Abstract
Warts are caused by human papillomavirus (HPV) infection and can involve multiple parts of skin and mucosa, of which periungual and subungual warts are the most difficult to treat. Periungual or subungual wart is verruca vulgaris growing around or under the fingernail, destroying and deforming the nail and nail bed. Currently, liquid nitrogen cryotherapy and CO2 laser are often used for the treatment. Clinically, few doctors routinely use photodynamic therapy (PDT) to treat viral warts. We used PDT combined with liquid nitrogen cryotherapy and curettage to successfully treat a case of intractable periungual and subungual warts.
KEY WORDS: Curettage, liquid nitrogen cryotherapy, photodynamic therapy, recalcitrant periungual or subungual wart
Introduction
Warts, caused by the human papillomavirus (HPV), were previously considered chronic and benign diseases. However, accumulating evidence indicates that HPV infections are associated with HPV-driven malignancies such as skin, tongue and cervical cancers, thus increasing attention being paid to them. Periungual or subungual wart is verruca vulgaris growing around or under the fingernail, destroying and deforming the nail and nail bed. Currently, liquid nitrogen cryotherapy and CO2 laser are often used for the treatment. Liquid nitrogen cryotherapy is characterised by shortages including pain, long treatment cycles, high recurrence rates and poor efficacy against nail grooves and margins. CO2 laser results in long wound healing time, secondary infection and after healing is prone to local scar formation and new nail deformation.[1] In recent years, it has been reported that 5-aminolevulinic acid photodynamic therapy (ALA-PDT) can successfully treat intractable arbovirus warts.[2] We used PDT combined with liquid nitrogen cryotherapy and curettage to successfully treat a case of intractable periungual and subungual warts. We report the clinical experience as follows and perform a literature review.
Clinical data
A 58-year-old farmer with a prior fitness history. The vegetations around and under the nail in the right hand have occurred repeatedly and he has visited many hospitals many times over the past 10 years [Figure 1]. He has been repeatedly treated with liquid nitrogen cryotherapy, traditional Chinese medicine soaking, topical imiquimod cream, topical interferon cream, BCG polysaccharide nucleic acid intramuscular injection and oral compound glycyrrhizin. Periungual and subungual vegetations in the right hand were reduced but were not completely eliminated, and they recurred and increased within a span of 2 weeks to 3 months. The patient’s life and work are deeply affected. He came to our hospital on 18 March 2020. We thought that the previous liquid nitrogen cryotherapy was not complete so a thorough cryotherapy was given once every 2–3 weeks. After each treatment, the patient’s skin lesions decreased significantly but still recurred after several treatments. After the attending doctor fully communicated with the patient and his family, PDT was readily accepted. In order to improve the curative effect, we used PDT combined with liquid nitrogen cryotherapy and curettage [Figure 2]. Physical examination before treatment: multiple fused verrucous papules and plaques can be seen around and under the middle nail of the right hand. The surface is rough, verrucous and hard to touch.
Figure 1.

One week after liquid nitrogen cryotherapy
Figure 2.

Illumination for 20 min. First PDT: Pain reaction occurred during the illumination process, and we used an electric fan to cool down. Two-step illumination: 50 J/cm² for 5 min and 72 J/cm² for 15 min
Treatment and result
Drug and instrument
Topical ALA hydrochloride powder (ALA, Shanghai Fudan Zhangjiang biomedical Co., Ltd, Specification: 118 mg each) LED-IA PDT apparatus (Wuhan Yager Optoelectronics Technology Co., Ltd, Output wavelength (633 ± 10) nm, Output power 20~100 mW J/cm2, Irradiation dose 40~100 J/cm2).
