Abstract
Background and Aims
More effective preventive care can potentially be provided if the characteristics of both the first ever and the recurrent foot ulcers can be clarified. The purpose of this study was to characterize first ever and recurrent foot ulcers in diabetic patients.
Methods
This study was conducted as a secondary analysis of a prospective study that was entitled: “Factors associated with the discontinuation of wound care specialist clinic visits in patients with diabetic foot ulcers.” In 73 diabetes‐related foot ulcer patients who visited one wound clinic in Indonesia between August 2020 and February 2021, we investigated characteristics of the patients and wounds, healing period, and cost.
Results
Trauma was shown to be the primary cause of the diabetic foot ulcer in both the first ever foot ulcer (n = 48) and recurrent foot ulcer (n = 25) patient groups (95.8% and 100.0%, respectively). The DMIST score for the first ever foot ulcer patients was significantly higher than the DMIST score for the recurrent foot ulcers. This was found to be especially the case in the first ever foot ulcer patients, as not only were there signs of inflammation (45.8%), but there were also signs of local infection (35.4%), or osteomyelitis and signs of local infection (14.6%) present. In the eight first ever foot ulcer patients and in the nine recurrent ulcer patients who were able to be followed through complete healing, the costs found for the first ever foot ulcer patients were significantly higher as compared to the costs for the recurrent foot ulcer patients.
Conclusion
To avoid diabetes‐related foot ulcers, specialized educational programs on trauma prevention need to be established. Moreover, patients without diabetes‐related foot ulcer histories should be educated regarding the need to undergo early consultations before developing any infections.
Keywords: cost, DMIST, infection, osteomyelitis, wound
Key points
More effective preventive care can potentially be provided if the characteristics of both the first ever and the recurrent foot ulcers can be clarified.
First ever foot ulcer patients visiting the clinic had more serious conditions with infections compared to recurrent foot ulcer patients, with trauma the primary reason for the wounds in both patient groups.
To avoid diabetes‐related foot ulcers, specialized educational programs on trauma prevention need to be established. Moreover, patients without diabetes‐related foot ulcer histories should be educated regarding the need to undergo early consultations before developing any infections.
1. INTRODUCTION
Prevention of diabetes‐related foot ulcers is important, as this can affect the physical prognosis, life prognosis, and quality of life. A prior history of foot ulcers is one of the risk factors for diabetes‐related foot ulcers. 1 Thus, averting further recurrences is an important key factor in the prevention of diabetes‐related foot ulcers.
Sensory neuropathy, peripheral artery disease, preulcerative lesions, osteomyelitis, depression, and high HbA1c are known risk factors for recurrence, 2 with multiple studies previously showing the benefits of integrated foot care interventions. 3 , 4 , 5 Furthermore, more effective preventive care can potentially be provided if the characteristics of both the first ever and the recurrent foot ulcers can be clarified. The purpose of this study was to better describe the characteristics of both the first ever foot ulcer and the recurrent foot ulcer in diabetic patients.
