Abstract
Background: The stress level of nurses, especially frontline staff, directly impacts their physical and mental health as well as work efficiency. However, few studies have been conducted to understand the stress level of nurses related to the coronavirus disease 2019 (COVID-19) pandemic.
Aim: The aim of this study is to assess the level of perceived stress among nurses at a tertiary care teaching hospital (King Abdulaziz University Hospital, Jeddah) in Saudi Arabia during the COVID-19 pandemic.
Methods: A cross-sectional survey-based descriptive study involved 1044 nurses working at a tertiary care/teaching hospital in Saudi Arabia. The Perceived Stress Scale (PSS) was used to assess nurses' stress levels. The study was conducted in July 2021 by selecting clinical nurses from different nursing units. Considering the current situation of social isolation, an online cross-sectional survey using Google Forms was used. Data analysis was performed using IBM SPSS Statistics for Windows, Version 21 (Released 2012; IBM Corp., Armonk, New York, United States).
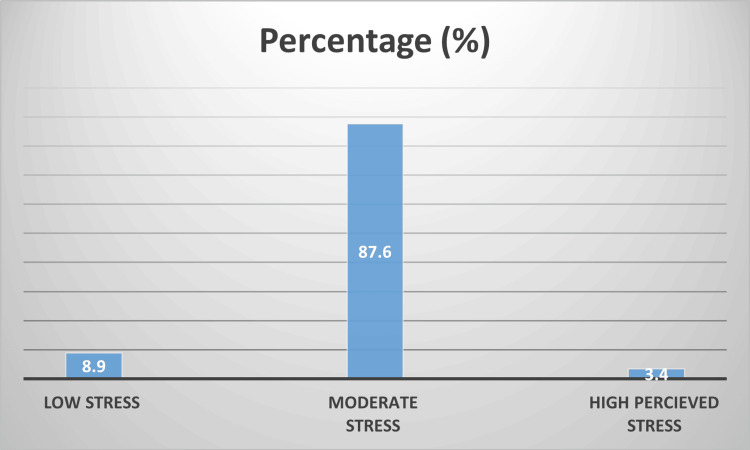
Results: Out of 1044 nursing professionals, 93 (8.9%) reported experiencing low levels of stress, 915 (87.6%) reported moderate levels of stress, and 36 (3.4%) reported high perceived stress during the COVID-19 pandemic. The study found that gender (p=0.001) and nationality (p=0.016) had significant effects on stress levels. The three major causes of stress identified by the nurses were workload, lack of resources, and fear of contracting COVID-19.
Conclusion: Job-related stress continues to be an issue in the nursing workforce. The effects of stress experienced by nurses impact job satisfaction and retention, which, in turn, can affect the quality of patient care. This study highlights that nurses in a tertiary care (COVID care) teaching hospital in our setting often experience stress and anxiety during the pandemic. It is worth noting that this is the first study conducted to understand the level of stress perceived by nursing staff during the COVID-19 pandemic in our current study setting. The findings indicate that a considerable number of nurses experienced moderate levels of stress during COVID-19, which can have implications for patient care. Recognizing and understanding the job-related stressors of nurses can help nurse leaders implement more effective strategies aimed at reducing nurses' stress and subsequently improving patient outcomes.
Keywords: workload, pss score, covid-19, stress, nurses
Introduction
Coronavirus disease 2019 (COVID-19) is a respiratory disease caused by a novel coronavirus (nCoV) that was first identified in Wuhan, China, in December 2019. The outbreak was linked to the South China local Huanan seafood market in Wuhan, Hubei Province, China [1]. Since then, COVID-19 has become a global pandemic, leading to significant challenges for healthcare workers (HCWs) worldwide. The impact on HCWs includes increased demand for medical and nursing staff, rising costs for personal protective equipment (PPE), diagnostic tests for HCWs, beds, and ventilators, as well as a higher mortality rate [2].
The World Health Organization (WHO) declared COVID-19 a Public Health Emergency of International Concern on January 30, 2020, as the disease rapidly spread and reached a pandemic level. As of February 11, 2022, the WHO reported a staggering number of confirmed cases and deaths due to COVID-19 globally [3]. The psychological toll on HCWs during the COVID-19 pandemic is evident from various studies. A meta-analysis conducted by Al Maqbali et al. revealed that approximately one-third of nurses working during the pandemic experienced psychological symptoms [4]. HCWs working in high-risk environments during emergencies, such as the COVID-19 outbreak, are more susceptible to mental health issues like stress, anxiety, and depression [5]. Research conducted among nurses in Hubei province showed that working in isolation wards was a risk factor for depression, anxiety, and stress [6]. Similar studies during previous outbreaks, such as SARS, also found that nurses experienced moderate psychological distress [7]. Additionally, COVID-19 has been identified as an independent risk factor for stress among HCWs [8].
Stress is an inevitable part of life, involving both psychological and physiological components. Chronic stress has been linked to aging and cancer development [9]. The implementation of mass quarantines during the COVID-19 pandemic has caused fear and anxiety among HCWs [10]. Nurses, in particular, have faced heightened stress due to the highly contagious nature of COVID-19. They worry about contracting the virus themselves and transmitting it to others [11]. Frontline health professionals, exposed to COVID-19, are at a higher risk of developing mental health issues [12]. Studies have shown that a significant proportion of HCWs have experienced mood and sleep disturbances during the COVID-19 outbreak [13]. Past research on individuals exposed to SARS outbreaks indicated that they were more likely to experience post-traumatic stress symptoms [14]. In disaster situations, such as the COVID-19 pandemic, nurses tend to face higher levels of adverse mental health outcomes compared to physicians [15].
Despite the risks of infection, nurses' commitment to their profession motivates them to continue caring for COVID-19 patients [16]. Overall, the COVID-19 pandemic has placed immense psychological pressure on HCWs, particularly nurses, due to the challenges they face on the frontline [17]. Understanding and addressing these stress-related issues are crucial to support the well-being and resilience of HCWs during this unprecedented global health crisis [18].
Materials and methods
Study design
A cross-sectional survey-based descriptive design was conducted at a tertiary care teaching hospital (King Abdulaziz University Hospital, Jeddah) in the Kingdom of Saudi Arabia, designated to treat patients with COVID-19.
Sample
The participants in the study were nurses working in different units. We used convenience sampling to select study respondents. The sample consisted of 1044 nurses who were working in different nursing units such as General Wards, Critical Care Areas, Outpatient Departments, Operation Rooms, and Emergency Departments. The inclusion criteria were all nursing staff working currently in our setting and surveys with complete information and the exclusion criteria were surveys with incomplete information. Out of 1433 nurses, 1044 nurses responded to the survey and 4 were excluded due to incomplete information.
Ethical consideration
Ethical approval was obtained from the KAU Biomedical Research Ethics Committee. The participants were asked to answer a ‘YES’ or ‘NO’ question to confirm their willingness to participate voluntarily. After the confirmation, participants were directed to complete the self-reported questionnaire. Nurses were assured that their participation and the information provided would be anonymous and kept confidential.
Data collection
An online survey was conducted using Google Forms from July 18, 2021, to September 6, 2021. The questionnaire collected demographic data of the participants. The online survey link was sent to all nursing staff through the head nurses via email with the approval of the Nursing Director. Participants were informed about the study objectives. The data collection was divided into three sections: first, the perceived stress level of nurses during the COVID-19 outbreak, second the association of selected socio-demographic characteristics with perceived stress level and finally the identification of the three major causes of stress among nurses at KAUH during the COVID-19 pandemic. The Perceived Stress Scale (PSS) was used to assess nurses' stress levels. This scale is a widely used psychological instrument for measuring the perception of stress. It assesses the degree to which situations in one's life are appraised as stressful. Respondents rate items on a five-point Likert scale, ranging from never (0) to very often (4), with a total score range of 0 to 40. PSS scores are categorized as follows: 0 to 13 for low stress, 14 to 26 for moderate stress, and 27 to 40 for high perceived stress [19].
