Abstract
The squat is one of the most frequently prescribed exercises in the rehabilitative setting. Performance of the squat can be modified by changing parameters such as stance width, foot rotation, trunk position, tibia position, and depth. An understanding of how the various squatting techniques can influence joint loading and muscular demands is important for the proper prescription of this exercise for various clinical conditions. The purpose of this clinical commentary is to discuss how the biomechanical demands of the squat can be influenced by various modifiable parameters. General recommendations for specific clinical conditions are presented.
Level of Evidence
5
Keywords: kinetics, kinematics, biomechanics, squatting, clinical commentary
INTRODUCTION
Squatting is an essential movement pattern for activities of daily living (i.e., toileting and getting into or out of a chair) and various athletic tasks. As such, the squat exercise is commonly used in rehabilitation and sport performance settings to strengthen the primary lower extremity muscle groups (i.e., hip extensors and knee extensors).1–5 In addition, the squat exercise requires a high level of recruitment from the trunk muscles to provide stabilization for the spine and torso.4,6,7
The squat exercise can be highly variable in its execution. For example, the squat can be adapted by modifying trunk position, tibia position, foot rotation, stance width, and depth. Given that each modifiable factor can influence the biomechanics of the squat (i.e., muscular demands, joint loading, etc.), it is not surprising that the literature is conflicting when recommending various squatting techniques for different clinical situations.4,8 Interpretation of research related to squatting is difficult owing to the fact that many studies fail to control for the various modifiable parameters when assessing the influence of a specific variable.
It is important that clinicians be mindful of the various interactions among the modifiable parameters so that correct clinical recommendations can be made. As such, the purpose of this clinical commentary is to discuss how the biomechanical demands of the squat can be influenced by various modifiable parameters. General recommendations for specific clinical conditions are presented. It is hoped that the information presented will assist clinicians in the appropriate prescription of the squat exercise for patients with various diagnoses.
MODIFIABLE SQUAT PARAMETERS
Trunk Inclination
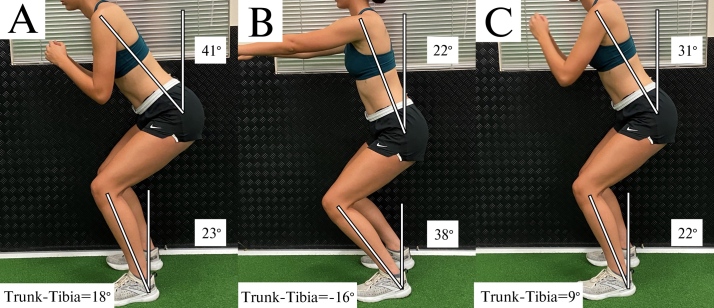
The moments at the hip and knee during squatting are highly influenced by the orientation of the trunk, which in turn affects the center of mass of the body.9,10 During a typical squat, the resultant ground reaction force vector passes anterior to the hip and posterior to the knee, thereby creating flexion moments at both joints (Figure 1).9 Muscular actions of the hip and knee extensors are required to generate extensor moments to counteract these external moments. Moving the trunk from a more upright position (Figure 1A) to more forward position (Figure 1B) shifts the resultant ground reaction force vector anteriorly, resulting in an increase in the hip flexion moment while simultaneously decreasing the knee flexion moment.11 Conversely, moving the trunk from a forward position (Figure 1B) to more upright position (Figure 1A) shifts the resultant ground reaction force vector posteriorly, thereby decreasing the hip flexion moment while simultaneously increasing the knee flexion moment.11
Figure 1. Sagittal plane orientation of the trunk influences the external moments at the hip and knee.
- Squatting with the trunk in a more upright position increases the knee flexion moment while decreasing the hip flexion moment. (B) Moving the trunk forward increases the hip flexion moment while decreasing the knee flexion moment.
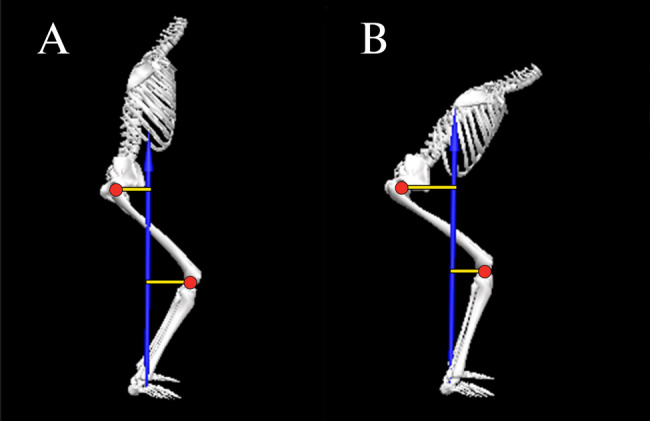
Apart from its influence on the hip and knee flexion moments, squatting with a forward trunk has an impact on the lumbar spine flexion moment. Generally speaking, the greater the forward trunk inclination, the greater the muscular demand on the back extensors to stabilize the trunk.12 It should be noted however, that forward inclination of the trunk can be obtained through flexion of the hip or flexion of the lumbar spine (Figure 2).13 Attainment of a forward trunk position using lumbar spine flexion (Figure 2A) results in decreased tolerance to compressive loads14 and lumber spine anterior shear forces as compared to when forward trunk inclination is achieved with a neutral spine position (Figure 2B).15 Maintaining a neutral spine position increases the moment arm for the spinal extensors thereby allowing better control of compressive loads and shear forces.14,15
Figure 2. Forward inclination of the trunk that is achieved by spine flexion (A) results in decreased tolerance to compressive loads and less control of anterior shear forces as compared to when forward trunk inclination is achieved with a neutral spine position (B).
