Abstract
Child and infant mortality is a global problem. Almost half of deaths of children under age 5 years occur in the neonatal period, the first 28 days of life, with 2.4 million neonatal deaths globally in 2020. Sub-Saharan Africa has disproportionately high numbers of neonatal deaths. Ghana's neonatal mortality rate is 22.8 per 1000 live births and remains behind targets set by the United Nations Sustainable Development Goals. Quality antenatal care, postnatal monitoring, breastfeeding support, and postnatal family planning are important in preventing neonatal deaths. While Ghana has made progress in making care more financially accessible, it has not been matched with the improvements in the critical infrastructure required to ensure quality health care. The improvements have also not eliminated out-of-pocket costs for care, which have hindered progress in decreasing infant mortality. Policymakers should consider investments in health care infrastructure, including expanding public–private partnerships. Policies that improve workforce development programs, transportation infrastructure, and health insurance systems improvements are needed.
Keywords: infant mortality, neonatal mortality, child mortality, Ghana, policy, health care infrastructure, workforce development, systems thinking
Introduction
Child and infant mortality are global public health concerns and common indicators used to assess the population health status of the community.1-3 Despite global progress in reducing child and infant mortality, the 2022 Child Mortality Report by the United Nations (UN) Inter-agency Group for Child Mortality Estimation reports that, in 2021, approximately 5 million children died before age 5.2,4 This child mortality rate estimation refers to the number of deaths per 1000 live births of neonates, those in their first month of life, infants aged 1–11 months, and children under age 1–4 years.4 The leading causes of neonatal mortality globally are premature birth and birth complications.4,5 Almost half of all under-5 deaths occurred during the first 28 days of life, known as the neonatal period, the riskiest period for child survival.4 Although under-5 child mortality has decreased within the last 30 years almost everywhere in the world, neonatal mortality is not decreasing as much as mortality in children between 1 and 59 months.4 Progress has been made in reducing infant and child mortality, but stark disparities between and within countries persist.4 Thus, child survival chances vary dramatically among regions, with children born in sub-Saharan Africa at the highest risk of infant death in the world.3,6 Globally, sub-Saharan Africa remains the area with the highest child mortality disparity rates, reporting 1 in 13–14 children dying before reaching the age of 5 years, 14 times higher than the risk in high-income countries, and accounting for 56% of global under-5 deaths.1,4 A newborn aged 1–28 days old in sub-Saharan Africa is 11 times more likely to die than a newborn in the Australia/New Zealand region.4
The Sustainable Development Goals (SDGs), adopted by the UN, call for a reduction in neonatal mortality to 12 or fewer deaths per 1000 live births and a reduction in under-5 mortality to 25 or fewer per 1000 live births by 2030.7,8 The goal to decrease the neonatal mortality rate to 12 or fewer deaths per 1000 live births has already been achieved by 126 countries; however, 63 countries will not meet this goal if current trends continue.4 Most countries that are not meeting the goal will need to double their rate of progress to achieve the goal.4 Similarly, 133 countries have met the under-5 mortality target, and 54 countries are not on target to meet the goal.4,8
Ghana is among the countries needing to accelerate progress toward the under-5 and neonatal mortality targets.9 Ghana's neonatal mortality rate is 22.8 deaths per 1000 live births, and its under-5 mortality rate is 44 deaths per 1000 live births.10 Ghana's infant mortality rate is 32.6 deaths per 1000 live births, and its stillbirth rate is 21.4 deaths per 1000 live births.10 While Ghana's neonatal and under-5 mortality rates are better than many countries in the region, with Nigeria's at 34.9 and 110.8 deaths per 1000 live births, respectively, and Cote d’Ivoire's at 55.9 and 74.9 deaths per 1000 live births, respectively,10 Ghana's rate of progress remains behind targets set by the SDGs.9
The determinants of infant mortality are multifactorial and complex and include factors related to the mother’s age, health, residence, employment status, marital status, educational level, and age at first birth.3,6 Additional significant factors include the sex of the child, desire for pregnancy, gestational age, birth type, birth size, preceding birth interval, breastfeeding status, breastfeeding initiation, vaccination status, antenatal care visits, place of delivery, use of family planning, family size, available source of water and household electricity, birth asphyxia, distance to the health facility, age of the infant, maternal medical complications during pregnancy, and maternal death at birth.3,6,11,12 Many of these factors are primarily preventable bio-demographic factors. Preterm birth, low birth weight, neonatal sepsis and other infections, birth asphyxia, congenital anomalies, neonatal jaundice, and pneumonia are frequent causes of infant mortality in Ghana.13-15 Hence, the possibility of impactful change is significant since these include eminently addressable leading causes of global neonatal mortality, such as prematurity, infections, intrapartum-related events, and access to health care.8