Treatment method
One week before ALA-PDT treatment, liquid nitrogen cryotherapy was given. On the day of treatment, the lesion was soaked in normal saline for 10 min. After the scab on the surface was soft, we routinely disinfected the periungual and subungual skin of the patient with iodophor. The patient was instructed to remain calm, and a sterile surgical blade was used to cut part of the nail plate, periungual and subungual wart keratinisation layer until there was punctate slight bleeding at the base. 236 mg of ALA hydrochloride topical powder was formulated into a solution with a concentration of 20%, applied topically and encapsulated for 3 hours. 635 nm semiconductor laser therapeutic instrument was used for local irradiation. Parameter selection: wavelength of 635 nm, power density of 80 mW/cm2, spot area of 3 cm. The edge of the lesion expanded by 1 cm, irradiation time of 20 min, once a week, and a total of 3 treatments. During the treatment, the patient was instructed to pay attention to personal hygiene, especially hand hygiene. When doing agricultural work, the hands were wrapped with medical gauze to avoid scratching. Iodophor was soaked twice a day for 5–10 min each time, and fuxidi acid cream was applied externally to prevent secondary infection. The patient had obvious pain during the treatment and within 24 hours after operation but still insisted on completing the treatment for three times [Figure 3a and b]. In order to reduce the patient’s pain, we gave the patient a small electric fan to blow cold air at the treatment site during operation, and oral nonsteroidal painkillers 2 hours before operation. The whole process of treatment is shown in the figures 2 and 3. Four weeks after the third treatment, the wart completely disappeared. There was no recurrence in the follow-up visit 3 months after the end of treatment. There was no recurrence in the follow-up visit 6 months/1 year after the end of treatment [Figure 4].
Figure 3.
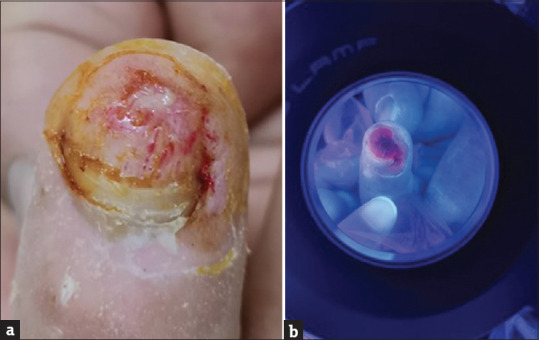
Pretreatment before the third illumination. (a) The pretreatment steps are basically the same as the second treatment, (b) The plate around the wart is cut with a blade to facilitate the removal of the latent infection foci 3-hour fluorography of the third photodynamic application
Figure 4.

Six months after treatment
Discussion
Warts are caused by HPV infection and can involve multiple parts of skin and mucosa, of which periungual and subungual warts are the most difficult to treat and can relapse repeatedly. The treatment of warts usually focuses on the physical destruction of lesions (i.e., viral cells), including liquid nitrogen cryotherapy,[3] curettage, excision, CO2 laser ablation, pulsed dye laser therapy,[4] electrosurgery, and the application of various local acid preparation.[5,6] Other methods reported in the dermatological literature include the use of infrared coagulation,[7] interferon-a, local application of 5-fluorouracil,[8] intralesional injection of bleomycin[9] and local application of dinitrochlorobenzene.[10] However, external use of drugs often causes local skin allergy to contact dermatitis and termination of treatment; CO2 laser and liquid nitrogen cryotherapy may leave scars, affect the nail matrix and the repair of the nail plate.[1] Moreover, some patients still have recurrent attacks after the above treatment, especially periungual warts and subungual warts. Therefore, the choice of treatment methods with better therapeutic effects and less adverse reactions has always been the demand of patients with periungual warts and subungual warts at home and abroad, and it is also the pursuit of dermatologists.