Tibia Inclination
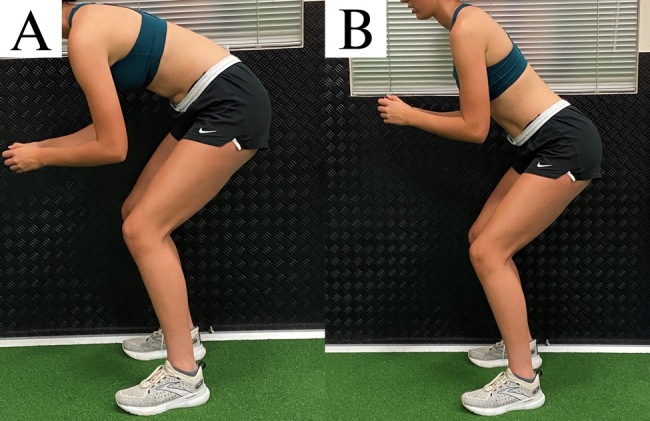
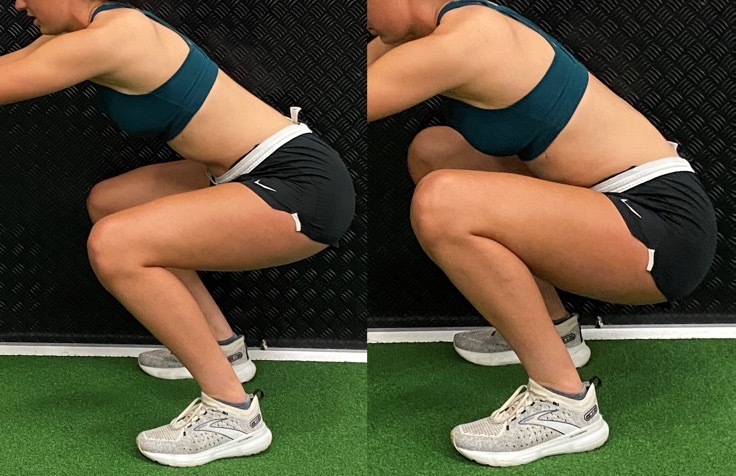
Compared to trunk inclination, inclination of the tibia during squatting has an opposite influence on the knee flexion moment.9,10,16–18 Moving the tibia from a more upright position (Figure 3A) to more forward position (Figure 3B) shifts the knee joint center further away from the resultant ground reaction force vector, thereby increasing the knee flexion moment. Conversely, moving the tibia from a forward position (Figure 3B) to more upright position (Figure 3A) shifts the knee joint center closer to the resultant ground reaction force vector, thereby decreasing the knee flexion moment.
Figure 3. Sagittal plane orientation of the tibia influences the external moment at the knee.
- Squatting with the tibia in a more upright position decreases the knee flexion moment. (B) Moving the tibia forward increases the knee flexion moment.
Forward tibia inclination can be achieved by either ankle dorsiflexion (with the foot flat on the floor) or squatting with the heels off the floor (i.e., using an external lift under the rearfoot or weightlifting shoes with an elevated heel).19 In general, elevating the heels during squatting facilitates a greater degree of forward tibia inclination, thereby increasing the knee flexion moment and the demand on the quadriceps.19,20 It should be noted however, that the forward tibia position when squatting with the heels elevated can occur without a corresponding increase in ankle dorsiflexion.
Foot Rotation
The degree of foot rotation during squatting can be accomplished by hip external rotation, knee external rotation, or a combination of both. The degree of toe out influences the frontal and transverse plane moments at the knee while having a negligible effect on the sagittal plane moments. For example, rotating the feet outward 30° has been reported to decrease the valgus moment at the knee by 50% while simultaneously increasing the varus moment by 80%.21 In addition, rotating the feet outward 30° decreases the external rotation moment at the knee by 20% when compared to a neutral stance.21
From a muscle recruitment standpoint, rotation of the foot outward 30° has no effect on activation of the quadriceps, hamstrings, or gastrocnemius when compared to a neutral foot position.2,22 Similarly, varying rotations of the tibia and femur from 30° inward to 80° outward has no effect on quadriceps activity.23 However, squatting with the hip externally rotated 30° to 50° has been reported to increase hip adductor activity compared to a neutral stance by 17% and 23% respectively (neutral: 13% of maximum voluntary isometric contraction [MVIC] vs. 17% and 23% MVIC for 30° and 50° rotation, respectively).24
Stance Width
For the purposes of this perspective, the authors operationally define stance width as narrow (75% to 100% shoulder width), medium (100% to 150% shoulder width), or wide (150% to 200% shoulder width). With respect to the frontal and transverse planes, a wide stance results in greater knee valgus moments (23%)25 and higher hip external rotation moments (19%-37%) when compared to narrow/medium stance squats.26 In terms of the sagittal plane, however, the impact of stance width is conflicting.25–27 Compared to a narrow/medium stance, the knee flexion moment during wide stance squatting has been reported to be higher (69%-80%),27 lower (11%),25 or not different.26 Similarly, the hip flexion moment during wide stance squatting has been reported to be higher (10%-48%)26,27 or not different compared to narrow/medium stance squatting.25 The conflicting results among studies can be explained by how authors controlled for other modifiable factors such as trunk and tibia orientation. For example, performing a wide stance squat with the trunk inclined would yield a different result than if the squat was performed with the trunk more upright.
From a muscle recruitment standpoint, a medium/wide stance squat has been reported to result in higher gluteus maximus activity (13%-61%)28,29 and 18% lower gastrocnemius activity (14% vs. 17% MVIC) compared to narrow/medium stance squats.2 Stance width does not appear to influence hamstring,28,29 quadriceps,28,29 or gluteus medius activity.29 In regards to hip adductor recruitment, stance width does not influence overall muscle activation.29 However, if the descending and ascending phases are analyzed separately, a wider stance increases hip adductor activity during the accent phase of squatting compared to the descent phase by approximately 50%.28
Squat Depth
For the purposes of this perspective, the authors operationally define squat depth as partial/shallow (0°-90° knee flexion), medium (90°-110° knee flexion or thigh parallel to floor), or full/deep (110°-135° knee flexion). Generally speaking, the knee flexion moment tends to steadily increase from an upright position to maximum knee flexion during squatting.30–32 Similarly, the hip flexion moment also increases with squat depth.32 However, the increase in the knee flexion moment with greater squat depth is not consistent across studies,33,34 and can be affected by the trunk and tibia orientation. For example, if the increase in trunk inclination with increasing depth is more pronounced than the increase in tibia inclination, this could potentially result in a relatively higher hip flexion moment relative to the knee flexion moment at higher depths. Conversely, if the increase in tibia inclination with increasing depth is more pronounced than the increase in trunk inclination, this could potentially result in a higher knee flexion moment relative to the hip flexion moment at greater squatting depths.
