Abstract
US health care administrative spending is approximately $1 trillion annually. A major operational area is the financial transactions ecosystem, which has approximately $200 billion in spending annually. Efficient financial transactions ecosystems from other industries and countries exhibit 2 features: immediate payment assurance and high use of automation throughout the process. The current system has an average transaction cost of $12 to $19 per claim across private payers and providers for more than 9 billion claims per year; each claim on average takes 4 to 6 weeks to process and pay. For simple claims, the transaction cost is $7 to $10 across private payers and providers; for complex claims, $35 to $40. Prior authorization on approximately 5000 codes has an average cost of $40 to $50 per submission for private payers and $20 to $30 for providers. Interventions aligned with a more efficient financial transactions ecosystem could reduce spending by $40 billion to $60 billion; approximately half is at the organizational level (scaling interventions being implemented by leading private payers and providers) and half at the industry level (adopting a centralized automated claims clearinghouse, standardizing medical policies for a subset of prior authorizations, and standardizing physician licensure for a national provider directory).
Keywords: health care spending, administrative spending, claims processing, prior authorization
Introduction
US health care administrative spending—defined as all activities in support of the delivery of care, including payment transactions, back-office corporate and operational functions, customer and patient services, and administrative clinical support—is approximately $1 trillion annually.1 A central question in health care is how to reduce this amount. In this article, we focus on the approximately $200 billion in annual spending related to interactions among patients, providers, and payers involving claims processing, payment, patient collections, and prior authorization.1 We refer to this spending as the financial transactions ecosystem.
We look at the criteria that must be met to optimize the financial transactions ecosystem and offer examples of US service industries and health care systems abroad that have done this successfully. We then break down the financial transactions ecosystem from an operational productivity lens—specifically, service throughput, cost efficiency, and quality outcomes. We conclude with a review of the organizational- and industry-level interventions available today.
We note that the author team is drawn from the academic and management consulting worlds. We base our insights on data from both academic sources and industry experience. A Technical Appendix delineates the information sources and estimation methodology we use.
What other US industries and countries have achieved
Industries with efficient financial transactions ecosystems share 2 features: immediate payment assurance and high use of automation throughout the process. By payment assurance, think of a meal at a restaurant where the customer uses a credit card. The restaurant needs immediate assurance that the payment will be transferred, not immediacy in the dollars transferred. Obtaining immediate payment assurance in health care could free up more than $200 billion on the balance sheets of hospitals and physician groups, materially alleviating working capital and debt required to fund operations. In addition, lowering processing costs through automation could improve the cash flow of providers and payers. Both features will require greater use of technology and the harmonization of processes across private payers and providers.
Examples from other US service industries and from health care systems in other countries suggest that this is possible through joint private and public sector action.2-8 For example, the banking system in the United States collaborated in the 1970s to form an automated clearinghouse, which reduced transaction costs, shifted innovation to product design and other areas, and eventually enabled same-day transactions.2 In the airline industry, the private sector collaborated to build an automated booking platform called Sabre, which eventually was adapted to support other airlines, travel agents, and hotels.3
Even health care has examples of more-efficient financial transactions ecosystems. In Israel, patients do not pay providers directly. Instead, co-payments are withdrawn monthly from patients’ bank accounts and sent to their insurance plans, which then reimburse providers, creating payment assurance for all stakeholders.4 In Singapore, the central government manages an information hub for health care data across multiple payers (both private and public), enabling patients to log on to 1 site where they can see their comprehensive health records and pay their bills as required.5 Estonia operates a centralized single-payer health system in which a fully automated claims process features data transferring directly from patient records into a billing platform, also allowing providers to monitor the status of their claims in real time.6
There are also examples of more efficient financial transactions ecosystems within the US health care system. With prescription drugs, in the 2000s, both the public and private sectors innovated to enable a common infrastructure for the processing of electronic prescriptions. In the later part of the decade, some came together into a single network, which allowed for the immediate transfer of prescription information about a patient and the ability to see the patient's cost at the time insurance is provided, all at a very low transaction cost.7 Further, nearly 20 states have created all-payer claims databases to collect information on claims to monitor cost and quality.8
Challenges in the health care financial transactions ecosystem
The US health care system is more complicated than other US services industries and health care systems in other countries, with more than 6000 hospitals, 900 payers, and 11 000 nonemployed physician groups (defined as hospital-affiliated and independent practices with 5 or more physicians).9-11 Such large numbers of participants inevitably complicate many administrative processes, including financial transactions.
