divided by the standard deviation of differences.
Results
There were 262 expressions of interest, 131 completed baseline questionnaires and 115 (93/80.9% women; mage 23.9; SD = 2.8) were finally recruited. There was greater demand for Reboot than spaces available. There were 8 (7.0%) participants in year 3 of their degree, 46 (40.0%) in year 4, 54 (47.0%) in year 5. Six participants were in other years (5.2%) and one preferred not to say (0.9%). There were 57 (49.6%) White participants, 27 (23.5%) Asian or Asian British participants, 13 Black or Black British participants (11.3%) and 15 (13.0%) describing their ethnicity as ‘other’. Three (2.6%) preferred not to say. There were 42 (36.5%) participants from Northern England, 25 (21.7%) from Southern England, 35 (30.4%) from the Midlands, 9 (7.8%) from Scotland, 1 (0.9%) from Wales and 3 (2.6%) preferring not to say.
Primary feasibility outcomes: Demand, recruitment and retention. Expressions of interest (n = 262) and recruited participants (n = 115), both surpassed the demand and recruitment targets of 80. Of the 115 participants recruited, 83 (72.2%) completed all intervention elements and 82 (71.3%) provided T4 data, surpassing retention targets of 70% and 50%, respectively.
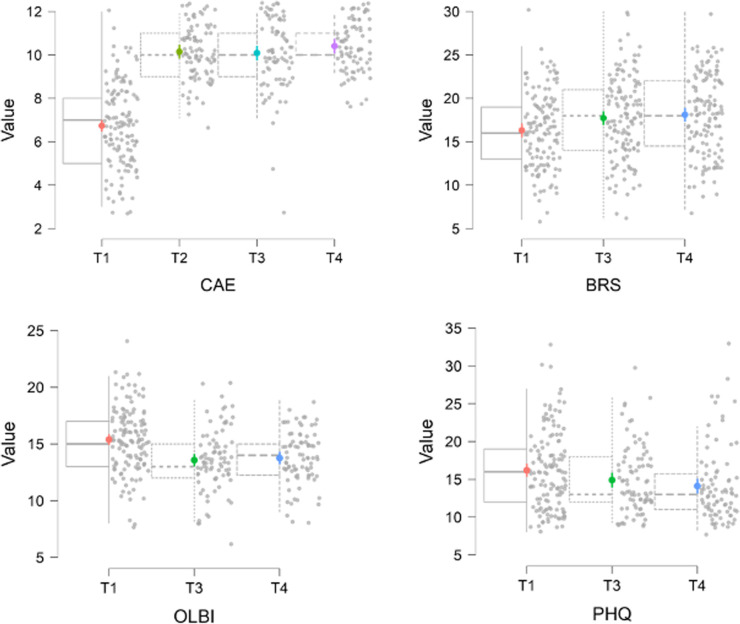
Secondary outcomes. For descriptive statistics, see Table 1. For unadjusted model-fit statistics, see Table 2 and for plots, see Figure 1. All analyses indicated considerable clustering, supporting the use of random intercepts. The proportion of variance explained by all indicator variables was mixed across measures. In all cases, a large proportion of variance was explained by fixed time points explained plus random effects. Adjusting the model for control variables did not substantially alter model fit. Though association sizes were generally smaller, results in LPCF models were consistent with CC analyses. CC results are reported here. LPCF analyses and adjusted analyses are in Appendix 2.
Table 1.
Descriptive statistics for all outcome measures.
| Measure (timepoint) | Mean | Standard deviation | Min, Max |
|---|---|---|---|
| Resilience (BRS) | |||
| T1 (n = 130) | 16.33 | 4.34 | 6, 30 |
| T3 (n = 83) | 18.40 | 4.66 | 6, 30 |
| T4 (n = 82) | 19.00 | 4.34 | 12, 30 |
| Confidence in coping with adverse wvents (CAE) | |||
| T1 (n = 131) | 6.74 | 1.90 | 3, 12 |
| T2 (n = 93) | 10.13 | 1.22 | 7, 12 |
| T3 (n = 83) | 10.06 | 1.66 | 3, 12 |
| T4 (n = 82) | 10.38 | 1.17 | 8, 12 |
| Burnout (OLBI-abbreviated) | |||
| T1 (n = 131) | 15.40 | 2.87 | 8, 24 |
| T3 (n = 83) | 13.61 | 2.74 | 6, 20 |
| T4 (n = 82) | 13.84 | 2.34 | 8, 19 |
| Depression (PHQ-9) | |||
| T1 (n = 129) | 7.27 | 5.21 | 0, 24 |
| T3 (n = 83) | 6.00 | 4.60 | 0, 21 |
| T4 (n = 81) | 5.32 | 5.02 | 0, 24 |
Table 2.