Apart from the influence of squat depth on hip and knee moments, studies examining muscle recruitment with increasing depth are conflicting. In regards to quadriceps activity, some studies have reported an increase in EMG activity with squat depth (29%),35 while others have not.1,5,36 Similarly, evidence related to hamstring activity also is conflicting, as studies have reported no change1,5,35 or a slight decrease in activation (absolute difference: 12% MVIC) with increasing squat depth.36 With respect to gluteus maximus, activity has been shown to increase from shallow to medium depth squatting by 65%1 but what happens thereafter is controversial. Compared to medium depth squats, gluteus maximus activity has been reported to be similar,5 or 25% greater with deep squats (28% vs. 35% MVIC).1 When comparing partial to deep squats, gluteus maximus activity has been reported to be higher with partial depths (absolute difference: 29% MVIC).36 As noted above, failure to account for trunk and tibia position with deep squatting likely underlies the inconsistent findings among studies.
From a joint motion standpoint, the primary limitation to deep squatting is the amount of available hip flexion. When end range of hip flexion is reached during squatting, a posterior pelvic tilt will occur (Figure 4). The posterior rotation of the pelvis is the result of the femur compressing into the acetabulum.37 Given that posterior pelvic tilt is coupled with lumbar spine flexion,37,38 compressive and shear forces occur at the lumbar spine.14,15,39 The fact that lumbar erector spinae activity does not increase beyond 90° of knee flexion,36 suggests that passive structures (i.e., posterior longitudinal ligament) provide the resistance to the spine flexion moment.
Figure 4. Squatting to a depth that exceeds available hip flexion results in a posterior pelvic tilt.
KNEE VS. HIP EXTENSOR BIASED SQUATTING
As noted above, inclination of the trunk and tibia have opposite effects on the knee flexion moments and therefore the demand on the quadriceps. Forward inclination of the tibia increases the knee flexion moment, while forward trunk inclination decreases the knee flexion moment. As such, considering the degree of tibia inclination without considering the degree of trunk inclination can result in erroneous interpretation of the biomechanical demand at the knee. For example, the increase in the knee flexion moment resulting from inclination of the tibia could be offset by forward inclination of the trunk.10 Therefore, the relationship between trunk and tibia inclination may be a better way to characterize the biomechanical demands of the knee extensors during squatting.
Evidence in support of this premise is provided by Barrack et al., who demonstrated that the relative demand of the hip and knee extensors during squatting could be predicted based on the relative inclination of the trunk and tibia.11 Specifically, the authors reported that the difference between sagittal plane inclination of the trunk and sagittal plane inclination of the tibia (i.e., trunk-tibia angle) at peak knee flexion was predictive of the average hip/knee flexion moment ratio during the decent phase of squatting. The regression model indicated that a trunk-tibia angle of -8° resulted in a hip/knee flexion moment ratio equal to 1.0.11 When the degree of trunk inclination exceeded the degree of tibia inclination (i.e., trunk-tibia angle > 0), a hip extensor bias squat was observed (i.e., hip/knee flexion moment ratio > 1.0). Conversely, when tibia inclination exceeded trunk inclination (by at least 8°), the squat became knee extensor biased (i.e., hip/knee flexion moment ratio < 1.0).11
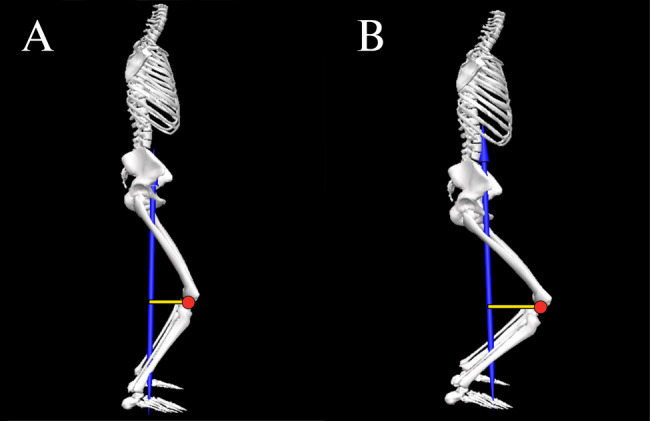
Based on the findings of Barrack et al., it is possible to characterize the relative demand of the hip and knee extensors using the trunk-tibia inclination difference.11 When the degree of trunk inclination exceeds the degree of tibia inclination by 10°, a hip extensor bias can be inferred (Figure 5A). When the degree of tibia inclination exceeds the degree of trunk inclination by 10°, a knee extensor bias squat can be inferred (Figure 5B). In situations where the degree of trunk and tibia inclination are within 10° or each other, the relative demands on the hip and knee extensors can be considered equal (i.e., neutral bias) (Figure 5C).
Figure 5. Trunk-tibia angle (bottom left).
- Hip extensor bias with trunk-tibia angle > 10°; (B) Knee extensor bias with trunk-tibia angle < -10°; (C) Neutral bias with -10° trunk-tibia angle 10°.
The orientation of the trunk relative to the tibia (and therefore the hip/knee flexion moment ratio) can be influenced by the location of the applied load. For example, when the load is placed anteriorly (i.e., barbell front squat or goblet squat), the trunk is typically held in a more upright position. Conversely, a traditional barbell back squat typically is performed with greater trunk flexion.4,40 Therefore, it is not surprising that studies have reported differing muscular demands during these squat types. Back squats are associated with higher hip flexion moments, whereas front squats exhibit higher knee flexion moments, assuming the same absolute load.40
CLINICAL APPLICATIONS
When prescribing the squat as a therapeutic exercise, the desired clinical outcome needs to be considered. For example, knee extensor bias squatting may be indicated for patients with quadriceps weakness. In contrast, performing the squat with a hip extensor bias may be preferred if the goal is to the increase strength of the hip musculature. Based on the literature reviewed above, recommendations for performing the squat exercise for various clinical conditions are presented below (Table 1).