2. MATERIALS AND METHODS
This study was conducted as a secondary analysis of a prospective observational study entitled: “Factors associated with the discontinuation of wound care specialist clinic visits in patients with diabetic foot ulcers.” 6 In 73 diabetes‐related foot ulcer patients who visited one private wound clinic in Pontianak, Indonesia between August 2020 and February 2021, we investigated characteristics of the patients and wounds, healing period, and cost. This clinic has an outpatient clinic and a five‐bed inpatient facility, staffed 24 h a day, 7 days a week by physicians and specialized wound care nurses. All patients were followed until completion of the healing. The study collected information on the characteristics of the patients, data on age, sex, body mass index, educational background, monthly income, duration of diabetes, whether or not there was a regular consultation for diabetes, HbA1c, blood glucose levels, results for the monofilament test, and the ankle brachial pressure index. The Semmes−Weinstein monofilament was conducted based on the Practical guidelines of the International Working Group on the Diabetic Foot. 1 Ankle brachial pressure index was measured using a handheld Doppler (Bidop ES‐100V3; Hadeco‐Kawasaki). For the characteristics of wounds, we collected data regarding the injury site, the cause of the diabetic foot ulcer, treatment, and the DMIST score. 7 Wound size was measured by length × width based on DMIST. Length was defined as the longest measurement of the wound; width was defined as the longest measurement perpendicular to the length. Osteomyelitis was determined to be a condition in which osteomyelitis was present based on clinical observation or medical records according to DMIST evaluation criteria. These measurements were taken by the same researcher who was a specialized wound care nurse, regardless of the first ever or recurrent foot ulcers. To calculate time to heal and number of visits, we counted the number of days from the first visit to the healing date completion and number of times they visited this clinic. Wound healing was defined as a total DMIST score of 0. In terms of costs, we examined expenses for the drugs, medical service, laboratory, equipment, and wound care service fees as direct costs, while the transportation costs for the patient's visits to the hospital were analyzed as indirect costs. Due to the Indonesian healthcare system, private clinics are not covered by insurance. Therefore, costs were calculated on an actual cost basis. As of February 1, 2021, 1 USD was converted to 14,036.7 IDR. 8
The study was conducted in compliance with the Declaration of Helsinki. The study protocol was approved by the Muhammadiyah School of Nursing Ethics Committee in Pontianak, Indonesia (01/II.I.AU/KET.ETIK/VIII/2020). All participants gave written informed consent.
2.1. Statistical analysis
First ever foot ulcer was defined as a foot ulcer that a foot ulcer occurring in a person who has never before had a foot ulcer, while a recurrent foot ulcer was defined as a new foot ulcer in a person who has a history of foot ulceration, irrespective of the location and time since the previous foot ulcer. 9 Continuous data were compared between first ever foot ulcer and recurrent foot ulcer using the t‐test or Mann−Whitney U test. Categorical data were compared between the first ever foot ulcer and recurrent foot ulcer patients using a χ 2 test or Fisher's exact test. All tests were two‐sided. SPSS version 22 was used for statistical analysis, with a significance level of p = 0.05.