In the late 1970s, Thomas Doherty and his colleagues developed PDT using hematoporphyrin derivatives. PDT is a treatment modality that uses photosensitisers and light to selectively cause cell death in the presence of oxygen and an appropriate light source, thereby removing the corresponding lesions. Reactive oxygen species (ROS) can directly kill HPV-infected keratinocytes and activate local antiviral immunity.[11] The application of ALA in PDT in the treatment of skin diseases was first introduced in 1990.[12] 5-ALA is an amino acid and a precursor of Protoporphyrin IX (PPIX). Topically applied ALA enters epidermal cells and their appendages and is endogenously converted to PPIX, an active photosensitising compound, via the porphyrin pathway.[12,13] PPIX selectively accumulates in malignant cells, epidermal cells, sebaceous glands and hair follicles.[14] PDT uses a variety of light sources. In order to achieve the most effective treatment effect of PDT, it is important to select the appropriate wavelength of light corresponding to the largest area of the porphyrin activation spectrum in the tissue.[15] Longer wavelengths of light, such as red light, are suitable for thicker skin lesions.[15] In addition to the direct phototoxic effect on target tissues, PDT can also stimulate a variety of immune cells and inflammatory cell mediators, and vice versa. Immune-specific responses during PDT include the production of various cytokines, such as interleukin (IL)-1-β IL-2 and tumour necrosis factor-α. Matrix metalloproteinase (MMP)-1 and MMP-3 are also secreted by fibroblasts in response to PDT.[16,17] Following low light doses, PDT and various photosensitisers have been proved to change the expression of cytokines and induce immune-specific response, so as to produce immune regulation in inflammatory skin diseases.[18,19] The main advantages of local ALA-PDT are that it has no photosensitivity of the whole-body skin and can treat multiple lesions at the same time with low invasiveness, good tolerance and cosmetic effect.[15] PDT has been widely used in many dermatological diseases especially those related to HPV infection[20,21] without causing significant side effects and with satisfactory cosmetic results.[22] Kai Huang et al.[2] found that the superficial shaving with-PDT (SSPDT) group achieved a 91.3% success rate after 6 months of treatment compared to only 23.1% in the cryotherapy group and after 6 months of follow-up, the recurrence rate of SSPDT group was significantly lower than that of cryotherapy group (8.7% vs. 76.9%, P < 0.001) in a comparative study of superficial curettage combined with PDT and cryotherapy in the treatment of intractable plantar warts. Satisfaction with treatment was higher in SSPDT patients than in cryotherapy patients. They found that moderate pain is the main adverse event of SSPDT, and cryotherapy can cause severe pain and blistering. Their results showed that superficial curettage combined with PDT is a safe and effective method for the treatment of plantar warts, especially for patients with multiple intractable warts. The efficacy and safety are significantly better than liquid nitrogen cryotherapy.
Possible side effects of PDT include pain, erythema, swelling, blister, ulcer, burning, pigmentation and so on.[12,23] Pain is the most common side effect of local PDT and can often be severe. The generation of pain in ALA-PDT treatment is related to the generation of a large amount of ROS during illumination, and its specific mechanism is not clear. The degree of pain is associated with lesion type, lesion location, lesion area and illumination parameters.[24,25] Pain management is an important part of ALA-PDT in the treatment of skin diseases.[24] It is recommended to carry out a numeric pain rating scale (NPRS, 0 to 10 points) for patients when illuminated and take corresponding treatment schemes according to the pain classification.[26] Although there are many ways to deal with pain, many patients still cannot tolerate it and terminate treatment.