Table 1. Summary of Squat Parameters for Clinical Conditions.
| Patellofemoral pain |
Acute Phase (hip bias)
Sub-Acute Phase (progress to neutral and/or knee bias squat)
|
| Post Anterior Cruciate Ligament Reconstruction |
Acute Phase (hip bias)
Sub-Acute Phase (progress to knee bias squat)
|
| Femoroacetabular impingement |
|
| Low Back Pain |
|
| Tibiofemoral Osteoarthritis |
Acute Phase (hip bias)
Sub-Acute Phase (progress to knee bias squat)
|
Patellofemoral pain (PFP)
Clinical guidelines for persons with PFP advocate for hip and knee extensor strengthening.41 During the acute phase of the rehabilitation process, hip biased squats should be considered to reduce the demand on the quadriceps. This is important as quadriceps force contributes directly to patellofemoral joint reaction force and patellofemoral joint stress.42 During the sub-acute or recovery phase, squats can be progressed as tolerated to be more neutral biased or even quadriceps biased by modifying the trunk-tibia relationship.
During the acute phase, gluteus maximus activation should be emphasized as this muscle controls hip adduction and internal rotation, motions known to contribute to patellofemoral joint stress and PFP.43,44 Increased gluteus maximus activation can be achieved through the use of wider stance squats,26–29 as well as external band resistance around the thighs.45,46 However, a squat stance that exceeds 150% shoulder width may result in elevated knee valgus moments.25 During the sub-acute or recovery phase, transitioning to more narrow/medium stance squats will promote greater tibial inclination47 and a quadriceps bias. Regardless of phase, a toe out position should be considered as this will result in a decrease in the knee valgus moment.21
Another important consideration for the patient with patellofemoral pain is squat depth. Patellofemoral joint stress steadily increases from partial to medium depth squatting (0° to 90°).42 The increase in patellofemoral joint stress is the result of a steadily increasing patellofemoral joint reaction force that is more pronounced than the increase in contact area as the knee flexes.42 Generally speaking, shallow-medium depth squats should be prescribed for the patient with patellofemoral pain to minimize joint stress. Furthermore, there is evidence that shallow squats may be more desirable for gluteus maximus activation compared to deep squats.36
Post Anterior Cruciate Ligament (ACL) Reconstruction
Clinical guidelines for persons post ACL reconstruction advocate for the restoration of knee extensor strength and symmetry.48,49 Patients with patellar tendon or quadriceps tendon autografts regain quadriceps strength more slowly and are more prone to anterior knee pain.50 Thus, slow and progressive loading of the quadriceps should be the focus. For patients with donor-site pain, slower rates of loading/tempo may be better tolerated to stimulate tendon remodeling and muscular strengthening.50 Given that patients post ACL reconstruction are susceptible to anterior knee pain, hip biased squatting should be considered to lower the demand on the quadriceps using the trunk-tibia relationship recommendations above. Secondary considerations for hip bias squatting early in the recovery process include external band resistance around the thighs to promote gluteus maximus and gluteus medius activation45,46 and avoidance of deep squats (i.e., recommendations highlighted above for PFP). Medium stance squats are preferred over wide stance squats to minimize the knee valgus moment.
As tolerance to donor site loading improves, squats should be modified to progressively emphasize quadriceps loading (i.e., knee biased squatting). This can be achieved by either modifying the trunk position (more upright), promoting greater tibial inclination, or a combination of both. Secondary considerations for the introduction of more knee bias squatting include the use of deeper squats to increase quadriceps demands (moments)30,32 and narrow/medium stance widths. Regardless of squat type utilized (hip vs. knee bias), care should be taken to avoid valgus and transverse plane moments at the knee by promoting some degree of toe out.21
Femoroacetabular impingement (FAI)
FAI, or abutment or impingement of the femoral neck against the acetabular labrum, can result in chondrolabral damage, thereby contributing to early onset of hip osteoarthritis.51,52 Persons with FAI exhibit impaired mobility at the hip (specifically hip flexion) and deficits in gluteal muscle activation.51,53 As such, selecting squatting mechanics that emphasize gluteus maximus and medius activation is prudent by optimizing the trunk-tibia relationship, utilizing a wider stance, and external band resistance around the thighs (see recommendations above).
Squat depth should be limited to avoid hip flexion beyond the patient’s available range of motion. This is important as patients with FAI have limited ability to posteriorly tilt the pelvis during squatting, which places them at greater risk for impingement.54 Deep squats (even if pain free) should be avoided. Although up to 25% of patients with FAI can perform deep squats without pain,55 it is important to note that deep squats impose large amplitudes of hip joint stress56 and increase the requirements for hip flexion and hip internal rotation,54,57 the hallmark movements that contribute to impingement. A toe out stance also should be considered as this will promote a greater degree of hip external rotation and gluteal activation, thereby minimizing the potential for impingment.54,58
Low Back Pain
Hip weakness (abductors, adductors, and extensors) is a common finding in persons with low back pain.59 As such, squatting recommendations for low back pain should aim to minimize the compressive and shear loads on the lumbar spine, while simultaneously promoting adequate hip muscle activation. However, trunk inclination should be limited to avoid excessive lumbar muscle strain. To obtain a hip bias squat with limited forward trunk lean, a wider stance width can be used. A wider stance will reduce ankle dorsiflexion,47 which will facilitate a more favorable trunk-tibia relationship to produce a hip bias. Additionally, a wider stance during squatting reduces lumbar loading26 and permits a more upright lumbar (less kyphosis).60 Secondary considerations for hip bias squatting include external band resistance around the thighs to promote gluteus maximus and gluteus medius activation.45,46
Similar to what was described above for FAI, squat depth should be limited to avoid flexing the hip beyond the available range of motion, thereby limiting posterior pelvic tilt. That is, squat depth should be limited to a depth in which a neutral spine can be maintained. As noted above, posterior pelvic tilt is coupled with lumbar spine flexion,37,38 resulting in compressive and shear forces occur at the lumbar spine.14,15,39
Tibiofemoral Osteoarthritis
Osteoarthritis is the most common joint disease,61 primarily affecting the tibiofemoral joint.62,63 Lower-extremity strength deficits are common in patients with knee osteoarthritis,64 highlighting the importance of appropriate squatting for overall lower extremity strength. High compressive loads in the tibiofemoral joint can worsen osteoarthritis by increasing stress/strain on internal structures (e.g., articular cartilage and menisci).65,66 Therefore, squatting recommendations for tibiofemoral osteoarthritis should prioritize lower extremity strengthening while reducing tibiofemoral loading. Similar to PFP and ACL recommendations above, patients with tibiofemoral joint arthritis should progress from a hip bias to knee bias using the trunk-tibia relationship recommendations.