3. RESULTS
There were 48 patients with first ever foot ulcer and 25 patients with recurrent foot ulcer (Figure 1, Table 1). The highest education background found for the first ever foot ulcer patients was elementary school (39.6%), with the highest monthly income for these patients determined to be 2−3 million IDR (43.8%). For the recurrent foot ulcer patients, the highest education background was senior high school (36.0%), with the highest monthly income determined to be 4−5 million IDR (44.4%). Regular diabetes visits were 66.7% and 92.0% for the first ever foot ulcers and recurrent foot ulcer patients, respectively.
Figure 1.
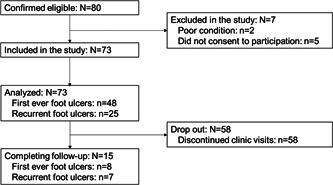
Flow diagram.
Table 1.
Characteristics of participants and ulcers.
| First ever foot ulcers (n = 48) | Recurrent foot ulcers (n = 25) | p | |
|---|---|---|---|
| (A) Characteristics of participants | |||
| Age (years) | 57.1 ± 8.6 | 53.6 ± 12.1 | 0.16a |
| Sex | 0.63b | ||
| Male | 24 (50.0) | 11 (44.0) | |
| Female | 24 (50.0) | 14 (56.0) | |
| Body mass index | 23.2 ± 3.1 | 23.7 ± 3.7 | 0.55a |
| Educational background | 0.04b | ||
| Elementary school | 19 (39.6) | 4 (16.0) | |
| Junior high school | 3 (6.3) | 4 (16.0) | |
| Senior high school | 16 (33.3) | 9 (36.0) | |
| Diploma | 6 (12.5) | 1 (4.0) | |
| Undergraduate | 4 (8.3) | 7 (28.0) | |
| Monthly income (million IDR/USD)d | 0.03b | ||
| 1−2/71.24−142.48 | 5 (10.4) | 5 (20.0) | |
| >2−3/>142.48−213.73 | 21 (43.8) | 6 (24.0) | |
| >3−4/>213.73−284.97 | 13 (27.1) | 2 (8.0) | |
| >4−5/>284.97−356.21 | 8 (16.7) | 11 (44.0) | |
| >5/>356.21 | 1 (2.1) | 1 (4.0) | |
| Duration of diabetes (years) | 8.8 ± 7.6 | 10.3 ± 5.9 | 0.39a |
| Regular consultation for diabetes | 0.02b | ||
| Yes | 32 (66.7) | 23 (92.0) | |
| No | 16 (33.3) | 2 (8.0) | |
| HbA1c (%) | 12.0 ± 1.9 | 12.2 ± 2.0 | 0.59a |
| Blood glucose levels (mg/dL) | 303.6 ± 106.0 | 309.6 ± 126.0 | 0.82a |
| Monofilament test | 0.57b | ||
| Normal | 32 (66.7) | 15 (60.0) | |
| Abnormal | 16 (33.3) | 10 (40.0) | |
| Ankle brachial pressure index | 1.03 ± 0.19 | 0.97 ± 0.17 | 0.17a |
| (B) Characteristics of ulcers | |||
| Wound site | 0.62b | ||
| Toes | 10 (20.8) | 7 (28.0) | |
| Dorsal | 4 (8.3) | 4 (16.0) | |
| Ankle | 2 (4.2) | 0 (0.0) | |
| Heel | 1 (2.1) | 1 (4.0) | |
| Plantar region | 20 (41.7) | 10 (40.0) | |
| Whole foot | 11 (22.9) | 3 (12.0) | |
| Cause of the diabetic foot ulcer | 0.59b | ||
| Trauma | 46 (95.8) | 25 (100.0) | |
| Callus | 1 (2.1) | 0 (0.0) | |
| Postoperation | 1 (2.1) | 0 (0.0) | |
| Systemic treatment | |||
| Antibiotic | 30 (62.5) | 12 (48.0) | 0.23b |
| Antithrombotic agent | 1 (2.1) | 2 (8.0) | 0.27c |
| Analgesic | 16 (33.3) | 4 (16.0) | 0.17c |
| Vitamin | 6 (12.5) | 1 (4.0) | 0.41c |
| Topical therapy | |||
| Sharp debridement | 28 (58.3) | 5 (20.0) | 0.003c |
| Modern dressing | 29 (60.4) | 23 (92.0) | 0.006c |
| Complementary dressing | 21 (43.8) | 2 (8.0) | 0.002c |
| DMIST score | |||
| Depth | 3.2 ± 1.3 | 2.4 ± 1.3 | 0.02a |
| Maceration | 1.0 ± 0.7 | 0.7 ± 0.6 | 0.02a |
| Inflammation/infection | 1.8 ± 1.1 | 0.9 ± 0.8 | 0.001a |
| Size | 4.4 ± 2.5 | 3.0 ± 2.1 | 0.02a |
| Tissue type of wound bed | 1.8 ± 0.6 | 1.6 ± 0.6 | 0.15a |
| Type of wound edge | 1.1 ± 0.3 | 1.6 ± 0.8 | 0.012a |
| Tunneling or undermining | 0.0 ± 0.1 | 0.0 ± 0.0 | 0.47a |
| Total | 13.4 ± 4.7 | 10.2 ± 3.8 | 0.006a |
| DMIST item frequency | |||
