Abstract
Introduction
Pityriasis amiantacea (PA) is a rare presentation characterized by the presence of extensive adherent scaling that tightly encircles and affixes tufts of hairs secondary to inflammatory or infectious dermatoses. However, the occurrence of PA as a consequence of leukaemia cutis has not been previously reported.
Case Report
A 32-year-old man with B-cell acute lymphoblastic leukaemia (B-ALL) presented with severe scalp scaling and hair loss for 2 months. Examination revealed extensive, tightly adherent scales encircling and binding down hairs, along with haemorrhagic crusts. Skin examination showed nontender, partially blanchable papules forming ill-defined plaques, giving a cobblestone appearance. Trichoscopy revealed white crusts, tufting, and micro-haemorrhages. Scalp biopsy confirmed precursor B-ALL infiltration. He was diagnosed with PA with secondary cutis verticis gyrata due to leukaemia cutis and referred to a haemato-oncologist for further management.
Discussion
Leukaemia cutis is a rare condition where leukaemia cells infiltrate the skin, often associated with acute myeloid leukaemia and ALL. It can lead to secondary verticis gyrata. The co-occurrence of PA and cutis verticis gyrata is rare and previously unreported, highlighting the need for increased awareness among clinicians.
Keywords: Leukaemia cutis, Pityriasis amiantacea, Cutis verticis gyrata, Dermoscopy, B-cell acute lymphoblastic leukaemia
Established Facts
-
•
Pityriasis amiantacea is a rare presentation associated with inflammatory or infectious dermatoses of the scalp.
-
•
Cutis verticis gyrata secondary to leukaemia cutis of the scalp has been reported previously.
Novel Insights
-
•
Pityriasis amiantacea secondary to leukaemia cutis has not been reported previously.
-
•
Trichoscopy can be a valuable tool in diagnosis of leukaemia cutis.
Introduction
Pityriasis amiantacea (PA) is a rare reaction pattern characterized by the presence of extensive adherent scaling that tightly encircles and affixes tufts of hairs. Although it usually presents in association with inflammatory dermatoses (scalp psoriasis, seborrhoeic dermatitis, atopic dermatitis) or infections (tinea capitis, pediculosis capitis with secondary bacterial infection), it may also occur as an idiopathic entity [1]. However, the occurrence of PA as a consequence of leukaemia cutis has not been previously reported. We report a rare occurrence of PA with cutis verticis gyrata (CVG) secondary to leukaemia cutis in an adult male.
Case Report
A 32-year-old male presented with thick adherent scales on the scalp associated with hair loss for 2 months. He was diagnosed with B-cell acute lymphoblastic leukaemia (B-ALL) 2 weeks back and was planned for chemotherapy. On examination, there were thick adherent scales limited to the scalp encircling the hair, leading to tufting and binding down of hairs (Fig. 1), with a diffusely decreased density of hair and haemorrhagic crusts. Punctate bleeding points were visible upon removal of scales. A closer examination of the scalp revealed skin coloured to erythematous nontender, partially blanchable, 3–4 mm papules coalescing to form ill-defined plaques, giving it a cobblestone appearance. The scalp skin was folded at places resembling the ridge and furrow of the cerebral cortex. The rest of the cutaneous examination, including nails, did not reveal any abnormality. Regional lymphadenopathy was present. Trichoscopy revealed white crusts and tufting with polytrichia (multiple hairs arising from a single opening). Multiple areas of micro-haemorrhages were also identified, more conspicuous in areas devoid of scales (Fig. 1b). In addition, multiple coalescent skin-coloured papules leading to cobble stoning were also visualized (Fig. 2c).
Fig. 1.
a Thick adherent scales with tufting of hair. b Polarized trichoscopy showing thick adherent scales with tufting of hair and multiple areas of micro-haemorrhages (×10).