Importance of a skilled antenatal, delivery, postnatal, and neonatal care workforce
A key factor in preventing infant deaths is quality medical care in all stages of pregnancy, delivery, and post-delivery for both mother and neonate. Infants whose mothers attend the recommended number of high-quality antenatal visits with care provided by a doctor have much better odds of survival.15,16 Skilled antenatal care throughout pregnancy has been found to significantly reduce the risk of having a low-birth-weight infant, which is a high-risk factor for neonatal mortality.16 Recent research indicates that the quality of antenatal care, such as screening and clinical counseling, is likely even more important than the number of visits in reducing neonatal mortality.15-17
An infant delivered by a doctor is almost 3 times more likely to survive than those delivered by traditional birth attendants.15 Most births in Ghana occur at a facility; however, most neonatal deaths occur at home soon after birth among infants born in a hospital, which suggests a need to improve immediate neonatal care and screening of symptoms after birth in both hospital and community settings.14 The most common cause of neonatal death following home birth is infection, indicating a need for improved access to skilled birth attendants who are trained in infection-control procedures.14 Early breastfeeding initiation has also been found to reduce the risk of neonatal infection, which can be facilitated by direct breastfeeding support and maternal health education.18
High-risk deliveries require well-resourced hospitals for delivery and extended neonatal care.14 Identifying high-risk pregnancies and deliveries, such as multiple births, requires early and consistent antenatal care and highly skilled medical team involvement throughout pregnancy and birth to ensure the best outcomes.19,20 Congenital anomalies make up a large portion of neonatal deaths in low- and middle-income countries.20 Many of these conditions require early access to skilled surgical care for infant survival.20 Skilled specialist care is also essential for preterm infants to support feeding needs, ensure they receive adequate oxygen, maintain the necessary temperature for survival, and provide other life-saving therapies.21
Postnatal maternal care is also essential, not only for the health of the mother but also to prevent future infant mortality. Spacing of births less than 24 months apart comes with a significantly higher risk of infant mortality due to a higher risk of high blood pressure and premature membrane rupture.19 Postnatal family planning services must be routine and widely available to optimize the spacing of births to at least 24 months apart.19
Current programs and policy successes in Ghana
Ghana has implemented several programs over the past 2 decades that have contributed to progress in reducing infant and maternal mortality. The implementation of the free maternal health care policy in 2008 as a component of the National Health Insurance Scheme (NHIS) mandates free health care coverage for antenatal visits, delivery, and postnatal and neonatal care to women registered with the insurance.22,23 The program was credited with an increase in the registration of more than 300 000 mothers between 2008 and 2012.24 A study comparing 2 countries that implemented a free maternal health care policy, Ghana and Burkina Faso, with 2 countries in the region, Nigeria and Zambia, that did not have such a policy found that the policy was associated with a 45% reduction in risk for neonatal mortality and a 54% reduction in risk for infant mortality between 2008 and 2014.22
The Ghana Child Health Policy and the Child Health Strategy focused on improving health care quality and accessibility, prevention, and treatment of diseases affecting infants.25 This resulted in improved standards for managing diarrhea and the availability of immunization programs, which increased infant vaccination rates.25 Further strides were made in addressing diseases affecting infants and children by the Ghana Essential Health Intervention Project and the Community-based Health Planning and Services (CHPS) by increasing the distribution of services to rural areas.25
Ghana's CHPS provides community-based support and a basic facility to rural communities and mobilizes the resources within the community to do so, involving many stakeholders, including community leaders, community health nurses, and traditional birth attendants.24 The CPHS has contributed to increased utilization of skilled medical facilities for births when one was within close proximity, increased utilization of contraception, and has been a contributing factor in lowering the infant mortality rate in Ghana by acting as gatekeepers.24,26,27 Despite the progress achieved with these programs and policies, many barriers to care remain.