Data analysis
Data analysis was conducted using IBM SPSS Statistics for Windows, Version 21 (Released 2012; IBM Corp., Armonk, New York, United States). Descriptive analysis was used to calculate the mean and percentage. The association between socio-demographic characteristics and perceived stress level was assessed using the chi-square test and Fisher's exact test at 5% and 1% levels of significance. Univariate ordinal regression analysis was performed to assess the association of perceived stress levels with socio-demographic factors. Multivariable logistic regression was also employed to control for the socio-demographic factors of the participants. The study reported both unadjusted/crude odds ratio (COR) obtained from univariate analysis and adjusted odds ratio (AOR) obtained from multivariable logistic regression, which takes into account other covariates, including confounders.
Results
Participant characteristics
A total of 1044 nursing professionals participated in the survey, with the majority being female (88.6%) and male respondents comprising only 11.4%. The distribution of participants across different age groups was as follows: below 25 years (1.1%), 25-30 years (21.4%), 31-35 years (31.8%), 36-40 years (19.5%), 41-45 years (10.7%), 46-50 years (8.5%), and above 50 years (7.9%); 76.6% of the participants were married, while 22.3% were single. 1.1% of participants held a master's degree, 529 (50.7%) had a bachelor's degree, and 504 (48.3%) had a diploma in nursing. The majority of the participants were from India (69.7%), followed by the Philippines (25.8%) and Saudi Arabia (3.2%). Seventy-seven percent of the staff were on shift duties, while 23.0% worked on straight shifts. Three hundred and sixteen participants (30.3%) had 5-10 years of experience, 27.6% had 11-15 years, 12.0% had 16-20 years, 22.2% had less than five years, and 8% had more than 20 years of experience. Out of the total participants, 79.0% had experience in dealing with COVID-19 patients. The study participants were categorized based on their roles as follows: Frontline Staff (83.6%), Middle Management (12.9%), Education and Training (2.2%), and Upper Management (1.2%).
Frequency and percentage distribution of perceived stress levels among nurses working during COVID-19
Figure 1 displays the distribution of perceived stress levels among 1044 nursing professionals at KAUH during the COVID-19 pandemic. Of the participants, 93 (8.9%) experienced low levels of stress, 915 (87.6%) had a moderate level of stress, and 36 (3.4%) reported high perceived stress.
Figure 1. Frequency and Percentage Distribution of Level of Perceived Stress Among Nurses Working During COVID-19.
COVID-19: Coronavirus disease 2019
Frequency and percentage distribution of causes of stress
The study investigated 10 common causes of stress among nurses, and the results revealed that the three primary causes were as follows: workload: 284 (27.8%) of the participants reported workload as a significant cause of stress; lack of resources: 213 (20.9%) of the participants cited the lack of resources as a major stress factor; and fear of getting COVID-19: 126 (12.3%) of the participants expressed fear of contracting COVID-19 as a significant source of stress. These findings indicate that workload, lack of resources, and fear of COVID-19 are the top three stressors among nurses during the COVID-19 pandemic as shown in Table 1.
Table 1. Frequency and Percentage Distribution for Causes of Stress Among Nurses Working During COVID-19 (N=1044).
COVID-19: Coronavirus disease 2019
| What causes you the most stress on your job? | N(%) |
| Death and dying | 32 (03.1) |
| Documentation | 34 (03.3) |
| Fear of getting COVID-19 | 126 (12.3) |
| Follow up with other health care team to complete the required task | 76 (07.4) |
| High demand from patient / family | 70 (06.9) |
| High patient acuity | 15 (01.5) |
| Lack of resources | 213 (20.9) |
| Medication dispensing process | 42 (04.1) |
| Pressure from immediate superiors | 106 (10.4) |
| Workload | 284 (27.8) |
| Others | 23 (02.3) |
Distribution of stress levels across socio-demographic characteristics
It is evident that among the 1044 nursing professionals, there is a significant association between the level of stress and nationality (p-value= 0.006), work experience (p-value= 0.001), and experience with COVID patients (p-value= 0.05) as shown in Table 2. On the other hand, the following socio-demographic variables showed no significant association with stress levels: age, gender, marital status, educational level, unit, work schedule, and work status. These variables did not have a significant impact on the perceived stress levels of the nursing professionals in the study.
Table 2. Distribution of Stress Levels Across Socio-Demographic Characteristics.
*Significant at 0.05 level
| Variable | Category | Stress Levels | Total | χ2 value | p-value | ||
| Low Stress | Moderate Stress | High Perceived Stress | |||||
| Age | 25-30 Years | 14 | 202 | 7 | 223 | 8.761 | 0.687 |
| 15.1% | 22.1% | 19.4% | 21.4% | ||||
| 31-35 Years | 27 | 292 | 13 | 332 | |||
| 29.0% | 31.9% | 36.1% | 31.8% | ||||
| 36-40 Years | 22 | 172 | 10 | 204 | |||
| 23.7% | 18.8% | 27.8% | 19.5% | ||||
| 41-45 Years | 8 | 92 | 3 | 103 | |||
| 8.6% | 10.1% | 8.3% | 9.9% | ||||
| 46-50 Years | 10 | 77 | 2 | 89 | |||
| 10.8% | 8.4% | 5.6% | 8.5% | ||||
| Less than 25 Years | 1 | 10 | 0 | 11 | |||
| 1.1% | 1.1% | 0.0% | 1.1% | ||||
| More than 50 Years | 11 | 70 | 1 | 82 | |||