| Depth | 0.07b | ||
| 0: Intact | 0 (0.0) | 0 (0.0) | |
| 1: Superficial layer/epidermis | 4 (8.3) | 4 (16.0) | |
| 2: Subcutaneous/dermis to fatty tissue | 16 (33.3) | 15 (60.0) | |
| 3: Tendons | 1 (2.1) | 0 (0.0) | |
| 4: Fascia tissue and/or muscle | 19 (39.6) | 3 (12.0) | |
| 5: Bones | 8 (16.7) | 3 (12.0) | |
| Maceration | 0.28b | ||
| 0: None | 9 (18.8) | 9 (36.0) | |
| 1: Slight: only at wound edge | 32 (66.7) | 14 (56.0) | |
| 2. Moderate: surrounding skin | 4 (8.3) | 2 (8.0) | |
| 3: Heavy: beyond surrounding skin | 3 (6.3) | 0 (0.0) | |
| Inflammation/infection | 0.002b | ||
| 0: None | 2 (4.2) | 8 (32.0) | |
| 1: Signs of inflammation | 22 (45.8) | 12 (48.0) | |
| 2: Signs of local infection | 17 (35.4) | 4 (16.0) | |
| 3: Osteomyelitis | 0 (0.0) | 1 (4.0) | |
| 4: Osteomyelitis and signs of local infection | 7 (14.6) | 0 (0.0) | |
| 5: Systemic infection | 0 (0.0) | 0 (0.0) | |
| Size (cm2) | 0.13b | ||
| 0: Intact | 0 (0.0) | 0 (0.0) | |
| 1: ≤1 | 3 (6.3) | 6 (24.0) | |
| 2: <1 − ≤4 | 7 (14.6) | 8 (32.0) | |
| 3: <4 − ≤9 | 13 (27.1) | 2 (8.0) | |
| 4: <9 − ≤16 | 9 (18.8) | 5 (20.0) | |
| 5: <16 − ≤25 | 2 (4.2) | 1 (4.0) | |
| 6: <25 − ≤36 | 3 (6.3) | 1 (4.0) | |
| 7: <36 − ≤49 | 2 (4.2) | 1 (4.0) | |
| 8: <49 − ≤64 | 3 (6.3) | 0 (0.0) | |
| 9: >64 | 6 (12.5) | 1 (4.0) | |
| Tissue type of wound bed | 0.35b | ||
| 0: Intact | 0 (0.0) | 0 (0.0) | |
| 1: Granulation tissue or granulation cannot be assessed because the wound is healed or too shallow | 14 (29.2) | 11 (44.0) | |
| 2: White, yellow, and/or gray necrotic tissue | 29 (60.4) | 13 (52.0) | |
| 3: Black necrotic tissue | 5 (10.4) | 1 (4.0) | |
| 4: Gangrene | 0 (0.0) | 0 (0.0) | |
| Type of wound edge | 0.014b | ||
| 0: Complete epithelialization | 0 (0.0) | 0 (0.0) | |
| 1: No special feature/too shallow to assess | 43 (89.6) | 15 (60.0) | |
| 2: Hyperkeratosis/lining/epibole | 5 (10.4) | 7 (28.0) | |
| 3: Red ring | 0 (0.0) | 2 (8.0) | |
| 4: Ill‐defined or unable to assess due to infection etc. | 0 (0.0) | 1 (4.0) | |
| Tunneling or undermining (cm) | 0.47b | ||
| 0: None | 47 (97.9) | 25 (100.0) | |
| 1: ≤2 | 1 (2.1) | 0 (0.0) | |
| 2: <2 − ≤4 | 0 (0.0) | 0 (0.0) | |
| 3: <4 − ≤8 | 0 (0.0) | 0 (0.0) | |
| 4: >8 | 0 (0.0) | 0 (0.0) | |
Mean ± standard deviation or n (%), a t‐test, b χ 2 test, cFisher's exact test, dAs of February 1, 2021, 1 USD was converted to 14,036.7 IDR. 8
Trauma was shown to be the primary cause of the diabetic foot ulcer in both the first ever foot ulcer and recurrent foot ulcer patient groups (95.8% and 100.0%, respectively). The DMIST score for the first ever foot ulcer patients was significantly higher than the DMIST score for the recurrent foot ulcers (13.4 ± 4.7 and 10.2 ± 3.8, respectively; 95% confidence interval: 0.929−5.299). This was found to be especially the case in the first ever foot ulcer patients, as not only were there signs of inflammation (45.8%), but there were also signs of local infection (35.4%), or osteomyelitis and signs of local infection (14.6%) present. In contrast, some recurrent foot ulcer patients exhibited a red ring (8.0%) or an area that was ill‐defined or unable to be assessed due to the infection wound edges (4.0%). In the eight first ever foot ulcer patients and in the nine recurrent ulcer patients who were able to be followed through complete healing, the costs found for the first ever foot ulcer patients were significantly higher as compared to the costs for the recurrent foot ulcer patients (Table 2).
Table 2.