Barriers to care
Out-of-pocket costs
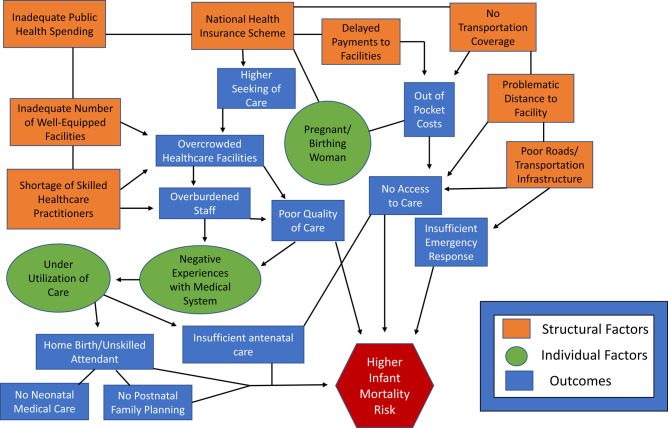
Studies have determined that many women covered by the NHIS free maternal health care policy continue to face out-of-pocket costs for ultrasound and other laboratory services, drugs, supplies, and items required for childbirth.27-30 There is also a lack of funding for transport for births, birth emergencies, or when a woman or neonate is referred to a better-resourced hospital for more skilled care, requiring even more out-of-pocket costs.27 Health practitioners and managers have indicated that reimbursement from the NHIS is frequently delayed, erratic, or amounts are inadequate to provide quality care to pregnant women, necessitating out-of-pocket charges.27-32 This may be resulting in the underutilization of services (Figure 1).
Figure 1.
Framework of factors and outcomes for infant mortality risk.
Inadequate number and distribution of facilities, skilled birth attendants, and neonatal specialists
Although the increased utilization of services created by the free maternal health care policy has improved financial access to care, an adequate supply of skilled services and facilities to accommodate this increase is lacking in many areas in Ghana.33,34 Living near a health care facility is associated with the use of antenatal care,35 and women who live at a problematic distance from a health facility are at higher risk for neonatal death than women who live near facilities.23 Facilities for care and delivery are not geographically accessible to many rural women.23,27,34,36-38 Transportation to facilities many miles away for both antenatal care and delivery is cost-prohibitive for many women and results in low utilization of services.23,27,34-36 Skilled physicians, midwives, and birth attendants are in short supply and unevenly distributed throughout the country, generally in urban areas, resulting in more significant shortages in some areas than in others.25,34,38 Women and neonates receiving facility care also face significant risks, as many skilled birth attendants lack training in neonatal care and many facilities are overcrowded, which evidence suggests contributes to inadequate postnatal screening and monitoring before discharge, resulting in infants dying at home soon after birth in a facility.14
Limited resources and infrastructure supporting the health system
The health system relies on well-functioning infrastructure, such as available transportation systems, including efficient roads, water, and electricity.27 Many CHPS facilities in northern Ghana were found to be under-resourced, lacking reliable water, electricity services, and adequate physical space.27,39 Poor road conditions between many rural facilities and better-resourced hospitals and facilities hinder transport for emergencies, resulting in a higher risk of neonatal deaths.23 Health care facilities also rely on an adequate supply of essential drugs and medical equipment. Recent studies have found these resources to be inadequate to support the needs of facilities serving pregnant and birthing women covered under the free maternal health care policy.27,30,33,38
Poor quality of care resulting in women choosing not to seek health care
Several studies of maternal and child health care in Ghana found many overburdened and under-resourced health care facilities, with staff shortages and heavy workloads for both patient care workers and administrators.27,33,34 Health care workers in rural areas often experience poor working conditions and cannot provide quality care to birthing mothers and neonates.14,27,33,34 Both patients and health care providers in several communities report maternal care as substandard.33,37 Higher utilization of health care facilities in urban areas, brought forth by the free maternal health care policy, may be having the unintended effect of rendering the care poor quality and negatively impacting hospital birth outcomes due to crowding of facilities and lack of capacity to meet the demands.23 Many women choose not to seek antenatal care and give birth at home with a traditional birth attendant because they experienced poor care, including long wait times, negative attitudes of health care workers, in some cases neglect or abuse, and a lack of privacy at a health care facility during prior pregnancies and births.23,33,37 The dissatisfaction with the health care system is widespread among women in Ghana.23,28,33,34,37