| 11.8% | 7.7% | 2.8% | 7.9% | ||||
| Gender | Female | 77 | 815 | 33 | 925 | 3.399 | 0.181 |
| 82.8% | 89.1% | 91.7% | 88.6% | ||||
| Male | 16 | 100 | 3 | 119 | |||
| 17.2% | 10.9% | 8.3% | 11.4% | ||||
| Marital Status | Married | 72 | 702 | 26 | 800 | 0.862 | 0.876 |
| 77.4% | 76.7% | 72.2% | 76.6% | ||||
| Single | 20 | 203 | 10 | 233 | |||
| 21.5% | 22.2% | 27.8% | 22.3% | ||||
| Others | 1 | 10 | 0 | 11 | |||
| 1.1% | 1.1% | 0.0% | 1.1% | ||||
| Educational Level | Bachelor's Degree | 46 | 462 | 21 | 529 | 7.020 | 0.109 |
| 49.5% | 50.5% | 58.3% | 50.7% | ||||
| Diploma | 46 | 445 | 13 | 504 | |||
| 49.5% | 48.6% | 36.1% | 48.3% | ||||
| Master's Degree | 1 | 8 | 2 | 11 | |||
| 1.1% | 0.9% | 5.6% | 1.1% | ||||
| Nationality | India | 64 | 645 | 19 | 728 | 16.781 | 0.006* |
| 68.8% | 70.5% | 52.8% | 69.7% | ||||
| Philippines | 20 | 235 | 14 | 269 | |||
| 21.5% | 25.7% | 38.9% | 25.8% | ||||
| Saudi | 5 | 27 | 1 | 33 | |||
| 5.4% | 3.0% | 2.8% | 3.2% | ||||
| Others | 4 | 8 | 2 | 14 | |||
| 4.3% | 0.9% | 5.6% | 1.3% | ||||
| Unit | Cath Lab | 1 | 8 | 0 | 9 | 59.234 | 0.308 |
| 1.1% | 0.9% | 0.0% | 0.9% | ||||
| CCU | 4 | 31 | 1 | 36 | |||
| 4.3% | 3.4% | 2.8% | 3.4% | ||||
| Day Care | 2 | 11 | 1 | 14 | |||
| 2.2% | 1.2% | 2.8% | 1.3% | ||||
| Dialysis | 3 | 30 | 1 | 34 | |||
| 3.2% | 3.3% | 2.8% | 3.3% | ||||
| Endoscopy | 1 | 18 | 0 | 19 | |||
| 1.1% | 2.0% | 0.0% | 1.8% | ||||
| ER | 11 | 94 | 4 | 109 | |||
| 11.8% | 10.3% | 11.1% | 10.4% | ||||
| FMW | 3 | 24 | 3 | 30 | |||
| 3.2% | 2.6% | 8.3% | 2.9% | ||||
| FSW | 3 | 18 | 0 | 21 | |||
| 3.2% | 2.0% | 0.0% | 2.0% | ||||
| Hema/Onco | 1 | 9 | 1 | 11 | |||
| 1.1% | 1.0% | 2.8% | 1.1% | ||||
| Isolation 1 | 2 | 17 | 1 | 20 | |||
| 2.2% | 1.9% | 2.8% | 1.9% | ||||
| Isolation 2 | 2 | 43 | 2 | 47 | |||
| 2.2% | 4.7% | 5.6% | 4.5% | ||||
| LD | 3 | 21 | 0 | 24 | |||
| 3.2% | 2.3% | 0.0% | 2.3% | ||||
| MICU | 8 | 89 | 4 | 101 | |||
| 8.6% | 9.7% | 11.1% | 9.7% | ||||
| MMW | 2 | 40 | 1 | 43 | |||
| 2.2% | 4.4% | 2.8% | 4.1% | ||||
| MSW | 0 | 14 | 1 | 15 | |||
| 0.0% | 1.5% | 2.8% | 1.4% | ||||
| NICS | 0 | 8 | 0 | 8 | |||
| 0.0% | 0.9% | 0.0% | 0.8% | ||||
| NICU | 8 | 50 | 3 | 61 | |||
| 8.6% | 5.5% | 8.3% | 5.8% | ||||
| NICU 2 | 1 | 6 | 0 | 7 | |||
| 1.1% | 0.7% | 0.0% | 0.7% | ||||
| Nursery | 7 | 34 | 0 | 41 | |||
| 7.5% | 3.7% | 0.0% | 3.9% | ||||
| OB Gyane | 0 | 16 | 0 | 16 | |||
| 0.0% | 1.7% | 0.0% | 1.5% | ||||
| OPD | 4 | 41 | 1 | 46 | |||
| 4.3% | 4.5% | 2.8% | 4.4% | ||||
| OR | 4 | 65 | 2 | 71 | |||
| 4.3% | 7.1% | 5.6% | 6.8% | ||||
| PCICU | 5 | 42 | 2 | 49 | |||
| 5.4% | 4.6% | 5.6% | 4.7% | ||||
| Pedia 1 | 0 | 7 | 0 | 7 | |||
| 0.0% | 0.8% | 0.0% | 0.7% | ||||
| Pedia 2 | 4 | 43 | 0 | 47 | |||
| 4.3% | 4.7% | 0.0% | 4.5% | ||||
| PICU | 1 | 48 | 1 | 50 | |||
| 1.1% | 5.2% | 2.8% | 4.8% | ||||
| PICU 2 | 4 | 3 | 0 | 7 | |||
| 4.3% | 0.3% | 0.0% | 0.7% | ||||
| Private | 2 | 24 | 1 | 27 | |||
| 2.2% | 2.6% | 2.8% | 2.6% | ||||
| Radiotherapy | 2 | 2 | 0 | 4 | |||
| 2.2% | 0.2% | 0.0% | 0.4% | ||||
| SICU | 1 | 37 | 4 | 42 | |||
| 1.1% | 4.0% | 11.1% | 4.0% | ||||
| SIMCU | 0 | 1 | 0 | 1 | |||
| 0.0% | 0.1% | 0.0% | 0.1% | ||||
| Others | 4 | 21 | 2 | 27 | |||
| 4.3% | 2.3% | 5.6% | 2.6% | ||||
| Work Schedule | Shift Duty | 71 | 703 | 30 | 804 | 0.853 | 0.653 |
| 76.3% | 76.8% | 83.3% | 77.0% | ||||
| Straight Duty | 22 | 212 | 6 | 240 | |||
| 23.7% | 23.2% | 16.7% | 23.0% | ||||
| Work Experience | 5-10 Years | 24 | 274 | 18 | 316 | 24.503 | 0.001* |
| 25.8% | 29.9% | 50.0% | 30.3% | ||||
| 11-15 Years | 23 | 257 | 8 | 288 | |||
| 24.7% | 28.1% | 22.2% | 27.6% | ||||
| 16-20 Years | 24 | 96 | 5 | 125 | |||
| 25.8% | 10.5% | 13.9% | 12.0% | ||||
| Less than 5 Years | 16 | 211 | 5 | 232 | |||
| 17.2% | 23.1% | 13.9% | 22.2% | ||||
| More than 20 Years | 6 | 77 | 0 | 83 | |||
| 6.5% | 8.4% | 0.0% | 8.0% | ||||
| Experience with COVID patients - Taken care of covid -19 patients | No | 28 | 186 | 5 | 219 | 6.001 | 0.05* |
| 30.1% | 20.3% | 13.9% | 21.0% | ||||
| Yes | 65 | 729 | 31 | 825 | |||
| 69.9% | 79.7% | 86.1% | 79.0% | ||||
| Work Status | Education and Training | 2 | 21 | 0 | 23 | 1.670 | 0.912 |
| 2.2% | 2.3% | 0.0% | 2.2% | ||||
| Frontline Staff | 78 | 764 | 31 | 873 | |||
| 83.9% | 83.5% | 86.1% | 83.6% | ||||
| Middle Management | 12 | 119 | 4 | 135 | |||
| 12.9% | 13.0% | 11.1% | 12.9% | ||||
| Upper Management | 1 | 11 | 1 | 13 | |||
| 1.1% | 1.2% | 2.8% | 1.2% | ||||
Univariate ordinal logistic regression for socio-demographic factors affecting the stress level
Univariate ordinal logistic regression was used to assess the association of the perceived stress level with socio-demographic factors (Table 3). Among these factors, experience with COVID patients showed a significant association with the perceived stress level (COR = 5.86, 95% CI 0.380-9.03). This indicates that nursing professionals who have taken care of COVID-19 patients were 5.86 times more likely to report higher levels of perceived stress compared to those who have not taken care of COVID-19 patients, based on the unadjusted odds ratio. On the other hand, the following socio-demographic variables showed no significant association with stress levels: age, gender, marital status, educational level, unit, work schedule, and work status. These variables did not have a significant impact on the perceived stress levels of the nursing professionals in the study as shown in Table 3.
Table 3. Univariate Ordinal Logistic Regression for Factors Affecting the Stress Level.