Unadjusted complete case (CC) models: results.
| Outcome | BIC | Variance (ICC) | R2m | R2c | Predictor | Contrast | beta | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Resilience (BRS) | 1602 | 74% | 7% | 76% | Time | T3 versus T1 | 2.19*** | 1.51–2.87 |
| T4 versus T1 | 2.83*** | 2.15–3.52 | ||||||
| Confidence (CAE) | 1462 | 30% | 52% | 67% | Time | T2 versus T1 | 3.41*** | 3.05–3.77 |
| T3 versus T1 | 3.35*** | 2.98–3.72 | ||||||
| T4 versus T1 | 3.67*** | 3.29–4.04 | ||||||
| Burnout (OLBI) | 1368 | 62% | 9% | 66% | Time | T3 versus T1 | −1.82*** | −2.33 to −1.33 |
| T4 versus T1 | −1.63*** | −2.13 to −1.14 | ||||||
| Depression (PHQ-9) | 1685 | 73% | 3% | 73% | Time | T3 versus T1 | -1.30*** | -2.09 to −0.51 |
| T4 versus T1 | -2.09*** | -2.88 to −1.30 |
p ≤ 0.001; BIC = Bayesian Information Criterion; ICC = Intraclass Correlation Coefficient; R2m = R squared marginal; R2c = R-squared conditional; CI = confidence interval. For adjusted and LPCF analyses, see Appendix 2.
Figure 1.
Outcome variables at each time point. CAE = Confidence in coping with adverse events; SUM_BRS = Brief Resilience Scale; SUM_OLBI = Oldenburg Burnout Inventory; PHQ_SUM = Patient Health Questionnaire (Depression).
Resilience (BRS) scores increased significantly from T1 to T3 (d = 0.68) and from T1 to T4 (d = 0.89). Resilience remained static from T3 to T4, suggesting stability in initial gains (pHolm = 0.13). At T1, n = 79 (60.8%) reported low resilience, n = 49 (34.6%) reported normal resilience and n = 2 (1.5%) reported high resilience. At T3, n = 27 (44.6%) reported low resilience, n = 41 (49.4%) reported normal resilience and n = 5 (6%) reported high resilience. At T4, n = 30 (36.6%) reported low resilience, n = 48 (58.5%) reported normal resilience and n = 4 (4.9%) reported high resilience.
Confidence (CAE) scores increased significantly following T1 (T2: d = 1.76; T3: d = 1.57; T4: d = 1.72). There were no further increases following T2, suggesting stability in initial gains (T2–T3 pHolm = 0.68; T2–T4 pHolm = 0.17; T3–T4 pHolm = 0.11).
Burnout (OLBI) scores reduced significantly from T1 to T3 (d = −0.73) and from T1 to T4 (d = −0.69). There was no difference from T3 and T4, suggesting stability in gains (pholm = 0.38).
Depression scores (PHQ) indicated a significant decrease following T1 (T1–T3: d = −0.32; T1–T4: d = −0.52). There was a small, but further decrease from T3 to T4 (d = −0.29; pholm = 0.04). At T1, n = 37 (32.7%) participants had no depression symptoms. At T3, n = 42 (50.6%) participants had no depression symptoms and at T4, n = 46 (56.8%) had no depression symptoms. Of the 73 participants who completed all time points, at T1, n = 18 (25%) reported no depression symptoms, at T3, n = 32 (43.8%) reported no depression symptoms and at T4, n = 38 (52.1%) reported no depression symptoms.
Reactions to the workshops were overall positive (Table 3). For open-text comments provided in response to questions 5–8, see Appendix 3.