Discussion of policy recommendations
A primary focus for policymakers in reducing infant and neonatal mortality in Ghana should be to substantially improve the availability of quality skilled medical care. The shift from home births to facility births alone will not likely affect outcomes if the facilities are not equipped to provide skilled care.14,25 Improving the quality of medical care for pregnant, birthing, and postnatal women, neonates, and infants will affect outcomes for those using the medical system and encourage more women to use lifesaving medical pregnancy, delivery, and infant care services.
A 2020 analysis of 46 countries in sub-Saharan Africa found that increased public health expenditure to support health service infrastructure was associated with reduced infant and neonatal mortality.40 It should be noted that the success of increased public health expenditure in impacting health outcomes depends on efficient allocation and oversight of funds.41 Other economic factors, such as GDP (Gross Domestic Product) per capita, also impact health outcomes.41 However, recent analyses support the need for Ghana to increase its public health expenditure. Past public health expenditure increases have been associated with reduced infant mortality, and current expenditures are inadequate to meet the SDGs.42-44 Spending recommendations to improve access to quality maternal and infant health care are outlined here in order of priority.
Invest in medical facility infrastructure
Early access to facilities that can respond to obstetric and infant emergencies and provide effective neonatal surgical care can significantly reduce infant deaths.20,23,27,34,38,45 Inadequate physical space, medical equipment, and essential drugs are sources of problems in the quality provision of obstetric and neonatal care, and maternal concern for being referred to a very distant hospital at a high cost is factoring into decisions not to utilize medical systems for pregnancy and delivery care.23,33,34,38 The construction of facilities in under-resourced areas is foundational to address many of the aforementioned issues and should be prioritized. An infrastructure with cutting-edge facilities and medical equipment paired with skilled providers can lead to the development of innovative interventions in neonatal/obstetrics emergencies and referrals from CHPS facilities to prevent undue neonatal complications.46 Increased resources for the CHPS compounds are also needed to improve birth outcomes in rural areas where women receive care.39
Strong consideration should be given to the value of public–private partnerships to bolster the health care infrastructure in Ghana. Private-sector health care facilities, including nonprofit health care organizations, can partner with public institutions to improve service delivery and health outcomes.47,48
Increase workforce development efforts and incentivize health care workers to practice in lower-resourced communities
There is a shortage of skilled maternal health care workers in Ghana, including nurses, midwives, and specialist doctors, and these practitioners are disproportionately located in urban areas.33,34,42 Programs to increase quality maternal and neonatal medical training and incentivize health care workers to remain in or relocate to low-resourced areas should be strongly considered.38 Evidence suggests that infrastructure investments, as outlined above, create better working conditions for medical practitioners and serve to retain staff, positively impacting maternal and child health outcomes.38 Creating improved housing for staff has also been suggested as a solution for attracting skilled health care workers.46 Alleviating overburdened health care staff in under-resourced areas will improve the overall quality of care for pregnant and birthing mothers and neonates.