OR: Odds ratio
| Variables | Category | Estimate | Sig. | Unadjusted OR | 95% Confidence Interval | |
| Lower Bound | Upper Bound | |||||
| Years | Less than 25 | -0.397 | 0.654 | 0.672 | 0.118 | 3.815 |
| 25-30 | 0.104 | 0.702 | 1.109 | 0.652 | 1.887 | |
| 36-40 | -0.158 | 0.563 | 0.854 | 0.501 | 1.457 | |
| 41-45 | -0.054 | 0.876 | 0.947 | 0.479 | 1.874 | |
| 46-50 | -0.405 | 0.247 | 0.667 | 0.335 | 1.325 | |
| More than 50 | -0.641 | 0.065 | 0.527 | 0.267 | 1.040 | |
| 31-35 | 0a | |||||
| Gender | Male | -0.507 | 0.065 | 0.602 | 0.351 | 1.032 |
| Female | 0a | |||||
| Marital Status | Single | 0.126 | 0.580 | 1.135 | 0.725 | 1.777 |
| Others | -0.257 | 0.768 | 0.773 | 0.140 | 4.269 | |
| Married | 0a | |||||
| Educational Level | Diploma | -0.155 | 0.413 | 0.856 | 0.591 | 1.241 |
| Master's Degree | 1.308 | 0.133 | 3.700 | 0.672 | 20.359 | |
| Bachelor's Degree | 0a | |||||
| Nationality | Philippines | 0.356 | 0.114 | 1.427 | 0.918 | 2.219 |
| Saudi | -0.480 | 0.323 | 0.619 | 0.239 | 1.602 | |
| Others | -0.754 | 0.270 | 0.470 | 0.123 | 1.798 | |
| India | 0a | |||||
| Unit | Cath Lab | -0.373 | 0.706 | 0.689 | 0.099 | 4.781 |
| CCU | -0.167 | 0.773 | 0.846 | 0.272 | 2.629 | |
| Day Care | -0.091 | 0.916 | 0.913 | 0.168 | 4.954 | |
| Dialysis | 0.056 | 0.928 | 1.057 | 0.318 | 3.516 | |
| Endoscopy | 0.130 | 0.868 | 1.139 | 0.244 | 5.318 | |
| FMW | 0.652 | 0.337 | 1.920 | 0.507 | 7.272 | |
| FSW | -0.603 | 0.355 | 0.547 | 0.152 | 1.963 | |
| Hema/Onco | 0.652 | 0.534 | 1.920 | 0.245 | 15.019 | |
| Isolation 1 | 0.130 | 0.866 | 1.139 | 0.252 | 5.144 | |
| Isolation 2 | 0.652 | 0.255 | 1.920 | 0.625 | 5.896 | |
| LD | -0.477 | 0.453 | 0.621 | 0.179 | 2.156 | |
| MICU | 0.240 | 0.584 | 1.271 | 0.539 | 2.997 | |
| MMW | 0.412 | 0.481 | 1.511 | 0.480 | 4.752 | |
| MSW | 1.304 | 0.129 | 3.686 | 0.683 | 19.898 | |
| NICS | 0.652 | 0.592 | 1.920 | 0.177 | 20.841 | |
| NICU | -0.171 | 0.723 | 0.842 | 0.327 | 2.171 | |
| NICU 2 | -0.603 | 0.565 | 0.547 | 0.070 | 4.263 | |
| Nursery | -0.786 | 0.113 | 0.456 | 0.173 | 1.203 | |
| OB Gyane | 0.652 | 0.462 | 1.920 | 0.338 | 10.910 | |
| OPD | 0.000 | 1.000 | 1.000 | 0.344 | 2.905 | |
| OR | 0.361 | 0.462 | 1.434 | 0.549 | 3.749 | |
| PCICU | 0.026 | 0.961 | 1.026 | 0.360 | 2.924 | |
| Pedia 1 | 0.652 | 0.615 | 1.920 | 0.151 | 24.330 | |
| Pedia 2 | -0.162 | 0.758 | 0.850 | 0.303 | 2.387 | |
| PICU | 0.652 | 0.244 | 1.920 | 0.641 | 5.753 | |
| PICU 2 | -2.587 | 0.002 | 0.075 | 0.015 | 0.376 | |
| Private | 0.267 | 0.699 | 1.306 | 0.337 | 5.063 | |
| Radiotherapy | -2.301 | 0.027 | 0.100 | 0.013 | 0.773 | |
| SICU | 1.363 | 0.017 | 3.907 | 1.278 | 11.943 | |
| Others | -0.118 | 0.856 | 0.888 | 0.248 | 3.186 | |
| ER | 0a | |||||
| Work Schedule | Straight Duty | -0.131 | 0.553 | 0.877 | 0.569 | 1.352 |
| Shift Duty | 0a | |||||
| Less than 5 Years | -0.262 | 0.338 | 0.769 | 0.450 | 1.316 | |
| Work Experience | 11-15 Years | -0.308 | 0.232 | 0.735 | 0.443 | 1.218 |
| 16-20 Years | -1.107 | 0.000 | 0.331 | 0.184 | 0.595 | |
| More than 20 Years | -0.471 | 0.212 | 0.624 | 0.298 | 1.308 | |
| 5-10 Years | 0a | |||||
| Experience with COVID patients | No | -0.534 | 0.015 | 0.586 | 0.380 | 0.903 |
| Yes | 0a | |||||
| Work Status | Education and Training | -0.257 | 0.674 | 0.773 | 0.233 | 2.563 |
| Middle Management | -0.045 | 0.872 | 0.956 | 0.553 | 1.653 | |
| Upper Management | 0.498 | 0.574 | 1.646 | 0.289 | 9.365 | |
| Frontline Staff | 0a | |||||
| Variables | Category | Estimate | Sig. | Unadjusted OR | 95% Confidence Interval | |
| Lower Bound | Upper Bound | |||||
| Years | Less than 25 | -0.397 | 0.654 | 0.672 | 0.118 | 3.815 |
| 25-30 | 0.104 | 0.702 | 1.109 | 0.652 | 1.887 | |
| 36-40 | -0.158 | 0.563 | 0.854 | 0.501 | 1.457 | |
| 41-45 | -0.054 | 0.876 | 0.947 | 0.479 | 1.874 | |
| 46-50 | -0.405 | 0.247 | 0.667 | 0.335 | 1.325 | |
| More than 50 | -0.641 | 0.065 | 0.527 | 0.267 | 1.040 | |
| 31-35 | 0a | |||||
| Gender | Male | -0.507 | 0.065 | 0.602 | 0.351 | 1.032 |
| Female | 0a | |||||
| Marital Status | Single | 0.126 | 0.580 | 1.135 | 0.725 | 1.777 |
| Others | -0.257 | 0.768 | 0.773 | 0.140 | 4.269 | |
| Married | 0a | |||||
| Educational Level | Diploma | -0.155 | 0.413 | 0.856 | 0.591 | 1.241 |
| Master's Degree | 1.308 | 0.133 | 3.700 | 0.672 | 20.359 | |
| Bachelor's Degree | 0a | |||||
| Nationality | Philippines | 0.356 | 0.114 | 1.427 | 0.918 | 2.219 |
| Saudi | -0.480 | 0.323 | 0.619 | 0.239 | 1.602 | |
| Others | -0.754 | 0.270 | 0.470 | 0.123 | 1.798 | |
| India | 0a | |||||
| Unit | Cath Lab | -0.373 | 0.706 | 0.689 | 0.099 | 4.781 |
| CCU | -0.167 | 0.773 | 0.846 | 0.272 | 2.629 | |
| Day Care | -0.091 | 0.916 | 0.913 | 0.168 | 4.954 | |
| Dialysis | 0.056 | 0.928 | 1.057 | 0.318 | 3.516 | |
| Endoscopy | 0.130 | 0.868 | 1.139 | 0.244 | 5.318 | |
| FMW | 0.652 | 0.337 | 1.920 | 0.507 | 7.272 | |
| FSW | -0.603 | 0.355 | 0.547 | 0.152 | 1.963 | |
| Hema/Onco | 0.652 | 0.534 | 1.920 | 0.245 | 15.019 | |
| Isolation 1 | 0.130 | 0.866 | 1.139 | 0.252 | 5.144 | |
| Isolation 2 | 0.652 | 0.255 | 1.920 | 0.625 | 5.896 | |
| LD | -0.477 | 0.453 | 0.621 | 0.179 | 2.156 | |
| MICU | 0.240 | 0.584 | 1.271 | 0.539 | 2.997 | |
| MMW | 0.412 | 0.481 | 1.511 | 0.480 | 4.752 | |
| MSW | 1.304 | 0.129 | 3.686 | 0.683 | 19.898 | |
| NICS | 0.652 | 0.592 | 1.920 | 0.177 | 20.841 | |
| NICU | -0.171 | 0.723 | 0.842 | 0.327 | 2.171 | |
| NICU 2 | -0.603 | 0.565 | 0.547 | 0.070 | 4.263 | |
| Nursery | -0.786 | 0.113 | 0.456 | 0.173 | 1.203 | |
| OB Gyane | 0.652 | 0.462 | 1.920 | 0.338 | 10.910 | |
| OPD | 0.000 | 1.000 | 1.000 | 0.344 | 2.905 | |
| OR | 0.361 | 0.462 | 1.434 | 0.549 | 3.749 | |
| PCICU | 0.026 | 0.961 | 1.026 | 0.360 | 2.924 | |
| Pedia 1 | 0.652 | 0.615 | 1.920 | 0.151 | 24.330 | |
| Pedia 2 | -0.162 | 0.758 | 0.850 | 0.303 | 2.387 | |
| PICU | 0.652 | 0.244 | 1.920 | 0.641 | 5.753 | |
| PICU 2 | -2.587 | 0.002 | 0.075 | 0.015 | 0.376 | |
| Private | 0.267 | 0.699 | 1.306 | 0.337 | 5.063 | |
| Radiotherapy | -2.301 | 0.027 | 0.100 | 0.013 | 0.773 | |
| SICU | 1.363 | 0.017 | 3.907 | 1.278 | 11.943 | |
| Others | -0.118 | 0.856 | 0.888 | 0.248 | 3.186 | |
| ER | 0a | |||||
| Work Schedule | Straight Duty | -0.131 | 0.553 | 0.877 | 0.569 | 1.352 |
| Shift Duty | 0a | |||||
| Less than 5 Years | -0.262 | 0.338 | 0.769 | 0.450 | 1.316 | |
| Work Experience | 11-15 Years | -0.308 | 0.232 | 0.735 | 0.443 | 1.218 |
| 16-20 Years | -1.107 | 0.000 | 0.331 | 0.184 | 0.595 | |
| More than 20 Years | -0.471 | 0.212 | 0.624 | 0.298 | 1.308 | |
| 5-10 Years | 0a | |||||
| Experience with COVID patients | No | -0.534 | 0.015 | 0.586 | 0.380 | 0.903 |
| Yes | 0a | |||||
| Work Status | Education and Training | -0.257 | 0.674 | 0.773 | 0.233 | 2.563 |
| Middle Management | -0.045 | 0.872 | 0.956 | 0.553 | 1.653 | |
| Upper Management | 0.498 | 0.574 | 1.646 | 0.289 | 9.365 | |
| Frontline Staff | 0a | |||||
Multivariate ordinal logistic regression for socio-demographic factors affecting the stress level
The multivariable ordinal logistic regression analysis (Table 4) was conducted to assess the combined effect of socio-demographic factors on stress levels. The likelihood ratio chi-square test resulted in a significant p-value of 0.024, indicating that the model as a whole (gender and nationality as predictors) was statistically significant. This suggests that the combination of gender and nationality had a significant effect on stress levels among nursing professionals. Regarding individual predictors, the analysis found that both gender and nationality had significant effects on stress levels after controlling for other factors. first gender, the AOR for gender was 0.319, with a 95% confidence interval (CI) of 0.166-0.613. This indicates that, after adjusting for other factors, female nursing professionals were 68.1% less likely to report higher levels of perceived stress compared to male nursing professionals. Second is the nationality; the analysis showed that the stress levels of nurses from the Philippines were significantly different from those of Indian nurses. The AOR for Filipino nurses was 2.559, with a 95% CI of 1.297-5.051. This means that, after adjusting for other factors, Filipino nursing professionals were 2.559 times more likely to report higher levels of perceived stress compared to Indian nursing professionals. These results indicate that both gender and nationality are important factors that influence the perceived stress levels among nursing professionals. Female nurses were less likely to report high stress levels compared to male nurses, and there was a significant difference in stress levels between nurses from the Philippines and Indian nurses. It is essential to consider these findings while designing interventions and support systems to address stress and improve the well-being of nursing professionals, especially during challenging times like the COVID-19 pandemic.