Much research has focused on the financial transactions ecosystem, but unlike these studies, we took an operational productivity lens.1,12-18 We examine 3 dimensions: service throughput, cost efficiency, and quality outcomes.
Service throughput
Nearly 9 billion claims are processed annually, or approximately 30 per insured life in the United States.19,20 On average, approximately 80% of these claims are either auto-adjudicated or adjudicated with a minor adjustment. With regard to prior authorization, we estimate that private payers have in place approximately 5000 prior authorization codes across procedures, diagnostics, drugs, and sites of care. Of these, more than 90% of prior authorizations are ultimately approved by private payers, but fewer than 25% are auto-determined.
Cost efficiency
We estimate that the average cost to process a single claim is $2 to $4 for private payers and $10 to $15 for providers. For simple claims (80% to 90% of the total), the cost is approximately $7 to $8 per claim, including both private payers and providers; for more complex claims, the joint cost is $35 to $40 (eg, a cesarean section, where the claim could include multiple clinicians such as an OB/GYN and anesthesiologist, multiple payers such as commercial and Medicaid, and multiple conditions such as a postsurgery hospital-acquired infection). Labor is the dominant source of costs, accounting for more than half of total costs for private payers and up to 90% of costs for providers. Other types of costs include technology infrastructure, spanning both the software and hardware needed to facilitate the claims process.
In general, prior authorization remains a labor-intensive process, with an average cost of $40 to $50 per submission for private payers and $20 to $30 for providers. There are also a number of indirect costs, such as physician burnout and employee turnover, associated with the administrative burden of dealing with prior authorization.21
Quality outcomes
On average, a claim can take 4 to 6 weeks to process and pay. This starts with 1 to 2 days for a provider to submit a claim. Private payers process many claims in 1 to 3 days. Some claims require additional steps, such as manual intervention, which result in an additional 1 to 2 weeks. A few claims take several months because of back-and-forth between the payer and the provider. Following payer approval, it may take a few weeks for a provider to be paid, an amount of time usually within prompt-pay statutory rules.
The overall timing of payment has substantial balance sheet consequences for providers. For example, for every week of reduced time-to-payment, working capital on hospitals and physician groups' balance sheets would fall by approximately $25 billion to $40 billion, money that could then be used for other productive investments.
For all of the benefits associated with prior authorization in cost management and appropriate care, there are also drawbacks, including delays in care and workforce burden.22-25 Further, all of the financial transactions processes require additional datasets, such as provider directories. These directories need regular updating, with more than 1 million professionally active physicians today and an average turnover rate of 6% to 7% annually as doctors move to other organizations or retire.26 Generally, physicians have to update some component of their job information—such as location, specialization, or work status—every 6 to 12 months. Each update can take up to a few hours. Overall, physicians have to submit approximately 18 credentialing applications between payers, hospitals, and other facilities annually, creating frustration for both physicians and private payers.27,28 Inaccuracies in these provider directories can inhibit patient access and diminish member experience, just as with prior authorizations.
The savings potential of available interventions
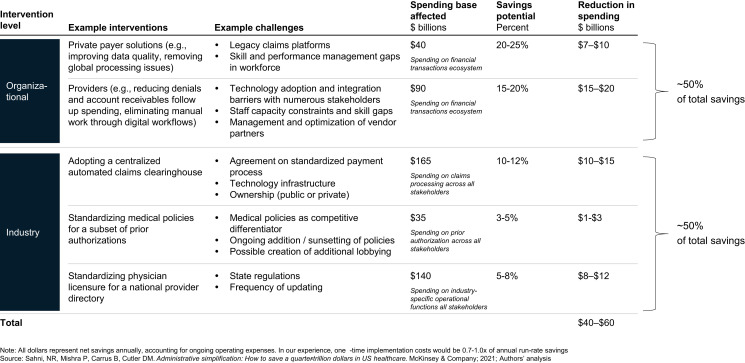
Previous research has estimated the savings opportunity on the overall financial transactions ecosystem.1,13,29-31 Our approach differs from these analyses by specifically dividing interventions into 2 levels: organizational and industry (see the Technical Appendix for more information on how estimated savings by level were made) (Figure 1). By organizational level, we mean interventions that individual organizations can control and implement on their own or through bilateral collaboration between organizations. Industry-level interventions are those that require broader, structural collaboration across the health care sector.