As for the tibiofemoral joint, compressive forces steadily increase when squatting from a partial to a deep position.3,67 Since tibiofemoral contact area decreases with increasing knee flexion, contact stresses also increase.68,69 Therefore, deep squats should be avoided. Additional considerations for hip bias squatting early in the rehabilitation process to improve gluteal activation include external band resistance around the thighs45,46 and a wider stance.28,29 However, tibiofemoral compressive forces during a wide squat (compared to narrow squat) are approximately 15% higher.2
Considerations for knee bias squatting later in the rehabilitation process include transitioning to more narrow/medium stance squats to promote greater tibial inclination47 and a quadriceps bias. Regardless of squat type (hip vs. knee bias), outward foot rotation may need to be limited in the presence of medial compartment osteoarthritis but advised in the presence of lateral compartment osteoarthritis. An outwardly rotated foot decreases loading in the lateral compartment (by decreasing the knee valgus moment) but increases loading in the medial compartment (by increasing the knee varus moment).21
CONCLUSION
The squat can be a safe and effective exercise if properly executed for both rehabilitation and sport performance purposes. However, selection of specific squatting parameters requires a thorough understanding of their impact on muscle activity and joint loading. The preceding review examines these factors in detail and provides evidence to guide clinical decision making. It is important for clinicians to prescribe appropriate squatting parameters based on the individual needs of the patient to maximize the effectiveness of the exercise. Additional work is necessary to establish the appropriateness and effectiveness of squat exercise for patients with various musculoskeletal conditions. While the current review summarizes important research in this area, it should be noted that comparisons across the numerous studies cited (particularly those related to EMG) should be approached with caution owing to differences in data reduction/analysis (including normalization) and how various confounding factors were controlled.
Conflicts of interest
The authors report no conflicts of interest.
References
- The effect of back squat depth on the EMG activity of 4 superficial hip and thigh muscles. Caterisano A., Moss R.F., Pellinger T.K.., et al. 2002J Strength Cond Res. 16(3):428–32. [PubMed] [Google Scholar]
- Escamilla RAFAEL F., Fleisig GLENN S., Zheng NAIQUAN, LANDER JEFFERY E., BARRENTINE STEVEN W., ANDREWS JAMES R., BERGEMANN BRIAN W., MOORMAN CLAUDE T. III. Medicine & Science in Sports & Exercise. 9. Vol. 33. Ovid Technologies (Wolters Kluwer Health); Effects of technique variations on knee biomechanics during the squat and leg press; pp. 1552–1566. [DOI] [PubMed] [Google Scholar]
- Escamilla RAFAEL F. Medicine and Science in Sports and Exercise. 1. Vol. 33. Ovid Technologies (Wolters Kluwer Health); Knee biomechanics of the dynamic squat exercise; pp. 127–141. [DOI] [PubMed] [Google Scholar]
- Yavuz Hasan Ulas, Erdağ Deniz, Amca Arif Mithat, Aritan Serdar. Journal of Sports Sciences. 10. Vol. 33. Informa UK Limited; Kinematic and EMG activities during front and back squat variations in maximum loads; pp. 1058–1066. [DOI] [PubMed] [Google Scholar]
- Contreras Bret, Vigotsky Andrew D., Schoenfeld Brad J., Beardsley Chris, Cronin John. Journal of Applied Biomechanics. 1. Vol. 32. Human Kinetics; A Comparison of Gluteus Maximus, Biceps Femoris, and Vastus Lateralis Electromyography Amplitude in the Parallel, Full, and Front Squat Variations in Resistance-Trained Females; pp. 16–22. [DOI] [PubMed] [Google Scholar]
- Hamlyn Nicolle, Behm David G., Young Warren B. The Journal of Strength and Conditioning Research. 4. Vol. 21. Ovid Technologies (Wolters Kluwer Health); Trunk muscle activation during dynamic weight-training exercises and isometric instability activities; pp. 1108–12. [DOI] [PubMed] [Google Scholar]
- Andersen V., Fimland M.S., Brennset Ø., Haslestad L., Lundteigen M., Skalleberg K., Saeterbakken A. International Journal of Sports Medicine. 14. Vol. 35. Georg Thieme Verlag KG; Muscle activation and strength in squat and Bulgarian squat on stable and unstable surface; pp. 1196–1202. [DOI] [PubMed] [Google Scholar]
- Gullett Jonathan C, Tillman Mark D, Gutierrez Gregory M, Chow John W. Journal of Strength and Conditioning Research. 1. Vol. 23. Ovid Technologies (Wolters Kluwer Health); A biomechanical comparison of back and front squats in healthy trained individuals; pp. 284–292. [DOI] [PubMed] [Google Scholar]
- Biscarini Andrea, Benvenuti Paolo, Botti Fabio, Mastrandrea Francesco, Zanuso Silvano. Journal of Sports Sciences. 5. Vol. 29. Informa UK Limited; Modelling the joint torques and loadings during squatting at the Smith machine; pp. 457–469. [DOI] [PubMed] [Google Scholar]
- Straub Rachel K., Barrack Adam J., Cannon Jordan, Powers Christopher M. Journal of Sport Rehabilitation. 6. Vol. 30. Human Kinetics; Trunk Inclination During Squatting is a Better Predictor of the Knee-Extensor Moment Than Shank Inclination; pp. 899–904. [DOI] [PubMed] [Google Scholar]
- Barrack Adam J, Straub Rachel K, Cannon Jordan, Powers Christopher M. International Journal of Sports Science & Coaching. 4. Vol. 16. SAGE Publications; the relative orientation of the trunk and tibia can be used to estimate the demands on the hip and knee extensors during the barbell back squat; pp. 1004–1010. [DOI] [Google Scholar]