Clinically, few doctors routinely use PDT to treat viral warts, which may be due to a lack of standardised protocol.[15] We reviewed and summarised the literature findings on the treatment of periungual warts and subungual warts: Wu et al.[1] successfully treated a case of periungual and subungual warts with an electric shaver and PDT. After two PDT treatments, the warts were completely removed without scars or nail deformities. During the 2-year follow-up, no recurrence was observed. Wu et al.[27] observed the efficacy of superficial curettage and PDT in the treatment of intractable periungual warts. In 23 patients, a 96% success rate was obtained after 3 months of superficial shaving combined with PDT. At the 12-month follow-up, 21 patients (91%) had good cosmetic results. All patients were satisfied with the treatment effect and their quality of life was significantly improved. Pain during irradiation was the major adverse event but was tolerated by all patients. They also found that frequent or sustained hand activities, such as playing Mahjong, may be a potential risk factor for periungual warts. Yoo et al.[28] treated 40 periungual warts with CO2 laser combined with PDT. After an average of 2.2 treatments for each wart, the average clearance rate of 36 (90%) warts reached 100%. The clearance rate of 2 warts (5%) was 50%, and 2 warts (5%) did not respond after 3 treatments. During the 6-month follow-up period, warts that achieved 100% clearance did not recur. Most patients had no serious side effects during or after treatment. Schroeter et al.[29] used a sandpaper sheet 2 days before treatment to reduce the epithelial layer of the wart in 20 patients with a total of 40 periungual and subungual warts. At least 48 hours before each irradiation, the warts were scraped off with a scalpel and treated with PDT. After an average of 4.5 treatments, 18 of 20 patients (36 of 40) had complete clearance of the hand periungual warts, with a mean clearance rate of 100% in 90% of patients. One patient (5%) had a 50% clearance rate and the other did not improve. The periungual or subungual position of warts had no effect on the number of treatments or the final result (P > 0.05). During an average follow-up of 5.9 months, 2 cases recurred. Before the administration of PDT, the skin lesions of the above patients were scraped or pretreated with CO2 laser to enhance the transdermal efficiency of ALA and improve the curative effect. The main side effect was pain, but the treatment was not stopped [Table 1].
Table 1.
Clinical study of local PDT in the treatment of periungual and subungual warts
| First Author, Year [Reference] | Number of Patients | number of treatments | Effective rate (%) | Side effects | Combined approaches | Recurrence rate |
|---|---|---|---|---|---|---|
| Wu MF, 2020[1] | 1 | 2 | 100 | Local burning pain, erythema and blisters | Electric shaving, curettage and photodynamic therapy | 0 |
| Wu L, 2019[27] | 23 patients, 61 periungual lesions | 3 | 96% after treatment for 3 months. 91%, At the 12-month follow-up | Pain, Secondary Onychodystrophy, Mild itching Blister the patients did not need to stop treatment | The combination of superficial shaving with photodynamic therapy | 2 cases, 9% |
| Yoo KH, 2009[28] | 12 patients, 40 periungual lesions | 1-3 | 96% | Mostly mild pain and erythema | CO2 fractional laser ALA-PDT | Warts that achieved 100% clearance did not recur. |
| Schroeter CA, 2007[29] | 20 patients, 40 periungual lesions | Average 4.5 | 90% | Pain, Erythema, Burning, Itching, Oedema | using sandpaper sheets + scalpel curettage + PDT | 1.2% |
In this patient, due to the large area of skin lesions, we used liquid nitrogen cryotherapy before the first PDT, and they crusted after one week. On the day of treatment, the lesions were soaked in normal saline for 10 min. After the surface crust was soft, we routinely disinfected the affected area around and under the nail with iodophor. A sterile surgical blade was used to remove the scab, the superficial skin lesions of the periungual and subungual hyperplasia and part of the nail plate. After the base saw punctate slight bleeding, we performed ALA-PDT treatment three consecutive times. Curettage combined with PDT rather than cryotherapy was performed for the second and third time. Except for pain (the patient did not stop treatment due to pain), there were no other adverse reactions. It shows that PDT combined with liquid nitrogen cryotherapy and curettage therapy is indeed worth trying to treat patients with intractable periungual and subungual warts, and we look forward to more literature reports. It is worth noting that there is no good solution to the adverse pain reactions brought to patients during treatment, and some even hinder the further treatment of patients. Domestic experts recommend that patients should be given a numeric pain rating scale (NPRS, 0–10 points) when exposed to light, and corresponding treatment plans should be adopted according to the pain classification, see Table 2.
Table 2.