Comparison of healing days and cost between first ever foot ulcers and recurrent foot ulcers.
| First ever foot ulcers (n = 8) | Recurrent foot ulcers (n = 7) | p | |
|---|---|---|---|
| Healing time (days) | 43.5 (11−68) | 21 (4−62) | 0.07 |
| Number of visits (times) | 11.5 (5−27) | 5 (4−21) | 0.03 |
| Direct cost (USD) | |||
| Drug | 9.08 (0−5521.52) | 2.14 (0−6.41) | 0.07 |
| Medical service | 1.07 (0−2351.10) | 0 (0−3.56) | 0.69 |
| Laboratory | 3.56 (0−4096.61) | 0 (0−27.43) | 0.12 |
| Equipment | 43.60 (17.10−12,325.45) | 16.74 (11.04−81.14) | 0.014 |
| Wound care service | 63.05 (26.72−17,597.61) | 21.37 (16.03−138.92) | 0.02 |
| Total | 117.73 (50.94−38,757.48) | 49.16 (27.07−253.19) | 0.009 |
| Indirect cost (USD) | |||
| Transportation | 13.54 (4.70−5129.67) | 5.70 (1.78−44.88) | 0.28 |
| Total cost (USD) | 132.90 (65.19−39,541.18) | 50.94 (29.92−298.08) | 0.04 |
Median value (minimum value−maximum value), Mann−Whitney U test.
As of February 1, 2021, 1 USD was converted to 14,036.7 IDR. 8
4. DISCUSSION
To our knowledge, this study is the first time that the characteristics between diabetic patients with first ever and recurrent foot ulcers have been specifically elucidated and compared. The current results revealed that first ever foot ulcer patients visit clinics when there is a more serious condition combined with infection as compared to patients with recurrent foot ulcers.
Although the results are somewhat surprising, this may be a logical behavior, as recurrent foot ulcer patients would be expected to present at a wound clinic with milder foot ulcers, as compared to patients who are presenting with first ever foot ulcers. Even though the higher DMIST wound edge scores will need to be validated in detail with a larger sample size, the current results may indicate that these patients are seen at an earlier stage, at times before the wound edge has completely formed. Since all causes of the diabetic foot ulcer were associated with trauma, patients need to be educated about this, especially with regard to the toes and plantar region, as early evaluations of these areas are important in helping to prevent recurrent foot ulcers.
Patients with first ever foot ulcers, the majority of whom were triggered due to toe or plantar area trauma and visited wound clinics after the development of severe conditions with infection, were found to be associated with significantly higher costs for healing as compared to that encountered for recurrent foot ulcer patients. Furthermore, as it has been reported that the severity of foot ulcers can affect the cost, 10 , 11 the results found for the cost in this study are unsurprising. By providing education for patients on how to prevent trauma of the toe and plantar region, this would be effective in helping patients prevent the development of foot ulcers. In addition, persons with diabetes need to be educated about the importance of seeking medical attention early, before when an infection is present. Given that patients with recurrent ulcers were seen earlier, a virtual reality experience showing a foot ulcer from onset to healing may be an effective way to help educate patients with no history of diabetes‐related foot ulcers about the importance of seeing a doctor at a much earlier time point. Review of previous data has also revealed that many people do not undergo regular diabetes checkups, and thus, it may be necessary to provide additional information on importance of these actions along with assistance from insurance systems to encourage regular checkups regardless of one's educational background or monthly income.
Because this study was conducted in Indonesia, differences in the cost of living and in insurance systems must be taken into account when extrapolating the results of this study. Furthermore, as this study was a secondary analysis, the available data was limited, with details of the specific trauma often unknown, and recommendations for specific preventive education perhaps not sufficient with regard to improving patient knowledge of their physical conditions. The findings of this study are based on an analysis of limited data from a single institution, and there are many dropouts with respect to cost results. Interpretation should be done with extrapolation in mind. However, even with these limitations, the findings of our current study, which revealed the characteristics that are present between the first ever and recurrent foot ulcer patient groups, should be helpful in establishing guidelines for preventive care for each of these patient groups.
In conclusion, visits to clinics by patients with first ever foot ulcers were associated with more serious conditions along with infections as compared to those for patients with recurrent foot ulcers, with the majority of the cause of the diabetic foot ulcers found to be trauma of the toes and plantar regions in both patients with first ever and with recurrent foot ulcers. Therefore, to establish guidelines for the prevention of diabetes‐related foot ulcers, education programs on the prevention of trauma, especially to the toes and plantar regions, need to be specialized, regardless of whether the patients have a first ever or recurrent foot ulcers. Moreover, persons without any history of diabetes‐related foot ulcers should be provided with educational materials that stress the importance of early consultation with medical personnel before the occurrence of any infection.