Discussion
This is the first study to evaluate a targeted intervention for medical students which is specifically tailored towards providing support with placement-related stressors, Reboot. Reboot was found to be acceptable by medical students and feasible to evaluate in this group. With high demand, recruitment targets exceeded feasibility thresholds and retention thresholds were met. Participating in Reboot was associated with significant increases in measures of resilience and confidence in coping with adverse events, and significant reductions in measures of burnout and depression. At the final time point, a greater proportion of participants were in the ‘normal’ and ‘high’ ranges for resilience, and more students were screening as asymptomatic for depression. Reactions to the workshops were generally positive, with most participants agreeing that Reboot was engaging, imparted useful skills and stating that they would do something differently, if they were involved in a stressful placement event, as a result of participating. The present findings extend existing knowledge in two main ways.
First, these positive results have relevance for the literature into supportive interventions in medical students more widely. To date, evaluations of supportive interventions for medical students have focused on generic interventions such as mindfulness and yoga. 10 These have been criticised on conceptual grounds, suggesting they lack relevance for medical students and professionals.11,12 Systematic reviews have also reported mixed evidence regarding their effectiveness. For example, in a review of 39 studies testing interventions such as mindfulness, stress management training and psychoeducation in medical students, findings were mixed, with no clear evidence suggesting any individual intervention was effective for improving depression or burnout. 10 In a systematic review of mindfulness interventions in medical students and junior doctors, no significant reductions in depression or anxiety were identified. 25 In this context, the current study results are promising, identifying Reboot – a targeted, tailored intervention – as a potential candidate intervention suitable for investigation in further controlled studies.
Second, this is the first study to adapt and evaluate the Reboot Coaching Programme in medical students. Previous studies have evaluated Reboot in a range of healthcare student and professional groups including midwives, paramedics, obstetricians and physician associate students 15 and critical care nurses. 18 A workshop-only version of Reboot (without a coaching call) has also been evaluated in trainee surgeons. 16 As with previous studies of Reboot, demand was sufficient and recruitment targets were met. Attrition was also comparable to previous studies,18,21 as were results regarding outcome variables.15,16,18 This further confirms that Reboot is a flexible intervention which can be adapted for different healthcare professional student groups with similar outcomes.
Rates of depression in our sample were higher than anticipated, with two-thirds reporting mild, moderate or severe depression symptoms at baseline. This is higher than previous studies of medical students in the UK, 26 US, 27 Korea 28 and Vietnam, 29 and could be due to two main reasons. First, while we did not recruit students with depression, students experiencing depression may have been more likely to be attracted to the study. Second, mental health in young adults has suffered over the COVID-19 pandemic period, and our sample may also reflect this wider trend. 30
Strengths and limitations
The study benefited from adequate statistical power and a varied participant group, who were both geographically diverse within the UK, and ethnically diverse. Rates of missing data for individual variables were also low. The study was primarily limited by a lack of a control group, which prevents conclusions regarding causality being drawn. Furthermore, we did not monitor psychoactive medications which the participants were prescribed, which may have influenced their mental health and response to the intervention. We also did not include a method of monitoring participant engagement, beyond monitoring retention rates. In future studies, researchers could consider addressing this by monitoring (1) the number of participants who have their camera on during the workshops, (2) the number of participants who speak during whole-group discussions, and the number of utterances per participant and (3) a memory test of the material covered.
Implications for practice and research
There is a need for more effective interventions for improving mental health outcomes in medical students. The present study suggests that Reboot is a feasible intervention in this group with potential benefits for mental health outcomes in medical students. Reboot is suitable for delivery to this group in its present form and as an online intervention, could be delivered from a central hub to students from a group of medical schools simultaneously. While Reboot has only been tested in UK participants to date, it is based on CBT principles which have been found to be suitable for use in a range of countries and cultures including Asian and African nations.31–33 As such, it is possible that Reboot could be an internationally translatable intervention for medical students. However, further research is needed to (1) evaluate Reboot with a control group, to establish whether improvements can be attributed to the programme and (2) involve cohorts from other countries, to establish its potential generalisability.
Conclusion
Mental health concerns affect a high proportion of medical students. Medical students are the physician workforce of the future; interventions to support, strengthen and retain this group are imperative. This is the first study to evaluate an intervention for medical students which is specifically tailored towards providing support with placement-related stressors, Reboot. Our findings indicate that Reboot is a feasible and acceptable intervention in medical students and may lead to benefits for improving resilience and confidence and reducing depression and burnout.