Dedicate resources to transport services for maternal care and transportation infrastructure
A lack of transportation and spatial access to medical facilities hinders many women in accessing antenatal, delivery, postnatal, and neonatal care.27,34 The NHIS free maternal health care policy can be expanded to include transportation services for low-income women.27 Investment in safe and efficient road networks will also improve emergency response time and enable more women to travel for life-saving medical care.27,39,46 Another consideration for stakeholders is the use of mobile health clinics, which are effective for providing antenatal and postnatal care in remote areas.49,50
Prioritize timely reimbursement and expand coverage to minimize out-of-pocket charges
Delays and inconsistencies in claims reimbursements result in out-of-pocket charges to patients who should be receiving free care, discouraging women from utilizing the recommended antenatal care and skilled delivery.27-32 Government officials should take action to ensure that the NHIS is both sustainable and efficient.51 Improvements to the claims process must be ongoing, as evidence suggests that, although an electronic claims system was implemented, timely payment of claims continued to be lacking.51 Funding should be used to ensure expedited reimbursement payments to health care providers.46 Hidden out-of-pocket expenses for required delivery items are also cost-prohibitive to many and discourage facility delivery.28 The free maternal health care policy should ensure full coverage for required delivery items and services.28
Conclusion
A systems approach is needed to minimize barriers to quality prenatal, delivery, and postnatal maternal and child health care in Ghana to accelerate progress toward the SDG of decreasing neonatal mortality to 12 or fewer deaths per 1000 live births. Evidence suggests that strengthening multiple systems, including transportation and utility infrastructure, skilled workforce and medical facility capacity, and full financial coverage of health care services, would improve the utilization and quality of services throughout pregnancy, birth, and the postnatal period, and improve birth outcomes and neonatal mortality rates. The engagement of multiple stakeholders is crucial for fostering public–private partnerships and community involvement in strengthening the interacting systems that impact maternal and neonatal health care.
Supplementary Material
Contributor Information
Danielle Poulin, TERSHA LLC, Alpharetta, GA 30005, United States.
Gloria Nimo, Amazing Grace Children's Charity, Dansoman Accra GA-542-8377, Ghana.
Dorian Royal, Amazing Grace Children's Charity, Dansoman Accra GA-542-8377, Ghana.
Paule Valery Joseph, Amazing Grace Children's Charity, Dansoman Accra GA-542-8377, Ghana.
Tiffany Nimo, Amazing Grace Children's Charity, Dansoman Accra GA-542-8377, Ghana.
Tyra Nimo, Amazing Grace Children's Charity, Dansoman Accra GA-542-8377, Ghana.
Kofi Sarkodee, Amazing Grace Children's Charity, Dansoman Accra GA-542-8377, Ghana.
Sharon Attipoe-Dorcoo, TERSHA LLC, Alpharetta, GA 30005, United States; Healthcare Administration Program, College of Business, Texas Woman's University, Denton, TX 76204, United States.
Supplementary material
Supplementary material is available at Health Affairs Scholar online.
Notes
- 1.Nwagbara UI, Osuala EC, Chireshe R, et al. Mapping evidence on factors contributing to maternal and child mortality in sub-Saharan Africa: a scoping review protocol. PLoS One. 2022;17(8):e0272335. doi. 10.1371/journal.pone.0272335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UN Inter-agency Group for Child Mortality Estimation . Subnational under-five and neonatal mortality estimates, 2000-2021 estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation, United Nations Children's Fund. Published 2023. Accessed December 27, 2023. https://childmortality.org/wp-content/uploads/2023/10/UN-IGME_Subnational_U5MR_and_NMR_2000-2021-1.pdf