Table 4. Multivariable Ordinal Logistic Regression for Socio-Demographic Factors Affecting the Stress Level.
0a - reference; OR: Odds ratio
| Variables | Category | B | p-value | Adjusted OR | 95% Wald Confidence Interval | ||
| Category | Overall | Lower | Upper | ||||
| Age | Less than 25 Years | -0.452 | 0.644 | 0.920 | 0.636 | 0.093 | 4.339 |
| 25-30 Years | 0.133 | 0.692 | 1.142 | 0.591 | 2.207 | ||
| 36-40 Years | 0.211 | 0.510 | 1.235 | 0.659 | 2.315 | ||
| 41-45 | 0.294 | 0.510 | 1.342 | 0.559 | 3.224 | ||
| 46-50 Years | -0.028 | 0.953 | 0.972 | 0.379 | 2.491 | ||
| More than 50 Years | -0.246 | 0.664 | 0.782 | 0.258 | 2.369 | ||
| 31-35 Years | 0a | 1 | |||||
| Gender | Male | -1.142 | 0.001 | 0.001 | 0.319 | 0.166 | 0.613 |
| Female | 0a | 1 | |||||
| Marital Status | Single | -0.135 | 0.643 | 0.873 | 0.873 | 0.492 | 1.549 |
| Others | -0.267 | 0.778 | 0.766 | 0.119 | 4.921 | ||
| Married | 0a | 1 | |||||
| Educational Level | Diploma | 0.114 | 0.690 | 0.178 | 1.121 | 0.640 | 1.963 |
| Master's Degree | 1.855 | 0.055 | 6.389 | 0.965 | 42.314 | ||
| Bachelor's Degree | 0a | 1 | |||||
| Nationality | Philippines | 0.940 | 0.007 | 0.016 | 2.559 | 1.297 | 5.051 |
| Saudi | -0.646 | 0.268 | 0.524 | 0.167 | 1.644 | ||
| Others | 0.018 | 0.984 | 1.018 | 0.174 | 5.957 | ||
| India | 0a | 1 | |||||
| Unit | Cath Lab | -0.457 | 0.670 | 0.296 | 0.633 | 0.077 | 5.192 |
| CCU | -0.100 | 0.866 | 0.905 | 0.284 | 2.889 | ||
| Day Care | -0.283 | 0.763 | 0.754 | 0.120 | 4.735 | ||
| Dialysis | -0.073 | 0.913 | 0.929 | 0.252 | 3.433 | ||
| Endoscopy | -0.201 | 0.810 | 0.818 | 0.158 | 4.230 | ||
| FMW | 0.477 | 0.509 | 1.611 | 0.391 | 6.641 | ||
| FSW | -0.674 | 0.322 | 0.510 | 0.134 | 1.937 | ||
| Hema/Onco | 0.505 | 0.658 | 1.657 | 0.177 | 15.520 | ||
| Isolation 1 | -0.175 | 0.827 | 0.839 | 0.174 | 4.040 | ||
| Isolation 2 | 0.331 | 0.576 | 1.392 | 0.436 | 4.442 | ||
| LD | -0.542 | 0.422 | 0.582 | 0.155 | 2.184 | ||
| MICU | 0.300 | 0.502 | 1.350 | 0.562 | 3.240 | ||
| MMW | 0.635 | 0.281 | 1.888 | 0.594 | 5.996 | ||
| MSW | 1.350 | 0.117 | 3.857 | 0.714 | 20.842 | ||
| NICS | 0.551 | 0.653 | 1.735 | 0.157 | 19.212 | ||
| NICU | -0.222 | 0.685 | 0.801 | 0.274 | 2.343 | ||
| NICU 2 | -0.422 | 0.702 | 0.656 | 0.075 | 5.700 | ||
| Nursery | -1.017 | 0.064 | 0.362 | 0.123 | 1.061 | ||
| OB Gyane | 0.326 | 0.706 | 1.385 | 0.255 | 7.519 | ||
| OPD | -0.192 | 0.751 | 0.825 | 0.252 | 2.705 | ||
| OR | 0.438 | 0.377 | 1.550 | 0.586 | 4.101 | ||
| PCICU | -0.019 | 0.975 | 0.981 | 0.307 | 3.142 | ||
| Pedia 1 | 0.823 | 0.523 | 2.278 | 0.182 | 28.520 | ||
| Pedia 2 | -0.073 | 0.897 | 0.930 | 0.310 | 2.788 | ||
| PICU | 0.555 | 0.346 | 1.741 | 0.549 | 5.525 | ||
| PICU 2 | -2.401 | 0.005 | 0.091 | 0.017 | 0.492 | ||
| Private | 0.015 | 0.983 | 1.015 | 0.256 | 4.031 | ||
| Radiotherapy | -2.808 | 0.017 | 0.060 | 0.006 | 0.611 | ||
| SICU | 1.403 | 0.017 | 4.067 | 1.291 | 12.811 | ||
| SIMCU | 0.009 | 0.998 | 1.009 | 0.001 | 1000.638 | ||
| Others | -0.334 | 0.637 | 0.716 | 0.179 | 2.862 | ||
| ER | 0a | 1 | |||||
| Work Schedule | Straight Duty | 0.271 | 0.388 | 0.386 | 1.311 | 0.709 | 2.423 |
| Shift Duty | 0a | 1 | |||||
| Less than 5 Years | -0.129 | 0.672 | 0.072 | 0.879 | 0.483 | 1.599 | |
| Work Experience | 11-15 Years | -0.495 | 0.115 | 0.610 | 0.329 | 1.128 | |
| 16-20 Years | -1.250 | 0.005 | 0.286 | 0.120 | 0.682 | ||
| More than 20 Years | -0.586 | 0.308 | 0.557 | 0.181 | 1.716 | ||
| 5-10 Years | 0a | 1 | |||||
| Experience with COVID patients | No | -0.391 | 0.168 | 0.169 | 0.676 | 0.388 | 1.179 |
| Yes | 0a | 1 | |||||
| Work Status | Education and Training | -0.440 | 0.500 | 0.898 | 0.644 | 0.179 | 2.314 |
| Middle Management | 0.002 | 0.996 | 1.002 | 0.545 | 1.840 | ||
| Upper Management | 0.372 | 0.709 | 1.451 | 0.205 | 10.247 | ||
| Frontline Staff | 0a | 1 | |||||
Discussion
Perceived stress level of nurses during the COVID-19 outbreak
The findings of this study reveal that among 1044 nursing professionals in our setting, 87.6% had a moderate level of stress, and 3.4% experienced high perceived stress during the COVID-19 pandemic. The average stress score obtained was 18.8 ± 4.1, indicating a moderate level of self-perceived stress. These results are consistent with similar studies conducted in different regions during the pandemic. Studies from South Korea, Wuhan (China), and Medina (Saudi Arabia) reported stress scores around the same range [20-22]. Other studies have also highlighted the high levels of stress, anxiety, and depression among frontline HCWs caring for COVID-19 patients [23]. The elevated stress levels observed among nurses can be attributed to factors such as increased workload, fear of getting infected, and the emotional toll of caring for critically ill patients during a pandemic [24].