Supplemental Material
Supplemental material, sj-docx-1-scm-10.1177_00369330231213981 for Reboot coaching programme: a mixed-methods evaluation assessing resilience, confidence, burnout and depression in medical students by Judith Johnson, Lucy Pointon, Rebecca Talbot, Rebecca Coleman, Luke Budworth, Ruth Simms-Ellis, Katharina Vogt, Dialechti Tsimpida, Chandra Shekha Biyani, Reema Harrison, Gloria Cheung, Colin Melville, Vijay Jayagopal and William Lea in Scottish Medical Journal
Acknowledgements
The views expressed in this publication are those of the authors and not necessarily those of the British Medical Association Foundation or the National Institute for Health and Care Research or the Department of Health and Social Care. We would like to thank our participants for their time in taking part in the evaluation. We would also like to thank the UK Medical Schools Council for supporting our recruitment to the project.
Footnotes
Author contributions: The work was originally conceived and designed by JJ, RSE, RH and WL. Further substantial design decisions to ensure compliance, safety and feasibility were made by DT, SB, KV and GC. Data acquisition, preparation, analysis and interpretation were conducted by JJ, LP, RT, RC and LB. The work was originally drafted by JJ and LB, with critical revisions offered by RT, RC, LP, RSE, KV, DT, SB, RH, GC and WL. All authors approved the final version and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Data access statement: Anonymous qualitative data is available as a supplementary file. Anonymised quantitative data can be accessed on request from the lead author at j.johnson@leeds.ac.uk.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics: The study was approved by the School of Psychology, University of Leeds Ethics Committee (date: 19/01/2022; approval number: PSYC-542).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The work was funded by an award from the British Medical Association Foundation, the Scholarship Grant 2021. It was also supported by the National Institute for Health and Care Research Yorkshire and Humber ARC (NIHR 200166).
ORCID iDs: Judith Johnson https://orcid.org/0000-0003-0431-013X
Shekhar Biyani https://orcid.org/0000-0003-3443-8425
William Lea https://orcid.org/0000-0002-0847-445X
Supplemental material: Supplemental material for this article is available online.
References
- 1.Slavin SJ. Medical student mental health: culture, environment, and the need for change. JAMA 2016; 316: 2195–2196. [DOI] [PubMed] [Google Scholar]
- 2.Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among US medical students. Ann Intern Med 2008; 149: 334–341. [DOI] [PubMed] [Google Scholar]
- 3.Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA 2016; 316: 2214–2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puthran R, Zhang MW, Tam WWet al. et al. Prevalence of depression amongst medical students: a meta-analysis. Med Educ 2016; 50: 456–468. [DOI] [PubMed] [Google Scholar]
- 5.Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online 2018; 23: 1530558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu KS, Chibnall JT, Slavin SJ. Maladaptive perfectionism, impostorism, and cognitive distortions: threats to the mental health of pre-clinical medical students. Acad Psychiatry 2019; 43: 381–385. [DOI] [PubMed] [Google Scholar]
- 7.Weurlander M, Lönn A, Seeberger A, et al. How do medical and nursing students experience emotional challenges during clinical placements? Int J Med Educ 2018; 9: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ratanawongsa N, Teherani A, Hauer KE. Third-year medical students’ experiences with dying patients during the internal medicine clerkship: a qualitative study of the informal curriculum. Acad Med 2005; 80: 641–647. [DOI] [PubMed] [Google Scholar]
- 9.Martinez W, Lo B. Medical students’ experiences with medical errors: an analysis of medical student essays. Med Educ 2008; 42: 733–741. [DOI] [PubMed] [Google Scholar]
- 10.Witt K, Boland A, Lamblin M, et al. Effectiveness of universal programmes for the prevention of suicidal ideation, behaviour and mental ill health in medical students: a systematic review and meta-analysis. Evid-Based Ment Health 2019; 22: 84–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gridley K. Resilience training is just a band-aid solution for doctor well-being. Emergency Medicine Australasia 2018; 30: 261–262. [DOI] [PubMed] [Google Scholar]
- 12.Balme E, Gerada C, Page L. Doctors need to be supported, not trained in resilience. BMJ 2015; 351: h4709. [Google Scholar]