Figure 1.
Net annual savings opportunity within financial transactions ecosystem by intervention level.
Organizational-level interventions
While there are many organizations involved in US health care, this article focuses on 3 stakeholder groups: private payers, hospitals, and physician groups. These stakeholders represent approximately two-thirds of US health care administrative spending.1 Along with internal innovation and performance management, a vendor ecosystem has recently emerged.
Private payers
For private payers, best-in-class claims processing is automated (∼95% of claims are adjudicated without manual intervention), accurate (with improved precision of adjudication to minimize adjustments and reworks), and efficient (claims requiring manual intervention have clear performance targets, and the people tasked with handling them have the necessary training and tools). Achieving these ends can result in lower administrative spending through reduced call volumes, increased labor productivity, and lower employee attrition. It can also improve the patient and clinician experience through faster processing times and less back-and-forth on adjustments. Despite recent advances, most private payers continue to have inefficient payment processes, driven by legacy claims platforms, limited improvement in process efficiency and automation, and skill and performance management gaps in their workforce.
The focus on improving the operational productivity of administrative functions could also complement the longstanding need of payers to root out fraud, waste, and abuse (FWA)—a problem costing more than $60 billion annually.32 A useful system of FWA detection would run in real time, alongside the billing and prior authorization systems. Given that the savings accrue to medical spending, we did not include them in this analysis. However, examples such as what the credit card industry has accomplished show that reducing FWA is possible.33
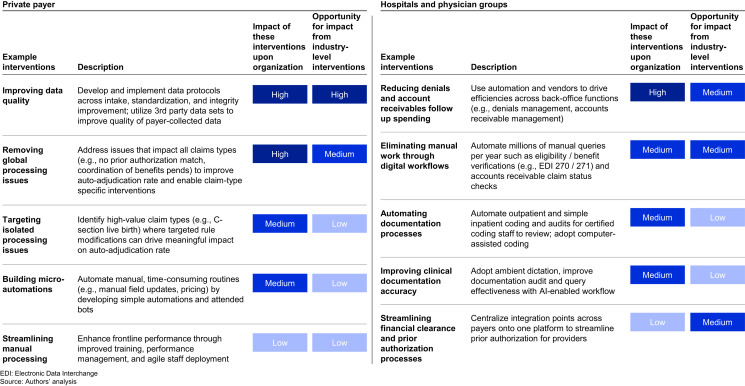
Leading private payers are generally improving operational productivity in 5 ways: improving data quality, removing global processing issues, targeting isolated processing issues, building micro-automations, and streamlining manual processing (Figure 2). Evidence from successful examples suggests that extending these interventions to all private payers could reduce spending by 20% to 25%, or $7 billion to $10 billion annually.
Figure 2.
Examples of organizational-level interventions to reduce administrative spending associated with financial transactions.
Take the case of 1 national payer with consistently strong performance. Seeking to improve performance, the payer identified 2 areas of interventions that would yield the greatest impact: minimizing rework driven by adjusted claims and increasing claims automation. To reduce the volume of claims adjustments, the payer focused on finding the most important sources of inefficiency, such as provider and member data discrepancies and prior authorization record matches. This effort decreased the number of claims that were adjudicated but then required an adjustment by 40% (from >5% to <3%). To improve auto-adjudication, the payer used AI (artificial intelligence)-enabled interventions like claim logic refinement and natural language processing for medical record processing. This initiative increased the auto-adjudications rate from 87% to more than 92%.
Hospitals and physician groups
For hospitals and physician groups, claims processing is commonly referred to as revenue cycle management and is divided into 3 areas: the front end, which includes patient scheduling and insurance verification; the mid-cycle, which includes utilization management and appropriate documentation; and the back end, which includes accounts-receivable management, underpayment and denials recovery, and appeals management.
The preparation of claims for submission to payers is costly. Part of this cost reflects the complexity that hospitals and physician groups face in preparing an accurate bill in a timely fashion; our experience shows that a substantial portion of initial claims have errors versus what would be found in a detailed audit reviewing the associated activities (>15%).