Association of selected socio-demographic characteristics and perceived stress levels
The study identified significant associations between perceived stress levels and certain socio-demographic variables such as nationality, work experience, and experience with COVID-19 patients. However, no significant associations were found with age, gender, marital status, education, unit, work schedule, and work status.
Gender
The analysis revealed significant gender differences in stress levels during the COVID-19 pandemic, with female nursing professionals reporting lower stress levels compared to males. This finding is consistent with several other studies that have reported higher stress levels among male HCWs compared to females [25,26]. However, it is worth noting that there have been conflicting results in some studies, with others reporting higher stress levels among females [27]. The reasons behind these gender differences in stress perception may be multifactorial and warrant further investigation.
Nationality
Nationality was another significant predictor of stress levels among nursing professionals in the study. This study describes that nurses from the Philippines were more stressed than others. In the current study, a high perceived stress level was observed more in Philippine nurses than in Indian and Saudi nurses. This difference could be attributed to variations in cultural norms, coping mechanisms, and support systems, which can influence how individuals perceive and manage stress during challenging situations. Similar to our study another study from Saudi Arabia also found that Philippine nurses had more negative feelings and experienced more factors causing stress compared to other nationalities [28]. In contrast to the current study, the other two studies from India [29] and Saudi Arabia [30] showed that Indian nurses had higher stress levels compared with nurses from other nationalities. It may be due to the family-oriented structure of Indian society [31], which might increase their homesickness due to the environmental changes. Another study by Bhatia et al., among 87 nurses working in two of the tertiary care teaching hospitals of Central Delhi, found that the majority (87.4%) of nurses reported their job as stressful [32]. Similar to the current study, a nationwide observational study conducted among 433 healthcare practitioners in India shows that the prevalence of high-level stress was low, only 3.7% (45), and another multicenter study from the Asia-Pacific region, including HCWs from major tertiary healthcare institutions from India, Singapore, Malaysia, Vietnam, and Indonesia, India showed the lowermost prevalence of adverse psychological effects [33]. On the other hand, another study from Saudi Arabia shows no significant association between nurses' stress levels and nationality [34].
Work experience
The current study shows a high level of stress with moderately experienced nurses. The high perceived stress level was observed more in the nurses with an experience of 5-10 years (50.0%) than those experienced 11-15 years (22.2%), 16-20 years, and less than five years of experience (13.9%). Nurses with more than 20 years of experience have not been exposed to high levels of stress. The association between the perceived stress level and work experience (p = 0.001) remained significant in the analysis. Similarly, a study among HCWs from China revealed an increased risk of developing psychological stress among HCWs with 10 years or more of work experience [35]. In contrast to the current study, a study conducted in Turkey shows that those who were younger and had fewer years of work experienced significantly more stress than their counterparts who had worked for longer [36]. Similarly, a study among oncology nurses shows that the demographic variables of age and work experience in nursing showed a substantial positive association with work-related stress scores [37]. Also, a study from Pakistan reported job experience as an important forecaster, where nurses with less experience were more likely to develop depression, anxiety, and stress [38]. Another study by Humpel & Caputi also concluded that nurses with shorter experience displayed more depression, anxiety, and stress [39]. Another study from Iran also indicated that nurses with fewer years of work experience show more stress while more experienced nurses exhibit more resilience [40]. Therefore, it needs further research to find out the reason behind high levels of stress among moderately experienced nurses, which is different from other studies around the world. The hypothesis for this variation might be because the majority of our study participants were females (88.6%) and between the ages of 25-35 years (53%), which is supported by several studies that females and young age groups are prone to mental stress compared to male gender and older adults [41-45]. In addition, this may be because this group of nurses in our setting were assigned as senior nurses need to make more decisions regarding the care of COVID-19 patients and therefore possessed more responsibilities and pressure.
Experience with COVID-19 patients
High perceived stress levels were observed more in professionals who have taken care of COVID-19 patients (86.1%) than those who haven’t (13.9%). A moderate level of stress was also observed more in professionals who have taken care of COVID-19 patients (79.7%) than those who haven’t (20.3%). The association between the perceived stress level and experience with COVID-19 patients (p = 0.05) remained significant in the analysis. Experience with COVID patients or taking care of COVID-19 patients (COR = 5.86 (95% CI 0.380-9.03) was found to be a significant factor in univariate analysis. Similarly, a study among 218 HCWs from Italy found that HCWs assisting patients with COVID-19 acquired significantly much higher scores on depression, anxiety, and stress than other participants [46]. A study involving a sample of 1257 Chinese HCWs reported that the frontline HCWs involved in direct diagnosis, treatment, and care of patients with COVID-19 were associated with a higher risk of symptoms of depression, anxiety, insomnia, and distress [47]. Another study from Italy among HCWs assisting patients with COVID-19 displayed work-related psychological pressure, emotional exhaustion, and somatic symptoms [48]. A study from Kenya among 255 nurses shows that depression, anxiety, insomnia, distress, and burnout were reported in 45.9%, 48.2%, 37.0%, 28.8%, and 47.9% of all nurses. Also, the study displays that nurses directly involved with COVID-19 patients reported higher rates of mental health symptoms [49]. A study with the participation of 125 nurses working in COVID-19 wards in Iran displays that the rate of depression, anxiety, and stress in nurses working in COVID-19 wards is moderate. [50]. Other studies also report that HCWs/nurses working with COVID-19 patients exhibit moderate rates of stress [51,52]. In contrary to the present study, a study from Turkey displays no significant relationship between psychological symptoms and the organization or working units or COVID-19 services [53].
Major causes of stress among nurses during the COVID-19 pandemic
In the present study, the major three causes of stress raised by the nurses were workload (27.8%), lack of resources (20.9%), and fear of getting COVID-19 (12.3%). Similar to this study a study by Cai et al. from China says that the COVID-19 epidemic in Hubei caused an increased workload and stress for medical staff and the factors associated with stress included the risk of infection to themselves and their families and increased patient mortality [54]. Studies from India, Palestine, Australia, and Iran even before the COVID-19 Pandemic, show that the major stressors experienced by nurses were death and dying patients and excessive workload [55-58]. A study from Malaysia also shows that workload and manpower availability are the major stressors among nurses [59]. A study conducted in central China showed death and dying, workload, and inadequate preparation as the most common sources of nursing stress [60]. Another study among oncology nurses also declares workload and patient death and dying are the main causes of stress [61]. The current study findings are in line with the study conducted by Purcell et al., which declares that patient workload and day of the week worked are important factors affecting nurses' stress levels [62]. A study conducted at the Department of Critical Care Medicine, Wuhan Pulmonary Hospital during the peak of the COVID-19 pandemic shows that the front-line nurses carried enormous workload, enduring fatigue, infection risk, and frustration with the death of patients as the factors causing high stress among them [63]. A comparative study conducted between a COVID-19 and non-COVID-19 hospital in Egypt displays Workload, dealing with death and dying, individual demands and worries, employing strict biosecurity measures, and disgrace represented the high-priority stressors among nurses of COVID hospitals [64]. Similar to this study, a study among nurses from a major university hospital in China, who responded to a national call to go to help the epic entre in early February 2020, included working in an isolated environment, PPE shortage, and the discomfort of pronged usage, sleep problems, the intensity of workload, cultural and language barriers, lack of family support, fear of being infected, and insufficient work experiences with COVID-19 as significant stressors [21]. A qualitative study from a center similar to our setting says that the nursing care of patients with COVID-19 was challenging and strenuous. The variety of patient care needs and an inadequate number of nursing staff increase the nurses' workload and physical fatigue [65]. Another supporting finding can be seen in a study from South Korea which mentions that the PSS-10 score was significantly connected with the fear of COVID-19 infection and fear of blame for COVID-19 infection [20]. A study by Chaudhari et al. also found that the Common causes of stress were conflicts with supervisors, unreasonable demands from patients and their families, workload, and dealing with death and dying [29]. Contrary to the present study, a study from Hubei province in China involving 1208 HCWs demonstrates that the main source of stress among frontline HCWs caring for COVID-19 patients is fear of being infected and the uneasiness caused by protective equipment [66].