- Lee Tae-Sik, Song Min-Young, Kwon Yu-Jeong. Journal of Physical Therapy Science. 12. Vol. 28. Society of Physical Therapy Science; Activation of back and lower limb muscles during squat exercises with different trunk flexion; pp. 3407–3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esola Marcia A., McClure Philip W., Fitzgerald G. Kelley, Siegler Sorin. Spine. 1. Vol. 21. Ovid Technologies (Wolters Kluwer Health); Analysis of lumbar spine and hip motion during forward bending in subjects with and without a history of low back pain; pp. 71–78. [DOI] [PubMed] [Google Scholar]
- McGill Stuart M. Journal of Biomechanics. 5. Vol. 30. Elsevier BV; The biomechanics of low back injury: implications on current practice in industry and the clinic; pp. 465–475. [DOI] [PubMed] [Google Scholar]
- McGill Stuart M, Hughson Richard L, Parks Kellie. Clinical Biomechanics. 10. Vol. 15. Elsevier BV; Changes in lumbar lordosis modify the role of the extensor muscles; pp. 777–780. [DOI] [PubMed] [Google Scholar]
- Kernozek Thomas W., Gheidi Naghmeh, Zellmer Matthew, Hove Jordan, Heinert Becky L., Torry Michael R. Journal of Sport Rehabilitation. 3. Vol. 27. Human Kinetics; Effects of anterior knee displacement during squatting on patellofemoral joint stress; pp. 237–243. [DOI] [PubMed] [Google Scholar]
- Effect of knee position on hip and knee torques during the barbell squat. Fry A.C., Smith J.C., Schilling B.K. 2003J Strength Cond Res. 17(4):629–33. doi: 10.1519/1533-4287(2003)017<0629:eokpoh>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Lorenzetti Silvio, Gülay Turgut, Stoop Mirjam, List Renate, Gerber Hans, Schellenberg Florian, Stüssi Edgar. Journal of Strength and Conditioning Research. 10. Vol. 26. Ovid Technologies (Wolters Kluwer Health); Comparison of the angles and corresponding moments in the knee and hip during restricted and unrestricted squats; pp. 2829–2836. [DOI] [PubMed] [Google Scholar]
- Pangan Aaron Michael, Leineweber Matthew. Journal of Biomechanical Engineering. 9. Vol. 143. ASME International; Footwear and elevated heel influence on barbell back squat: A review. [DOI] [PubMed] [Google Scholar]
- Legg Hayley S., Glaister Mark, Cleather Daniel J., Goodwin Jon E. Journal of Sports Sciences. 5. Vol. 35. Informa UK Limited; The effect of weightlifting shoes on the kinetics and kinematics of the back squat; pp. 508–515. [DOI] [PubMed] [Google Scholar]
- Han Shuyang, Ge Shirong, Liu Hongtao, Liu Rong. Journal of Human Kinetics. 1. Vol. 39. Termedia Sp. z.o.o.; Alterations in three-dimensional knee kinematics and kinetics during neutral, squeeze and outward squat; pp. 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ninos Joel C., Irrgang James J., Burdett Ray, Weiss Jeffery R. Journal of Orthopaedic & Sports Physical Therapy. 5. Vol. 25. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Electromyographic analysis of the squat performed in self-selected lower extremity neutral rotation and 30 degrees of lower extremity turn-out from the self-selected neutral position; pp. 307–315. [DOI] [PubMed] [Google Scholar]
- Signorile Joseph F., Kacsik Denise, Perry Arlette, Robertson Bobby, Williams Richard, Lowensteyn Ilka, Digel Sarah, Caruso John, LeBlanc William G. Journal of Orthopaedic & Sports Physical Therapy. 1. Vol. 22. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); The effect of knee and foot position on the electromyographical activity of the superficial quadriceps; pp. 2–9. [DOI] [PubMed] [Google Scholar]
- Pereira Glauber Ribeiro, Leporace Gustavo, Chagas Daniel, Furtado Luis F L, Praxedes Jomilto, Batista Luiz A. Journal of Strength and Conditioning Research. 10. Vol. 24. Ovid Technologies (Wolters Kluwer Health); Influence of hip external rotation on hip adductor and rectus femoris myoelectric activity during a dynamic parallel squat; pp. 2749–2754. [DOI] [PubMed] [Google Scholar]
- Lahti Johan, Hegyi András, Vigotsky Andrew D., Ahtiainen Juha P. Scandinavian Journal of Medicine & Science in Sports. 1. Vol. 29. Wiley; Effects of barbell back squat stance width on sagittal and frontal hip and knee kinetics; pp. 44–54. [DOI] [PubMed] [Google Scholar]
- Swinton Paul A., Lloyd Ray, Keogh Justin W. L., Agouris Ioannis, Stewart Arthur D. Journal of Strength and Conditioning Research. 7. Vol. 26. Ovid Technologies (Wolters Kluwer Health); A biomechanical comparison of the traditional squat, powerlifting squat, and box squat; pp. 1805–1816. [DOI] [PubMed] [Google Scholar]
- Escamilla RAFAEL F., Fleisig GLENN S., Lowry TRACY M., Barrentine STEVEN W., Andrews JAMES R. Medicine and Science in Sports and Exercise. 6. Vol. 33. Ovid Technologies (Wolters Kluwer Health); A three-dimensional biomechanical analysis of the squat during varying stance widths; pp. 984–998. [DOI] [PubMed] [Google Scholar]
- McCaw STEVEN T., Melrose DONALD R. Medicine & Science in Sports & Exercise. 3. Vol. 31. Ovid Technologies (Wolters Kluwer Health); Stance width and bar load effects on leg muscle activity during the parallel squat; pp. 428–436. [DOI] [PubMed] [Google Scholar]
- Paoli Antonio, Marcolin Giuseppe, Petrone Nicola. Journal of Strength and Conditioning Research. 1. Vol. 23. Ovid Technologies (Wolters Kluwer Health); The effect of stance width on the electromyographical activity of eight superficial thigh muscles during back squat with different bar loads; pp. 246–250. [DOI] [PubMed] [Google Scholar]