Despite advances in technology and the vendor ecosystem, hospitals and physician groups still face challenges, including technology adoption, staff capacity constraints and skill gaps, management and optimization of vendor partners, and changing payer medical policies.
Revenue cycle management is labor-intensive, whether carried out internally or outsourced. Leading hospitals and physician groups are generally improving operational productivity in 5 ways: reducing denials and account receivables follow-up spending, eliminating manual work through digital workflows, automating documentation processes, improving clinical documentation accuracy, and streamlining financial clearance and prior authorization processes (Figure 2). Evidence from highly optimized revenue cycle operations suggests that extending these interventions to all hospitals and physician groups could reduce spending by 15% to 20%, or $15 billion to $20 billion annually.
Take the example of 1 large health system's attempt to improve payer denial overturn rates and reduce write-offs. The health system developed a large payer benefit plan policy dataset through natural language processing to better manage billing interventions and implemented a denial management optimization algorithm to more expeditiously respond to payer denials. The health system also built out a revamped organizational structure that centralized the non–patient-facing case management staff to improve efficiency. These interventions improved the overturn rate—the rate of successful appeals to denials—from 16% of all pre-billing medical necessity denials (excludes all denials with a dollar value of less than or equal to zero) to 32%.
Industry-level interventions
Industry-level interventions generally play 2 types of roles: acceleration and augmentation of organizational-level interventions. We focused on 3 industry-level interventions that could accelerate and augment the operational productivity interventions private payers and providers are undertaking.
Adopting a centralized automated claims clearinghouse
Private payers and providers use a number of claims clearinghouses based on region and line of business. Generally, national and larger regional private payers and hospitals have worked to lower costs per claim by working with external vendors and allocating more internal resources to the claims process. Physician groups, smaller hospitals, and smaller private payers, lacking the resources of larger organizations to address the claims process, face higher transaction costs per claim. One potential intervention is a more centralized, automated clearinghouse that could accelerate the standardization and automation of the financial transactions ecosystem. That could allow smaller organizations to achieve similar transaction costs per claim as the larger organizations. In addition, the use of incentives to promote the centralized clearinghouse could reduce transaction costs further. We estimate that accelerating standardization and automation to decrease transaction costs to match those of the most efficient organizations could reduce spending by 10% to 12%, or $10 billion to $15 billion annually.
A historical barrier to this intervention is the need for the appropriate technology infrastructure. With recent technology advances, it could be technically feasible to migrate to a central clearinghouse, but questions about governance and ownership will need to be addressed first. One such example is who owns it. The banking industry developed its centralized claims clearinghouse through the private sector, while health care systems in other countries have built clearinghouses through the public sector. Important factors to consider when choosing an ownership model include speed to launch, level of standardization, ability to execute, and motivation for ongoing innovation.
Eventually, additional savings could come from introducing data such as electronic medical records into the clearinghouse, which could reduce transaction costs for other financial transactions, such as prior authorization.
Standardizing medical policies for a subset of prior authorizations
Prior authorization is a specific function within the medical management operations of private payers and revenue cycle management functions of hospitals and physician groups. In the market-based US healthcare system, prior authorization has come about as a check and balance between these stakeholder groups. The primary goal of prior authorization is to assess the medical necessity and coverage of health care services and procedures according to established criteria or guidelines under the provisions of payer programs to prevent excess and unnecessary utilization. Benefits of prior authorization can include flagging newer, better treatments, and improving the quality of care (eg, in evolving specialties such as oncology where the standards of care are being refined). While we acknowledge the clinical aspects of prior authorization, we are focused on the direct, administrative spending associated with this process.
Overall, the administration of prior authorization is complex not only because of the total number of prior authorizations but also because private payers may have different policies for the same treatment or drug, depending on how permissive the policy is. For example, approval to administer magnetic resonance imaging for back pain may vary from payer to payer and even from insurance product to product offered by a payer.
In our experience, the opportunity to simplify and standardize common policies across the industry is only, if at all, for a subset of prior authorizations, while leaving others to be customized by private payers. The primary goal would be to focus standardization on policies that have clear evidence—for example, when should a medication refill be approved? Complex decisions associated with expensive treatments and uncertain clinical presentation could remain the decision of the individual payer.