Conclusions
The first wave of COVID-19 caused significant psychological stress for nurses, including safety concerns, uncertainty about the disease, stigma, and social isolation. This study highlights the significant stress levels experienced by nursing professionals during the COVID-19 pandemic. The findings underscore the importance of addressing the mental health and well-being of nurses, as they are critical frontline HCWs facing unprecedented challenges. The association between stress levels and nationality, work experience, and experience with COVID-19 patients emphasizes the need for tailored interventions and support systems to meet the unique needs of different subgroups of nursing professionals. Healthcare institutions and policymakers should prioritize the implementation of evidence-based strategies to support nurses' mental health, such as providing access to mental health services, stress management training, and creating supportive work environments. Further research is warranted to explore the underlying factors contributing to the observed gender and nationality-based differences in stress levels among nursing professionals. By gaining a deeper understanding of these factors, targeted interventions can be developed to enhance the well-being and resilience of nurses, ultimately benefiting both healthcare providers and patients alike.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Sabeena M. Rasheed, Lamees S. Bakhsh, Reem S. Alhameedi, Sharifah Mohidin
Acquisition, analysis, or interpretation of data: Sabeena M. Rasheed, Lamees S. Bakhsh, Reem S. Alhameedi, Sharifah Mohidin
Drafting of the manuscript: Sabeena M. Rasheed, Lamees S. Bakhsh, Reem S. Alhameedi, Sharifah Mohidin
Critical review of the manuscript for important intellectual content: Sabeena M. Rasheed, Lamees S. Bakhsh, Reem S. Alhameedi, Sharifah Mohidin
Human Ethics
Consent was obtained or waived by all participants in this study. Unit of Biomedical Ethics Research Committee issued approval 204-21
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.A novel coronavirus from patients with pneumonia in China, 2019. Zhu N, Zhang D, Wang W, et al. N Engl J Med. 2019;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Exploring nurses' experiences of psychological distress during care of patients with COVID-19: a qualitative study. Galehdar N, Kamran A, Toulabi T, Heydari H. BMC Psychiatry. 2020;20:489. doi: 10.1186/s12888-020-02898-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Coronavirus (COVID-19) Dashboard. [ Feb; 2022 ]. 2022. https://data.who.int/dashboards/covid19/cases?n=c https://data.who.int/dashboards/covid19/cases?n=c
- 4.Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. Al Maqbali M, Al Sinani M, Al-Lenjawi B. J Psychosom Res. 2021;141:110343. doi: 10.1016/j.jpsychores.2020.110343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The major worldwide stress of healthcare professionals during the first wave of the COVID-19 pandemic - the international COVISTRESS survey. Couarraze S, Delamarre L, Marhar F, et al. PLoS One. 2021;16:0. doi: 10.1371/journal.pone.0257840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prevalence and associated factors of depression, anxiety, and stress among Hubei pediatric nurses during COVID-19 pandemic. Zheng R, Zhou Y, Qiu M, et al. Compr Psychiatry. 2021;104:152217. doi: 10.1016/j.comppsych.2020.152217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Chen CS, Wu HY, Yang P, Yen CF. Psychiatr Serv. 2005;56:76–79. doi: 10.1176/appi.ps.56.1.76. [DOI] [PubMed] [Google Scholar]
- 8.Mental health problems faced by healthcare workers due to the COVID-19 pandemic-a review. Spoorthy MS, Pratapa SK, Mahant S. Asian J Psychiatr. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inc. Boston, MA. Boston: Butterworth-Heinemann; 1976. Stress in Health and Disease. [Google Scholar]
- 10.Psychological stress and cellular aging in cancer: a meta-analysis. Kruk J, Aboul-Enein BH, Bernstein J, Gronostaj M. Oxid Med Cell Longev. 2019;2019:1270397. doi: 10.1155/2019/1270397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stress, anxiety and depression among healthcare workers facing COVID-19 pandemic in Egypt: a cross-sectional online-based study. Aly HM, Nemr NA, Kishk RM, Elsaid NM. BMJ Open. 2021;11:0. doi: 10.1136/bmjopen-2020-045281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Special attention to nurses' protection during the COVID-19 epidemic. Huang L, Lin G, Tang L, Yu L, Zhou Z. Crit Care. 2020;24:120. doi: 10.1186/s13054-020-2841-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Survey on perceived work stress and its influencing factors among hospital staff during the COVID-19 pandemic in Taiwan. Kuo FL, Yang PH, Hsu HT, et al. Kaohsiung J Med Sci. 2020;36:944–952. doi: 10.1002/kjm2.12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nurse reports of stressful situations during the Covid-19 pandemic: qualitative analysis of survey responses. Arnetz JE, Goetz CM, Arnetz BB, Arble E. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17218126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Cabrera-Troya J, Carmona-Rega MI, Ortega-Galán ÁM. J Clin Nurs. 2020;29:4321–4330. doi: 10.1111/jocn.15469. [DOI] [PubMed] [Google Scholar]
- 16.Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Wu P, Fang Y, Guan Z, et al. Can J Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.A systematic review of the impact of disaster on the mental health of medical responders. Naushad VA, Bierens JJ, Nishan KP, et al. Prehosp Disaster Med. 2019;34:632–643. doi: 10.1017/S1049023X19004874. [DOI] [PubMed] [Google Scholar]
- 19.A global measure of perceived stress. Cohen S, Kamarck T, Mermelstein R. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 20.The association of gratitude with perceived stress among nurses in Korea during COVID-19 outbreak. Lee JY, Kim M, Jhon M, et al. Arch Psychiatr Nurs. 2021;35:647–652. doi: 10.1016/j.apnu.2021.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mental distress and influencing factors in nurses caring for patients with COVID-19. Leng M, Wei L, Shi X, et al. Nurs Crit Care. 2021;26:94–101. doi: 10.1111/nicc.12528. [DOI] [PubMed] [Google Scholar]
- 22.Exploring the vulnerability of frontline nurses to COVID-19 and its impact on perceived stress. Pasay-An E. J Taibah Univ Med Sci. 2020;15:404–409. doi: 10.1016/j.jtumed.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perceived stress and its associated factors during COVID-19 among healthcare providers in Ethiopia: a cross-sectional study. Chekole YA, Yimer Minaye S, Mekonnen Abate S, Mekuriaw B. Adv Public Health. 2020;2020:5036861. [Google Scholar]
- 24.The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Salari N, Khazaie H, Hosseinian-Far A, et al. Hum Resour Health. 2020;18:100. doi: 10.1186/s12960-020-00544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gender differences in job stress and stress coping strategies among Korean nurses. Lee J, Cho YH. Int J Bio-Sci Bio-Technol. 2016;8:143–148. [Google Scholar]
- 26.Gender-based analysis of the psychological impact of the COVID-19 pandemic on healthcare workers in Spain. López-Atanes M, Pijoán-Zubizarreta JI, González-Briceño JP, et al. Front Psychiatry. 2021;12:692215. doi: 10.3389/fpsyt.2021.692215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. PLoS One. 2021;16:0. doi: 10.1371/journal.pone.0247679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feelings, stress, and coping of nurses amidst COVID-19 outbreak in Saudi Arabia. Natividad MJ, Aljohani KA, Roque MY, Gamboa HM. Sudan J Med Sci. 2021;16:285–300. [Google Scholar]
- 29.A profile of occupational stress in nurses. Chaudhari AP, Mazumdar K, Motwani YM, Ramadas D. Ann Indian Psych. 2018;2:109–114. [Google Scholar]