- 13.Chew-Graham CA, Rogers A, Yassin N. ‘I wouldn’t want it on my CV or their records’: medical students’ experiences of help-seeking for mental health problems. Med Educ 2003; 37: 873–880. [DOI] [PubMed] [Google Scholar]
- 14.Dyrbye LN, Eacker A, Durning SJ, et al. The impact of stigma and personal experiences on the help-seeking behaviors of medical students with burnout. Acad Med 2015; 90: 961–969. [DOI] [PubMed] [Google Scholar]
- 15.Johnson J, Simms-Ellis R, Janes G, et al. Can we prepare healthcare professionals for involvement in adverse events? Feasibility study of a resilience training intervention. BMC Health Serv Res 2020; 20: 1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Ghunaim T, Johnson J, Biyani CS, et al. Evaluation of the reboot coaching workshops among urology trainees: A mixed method approach. BJUI Compass 2023; 4: 533–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smidt A, Balandin S, Sigafoos Jet al. et al. The Kirkpatrick model: a useful tool for evaluating training outcomes. J Intellect Dev Disabil 2009; 34: 266–274. [DOI] [PubMed] [Google Scholar]
- 18.Vogt K, Grange A, Johnson J, et al. Study protocol for the online adaptation and evaluation of the ‘Reboot’ (Recovery-boosting) coaching programme, to prepare critical care nurses for, and aid recovery after, stressful clinical events. Pilot Feasibility Stud 2022; 8: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith BW, Dalen J, Wiggins K, et al. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008; 15: 194–200. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cameron IM, Crawford JR, Lawton Ket al. et al. Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. Br J Gen Pract 2008; 58: 32–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoon S, Lee Y, Han C, et al. Usefulness of the patient health questionnaire-9 for Korean medical students. Acad Psychiatry 2014; 38: 661–667. [DOI] [PubMed] [Google Scholar]
- 23.Personal communication from a sonographer gathered as part of PPI activities. 2016.
- 24.Bates D, Mächler M, Bolker BMet al. et al. Fitting linear mixed-effects models using lme4. Journal of Statistical Software. 2015; 67: 1–48. [Google Scholar]
- 25.Sekhar P, Tee QX, Ashraf G, et al. Mindfulness-based psychological interventions for improving mental well-being in medical students and junior doctors. Cochrane Database Syst Rev 2021; 12: CD013740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Honney K, Buszewicz M, Coppola Wet al. et al. Comparison of levels of depression in medical and non-medical students. Clin Teach 2010; 7: 180–184. [DOI] [PubMed] [Google Scholar]
- 27.Halperin SJ, Henderson MN, Prenner Set al. et al. Prevalence of anxiety and depression among medical students during the COVID-19 pandemic: a cross-sectional study. J Med Educ Curric Dev 2021; 8: 2382120521991150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoon S, Lee Y, Han C, et al. Usefulness of the patient health questionnaire-9 for Korean medical students. Acad Psychiatry 2014; 38: 661–667. [DOI] [PubMed] [Google Scholar]
- 29.Pham T, Bui L, Nguyen A, et al. The prevalence of depression and associated risk factors among medical students: an untold story in Vietnam. PLoS One 2019; 14: e0221432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alzueta E, Podhajsky S, Zhao Q, et al. Risk for depression tripled during the COVID-19 pandemic in emerging adults followed for the last 8 years. Psychol Med 2023; 53: 2156–2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ara J, Deeba F. Clinical experiences of CBT practitioner in Bangladesh. J Psychiatry 2020; 23: 472. [Google Scholar]
- 32.Naeem F, Gul M, Irfan M, et al. Brief culturally adapted CBT (CaCBT) for depression: a randomized controlled trial from Pakistan. J Affect Disord 2015; 177: 101–107. [DOI] [PubMed] [Google Scholar]
- 33.Naab F, Brown R, Ward EC. Culturally adapted depression intervention to manage depression among women with infertility in Ghana. J Health Psychol 2021; 26: 949–961. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-scm-10.1177_00369330231213981 for Reboot coaching programme: a mixed-methods evaluation assessing resilience, confidence, burnout and depression in medical students by Judith Johnson, Lucy Pointon, Rebecca Talbot, Rebecca Coleman, Luke Budworth, Ruth Simms-Ellis, Katharina Vogt, Dialechti Tsimpida, Chandra Shekha Biyani, Reema Harrison, Gloria Cheung, Colin Melville, Vijay Jayagopal and William Lea in Scottish Medical Journal