We estimate that some standardization, which will decrease the staff required to review prior authorizations at both private payers and providers, could reduce spending by 3% to 5%, or $1 billion to $3 billion annually. Approximately half of this staff is clinical, including physicians and nurses. Relieving this burden could allow clinicians to spend more time on patient care—an increasingly important consideration given ongoing physician and nursing shortages.34
One barrier to moving in this direction is that differentiation in medical policies is part of the value proposition for private payers when vying for customers and managing medical costs. Employers who purchase insurance and patients may also object to the change, to the extent that they choose plans based on variation in prior authorization requirements. Another challenge is the ongoing maintenance of this system as new treatments arise and older ones are discontinued. Finally, innovation of new interventions such as intelligent and personalized processes driven by generative AI, which could have a greater savings impact, may be stifled.
Standardizing physician licensure for a national provider directory
There are more than 1 million professionally active physicians in the United States.26 On average, each contracts with more than 20 private payers.35 Each payer has its own process for ensuring a physician is in its provider directory. This is needed to establish the back-and-forth mechanisms for financial transactions.
Separately, each physician undergoes a credentialing process, usually state-driven (as some raise concerns about lower-quality-care provision and de-emphasizing localized standards of care), although there are some basic, consistent national components.28 These include graduating from a school accredited by the American Medical Association, passing a comprehensive national medical licensing examination, and meeting standards for work history and health status. Standardizing the licensure process would reduce the amount of time physicians spend to comply with state regulations, especially when changing states or hospital affiliations.36 The private sector has created systems like the Federation Credentials Verification Service to aid physicians in this process, with the goal of reducing compliance time and costs.37 We estimate that fully standardizing physician licensure to decrease nonclinical staff needed for this process could reduce spending by $7 billion to $10 billion annually. In addition, creating 1 centrally managed directory could further reduce spending by $1 billion to $2 billion annually.
Conclusion
We estimate that the total reduction in spending from these interventions would be $40 billion to $60 billion annually, split approximately half at the organizational level and half at the industry level. Put another way, the savings are a bit more than 1% of total US health care spending. The total is not trivial. Ongoing operating costs are factored into the savings—that is, the savings are net of new spending needs. In addition, there will be start-up costs to achieving these run-rate savings, normally 0.7 to 1.0 times the total.1 Another benefit of these interventions is potentially freeing up tens of billions of dollars on balance sheets.
For the most part, carrying out these interventions requires no new technology. Rather, the interventions push stakeholders to prioritize operational productivity—specifically, service throughput, cost efficiency, and quality outcomes.
The current financial transactions ecosystem has arisen, in part, by design and, in part, by accident. Many health care organizations view their data as proprietary and patients value data privacy; thus, data sharing is limited. Private payers have legacy computer systems and are hesitant to invest in newer systems without a clear purpose. There have been public sector efforts to address the situation, although they have not been fully implemented. The Health Insurance Portability and Accountability Act of 1996 required a common claims form. The Affordable Care Act of 2010 called for a national system to determine benefits eligibility, coverage information, patient cost-sharing to improve collections at the time of care, real-time claim status updates, auto-adjudication standards, and real-time and automated approval for referrals and prior authorizations.38
Traditionally, such needs have taken a back seat to more pressing clinical or financial concerns. In part, this is because the potential savings from these actions have been hidden. But our analysis suggests that the potential savings could be substantial. Thus, the financial transactions ecosystem deserves more attention than it has received.
Supplementary Material
Acknowledgments
The authors thank Allan Gold, Vishnu Murale, Ivan Orellana, Ryan Smith, and Zoe Williams for their contributions to this article.
Contributor Information
Nikhil R Sahni, Department of Economics, Harvard University, Cambridge, MA 02138, United States; Center for US Healthcare Improvement, McKinsey & Company, Boston, MA 02210, United States.
Pranay Gupta, Center for US Healthcare Improvement, McKinsey & Company, Boston, MA 02210, United States.
Michael Peterson, Center for US Healthcare Improvement, McKinsey & Company, Boston, MA 02210, United States.
David M Cutler, Department of Economics, Harvard University, Cambridge, MA 02138, United States; National Bureau of Economic Research, Cambridge, MA 02138, United States.