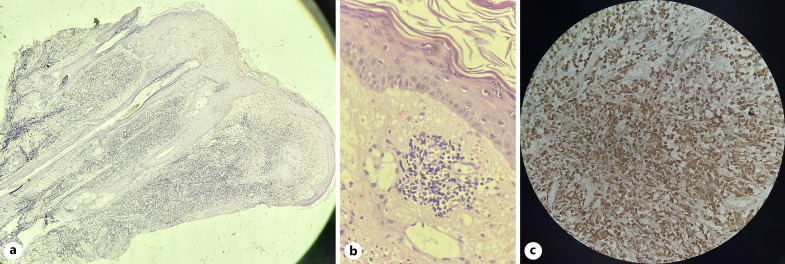
Fig. 2.
Histopathological examination showing (a) Dense diffuse dermal infiltrate of atypical intermediate-to-large-sized lymphocytes below a broad grenz zone (×40); (b) Intermediate-to-large-sized atypical lymphocytes (×100); (c) Strong immunopositivity of lymphocytes for TdT (×100).
The potassium hydroxide mount of the scales did not reveal any fungal elements. Histology of scalp punch biopsy showed a dense dermal infiltrate of atypical lymphocytes extending up to the subcutaneous tissue below a broad grenz zone (Fig. 2a). The cells were variable-sized and showed hyperchromasia and atypia (Fig. 2b). The atypical cells were positive for TdT (Fig. 2c) and negative for CD3 and CD20, consistent with precursor B-ALL.
Based on the history, examination, dermoscopy, and histology, the patient was diagnosed as a case of PA with secondary CVG due to leukaemia cutis of the scalp and was prescribed clobetasol propionate 0.05% (w/v) + salicylic acid 6% (w/v) lotion for topical application and referred to a haemato-oncologist for the management of B-ALL. However, the treatment response could not be assessed as the patient was lost to follow-up.
Discussion
Leukaemia cutis is a rare manifestation of leukaemia, characterized by the infiltration of leukaemic cells into the skin, presenting as macules, papules, nodules, plaques, or ulcers. It can be the presenting sign or a marker of relapse in patients with leukaemia. Acute myeloid leukaemia and ALL are the most common leukaemia associated with leukaemia cutis [2]. The diagnosis relies on a combination of clinical evaluation, histopathology for confirming the presence of leukaemic infiltrates, immunophenotyping for delineating specific lineage of leukaemic cells, and molecular studies to identify the specific subtype of leukaemia. Skin infiltration occurs due to the migration of leukaemic cells through the blood vessels under the influence of chemoattractants [3]. Dermoscopy shows variable-coloured structureless areas and polymorphic vessels [4].
Leukaemia cutis is known to result in the development of secondary CVG characterized by folding and thickening of the scalp with both horizontal and vertical furrows, resulting in a convoluted appearance that resembles the gyri of the brain. However, the involvement is usually focal; global involvement of the scalp, as seen in the present case, is usually rare [5]. Other reported associations include neurofibromatosis type 1, acromegaly, tuberous sclerosis, pachydermoperiostosis, intradermal naevi, systemic lupus erythematosus, seborrhoeic dermatitis, and psoriasis. Medications, such as phenytoin and minoxidil, have also been implicated. However, the pathogenesis remains enigmatic [1]. Dermoscopy of leukaemia-associated CVG shows the presence of multiple dotted and linear vessels with background erythema [6].
PA presents as thick, silvery-white adherent scales that tightly adhere to the hair shafts, resulting in a distinctive asbestos-like appearance. The hair gets matted and the scales are difficult to remove. Scalp pruritus, tenderness, and/or alopecia may be associated [1]. Like CVG, localized scalp involvement is more common than diffuse involvement. It is considered a secondary phenomenon resulting from an underlying dermatosis rather than a distinct primary condition. The associated diseases include seborrhoeic dermatitis, psoriasis, atopic dermatitis, tinea capitis, and pyoderma. The diagnosis of PA is primarily clinical [1]. Dermoscopy aids in the visualization of asbestos-like scales and polytrichia resulting from matting of hair [7]. However, identification of the underlying condition may require a potassium hydroxide mount of hair and skin scrapings, fungal culture, or scalp biopsy [1].