- 3.Irana T, Mekebo GG, Diriba G, Sisay AL, Woldeyohannes B, Yohannes Z. Determinants of infant mortality in Oromia region, Ethiopia. Ann Med Surg (Lond). 2023;85(6):2791–2796. 10.1097/MS9.0000000000000842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UN Inter-agency Group for Child Mortality Estimation . Levels and trends in child mortality: 2022 report estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation. Published 2023. United Nations Children's Fund. Accessed December 28, 2023. https://childmortality.org/wp-content/uploads/2023/01/UN-IGME-Child-Mortality-Report-2022.pdf
- 5.Griffin JB, Jobe AH, Rouse D, McClure EM, Goldenberg RL, Kamath-Rayne BD. Evaluating WHO-recommended interventions for preterm birth: a mathematical model of the potential reduction of preterm mortality in Sub-Saharan Africa. Glob Health Sci Pract. 2019;7(2):215–227. 10.9745/GHSP-D-18-00402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahinkorah BO. Maternal age at first childbirth and under-five morbidity in sub-Saharan Africa: analysis of cross-sectional data of 32 countries. Arch Public Health. 2021;79(1):151. 10.1186/s13690-021-00674-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Nations . Sustainable Development Goal 3. Accessed August 29,2023. https://sdgs.un.org/goals/goal3
- 8.Lawn JE, Bhutta ZA, Ezeaka C, Saugstad O. Ending preventable neonatal deaths: multicountry evidence to inform accelerated progress to the sustainable development goal by 2030. Neonatology. 2023;120(4):491–499. 10.1159/000530496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United Nations . Child-related SDG progress assessment for Ghana. Accessed August 29, 2023. https://data.unicef.org/sdgs/country/gha/
- 10.UN Inter-agency Group for Child Mortality Estimation . Child mortality estimation: Ghana. Accessed August 29, 2023. https://childmortality.org/data
- 11.Argawu AS, Mekebo GG. Risk factors of under-five mortality in Ethiopia using count data regression models, 2021. Ann Med Surg (Lond). 2022;82:104764. 10.1016/j.amsu.2022.104764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tiruneh SA, Zeleke EG, Animut Y. Time to death and its associated factors among infants in sub-Saharan Africa using the recent Demographic and Health Surveys: shared frailty survival analysis. BMC Pediatr. 2021;21(1):433. 10.1186/s12887-021-02895-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tette EMA, Nartey ET, Nuertey BD, et al. The pattern of neonatal admissions and mortality at a regional and district hospital in the Upper West Region of Ghana; a cross sectional study. PLoS One. 2020;15(5):e0232406. 10.1371/journal.pone.0232406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dare S, Oduro AR, Owusu-Agyei S, et al. Neonatal mortality rates, characteristics, and risk factors for neonatal deaths in Ghana: analyses of data from two health and demographic surveillance systems. Glob Health Action. 2021;14(1):1938871. 10.1080/16549716.2021.1938871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Annan GN, Asiedu Y. Predictors of neonatal deaths in Ashanti region of Ghana: a cross-sectional study. Adv Public Health. 2018;2018:1–11. 10.1155/2018/9020914 [DOI] [Google Scholar]
- 16.Banchani E, Tenkorang EY. Determinants of low birth weight in Ghana: does quality of antenatal care matter? Matern Child Health J. 2020;24(5):668–677. 10.1007/s10995-020-02895-6 [DOI] [PubMed] [Google Scholar]
- 17.Adongo EA, Ganle JK. Predictors of neonatal mortality in Ghana: evidence from 2017 Ghana Maternal Health Survey. BMC Pregnancy Childbirth. 2023;23(1):556. 10.21203/rs.3.rs-1051118/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edmond KM, Kirkwood BR, Amenga-Etego S, Owusu-Agyei S, Hurt LS. Effect of early infant feeding practices on infection-specific neonatal mortality: an investigation of the causal links with observational data from rural Ghana. Am J Clin Nutr. 2007;86(4):1126–1131. 10.1093/ajcn/86.4.1126 [DOI] [PubMed] [Google Scholar]