Supplementary material
Supplementary material is available at Health Affairs Scholar online.
Conflicts of interest
Please see ICMJE form(s) for author conflicts of interest. These have been provided as supplementary materials.
Notes
- 1.Sahni NR, Mishra P, Carrus B, Cutler DM. Administrative Simplification: How to Save a Quarter-Trillion Dollars in US Healthcare. McKinsey & Company; 2021. Accessed September 23, 2023. https://www.mckinsey.com/industries/healthcare/our-insights/administrative-simplification-how-to-save-a-quarter-trillion-dollars-in-us-healthcare [Google Scholar]
- 2.History of Nacha and the ACH Network. Nacha. April 20, 2019. Accessed September 23, 2023. www.nacha.org/content/history-nacha-and-ach-network
- 3.Wichter Z. How one computer system tangled up several airlines. The New York Times. April 29, 2019. Accessed September 23, 2023. www.nytimes.com/2019/04/29/business/airlines-computer-glitch-sabre.html
- 4.Roosa T, Osborn R, Mossialo E, et al. Israel. The Commonwealth Fund. June 5, 2020. Accessed September 23, 2023. www.commonwealthfund.org/international-health-policy-center/countries/israel
- 5.Roosa T, Osborn R, Mossialo E, et al. Singapore. The Commonwealth Fund. June 5, 2020. Accessed September 23, 2023. www.commonwealthfund.org/international-health-policy-center/countries/singapore
- 6.World Health Organization. The role of digital claims management for Estonia's health insurance: a leverage for making healthcare purchasing more strategic. February 14, 2023. Accessed September 23, 2023. www.who.int/publications/i/item/9789240066687
- 7.The history of electronic prescribing (eRx) and its benefits in healthcare tech. Covetus. August 7, 2020. Accessed September 23, 2023. https://www.covetus.com/blog/the-history-of-electronic-prescribing-erx-and-its-benefits-in-healthcare-tech
- 8. [Interactive State Report Map. APCD Council. June 17, 2015. Accessed September 23, 2023.]. www.apcdcouncil.org/state/map
- 9.https://www.aha.org/ American Hospital Association. Fast facts on U.S. hospitals, 2021, partial data from 2019 survey. Updated January 2021.
- 10.https://www.definitivehc.com/ Top physician groups by size and Medicare charges. Definitive Healthcare, Healthcare Insights; 2021.
- 11.https://www.iii.org/ Facts + statistics: Industry overview. Insurance Information Institute, August 2021.
- 12.Tseng P, Kaplan RS, Richman BD, Shah MA, Schulman KA. Administrative costs associated with physician billing and insurance-related activities at an academic health care system. JAMA. 2018;319(7):691–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Institute of Medicine (US) Roundtable on Evidence-Based Medicine; Yong PL, Saunders RS, Olsen LA, eds. The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. National Academies Press (US); 2010. 4, Excess Administrative Costs. https://www.ncbi.nlm.nih.gov/books/NBK53942/ [PubMed] [Google Scholar]
- 14.Himmelstein DU, Jun M, Busse R, et al. . A comparison of hospital administrative costs in eight nations: US costs exceed all others by far. Health Aff (Millwood). 2014;33(9):1586–1594. [DOI] [PubMed] [Google Scholar]
- 15.Morra D, Nicholson S, Levinson W, Gans DN, Hammons T, Casalino LP. US physician practices versus Canadians: spending nearly four times as much money interacting with payers. Health Aff (Millwood). 2011;30(8):1443–1450. [DOI] [PubMed] [Google Scholar]
- 16.Casalino LP, Nicholson S, Gans DN, et al. . What does it cost physician practices to interact with health insurance plans? Health Aff (Millwood). 2009;28(Suppl 1):w533–w543. [DOI] [PubMed] [Google Scholar]
- 17.Sakowski JA, Kahn JG, Kronick RG, Newman JM, Luft HS. Peering into the black box: billing and insurance activities in a medical group. Health Aff (Millwood). 2009;28(Suppl 1):w544–w554. [DOI] [PubMed] [Google Scholar]
- 18.Blanchfield BB, Heffernan JL, Osgood B, Sheehan RR, Meyer GS. Saving billions of dollars–and physicians’ time–by streamlining billing practices. Health Aff (Millwood). 2010;29(6):1248–1254. [DOI] [PubMed] [Google Scholar]