- Cotter Joshua A., Chaudhari Ajit M., Jamison Steve T., Devor Steven T. Journal of Strength and Conditioning Research. 7. Vol. 27. Ovid Technologies (Wolters Kluwer Health); Knee joint kinetics in relation to commonly prescribed squat loads and depths; pp. 1765–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace David A., Salem George J., Salinas Ruben, Powers Christopher M. Journal of Orthopaedic & Sports Physical Therapy. 4. Vol. 32. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Patellofemoral joint kinetics while squatting with and without an external load; pp. 141–148. [DOI] [PubMed] [Google Scholar]
- Bryanton Megan A., Kennedy Michael D., Carey Jason P., Chiu Loren Z.F. Journal of Strength and Conditioning Research. 10. Vol. 26. Ovid Technologies (Wolters Kluwer Health); Effect of squat depth and barbell load on relative muscular effort in squatting; pp. 2820–2828. [DOI] [PubMed] [Google Scholar]
- Zavala Linnea, Flores Victoria, Cotter Joshua A., Becker James. European Journal of Sport Science. 7. Vol. 21. Wiley; Patellofemoral joint kinetics in females when using different depths and loads during the barbell back squat; pp. 976–984. [DOI] [PubMed] [Google Scholar]
- Salem George J., Powers Christopher M. Clinical Biomechanics. 5. Vol. 16. Elsevier BV; Patellofemoral joint kinetics during squatting in collegiate women athletes; pp. 424–430. [DOI] [PubMed] [Google Scholar]
- Gorsuch Joshua, Long Janey, Miller Katie, Primeau Kyle, Rutledge Sarah, Sossong Andrew, Durocher John J. Journal of Strength and Conditioning Research. 9. Vol. 27. Ovid Technologies (Wolters Kluwer Health); The effect of squat depth on multiarticular muscle activation in collegiate cross-country runners; pp. 2619–2625. [DOI] [PubMed] [Google Scholar]
- da Silva Josinaldo J., Schoenfeld Brad J., Marchetti Priscyla N., Pecoraro Silvio L., Greve Julia M.D., Marchetti Paulo H. Journal of Strength and Conditioning Research. 6. Vol. 31. Ovid Technologies (Wolters Kluwer Health); Muscle activation differs between partial and full back squat exercise with external load equated; pp. 1688–1693. [DOI] [PubMed] [Google Scholar]
- Hip flexion angles during supine range of motion and bodyweight squats. Mata A.J., Hayashi H., Moreno P.A., Dudley R.I., Sorenson E.A. 2021Int J Exerc Sci. 14(1):912–918. doi: 10.70252/LMEG8374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The geometric curvature of the lumbar spine during restricted and unrestricted squats. Campos M.H., Alaman L.I., Seffrin-Neto A.A., Vieira C.A., MC D.E.P., CA D.E.L. 2016J Sports Med Phys Fitness. 57(6):773–781. doi: 10.23736/S0022-4707.16.06184-3. [DOI] [PubMed] [Google Scholar]
- Delitto Ronna S, Rose Steven J. Physical Therapy. 6. Vol. 72. Oxford University Press (OUP); An electromyographic analysis of two techniques for squat lifting and lowering; pp. 438–448. [DOI] [PubMed] [Google Scholar]
- Krzyszkowski John, Kipp Kristof. Journal of Sports Sciences. 17. Vol. 38. Informa UK Limited; Load-dependent mechanical demands of the lower extremity during the back and front squat; pp. 2005–2012. [DOI] [PubMed] [Google Scholar]
- Wallis Jason A, Roddy Leanne, Bottrell Judy, Parslow Sue, Taylor Nicholas F. Physical Therapy. 3. Vol. 101. Oxford University Press (OUP); A systematic review of clinical practice guidelines for physical therapist management of patellofemoral pain. [DOI] [PubMed] [Google Scholar]
- Powers Christopher M., Ho Kai-Yu, Chen Yu-Jen, Souza Richard B., Farrokhi Shawn. Journal of Orthopaedic & Sports Physical Therapy. 5. Vol. 44. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Patellofemoral joint stress during weight bearing and non-weight bearing quadriceps exercises; pp. 320–327. [DOI] [PubMed] [Google Scholar]
- Liao TZU-CHIEH, Yang NICHOLAS, Ho KAI-YU, Farrokhi SHAWN, Powers CHRISTOPHER M. Medicine & Science in Sports & Exercise. 9. Vol. 47. Ovid Technologies (Wolters Kluwer Health); Femur rotation increases patella cartilage stress in females with patellofemoral pain; pp. 1775–1780. [DOI] [PubMed] [Google Scholar]
- Nakagawa T.H., Serrão F.V., Maciel C.D., Powers C.M. International Journal of Sports Medicine. 11. Vol. 34. Georg Thieme Verlag KG; Hip and knee kinematics are associated with pain and self-reported functional status in males and females with patellofemoral pain; pp. 997–1002. [DOI] [PubMed] [Google Scholar]
- Effects of a band loop on lower extremity muscle activity and kinematics during the barbell squat. Foley R.C.A., Bulbrook B.D., Button D.C., Holmes M.W.R. 2017Int J Sports Phys Ther. 12(4):550–559. [PMC free article] [PubMed] [Google Scholar]
- Martins Eduardo C., Steffen Lucas B., Gomes Diogo, Herzog Walter, Haupenthal Alessandro, de Brito Fontana Heiliane. Journal of Functional Morphology and Kinesiology. 3. Vol. 7. MDPI AG; Looped elastic resistance during squats: How do band position and stiffness affect hip myoelectric activity? p. 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Effect of stance width and anthropometrics on joint range of motion in the lower extremities during a back squat. Demers E., Pendenza J., Radevich V., Preuss R. 2018Int J Exerc Sci. 11(1):764–775. doi: 10.70252/BWZE8275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade Renato, Pereira Rogério, van Cingel Robert, Staal J Bart, Espregueira-Mendes João. British Journal of Sports Medicine. 9. Vol. 54. BMJ; How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II) pp. 512–519. [DOI] [PubMed] [Google Scholar]