AUTHOR CONTRIBUTIONS
Makoto Oe: Conceptualization; formal analysis; writing—original draft; writing—review and editing. Supriadi Syafiie Saad: Conceptualization; investigation; writing—review and editing. Suriadi Jais: Investigation; supervision; writing—review and editing. Junko Sugama: Supervision; writing—review and editing.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Makoto Oe affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ACKNOWLEDGMENTS
This work was supported by JSPS KAKENHI Grant Number 23H03193. The funder was not involved in study design; collection, analysis, and interpretation of data; writing of the report; or the decision to submit the report for publication.
Oe M, Saad SS, Jais S, Sugama J. Differences in characteristics between first‐ever foot ulcer and recurrent foot ulcer in patients with diabetes: prospective observational study. Health Sci Rep. 2024;7:e2018. 10.1002/hsr2.2018
Makoto Oe and Supriadi Syafiie Saad contributed equally to this study.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created in this study.
REFERENCES
- 1. Schaper NC, van Netten JJ, Apelqvist J, et al. Practical guidelines on the prevention and management of diabetes‐related foot disease. Accessed December, 22, 2023. https://iwgdfguidelines.org/wp-content/uploads/2023/07/IWGDF-2023-01-Practical-Guidelines.pdf [DOI] [PubMed]
- 2. Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367‐2375. [DOI] [PubMed] [Google Scholar]
- 3. Dargis V, Pantelejeva O, Jonushaite A, Vileikyte L, Boulton AJ. Benefits of a multidisciplinary approach in the management of recurrent diabetic foot ulceration in Lithuania: a prospective study. Diabetes Care. 1999;22(9):1428‐1431. [DOI] [PubMed] [Google Scholar]
- 4. Plank J, Haas W, Rakovac I, et al. Evaluation of the impact of chiropodist care in the secondary prevention of foot ulcerations in diabetic subjects. Diabetes Care. 2003;26(6):1691‐1695. [DOI] [PubMed] [Google Scholar]
- 5. Qin Q, Oe M, Nakagami G, et al. The effectiveness of a thermography‐driven preventive foot care protocol on the recurrence of diabetic foot ulcers in low‐medical resource settings: an open‐labeled randomized controlled trial. Int J Nurs Stud. 2023;146:104571. [DOI] [PubMed] [Google Scholar]
- 6. Supriadi SS, Okuwa M, Suriadi, Sanada H, Sugama J, Qe M. Factors associated with the discontinuation of wound care specialist clinic visits in patients with diabetic foot ulcers. J Jpn WOCM. 2023;26(4):335‐346. [Google Scholar]
- 7. Oe M, Yotsu RR, Arisandi D, et al. Validity of DMIST for monitoring healing of diabetic foot ulcers. Wound Repair Regen. 2020;28(4):539‐546. [DOI] [PubMed] [Google Scholar]
- 8. Xe historical currency exchange rates chart Accessed December, 21 2023. https://www.xe.com/ja/currencycharts/?from=USD&to=IDR&view=5Y
- 9. van Netten JJ, Bus SA, Apelqvist J, et al. Definitions and criteria for diabetes‐related foot disease (IWGDF 2023 update). Diabetes Metab Res Rev. 2023;15:e3654. [DOI] [PubMed] [Google Scholar]
- 10. Girod I, Valensi P, Laforêt C, Moreau‐Defarges T, Guillon P, Baron F. An economic evaluation of the cost of diabetic foot ulcers: results of a retrospective study on 239 patients. Diabetes Metab. 2003;29(3):269‐277. [DOI] [PubMed] [Google Scholar]
- 11. Prompers L, Huijberts M, Schaper N, et al. Resource utilisation and costs associated with the treatment of diabetic foot ulcers. Prospective data from the Eurodiale Study. Diabetologia. 2008;51(10):1826‐1834. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created in this study.