- 19. [2022 CAQH Index. CAQH. Accessed September 23, 2023.]. www.caqh.org/sites/default/files/2022-caqh-index-report%20final%20spread%20version.pdf
- 20. [Health insurance coverage of the total population. Kaiser Family Foundation. October 28, 2022. Accessed September 23, 2023.]. www.kff.org/other/state-indicator/total-population/?dataView=1¤tTimeframe=0&sortModel=%7B%22colId%22%3A%22Location%22%2C%22sort%22%3A%22asc%22%7D
- 21. [2022 AMA prior authorization (PA) physician survey. American Medical Association. 2023. Accessed September 23, 2023.]. https://www.ama-assn.org/system/files/prior-authorization-survey.pdf
- 22.Shah ED, Amann ST, Hobley J, Islam S, Taunk R, Wilson L. 2021 National survey on prior authorization burden and its impact on gastroenterology practice. Am J Gastroenterol. 2022;117(5):802–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pereira DE, Kamara E, Krueger CA, et al. . Prior authorization in total joint arthroplasty: a survey of the American Association of Hip and Knee Surgeons Membership. J Arthroplasty. 2023;38(7):1203–1208. [DOI] [PubMed] [Google Scholar]
- 24.Kim H, Srivastava A, Gabani P, Kim E, Lee H, Pedersen KS. Oncology trainee perceptions of the prior authorization process: a national survey. Adv Radiat Oncol. 2021;7(2):100861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barnett BS, Bodkin JA. A survey of American psychiatrists concerning medication prior authorization requirements. J Nerv Ment Dis. 2020;208(7):566–573. [DOI] [PubMed] [Google Scholar]
- 26. [Professionally Active Physicians. Kaiser Family Foundation. June 8, 2023. Accessed September 23, 2023.]. www.kff.org/other/state-indicator/total-active-physicians/?currentTimeframe=0&sortModel=%7B%22colId%22%3A%22Location%22%2C%22sort%22%3A%22asc%22%7D
- 27.Cutler DM, Ly DP. The (paper) work of medicine: understanding international medical costs. J Econ Perspect. 2011;25(2):3–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bell DL, Katz MH. Modernize medical licensing, and credentialing, too-lessons from the COVID-19 pandemic. JAMA Intern Med. 2021;181(3):312–315. [DOI] [PubMed] [Google Scholar]
- 29.Richman BD, Kaplan RS, Kohli J, et al. . Billing and insurance-related administrative costs: a cross-national analysis. Health Aff (Millwood). 2022;41(8):1098–1106. [DOI] [PubMed] [Google Scholar]
- 30.Cutler D, Wikler E, Basch P. Reducing administrative costs and improving the health care system. N Engl J Med. 2012;367(20):1875–1878. [DOI] [PubMed] [Google Scholar]
- 31.Jiwani A, Himmelstein D, Woolhandler S, Kahn JG. Billing and insurance-related administrative costs in United States’ health care: synthesis of micro-costing evidence. BMC Health Serv Res. 2014;14(1):556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501–1509. [DOI] [PubMed] [Google Scholar]
- 33.The history and evolution of fraud. Fraud. Accessed September 23, 2023. https://www.fraud.com/post/the-history-and-evolution-of-fraud
- 34.Berlin G, Burns F, Lapointe M, Essick C, Murphy M. Nursing in 2023: how hospitals are confronting shortages. May 5, 2023. Accessed September 23, 2023. https://www.mckinsey.com/industries/healthcare/our-insights/nursing-in-2023
- 35.Urwongse R. How many payer contracts do providers have? Defacto health. June 6, 2023. Accessed September 23, 2023. defacto.health/2023/04/25/how-many-payer-contracts-do-providers-have/
- 36. [The hidden causes of inaccurate provider directories. CAQH; 2019. Accessed September 23, 2023.]. www.caqh.org/sites/default/files/explorations/CAQH-hidden-causes-provider-directories-whitepaper.pdf
- 37. [Federation Credentials Verification Service. Federation of State Medical Boards. Accessed September 23, 2023.]. https://www.fsmb.org/fcvs/
- 38.Kocher RP. Reducing administrative waste in the US health care system. JAMA. 2021;325(5):427–428. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.