- Kotsifaki Roula, Korakakis Vasileios, King Enda, Barbosa Olivia, Maree Dustin, Pantouveris Michail, Bjerregaard Andreas, Luomajoki Julius, Wilhelmsen Jan, Whiteley Rodney. British Journal of Sports Medicine. 9. Vol. 57. BMJ; Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction; pp. 500–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinlee Alexander W., Dickenson Scott B., Hunter-Giordano Airelle, Snyder-Mackler Lynn. Sports Health: A Multidisciplinary Approach. 5. Vol. 14. SAGE Publications; ACL Reconstruction rehabilitation: Clinical data, biologic healing, and criterion-based milestones to inform a return-to-sport guideline; pp. 770–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keogh Michael J., Batt Mark E. Sports Medicine. 10. Vol. 38. Springer Science and Business Media LLC; A review of femoroacetabular impingement in athletes; pp. 863–878. [DOI] [PubMed] [Google Scholar]
- Ganz Reinhold, Leunig Michael, Leunig-Ganz Katharina, Harris William H. Clinical Orthopaedics & Related Research. 2. Vol. 466. Ovid Technologies (Wolters Kluwer Health); The etiology of osteoarthritis of the hip: an integrated mechanical concept; pp. 264–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agricola R, Weinans H. British Journal of Sports Medicine. 4. Vol. 50. BMJ; What is femoroacetabular impingement? pp. 196–197. [DOI] [PubMed] [Google Scholar]
- Bagwell Jennifer J., Snibbe Jason, Gerhardt Michael, Powers Christopher M. Clinical Biomechanics. Vol. 31. Elsevier BV; Hip kinematics and kinetics in persons with and without cam femoroacetabular impingement during a deep squat task; pp. 87–92. [DOI] [PubMed] [Google Scholar]
- Ayeni Olufemi, Chu Raymond, Hetaimish Bandar, Nur Liin, Simunovic Nicole, Farrokhyar Forough, Bedi Asheesh, Bhandari Mohit. Knee Surgery, Sports Traumatology, Arthroscopy. 4. Vol. 22. Wiley; A painful squat test provides limited diagnostic utility in CAM-type femoroacetabular impingement; pp. 806–811. [DOI] [PubMed] [Google Scholar]
- Ng K. C. Geoffrey, Lamontagne Mario, Labrosse Michel R., Beaulé Paul E. PLoS One. 1. Vol. 11. Public Library of Science (PLoS); Hip joint stresses due to cam-type femoroacetabular impingement: A systematic review of finite element simulations; p. e0147813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delp Scott L, Hess William E, Hungerford David S, Jones Lynne C. Journal of Biomechanics. 5. Vol. 32. Elsevier BV; Variation of rotation moment arms with hip flexion; pp. 493–501. [DOI] [PubMed] [Google Scholar]
- Bagwell Jennifer J., Powers Christopher M. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 10. Vol. 33. Elsevier BV; The influence of squat kinematics and cam morphology on acetabular stress; pp. 1797–1803. [DOI] [PubMed] [Google Scholar]
- Pizol Gustavo Zanotti, Ferro Moura Franco Katherinne, Cristiane Miyamoto Gisela, Maria Nunes Cabral Cristina. BMC Musculoskeletal Disorders. 1. Vol. 24. Springer Science and Business Media LLC; Is there hip muscle weakness in adults with chronic non-specific low back pain? A cross-sectional study; p. 798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKean Mark R, Dunn Peter K, Burkett Brendan J. Journal of Strength and Conditioning Research. 10. Vol. 24. Ovid Technologies (Wolters Kluwer Health); The lumbar and sacrum movement pattern during the back squat exercise; pp. 2731–2741. [DOI] [PubMed] [Google Scholar]
- Epidemiology of osteoarthritis. D'Ambrosia R.D. 2005Orthopedics. 28(2 Suppl):S201–205. doi: 10.3928/0147-7447-20050202-04. [DOI] [PubMed] [Google Scholar]
- Felson David T., Zhang Yuqing, Hannan Marian T., Naimark Allan, Weissman Barbara N., Aliabadi Piran, Levy Daniel. Arthritis & Rheumatism. 10. Vol. 38. Wiley; The incidence and natural history of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study; pp. 1500–1505. [DOI] [PubMed] [Google Scholar]
- Zhang Yuqing, Hunter David J., Nevitt Michael C., Xu Ling, Niu Jingbo, Lui Li-Yung, Yu Wei, Aliabadi Piran, Felson David T. Arthritis & Rheumatism. 4. Vol. 50. Wiley; Association of squatting with increased prevalence of radiographic tibiofemoral knee osteoarthritis: the Beijing Osteoarthritis Study; pp. 1187–1192. [DOI] [PubMed] [Google Scholar]
- Alnahdi Ali H., Zeni Joseph A., Snyder-Mackler Lynn. Sports Health: A Multidisciplinary Approach. 4. Vol. 4. SAGE Publications; Muscle impairments in patients with knee osteoarthritis; pp. 284–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englund Martin, Guermazi Ali, Lohmander Stefan L. Radiologic Clinics of North America. 4. Vol. 47. Elsevier BV; The role of the meniscus in knee osteoarthritis: a cause or consequence? pp. 703–712. [DOI] [PubMed] [Google Scholar]
- Clements K.M., Bee Z.C., Crossingham G.V., Adams M.A., Sharif M. Osteoarthritis and Cartilage. 5. Vol. 9. Elsevier BV; How severe must repetitive loading be to kill chondrocytes in articular cartilage? pp. 499–507. [DOI] [PubMed] [Google Scholar]
- Joint load during the parallel squat in powerlifting and force analysis of in vivo bilateral quadriceps tendon rupture. Nisell R. 1986Scand J Sports Sci. 8:63–70. [Google Scholar]
- Maquet P G, Van de Berg A J, Simonet J C. The Journal of Bone & Joint Surgery. 6. Vol. 57. Ovid Technologies (Wolters Kluwer Health); Femorotibial weight-bearing areas. Experimental determination; pp. 766–771. [DOI] [PubMed] [Google Scholar]
- Nagura Takeo, Matsumoto Hideo, Kiriyama Yoshimori, Chaudhari Ajit, Andriacchi Thomas P. Journal of Applied Biomechanics. 4. Vol. 22. Human Kinetics; Tibiofemoral joint contact force in deep knee flexion and its consideration in knee osteoarthritis and joint replacement; pp. 305–313. [DOI] [PubMed] [Google Scholar]