Grading of pain during 5-aminolevulinic acid-based photodynamic therapy and the corresponding recommended strategies[26]
| Pain grades | Recommended countermeasures |
|---|---|
| Mild: 1≤ NPRS* ≤3 |
Advise the patients to relax and alleviate the pain with local cold air, cold spray cooling or lidocaine pump spray |
| Moderate: 3< NPRS ≤6 |
In addition to the measures for mild pain, local infiltration anaesthesia, nerve block anaesthesia, two-step intermittent illumination or reduction of the power density of illumination can also be carried out. |
| Severe: 6< NPRS ≤10 |
Pay close attention to the patient's vital signs. It is recommended to take tramadol, morphine and topical fentanyl patch, and the treatment can be terminated if necessary. General anaesthesia may be used in special cases. |
However, some patients still do not accept these pain management methods.[16,17] In addition, the high cost of ALA-PDT compared with topical drugs and other traditional physical therapy methods is also one of the reasons that prevent patients from choosing this treatment method in the first place.
Interestingly for this patient, one month ago, the patient came to our hospital again because of a wart on the upper lip mucosa. Because the upper lip mucosa was punctured by fish thorns when eating fish, and warts appeared 2 weeks later, he came to our hospital for treatment and chose liquid nitrogen cryotherapy. We checked again and found that the patient’s original hand periungual warts and subungual warts did not recur. Causes of wart recurrence or infection include: 1. virus invasion; 2. barrier destruction and 3. decreased immune function. How to reduce infection and recurrence is also what we should inform patients.
In conclusion, PDT is indeed a good method for the treatment of periungual warts and subungual warts, with clear curative effects and few side effects. Few doctors routinely use PDT to treat viral warts, possibly because: 1. of lack of standardised scheme, 2. of higher treatment cost, 3. each treatment takes a long time and 4. some patients have obvious pain, and there is no good and standardised method to solve the pain. Therefore, it is hoped that there will be a method to solve the above-mentioned problems, in order to bring greater benefits to patients. The painless ALA-PDT clinical studies currently being carried out by domestic scholars[30] are believed to overcome the pain problem in ALA-PDT treatment.
PDT endpoint should include a combination of pain and efficacy, ideally optimising for both. Consideration must also be given to including treatment time and the workload of medical staff. Long-term, reproducible and standardised data are still needed to provide effective, painless, cost-effective and clinically meaningful PDT protocols.[31]
Authorship: Kuixia Xie and Meihong Cheng performed the treatment. Bo He and Wenying Zhong proposed the study and wrote the manuscript. Wei Li performed the follow-up.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wu MF, Lv T, Miao F, Wang XL, Liu YQ, Wang HW. Periungual and subungual warts successfully treated with combination of electric shaving, curettage, and photodynamic therapy. Photodermatol Photoimmunol Photomed. 2021;37:82–4. doi: 10.1111/phpp.12599. [DOI] [PubMed] [Google Scholar]
- 2.Huang K, Xie Y, Li M, Liu D, Su J, Li F, et al. A comparative study: Superficial shaving combined with photodynamic therapy versus cryotherapy in the treatment of recalcitrant plantar warts. Lasers Surg Med. 2020;52:747–52. doi: 10.1002/lsm.23212. [DOI] [PubMed] [Google Scholar]
- 3.Bourke JF, Berth-Jones J, Hutchinson PE. Cryotherapy of common viral warts at intervals of 1, 2 and 3 weeks. Br J Dermatol. 1995 Mar;132:433–6. doi: 10.1111/j.1365-2133.1995.tb08678.x. [DOI] [PubMed] [Google Scholar]