- 19.Dwomoh D, Amuasi S, Agyabeng K, Incoom G, Alhassan Y, Yawson AE. Understanding the determinants of infant and under-five mortality rates: a multivariate decomposition analysis of Demographic and Health Surveys in Ghana, 2003, 2008 and 2014. BMJ Glob Health. 2019;4(4):e001658. 10.1136/bmjgh-2019-001658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdul-Mumin A, Anyomih TTK, Owusu SA, et al. Burden of neonatal surgical conditions in northern Ghana. World J Surg. 2020;44(1):3–11. 10.1007/s00268-019-05210-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Belay DM, Worku WZ, Wondim A, Hailemeskel HS, Bayih WA. Predictors of survival among preterm neonates admitted to FelegeHiwot Comprehensive Specialized Hospital, northwest Ethiopia. Front Pediatr. 2022;10:800300. 10.3389/fped.2022.800300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dwomoh D, Agyabeng K, Agbeshie K, et al. Impact evaluation of the free maternal healthcare policy on the risk of neonatal and infant deaths in four sub-Saharan African countries: a quasi-experimental design with propensity score kernel matching and difference in differences analysis. BMJ Open. 2020;10(5):e033356. 10.1136/bmjopen-2019-033356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lambon-Quayefio M, Owoo NS. Determinants and the impact of the National Health Insurance on neonatal mortality in Ghana. Health Econ Rev. 2017;7(1):34. 10.1186/s13561-017-0169-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson FA, Frempong-Ainguah F, Matthews Z, et al. Evaluating the impact of the community-based health planning and services initiative on uptake of skilled birth care in Ghana. PLoS One. 2015;10(3):e0120556. 10.1371/journal.pone.0120556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adua E, Frimpong K, Li X, Wang W. Emerging issues in public health: a perspective on Ghana’s healthcare expenditure, policies and outcomes. EPMA J. 2017;8(3):197–206. 10.1007/s13167-017-0109-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Russell S. Community-based health and planning services: decentralizing Ghana's health system. GU J Health Sci. 2008;5(1). [Google Scholar]
- 27.Dalinjong PA, Wang AY, Homer CSE. The implementation of the free maternal health policy in rural northern Ghana: synthesized results and lessons learnt. BMC Res Notes. 2018;11(1):341. 10.1186/s13104-018-3452-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boah M, Adampah T, Jin B, et al. “I couldn't buy the items so I didn't go to deliver at the health facility”. Home delivery among rural women in northern Ghana: a mixed-method analysis. PLoS One. 2020;15(3):e0230341. 10.1371/journal.pone.023034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anafi P, Mprah WK, Jackson AM, et al. Implementation of fee-free maternal health-care policy in Ghana: perspectives of users of antenatal and delivery care services from public health-care facilities in Accra. Int Q Community Health Educ. 2018;38(4):259–267. 10.1177/0272684X18763378 [DOI] [PubMed] [Google Scholar]
- 30.Azaare J, Akweongo P, Aryeetey GC, Dwomoh D, Asambo SA. Contextualizing the impact of ‘free’ Maternal Healthcare Policy implementation: an intrinsic case analysis of maternal healthcare utilization and stillbirth in Ghana. PREPRINT available at Research Square. 2020. 10.21203/rs.3.rs-103135/v1 [DOI] [Google Scholar]
- 31.Laar AS, Asare M, Dalinjong PA. What alternative and innovative domestic methods of healthcare financing can be explored to fix the current claims reimbursement challenges by the National Health Insurance Scheme of Ghana? Perspectives of health managers. Cost Eff ResourAlloc. 2021;19(1):69. 10.1186/s12962-021-00323-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akweongo P, Chatio ST, Owusu R, Salari P, Tediosi F, Aikins M. Correction: how does it affect service delivery under the National Health Insurance Scheme in Ghana? Health providers and insurance managers perspective on submission and reimbursement of claims. PLoS One. 2021;16(6):e0253357. 10.1371/journal.pone.0253357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ansu-Mensah M, Danquah FI, Bawontuo V, et al. Quality of care in the free maternal healthcare era in sub-Saharan Africa: a scoping review of providers' and managers' perceptions. BMC Pregnancy Childbirth. 2021;21(1):220. 10.1186/s12884-021-03701-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ganle JK, Parker M, Fitzpatrick R, Otupiri E. A qualitative study of health system barriers to accessibility and utilization of maternal and newborn healthcare services in Ghana after user-fee abolition. BMC Pregnancy Childbirth. 2014;14(1):425. 10.1186/s12884-014-0425-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abubakari A, Agbozo F, Abiiro GA. Factors associated with optimal antenatal care use in Northern Region, Ghana. Women Health. 2018;58(8):942–954. 10.1080/03630242.2017.1372842 [DOI] [PubMed] [Google Scholar]