- 30.Exploring nurses' work-related stress in an acute care hospital in KSA. Almazan JU, Albougami AS, Alamri MS. J Taibah Univ Med Sci. 2019;14:376–382. doi: 10.1016/j.jtumed.2019.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Indian family systems, collectivistic society and psychotherapy. Chadda RK, Deb KS. Indian J Psychiatry. 2013;55:0–309. doi: 10.4103/0019-5545.105555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Occupational stress amongst nurses from two tertiary care hospitals in Delhi. Bhatia N, Kishore J, Anand T, Jiloha RC. Australas Med J. 2010;3:731–738. [Google Scholar]
- 33.Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID-19 pandemic in India: a nationwide observational study. Wilson W, Raj JP, Rao S, Ghiya M, Nedungalaparambil NM, Mundra H, Mathew R. Indian J Psychol Med. 2020;42:353–358. doi: 10.1177/0253717620933992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fear of nurses during COVID-19 pandemic in Saudi Arabia: a cross-sectional assessment. Moussa ML, Moussa FL, Alharbi HA, et al. Front Psychol. 2021;12:736103. doi: 10.3389/fpsyg.2021.736103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Psychological impact of COVID-19 pandemic on healthcare workers in China Xi'an central hospital. Wang N, Li Y, Wang Q, Lei C, Liu Y, Zhu S. Brain Behav. 2021;11:0. doi: 10.1002/brb3.2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. Murat M, Köse S, Savaşer S. Int J Ment Health Nurs. 2021;30:533–543. doi: 10.1111/inm.12818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stress levels of nurses in oncology outpatient units. Ko W, Kiser-Larson N. Clin J Oncol Nurs. 2016;20:158–164. doi: 10.1188/16.CJON.158-164. [DOI] [PubMed] [Google Scholar]
- 38.Depression, anxiety, and stress among nurses during the COVID-19 wave III: results of a cross-sectional assessment. Nadeem F, Sadiq A, Raziq A, Iqbal Q, Haider S, Saleem F, Bashaar M. J Multidiscip Healthc. 2021;14:3093–3101. doi: 10.2147/JMDH.S338104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Exploring the relationship between work stress, years of experience and emotional competency using a sample of Australian mental health nurses. Humpel N, Caputi P. J Psychiatr Ment Health Nurs. 2001;8:399–403. doi: 10.1046/j.1365-2850.2001.00409.x. [DOI] [PubMed] [Google Scholar]
- 40.Demographic predictors of resilience among nurses during the COVID-19 pandemic. Afshari D, Nourollahi-Darabad M, Chinisaz N. Work. 2021;68:297–303. doi: 10.3233/WOR-203376. [DOI] [PubMed] [Google Scholar]
- 41.Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, et al. J Affect Disord. 2020;277:347–357. doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Post-traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: a systematic review . d'Ettorre G, Ceccarelli G, Santinelli L, et al. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18020601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Impact of the COVID-19 pandemic on the mental health of healthcare workers. Chatzittofis A, Karanikola M, Michailidou K, Constantinidou A. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18041435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Age differences in COVID-19 risk perceptions and mental health: evidence from a national US survey conducted in March 2020. Bruine de Bruin W. J Gerontol B Psychol Sci Soc Sci. 2021;76:0–9. doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Löwe B, Wahl I, Rose M, et al. J Affect Disord. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 46.Depression, anxiety, and stress among healthcare workers during the COVID-19 outbreak and relationships with expressive flexibility and context sensitivity. Lenzo V, Quattropani MC, Sardella A, Martino G, Bonanno GA. Front Psychol. 2021;12:623033. doi: 10.3389/fpsyg.2021.623033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. Lai J, Ma S, Wang Y, et al. JAMA Netw Open. 2020;3:0. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Barello S, Palamenghi L, Graffigna G. Psychiatry Res. 2020;290:113129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.COVID-19 and mental well-being of nurses in a tertiary facility in Kenya. Ali SK, Shah J, Talib Z. PLoS One. 2021;16:0. doi: 10.1371/journal.pone.0254074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Depression, stress and anxiety of nurses in COVID-19 pandemic in Nohe-Dey Hospital in Torbat-e-Heydariyeh city, Iran. Abadi TS, Askari M, Miri K, Nia MN. J Mil Med. 2020;22:526–533. [Google Scholar]
- 51.Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. Xiao X, Zhu X, Fu S, Hu Y, Li X, Xiao J. J Affect Disord. 2020;274:405–410. doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-east Italy. Lasalvia A, Bonetto C, Porru S, et al. Epidemiol Psychiatr Sci. 2021;30:0. doi: 10.1017/S2045796020001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.The relationship between psychological resilience, burnout, stress, and sociodemographic factors with depression in nurses and midwives during the COVID-19 pandemic: a cross-sectional study in Turkey. Yörük S, Güler D. Perspect Psychiatr Care. 2021;57:390–398. doi: 10.1111/ppc.12659. [DOI] [PubMed] [Google Scholar]
- 54.Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID‑19) in Hubei, China. Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, Zhuang Q. Med Sci Monit. 2020;26:0. doi: 10.12659/MSM.924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.A study of work-related stress among nurses in a tertiary care hospital in Goa. Vernekar SP, Shah H. Int J Community Med Public Health. 2018;5:657–661. [Google Scholar]
- 56.Exploring the work related stress sources and its effect among the Palestinian nurses at the governmental hospitals. Ayed A, Eqtait F, Fashafsheh I, Basheer M, Aqel M, Nassar DA, Omary M. J Educ Pract. 2016;6:100–110. [Google Scholar]
- 57.The relationships among workplace stressors, coping methods, demographic characteristics, and health in Australian nurses. Chang EM, Daly J, Hancock KM, Bidewell JW, Johnson A, Lambert VA, Lambert CE. J Prof Nurs. 2006;22:30–38. doi: 10.1016/j.profnurs.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 58.Occupational stress and turnover intention: implications for nursing management. Mosadeghrad AM. Int J Health Policy Manag. 2013;1:169–176. doi: 10.15171/ijhpm.2013.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nurses’ perspective of work-related stressors. Samuel R, Zaini NH, Hassan WH, Talib AN, Ramly FA. IOP Conf Ser: Earth Environ Sci. 2021;704:12026. [Google Scholar]
- 60.Stress, coping, and psychological well-being among new graduate nurses in China. Qiao G, Li S, Hu J. Home Health Care Manag Pract. 2011;23:398–403. [Google Scholar]
- 61.Oncology nurses' perceptions of work stress and its sources in a university-teaching hospital: a qualitative study. Wazqar DY. Nurs Open. 2019;6:100–108. doi: 10.1002/nop2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.The relationship between nurses' stress and nurse staffing factors in a hospital setting. Purcell SR, Kutash M, Cobb S. J Nurs Manag. 2011;19:714–720. doi: 10.1111/j.1365-2834.2011.01262.x. [DOI] [PubMed] [Google Scholar]
- 63.Psychological stress of ICU nurses in the time of COVID-19. Shen X, Zou X, Zhong X, Yan J, Li L. Crit Care. 2020;24:200. doi: 10.1186/s13054-020-02926-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Occupational stress, job satisfaction, and intent to leave: nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Said RM, El-Shafei DA. Environ Sci Pollut Res Int. 2021;28:8791–8801. doi: 10.1007/s11356-020-11235-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Exploring nurses' perception of taking care of patients with coronavirus disease (COVID-19): a qualitative study. Galehdar N, Toulabi T, Kamran A, Heydari H. Nurs Open. 2021;8:171–179. doi: 10.1002/nop2.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Healthcare workers’ stress when caring for COVID-19 patients: an altruistic perspective. Wang H, Liu Y, Hu K, Zhang M, Du M, Huang H, Yue X. https://journals.sagepub.com/doi/full/10.1177/0969733020934146. Nurs Ethics. 2020;27:1490–1500. doi: 10.1177/0969733020934146. [DOI] [PubMed] [Google Scholar]