- 4.Tan OT, Hurwitz RM, Stafford TJ. Pulsed dye laser treatment of recalcitrant verrucae: A preliminary report. Lasers Surg Med. 1993;13:127–37. doi: 10.1002/lsm.1900130120. [DOI] [PubMed] [Google Scholar]
- 5.Hirose R, Hori M, Shukuwa T, Udono M, Yamada M, Koide T, et al. Topical treatment of resistant warts with glutaraldehyde. J Dermatol. 1994;21:248–53. doi: 10.1111/j.1346-8138.1994.tb01731.x. [DOI] [PubMed] [Google Scholar]
- 6.Bunney MH, Nolan MW, Williams DA. An assessment of methods of treating viral warts by comparative treatment trials based on a standard design. Br J Dermatol. 1976;94:667–79. doi: 10.1111/j.1365-2133.1976.tb05167.x. [DOI] [PubMed] [Google Scholar]
- 7.Halasz CL. Treatment of common warts using the infrared coagulator. J Dermatol Surg Oncol. 1994;20:252–6. doi: 10.1111/j.1524-4725.1994.tb01620.x. [DOI] [PubMed] [Google Scholar]
- 8.Brodell RT, Bredle DL. The treatment of palmar and plantar warts using natural alpha interferon and a needleless injector. Dermatol Surg. 1995;21:213–8. doi: 10.1111/j.1524-4725.1995.tb00155.x. [DOI] [PubMed] [Google Scholar]
- 9.James MP, Collier PM, Aherne W, Hardcastle A, Lovegrove S. Histologic, pharmacologic, and immunocytochemical effects of injection of bleomycin into viral warts. J Am Acad Dermatol. 1993;28:933–7. doi: 10.1016/0190-9622(93)70133-e. [DOI] [PubMed] [Google Scholar]
- 10.Shah KC, Patel RM, Umrigar DD. Dinitrochlorobenzene treatment of verrucae plana. J Dermatol. 1991;18:639–42. doi: 10.1111/j.1346-8138.1991.tb03148.x. [DOI] [PubMed] [Google Scholar]
- 11.Xie J, Wang S, Li Z, Ao C, Wang J, Wang L, et al. 5-aminolevulinic acid photodynamic therapy reduces HPV viral load via autophagy and apoptosis by modulating Ras/Raf/MEK/ERK and PI3K/AKT pathways in HeLa cells. J Photochem Photobiol B. 2019;194:46–55. doi: 10.1016/j.jphotobiol.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy JC, Pottier RH, Pross DC. Photodynamic therapy with endogenous protoporphyrin IX: Basic principles and present clinical experience. J Photochem Photobiol B. 1990;6:143–8. doi: 10.1016/1011-1344(90)85083-9. [DOI] [PubMed] [Google Scholar]
- 13.Iinuma S, Farshi SS, Ortel B, Hasan T. A mechanistic study of cellular photodestruction with 5-aminolaevulinic acid-induced porphyrin. Br J Cancer. 1994;70:21–8. doi: 10.1038/bjc.1994.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Divaris DX, Kennedy JC, Pottier RH. Phototoxic damage to sebaceous glands and hair follicles of mice after systemic administration of 5-aminolevulinic acid correlates with localized protoporphyrin IX fluorescence. Am J Pathol. 1990;136:891–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Kim M, Jung HY, Park HJ. Topical PDT in the treatment of benign skin diseases: Principles and new applications. Int J Mol Sci. 2015;16:23259–78. doi: 10.3390/ijms161023259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zheng Z, Zhang LL, Shi L, Zhang YF, Wang B, Wu QQ, et al. What is the most relevent factor causing pain during ALA-PDT?A multi-center, open clinical pain score research trial of actinic keratosis, acne and condylomata acuminata. Photodiagnosis Photodyn Ther. 2019;26:73–8. doi: 10.1016/j.pdpdt.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 17.Ang JM, Riaz IB, Kamal MU, Paragh G, Zeitouni NC. Photodynamic therapy and pain: A systematic review. Photodiagnosis Photodyn Ther. 2017;19:308–44. doi: 10.1016/j.pdpdt.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Mroz P, Yaroslavsky A, Kharkwal GB, Hamblin MR. Cell death pathways in photodynamic therapy of cancer. Cancers (Basel) 2011;3:2516–39. doi: 10.3390/cancers3022516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karrer S, Bosserhoff AK, Weiderer P, Landthaler M, Szeimies RM. Keratinocyte-derived cytokines after photodynamic therapy and their paracrine induction of matrix metalloproteinases in fibroblasts. Br J Dermatol. 2004;151:776–83. doi: 10.1111/j.1365-2133.2004.06209.x. [DOI] [PubMed] [Google Scholar]