The management of PA and secondary CVG involves treatment of the underlying disease. To alleviate symptoms like itching and inflammation, topical corticosteroids, keratolytic agents, and emollients are used. In severe or refractory cases of PA, systemic therapies such as oral corticosteroids, other immunomodulatory drugs, or phototherapy may be considered [1, 6]. However, in severe cases of CVG, cosmetic improvement may be sought through surgical interventions like scalp reduction or dermabrasion [6].
Leukaemia cutis has a poor prognosis as it is often associated with an aggressive form of leukaemia with higher relapse and mortality rates. Its management depends on the type and stage of underlying leukaemia [2]. Systemic chemotherapy remains the mainstay of therapy, and achieving remission in the bone marrow is critical. In some cases, local therapies such as radiation, topical corticosteroids, or targeted agents may be employed to alleviate the associated signs and symptoms. Haematopoietic stem cell transplantation may be considered for eligible patients with refractory disease or in cases of relapse [2].
Both PA and CVG are rare conditions, and their co-occurrence, as seen in the present case, has not been reported previously. Furthermore, leukaemia cutis of the scalp has not been previously reported to be a cause of PA. Through this report, we aim to expand the existing knowledge base and raise awareness among clinicians regarding this atypical manifestation of leukaemia cutis.
Statement of Ethics
The study was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The subject has given his written informed consent to publish the case (including the publication of images). Institutional Ethical Review Board approval was not required for this study in accordance with national guidelines.
Conflict of Interest Statement
The authors have no conflicts of interest to declare. None of the authors report any form of support or financial involvement. There are no nonfinancial relationships (personal, political, or professional) that may potentially influence the writing of the manuscript.
Funding Sources
The authors did not receive any funding.
Author Contributions
Dr. Ankur Lal, Dr. Sushant Agrawal, and Dr. Vishal Gaurav contributed equally to the concept, design, and definition of intellectual content, data acquisition, and data analysis. Dr. Sushant Agrawal prepared the first draft of the manuscript. Dr. Vishal Gaurav did manuscript editing and review. Dr. Vishal Gaurav acted as the guarantor.
Funding Statement
The authors did not receive any funding.
Data Availability Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
- 1. Abdel-Hamid IA, Agha SA, Moustafa YM, El-Labban AM. Pityriasis amiantacea: a clinical and etiopathologic study of 85 patients. Int J Dermatol. 2003;42:260–4. [DOI] [PubMed] [Google Scholar]
- 2. Wagner G, Fenchel K, Back W, Schulz A, Sachse MM. Leukemia cutis – epidemiology, clinical presentation, and differential diagnoses. J Dtsch Dermatol Ges. 2012;10(1):27–36. [DOI] [PubMed] [Google Scholar]
- 3. Rao AG, Danturty I. Leukemia cutis. Indian J Dermatol. 2012;57(6):504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sławińska M, Sokołowska-Wojdyło M, Biernat W, Zaryczańska A, Nowicki RJ, Sobjanek M. Dermoscopic features of leukemia cutis: case series. Indian J Dermatol. 2021;66(2):187–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fustà-Novell X, Riquelme-Mc Loughlin C, Morgado-Carrasco D, García-Herrera A, Mascaró JM Jr. Cutis verticis gyrata secondary to acute myelogenous leukaemia. Clin Exp Dermatol. 2020;45(3):342–4. [DOI] [PubMed] [Google Scholar]
- 6. Diven DG, Tanus T, Raimer SS. Cutis verticis gyrata. Int J Dermatol. 1991;30(10):710–2. [DOI] [PubMed] [Google Scholar]
- 7. Errichetti E, Stinco G. Dermoscopy as a useful supportive tool for the diagnosis of pityriasis amiantacea-like tinea capitis. Dermatol Pract Concept. 2016;6(3):63–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.