- 36.Atuoye KN, Dixon J, Rishworth A, et al. Can she make it? Transportation barriers to accessing maternal and child health care services in rural Ghana. BMC Health Serv Res. 2015;15(1):333. 10.1186/s12913-015-1005-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adatara P, Strumpher J, Ricks E. Exploring the reasons why women prefer to give birth at home in rural northern Ghana: a qualitative study. BMC Pregnancy Childbirth. 2020;20(1):500. 10.1186/s12884-020-03198-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ameyaw EK, Amoah RM, Njue C, Tran NT, Dawson A. An assessment of hospital maternal health services in northern Ghana: a cross-sectional survey. BMC Health Serv Res. 2020;20(1):1088. 10.1186/s12913-020-05937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dalinjong PA, Wang AY, Homer CSE. Are health facilities well equipped to provide basic quality childbirth services under the free maternal health policy? Findings from rural northern Ghana. BMC Health Serv Res. 2018;18(1):959. 10.1186/s12913-018-3787-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kiross GT, Chojenta C, Barker D, Loxton D. The effects of health expenditure on infant mortality in sub-Saharan Africa: evidence from panel data analysis. Health Econ Rev. 2020;10(1):5. 10.1186/s13561-020-00262-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Akinlo AE, Sulola AO. Health care expenditure and infant mortality in sub-Saharan Africa. J Policy Model. 2019;41(1):168–178. 10.1016/j.jpolmod.2018.09.001 [DOI] [Google Scholar]
- 42.Boachie MK, Põlajeva T, Frimpong AO. Infant mortality in low- and middle-income countries: does government health spending matter? J Dev Policy Pract. 2020;5(1):54–73. 10.1177/2455133320909916 [DOI] [Google Scholar]
- 43.Oladosu AO, Chanimbe T, Anaduaka US. Effect of public health expenditure on health outcomes in Nigeria and Ghana. Health Policy Open. 2022;3:100072. 10.1016/j.hpopen.2022.100072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boachie M K, Ramu K, Põlajeva T. Public health expenditures and health outcomes: new evidence from Ghana. Economies. 2018;6(4):58. 10.3390/economies6040058 [DOI] [Google Scholar]
- 45.Singh K, Speizer I, Barker PM, et al. Evaluating the impact of a hospital scale-up phase of a quality improvement intervention in Ghana on mortality for children under five. Int J Qual Health Care. 2019;31(10):752–758. 10.1093/intqhc/mzz073 [DOI] [PubMed] [Google Scholar]
- 46.Adu J, Mulay S, Owusu MF. Reducing maternal and child mortality in rural Ghana. Pan Afr Med J. 2021;39:263. 10.11604/pamj.2021.39.263.30593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Manhiça AJ. Institutional analysis on public-private partnerships in sub-Saharan Africa's healthcare systems and policy implications. J Int Bus Econ. 2020;21(2):67–96. [Google Scholar]
- 48.Dugle G, Akanbang BAA, Abiiro GA. The complementary role of private healthcare providers: perspectives of the regulator, provider and care seekers in the Upper West Region of Ghana. UDS Int J Deve. 2018;5(1):88–104. 10.47740/236.UDSIJD6i [DOI] [Google Scholar]
- 49.Kojima N, Krupp K, Ravi K, et al. Implementing and sustaining a mobile medical clinic for prenatal care and sexually transmitted infection prevention in rural Mysore, India. BMC Infect Dis. 2017;17(1):189. 10.1186/s12879-017-2282-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Neke NM, Gadau G, Wasem J. Policy makers' perspective on the provision of maternal health services via mobile health clinics in Tanzania—findings from key informant interviews. PLoS One. 2018;13(9):e0203588. 10.1371/journal.pone.0203588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aikins M, Tabong PT-N, Salari P, Tediosi F, Asenso-Boadi FM, Akweongo P. Positioning the National Health Insurance for financial sustainability and universal health coverage in Ghana: a qualitative study among key stakeholders. PLoS One. 2021;16(6):e0253109. 10.1371/journal.pone.0253109 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.