- 20.Wang YS, Tay YK, Kwok C, Tan E. Photodynamic therapy with 20% aminolevulinic acid for the treatment of recalcitrant viral warts in an Asian population. Int J Dermatol. 2007;46:1180–4. doi: 10.1111/j.1365-4632.2007.03210.x. [DOI] [PubMed] [Google Scholar]
- 21.Ozog DM, Rkein AM, Fabi SG, Gold MH, Goldman MP, Lowe NJ, et al. Photodynamic therapy: A clinical consensus guide. Dermatol Surg. 2016;42:804–27. doi: 10.1097/DSS.0000000000000800. [DOI] [PubMed] [Google Scholar]
- 22.Wan MT, Lin JY. Current evidence and applications of photodynamic therapy in dermatology. Clin Cosmet Investig Dermatol. 2014;7:145–63. doi: 10.2147/CCID.S35334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Itkin A, Gilchrest BA. delta-Aminolevulinic acid and blue light photodynamic therapy for treatment of multiple basal cell carcinomas in two patients with nevoid basal cell carcinoma syndrome. Dermatol Surg. 2004;30:1054–61. doi: 10.1111/j.1524-4725.2004.30317.x. [DOI] [PubMed] [Google Scholar]
- 24.Wang B, Shi L, Zhang YF, Zhou Q, Zheng J, Szeimies RM, et al. Gain with no pain?Pain management in dermatological photodynamic therapy. Br J Dermatol. 2017;177:656–65. doi: 10.1111/bjd.15344. [DOI] [PubMed] [Google Scholar]
- 25.Zheng Z, Zhang LL, Shi L, Zhang YF, Wang B, Wu QQ, et al. What is the most relevent factor causing pain during ALA-PDT?A multi-center, open clinical pain score research trial of actinic keratosis, acne and condylomata acuminata. Photodiagnosis Photodyn Ther. 2019;26:73–8. doi: 10.1016/j.pdpdt.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 26.Shi L, Wang H, Chen K, Yan J, Yu B, Wang S, et al. Chinese guidelines on the clinical application of 5-aminolevulinic acid-based photodynamic therapy in dermatology (2021 edition) Photodiagnosis Photodyn Ther. 2021;35:102340. doi: 10.1016/j.pdpdt.2021.102340. doi:10.1016/j.pdpdt.2021.102340. [DOI] [PubMed] [Google Scholar]
- 27.Wu L, Chen W, Su J, Li F, Chen M, Zhu W, et al. Efficacy of the combination of superficial shaving with photodynamic therapy for recalcitrant periungual warts. Photodiagnosis Photodyn Ther. 2019;27:340–4. doi: 10.1016/j.pdpdt.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 28.Yoo KH, Kim BJ, Kim MN. Enhanced efficacy of photodynamic therapy with methyl 5-aminolevulinic acid in recalcitrant periungual warts after ablative carbon dioxide fractional laser: A pilot study. Dermatol Surg. 2009;35:1927–32. doi: 10.1111/j.1524-4725.2009.01307.x. [DOI] [PubMed] [Google Scholar]
- 29.Schroeter CA, Kaas L, Waterval JJ, Bos PM, Neumann HA. Successful treatment of periungual warts using photodynamic therapy: A pilot study. J Eur Acad Dermatol Venereol. 2007;21:1170–4. doi: 10.1111/j.1468-3083.2007.02081.x. [DOI] [PubMed] [Google Scholar]
- 30.Zhang Y, Zhang H, Zhang L, Wang P, Shi L, Zhang G, et al. Modified 5-aminolevulinic acid photodynamic therapy to reduce pain in the treatment of moderate to severe acne vulgaris: A prospective, randomized, split-face study. J Am Acad Dermatol. 2021;84:218–20. doi: 10.1016/j.jaad.2020.04.146. [DOI] [PubMed] [Google Scholar]
- 31.Ang JM, Riaz IB, Kamal MU, Paragh G, Zeitouni NC. Photodynamic therapy and pain: A systematic review. Photodiagnosis Photodyn Ther. 2017;19:308–44. doi: 10.1016/j.pdpdt.2017.07.002. [DOI] [PubMed] [Google Scholar]


